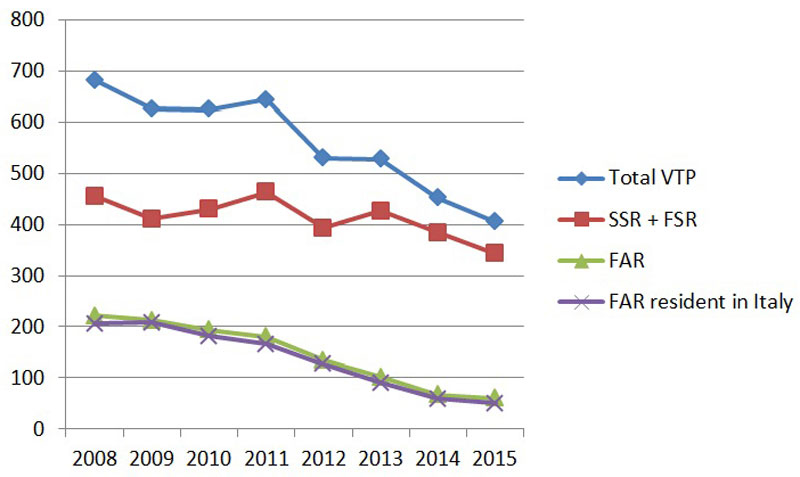
Figure 1 Number of abortions from 2008 to 2015 for women resident in Switzerland (SSR + FSR), foreign women resident abroad (FAR) and foreign women resident in Italy.
DOI: https://doi.org/10.4414/smw.2018.14636
Since the modification of the Swiss Criminal Code (art. 119–120) in 2002, termination of pregnancy within 12 weeks from the beginning of the last menstrual period is legal in Switzerland [1]. The law delegates the decision to the pregnant woman, who has to make a request and sign an official information document. Women under 16 years of age must visit a specialised consultation centre for minors. Termination of pregnancy after the 12th week from the last menstrual period is legal and voluntary, but requires a medical indication based on the particular condition of the pregnant woman (serious psychological distress or serious physical injury).
In Switzerland, voluntary termination of pregnancy (VTP) can be performed in all public and private hospitals with an obstetrics/gynaecology department. Some cantons also authorise private doctors to perform VTPs. In Canton Ticino (southern Switzerland, bordering Italy), all private doctors certified by the Swiss Medical Association (FMH) as specialists in obstetrics/gynaecology and in possession of cantonal permission to work as an independent doctor are authorised to perform VTPs.
In 2002, the modification of the Swiss Criminal Code had to be implemented in all 26 Swiss cantons in their own independent healthcare systems. It means that the cantons have to ensure that all women have access to VTP and they have to guarantee the presence of specialised consultation centres for counselling (family planning centres, FPCs) in their territory. Since 1981, the federal law concerning FPCs had already obligated the cantons to establish of this kind of institution, where trained specialists in sexual health, free of charge, give non-directive counselling and answer every type of question, whether it be ethical, psychological, social, legal or financial. For a population of 350,363 citizens, in Canton Ticino (2014) we have four FPCs situated in the four public hospitals [2].
The cantonal health system of Ticino can be used not only by Swiss residents, but also residents abroad, in particular from Italy. For various reasons, many Italian women living close to the Swiss border consult the Swiss healthcare system when they take the decision to have a VTP.
This study aimed to illustrate the trend in VTPs in the Canton Ticino, a border region adjacent to Italy, between 2008 and 2015 (before 2008 the dataset available was not complete), and demonstrate differences between the Swiss women resident in Switzerland (SSRs), foreign women resident in Switzerland (FSRs) and foreign women resident abroad (FARs), focusing in particular on Italian women in a period of legal changes. In addition, we wanted to evaluate the impact of the pre-VTP counselling at the FPC on the decision to have a VTP.
The results presented in this article focus on women who had decided to terminate their pregnancy within 12 completed weeks of gestation, as well as women who had to terminate the pregnancy for medical reasons after the 12th week of gestation.
For this study we used two sources of data, the VTP database of the office of the Chief Medical Officer of Ticino and the annual reports of the activities of the family planning centres in Ticino.
Based on article 119 of the Criminal Code of Switzerland, independently of the place of the intervention, all VTPs have to be declared anonymously to the cantonal health authorities; in Ticino this is the office of the Chief Medical Officer. Every canton has the duty to define the information which the doctors performing the VTP need to report for every VTP (data collection).
For all VTPs after the 12th week after the last menstrual period, doctors have in addition to record the reason for the VTP, either maternal (psychological distress or somatic complications) or fetal (malformations).
Since 2008, in the Canton Ticino physicians have to answer 15 multiple-choice questions on an official form and to send it to the office of the Chief Medical Officer. The form contains questions about: (1) sociodemographic data; (2) place and method of intervention; (3) pre- and post-VTP counselling; and (4) pre- and post-VTP contraception. All the data reported in the form are recorded in a specific database. Every year, the Swiss Federal Office for Statistics receives a basic dataset from all 26 cantons for the national VTP statistics, which can be used to compare data [3].
Statistical analysis was performed on reported data in the VTP database for a period from 1 January 2008 to 31 December 2015. Associations between categorical variables was tested using a chi-squared test, with a significance level of α = 0.05. In order to control for the false positive rate, a Bonferroni correction was applied on multiple tests of the four most common contraceptive methods (condom, coitus interruptus, contraceptive pill, infertile days) and no contraception. The strength of the relationships between the place of residence and a set of different dependent variables (place of intervention, VTP method, type of counselling, contraception method and year) was determined using binary logistic regressions, considering nationality/residence (resident and Swiss, resident but not Swiss and not resident) as predictor variable and all the other covariates as response variables. The strength of the relationships between repeated VTPs and nationality/residence, personal status, contraception method and children was measured by first selecting the set of variables through a bivariate analysis (chi-squared test; α = 0.05) and then performing a binary logistic regression analysis using repeated abortions (0 or ≥1) as dependent variable. Each regression model was controlled for the age as a continuous covariate. Data analysis was performed using IBM SPSS Statistics v.21, R language and Excel.
All FPCs in every canton have to document all their activities in an annual report; in Ticino this is sent every year to the office of the Chief Medical Officer. In the present study, we used the data collected from the FPCs for the years 2008–2015 to highlight the number of women who changed their minds after the pre-VTP counselling and decided to continue the pregnancy. We did not have any control over data registration and data processing by the FPCs.
The results of our retrospective study are based on analysis of the database of the office of the Chief Medical Officer of Ticino for VTPs performed from 1 January 2008 to 31 December 2015 (4492 VTPs; table 1). The cohort consisted of 2024 (45.1%) SSRs, 1281 (28.5%) FSRs and 1173 (26.1%) FARs (table 1). The majority of the interventions were in women living in Canton Ticino (3305, 73.5%), followed by foreign women resident in Italy, with 1088 VTPs (24.2%) (table 1). Only a few women from other Swiss cantons (84, 1.8%) came to Ticino for a VTP.
Table 1 Study sample characteristics.
| n | % | |
|---|---|---|
| Total | 4492 | 100 |
| Age | ||
| 10–14 years | 6 | 0.1 |
| 15–19 years | 434 | 9.7 |
| 20–24 years | 800 | 17.8 |
| 25–29 years | 839 | 18.7 |
| 30–34 years | 927 | 20.6 |
| 35–39 years | 894 | 19.9 |
| 40–44 years | 514 | 11.4 |
| ≥45 years | 78 | 1.7 |
| Personal status | ||
| Single | 859 | 19.1 |
| Single with child(ren) | 464 | 10.3 |
| With partner | 798 | 17.8 |
| With partner and child(ren) | 1293 | 28.8 |
| With friends | 79 | 1.8 |
| With parents/family | 999 | 22.2 |
| Children | ||
| No children | 2441 | 54.3 |
| One or more children | 2051 | 45.7 |
| Nationality/Residence | ||
| Swiss/Switzerland (SSR) | 2024 | 45.1 |
| Foreign/Switzerland (FSR) | 1281 | 28.5 |
| Foreign/abroad (FAR) | 1173 | 26.1 |
| Resident in Italy | 1088 | 24.2 |
| Swiss/abroad (SAR) | 14 | 0.3 |
| Previous VTP | ||
| No | 3391 | 75.5 |
| Yes | 1101 | 24.5 |
| Contraception before VTP | ||
| Present | 2525 | 56.2 |
| Absent | 1967 | 43.8 |
| Counselling pre-VTP | ||
| No | 280 | 6.2 |
| Yes | 4242 | 93.8 |
VTP = voluntary termination of pregnancy
For the Ticino, we observed a mean rate of 8.9 interventions per 1000 women 15–44 years of age per year; this rate is higher than the national mean of 6.8 interventions (table 2). For the women residents in Switzerland only (SSRs + FSRs), the mean rate of 6.5 is comparable to the national mean (table 2); moreover we observed a diminution in the VTPs required by women resident in Switzerland from 2008 to 2015 (fig. 1). The most significant difference was in the number of the VTPs performed on FAR women (26.1%, table 1), most of whom were foreign women resident in Italy (24.2%, table 1).
Table 2 Number and rate of abortions from 2008 to 2015.
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| VTPs (absolute number) | |||||||||
| Ticino | 682 | 626 | 625 | 644 | 530 | 528 | 452 | 405 | 4492 |
| Resident in Switzerland (SSR + FSR) | 455 | 411 | 430 | 463 | 393 | 426 | 384 | 343 | 3305 |
| Resident abroad (FAR) | 222 | 213 | 194 | 180 | 135 | 102 | 67 | 60 | 1173 |
| Resident in Italy | 206 | 208 | 182 | 166 | 127 | 90 | 59 | 50 | 1088 |
| VTPs (rate*) | Mean | ||||||||
| Ticino | 10.6 | 9.8 | 9.8 | 10.5 | 8.6 | 8.5 | 7.3 | 6.6 | 8.9 |
| Resident in Switzerland (SSR + FSR) | 7 | 6.3 | 6.7 | 7.4 | 6.3 | 6.8 | 6.1 | 5.6 | 6.5 |
| Switzerland | 7 | 6.8 | 7.1 | 7.1 | 6.9 | 6.7 | 6.5 | 6.4 | 6.8 |
VTP = voluntary termination of pregnancy * rate per 1000 women 15–44 years of age [3]
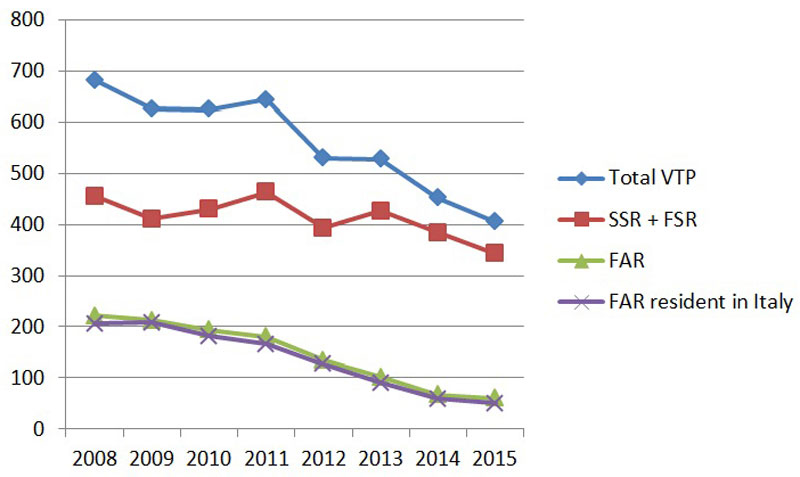
Figure 1 Number of abortions from 2008 to 2015 for women resident in Switzerland (SSR + FSR), foreign women resident abroad (FAR) and foreign women resident in Italy.
After many years of stability, the total number declined from 644 interventions in 2011 to 530 in 2012, a decrease of 17.7%. This trend continued to the end of the observation period, with 405 interventions in 2015. The total reduction from 2008 to 2015 was 41%, explained by the striking drop in VTPs in foreign women resident in Italy from 206 in 2008 to 50 in 2015 (decrease of 75.7%; table 2). Figure 1 shows the trends in VTPs from 2008 until 2015, which confirm the decrease in FAR women and, if the periods pre/post 2009 are compared, especially for those resident in Italy versus women resident in Switzerland (SSRs + FSRs) (odds ratio [OR] 0.574, 95% confidence interval [CI] 0.496–0.0665; p <0.001, age adjusted). The mean age of the women was 29 years for SSRs, 30 for FSRs and 32 for FARs. The total number of women <16 years of age was very small (0.9%) over all the observation time (data not shown).
In Switzerland, two methods are used to perform a VTP: medical (misoprostol) and surgical. In Ticino, for both SSR and FSR women the method was medical in 56%; a surgical method was used in 43.3 and 42.7%, respectively (table 3). For FAR women the medical method was used more frequently (86.8%, table 3) than for SSR women (OR 5.145, 95% CI 4.240–6.244; p <0.001, age adjusted).
Table 3 VTP method chosen (2008–2015).
|
Surgical
n (%) |
Medical
n (%) |
Both
n (%) |
n | |
|---|---|---|---|---|
| SSR | 883 (43.3) | 1141 (56.0) | 14 (0.7) | 2038 |
| FSR | 547 (42.7) | 718 (56.0) | 16 (1.3) | 1281 |
| FAR | 152 (13.0) | 1019 (86.8) | 2 (0.2) | 1173 |
| Total | 1582 (35.2) | 2878 (64.1) | 32 (0.7) | 4492 |
FAR = foreign women resident abroad; FSR = foreign women resident in Switzerland; SSR = Swiss women resident in Switzerland; VTP = voluntary termination of pregnancy
The majority of the VTPs were carried out in private or public hospitals (n = 3295, 73.3%). A total of 1197 (26.7%) interventions were in private doctors’ offices (table 4). FAR women underwent VTP at a private doctor’s office, rather than at private or public hospital, more often than the SSRs (65.7 vs 14.1%; table 4). There was a significant correlation between FAR status and a private doctor’s office as the place of intervention (OR 10.884, 95% CI 9.134–12.969; p <0.001, age adjusted). Women resident in Switzerland preferred to have the intervention in a hospital (2893, 87.2%; table 4).
Table 4 Place of VTP chosen (2008–2015).
|
Hospital (public or private)
n (%) |
Private doctor’s office
n (%) |
n | |
|---|---|---|---|
| SSR | 1751 (85.9) | 287 (14.1) | 2038 |
| FSR | 1142 (89.1) | 139 (10.9) | 1281 |
| FAR | 402 (34.3) | 771 (65.7) | 1173 |
| Total | 3295 (73.3) | 1197 (26.7) | 4492 |
FAR = foreign women resident abroad; FSR = foreign women resident in Switzerland; SSR = Swiss women resident in Switzerland; VTP = voluntary termination of pregnancy
An analysis of the choice of the place of intervention and the method used showed a significant difference between SSR and FAR women (p <0.01, data not shown).
Most of the VTPs (4370, 97.3%) were performed within the first 12 weeks of gestation. Only 122 VTPs (2.7%) were after week 12.
The reasons for the VTP after the 12th week were: maternal, such as psychiatric problems (n = 5), psychosocial problems (n = 22) and somatic complications (n = 3); or fetal, such as malformations (n = 92). By law, in Switzerland there are no recognised fetal indications for termination of pregnancy; rather, cases where VTP is requested because of fetal malformations require a medical indication, such as the pregnant woman being in a condition of serious psychological distress.
In our cohort three quarters of the women (3391, 75.5%) had no previous VTP, but a substantial proportion (1101, 24.5%) had already had a VTP in the past (table 1). Most of them (80%) had one VTP before and the 20% more than one.
Social factors, such as living with a partner and child(ren) (p <0.05) or living with parents/family (p <0.001) could represent a protective factor in reducing multiple VTPs (table 5). In contrast, the use of the contraceptive pill (p <0.001) did not seem to protect against multiple VTPs (table 5).
Table 5 Multiple VTP (regression model).
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| Nationality/residence | |||
| SSR | 1 | ||
| FSR | 1.709 | 1.447–2.018 | <0.001 |
| FAR | 0.958 | 0.798–1.152 | ns |
| Personal status | |||
| Single | 1 | ||
| Single with child(ren) | 1.122 | 0.801–1.572 | ns |
| With partner | 0.860 | 0.683–1.083 | ns |
| With partner and child(ren) | 0.682 | 0.504–0.923 | <0.05 |
| With parents/family | 0.506 | 0.390–0.656 | <0.001 |
| Contraception before VTP | |||
| No contraception | 1 | ||
| Condom | 1.015 | 0.854–1.206 | ns |
| Pill | 1.742 | 1.372–2.213 | <0.001 |
| Family | |||
| No children | 1 | ||
| Children | 1.416 | 1.080–1.854 | <0.05 |
FAR = foreign women resident abroad; FSR = foreign women resident in Switzerland; SSR = Swiss women resident in Switzerland; VTP = voluntary termination of pregnancy
Immigrant women (FSRs), regardless of the country of origin, had a higher probability of multiple VTPs than Swiss women living in Ticino (p <0.001; Table 5).
In our study cohort, 2525 (56.2%) used a contraceptive method before VTP and 1967 (43.8%) did not (table 1). The contraceptive method more frequently used was the condom followed by coitus interruptus, the contraceptive pill and infertile days (fig. 2). There was a significant difference in the frequency of no contraception use between SSR (39.1%), FSR (43.9%) and FAR (51.4%) women (p <0.01). FAR and FSR women used condoms less often (OR 0.583, 95% CI 0.484– 0.702; p <0.001, age adjusted and OR 0.663, 95% CI 0.554–0.793; p<0.001, age adjusted, respectively). Only the FAR women used the pill less frequently than SSR women (OR 0.471, 95% CI 0.344–0.644; p <0.001, age adjusted). The choice of the method changed with the age of the woman (fig. 3). In particular, no contraception method was correlated with increasing age (p <0.01).
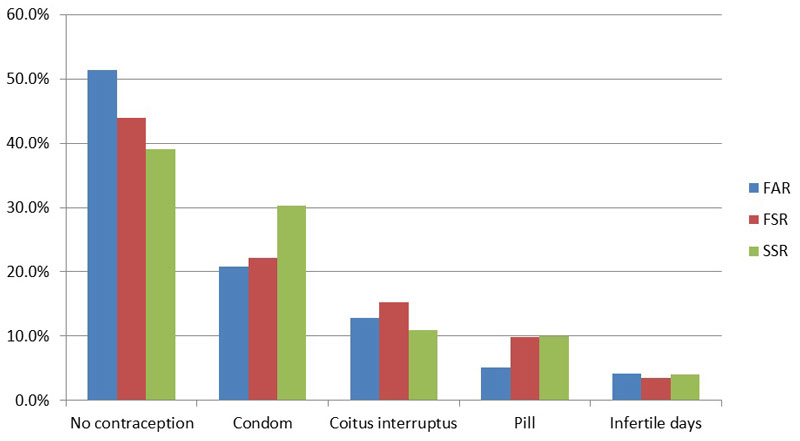
Figure 2 Contraception methods used by women before pre-VTP counselling according to nationality and residence group. FAR = foreign women resident abroad; FSR = foreign women resident in Switzerland; SSR = Swiss women resident in Switzerland; VTP = voluntary termination of pregnancy
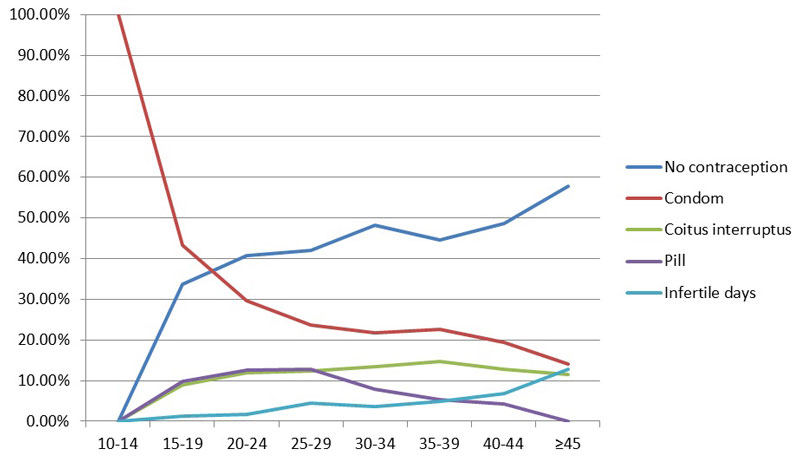
Figure 3 Percentage distribution of pre-VTP contraception method according to the woman’s age by woman’s age at termination according to nationality and residence groups. VTP = voluntary termination of pregnancy
In our study, only the 6.2% of the pregnant women did not request counselling before the VTP. The majority of the pregnant women visited an FPC (68%; table 6). FARs preferred counselling by a doctor more often than SSRs (OR 9.022, 95% CI 47.233–11.253; p <0.001, age adjusted).
Table 6 Women deciding to continue the pregnancy after pre-VTP counselling at the FPC.
| 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Pregnant women in consultation (n) | 459 | 429 | 363 | 408 | 354 | 387 | 330 | 333 | 3063 |
| Pre-VTP counselling at the FPC (n) | 1938 | 1907 | 1783 | 1817 | 1524 | 1653 | 1551 | 1488 | 13661 |
| Decisions to continue the pregnancy (n) | 47 | 68 | 33 | 42 | 48 | 40 | 46 | 45 | 369 |
| Women deciding to continue the pregnancy after pre-VTP counselling (%) | 10.2 | 15.8 | 9.1 | 10.3 | 13.5 | 10.3 | 13.9 | 13.5 | 12 |
FPC = family planning centre; VTP = voluntary termination of pregnancy
During the observation period, in all four FPCs 13,661 pre-VTPs counselling sessions took place and 12% of the pregnant women decided to continue the pregnancy (table 6).
In this study, we focused on 4492 VTPs performed between 2008 and 2015 in Ticino. Around half of these were in SSR women, a quarter in FSR and a quarter in FAR.
With 6.8 abortions per 1000 women between 15 and 44 years of age (2015), Switzerland has one of the lowest abortion rates worldwide; the global rate was estimated to be 35 abortions per 1000 women aged 15–44 per year in 2010–2014 [4, 5]. Abortion rates have declined significantly since 1990 in the developed world but not in the developing world, so the worldwide rate is still high [5].
On national level, the number of VTPs was constant (10,924 in 2008, 10,255 in 2015) [3]. The relatively high VTP rate in Ticino (8.9 per 1000 women between 15-44 years of age) results from the high number of women resident in Italy (24.2%) who come to Ticino for the intervention. In fact, the VTP rate for resident women (73.6%) is close to the national value (6.5 per 1000 women between 15 and 44 years of age).
Since 2012, in Ticino the number has progressively decreased by41% (from 682 in 2008 to 405 in 2015), mainly because of the significant reduction in VTPs in women resident in Italy (decrease of 75.7%). This decline in the number of VTPs may be presumed to be related to the changing situation in Italy caused by the availability of the mifepristone pill RU486 (medical VTP method). This received marketing authorisation in July 2009 [6], but the effect became visible a few years later, probably because it was initially difficult for women to find a doctor ready to prescribe it. In fact, conscientious objection by Italian gynaecologists remains a substantial obstacle [7]; about 70% of them use this option and only a few are available to perform VTPs. Another important argument that could lead the Italian women to seek a VTP in Switzerland is the guideline of the Italian Ministry of Health, which recommends a 3-day in-patient stay for medical VTP [8]. The availability of the drug seems now to prevail over the last two points.
In general, the abortion rates are decreasing in many countries [4, 5] and this trend was found in all study groups (FAR, FSR, SSR). For women resident in Switzerland, this diminution could be related to factors such as the access to the “morning after” pill (without prescription), counselling, and sexual education in schools, but other causes are not excluded. The number of minors (<16 years of age) was low at both national level (1% [3]) and cantonal level (Ticino 0.6%) from 2008 to 2015.
The place of intervention and the method used were significantly correlated with the residence of the women. Women resident in Switzerland preferred the combination of hospital (87.2%) and surgical (43.3%) or medical method (56%). In this case, access to the hospital was normally through the FPC. In contrast, FAR women most often had VTP at a private doctor’s office (65.7%) and with the medical method (86.9%). Women living abroad rarely know the FPC pathway and usually contact private doctors following personal recommendations. This disparity in patient information could partially explain the difference observed. Additionally, in Switzerland the costs of a VTP show wide variation, between 400 and 3500 CHF, depending on the method used [9]. The relatively low cost (average 620 CHF [9]) of a medical VTP in a doctor’s office could influence the choice of place of intervention by women from abroad.
The great majority (97.3%) of the VTPs were performed before the end of the 12th week of gestation. In the feedback form filled in by the doctor, the reasons for the procedure are not collected: this information is required only from the 13th week. In this case, fetal reasons such as malformations are predominant (75.4%), followed by maternal psychosocial problems (18%).
A quarter of women who required an abortion had had at least one previous abortion. Multiple VTPs seems to be reduced by social factors such as living with a partner and child(ren) or living with parents/family, which are protective factors. In our analysis, the use of the pill did not seem to prevent multiple VTPs. This could reflect a social acceptability bias in women's answers to the official questionnaire, which asks about the pre-VTP contraception, when they request a VTP.
In Switzerland, the pre-VTP counselling is voluntary and the women can choose between the FPC and private doctors’ offices. The place of counselling was correlated with nationality: FSR and FAR women preferred to visit a doctor. In our analysis, only the 6.2% of the women did not require professional support. The women’s point of view about the utility of the pre-VTP counselling has been evaluated in other countries with controversial results. In Flanders (Belgium), women highly appreciated the counselling session [10]. In contrast, a recent study in the UK shows that the 85% of the pregnant women did not use counselling, arguing that they were already certain of their decision [11]. In Ticino, this service, which is supported politically, seems to be very much appreciated and frequently women ask for more than one consultation. The multidimensional pre-VTP counselling at the FPC in Switzerland is part of national VTP prevention, giving support and help with decision making, and suggesting alternatives to VTP. In the UK, politicians consider the counselling a waste of resources and contrary to women’s wishes [11]. Most women have already made the decision to have an abortion before they approach a general practitioner or family planning clinic [12]. We suppose that the FPC counselling by sexual health specialists can cover different aspects such as ethical, psychological, social, legal or financial problems.
The place of counselling is strongly related to the place of the intervention. In fact, those who decide to have a hospital abortion will have access to an FCP, whereas those (mostly FSR and FAR) who choose an intervention at a private doctor’s office will have the pre-VTP counselling at the same place.
We observed an encouraging trend in changing the decision after pre-VTP counselling at the FPC, where 12% of the pregnant women decided to continue the pregnancy. The repeated visits to the FPC have an impact on the women’s decision-making process. We have no data about counselling at private doctors’ offices. This limitation did not allow a comparison between the two approaches.
During the study period, pre-VTP lack of contraception involved 43.8% of the women. A retrospective study (1995) in Ticino reported a similar pre-VTP lack of contraception of 44% [13]. This value has remained stable over the years. The most widely used method is the condom and in third place we find the contraceptive pill. In the earlier study, the condom was also in first place [13]. The woman’s origin is significantly related to the absence of contraception (FAR and FSR versus SSR). The first place of the condom in the young age group is replaced by absence of contraception with increasing age. We have no information about the contraception method used after a VTP.
Our study has evident limitations related to its retrospective nature and the use of database datasets. Nevertheless, we could illustrate how availability of certain drugs and methods in two border countries can influence the cross-border flow of patients. We could observe the effect not only for VTP, but also for the reproductive medicine sector in Ticino, where about 80% of the treated couples were resident abroad, principally in Italy (data not shown) until the legal situation changed in Italy in 2014 [14]. The regional health authorities of border regions have to respect the rights of patients coming from different countries with different legal frameworks. A possible solution to facilitate international harmonisation, collaboration and data exchange are international conventions such as the European Union Directive 2011/24/EU on the application of patients’ rights in cross-border healthcare. Switzerland, not being member of the EU but having four different border regions, should participate in this convention.
In conclusion, the decrease in number of VTPs in Ticino seems to follow an encouraging trend, in common with other countries, but was mainly influenced by the diminution of the cross-border flow of patients from Italy. The high number of consultations at FCPs shows the good acceptability of these centres, which have a low but extremely important impact on some births. Further efforts have to be made to better inform foreign women about the counselling available at the FCPs.
We thank Mirta Zurini for data concerning the activity of the Family Planning Centres and Mario Lazzaro for critical comments.
The authors alone are responsible for the content of the writing of the paper. No financial support and no other potential conflict of interest relevant to this article was reported.
1 Boland R , Katzive L . Developments in laws on induced abortion: 1998-2007. Int Fam Plan Perspect. 2008;34(3):110–20. doi:.https://doi.org/10.1363/3411008
2Ufficio di statistica: https://www4.ti.ch/dfe/dr/ustat/ufficio/
3Swiss federal office for statistics: https://www.bfs.admin.ch/bfs/en/home.html
4 Sedgh G , Henshaw SK , Singh S , Bankole A , Drescher J . Legal abortion worldwide: incidence and recent trends. Int Fam Plan Perspect. 2007;33(3):106–16. doi:.https://doi.org/10.1363/3310607
5 Sedgh G , Bearak J , Singh S , Bankole A , Popinchalk A , Ganatra B , et al. Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends. Lancet. 2016;388(10041):258–67. doi:.https://doi.org/10.1016/S0140-6736(16)30380-4
6 Day M . Medical abortion becomes available in Italy. BMJ. 2010;340(apr12 2):c2001. doi:.https://doi.org/10.1136/bmj.c2001
7 Minerva F . Conscientious objection in Italy. J Med Ethics. 2015;41(2):170–3. doi:.https://doi.org/10.1136/medethics-2013-101656
8 Di Carlo C , Savoia F , Ferrara C , Sglavo G , Tommaselli GA , Giampaolino P , et al. “In patient” medical abortion versus surgical abortion: patient’s satisfaction. Gynecol Endocrinol. 2016;32(8):650–4. doi:.https://doi.org/10.3109/09513590.2016.1149162
9 Perrin E , Berthoud M , Pott M , Toledo Vera AG , Perrenoud D , Bianchi-Demicheli F . Clinical course in women undergoing termination of pregnancy within the legal time limit in French-speaking Switzerland. Swiss Med Wkly. 2011;141:w13282. doi:.https://doi.org/10.4414/smw.2011.13282
10 Vandamme J , Wyverkens E , Buysse A , Vrancken C , Brondeel R . Pre-abortion counselling from women’s point of view. Eur J Contracept Reprod Health Care. 2013;18(4):309–18. doi:.https://doi.org/10.3109/13625187.2013.796586
11 Baron C , Cameron S , Johnstone A . Do women seeking termination of pregnancy need pre-abortion counselling? J Fam Plann Reprod Health Care. 2015;41(3):181–5. doi:.https://doi.org/10.1136/jfprhc-2014-101161
12 Brown S . Is counselling necessary? Making the decision to have an abortion. A qualitative interview study. Eur J Contracept Reprod Health Care. 2013;18(1):44–8. doi:.https://doi.org/10.3109/13625187.2012.750290
13 Bianchi-Demicheli F , Perrin E , Lüdicke F , Campana A . Contraception and sexuality after termination of pregnancy: a comparison between Lugano and Geneva. Swiss Med Wkly. 2001;131(35-36):515–20. doi:.https://doi.org/10.4414/smw.2001.09768
14Cerutti B, Lazzaro M. Cassis I. Consequences of the Italian laws on reproductive health and abortion on the neighborhood swiss jealth care system. Poster presentation at the 134th APHA (American Public Health Association) Meeting, Boston, 2006. Available at: https://apha.confex.com/apha/responses/134am/7312.pdf
The authors alone are responsible for the content of the writing of the paper. No financial support and no other potential conflict of interest relevant to this article was reported.