Figure 1 Completion of advance directives (ADs) by sociodemographic characteristics, adults aged 55+ in Switzerland, weighted percentage and 95% confidence intervals, SHARE 2015.
DOI: https://doi.org/10.4414/smw.2018.14642
In ageing societies, death happens at old age and is most likely to be the consequence of cumulated diseases and functional incapacities during the last years of life. In Switzerland, 62% of people who died in 2016 were aged 80 and over [1]. In addition, a Swiss study showed that 71% of all deaths that occurred in 2013 in Switzerland were not sudden and were expected [2]. Furthermore, the end of life tends to be highly medicalised and death mainly occurs in medicalised settings. Reich et al. showed that, among Swiss people who died between 2007 and 2011 at an average age of 79.3 years, 38% died in a hospital and 35% in a nursing home [3]. Moreover, 61% of these people had a hospital stay and 55% visited a general practitioner at least once during their last 6 months of life. Finally, the end of life and death often involve making specific treatment decisions, such as forgoing life-prolonging treatment or intensifying the alleviation of symptoms [2]. However, cognitive incapacities before death affect at least a quarter of patients [4] and can last several days [5], often leaving patients incapable of making their own end-of-life decisions during this critical life stage.
Advance directives are documents that record patients’ treatment decisions and preferences in the possible event of incapacity. The original objective of advance directives is to ensure a patient’s autonomy and self-determination. In reality, the perceived and expected benefits of advance directives among people who complete one are often even greater. They are generally understood as a means to prepare for the end of life and of death, to avoid over-treatment and being an unnecessary burden on the family, as well as to diminish the fear of not having one’s end-of-life wishes respected [6–8]. Thus, the completion of advance directives often contributes to maintaining a good quality of life at the end of life [9, 10].
In 2013, Switzerland introduced a new law on child and adult protection [11]. This law renders binding, through legal instruments, what people decide for themselves in advance in case they become incapable of making decisions; advance directives are one of these instruments. In Switzerland, advance directives consist of a written document that is to be used when its author is unable to make decisions and that (1) describes individual’s refusal or consent for potential future medical treatments and/or (2) designates a person to make medical decisions on the patient’s behalf (healthcare proxy). In other countries, the two documents are separated: advance decisions about medical treatments are written down in so-called “living wills”, whereas a healthcare proxy is designated through a “medical power of attorney”.
Structured templates aiming to help people complete an advance directive are provided by several institutions [12–14]. They list key end-of-life issues that can be addressed by an advance directive, such as resuscitation, pain alleviation, artificial nutrition and hydration, and organ donation. Some templates also ask about selected personal values regarding end-of-life decisions such as individuals’ motivation for completing an advance directive, previous or current disease experiences, fears regarding the end of life and death, attitudes toward potential dependency and functional limitations, and aspects of individuals’ spirituality and religiosity.
A large number of studies have investigated behaviours regarding advance directives in various countries that have legislation concerning them, making them binding for physicians. However, in Switzerland, knowledge about the prevalence of people who have heard of advance directives, who are interested in completing one and who have already completed one is scarce. Our study aimed to assess attitudes towards advance directives among adults aged 55 years and over in Switzerland. We examined the levels and the associations of awareness, approval and completion of advance directives both by and with sociodemographic characteristics, and explored the potential for improvement in the advance directive completion rate in view of individuals’ preferences regarding this.
We developed a questionnaire about end-of-life issues [15], which was administered as part of the 2015 data collection round (wave 6) of the Swiss component study of the Survey of Health, Ageing and Retirement in Europe (SHARE) [16]. SHARE is a longitudinal, interdisciplinary and cross-national data infrastructure that comprises individual-level information on the health, socioeconomic status, social and family networks and other life circumstances of older persons from 18 European countries and Israel. The Swiss SHARE sample is designed to be nationally representative of community-dwelling individuals aged 50 years and older and their partners, and is periodically refreshed to maintain its target population. Details of the way SHARE samples were drawn can be found in Börsch-Supan et al. [17] and Malter et al. [18]. Since the last refreshment sample for SHARE Switzerland was drawn in 2011, the 2015 follow-up study included only adults aged 55 and older. Our end-of-life survey was administered as a 15-page paper-and-pencil self-completion questionnaire at the end of the regular SHARE face-to-face interview.
Our study obtained ethical approval number 66/14 from the ethics committee of the canton of Vaud in March 2014. A total of 2806 respondents participated in the 2015 interview round in Switzerland and 94% of those also completed our end-of-life questionnaire, resulting in a sample of 2630 respondents. Retention of only observations with no missing data on all variables selected for the analysis results in a final analytical study sample of 2085 respondents.
Respondents were first given a description of the concept of advance directives. They were told that these are a binding document describing personal preferences for medical treatments that allows for appointing a healthcare proxy, and is used when a person has become incapable of making decisions. The survey then asked respondents about prior awareness of advance directives. Respondents were considered to have completed an advance directive if they reported either having a written document about their preferences for medical treatments (living will), already having a designated a healthcare proxy, or both. We classified respondents as approving of advance directives if they reported either have one already or planned to complete one sometime in the future. Respondents who had not yet completed an advance directive were asked to select one or more of seven prespecified potential reasons for why they had not (yet) done so.
We further extracted various sociodemographic characteristics of our respondents from the main SHARE data base, namely: sex; age (reported in three groups – 55–64, 65–74 and 75+ years); education level (recorded according to the ISCED1997 classification and grouped in three categories – elementary and lower secondary education, upper- and post-secondary education, tertiary education); whether they were living with a partner in the same household; whether they had living children; the type of their place of residence (urban vs rural area); and the linguistic region as defined by the language used during the interview (German, French or Italian).
In order to make the analysis sample representative of the target population, rates and 95% confidence intervals (CIs) presented in descriptive statistics (table 1 and figures 1, 2, and 3 ) were weighted using calibrated cross-sectional individual weights provided by SHARE [19, 20]. We employed logistic regression to assess the multivariable partial associations between advance directive awareness, approval and completion on the one hand and the sociodemographic characteristics of respondents on the other. To facilitate the interpretation of the estimates from our non-linear logit models as partial associations of the binary outcomes of interest and our categorical explanatory variables, we expressed our estimate results in terms of average marginal effects (AMEs). These AMEs report how the average probability P(Y = 1) changes when a given explanatory variable changes from 0 to 1, holding all other variables at their observed values [21]. Estimated standard errors account for clustering at the household level to correct for potential unobserved dependencies between two observations coming from the same household. All statistical analyses were conducted using Stata SE v. 14.0 (StataCorp, College Station).
Table 1 displays selected sociodemographic characteristics of our analytical sample. Nearly three quarters (73.6%) of our respondents lived in German-speaking Switzerland, which represents the linguistic majority in Switzerland; 52.6% of respondents were from rural areas.
Table 1 Sociodemographic characteristics of the analytical sample, adults aged 55+ in Switzerland (n = 2085), SHARE 2015.
|
Unweighted
n |
Weighted
% |
95% CI | |
|---|---|---|---|
| Gender | |||
| Men | 971 | 49.0 | 46.9–51.1 |
| Women | 1114 | 51.0 | 48.9–53.1 |
| Age groups | |||
| 55–64 years | 776 | 48.6 | 45.9–51.2 |
| 65–74 years | 756 | 28.5 | 26.4–30.7 |
| 75+ years | 553 | 23.0 | 21.0–25.0 |
| Education level | |||
| Low | 391 | 17.5 | 15.8–19.3 |
| Medium | 1348 | 65.9 | 63.5–68.1 |
| High | 346 | 16.7 | 14.9–18.7 |
| Partner living in household | |||
| No partner | 469 | 28.6 | 26.3–31.1 |
| Partner | 1616 | 71.4 | 68.9–73.7 |
| Living children | |||
| No child | 320 | 17.0 | 15.0–19.1 |
| Children | 1765 | 83.0 | 80.9–85.0 |
| Residence | |||
| Rural area | 1115 | 52.6 | 49.9–55.3 |
| Urban area | 970 | 47.4 | 44.7–50.1 |
| Linguistic region | |||
| German-speaking | 1539 | 73.6 | 71.1–75.9 |
| French-speaking | 490 | 24.1 | 21.9–26.5 |
| Italian-speaking | 56 | 2.3 | 1.7–3.2 |
CI = confidence interval
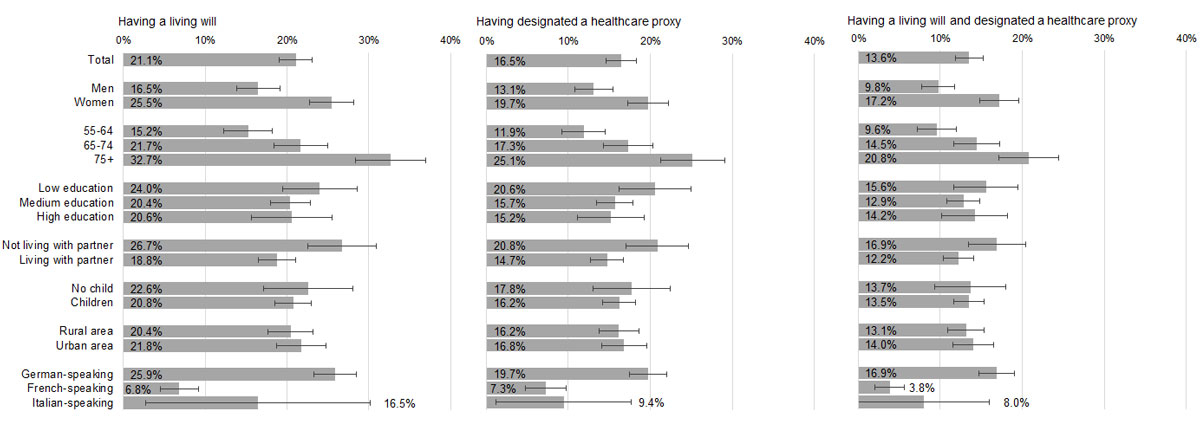
Figure 1 presents completion rates of different types of advance directives by sociodemographic characteristics. Levels of completion of living wills by sociodemographic characteristics were slightly higher than completion levels of the two other forms of advance directive, i.e., having designated a healthcare proxy or having both a living will and a healthcare proxy. However, the sociodemographic differences of the groups having completed a living will, having appointed a healthcare proxy or having done both were very similar. Levels of living will completion were lower among men (16.5%), among respondents aged 55 to 64 years (15.2%), and among individuals living with a partner (18.8%). Furthermore, 6.8% of people living in the French-speaking part of Switzerland had completed a living will, compared with 25.9% in German-speaking Switzerland.
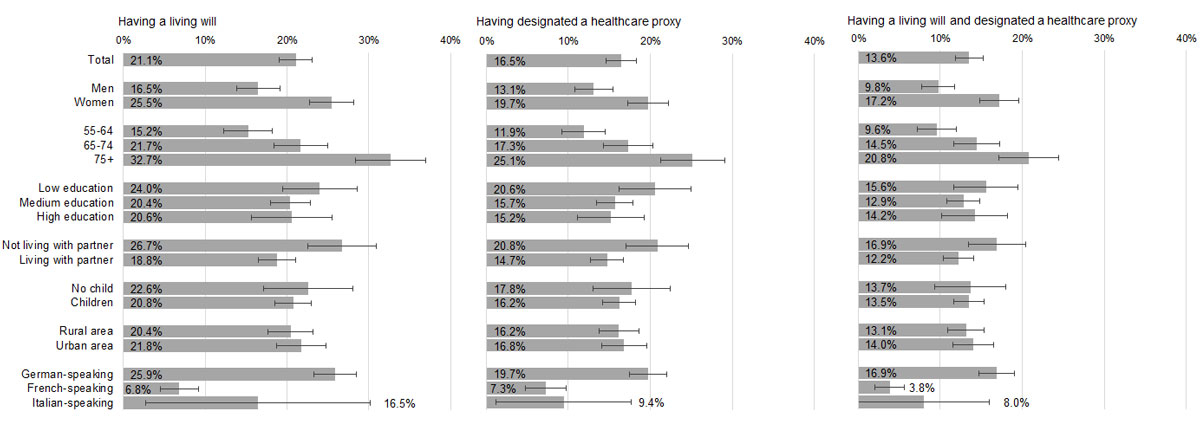
Figure 1 Completion of advance directives (ADs) by sociodemographic characteristics, adults aged 55+ in Switzerland, weighted percentage and 95% confidence intervals, SHARE 2015.
Figure 2 shows levels of awareness, approval and completion of advance directives by sociodemographic characteristics. The overall rate of advance directive awareness was 78.7%. The awareness rate was relatively low among respondents with a low education level (66.6%). Advance directive awareness was also particularly low in the French- and Italian-speaking parts of Switzerland (43.3% and 57.1%, respectively) compared with older persons living in German-speaking Switzerland (91%). Advance directive approval rates were close to the awareness rates. More specifically, men (73.0%), older respondents (67.8%), people with a low education level (62.2%) and those coming from French- (56.8%) and Italian- (49.4%) speaking Switzerland had relatively low advance directive approval rates when compared to people from their opposed category. In French-speaking Switzerland advance directive approval (56.8%) was significantly higher than awareness (43.3%). Finally, figure 2 shows that there is a large gap between awareness and approval of advance directives and their completion in most sociodemographic population groups.
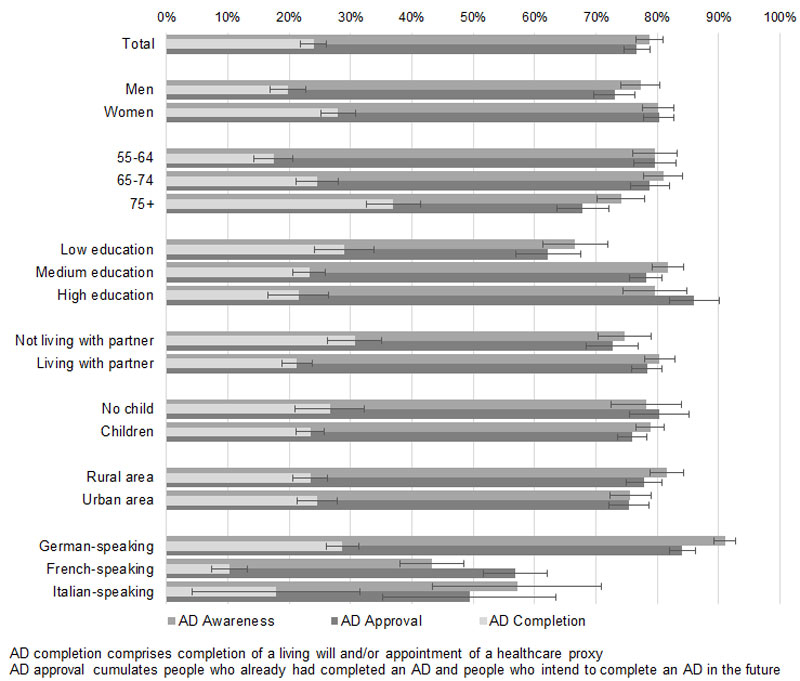
Figure 2 Awareness, approval and completion of advance directives (ADs) by sociodemographic characteristics, adults aged 55+ in Switzerland, weighted percentage and 95% confidence intervals, SHARE 2015.
Table 2 presents estimated AMEs based on logistic regression models of advance directive awareness, approval, and completion on sociodemographic characteristics (models 1a, 2a, 3a). In addition, in models 2b and 3b, advance directive approval and completion were controlled for advance directive awareness. Being a woman increased the probability of being aware of advance directives by 5.58 percentage points (model 1a), and of approving them by 11.3 percentage points (model 2a). Similarly, positive partial associations with advance directive awareness and approval were found for people with a higher education level and for those living with a partner. Conversely, being older (75+) and living in the French- and Italian-speaking parts of Switzerland were negatively associated with advance directive awareness and approval. Specifically, living in French- or Italian-speaking Switzerland decreased the probability of being aware of advance directives by 47.4 and 36.5 percentage points, respectively, compared with living in German-speaking Switzerland (reference group). People living in French- and Italian-speaking Switzerland were also less likely to approve of advance directives, but when controlled for advance directive awareness, the AMEs for approval were reduced by two thirds in French-speaking Switzerland, dropping from −27.2 to −8.11, and by roughly one half in Italian-speaking Switzerland, changing from −35.2 to −19.9. Women and older adults (age 65+) were more likely to have completed advance directives, whereas living with a partner and living in French- and Italian-speaking Switzerland reduced the chance of having completed an advance directive (models 3a and 3b in table 2). However, after controlling for advance directive awareness, AMEs of completion for people from French- and Italian-speaking Switzerland were again reduced by about one half (French-speaking Switzerland: −18.3 to −10.4 percentage points; Italian-speaking Switzerland: −15.7 to −8.11 percentage points).
Table 2 Average marginal effects (AMEs) of views of advance directives (ADs) by sociodemographic characteristics and AD awareness, adults aged 55+ in Switzerland (n = 2085), SHARE 2015.
|
AD awareness
AME (95% CI) |
AD approval
AME (95% CI) |
AD completion
AME (95% CI) |
|||
|---|---|---|---|---|---|
| Model 1a | Model 2a | Model 2b | Model 3a | Model 3b | |
| Women | 5.58**
(2.62–8.55) |
11.3**
(7.89–14.6) |
9.2**
(5.95–12.5) |
6.87**
(3.66–10.1) |
5.88**
(2.72–9.05) |
| Age groups | |||||
| 55–64 years (ref.) | – | – | – | – | – |
| 65–74 years | 0.21 (−3.25–3.67) |
-0.11 (−4.06–3.84) |
-0.29 (−4.01–3.44) |
7.95** (3.62–12.3) |
7.76** (3.51–12.0) |
| 75+ years | −4.35*
(−8.56 – −0.13) |
−7.51**
(−12.2 – −2.79) |
-5.77**
(−10.1 – −1.42) |
18.5**
(13.1–23.9) |
19.7**
(14.3–25.0) |
| Education level | |||||
| Low (ref.) | – | – | – | – | – |
| Medium | 7.84**
(3.41–12.3) |
11.6**
(6.66–16.6) |
8.34**
(3.77–12.9) |
−0.46 (−5.45–4.53) |
−2.38 (−7.44–2.68) |
| High | 9.63**
(4.21–15.1) |
18.40**
(12.4–24.4) |
14.30**
(8.69–20.0) |
2.53 (−4.44–9.49) |
0.012 (−6.84–6.87) |
| Partner living in household | 3.63 (−0.35–7.61) |
6.41**
(1.88–10.9) |
5.03*
(0.88–9.18) |
−5.01*
(−9.94–−0.08) |
−5.84*
(−10.7–−0.99) |
| Having children | −1.84 (−6.08–2.4) |
−2.64 (−7.55–2.28) |
−1.95 (−6.55–2.65) |
−4.45 (−10.5–1.58) |
−4.19 (−9.94–1.56) |
| Urban area | −0.54 (−3.70–2.62) |
1.38 (−2.2–4.96) |
1.66 (−1.64–4.97) |
−0.41 (−4.49–3.67) |
−0.48 (−4.47–3.52) |
| Linguistic region | |||||
| German-speaking (ref.) | – | – | – | – | – |
| French-speaking | −47.4**
(−52.5 – −42.4) |
−27.2**
(−32.1 – −22.3) |
−8.11**
(−13.0 – −3.26) |
−18.3**
(−22.2 – −14.4) |
−10.4**
(−15.2 – −5.66) |
| Italian-speaking | −36.50**
(−49.6 – −23.5) |
−35.20**
(−48.2 – −22.1) |
−19.9**
(−32.0 – −7.89) |
−15.7**
(−26.1 – −5.20) |
−8.11 (−20.4–4.19) |
| AD awareness | 26.0**
(22.8–29.2) |
26.6**
(19.3–33.9) |
|||
CI = confidence interval Average marginal effects based on logistic regression models. All probabilities are multiplied by 100. Asterisks indicate levels of significance: ** 1%; * 5%. The numbering of the models refers to the outcome variable of the regression model: (1) AD awareness; (2) AD approval; (3) AD completion. The alphabetic indicator refers to the set of independent variables used in the regression models: (a) sociodemographic variables only; (b) sociodemographic variables and AD awareness. Interpretation: Being a woman increases the probability of being AD aware by 5.58 percentage points.
Finally, respondents who had not completed advance directives at the time of the survey were asked for their reason(s) for not doing so (fig. 3). The most common response was “intending to complete advance directives in the future” (49.1%), followed by “it is too early” (32.9%) and “it's pointless to prepare for a hypothetical situation that one cannot judge well in advance” (22.7%). A few respondents declared that they did not think they needed and advance directive (10.4%) and that they were afraid of receiving lower quality of healthcare if they completed one (3.8%).
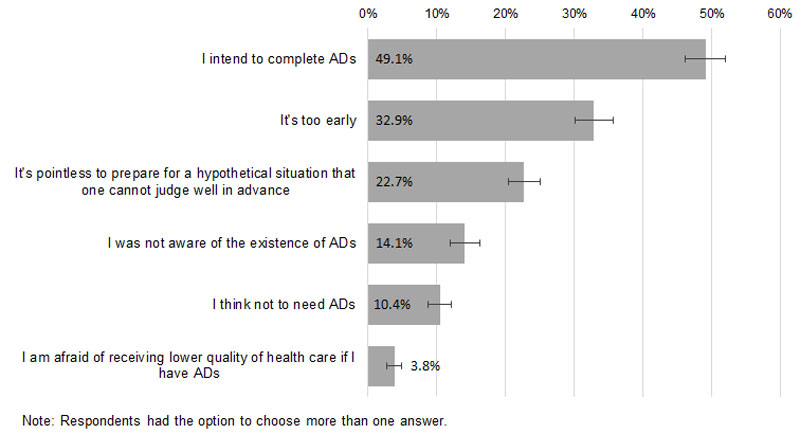
Figure 3 Reasons for not having completed an advance directive (AD), adults aged 55+ in Switzerland, weighted percentage and 95% confidence intervals, SHARE 2015.
To the best of our knowledge, our study is the first to provide information about sociodemographic patterns of awareness, approval and completion of advance directives among the general population aged 55 and over following the introduction of advance directives in Switzerland.
Our data show that slightly less than one quarter of all respondents had completed an advance directive, with significant variation across different population groups. In countries where advance directives have legal value, such as in the USA and in some European countries, a large number of studies have assessed completion rates. Comparisons of completion rates across countries are challenging because of (i) differences in the definition of advance directives, (ii) differences in study populations (e.g., young adults vs older persons, general population vs cancer patients), and (iii) national variation in the time of legal implementation of advance directives, ranging from the early 1990s in some US states (Patient Self-Determination Act) to the first decade of the 21st century in some European countries (United Kingdom, Spain, Germany, the Netherlands, Belgium…) [22]. A recent literature review on advance directive completion rates within the USA stated that the prevalence rates across studies ranged from 0.0 to 93.8% [23].
However, some determinants of advance directive completion remained stable across the different studies. Being a woman, being older and having higher levels of education was positively associated with completion [24–29]. The results of our study are largely in line with these findings, with the exception of the education gradient. In Switzerland, older people with a higher education level were more advance directive aware and more likely to approve of them than less educated older persons, but not more likely to complete an advance directive. In our study, women had higher levels of advance directive awareness, approval and completion than men. Women have a higher chance of surviving their spouse, as they are often younger than their husband and women have a higher life expectancy than men. Women are usually also more involved in caring for relatives [30]. It has been shown that people who took care of a dying person are themselves more likely to complete an advance directive [29]. These may be reasons why women were more likely to complete one: they experience more often the end of life of loved ones and know what they are very likely to face at the end of their own life.
Not surprisingly, older adults were more likely to have completed an advance directive than younger adults aged 55 to 64 years. It is well known that proximity to death and experience of the deaths of loved ones, which both increase with age, are conducive to advance directive completion [27–29]. Conversely, adults living with a partner in the same household were less likely to have completed an advance directive than people living alone, most likely due to the belief that the partner may know about one’s own end-of-life treatment preferences and will make the right decisions on one’s behalf [31]. Indeed, daily life with the spouse favours informal discussion around end-of-life preferences and increases the knowledge of the spouse’s values regarding end-of-life issues, which does not happen with children, other relatives or physicians [31].
Older adults from French- and Italian-speaking Switzerland were considerably less likely than adults from German-speaking Switzerland to be aware and to have completed an advance directive. Interestingly, this lack of awareness in French- and Italian-speaking Switzerland may be an important driver of the lower approval and completion of advance directives in these regions. The relationship between awareness and completion of advance directives warrants further prospective investigation.
A main factor that could reasonably explain the significantly higher level of advance directive awareness in German-speaking Switzerland might be a broader exposure to media information about advance directives in this region. Alano et al. showed that having seen mass media information about advance directives was a factor associated with completion of one [24]. In Germany, there was extensive media coverage of the parliamentary debate about the law on advance directives, which lasted over two legislative periods [32], until the legislation finally came into force on 1 September 2009. Besides, since the 1990s, the German media widely relayed court decisions about demands for treatment withdrawal made for mentally incapacitated patients [33]. Consequently, 94% of the German population aged 16 years and over knew of advance directives in 2014 [34]. People from the German-speaking part of Switzerland have easy access to the German media and have thus been much more exposed to information about advance directives than French- or Italian-speaking adults. Interestingly, the level of advance directive awareness in German-speaking Switzerland (91%) is very close to the corresponding awareness level measured in the German population (93%).
On the other hand, the promotion of patient self-determination and of the completion of advance directives is more recent in France, where physicians were often reported to have had a paternalistic relationship with their patients [35]. Indeed, the Leonetti law [36] that strengthens patient autonomy and renders advance directives legally binding came into force only in 2016. In Italy, a law on advance directives has been debated since 2009, with the Catholic Church being strictly opposed to the principle of withdrawing nutrition and hydration in patients in persistent vegetative states, and was finally adopted in December 2017 [37]. Thus, the patterns found in the three Swiss linguistic regions parallel the discussions on advance directives in Germany, France and Italy.
However, lack of awareness is not the only potential explanation for the lower advance directive completion rates in the French- and Italian-speaking parts of Switzerland. Cultural differences may also play a role. Swiss researchers demonstrated large regional differences in end-of-life healthcare utilisation, costs and place of death in Switzerland [3, 38–40]. Linguistic regions, considered as a proxy for cultural regions, accounted for some of the regional variance, as well as other factors such as healthcare infrastructure. Additionally, Fischer et al. showed that doctors’ attitudes regarding end-of-life decisions differ between the three language regions, although the same legislation applies and the guidelines for end-of-life decisions from the Swiss Academy of Medical Sciences are valid throughout Switzerland [41]. In the French-speaking region, doctors were more in favour of alleviation of pain and other symptoms, with possible life-shortening side effects, but were less inclined to make decisions on withholding or withdrawing treatment than doctors from the German-speaking part of Switzerland. In another Swiss study on cancer inpatients, one fifth of the patients did not want to take part in medical decision making, but this proportion reached 77% in Ticino [42]. These studies show that beliefs and expectations regarding the end of life differ across linguistic regions, suggesting that the impact of culture on end-of-life behaviours needs to be further investigated. Notably, only by informing our respondents about the existence of advance directives in Switzerland through our questionnaire, in French-speaking Switzerland more than one in three respondents who were not aware of advance directives before our survey, declared that they plan to complete one in the future.
Whereas about four out of five adults aged 55+ were aware of the existence of advance directives, and almost as many people approved their completion, only a minority of respondents had effectively completed an advance directive. Of those who did not, almost half declared that they intended to complete one in the future. These results suggest that people have the feeling that they still have time to complete an advance directive. In fact, one-third reported specifically that it was too early to complete an advance directive. The absence of a feeling of urgency may be motivated by a belief that the prospect of death is still distant or that the spouse will take care of one’s end-of-life wishes [31]. Although a large majority of adults indicated that advance directives should be completed when a person is healthy [43] and Swiss general practitioners largely agree with this view [44], Silveira et al. showed that advance directives were completed a mean of 40.3 months before death [45], indicating that a change in health status strongly promotes their completion.
Numerous other barriers to advance directive completion exist. Our study showed that 22.7% of our respondents without an advance directive declared that it is pointless to prepare for a hypothetical situation that one cannot judge well in advance. Some other studies stated the difficulty, and sometimes the nonsense, for some adults of making plans for an unknown future. In a systematic review of attitudes to advance care planning in older patients with no specific diagnosis, Sharp et al. exposed the uncertainty regarding the future illness and decline as a barrier for completing advance directives. This view was shared by older adults from the United Kingdom, who were concerned with the future applicability of advance directives [46]. Indeed, these doubts were also shared by people who had already completed an advance directive [6].
Our study has several limitations. On the subject of missing data, older people and people with a low education level were slightly more likely not to have answered the outcome questions. However, in both these population groups, non-response rates were always below 10%. Thus, it appears unlikely that missing data may have skewed our results in a meaningful way. The rates of advance directive awareness, approval and completion may be overestimated for two main reasons. First, although we described advance directives in detail in our questionnaire, some respondents may have confused them with a testament or similar document. Similarly, some respondents may have declared that they had appointed a healthcare proxy even if they had not done so in writing. Second, there may be a social desirability bias when reporting an intention to complete advance directives in the future, as people tend to believe that they are expected to have one. Furthermore, the data from the Italian-speaking part of Switzerland must be considered with caution, as the sample of this region in SHARE is very small (n = 56). Finally, age-group differences found in our study may be related in part to cohort differences. As a result of the cross-sectional design, our results did not allow us to determine whether age differences are an effect of life-cycle processes, views and preferences changing with age, or a change of mentality, need of self-determination and autonomy in healthcare reflecting contemporary values.
In Switzerland, additional interventions are needed to (i) increase awareness of advance directives, especially in the French- and Italian-speaking parts of Switzerland, and (ii) facilitate timely advance directive completion in view of their generally high level of approval. Information about the possibility of completing advance directives and their benefits is already distributed via social organisations defending the interests of older persons and specific patient groups, but could also be more broadly and systematically provided by family physicians, acute care hospitals, and the media. The recent revision of the Swiss outpatient financing system reducing the time for a consultation in general medicine to 20 minutes will probably constitute an additional barrier to advance directive discussions between family physicians and their patients in the future.
This paper benefited from comments by Simon Seiler.
This paper uses data from SHARE release 6.0.0, as of March 31th 2017. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N°211909, SHARE-LEAP: N°227822, SHARE M4: N°261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org). We gratefully acknowledge financial support from the Swiss National Science Foundation.
The authors declare that they have no competing interests.
1Décès. Neuchâtel: Office fédéral de la statistique; 2018 [cited 2018 06.02]; Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/population/naissances-deces/deces.html.
2 Bosshard G , Zellweger U , Bopp M , Schmid M , Hurst SA , Puhan MA , et al. Medical End-of-Life Practices in Switzerland: A Comparison of 2001 and 2013. JAMA Intern Med. 2016;176(4):555–6. doi:.https://doi.org/10.1001/jamainternmed.2015.7676
3 Reich O , Signorell A , Busato A . Place of death and health care utilization for people in the last 6 months of life in Switzerland: a retrospective analysis using administrative data. BMC Health Serv Res. 2013;13(1):116. doi:.https://doi.org/10.1186/1472-6963-13-116
4 Silveira MJ , Kim SY , Langa KM . Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–8. doi:.https://doi.org/10.1056/NEJMsa0907901
5 Pautex S , Herrmann FR , Zulian GB . Role of advance directives in palliative care units: a prospective study. Palliat Med. 2008;22(7):835–41. doi:.https://doi.org/10.1177/0269216308094336
6 van Wijmen MP , Pasman HR , Widdershoven GA , Onwuteaka-Philipsen BD . Motivations, aims and communication around advance directives: a mixed-methods study into the perspective of their owners and the influence of a current illness. Patient Educ Couns. 2014;95(3):393–9. doi:.https://doi.org/10.1016/j.pec.2014.03.009
7 Detering KM , Hancock AD , Reade MC , Silvester W . The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340(mar23 1):c1345. doi:.https://doi.org/10.1136/bmj.c1345
8 Martin DK , Emanuel LL , Singer PA . Planning for the end of life. Lancet. 2000;356(9242):1672–6. doi:.https://doi.org/10.1016/S0140-6736(00)03168-8
9 Carr D , Luth E . Advance Care Planning: Contemporary Issues and Future Directions. Innovation in Aging. 2017;1(1):igx012. doi:.https://doi.org/10.1093/geroni/igx012
10 Carr D . Death and dying in the contemporary United States: what are the psychological implications of anticipated death? Soc Personal Psychol Compass. 2012;6(2):184–95. doi:.https://doi.org/10.1111/j.1751-9004.2011.00416.x
11Des directives anticipées du patient, Art. 370 (2008). Available from: http://www.loisuisse.ch/fra/sr/210/210_033.htm
12Directives anticipées – pour plus de sécurité. Fédération des médecins suisses; 2018 [cited 2018 06.02]; Available from: https://www.fmh.ch/files/pdf16/FMH_PV_AV_2015_f.pdf.
13Dossier pour les directives anticipées. ProSenectute; 2018 [cited 2018 06.02]; Available from: https://www.prosenectute.ch/fr/shop/dossier-pour-les-directives-anticip%C3%A9es.html.
14Etablissez vos directives anticipées avec nous. Croix Rouge Suisse; 2018 [cited 2018 06.02]; Available from: http://directives-anticipees.redcross.ch/.
15SHARE. End-of-life questionnaire. Munich: Max Planck Institute for Social Law and Social Policy (MEA); 2018 [cited 2018 14.05.2018]; Available from: http://www.share-project.org/fileadmin/pdf_questionnaire_wave_6/DO_EN_SHARE_04.12.2014corr.pdf.
16Börsch-Supan A. Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 6. Release version: 6.0.0. In: SHARE-ERIC, editor. 2017.
17Klevmarken A, Hesselius P, Swensson P. The SHARE Sampling Procedures and Calibrated Designs Weights In: Börsch-Supan A, Jürges H, editors. The Survey of Health, Ageing and Retirement in Europe – Methodology. Mannheim: Mannheim Research Institute for the Economics of Aging (MEA); 2005. p. 66-9.
18Lynn P, De Luca G, Ganninger M, Häder S. Sample Design in SHARE Wave Four. In: Malter F, Börsch-Supan A, editors. SHARE Wave 4: Innovations & Methodology. Munich Munich Center for the Economics of Aging (MEA); 2013. p. 91-3.
19SHARE Release Guide 6.0.0. Munich: MEA, Munich Center for the Economics of Aging; 2017.
20Solon G, Haider SJ, Wooldridge J. What Are We Weighting For? NBER working paper series. 2013. Available from: https://msu.edu/~solon/WAWWFfeb2013.pdf
21 Williams R . Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12(2):308–31.
22 Andorno R , Biller-Andorno N , Brauer S . Advance health care directives: towards a coordinated European policy? Eur J Health Law. 2009;16(3):207–27. doi:.https://doi.org/10.1163/157180909X453053
23 Yadav KN , Gabler NB , Cooney E , Kent S , Kim J , Herbst N , et al. Approximately One In Three US Adults Completes Any Type Of Advance Directive For End-Of-Life Care. Health Aff (Millwood). 2017;36(7):1244–51. doi:.https://doi.org/10.1377/hlthaff.2017.0175
24 Alano GJ , Pekmezaris R , Tai JY , Hussain MJ , Jeune J , Louis B , et al. Factors influencing older adults to complete advance directives. Palliat Support Care. 2010;8(3):267–75. doi:.https://doi.org/10.1017/S1478951510000064
25 del Pozo Puente K , Hidalgo JL , Herráez MJ , Bravo BN , Rodríguez JO , Guillén VG . Study of the factors influencing the preparation of advance directives. Arch Gerontol Geriatr. 2014;58(1):20–4. doi:.https://doi.org/10.1016/j.archger.2013.07.009
26 Rao JK , Anderson LA , Lin FC , Laux JP . Completion of advance directives among U.S. consumers. Am J Prev Med. 2014;46(1):65–70. doi:.https://doi.org/10.1016/j.amepre.2013.09.008
27 Rurup ML , Onwuteaka-Philipsen BD , van der Heide A , van der Wal G , Deeg DJ . Frequency and determinants of advance directives concerning end-of-life care in The Netherlands. Soc Sci Med. 2006;62(6):1552–63. doi:.https://doi.org/10.1016/j.socscimed.2005.08.010
28 van Wijmen MP , Rurup ML , Pasman HR , Kaspers PJ , Onwuteaka-Philipsen BD . Advance directives in the Netherlands: an empirical contribution to the exploration of a cross-cultural perspective on advance directives. Bioethics. 2010;24(3):118–26. doi:.https://doi.org/10.1111/j.1467-8519.2009.01788.x
29 Wilson DM , Houttekier D , Kunju SA , Birch S , Cohen J , MacLeod R , et al. A population-based study on advance directive completion and completion intention among citizens of the western Canadian province of Alberta. J Palliat Care. 2013;29(1):5–12.
30Colombo F, Llena-Nozal A, Mercier J, Tjadens F. The impact of caring on families carers. In: Studies OHP, editor. Help wanted? Providing and paying for long-term care: OECD Publishing; 2011.
31 Hopp FP . Preferences for surrogate decision makers, informal communication, and advance directives among community-dwelling elders: results from a national study. Gerontologist. 2000;40(4):449–57. doi:.https://doi.org/10.1093/geront/40.4.449
32 Wiesing U , Jox RJ , Hessler HJ , Borasio GD . A new law on advance directives in Germany. J Med Ethics. 2010;36(12):779–83. doi:.https://doi.org/10.1136/jme.2010.036376
33 Horn R . “Why Should I Question a Patient’s Wish?” A Comparative Study on Physicians’ Perspectives on Their Duties to Respect Advance Directives. Eur J Health Law. 2017;24(5):523–40. doi:.https://doi.org/10.1163/15718093-12341437
34Deutlicher Anstieg bei Patientenverfügungen. Allensbach: Institut für Demoskopie Allensbach; 2014. Available from: https://www.ifd-allensbach.de/uploads/tx_reportsndocs/PD_2014_20.pdf
35Palazzolo J. Les nouvelles relations médecin-malade. Cerveau et Psycho. 1999;30 November. Available from: https://www.cerveauetpsycho.fr/sd/medecine/les-nouvelles-relations-medecin-malade-1697.php
36LOI n° 2016-87créant de nouveaux droits en faveur des malades et des personnes en fin de vie. 2016. Available from : https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000031970253&categorieLien=id
37C'è l'ok del Senatio, il biotestamento è legge: ecco che cosa prevede. La Stampa. 2017. 14 December. Available from: http://www.lastampa.it/2017/12/14/italia/c-lok-del-senato-il-biotestamento-legge-1JjGIIKEzi7W8autnHwnUO/pagina.html
38 Busato A , Künzi B . Primary care physician supply and other key determinants of health care utilisation: the case of Switzerland. BMC Health Serv Res. 2008;8(1):8. doi:.https://doi.org/10.1186/1472-6963-8-8
39 Luta X , Panczak R , Maessen M , Egger M , Goodman DC , Zwahlen M , et al. Dying among older adults in Switzerland: who dies in hospital, who dies in a nursing home? BMC Palliat Care. 2016;15(1):83. doi:.https://doi.org/10.1186/s12904-016-0156-x
40 Panczak R , Luta X , Maessen M , Stuck AE , Berlin C , Schmidlin K , et al. Regional Variation of Cost of Care in the Last 12 Months of Life in Switzerland: Small-area Analysis Using Insurance Claims Data. Med Care. 2017;55(2):155–63. doi:.https://doi.org/10.1097/MLR.0000000000000634
41 Fischer S , Bosshard G , Faisst K , Tschopp A , Fischer J , Bär W , et al. Swiss doctors’ attitudes towards end-of-life decisions and their determinants: a comparison of three language regions. Swiss Med Wkly. 2006;136(23-24):370–6.
42 Pautex S , Gamondi C , Philippin Y , Gremaud G , Herrmann F , Camartin C , et al. Advance directives and end-of-life decisions in Switzerland: role of patients, relatives and health professionals. BMJ Support Palliat Care. 2015 2 September:bmjspcare-2014-000730. doi:.https://doi.org/10.1136/bmjspcare-2014-000730
43 Nolan MT , Bruder M . Patients’ attitudes toward advance directives and end-of-life treatment decisions. Nurs Outlook. 1997;45(5):204–8. doi:.https://doi.org/10.1016/S0029-6554(97)90066-X
44 Otte IC , Jung C , Elger BS , Bally K . Advance directives and the impact of timing. A qualitative study with Swiss general practitioners. Swiss Med Wkly. 2014;144:w14035. doi:.https://doi.org/10.4414/smw.2014.14035
45 Silveira MJ , Wiitala W , Piette J . Advance directive completion by elderly Americans: a decade of change. J Am Geriatr Soc. 2014;62(4):706–10. doi:.https://doi.org/10.1111/jgs.12736
46 Seymour J , Gott M , Bellamy G , Ahmedzai SH , Clark D . Planning for the end of life: the views of older people about advance care statements. Soc Sci Med. 2004;59(1):57–68. doi:.https://doi.org/10.1016/j.socscimed.2003.10.005
JM and GDB contributed equally to the manuscript.
This paper uses data from SHARE release 6.0.0, as of March 31th 2017. The SHARE data collection has been primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N°211909, SHARE-LEAP: N°227822, SHARE M4: N°261982). Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and from various national funding sources is gratefully acknowledged (see www.share-project.org). We gratefully acknowledge financial support from the Swiss National Science Foundation.
The authors declare that they have no competing interests.