Coercion in substance use disorders: clinical course of compulsory admissions in a Swiss psychiatric hospital
DOI: https://doi.org/10.4414/smw.2018.14644
Benedikt
Habermeyera, Lea
Wydera, Patrik
Rosera, Marc
Vogelb
aDepartment of Addictive Disorders, Psychiatric Services Aargau (PDAG), Brugg, Switzerland
bUniversity of Basel Psychiatric Hospital, Division of Addictive Disorders, Basel, Switzerland
Summary
According to the Swiss legal system, involuntary admission is one of the farthest-reaching incursions into personal autonomy. The effect of compulsory admission in treatment of substance use disorders (SUDs) on variables such as length of stay or leaving treatment before recommended discharge remains elusive. In order to elucidate these effects, we retrospectively analysed the clinical course of treatment of 608 patients who were admitted between November 2016 and October 2017 to the Department of Addictive Disorders of the canton of Aargau.
Involuntarily admitted patients showed lower health and social functioning, as measured by the Health of the Nation Outcome Scales (HoNOS), compared with those with voluntary status. In involuntary admissions for SUD treatment, length of stay was significantly shorter and the proportion of patients who left treatment against recommendation was twice as high as in voluntarily admitted patients. Furthermore, if treatment was initiated on a compulsory basis, a subsequent switch to voluntary treatment status appeared to be very uncommon. We conclude that, at least in involuntary admission according to the Swiss legal system, these admissions do not lead to sustained inpatient treatment.
Introduction
In recent years, a discussion on coercion in general psychiatry has evolved [1]. Many authors have pointed out that the empirical basis for coercion is slight [2] and, consequently, various psychiatric wards in Germany [3] and Switzerland [4–6] have successfully transitioned from a locked- to an open-door policy. Coercion often starts with compulsory admission to inpatient treatment. A recently published Swiss study showed that one third of the involuntarily admitted patients were exposed to further coercive measures such as seclusion, restraint or coercive medication during inpatient treatment [7].
According to the Swiss legal system, involuntary admission to inpatient treatment is one of the farthest-reaching incursions into personal autonomy. The formal prerequisites changed in 2013, as a new federal legislation (Kindes- und Erwachsenenschutzrecht, KESR) was established. A person suffering from mental illness, including substance use disorder (SUD), mental retardation or severe neglect can be admitted against their will to a suitable institution, if necessary treatment or care cannot be provided otherwise [8]. However, an involuntary admission should be considered only when its main goal can be achieved with this measure and a suitable setting exists. This order, however, can and has to be suspended by the psychiatrist providing the coerced treatment if the underlying criteria are no longer fulfilled.
Local public authorities predominantly delegated the responsibility for compulsory admissions to medical doctors [9], and different local implementations have contributed to a high variability of involuntary admission rates in the different cantons: for example,. 37% in the canton of Aargau and 4% in the canton of Geneva [10]. In contrast to the canton of Geneva, in which only specialised doctors are authorised to order coerced inpatient treatment, every medical doctor can do so in the canton of Aargau.
Although some psychiatric addictions units in Switzerland, such as the University Hospital Basel [11] or the Geneva University Hospitals [12], aimed to reduce the use of coercion in the treatment of SUD, a recent study on compulsory admission in the canton of Zurich showed that SUD still was the second most prevalent diagnosis in involuntary admitted patients.
This finding might not be unexpected as, specifically in SUD, ambivalence toward initiation or maintenance of treatment is common. In fact, a large proportion of research in SUD addresses the goal of overcoming this ambivalence without the need for coercion, with treatment approaches such as motivational interviewing [13]. The association between SUDs and the use of coercive measures is also supported by a study from Finland, which showed that a SUD was a significant predictor for the use of restraint [14]. Proponents of coercion argue that the definition of addiction implies a loss of control over substance use, with the disorder “coercing” behaviour. Therefore, restricting autonomy of addicted patients at the outset of therapy may in fact be necessary in order to reinstate autonomous behaviour [15]. Advocates of coercion in SUD often cite clinical studies from forensic-psychiatric settings that suggest some merit of coercion in SUD [16, 17]. Research indicates that involuntary approaches promoting therapy instead of prison might show similar effects as voluntarily initiated treatment [18, 19]. However, there is also evidence that voluntary treatment yields better results than coerced therapy [20, 21] and it is a widely accepted fact that coercion has a negative effect on the therapeutic relationship [22], thus influencing outcomes.
Research on compulsory admission to psychiatric treatment itself is scarce, and there is even less information available for the treatment of SUD. The effect of compulsory admission in SUD treatment on variables such as length of stay (LOS) or leaving treatment against recommendation remains elusive. In SUD treatment, retention is often used as a primary outcome parameter and can be quantified by the LOS in inpatient treatment. Longer LOS in SUD is associated with lower substance use after discharge [23, 24] and lower readmission rates [25]. Furthermore, treatment outcomes are worse if treatment is terminated prematurely or against the recommendations of the therapists [26, 27]. One study from Israel suggests that a smaller proportion of involuntarily admitted patients were in remission at discharge compared with those who were discharged after voluntary admission [28]. However, the authors claimed that involuntary admission was associated with a longer time to the next hospitalisation.
To the best of our knowledge, the clinical course of involuntary admission for the treatment of SUD in Switzerland has not been addressed in research so far. Therefore, this study aims to compare the clinical course of involuntary and voluntary admissions for SUD inpatient treatment.
Methods
Setting and sample
The mental hospital of the Psychiatric Services Aargau (PDAG) provides inpatient treatment for the approximately 650,000 inhabitants of the canton of Aargau, Switzerland. The canton of Aargau consists of both urban and semi-rural parts. The hospital of the PDAG is the only facility providing acute psychiatric inpatient treatment in the canton (for more information on the catchment area, see [29]). We retrospectively analysed all admissions to the hospital's Department of Addictive Disorders between November 2016 and October 2017. The department consists of three separate wards, of which one provides 11 places for closed treatment. On this ward, another 11 patients can be treated in an open setting, and the other two open wards provide 40 additional treatment places.
The study was approved by the responsible regional ethics committee (BASEC 2017-01533) and received no financial support from any public or commercial funding agency.
Data collection
Information on patients’ age and sex, termination of treatment against recommendation, LOS, length of coercion, length of voluntary treatment after removal of coercion and all psychiatric diagnoses according to ICD-10 was drawn from the medical database of the PDAG. In order to assess clinical severity, we also incorporated the Health of the Nation Outcome Scale (HoNOS) [30], which is assessed routinely in all inpatients of the PDAG. The HoNOS is an established rating instrument for the assessment of symptom severity and social functioning in patients with mental disorders. It consists of 12 items measuring four broader categories: behaviour, impairment, symptoms and social functioning. Each item can be rated from 0 to 4, resulting in total values between 0 and 48. According to the thresholds suggested by Parabiaghi [31], total HoNOS scores over 13 are considered to indicate a severe stage of illness, whereas lower scores indicate a rather moderate stage of illness. In this context, recent research has confirmed that the HoNOS score is able to predict service utilisation in patients with substance-related disorders [32]. Cases without SUDs were excluded from the analysis.
Data analysis
Data regarding age, sex, LOS, HoNOS, ICD-10 diagnosis, substances used, and termination of treatment against recommendation were first analysed descriptively. Afterwards, data of both subgroups (i.e., patients admitted voluntarily and patients admitted involuntarily) were analysed separately. As data were not normally distributed and generally skewed by extremely large or small values, we used non-parametric methods for all statistical tests. Group comparisons were calculated using the Kruskal-Wallis test. All analyses were performed with IBM SPSS, version 23.
Results
From November 2016 to October 2017, 636 patients were admitted to the Department of Addictive Disorders. Of these, 28 were excluded from the analysis as they had no SUD and were admitted to the Department of Addictive disorders because of lacking capacity in the other departments of the PDAG. Of the remaining 608 patients, 79.4% (n = 483) were admitted on a voluntary basis and 20.6% (n = 125) involuntarily. If a patient were admitted more than once, we analysed only the first treatment case for each patient in order to avoid interdependencies. There was no significant difference regarding distribution of sex within the two subgroups (table 1).
Table 1 Distribution of sex, diagnoses leading to admission, predominantly used substances and proportion of patients that terminated the treatment against the recommendation for all patients with SUD and for the respective subgroups.
|
|
All
|
Voluntary admission
|
Involuntary admission
|
χ2
|
df
|
sig.
|
|
|
n
|
%
|
n
|
%
|
n
|
%
|
|
Total
|
|
608 |
100.0 |
483 |
100.0 |
125 |
100.0 |
|
|
|
|
Sex
|
Female |
195 |
32.1 |
153 |
31.7 |
42 |
33.6 |
0.169 |
1 |
n.s. |
| Male |
413 |
67.9 |
330 |
68.3 |
83 |
66.4 |
|
|
|
|
Substance use disorders
|
Intoxication |
60 |
9.9 |
3 |
0.6 |
57 |
45.6 |
290.9 |
8 |
p <0.001 |
| Harmful use |
6 |
1.0 |
5 |
1.0 |
1 |
0.8 |
|
|
|
| Dependence syndrome |
302 |
49.7 |
284 |
58.8 |
18 |
14.4 |
|
|
|
| Withdrawal state |
4 |
0.7 |
0 |
0.0 |
4 |
3.2 |
|
|
|
| Psychotic disorder |
14 |
2.3 |
5 |
1.0 |
9 |
7.2 |
|
|
|
|
Dual diagnosis
|
Psychotic disorder + SUD |
30 |
4.9 |
24 |
5.0 |
6 |
4.8 |
|
|
|
| Affective disorder + SUD |
119 |
19.6 |
110 |
22.8 |
9 |
7.2 |
|
|
|
| Neurotic disorder + SUD |
22 |
3.6 |
17 |
3.5 |
5 |
4.0 |
|
|
|
| Personality disorder + SUD |
51 |
8.4 |
35 |
7.2 |
16 |
12.8 |
|
|
|
|
Substance
|
Alcohol |
390 |
64.1 |
304 |
62.9 |
86 |
68.8 |
10.99 |
7 |
n.s. |
| Opioids |
59 |
9.7 |
53 |
11.0 |
6 |
4.8 |
|
|
|
| Cannabinoids |
44 |
7.2 |
35 |
7.2 |
9 |
7.2 |
|
|
|
| Sedatives/hypnotics |
20 |
3.3 |
14 |
2.9 |
6 |
4.8 |
|
|
|
| Cocaine |
44 |
7.2 |
39 |
8.1 |
5 |
4.0 |
|
|
|
| Stimulants |
9 |
1.5 |
8 |
1.7 |
1 |
0.8 |
|
|
|
| Hallucinogens |
2 |
0.3 |
2 |
0.4 |
0 |
0.0 |
|
|
|
| Multiple drugs |
40 |
6.6 |
28 |
5.8 |
12 |
9.6 |
|
|
|
|
Termination of treatment against recommendation
|
|
155 |
25.5 |
103 |
21.3 |
52 |
41.6 |
20.6 |
1 |
p <0.001 |
|
Discharged from facultatively closed ward
|
|
242 |
39.8 |
134 |
27.7 |
108 |
86.4 |
142.6 |
1 |
p <0.001 |
Of all patients, 9.9% (n = 60) were admitted as a result of intoxication. Admissions for intoxication could further be separated according to the combination of with or without substance dependence, and with or without harmful substance use. More than 80% of the intoxicated patients (n = 49) suffered from additional harmful use (n = 12) or dependence (n = 37), only in 18.3% of the patients with intoxication, no harmful use or dependence was diagnosed. One percent of the patients (n = 6) showed a harmful use of substances, 49.7% were admitted for the treatment of substance dependence (n = 302). A clinical state of withdrawal leading to admission was found in 0.7% (n = 4), and 2.3% suffered from drug-induced psychotic disorders (n = 14).
Dual diagnosis was found in 36.5% of patients. The combination of psychotic disorders and SUD was present in 4.9% (n = 30), a combination of affective disorders and SUD in 19.6% (n = 119), a combination of neurotic disorders and SUD in 3.6% (n = 22), and 8.4% suffered from both personality disorders and SUD (n = 51).
In voluntarily admitted patients, referral for the treatment of substance dependence was the most frequent reason for admission (58.8%, n = 284), followed by affective disorders in combination with SUD (22.8%, n = 110) or personality disorders in combination with SUD (7.2%, n = 35). In involuntarily admitted patients, intoxication was responsible for 45.6% (n = 57) of the admissions, and 14.4% were admitted for the treatment of substance dependence (n = 18) or of personality disorders in combination with SUD (12.8%, n = 16).
We found alcohol to be the predominant substance used by the patients (64.1%, n = 390), followed by opioids (9.7%, n = 59), cocaine (7.2%, n = 44), cannabinoids (7.2%, n = 44) and multiple drug use (6.6%, n = 40). The distribution of the substances used did not differ significantly between the subgroups.
Termination of treatment against recommendation was encountered in 25.5% (n = 155) of all patients. In voluntarily admitted patients, 21.3% (n = 103) terminated treatment against advice. In involuntarily admitted patients, this proportion was 41.6% (n = 52). The distribution of termination of treatment against recommendation in both subgroups differed significantly (χ2 = 20.6, degrees of freedom [df] = 1, p <0.001).
A proportion of 39.8% (n = 242) patients were discharged from the facultatively closed ward. Among these patients, 27.7% (n = 134) were admitted voluntarily and 86.4% (n = 108) involuntarily. The distribution differed significantly (χ2 = 142.6, df = 1, p <0.001) between groups.
The mean total HoNOS score in the involuntarily admitted patients was 19.5 (± 48.5), the median was 14.2. The total HoNOS score was significantly higher in involuntarily admitted patients (χ2 = 9.4, df = 1, p <0.05). Among the subscales, we found a significant difference between the subgroups only for behaviour (χ2 = 32.8, df = 1, p <0.001), but not for impairment, symptoms or functioning (table 2).
Table 2 Age, Health of the Nation Outcome Scales (HoNOS) score, length of stay, length of coercion and length of stay after release of coercion for voluntarily and involuntarily admitted patients (range is displayed with minimum and maximum values of the respective variable.
|
|
Voluntary admission
|
Involuntary admission
|
χ2
|
df
|
sig.
|
|
|
Mean
|
Range
|
SD
|
Median
|
Mean
|
Range
|
SD
|
Median
|
|
Age
|
|
40.0 |
17/67 |
12.0 |
40.0 |
39.0 |
18/65 |
12.8 |
41.0 |
1.6 |
1 |
n.s. |
|
HoNOS Score
|
Total |
13.2 |
2/31 |
4.9 |
13.0 |
15.0 |
2/33 |
6.6 |
14.0 |
9.4 |
1 |
p <0.05 |
| Behaviour |
4.0 |
0/12 |
1.5 |
4.0 |
5.2 |
0/11 |
2.2 |
5.0 |
32.8 |
1 |
p <0.001 |
| Impairment |
1.3 |
0/6 |
1.5 |
1.0 |
1.3 |
0/8 |
1.7 |
1.0 |
0 |
1 |
n.s. |
| Symptoms |
3.8 |
0/11 |
2.0 |
4.0 |
4.1 |
0/10 |
2.2 |
4.0 |
2.1 |
1 |
n.s. |
| Functioning |
4.1 |
0/15 |
3.2 |
4.0 |
4.6 |
0/14 |
3.8 |
4.0 |
0.8 |
1 |
n.s. |
|
Length of stay
|
|
23.2 |
1/108 |
17.5 |
20.0 |
18.8 |
0/145 |
26.1 |
7.0 |
28.3 |
1 |
p <0.001 |
|
Length of coercion
|
|
|
|
|
|
11.2 |
0/145 |
21.5 |
3.0 |
|
|
|
|
LOS after release of coercion
|
|
|
|
|
|
6.5 |
0/90 |
12.7 |
0.0 |
|
|
|
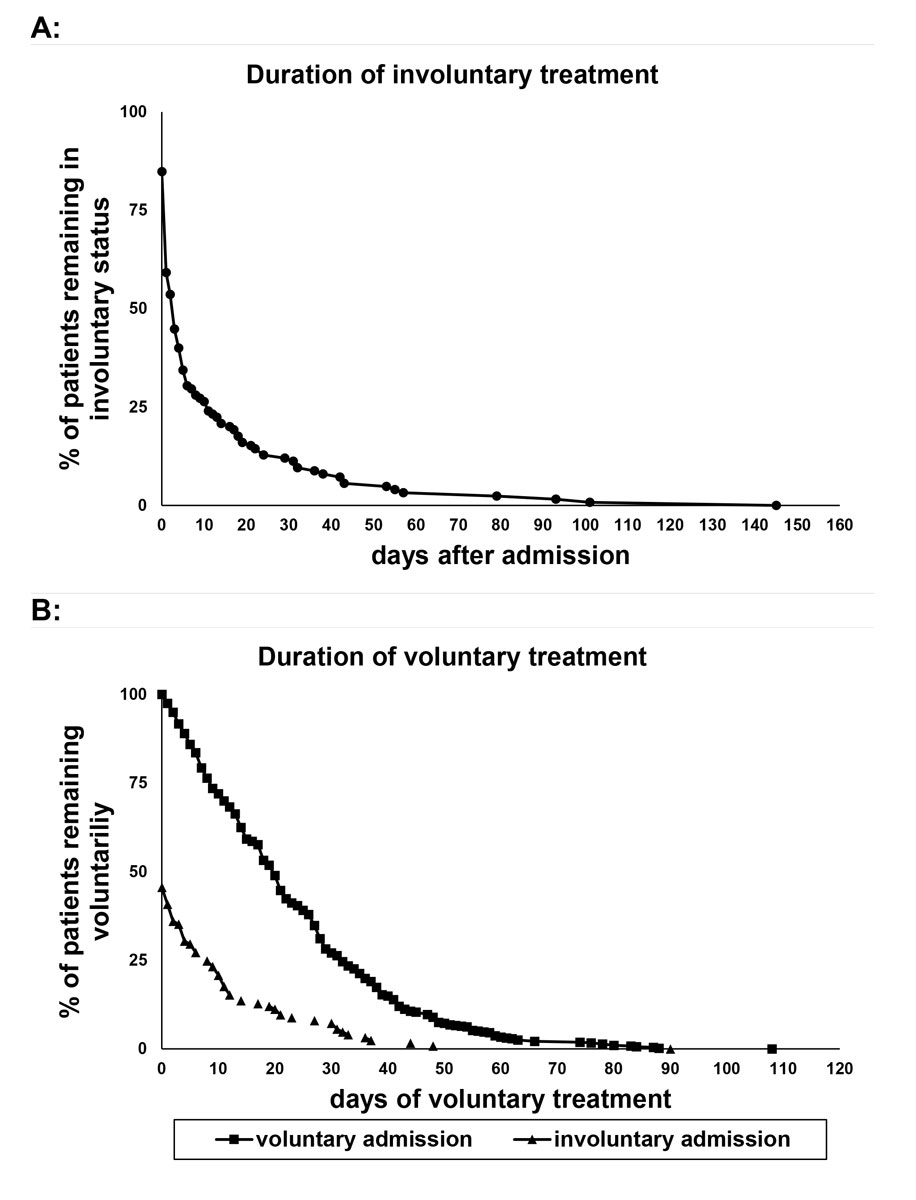
Mean LOS for all involuntarily admitted patients was 18.8 (± 26.1) days, the median was 7.0 days. Mean LOS in voluntary admissions was 23.2 (± 17.5) days, the median 20.0 days. LOS differed significantly between both groups (χ2 = 28.3, df = 1, p <0.001). In the group of involuntarily admitted patients, the mean duration of involuntary status was 11.2 (± 21.5) days, the respective median was 3.0 days. After repeal of involuntary status, the mean duration of voluntary treatment was 6.5 (± 12.7) days, the median 0.0 days, indicating that many patients left treatment on the day of admission (table 2). As illustrated in figure 1, more than 75% of the involuntarily admitted patients remained in treatment for less than 10 days, but there was also one patient who stayed for 145 days. In the voluntarily admitted patients, the proportion remaining in treatment declined much more evenly and the longest LOS was 108 days.
Discussion
The demographic findings in our study are in line with the literature on SUD. Overall, male sex is more frequent in SUD. In contrast to a study from Norway, which showed a higher proportion of female patients in the involuntarily admitted patients [33], we did not find a sex difference between voluntary and involuntary admissions. Whereas in the Norwegian study this difference was explained by the notion that female patients might be considered more vulnerable by the evaluating doctors, this factor obviously did not influence our sample. Moreover, we did not find a significant difference in mean age between both subgroups. Thus, our findings suggest that coercion is not related to age.
For compulsory admissions, intoxication was the most common reason for admission, but this was less often the reason for admission in the voluntary group. These results suggest that, in Switzerland, compulsory admissions of SUD patients often happen in the context of intoxication, where patients may be more likely to come into contact with admitting health authorities, owing to aggression, violence, or medical complications such as respiratory depression, for example. However, it has to be kept in mind that more than 80% of all intoxicated patients also fulfilled the clinical criteria for harmful substance use or dependence, thus warranting SUD treatment in addition to management of the intoxication.
In voluntarily admitted patients, admissions in order to treat dependence syndromes were more common than in the involuntary subgroup. However, given the high rate of concomitant dependence or at least harmful substance use diagnoses in intoxicated patients, there appears to be a substantial overlap between these diagnostic categories. Substance-induced psychotic disorders and withdrawal states were rather more likely to be found in the involuntary subgroup than in the voluntary subgroup. Harmful substance use was scarce in both groups.
Admission due to dual diagnoses contributed to one in three admissions. This proportion appeared to be slightly higher in the voluntary group, in which the most prominent dual diagnosis was the combination of affective disorders with SUD. In the involuntary group, however, the combination of personality disorders with SUD prevailed. This combination is known to be associated with more legal and social problems, greater mood disturbances and impulsivity [34]. In a study on aggressive behaviour preceding admission, patients suffering from personality disorders showed aggressive behaviour more often than, for example, patients with psychotic disorders [35]. The rates for psychotic disorders (4.9%) or neurotic disorders (3.6%) in combination with SUD did not differ across both admission subgroups.
The total HoNOS score was significantly higher in involuntarily admitted patients. This finding derives most likely from the subscale for behaviour. This can probably be explained by the significantly different distribution of diagnoses in both subgroups. As already mentioned, we found a rather high rate of intoxicated patients in the involuntary group. Behavioural disturbances are classified under criteria B of the ICD-10 criteria for intoxication [36]. Patients with intoxication thus automatically score also in the respective HoNOS scale. Other items that define the behavioural score in the HoNOS include suicidality or self-harm. These are also frequent criteria for coercion in the Swiss legal system. Against that background, the significant difference between the groups was not surprising. However, bearing in mind that involuntary admission should be restricted to patients for whom no other alternative to provide care exists, one might expect differences in the scales for impairment, psychopathology or social functioning, corresponding to higher clinical severity in the involuntary group. Our findings indicate, however, that both groups have many more clinical and social similarities than differences, and that mostly behavioural deviations determine the mode of admission.
Although clinical characteristics did not differ as expected, we found clear differences regarding the course of treatment. Compulsorily admitted patients spent significantly less time in hospital treatment than patients who were admitted voluntarily. Furthermore, our data show that the involuntary status is often removed by treating physicians within the first days of treatment. The mean length of involuntary status was 3 days. Figure 1 shows that, in more than 50% of the patients, the coercion was already removed by the treating physician on the first day of treatment. Thus, after very short duration of hospitalisation, most patients no longer fulfilled the criteria for compulsory treatment. The most likely explanation might be seen in the relatively large proportion of intoxicated patients in the involuntary group. With the acute effects of intoxication subsiding, the behavioural disturbances equally resolve. In light of the obviously problematic pattern of substance use leading to admission and the high rates of substance dependence in these patients, longer treatment episodes are often indicated from a medical perspective, in order to achieve sustainable treatment results. The fact that only a few patients remained in treatment once coercion had been removed suggests that involuntary admission may not facilitate voluntary treatment continuation. The median length of voluntary continuation of treatment after discontinuation of commitment was 0 days and was therefore disappointingly low.
Furthermore, the rate of patients who terminated treatment against recommendation of the treating physicians was twice as high in involuntarily admitted patients and differed significantly from voluntarily admitted patients. Therefore, we conclude that involuntary admission only rarely contributes to a sustained treatment of SUDs. These findings indicate that coercion may not be the best option to facilitate adequate treatment of SUDs. However, we did not investigate the number of these patients initiating or continuing outpatient treatment of their SUD.
There are some other limitations to our study that have to be considered. We could show that LOS differed between groups; however this finding has to be interpreted cautiously. Factors such as the high proportion of intoxication or the higher total HoNOS score in the involuntary group might contribute to this difference. Although involuntarily admitted patients in our study may also have been treated on open wards and voluntarily admitted patients in a closed setting, the setting might also contribute to our findings, because most involuntary admitted patients were staying on a facultatively closed ward. According to Hotzy et al. [37], even the experience of a physician ordering involuntary admission might influence the LOS. It is therefore conceivable that many other factors contribute to our findings, which render causal interpretation of our data difficult.
Since our study was retrospective, we had to rely on the clinical diagnosis and information instead of using structured or semi-structured interviews or more systematic assessments. Larger and prospective studies on the subject are therefore encouraged and might contribute to a better understanding of the clinical course of involuntary admissions in SUD.
In SUD, the individual treatment goals are manifold and extend from harm reduction to abstinence. Whereas there is no doubt that psychiatric interventions can help to achieve these goals, it is clear that not only medical treatment leads to remission of the disease. A prerequisite of compulsory admission in Switzerland is that commitment must be the only option left to avoid harm to the patient and/or others, and the coerced treatment must be suitable to overcome this harm. Involuntary admission for the management of intoxication may help to avoid harm from intoxication, but our findings suggest that it may not contribute to a sustained inpatient treatment of the underlying dependence. There are many ways to remission from substance use disorder, and several studies on the clinical course of addiction show that patients may recover even without any intervention [38–40]. With this in mind, the notion that there may be no other options than involuntary admission appears to be questionable.
Conclusion
Involuntarily admitted patients show poorer health and social functioning as measured by HoNOS compared with those with voluntary status. This difference is probably driven by behavioural abnormalities, which may be related to intoxication. In involuntary admissions for treatment of SUD, LOS is significantly shorter and the proportion of patients who leave treatment against recommendation is twice as high as in voluntarily admitted patients. We conclude that, at least in involuntary admission according to the Swiss legal system, these admissions do not lead to sustained inpatient treatment. Furthermore, if treatment is initiated on a compulsory basis, a subsequent switch to voluntary treatment status appears to be uncommon. As short LOS and termination of treatment against recommendation have been related to an impaired outcome [23, 24, 26, 27], we suggest refraining from involuntary admission whenever possible and rather promote motivational approaches in order to facilitate adequate treatment for SUD.
References
1
Steinert
T
,
Fallgatter
A
. Psychiatrie mit offenen Türen. Psychiatr Prax. 2016;43(8):452–4. doi:.https://doi.org/10.1055/s-0042-119111
2
Muralidharan
S
,
Fenton
M
. Containment strategies for people with serious mental illness. Cochrane Database Syst Rev. 2006;(3):CD002084.
3
Lang
UE
,
Hartmann
S
,
Schulz-Hartmann
S
,
Gudlowski
Y
,
Ricken
R
,
Munk
I
, et al.
Do locked doors in psychiatric hospitals prevent patients from absconding?
Eur J Psychiatry. 2010;24(4):199–204. doi:.https://doi.org/10.4321/S0213-61632010000400001
4
Sollberger
D
,
Lang
UE
. Psychiatrie mit offenen Türen. Teil 1: Rational für Türöffnungen in der Akutpsychiatrie [Psychiatry with open doors. Part 1: Rational for an open door for acute psychiatry]. Nervenarzt. 2014;85(3):312–8. Article in German. doi:.https://doi.org/10.1007/s00115-013-3769-9
5
Jungfer
H-A
,
Schneeberger
AR
,
Borgwardt
S
,
Walter
M
,
Vogel
M
,
Gairing
SK
, et al.
Reduction of seclusion on a hospital-wide level: successful implementation of a less restrictive policy. J Psychiatr Res. 2014;54:94–9. doi:.https://doi.org/10.1016/j.jpsychires.2014.03.020
6
Lang
UE
,
Walter
M
,
Borgwardt
S
,
Heinz
A
. Über die Reduktion von Zwangsmaßnahmen durch eine “offene Türpolitik” [About the Reduction of Compulsory Measures by an “Open Door Policy”]. Psychiatr Prax. 2016;43(6):299–301. Article in German. doi:.https://doi.org/10.1055/s-0042-111032
7
Hotzy
F
,
Moetteli
S
,
Theodoridou
A
,
Schneeberger
AR
,
Seifritz
E
,
Hoff
P
, et al.
Clinical course and prevalence of coercive measures: an observational study among involuntarily hospitalised psychiatric patients. Swiss Med Wkly. 2018;148:w14616. doi:.https://doi.org/10.4414/smw.2018.14616
8Art ZGB. 426 Das Familienrecht Der Erwachsenenschutz Die behördlichen Massnahmen Die fürsorgerische Unterbringung [Internet]. [cited 2018 Jan 16]. Available from: https://zgb.gesetzestext.ch/artikel.cfm?key=493&art=Der_Erwachsenenschutz
9Schweizerisches Zivilgestzbuch vom 10. Dezember 1907. [Internet]. Available from: https://www.admin.ch/opc/de/classified-compilation/19070042/201604010000/210.pdf
10Vögeli D. Hohe Einweisungsraten im Kanton Zürich | NZZ. Neue Zürcher Zeitung [Internet]. 2013 Jan 28 [cited 2018 May 26]; Available from: https://www.nzz.ch/zuerich/ein-viertel-aller-psychiatrischen-hospitalisierungen-unfreiwillig-1.17965215
11
Steinauer
R
,
Huber
CG
,
Petitjean
S
,
Wiesbeck
GA
,
Dürsteler
KM
,
Lang
UE
, et al.
Effect of Door-Locking Policy on Inpatient Treatment of Substance Use and Dual Disorders. Eur Addict Res. 2017;23(2):87–96. doi:.https://doi.org/10.1159/000458757
12Le Service d’addictologie est ‘No restraint’ [Internet]. ADDICTOHUG. [cited 2018 May 26]. Available from: https://addictohug.ch/addictologie/no-restraint/
13Bennett G, Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press, 1991. pp. xvii
14
Korkeila
JA
,
Tuohimäki
C
,
Kaltiala-Heino
R
,
Lehtinen
V
,
Joukamaa
M
. Predicting use of coercive measures in Finland. Nord J Psychiatry. 2002;56(5):339–45. doi:.https://doi.org/10.1080/080394802760322105
15
Caplan
A
. Denying autonomy in order to create it: the paradox of forcing treatment upon addicts. Addiction. 2008;103(12):1919–21. doi:.https://doi.org/10.1111/j.1360-0443.2008.02369.x
16
O’Brien
C
,
Cornish
JW
. Naltrexone for probationers and parolees. J Subst Abuse Treat. 2006;31(2):107–11. doi:.https://doi.org/10.1016/j.jsat.2006.06.002
17
Farabee
D
,
Prendergast
M
,
Anglin
MD
. The effectiveness of coerced treatment for drug-abusing offenders. Fed Probat. 1998;62:3.
18
Schaub
M
,
Stevens
A
,
Berto
D
,
Hunt
N
,
Kerschl
V
,
McSweeney
T
, et al.
Comparing outcomes of ‘voluntary’ and ‘quasi-compulsory’ treatment of substance dependence in Europe. Eur Addict Res. 2010;16(1):53–60. doi:.https://doi.org/10.1159/000265938
19
Stevens
A
,
Berto
D
,
Heckmann
W
,
Kerschl
V
,
Oeuvray
K
,
van Ooyen
M
, et al.
Quasi-compulsory treatment of drug dependent offenders: an international literature review. Subst Use Misuse. 2005;40(3):269–83. doi:.https://doi.org/10.1081/JA-200049159
20
Parhar
KK
,
Wormith
JS
,
Derkzen
DM
,
Beauregard
AM
. Offender Coercion in Treatment: A Meta-Analysis of Effectiveness. Crim Justice Behav. 2008;35(9):1109–35
. [doi:.].https://doi.org/10.1177/0093854808320169
21
Werb
D
,
Kamarulzaman
A
,
Meacham
MC
,
Rafful
C
,
Fischer
B
,
Strathdee
SA
, et al.
The effectiveness of compulsory drug treatment: A systematic review. Int J Drug Policy. 2016;28:1–9. doi:.https://doi.org/10.1016/j.drugpo.2015.12.005
22
Theodoridou
A
,
Schlatter
F
,
Ajdacic
V
,
Rössler
W
,
Jäger
M
. Therapeutic relationship in the context of perceived coercion in a psychiatric population. Psychiatry Res. 2012;200(2-3):939–44. doi:.https://doi.org/10.1016/j.psychres.2012.04.012
23
Greenfield
L
,
Burgdorf
K
,
Chen
X
,
Porowski
A
,
Roberts
T
,
Herrell
J
. Effectiveness of long-term residential substance abuse treatment for women: findings from three national studies. Am J Drug Alcohol Abuse. 2004;30(3):537–50. doi:.https://doi.org/10.1081/ADA-200032290
24
Simpson
DD
,
Joe
GW
,
Rowan-Szal
GA
. Drug abuse treatment retention and process effects on follow-up outcomes. Drug Alcohol Depend. 1997;47(3):227–35. doi:.https://doi.org/10.1016/S0376-8716(97)00099-9
25
Moos
RH
,
Moos
BS
. Stay in residential facilities and mental health care as predictors of readmission for patients with substance use disorders. Psychiatr Serv. 1995;46(1):66–72. doi:.https://doi.org/10.1176/ps.46.1.66
26
Ball
SA
,
Carroll
KM
,
Canning-Ball
M
,
Rounsaville
BJ
. Reasons for dropout from drug abuse treatment: symptoms, personality, and motivation. Addict Behav. 2006;31(2):320–30. doi:.https://doi.org/10.1016/j.addbeh.2005.05.013
27
Deane
FP
,
Wootton
DJ
,
Hsu
C-I
,
Kelly
PJ
. Predicting dropout in the first 3 months of 12-step residential drug and alcohol treatment in an Australian sample. J Stud Alcohol Drugs. 2012;73(2):216–25. doi:.https://doi.org/10.15288/jsad.2012.73.216
28
Delayahu
Y
,
Nehama
Y
,
Sagi
A
,
Baruch
Y
,
M Blass
D
. Evaluating the clinical impact of involuntary admission to a specialized dual diagnosis ward. Isr J Psychiatry Relat Sci. 2014;51(4):290–5.
29
Stulz
N
,
Nevely
A
,
Hilpert
M
,
Bielinski
D
,
Spisla
C
,
Maeck
L
, et al.
Referral to Inpatient Treatment Does not Necessarily Imply a Need for Inpatient Treatment. Adm Policy Ment Health. 2015;42(4):474–83. doi:.https://doi.org/10.1007/s10488-014-0561-5
30
Andreas
S
,
Harfst
T
,
Rabung
S
,
Mestel
R
,
Schauenburg
H
,
Hausberg
M
, et al.
The validity of the German version of the Health of the Nation Outcome Scales (HoNOS-D): a clinician-rating for the differential assessment of the severity of mental disorders. Int J Methods Psychiatr Res. 2010;19(1):50–62. doi:.https://doi.org/10.1002/mpr.305
31
Parabiaghi
A
,
Barbato
A
,
D’Avanzo
B
,
Erlicher
A
,
Lora
A
. Assessing reliable and clinically significant change on Health of the Nation Outcome Scales: method for displaying longitudinal data. Aust N Z J Psychiatry. 2005;39(8):719–24. doi:.https://doi.org/10.1080/j.1440-1614.2005.01656.x
32
Andreas
S
,
Harries-Hedder
K
,
Schwenk
W
,
Hausberg
M
,
Koch
U
,
Schulz
H
. Is the Health of the Nation Outcome Scales appropriate for the assessment of symptom severity in patients with substance-related disorders?
J Subst Abuse Treat. 2010;39(1):32–40. doi:.https://doi.org/10.1016/j.jsat.2010.03.011
33
Opsal
A
,
Kristensen
Ø
,
Larsen
TK
,
Syversen
G
,
Rudshaug
EB
,
Gerdner
A
, et al.
Factors associated with involuntary admissions among patients with substance use disorders and comorbidity: a cross-sectional study. BMC Health Serv Res. 2013;13(1):57. doi:.https://doi.org/10.1186/1472-6963-13-57
34
Heath
LM
,
Laporte
L
,
Paris
J
,
Hamdullahpur
K
,
Gill
KJ
. Substance Misuse Is Associated With Increased Psychiatric Severity Among Treatment-Seeking Individuals With Borderline Personality Disorder. J Pers Disord. 2017;•••:1–15. doi:.https://doi.org/10.1521/pedi_2017_31_307
35
Colasanti
A
,
Natoli
A
,
Moliterno
D
,
Rossattini
M
,
De Gaspari
IF
,
Mauri
MC
. Psychiatric diagnosis and aggression before acute hospitalisation. Eur Psychiatry. 2008;23(6):441–8. doi:.https://doi.org/10.1016/j.eurpsy.2007.09.005
36World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993.
37
Hotzy
F
,
Kieber-Ospelt
I
,
Schneeberger
AR
,
Jaeger
M
,
Olbrich
S
. Length of Involuntary Hospitalization Related to the Referring Physician’s Psychiatric Emergency Experience. Adm Policy Ment Health. 2018;45(2):254–64. doi:.https://doi.org/10.1007/s10488-017-0819-9
38
Dawson
DA
,
Grant
BF
,
Stinson
FS
,
Chou
PS
,
Huang
B
,
Ruan
WJ
. Recovery from DSM-IV alcohol dependence: United States, 2001-2002. Addiction. 2005;100(3):281–92. doi:.https://doi.org/10.1111/j.1360-0443.2004.00964.x
39
Sobell
LC
,
Cunningham
JA
,
Sobell
MB
. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86(7):966–72. doi:.https://doi.org/10.2105/AJPH.86.7.966
40
Wang
Y
,
Henriksen
CA
,
Ten Have
M
,
de Graaf
R
,
Stein
MB
,
Enns
MW
, et al.
Common Mental Disorder Diagnosis and Need for Treatment are Not the Same: Findings from the NEMESIS Study. Adm Policy Ment Health. 2017;44(4):572–81. doi:.https://doi.org/10.1007/s10488-016-0745-2