
Figure 1 Types of agents reported by the different parties who contacted Tox Info Suisse on agent intake during pregnancy (n = 2871)
DOI: https://doi.org/10.4414/smw.2018.14620
Pregnancy is an exceptional period in a woman’s life and brings numerous physiological, psychological and social changes for the future mother. The sudden responsibility for the unborn child’s health can cause uncertainty, especially concerning potentially detrimental and possibly preventable factors such as exposure to harmful agents [1]. The still sparse knowledge about exogenous influences on the health of a pregnant woman and on the development of her unborn child can cause insecurity among health professionals [2], employers of pregnant women and even manufacturers of products that might be used by pregnant women.
As early as 1909, Féré had the idea that external influences could have an impact on the child’s intrauterine maturation and was one of the first investigators to start experimenting with various chemicals applied to chicken embryos to produce abnormalities [3]. Since the thalidomide scandal of 1961/62, both the research community and the general public have become keenly aware that medications can be dangerous for a child’s intrauterine development. However, it remains a challenge to ensure the safety of unborn children, mainly because prospective clinical trials can be performed on pregnant women only in exceptional cases. In this context, retrospective studies on cases of accidental and suicidal poisonings with medications, and on outcomes after immediate treatment of acute intoxications can provide important information concerning teratogenicity and abortion induction [4–9]. Finally, how physicians and pregnant women perceive the teratogenic risk of several medications has been investigated [10, 11]. These studies focused on the use of medications during pregnancy, whereas pregnant women are exposed to many other potentially harmful agents daily, such as food products and household chemicals.
The present work provides an overview of exposures to all potentially harmful agents of pregnant women in Switzerland, as documented by Tox Info Suisse. This organisation provides poisons information in Switzerland both for members of the general public and for healthcare professionals. In addition to this service, Tox Info Suisse contributes to clinical and evidence-based knowledge about intoxications through systematic documentation of cases, treatment instructions and outcomes.
The data were generated from the database of Tox Info Suisse and handed over to the authors with patient identities encrypted (approval by the ethics committee of the canton of Zurich, BASEC-Nr PB 2016-00472).
Tox Info Suisse is a financially independent foundation, established in 1966 and associated with the University of Zurich since 2011. Its principal responsibility is operating a free 24-hour helpline (telephone number 145), which covers all Switzerland, for all questions concerning poisoning. The information is provided by physicians, veterinarians, pharmacists and nurses trained in clinical toxicology. The service is provided in three of the four official languages in Switzerland (German, French, Italian), as well as in English, and covers a population of about 8.5 million people. In the electronic in-house database, demographic information, agents involved in exposures, circumstances of exposure, route of application, and any specific measures advised are recorded in a systematic and standardised manner. Further information such as questions posed by the calling party, symptoms described and specific measures recommended by Tox Info Suisse are noted in free-text fields. In cases of calls from health professionals, Tox Info Suisse asks for follow-up reports on the clinical course of the exposure. This supplementary information includes the systematic assessment of the overall severity of the exposure and the causal correlation between symptoms and exposure as evaluated by the trained staff of Tox Info Suisse. Furthermore, as in the primary calls, information on symptoms, clinical course, decontamination measures, and both specific and symptomatic therapies is noted, both in a standardised way and in free-text fields.
Appropriate cases were identified from among those archived between 1995 and 2015 in the Tox Info Suisse in-house database. The inclusion criterion was “exposure during pregnancy”, and all calls addressing effects on the mother and/or on the child were considered. It should be noted that “agent exposure” is not synonymous with “intoxication”. The latter is defined as an agent exposure that causes symptoms, whereas agent exposure per se does not necessarily cause symptoms.
Since the criterion “exposure during pregnancy” was not systematically recorded, the free-text field for the patient’s medical history was screened for expressions synonymous with or related to pregnancy in the English, German, French and Italian languages. These included conception, gestation, gravidity, pregnant, pregnancy, Gravida (Ger.: pregnant woman), schwanger (Ger.: pregnant), SSW (Ger. abbr.: week of pregnancy), SSM (Ger. abbr.: month of pregnancy), enceinte (Fr.: pregnant), gravidité (Fr.: pregnancy), grossesse (Fr.: pregnancy), gravidanza (It.: pregnancy) and incinta (It.: pregnant). The cases identified were extracted from the database and reviewed one by one to eliminate those mentioning the search terms in contexts other than pregnancy at the time of agent exposure (e.g., “since her pregnancy, two years ago, the patient…”).
For the evaluation of follow-up reports by health professionals, only exposures where the association between women’s symptoms and the agent was considered proven or likely or no symptoms occurred at all were included in the analysis. For sake of clarity, exposures with agents involved in four or fewer cases are not shown.
The queries made by the caller were assigned to one of eleven predefined question categories. The symptoms were allocated to either the mother or the child, assessed for severity based on the Poisoning Severity Score first presented by Persson et al. [12], and assigned to the organ or functional system afflicted. Since the description of complaints was not always precise enough to assign them to one symptom or its associated system, certain symptoms were combined into larger symptom-groups (for example: irritation of pharynx/larynx/trachea). Finally, headache was assigned to the organ system “neurological”, stomach ache to “gastrointestinal” and “irritation of pharynx/larynx/trachea” to otorhinolaryngeal, although strictly speaking they do not afflict only one single system.
The correlation between the patient’s account, the agent involved and symptoms was evaluated by the specialised staff of Tox Info Suisse with the support of their internal database, books, publications, specialist literature, swissmedicinfo.ch and material safety data sheets. A correlation was defined as adequate if at least one symptom fitted the possible clinical manifestation of the agent involved.
In addition to the systematically recorded parameters, information in the free text fields was translated into new phrased parameters. These included additional symptoms – assigned to the corresponding organ system or functional system – the decontamination measures, and specific and symptomatic therapy.
All parameters were analysed with descriptive statistics using the statistics program “SPSS” Version 22.0. Unless otherwise mentioned, data are shown as number (n) and as percentage (%).
A total of 2871 cases of exposure during pregnancy were identified. The majority of the calls were made by members of the general public (2035/2871, 70.9%), followed by physicians (733/2871, 25.5%) and in 103 cases (out of 2871, 3.6%), Tox Info Suisse was contacted by other parties (pharmacists, veterinarians, toxicological centres, other organisations, unknown callers; fig.1). Among the calls made by members of the general public, most were made by the affected women themselves (1562/2035, 76.8%), but in some cases their partners, parents, relatives, friends and others phoned.

Figure 1 Types of agents reported by the different parties who contacted Tox Info Suisse on agent intake during pregnancy (n = 2871)
The latency between exposure and time of phone call was documented in 1806 cases and was usually 24 hours or less (1576/1806, 87.3%). In a few cases, it was less than 1 hour (298/1806, 16.5%). In 230 cases (out of 1806, 12.7%), more than a day had passed by the time Tox Info Suisse was contacted. In cases where the stage of pregnancy at the time of the call was noted (1962), only 46 calls (2.3%) were made postpartum (fig. 1); all others (1916/1962, 97.7%) were made during pregnancy. The number of calls decreased slightly from the first to the third trimester (731, 637 and 548, respectively). This decrease was due to declining queries from physicians (265, 173 and 124, respectively).
The majority of agent exposures (2297/2871, 80.0%) occurred accidentally: 1854 at home, 232 at work, 33 outdoors and 178 in another place. Less frequently, exposures were intentional (471/2871, 16.4%). In 103 cases, the circumstances were adverse drug reactions, iatrogenic applications or not further specified (fig. 2). Accidental exposures mostly happened at home (1854/2297, 80.7%) or at work (232/2297, 10.1%). Intentional exposures were in more than half of all cases with suicidal intentions (254/471, 53.9%); otherwise they had an abusive (41), criminal (3) or other (173) character. Physicians called more often because of intentional intoxications (331/733, 45.2%) than did members of the general public (115/2035, 5.7%). The frequency of accidental exposures where the trimester at the time of the call was known (1490) remained approximately constant throughout all trimesters (511, 513 and 466, respectively). Of the intentional exposures with trimester information at the time of the call, the number and the number of exposures with suicidal intentions (in total 359 and 215, respectively) decreased from the first to the third trimester (180 and 97, 105 and 76, 74 and 42).
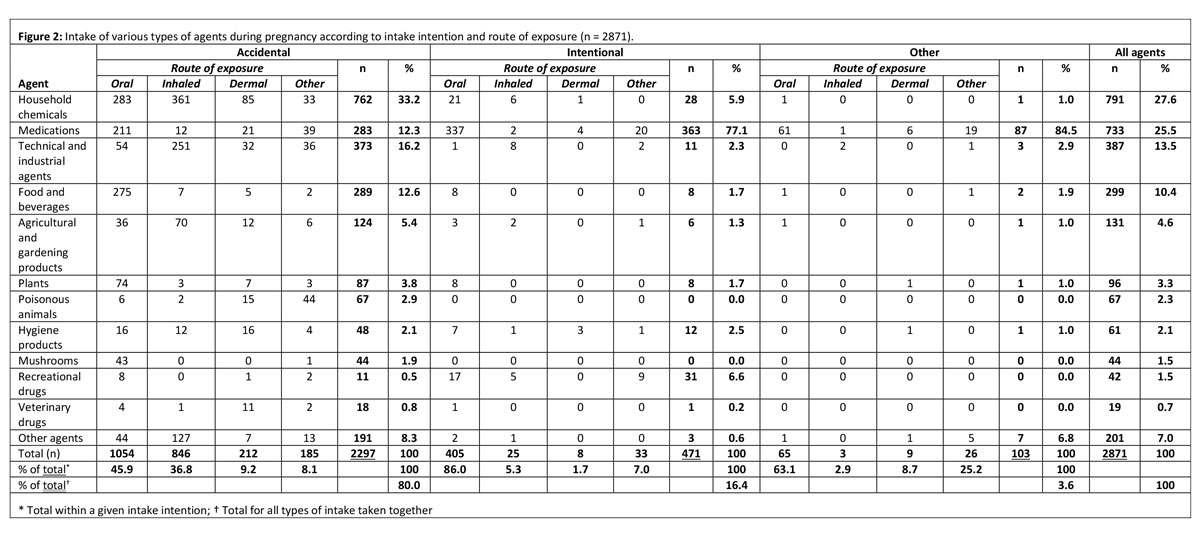
Figure 2 Intake of various types of agents during pregnancy according to intake intention and route of exposure (n = 2871).
Figure 2 shows that the main route of exposure was oral (1524/2871, 53.1%), followed by inhalation (874/2871, 30.4%), dermal (229/2871, 8.0%) and by other routes of exposure (244/2871, 8.5%), including animal bite/sting, intravenous, intramuscular, subcutaneous, paravenous, sublingual, ocular, nasal, rectal, vaginal and transplacental). For intentional exposures, oral intake was by far the most prevalent route (405/471, 86.0%), whereas for accidental exposures, the oral route was closely followed by inhalation (1054/2297, 45.9%; 846/2297, 36.8%). From the 846 accidental inhalations, 603 occurred at home and 179 in an occupational setting (71.3% and 21.2%, respectively).
Leading to approximately one third of all calls, household products were the frontrunner among agents involved (791/2871, 27.6%), closely followed by medications (733/2871, 25.5%). Ranking third and fourth were technical and industrial agents (387/2871, 13.5%) and food and beverages (299/2871, 10.4%), followed by agricultural and gardening products, plants, poisonous animals, hygiene products, mushrooms, recreational drugs, veterinary drugs and other agents (shown in figs 1 and 2 ). When the medication subclass was analysed according to the Anatomic Therapeutic Chemical (ATC) classification system [13], two main groups were identified: remedies for the nervous system (265/733, 36.2%) and the genitourinary system (74/733, 10.1%).
Members of the general public contacted Tox Info Suisse most frequently owing to exposure to household chemicals (675/2035, 33.2%), followed by food and beverages (281/2035, 13.8%), technical and industrial agents (278/2035, 13.7%), and medications (274/2035, 13.5%). Physicians called most often to check medications (415/733, 56.6%), household products (100/733, 13.6%), and technical and industrial agents (88/733, 12.0%). The prevalence of the two most frequent agent groups changed according to the trimester of pregnancy when the call took place: during the first trimester, calls about exposures to medications were more numerous than calls about household products (273/731, 37.3% vs 153/731, 20.9%), whereas this changed in the second (154/637, 24.2% vs 165/637, 25.9%) and the third trimesters (112/548, 20.4% v. 163/548, 29.7%).
The agents involved in accidental exposures were more heterogeneous than those in intentional exposures (fig. 2). Household products represented a third of all accidental exposures (762/2297, 33.2%), followed by technical and industrial agents (373/2297, 16.2%), and medications (283/2297, 12.3%). In contrast, three quarters of intentional exposures involved medications (363/471, 77.1%). Of the two most frequently mentioned types of agents, household products were most often inhaled (367/791, 46.4%; 35 thereof in an accidental occupational setting), whereas medications were mostly taken orally (609/733, 83.1%).
A total of 3507 questions were asked (fig. 3). The question posed most frequently was whether the situation was dangerous in general (1377/3507, 39.3%), followed by the question whether the situation was dangerous specifically for the unborn child (904/3507, 25.8%) and what measures should be taken (582/3507, 16.6%). Only a small number of queries were about specific danger to the mother (82/3507, 2.3%). Questions about abortion were very rare and comparable in intentional and in accidental exposures (total 13/3507, 0.4%; 6 vs 4, respectively).
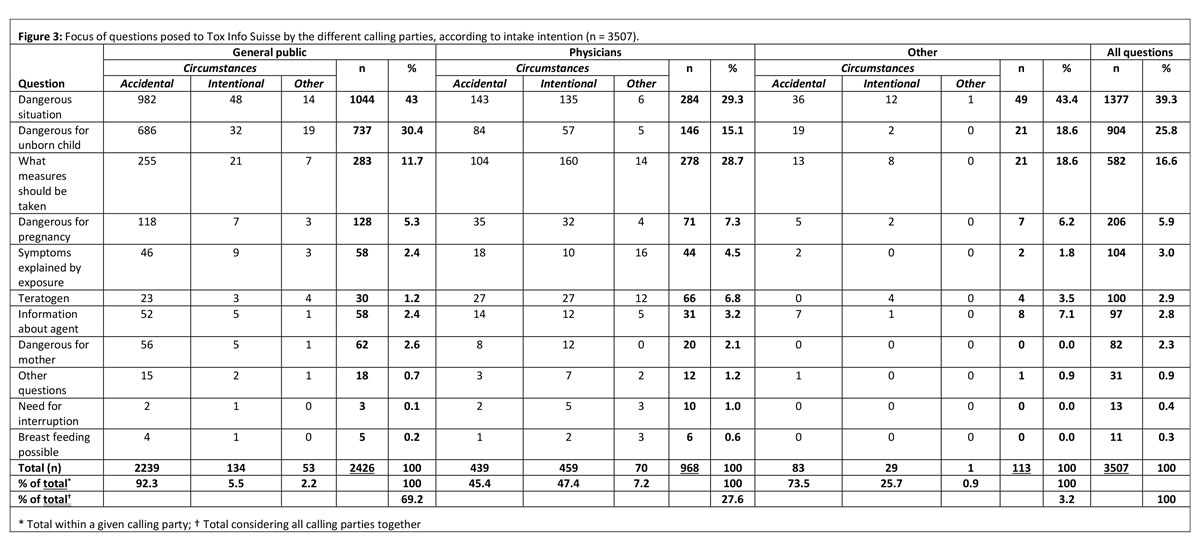
Figure 3 Focus of questions posed to Tox Info Suisse by the different calling parties, according to intake intention (n = 3507).
Within the calling parties “general public” and “physicians”, the question posed most frequently was how dangerous the situation was (1044/2426, 43.0% of all questions from the general public, and 284/968, 29.3% of all physician-posed questions). In contrast, the second most frequently posed question differed: members of the general public asked 737 times if the situation was dangerous for the unborn child (737/2426, 30.4%), whereas physicians asked 278 times what measures should be taken (278/968, 28.7%).
During the different trimesters, the ranking of the questions remained similar to that for the overall total, except that the questions concerning teratogenicity were remarkably more frequent in the first trimester than in the second or third, or postpartum (50, 20, 6 and 4, respectively). The question about teratogenicity was most often posed by physicians (66/100, 66%).
After both accidental and intentional exposures, the question about the danger of the situation was the one posed most frequently (1161/2761, 42.0% of all questions asked after an accident and 195/622, 31.4% of all questions asked after intentional exposure). However, the second most frequently posed question differed: after an accident, the callers were more concerned about the danger to the unborn child (789/2761, 28.6%) and after an intentional exposure more often about what measures should be taken (189/622, 30.4%).
Among all 2871 calls, 905 (31.5%) cases with symptoms and 684 (23.8%) without symptoms were recorded. No documentation on symptoms was available for the remaining 1282 calls (44.7% of the total). In 742 of the 905 cases with documented symptoms (742/905, 82.0%), the correlation between the symptoms and the known effects of the agent was evaluated as likely.
As shown in figure 4, a total of 1268 symptoms were recorded. The four organ systems affected the most were the gastrointestinal with 423 symptoms (33.4%), the neurological with 264 symptoms (20.8%), the otorhinolaryngeal with 165 symptoms (13.0%) and the dermatological system with 139 symptoms (11.0%). Furthermore, symptoms related to the respiratory (89), ophthalmological (60), cardiovascular (31), hepatic (7), metabolic (4), muscular (3), urological (2) and blood (1) systems, as well as 55 symptoms not assignable to an organ system, were recorded. Gynaecological-obstetric problems were seldom reported, and comprised 6 cases of vaginal bleed, 5 cases of uterine contractions, 2 cases of threatened abortion and 12 abortions (note that threatened abortions are listed in figure 4 as pregnant women’s symptoms, classified as severe).
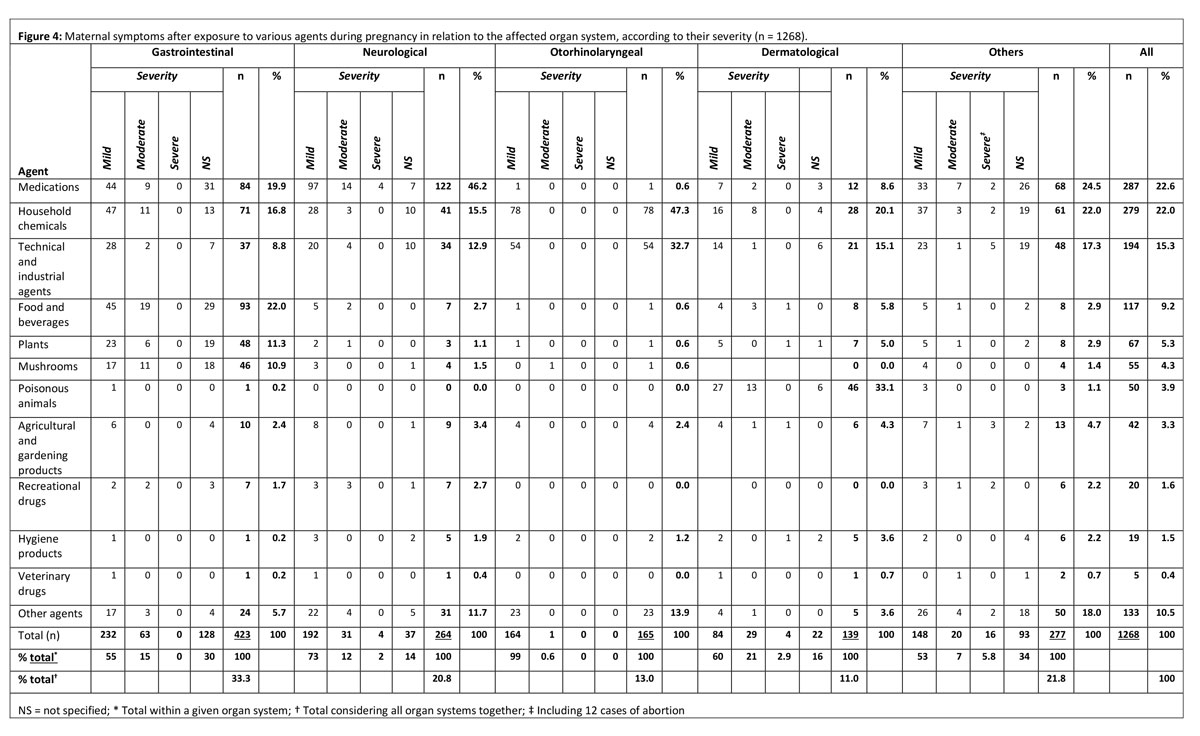
Figure 4 Maternal symptoms after exposure to various agents during pregnancy in relation to the affected organ system, according to their severity (n = 1268).
Around 800 symptoms were classified as mild (820/1268, 64.7%), 144 as moderate (144/1268, 11.4%), 24 as severe (24/1268, 1.9%; including 12 abortions) and further 280 symptoms could not be specified concerning severity (280/1268, 22.1%) (fig. 4). In all organ systems except gynaecological-obstetric (0 mild, 0 moderate, 2 severe, 11 not further specified, 12 abortions) and muscular systems (only 2 moderate), the predominant symptom severity was mild, followed by moderate. Severe symptoms occurred only in the neurological, dermatological and in the gynaecological-obstetric systems (in fig. 4 mentioned under “others”).
In 19 children, unborn or postpartum, a total of 28 symptoms and two premature deliveries were recorded (data not shown). The symptoms recorded in the children were mild in 5, moderate in 7, severe in 5 and not further specified in 11 cases. The symptoms were: decreased intrauterine movement and malformation (4 of each), respiratory insufficiency (3), mild somnolence, bradycardia and no appetite (2 of each), cramps, reduced tone, symptoms of withdrawal, tachypnoea, metabolic acidosis, aspiration, hypothermia, thrombopenia, ascites, hepatosplenomegaly and hearing loss (all 1 each).
Among the various types of agents to which the women were exposed, medications were most often associated with the occurrence of symptoms (fig. 4). In 733 cases where medications were involved, 205 (205/733, 28%) patients developed symptoms. The sum of all symptoms was 287, of which 182 were mild, 32 moderate, 4 severe and 67 not further specified; moreover, 2 abortions were detected. Three out of the four severe symptoms were caused by medications for the central nervous system and one by a medication for the respiratory system. Of the two abortions, one was associated with hormonal medication and the other with an intake of a dietary supplement.
After medications, household chemicals caused the most frequent occurrence of symptoms (195/791, 24.7% symptomatic exposures in all cases exposed to household products). As shown in figure 4, these exposures led to 279 symptoms, of which the majority was mild (206), followed by moderate (25), severe (2, including an abortion) and not further specified (46).
In 374/2871 (13.0%) of all cases, some measures had already been taken before Tox Info Suisse was contacted. Among these cases, a total of 385 measures were taken, of which the two most popular actions were exposure interruption (e.g., airing the room, stopping application of the agent), which was carried out 150 times, and active decontamination measures (rinsing of eyes, cleaning of skin, etc.), carried out 144 times.
In 1867/2871 (65%), a total of 2331 measures were recommended. These measures were divided into two groups: immediate measures, which had to be taken unconditionally, and conditional measures, the execution of which was linked to a certain condition in clinical development or diagnostic result. The top two of the immediate measures (total 1961) were exposure interruption (412) and forwarding to another institution (345) mostly to an embryo toxicological centre (88). A considerable proportion of the conditional measures recommended consisted of administration of medication (119/370).
Two hundred and seventy-four of all members of the general public (274/2035, 13.5%) took autonomous measures before contacting Tox Info Suisse. In 1193 cases (1193/2035, 58.6%), Tox Info Suisse recommended further measures. Of these, the three most common immediate measures were exposure interruption (365), non-pharmaceutical decontamination (212) and contacting another institution (109). The physicians took slightly fewer measures (87/733, 11.9%), but more frequently obtained advice for further immediate measures (599/733, 81.7%). These involved contacting another institution in 218 cases, surveillance measures in 164 and medicinal decontamination measures (e.g., activated charcoal) in 10.
The in-house database of Tox Info Suisse included 314 follow-up reports from health professionals; in 265 of these, the symptom’s relationship with the agent in question was considered certain or likely, or no symptoms occurred at all. A variety of agents was involved in these 265 cases. In the present analysis, only exposures with agents involved in at least 5 cases were considered (9 agents; 70 exposures). As shown in figure 5, a total of 137 symptoms were considered to be caused by these agents. In the majority of the cases, medications were involved (56/70, 80.0%). Paracetamol was the agent most often involved (15), followed by mefenamic acid (9) and the household product sodium hypochlorite (9). Mostly, the symptoms were mild (122/137, 89.1%), a few were moderate (10), one was severe and four could not be further specified. Among the various organ systems affected, the nervous system showed the most symptoms (46), followed by the gastrointestinal system (23). In total, 25 decontamination measures were taken, of which the application of a single dose of activated charcoal was the most frequent (10) (fig. 6). Fifteen specific therapies were initiated, of which the administration of N-acetyl cysteine was most frequent (10). A total of 48 different symptomatic therapies were applied (fig. 6).
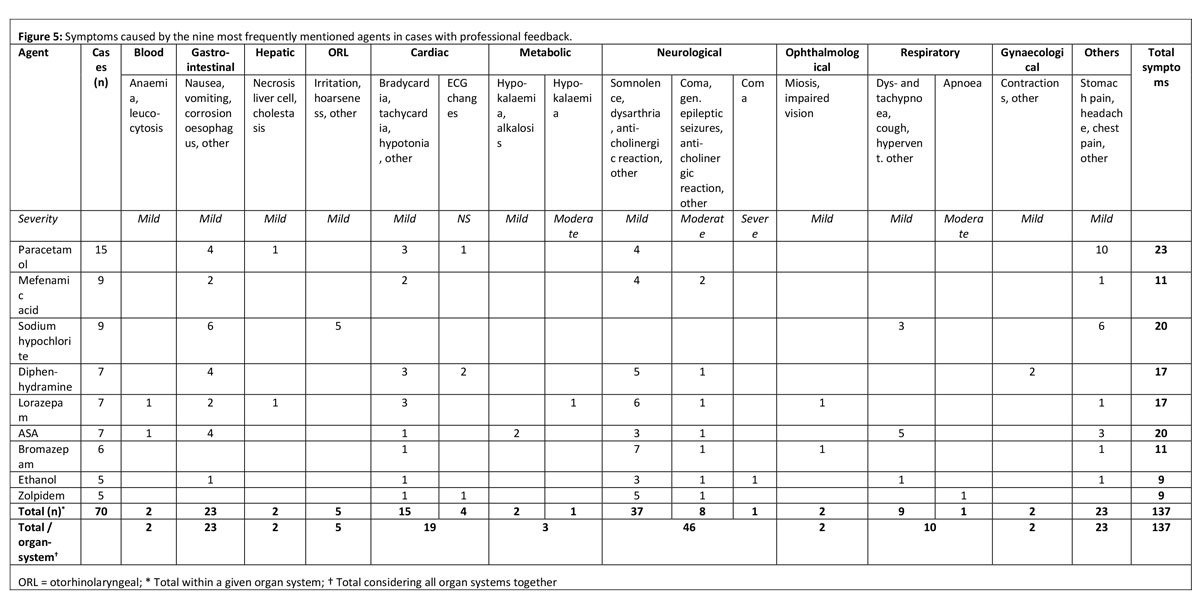
Figure 5 Symptoms caused by the nine most frequently mentioned agents in cases with professional feedback.
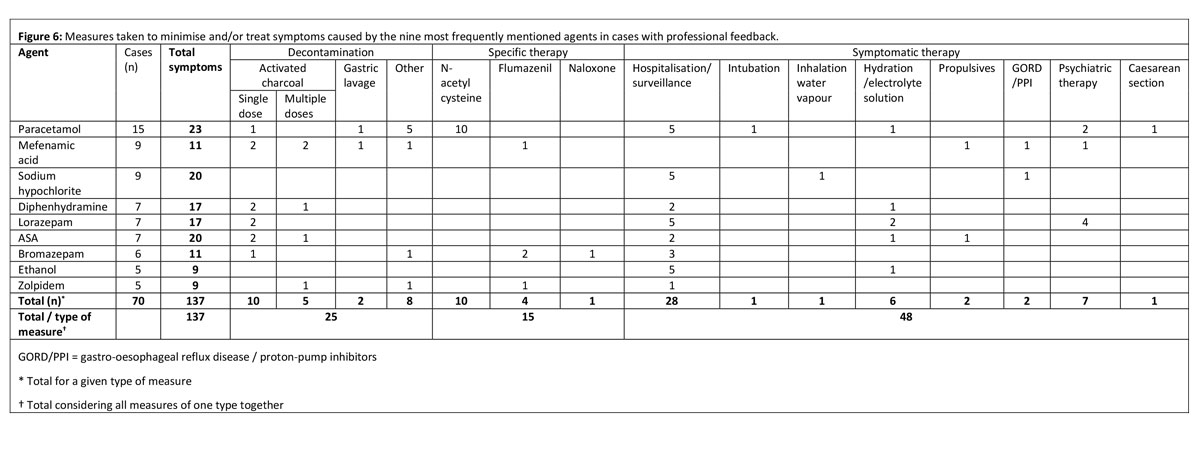
Figure 6 Measures taken to minimise and/or treat symptoms caused by the nine most frequently mentioned agents in cases with professional feedback.
Between 1995 and 2015, Tox Info Suisse recorded an annual average of 137 calls due to agent exposure during pregnancy. This suggests that agent exposure during pregnancy is not rare. The strengths of the present study are the high number of calls analysed and the access to data that are otherwise not available. Still, and for various reasons (lack of looking for help, contacting other institutions, language limitations, etc.) the documented exposures are likely to represent only part of all exposures taking place in Switzerland. A further limitation of the present study is that the database was not specifically designed to answer the questions addressed. Moreover, the purpose of Tox Info Suisse implies a high heterogeneity of cases and limits data clustering. In the case of calls by members of the general public, some medical and technical information might not be complete. Finally, the information on most recorded cases reflects a brief time period.
The great majority of calls were made by members of the general public, implying that uncertainty about how to handle such situations is widespread in the population. These uncertainties mostly concerned exposures to agents such as household products, technical and industrial agents, and food and beverages. One quarter of all calls were made by physicians, showing that even for health professionals this issue remains challenging [14]. They were most frequently concerned with exposures to medications, and such exposures were most often associated with symptomatic cases. Besides wanting to know how dangerous the situation was, physicians also wanted to find out what measures should be taken to protect both mother and unborn child in such unfamiliar and particularly challenging circumstances.
Awareness of agent teratogenicity is crucial [15] and the malformation risk associated with agent exposure during pregnancy is perceived as high in the general population [10]. Accordingly, members of the general public frequently asked about the wellbeing of the unborn child, but teratogenicity was even more often an issue when physicians contacted Tox Info Suisse than when members of the general public did. This is in line with the comparatively high frequency of physicians’ queries in the first trimester. Both observations can be explained by the professionals’ knowledge that the risk of teratogenicity after agent exposure is highest during the first 8 gestational weeks [16]. The fear of long-term damage can also explain why a considerable number of phone calls were made 24 hours after the exposure – or even later – when acute symptoms are usually waning and queries about exposures in non-pregnant persons seldom occur. In contrast to these fears, the number of symptoms that occurred in children were low compared with the number of symptoms developed by the mothers (28 vs 1268 in 2871 primary calls; 0 vs 137 in the 70 follow-up reports from health professionals that were analysed). Four cases of malformation were observed in our primary calls, and none in the follow-up reports from health professionals. The causal correlation of the reported 12 abortions with the substance to which the pregnant women had been exposed was classified as possible in two cases. In one case, a technical/industrial product was involved (glue for foam material); in the other case, a recreational drug (cannabis) could have played a role.
The relatively low number of malformations and abortions seem to suggest that the first concern when confronted with agent exposure during pregnancy should be the mother’s wellbeing. Furthermore, our finding corroborates previous studies in which, after drug overdose, no higher rate of malformations were found [4, 7]. Schaefer et al. stated that the acute treatment of intoxications during pregnancy should not differ from procedures for non-pregnant women [9]. We feel that concern about teratogenicity was almost excessive compared with other possible – rather immediate – dangers through agent exposures, such as direct effects on the mother. The majority of symptoms the mothers experienced after accidental and intentional exposures were mild. Comparable observations were reported by Sein Anand et al., who investigated a case series of self-poisonings, in which the clinical courses were mostly mild or moderate [17].
More than half the intentional exposures occurred with suicidal intent. This finding is consistent with a previous evaluation of hospital admissions of pregnant women due to self-intoxications, which showed that 68.6% were attempted suicides [18]. Earlier work further showed that attempted suicides during pregnancy do not seem to induce a higher prevalence of structural birth defects [4] and completed suicides are seldom caused by medication overdose, especially as compared to deaths by violent acts [19]. We observed that medications in general and, among these, medications for the nervous system were the agents mainly involved in intentional exposures, which again is in line with previous work [20, 21]. The latter reported that the highest incidence of suicidal attempts is within the first trimester, which our data confirm. Generally, pregnancy is a protective factor against suicide [22], but it is known that almost 80% of all suicide attempts during pregnancy are carried out for the first time [17]. Our data clearly show that suicide attempts during pregnancy in Switzerland – especially during early pregnancy – cannot be ignored.
Most available feedback concerned exposure to medications. This correlates with the most frequent reason for the first calls from physicians (medications in 56.6%). Easily accessible analgesic drugs (paracetamol, mefenamic acid, acetylsalicylic acid) showed the highest incidence (31), followed by benzodiazepines and Z-drugs (18; lorazepam, bromazepam, zolpidem), which are available only on prescription. The symptoms caused by these exposures were however mostly mild. In Switzerland, 16.7% of all women use mental-health services during the perinatal period [23], implying that mental issues appear with high frequency in this period and hence such medications are present in a considerable proportion of households. As to be expected from the types of agents involved, the decontamination measure initiated most frequently was the application of activated charcoal, which inhibits gastrointestinal absorption of agents [24], and the specific treatment with N-acetyl cysteine, which is the antidote to paracetamol.
Our results on agent exposure during pregnancy have implications for Tox Info Suisse, for several professional groups and for public health. For Tox Info Suisse, the present work means that special attention should be paid to pregnancy, and that cooperation with institutions dedicated to issues of teratogenicity should be intensified. These institutions include the Swiss Teratogen Information Service (STIS), the Federal Office of Public Health (“Bundesamt für Gesundheit”, BAG), the Swiss Working Group for Perinatal Pharmacology (“Schweizerische Arbeitsgemeinschaft für Perinatale Pharmakologie, SAPP), maternity and gynaecological hospitals and universities.
The prevalence of occupational exposure was considerable, and twice as high as that for other women in the same age range contacting Tox Info Suisse (data not shown). Since exposure can be relevant as early as during the first trimester, protective measures established before pregnancy occurs are likely to be more effective and could contribute to reducing situations of insecurity. Employers, especially those from work domains involving exposure to possibly toxic chemical agents, should invest in information for women of reproductive age. Moreover, since current warning notices about (toxic) household products are not fully effective in preventing unintentional exposures, the manufacturers concerned should re-think their warning texts.
Physicians directly confronted with agent exposure during pregnancy should be aware that most immediate consequences will affect the mother, and only a few the unborn child. Therefore, it is important to prioritise the treatment of symptoms affecting the pregnant woman. At the same time, it appears reasonable to reduce the distress caused by fear of miscarriage and/or teratogenicity. Since stress during pregnancy is per se associated with poor perinatal outcomes, this would contribute to a healthier pregnancy course [25]. Furthermore, physicians and other health professionals involved in antenatal care should be aware that suicide attempts during pregnancy do occur. Since a considerable proportion of the suicide attempts during pregnancy are first time events, an especially careful evaluation of the suicidal status of the pregnant woman is needed. Appropriate counselling of women facing difficult situations during pregnancy, including possible involvement of close social contacts might reduce the rate of attempted suicides.
Pregnancy remains a particularly challenging period in a women’s life. From the public health point of view, multiple efforts should be made to support and reassure pregnant women. Several professional groups and the society in general should be sensitised for this need and motivated to participate in those efforts thereby contributing to improve the future health of both mothers and their offspring.
We are very grateful to Prof. Dr R. Zimmermann for his support to both theses and for interesting discussions. We thank the whole team at Tox Info Suisse for their generous support and inputs, in particular the director, Dr H. Kupferschmidt. We are indebted to the research teams of the Obstetrics Department at the University Hospital of Zurich and of the Ehrbar Lab at the University Hospital of Zurich. Dr H. Murray is gratefully acknowledged for language corrections.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Zaki NM , Albarraq AA . Use, attitudes and knowledge of medications among pregnant women: A Saudi study. Saudi Pharm J. 2014;22(5):419–28. doi:.https://doi.org/10.1016/j.jsps.2013.09.001
2 Rasmussen SA . Human teratogens update 2011: can we ensure safety during pregnancy? Birth Defects Res A Clin Mol Teratol. 2012;94(3):123–8. doi:.https://doi.org/10.1002/bdra.22887
3 Barrow MV . A brief history of teratology to the early 20th century. Teratology. 1971;4(2):119–29. doi:.https://doi.org/10.1002/tera.1420040202
4 Czeizel AE , Tomcsik M , Tímár L . Teratologic evaluation of 178 infants born to mothers who attempted suicide by drugs during pregnancy. Obstet Gynecol. 1997;90(2):195–201. doi:.https://doi.org/10.1016/S0029-7844(97)00216-0
5 Czeizel AE , Gidai J , Petik D , Timmermann G , Puhó EH . Self-poisoning during pregnancy as a model for teratogenic risk estimation of drugs. Toxicol Ind Health. 2008;24(1-2):11–28. doi:.https://doi.org/10.1177/0748233708089020
6 Czeizel A , Szentesi I , Szekeres I , Molnár G , Glauber A , Bucski P . A study of adverse effects on the progeny after intoxication during pregnancy. Arch Toxicol. 1988;62(1):1–7. doi:.https://doi.org/10.1007/BF00316249
7 Gunnarskog J , Källén AJ . Drug intoxication during pregnancy: a study with central registries. Reprod Toxicol. 1993;7(2):117–21. doi:.https://doi.org/10.1016/0890-6238(93)90245-3
8 Flint C , Larsen H , Nielsen GL , Olsen J , Sørensen HT . Pregnancy outcome after suicide attempt by drug use: a Danish population-based study. Acta Obstet Gynecol Scand. 2002;81(6):516–22. doi:.https://doi.org/10.1034/j.1600-0412.2002.810607.x
9 Schaefer C , Hoffmann-Walbeck P . Intoxikationen bei Schwangeren [Poisonings in pregnancy]. Med Klin Intensivmed Notf Med. 2012;107(2):118–22. Article in German.
10 Nordeng H , Ystrøm E , Einarson A . Perception of risk regarding the use of medications and other exposures during pregnancy. Eur J Clin Pharmacol. 2010;66(2):207–14. doi:.https://doi.org/10.1007/s00228-009-0744-2
11 Gils C , Pottegård A , Ennis ZN , Damkier P . Perception of drug teratogenicity among general practitioners and specialists in obstetrics/gynecology: a regional and national questionnaire-based survey. BMC Pregnancy Childbirth. 2016;16(1):226. doi:.https://doi.org/10.1186/s12884-016-1025-6
12 Persson HE , Sjöberg GK , Haines JA , de Garbino JP . Poisoning severity score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998;36(3):205–13. doi:.https://doi.org/10.3109/15563659809028940
13WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index. 2017. Available from https://www.whocc.no/atc_ddd_index/.
14FMH Swiss Medical Association. Grundlagen der Behandlung von Patientinnen und Patienten: 4.1 Behandlungsvertrag zwischen Arzt und Patient. 2017. Available from http://www.fmh.ch/files/pdf11/Patientenbehandlung_D1.pdf.
15 Gils C , Pottegård A , Ennis ZN , Damkier P . Perception of drug teratogenicity among general practitioners and specialists in obstetrics/gynecology: a regional and national questionnaire-based survey. BMC Pregnancy Childbirth. 2016;16(1):226. doi:.https://doi.org/10.1186/s12884-016-1025-6
16Schaefer C, Spielmann H, Vetter K, Weber-Schöndorfer C. Arzneimittel in Schwangerschaft und Stillzeit (8 ed.). München: Urban and Fischer 2012.
17 Sein Anand J , Chodorowski Z , Ciechanowicz R , Klimaszyk D , Lukasik-Głebocka M . Acute suicidal self-poisonings during pregnancy. Przegl Lek. 2005;62(6):434–5.
18 Lester D . The timing of attempted suicide during pregnancy. Acta Paediatr Acad Sci Hung. 1987;28(3-4):259–60.
19 Oates M . Suicide: the leading cause of maternal death. Br J Psychiatry. 2003;183(4):279–81. doi:.https://doi.org/10.1192/bjp.183.4.279
20 Czeizel AE . Attempted suicide and pregnancy. J Inj Violence Res. 2011;3(1):45–54. doi:.https://doi.org/10.5249/jivr.v3i1.77
21 Czeizel AE , Gidai J , Petik D , Timmermann G , Puhó EH . Self-poisoning during pregnancy as a model for teratogenic risk estimation of drugs. Toxicol Ind Health. 2008;24(1-2):11–28. doi:.https://doi.org/10.1177/0748233708089020
22 Marzuk PM , Tardiff K , Leon AC , Hirsch CS , Portera L , Hartwell N , et al. Lower risk of suicide during pregnancy. Am J Psychiatry. 1997;154(1):122–3. doi:.https://doi.org/10.1176/ajp.154.1.122
23 Berger A , Bachmann N , Signorell A , Erdin R , Oelhafen S , Reich O , et al. Perinatal mental disorders in Switzerland: prevalence estimates and use of mental-health services. Swiss Med Wkly. 2017;147:w14417. doi:.https://doi.org/10.4414/smw.2017.14417
24 Levy G . Gastrointestinal clearance of drugs with activated charcoal. N Engl J Med. 1982;307(11):676–8. doi:.https://doi.org/10.1056/NEJM198209093071109
25Lockwood CJ. Pathogenesis of spontaneous preterm birth In S. M. Ramin (Ed.), UpToDate®. In V. A. Barss (Series Ed.). www.uptodate.com. Retrieved from www.uptodate.com. 2014
APSW suggested the project. TV, SL, CRL and APSW designed the present analysis. TV extracted the data on the first calls from the free-text fields of the database (n = 2871) and analysed them. RB extracted the data on the physicians’ follow-up reports from the free-text fields of the database (n = 70) and analysed them. TV wrote the first version of the manuscript. All authors reviewed the manuscript, then read and approved the submitted version. TV’s contribution constitutes her MD thesis; RB’s contribution constitutes her Master’s thesis in medicine; APSW supervised both theses.
No financial support and no other potential conflict of interest relevant to this article was reported.