Figure 1 Number of patients included in the study and the various analyses.
DOI: https://doi.org/10.4414/smw.2018.14659
Tuberculosis (TB) is a rare disease in Switzerland, with a constant decline in the number of notified cases up to 2007 [1]. Since then, the number of cases has been oscillating between 485 and 630 per year, with some indication of an increase from 2014 to 2016 [2]. For 2015, the World Health Organization reports for Switzerland an incidence rate of 7.4 per 100,000 population, similar to that of neighbouring countries (5.8 per 100,000 in Italy, 7.6 in Austria, 8.1 in Germany and 8.2 in France) [3].
As TB is an airborne transmissible disease, early diagnosis and appropriate treatment are important to reduce transmission of bacteria to the population. TB is often a slowly progressive disease, and therefore there may be a delay between the beginning of the symptoms, the first medical visit and the initiation of adequate treatment. This in turn depends on the awareness and sensitivity of the patients with symptoms, the ease of access to health care, and the knowledge level and alertness of the healthcare providers. Recent studies among TB patients in Europe have found a patient delay (the time from symptom onset to the first visit to a doctor) of between 2 and 4.5 weeks, and a health system delay (the time from the first medical visit to the start of TB treatment) of between 2 and 5.5 weeks [4–9].
To better understand the experiences of pulmonary TB patients in Switzerland before appropriate treatment is provided, the Federal Office of Public Health of Switzerland commissioned the Swiss Tropical and Public Health Institute to perform two studies: (i) a study on the knowledge level of general practitioners (family doctors) in Switzerland regarding tuberculosis and its management and (ii) a study of the experiences of patients with pulmonary TB, with a focus on the various delays between symptom onset and start of TB treatment (TB delay study). The first study, published in 2016, identified some uncertainties among general practitioners, mostly about the proper use of various diagnostic tests and on how to correctly conduct a contact investigation [10]. This paper presents the TB delay study. The main objectives of the study were: (i) to assess the various delays (onset of symptoms to first consultation and first consultation to start of TB treatment); and (ii) to establish the predictors of the various types of delay.
The study was approved by the ethics commission of Northwest- and Central Switzerland (Ethikkommission Nordwest- und Zentralschweiz; reference number EK: 328/13).
We carried out a survey in the cantons Aargau, Baselland, Geneva, Solothurn, Vaud and Zurich from November 2014 to June 2016 among patients with pulmonary tuberculosis. It was not feasible to include all cantons, thus four German-speaking and two French-speaking cantons were selected, all of them with a high number of TB cases compared with most other cantons. Patients were eligible if they had been diagnosed with smear- or culture-positive pulmonary tuberculosis and were at least 18 years old. All patients with residency in any of the six cantons and notified to the cantonal lung associations through the cantonal medical officer (Kantonsarzt) were included in the study.
For the patient interview, healthcare professionals of the cantonal lung associations, mandated by the cantonal health officer for the ambulatory care of TB patients and for contact investigations, approached the patients. The patients from Baselland were interviewed by the lung association Solothurn. With a few exceptions (mostly patients of very high age), all registered TB patients were invited by the healthcare providers of the lung associations to participate, and asked to provide written consent. The patients were interviewed face-to-face, at home or in an ambulatory care setting, between November 2014 and July 2016. Interviewers (mostly trained nurses) were experienced in taking care of TB patients. Given that some patients were not fluent in the local language of their canton, professional interpreters were solicited when required.
The paper-based questionnaire (available in German, French and English) consisted mainly of closed questions covering the following areas: (i) demographic data about the patient; (ii) beginning of the symptoms suggestive of TB; (iii) initial and follow-up contacts with the healthcare system; and (iv) personal situation when the symptoms began and when a health care provider was approached (the questionnaire is provided in appendix 1).
TB delay was captured through questions regarding the date of the start of symptoms (or the date when a healthcare provider was consulted if the health seeking was not triggered by symptoms), the date when the patient realised that a medical visit was needed (for establishing the “realisation delay”), the date of the first contact with the healthcare system (usually a doctor), and the date of the start of TB treatment.
For this study, the following concepts of delay were used:
The healthcare professionals of the participating lung associations wrote the answers provided by the patients during their interviews on a paper questionnaire form. Data from these forms were independently double entered into EpiData (version 3.1) and inconsistencies were addressed. Datasets were exported into STATA (Version 14.0) to carry out the statistical analyses.
The main focus of the data analysis was to study the predictors of the various delays (patient delay, including realisation delay and access delay, and the health system delay).
After careful deliberation, we decided to assess predictors of delay using quantile regression. Whereas classical linear regression is used to model the mean of a quantitative outcome variable, quantile regression allows modelling of specific percentiles instead. We focused on the median (P50) and the 75th percentile (P75) of the respective outcome variable (i.e., one of the delay times in our case). These models have the following forms:
All models included the core variables: sex, age, canton of residence, education level and indicator variables for “Swiss citizenship”, “smoker’s cough” and “status of asylum seeker”. These core variables were chosen on the basis of a review of the relevant literature and on our understanding of the situation of TB health seeking in Switzerland. Additional variables were added to the core model one by one.
In this article, we present results for median delay times, whereas results for the 75th percentile can be found in appendix 2.
Sex, age, canton of residence and nationality were assessed for all eligible and registered patients, including the nonparticipants. This enabled analyses adjusting for self-selection bias using inverse probability weighting (IPW). This method consists of giving observations from under-represented groups higher weights and observations from over-represented groups lower weights in the analyses. The weight of an observation is defined as the inverse of the respective person’s probability of accepting participation in the study, and these probabilities are estimated using a logistic regression model for the outcome “acceptance of participation”. All gathered variables, namely, age, sex, nationality (Swiss vs non-Swiss) and canton of residence, were included into this model. Results of the weighted analyses (IPW) are presented in appendix 2.
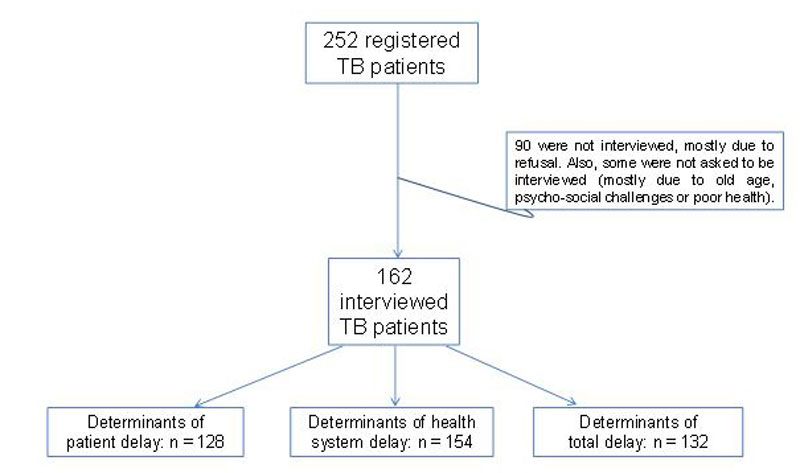
In the six cantons covered by the study, 252 patients were registered between November 2014 and June 2016. This represents 42% of all pulmonary TB cases (n = 601 [11]) aged 18 years and above registered in Switzerland over the study period. Among the 252 eligible cases, 162 could be interviewed (participation rate of 64%, ranging from 56% in the canton of Geneva to 93% in canton Aargau). Most of the others refused, some were not asked to be interviewed (mostly due to old age, psychosocial challenges or poor health status), and two died. Figure 1 presents the number of patients interviewed and the number of patients included in the various analyses.
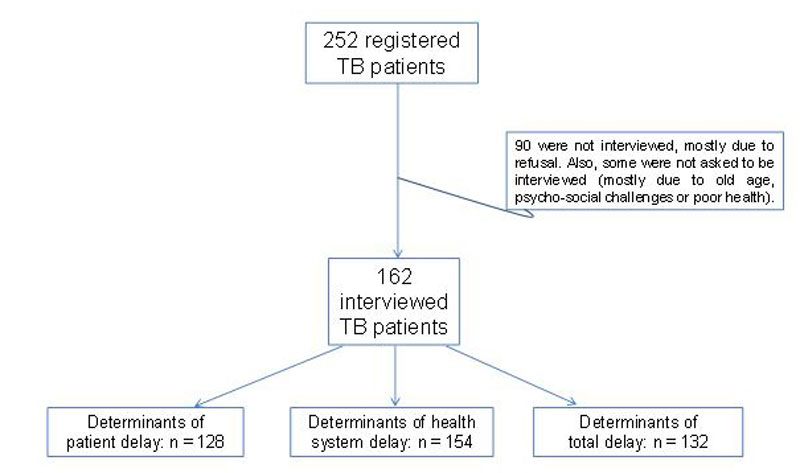
Figure 1 Number of patients included in the study and the various analyses.
The median age of the 162 participants was 35 years; 66% were male. Only 20.4% (33/162) were born in Switzerland. Among the 129 foreign-born patients (79.6%), 67 were working or living in Switzerland (15 of them had in the meantime acquired Swiss citizenship) and 62 were asylum seekers. Among the 62 asylum seekers, 22 had been granted refugee status; for 33, this was pending and for 7, the request for asylum had been rejected.
Among the non-Swiss patients, the most common countries of origin were Eritrea (n = 24), Portugal (n = 9), China (all from Tibet) (n = 7), Afghanistan (n = 6), Italy (n = 6), Germany (n = 4) and Somalia (n = 4). Among the six participating cantons, Geneva had the highest rate of non-Swiss and male participants (90.9 and 78.8%, respectively, of the 26 participants).
Sixty percent of the interviews were conducted in either German (30.3%) or French (29.6%), and 8% in English. Fifty-two interviews (32.1%) were conducted in other languages (see appendix 3), 49 of them with the help/intervention of an interpreter.
The median age of the 90 registered cases who did not participate in the study was 41 years, significantly higher than the median age of the participants (p = 0.02). Among those included, 9.3% (15/162) were older than 70 years: 13 of the 48 participants with Swiss citizenship (27.1%) versus 2 of the 114 non-Swiss participants (1.8%) (p <0.001). One third of the patients born in Switzerland (11/33) were older than 70 years.
Table 1 presents the patient characteristics in detail.
Table 1 Characteristics of the 162 tuberculosis patients interviewed.
| Patient characteristics | Number |
Percentage
(of 162) |
|---|---|---|
| Sex | ||
| Male | 107 | 66.0% |
| Female | 55 | 34.0% |
| Age | Median age was 35 years | |
| 18 to 29 years | 56 | 34.6% |
| 30 to 44 years | 57 | 35.2% |
| 45 to 59 years | 21 | 13.0% |
| 60 to 74 years | 16 | 9.9% |
| 75 to 90 years | 12 | 7.4% |
| Education | ||
| 0 to 5 years | 29 | 17.9% |
| 6 to 9 years | 56 | 34.6% |
| At least 10 years | 74 | 45.7% |
| Not clear | 3 | 1.9% |
| Country of birth | ||
| Switzerland | 33 | 20.4% |
| Elsewhere in Europe | 21 | 13.0% |
| Other | 108 | 66.7% |
| Nationality at time of interview | ||
| Swiss | 48* | 29.6% |
| Other European country | 38 | 23.5% |
| Other | 93† | 57.4% |
| Occupation when patient went to doctor for the first time | ||
| Employed | 55 | 34.0% |
| In asylum-seeking process | 41 | 25.3% |
| Retired | 24 | 14.8% |
| Jobless | 14 | 8.6% |
| Receiving social security pension | 12 | 7.4% |
| In school / training | 9 | 5.6% |
| Other (e.g., traveller) | 7 | 4.3% |
* 13 of with a second nationality †The total is higher than 162 because of 17 participants with two nationalities.
The study participants were asked about their knowledge on TB at the moment they had realised that they should visit a doctor. Approximately three quarters knew that TB is an infectious disease, that TB can kill and that TB can be treated (table 2).
Table 2 Knowledge of and experience with tuberculosis (TB).
| Knowledge/experience | Among the 162 participants | Among the 33 born in Switzerland | Among the 129 not born in Switzerland | |
|---|---|---|---|---|
| n | % | % | % | |
| TB is an infectious disease | 122 | 75.3% | 84.8% | 72.9% |
| TB can be deadly | 115 | 74.7% | 78.8% | 69.0% |
| TB can be treated | 121 | 71.0% | 81.8% | 72.9% |
| Knew at least one person who had had TB | 78 | 48.1% | 39.4% | 50.4% |
| Knew at least one person who had died of TB | 27 | 16.7% | 9.1% | 18.6% |
| Patient had had TB before the current TB episode | 15 | 9.3% | 0% | 11.6%* |
* This difference was statistically significant (p = 0.042, Fisher’s exact test, two-tailed).
The main complaint was cough, mentioned by 75.9% of patients. Other symptoms were less frequent (fig. 2). Among the 39 patients (24.1%) without cough, 9 (5.6% of the 162) had none of the other five symptoms commonly associated with tuberculosis (haemoptysis, tiredness, weight loss, sweating, chest pain). Four patients stated that they did not experience any symptom at all during the time before the start of TB treatment; they had a medical consultation because it had been planned in advance, for example, in the frame of a routine medical visit.
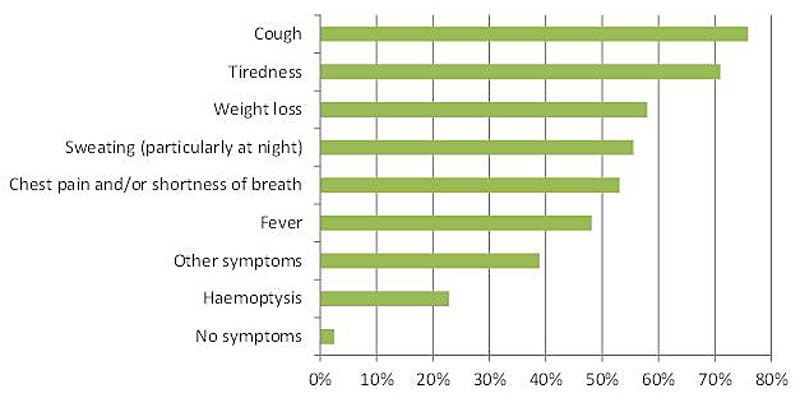
Figure 2 Frequency of symptoms among the 162 tuberculosis patients.
The most commonly identified comorbidities were smoker’s cough (14.8%) and chronic obstructive pulmonary disease (COPD) / bronchitis / asthma (11.1%). Seven patients mentioned alcoholism and six the use of illicit drugs. Five of the 162 TB patients were reportedly infected with the human immunodeficiency virus (HIV).
For most participants, the first medical consultation with a medical doctor took place in Switzerland; only 8% had first visited a doctor outside Switzerland (11 of these 13 were not Swiss). Almost half of the patients first visited a general practitioner in an ambulatory care setting (table 3).
Table 3 Place of the first consultation in Switzerland.
| Place of the first consultation | n | % |
|---|---|---|
| Primary care physician’s office | 74 | 45.7% |
| Hospital | 42 | 25.9% |
| Emergency / walk-in clinic | 14 | 8.6% |
| Doctor of the asylum-seeking centre / doctor of an institution | 10* | 6.1% |
| Practice of a paediatrician or pulmonologist | 4 | 2.5% |
| Other | 18 | 11.1% |
* Nine refugees and one prisoner
During this first consultation, 90% underwent a physical examination and 78.3% blood testing. For 58.6% of the patients, a chest X-ray was taken during the first consultation or a referral for an X-ray examination ordered. The three most common outcomes of this first consultation were: (i) prescription of medicines other than TB medication (for 57.6%); (ii) agreement to a second visit (for 36.1%) and (iii) referral to a hospital (for 34.1%).
Approximately one third of the patients (35.2%) had only one or two doctor appointments in Switzerland during the time from onset of symptoms to the start of TB treatment; 44.4% had three, four or five appointments and 16% had more than five appointments (for 3.7% the number was not clear).
The patient delay estimate was based on the reports of 128 patients. For another 34 patients, estimating the patient delay was not applicable: 4 patients had no symptoms, for 7 patients the data were incomplete and 23 patients went to see a doctor because this had already been agreed upon some time previously or because a medical visit was part of an on-going process (mostly among asylum seekers).
The median delay between symptom onset and first healthcare contact was 5.2 weeks (mean 2 weeks). The interquartile range was 1.6 to 14.2 weeks. The median delay ranged from 3 weeks in the canton of Zurich to 9.4 weeks in the canton of Geneva. Overall, the differences between the cantons were not statistically significant. However, when Geneva was compared with the other cantons, the patient delay was significantly longer in Geneva (p = 0.009; Wilcoxon rank sum test).
The median realisation delay was 4.1 weeks; one quarter had a realisation delay of 14 weeks or longer. The median access delay (among the 115 patients with data related to access delay) was 0 days (mean 1.7 weeks). In other words, many patients immediately accessed healthcare once they concluded that they needed health care. One quarter of the patients had an access delay of 1.3 week or longer.
Health system delay was estimated for 154 patients; data from eight patients were incomplete. The median delay between first consultation in Switzerland and the start of TB treatment was 2 weeks (mean 6.3 weeks). The interquartile range was 0.6 to 7.1 weeks. The median delay was shortest in canton Aargau (1.2 weeks) and longest in canton Vaud (3.3 weeks) (difference statistically not significant).
Total delay was estimated for 132 patients. The median delay between symptom onset and the start of TB treatment was 11.5 weeks (mean 22.6 weeks). The interquartile range was 5.6 to 22.5 weeks. The median delay was shortest in canton Baselland and longest in canton Geneva (no statistically significant differences).
Figure 3 presents an overview of the various delays.
Figure 3 Overview of the various delays (median) and their extent.
The quantile P50 regression analysis showed that there were no predictors of patient delay (appendix 2 presents P75 regression findings, with and without IPW, where some statistically significant predictors were identified). When the 16 patients who had a patient delay of 0 days were excluded from the analysis, the results were unchanged. Similarly, there were no statistically significant predictors for realisation delay nor for access delay (when applying P50 without IPW).
The symptom fever was a predictor of a longer health system delay: the estimated time span until 50% of the patients with fever had started TB treatment after the first consultation was 1.6 weeks longer (95% confidence interval [CI] 0.5 to 2.6 weeks) than the corresponding time span for the patients without fever (p = 0.004). Surprisingly, even patients who had fever and sweating and weight loss (n = 45) had a longer health system delay than patients without fever (p = 0.003). The estimated health system delay until 50% of the patients that had gone for the first consultation to a general practitioner or paediatrician was 1 week longer (95% CI 0.1 to 1.9 weeks) than the corresponding time for the patients not having gone to a general practitioner or paediatrician as first consultation. Not surprisingly, patients who visited three or four doctors during their journey from first consultation to start of TB treatment had a longer health system delay than patients who visited only one or two doctors for the same health trouble. Predictors of a longer delay with borderline significance (p-values between 0.051 and 0.098) were living in canton Vaud compared with living in Aargau, living in canton Zurich compared with living in Aargau, the symptom chest pain and comorbidity COPD.
A strong predictor for a short health system delay was having undergone an X-ray at the first consultation: the time until 50% of the patients that had an X-ray at their first consultation began treatment was 2.9 weeks shorter (95% CI −4.8 to −0.9 weeks) than the time until 50% of the patients without an X-ray at the first consultation began treatment. Being male was a predictor for a short health system delay with borderline statistical significance: being male was associated with a health system delay shorter by 2.6 weeks (95% CI −5.4 to 0.1 weeks). Table 4 presents details; it also presents predictors at the level p <0.1.
Table 4 Predictors of health system delay (P50 quantile regression model; n = 154).
| Predictor | Effect* (95% CI) | p-value | |
|---|---|---|---|
| Predictors of a long delay | |||
| Fever | 1.6 (0.5 to 2.6) | 0.004 | |
| First consultation at a general practitioner or paediatrician | 1.0 (0.1 to 1.9) | 0.024 | |
| 3 to 4 doctors seen until start of TB treatment (versus only 1 or 2) | 2.9 (0.7 to 5.1) | 0.01 | |
| Living in VD (compared with AG) | 1.9 (−0.004 to 3.8) | 0.051 | |
| Living in ZH (compared to AG) | 1.7 (−0.2 to 3.7) | 0.083 | |
| Chest pain | 1.8 (−0.2 to 3.7) | 0.071 | |
| Comorbidity COPD | 3.7 (−0.7 to 8.0) | 0.098 | |
| Predictors of a short delay | |||
| X-ray was taken at first consultation | −2.9 (−4.8 to −0.9) | 0.004 | |
| Male sex | −2.6 (−5.4 to 0.1) | 0.060 | |
AG = canton Aargau; CI = confidence interval; COPD = chronic obstructive pulmonary disease; TB = tuberculosis; VD = canton Vaud; ZH = canton Zurich All estimates were obtained from models which (also) included sex, age, nationality, canton of residence, education level and indicator variables for “Swiss citizenship”, “smoker’s cough” and “status of asylum seeker”. * Effect expressed in weeks
Table 5 presents the predictors of total delay: there was no predictor of a long total delay. There was one statistically significant predictor of a short total delay: the time until 50% of the patients who had an X-ray at their first consultation began treatment was 5.5 weeks shorter (95% CI −10.8 to −0.2 weeks) than the time until 50% of the patients without an X-ray at the first consultation began treatment. Predictors of a short total delay with borderline statistical significance were having submitted a sputum sample at first consultation and having had a comorbidity other than COPD/bronchitis/asthma, diabetes mellitus, cancer, alcoholism, smoker’s cough, drug addiction or HIV (see table 5).
Table 5 Predictors of total delay (P50 quantile regression model; n = 132).
| Predictor | Effect* (95% CI) | p–value | |
|---|---|---|---|
| X-ray examination at first consultation | –5.5 (–10.8 to –0.2) | 0.043 | |
| Sputum submitted at first consultation | –5.0 (–10.4 to 0.3) | 0.064 | |
| Co-morbidity other than COPD/bronchitis/asthma, diabetes mellitus, cancer, alcoholism, smoker’s cough, drug addition, HIV† | –6.9 (–14.3 to 0.6) | 0.071 | |
CI = confidence interval; COPD = chronic obstructive pulmonary disease: HIV = human immunodeficiency virus * Effect expressed in weeks. † Mostly conditions occurring in only 1 patient; 3 patients mentioned hepatitis B and 2 mentioned hypertension.
The patient delay (median 5.2 weeks) is slightly longer than the patient delays reported from some publications from low-prevalence countries (2 weeks in France [5], 4 week days in Norway [9], 4.3 weeks in Qatar [12]), but compares favourably with findings from other studies (9 weeks in East London [13], 6.1 weeks in Spain [14]). This delay is mainly due to the slowly progressive nature of TB and depends on individual factors such as sensitivity to health trouble.
To our knowledge, this is the first study reporting separately the “realisation delay” and the “access delay”, defined as the delay between the awareness of a health trouble that needs medical consultation and the time of the first medical visit, as a proxy for access to health care. It is reassuring to note that this access delay is short (median 0 days, mean 1.7 weeks), indicating that health care is readily available for all patients living in Switzerland, whatever their origin or legal status, with some differences between the cantons.
The health system delay (median 2 weeks, mean 6.3 weeks) seems to be shorter than in other low-prevalence countries (median 3.6 weeks in France [5], 4.7 weeks in Norway [9], 4.9 weeks in England [7]), but it has to be noted that for one quarter of the patients the delay was longer than 7 weeks, which may be surprising in a country where diagnostic equipment is readily available. This long delay may be due to the fact that half of the patients first visited a general practitioner, who may have no or limited experience with TB, and that approximately half of the patients had to visit three or more doctors to have a final diagnosis established. Another explanation may be that often patients with tuberculosis have symptoms compatible with common diseases (e.g., influenza, exacerbation of COPD, pneumonia) though the prominence of tiredness and weight loss (see fig. 2) does not support this explanation. The evaluation of the health system delay did not include the asylum seekers who were submitted to immediate medical examination after entry in Switzerland, for whom the delay may have been influenced by travel conditions and access to care prior to the immigration.
This survey found that the health system delay, i.e., the delay between the first medical visit and the initiation of TB treatment, was longer for patients with fever, for those who first went to see a general practitioner or paediatrician, for those who did not have a chest X-ray at first consultation and for female patients.
The literature reports many factors associated with delays in realising that symptoms may be due to TB, delay in obtaining an appointment at a healthcare structure and delays between the first medical visit and the initiation of treatment. Some factors seem to be similar whatever the local prevalence of TB, and are therefore independent of the degree of familiarity of the medical professionals with TB, whereas others differ between the regions of the world. Furthermore, some factors seem to be associated with longer delays in some regions of the world and with short delays in others. According to a large meta-analysis published in 2008, chronic cough, female sex, low awareness of TB, limited access to health care and history of immigration are the most common risk factors for a prolonged total delay [15]. The association of fever and especially of the combination of fever, sweating and weight loss with a longer health system delay, which we have observed, is surprising and was not reported in other studies. It may be due to the fact that fever is a common symptom in many minor infectious diseases, particularly during winter, and is thus considered as a self-limiting symptom not requiring further medical examinations. However, the increased health system delay among patients with fever and sweating and weight loss, a combination of symptoms which should create strong suspicion that the patient may have TB, is worrying.
The total delay observed in this study is comparable with the result of a prior study conducted in Geneva between 1999 and 2003 [16].
The health system delay was shorter among foreign-born than Swiss patients (though this was only seen when applying the P75 regression); this may reflect a higher degree of suspicion of TB among the doctors when a foreign-born person has symptoms suggestive of TB.
Surprisingly, several studies mention the fact that the occurrence of haemoptysis, reflecting the presence of extended and severe disease with tissue destruction, may be associated with a prolonged patient delay [17], which did not seem to be the case in this study.
The access delay, i.e., delay in obtaining an appointment at a healthcare facility (usually a general practitioner or a hospital), was rather short in this study, as distance to the facilities do not play a major role in Switzerland compared with large countries or developing countries with scarce availability of health structures [18, 19]. Financial constraints play a minimal role as all persons living in Switzerland are covered by a mandatory health insurance scheme (with the exception of undocumented migrants and tourists).
Cough is the main symptom of pulmonary TB, but also of many other medical conditions and the vast majority of patients with chronic or persistent cough have a disease other than TB, particularly in regions where TB is a rare disease [20]. For cost containment reasons, doctors are expected to use diagnostic procedures with caution. It is, therefore, not surprising that in most patients with cough a radiographic examination or a sputum test is not performed at the first visit, particularly if they are smokers. This translates into a risk factor for a prolonged health system delay. The correct balance should be a high level of suspicion of TB in the presence of additional risk factors for TB, such as a history of contact with TB, origin from a region with a high TB prevalence, association with other suggestive symptoms and progressive nature of the complaints. In situations where the likelihood of TB is elevated, performing a radiographic examination of the chest and – if abnormal – ordering a sputum examination is the appropriate procedure [21–23]. The Federal Office of Public Health of Switzerland has developed an automated, web-based interview tool for identifying people at high risk of having TB (www.tb-screen.ch), a tool that can also be used by general practitioners. Not performing the appropriate examination in due time may result in patients visiting the same facility repeatedly or searching for help at another healthcare insitution, thus prolonging the duration of transmission of mycobacteria [7, 12, 24].
Swiss-born patients tended to have a shorter access delay but had a longer health system delay than foreign-born patients (in P75 results). A similar observation has also been made in Italy, where Italian-born patients had a shorter patient delay than foreign-born migrants (median 0.4 vs 2 weeks) but a longer health-care delay (median 8.6 vs 2.6 weeks) [25]. This can be because Swiss citizens have better knowledge of available health services and are used to rapidly visiting a general practitioner in the event of health trouble, but that doctors rarely consider TB as a possible cause of cough, fever and fatigue among Swiss citizens, particularly as they seldom have the opportunity to detect TB in the resident population.
A weakness of this study is the incomplete recruitment of patients, some of whom were excluded for individual reasons (high age, difficult communication) or refused to participate. For these reasons, we performed a sensitivity analysis using inverse probability weights (IPW) to adjust for differences in participation rate associated with baseline characteristics of the patients. This resulted in effect estimates that were for the most part similar. Although this argues against the presence of major participation bias, some bias associated with unobserved characteristics of nonparticipants may have remained.
Patients were interviewed while still on treatment. However, the questions relating to delay referred to events in the past. Therefore, some recall bias cannot be excluded. Recall bias could not be addressed in the analysis.
Another limitation of the study is that patients from only six cantons were recruited. Thus, some findings may not be representative of the situation in Switzerland as a whole. For instance, in this study, there were only four patients from Somalia. Had canton Ticino also been included in the study, the number of patients from Somalia (and from other African countries) would have been higher as many asylum seekers from Somalia enter Switzerland through canton Ticino.
As TB is a slowly progressive disease, some delay in its diagnosis and treatment is unavoidable, but should be kept to a minimum. Easy access to health care for all should be granted, including migrants, underserved populations, patients without insurance coverage or patients with additional comorbidity. Transmission of medical information, including for cross-border migrants, is necessary for the adequate management of patients with unstable residency [26, 27]. Continuous medical education and regular reminders for general practitioners (including paediatricians) working in the ambulatory care setting, who may be the first to examine patients with symptoms suggestive of TB, is necessary for avoiding undue delays in diagnosis. In many countries, TB is the disease of limited, hard-to-reach populations. Interventions to facilitate the access of these vulnerable groups to health care, including efficient administrative procedures between facilities/shelters for arriving asylum seekers and appropriate education of the healthcare workers, may decrease the delay and associated transmission of the disease [28].
The appendices are available as separate files for downloading at https://smw.ch/en/article/doi/smw.2018.14659/
We are grateful for the excellent support received from numerous staff members of the cantonal lung associations. We thank the patients for their willingness to be interviewed. We are also grateful to the Kantonsärzte (cantonal medical officers) of the cantons Aargau, Baselland, Geneva, Solothurn, Vaud and Zurich for allowing this study.
This study was supported by a grant from the Federal Office of Public Health, given to the Swiss Tropical and Public Health Institute for conducting two TB studies in Switzerland: one on the knowledge of general practitioners on TB and the here described so-called TB delay study.
We report no conflict of interest or potential conflict of interest relevant to this article.
1 Brändli O . Tuberkulose aktuell. Swiss Med Forum. 2013;13(25):493–8. doi:https://doi.org/10.4414/smf.2013.01541
2Figures received from the Federal Office of Public Health in March 2017.
3 http://www.who.int/tb/country/data/profiles/en/, accessed on 29 March 2017.
4 Pezotti P , Pozzato S , Ferroni E , Mazzocato V , Altieri AM , Gualano G , et al. Delay in diagnosis of pulmonary tuberculosis: a survey in the Lazio region, Italy. Epidemiology Biostatistics and Public Health. 2015;12(1):e94941.
5 Tattevin P , Che D , Fraisse P , Gatey C , Guichard C , Antoine D , et al. Factors associated with patient and health care system delay in the diagnosis of tuberculosis in France. Int J Tuberc Lung Dis. 2012;16(4):510–5. doi:.https://doi.org/10.5588/ijtld.11.0420
6 Díez M , Bleda MJ , Alcaide J , Caloto T , Castells C , Cardenal JI , et al.; Multicentre Project for Tuberculosis Research Study Group. Determinants of patient delay among tuberculosis cases in Spain. Eur J Public Health. 2004;14(2):151–5. doi:.https://doi.org/10.1093/eurpub/14.2.151
7 Sultan H , Haroon S , Syed N . Delay and completion of tuberculosis treatment: a cross-sectional study in the West Midlands, UK. J Public Health (Oxf). 2013;35(1):12–20. Published online June 21, 2012. doi:.https://doi.org/10.1093/pubmed/fds046
8 Saldana L , Abid M , McCarthy N , Hunter N , Inglis R , Anders K . Factors affecting delay in initiation of treatment of tuberculosis in the Thames Valley, UK. Public Health. 2013;127(2):171–7. Published online January 11, 2013. doi:.https://doi.org/10.1016/j.puhe.2012.11.010
9 Farah MG , Rygh JH , Steen TW , Selmer R , Heldal E , Bjune G . Patient and health care system delays in the start of tuberculosis treatment in Norway. BMC Infect Dis. 2006;6(1):33. Published online February 24, 2006. doi:.https://doi.org/10.1186/1471-2334-6-33
10 Kiefer S , Auer C , Altpeter E , Zellweger J-P , Blum J , Wyss K . Tuberkulose in der Schweiz: das Wichtigste in Kürze. Swiss Med Forum. 2016;6:613–6.
11Figure received from the Federal Office of Public Health in April 2017.
12 Ibrahim WH , Alousi FH , Al-Khal A , Bener A , AlSalman A , Aamer A , et al. Diagnostic Delay among Adults with Pulmonary Tuberculosis in a High Gross Domestic Product Per Capita Country: Reasons and Magnitude of the Problem. Int J Prev Med. 2016;7(1):116. Published online October 26, 2016. doi:.https://doi.org/10.4103/2008-7802.193091
13 Lewis KE , Stephens C , Shahidi MM , Packe G . Delay in starting treatment for tuberculosis in east London. Commun Dis Public Health. 2003;6(2):133–8.
14 Altet Gómez MN , Alcaide Megías J , Canela Soler J , Milá Augé C , Jiménez Fuentes MA , de Souza Galvao ML , et al. [Pulmonary symptomatic tuberculosis’ diagnostic delay study]. Arch Bronconeumol. 2003;39(4):146–52. Article in Spanish.
15 Storla DG , Yimer S , Bjune GA . A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8(1):15. doi:.https://doi.org/10.1186/1471-2458-8-15
16 Kherad O , Herrmann FR , Zellweger JP , Rochat T , Janssens JP . Clinical presentation, demographics and outcome of tuberculosis (TB) in a low incidence area: a 4-year study in Geneva, Switzerland. BMC Infect Dis. 2009;9(1):217. doi:.https://doi.org/10.1186/1471-2334-9-217
17 Cai J , Wang X , Ma A , Wang Q , Han X , Li Y . Factors associated with patient and provider delays for tuberculosis diagnosis and treatment in Asia: a systematic review and meta-analysis. PLoS One. 2015;10(3):e0120088. doi:.https://doi.org/10.1371/journal.pone.0120088
18 Bogale S , Diro E , Shiferaw AM , Yenit MK . Factors associated with the length of delay with tuberculosis diagnosis and treatment among adult tuberculosis patients attending at public health facilities in Gondar town, Northwest, Ethiopia. BMC Infect Dis. 2017;17(1):145. doi:.https://doi.org/10.1186/s12879-017-2240-0
19 Samal J . Health Seeking Behaviour among Tuberculosis Patients in India: A Systematic Review. J Clin Diagn Res. 2016;10(10):LE01–06. Published online October 1, 2016.
20 Chung KF , Pavord ID . Prevalence, pathogenesis, and causes of chronic cough. Lancet. 2008;371(9621):1364–74. doi:.https://doi.org/10.1016/S0140-6736(08)60595-4
21 Helbling P , Zellweger JP , Altpeter E , Boubaker K . [Epidemiogy and treatment of tuberculosis in Switzerland]. Rev Med Suisse. 2006;2(82):2276–8, 2280–1. Article in French.
22World Health Organization. Systematic screening for active tuberculosis: principles and recommendations. Geneva: World Health Organization; 2013. Report No.: WHO/HTM/TB/2013.04.
23 Altpeter E , Schoch O , Helbling P . Tuberkulose in der Schweiz: selten, und manchmal kompliziert. Swiss Med Forum. 2015;15(41):925–30.
24 Martinez L , Xu L , Chen C , Sekandi JN , Zhu Y , Zhang C , et al. Delays and Pathways to Final Tuberculosis Diagnosis in Patients from a Referral Hospital in Urban China. Am J Trop Med Hyg. 2017;96(5):1060–5. Published online February 13, 2017. doi:.https://doi.org/10.4269/ajtmh.16-0358
25 Gagliotti C , Resi D , Moro ML . Delay in the treatment of pulmonary TB in a changing demographic scenario. Int J Tuberc Lung Dis. 2006;10(3):305–9.
26 Dara M , Sulis G , Centis R , D’Ambrosio L , de Vries G , Douglas P , et al. Cross-border collaboration for improved tuberculosis prevention and care: policies, tools and experiences. Int J Tuberc Lung Dis. 2017;21(7):727–36. doi:.https://doi.org/10.5588/ijtld.16.0940
27 Dara M , de Colombani P , Petrova-Benedict R , Centis R , Zellweger JP , Sandgren A , et al.; Wolfheze Transborder Migration Task Force. Minimum package for cross-border TB control and care in the WHO European region: a Wolfheze consensus statement. Eur Respir J. 2012;40(5):1081–90. Published online May 31, 2012. doi:.https://doi.org/10.1183/09031936.00053012
28 Heuvelings CC , de Vries SG , Greve PF , Visser BJ , Bélard S , Janssen S , et al. Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. Lancet Infect Dis. 2017;17(5):e144–58. Published online March 11, 2017. doi:.https://doi.org/10.1016/S1473-3099(16)30532-1
This study was supported by a grant from the Federal Office of Public Health, given to the Swiss Tropical and Public Health Institute for conducting two TB studies in Switzerland: one on the knowledge of general practitioners on TB and the here described so-called TB delay study.
We report no conflict of interest or potential conflict of interest relevant to this article.