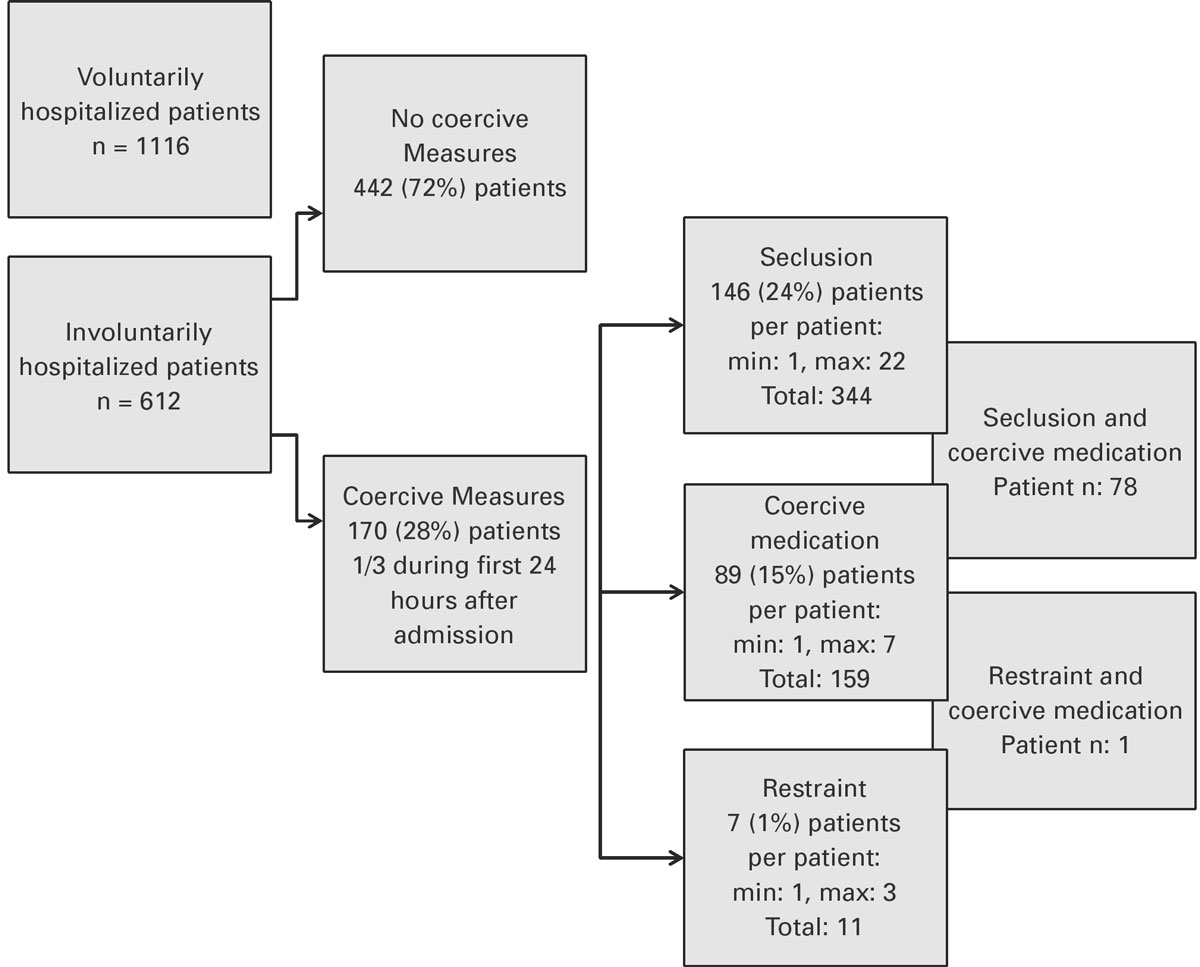
Figure 1 Prevalence of coercive measures at the University Hospital of Psychiatry Zurich.
DOI: https://doi.org/10.4414/smw.2018.14616
Although involuntary commitment and coercive measures are massive invasions of a person’s right to autonomy and self-determination, they are commonly used in psychiatric emergency situations [1, 2]. Because of the possible violation of the patient`s freedom, the use of coercive measures (e.g., involuntary commitment, seclusion, restraint, coercive medication) in psychiatry is regulated on a regional and national level [3, 4]. Although the criteria that have to be met to justify the use of coercive measures (mostly danger to self or others) are clearly defined in theory and comparable between different countries, situations occur that raise questions in patients [5] and in psychiatric staff [6] as to whether alternatives could have been used.
To reduce the prevalence of coercive measures and strengthen the autonomy of patients, most countries in the western world have reformed their legislation in reecent decades [7]. Not only legislative and medical conditions are relevant for the regulation of coercive measures. Cultural aspects such as beliefs, attitudes, and values of both society and mental-health service structures also have an important impact [8–11] on the execution of coercive measures. These different factors, as well as patient characteristics, are hypothesised to play a role in divergent prevalence levels of coercive measures in different countries [4, 11–26]. Supporting the findings that legislation is not the only factor that influences the use of coercive measures, some studies showed that the inconsistency in the use of coercive measures differs not only between countries but also within the same country and sometimes also between wards of a single hospital [12, 27–29].
Furthermore, there appear to be differences in the measures (seclusion, physical restraint, mechanical restraint, coercive medication) that are preferred. In some studies, seclusion was used more frequently [13–17, 19–21, 30], whereas in others mechanical [13] or physical restraint [18, 22, 26, 31] was the intervention of choice. Studies on the frequency of coercive medication are less common and one study revealed that it is mostly combined with other forms of coercion [15]. The characteristics of patients receiving coercive measures are also inconsistent in the literature. Younger [21, 32–34] or older age [26, 35], female [22, 35] but also male gender [32, 34, 36], psychotic disorders [36, 37], personality disorders [15, 32], substance use-related disorders [27], mental retardation [32], a history of former admissions [21, 27, 38], long duration of hospitalisation [15, 21, 34, 39], involuntary commitment [27] and aggressive behaviour prior to admission [40] were described in different studies.
Previous studies revealed high rates of involuntary commitment and coercion in Switzerland [13, 41], but to our knowledge there is no study evaluating the prevalence of coercion and the factors that are associated with its application. Hence, the aim of this study was to gain information about the rates of coercive measures and clinical characteristics in an inpatient population treated at the University Hospital of Psychiatry Zurich, the largest psychiatric hospital in Switzerland. On the basis of previous studies [15, 21, 34, 36–39], we wanted to test the hypothesis that, compared with patients without episodes of coercion during involuntary hospitalisation, those who experience coercion at the University Hospital of Psychiatry Zurich stay longer in the psychiatric hospital, have a history of former involuntary admissions and suffer more often from psychotic illness.
We used an observational study design. Commitment documents and the medical records of a cohort of patients admitted involuntarily to the University Hospital of Psychiatry Zurich during a 6-month period from 1 January to 30 June 2016 were analysed.
Fourteen wards of the Hospital for Adult Psychiatry and two wards of the Hospital for Geriatric Psychiatry of the University Hospital of Psychiatry Zurich, with a total of 252 beds, were included. These 16 wards are located in one hospital, with 6 wards for semi-acute treatment, mostly on a voluntary basis and 10 acute wards, responsible for the majority of patients with an involuntary status. The latter have different specialisations, but strive for a balanced patient distribution to avoid wards with a concentration of coercive measures. The hospital constitutes the largest hospital for adult psychiatry in Switzerland, providing mental-health services for a catchment area of 485,000 inhabitants.
The study was reviewed and approved by the Cantonal Ethics Commission of Zurich, Switzerland (Ref.-No. EK: 2016-00749, decision on 01.09.2016).
No exclusion criteria were defined. We screened a comprehensive cohort of all patients admitted to the University Hospital of Psychiatry Zurich during a six-month period from 1 January to 30 June 2016. Overall, 1728 inpatients were treated during this period. Of these patients, 577 (33%) were involuntarily and 1151 (67%) were voluntarily admitted. For the following analyses related to the occurrence of coercion, we included the 577 (33%) involuntarily admitted patients and 35 (2%) voluntarily admitted patients who were retained because of harm to themselves or others at a later stage during their hospitalisation, which led to a change of their legal status to involuntary hospitalisation. Thus, we conducted statistical analyses with a total of 612 (35%) patients.
In the canton of Zurich, seclusion is defined as being locked in a single room with surveillance through a window with a maximum interval of 15 minutes and, in some cases when danger to self may need immediate response, continuous surveillance through the window.
Patients are strapped to a bed with mechanical devices (belts). At the University Hospital of Psychiatry Zurich, bed belts with 5-point restraints are used. These belts can fix the patient’s arms, legs and torso. If possible less than 5 belts can be used. Restraint is always accompanied by staff during the whole time.
Coercive medication can be used as an acute intervention, orally or as an intramuscular injection. The patient must always be asked whether he or she is willing to take medication orally to avoid injection, which is perceived as more traumatic [42].
Data for this study were based on routine documentation in the patient’s electronic medical files. Those files were used to merge the data, which were collected during one hospitalisation and include documentation of the admission circumstances, prescribed medication, coercive measures and treatment planning. We included patients who were involuntarily hospitalised (as defined above) for detailed analysis. We analysed for the following parameters of the circumstances of admission: reason for admission, referring physician, reason for involuntary commitment, involvement of police during the admission process and at the time of admission. For the clinical course following the admission, we analysed the medical files for the occurrence of coercive measures, prescription of medication, time to day passes, duration of hospitalisation and the diagnosis at discharge. Also, we assessed procedural aspects such the occurrence of abscondence and episodes of re-hospitalisation during the 6-month study period. Furthermore, we analysed the included wards for differences in the usage of coercion.
Analyses were conducted using SPSS 23.0 (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp.) for Windows.
First, we compared sociodemographic data and clinical course of hospitalisation in voluntarily and involuntary hospitalised patients. Second, we conducted a two-group analysis in the involuntarily hospitalised group comparing patients who had undergone at least one coercive measure during hospitalisation with those without coercive measures. For the analysis, we used cross-tabulation with chi-square tests and Bonferroni-adjusted post-hoc tests for categorical variables. Because of the non-normal distribution of interval variables we used Mann-Whitney U-Test and rank regression analyses. The multiple comparisons were family-wise adjusted with the Bonferroni correction to prevent type I error inflation.
Of the 1728 patients who were hospitalised at the University Hospital of Psychiatry Zurich during a 6-month period, 612 were involuntarily hospitalised. These patients differed significantly from the voluntarily hospitalised inpatients in gender, age, occupation, psychiatric diagnosis, severity of symptoms at admission and prescription of medication. Details are shown in table 1.
Table 1 Comparison of voluntarily and involuntarily hospitalised patients.
|
Total
(n = 1728) |
Voluntary
(n = 1116) |
Involuntary
(n = 612) |
χ2 | df | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Gender | 5.39 | 1 | 0.020 | ||||||
| Male | 957 | 55 | 641a | 67 | 316b | 33 | |||
| Age at admission () | 145.33 | 4 | <0.001 | ||||||
| <30 years | 422 | 24 | 299a | 71 | 123b | 29 | |||
| 30–39 years | 374 | 22 | 266a | 71 | 108b | 29 | |||
| 40–49 years | 329 | 19 | 235a | 71 | 94b | 29 | |||
| 50–59 years | 303 | 18 | 213a | 70 | 90b | 30 | |||
| >60 years | 300 | 17 | 103a | 34 | 197b | 66 | |||
| Education | 17.37 | <0.001 | |||||||
| Higher education | 368 | 22 | 244a | 66 | 124a | 34 | |||
| No information | 176 | 10 | 91a | 52 | 85b | 48 | |||
| Occupation | 15.31 | <0.001 | |||||||
| Fully or partially occupied | 398 | 23 | 294a | 75 | 104b | 25 | |||
| Nationality | 0.64 | 0.422 | |||||||
| Swiss | 1187 | 69 | 774 | 65 | 413 | 35 | |||
| Psychiatric diagnosis | 181.20 | 6 | <0.001 | ||||||
| Organic disorder (F0) | 129 | 8 | 25a | 19 | 104b | 81 | |||
| Substance use disorder (F1) | 319 | 19 | 232a | 73 | 87b | 27 | |||
| Psychotic disorder (F2) | 514 | 30 | 287a | 56 | 227b | 44 | |||
| Affective disorder (F3) | 394 | 23 | 306a | 78 | 88b | 22 | |||
| Neurotic disorder (F4) | 233 | 14 | 169a | 73 | 64b | 27 | |||
| Personality disorder (F6) | 104 | 6 | 76a | 60 | 28a | 40 | |||
| Other | 35 | 2 | 21a | 65 | 14a | 35 | |||
| CGI | 109.93 | 3 | <0.001 | ||||||
| 1–2 | 20 | 1 | 12a | 60 | 8a | 40 | |||
| 2–3 | 57 | 3 | 30a | 53 | 27b | 47 | |||
| 4–5 | 1040 | 61 | 783a | 75 | 257b | 25 | |||
| 6–7 | 581 | 34 | 291a | 50 | 290b | 50 | |||
| Antipsychotics | 16.05 | 1 | <0.001 | ||||||
| Yes | 873 | 51 | 524a | 60 | 349b | 40 | |||
| Antidepressant | 38.34 | 1 | <0.001 | ||||||
| Yes | 642 | 37 | 474a | 74 | 168b | 26 | |||
| Benzodiazepines | 5.96 | 1 | 0.015 | ||||||
| Yes | 762 | 44 | 468a | 61 | 294b | 39 | |||
CGI = clinical global impression; df = degrees of freedom Missing values for all variables are less than 1.8%. Identical letters indicate no statistically significant difference by Bonferroni-adjusted chi-square post-hoc tests at p <0.05.
The mean age of the group of involuntarily hospitalised patients was 49 years (range 14–95 years, standard deviation [SD] 21 years). About half of the patients were male (51%, n = 314). Harm to self was the most frequent reason for involuntary commitment (55%) and 70 patients (11%) had attempted suicide prior to admission. Psychiatrists were responsible for most involuntary hospitalisations (40%). The admission process of 187 (30%) patients needed police involvement. Psychotic disorders were most frequently coded as primary diagnosis at discharge. Nearly half of the patients (46%) had a secondary diagnosis at discharge, with a substance use disorder being the most frequent (n = 123) comorbidity. About half of the patients had at least one former voluntary (56%) or involuntary (44%) hospitalisation at the University Hospital of Psychiatry Zurich with some patients having a history of numerous hospitalisations (mean 5, median 1, maximum 69). Abscondence was documented at least once in 105 patients (17% of all involuntarily hospitalised patients) and in 72 (68%) of these episodes the police were informed at least once because patients met the criteria for harm to self or others. Nearly half of those patients (45%) returned on their own. The others were brought back by the police (29%), their next of kin (4%) or discharged in absence (22%).
In 192 (31%) patients, the legal status of involuntary commitment was revoked during the course of hospitalisation, with the patients remaining in the inpatient setting voluntarily; thus, the length of hospitalisation (mean 25, median 17, maximum 245 days) was longer than the duration of involuntary commitment (mean 20, median 13, maximum 230 days). Day passes were issued after a mean duration of 12 days (median 6, maximum 161 days) if the patient’s condition allowed for it (no danger to self and others) and the physician on duty assessed the patient to be sufficiently reliable.
We found the documentation of at least one coercive measure in 28% (n = 170) of the involuntarily hospitalised patients, that is 10% of all patients treated at the University Hospital of Psychiatry Zurich during the study period. Seclusion was the coercive measure most frequently used, followed by coercive medication and then restraint, with the latter being used in only 7 patients (for detailed information see figure 1). Coercive measures, such as barriers to leaving the bed or devices that prevent injury if the patient falls, were specifically used in geriatric psychiatry. These measures were implemented at least once and documented as explicit coercive measures in 15 patients (2%). Nine percent (n = 53) of the involuntarily committed patients were exposed to coercive measures within the first 24 hours after admission.
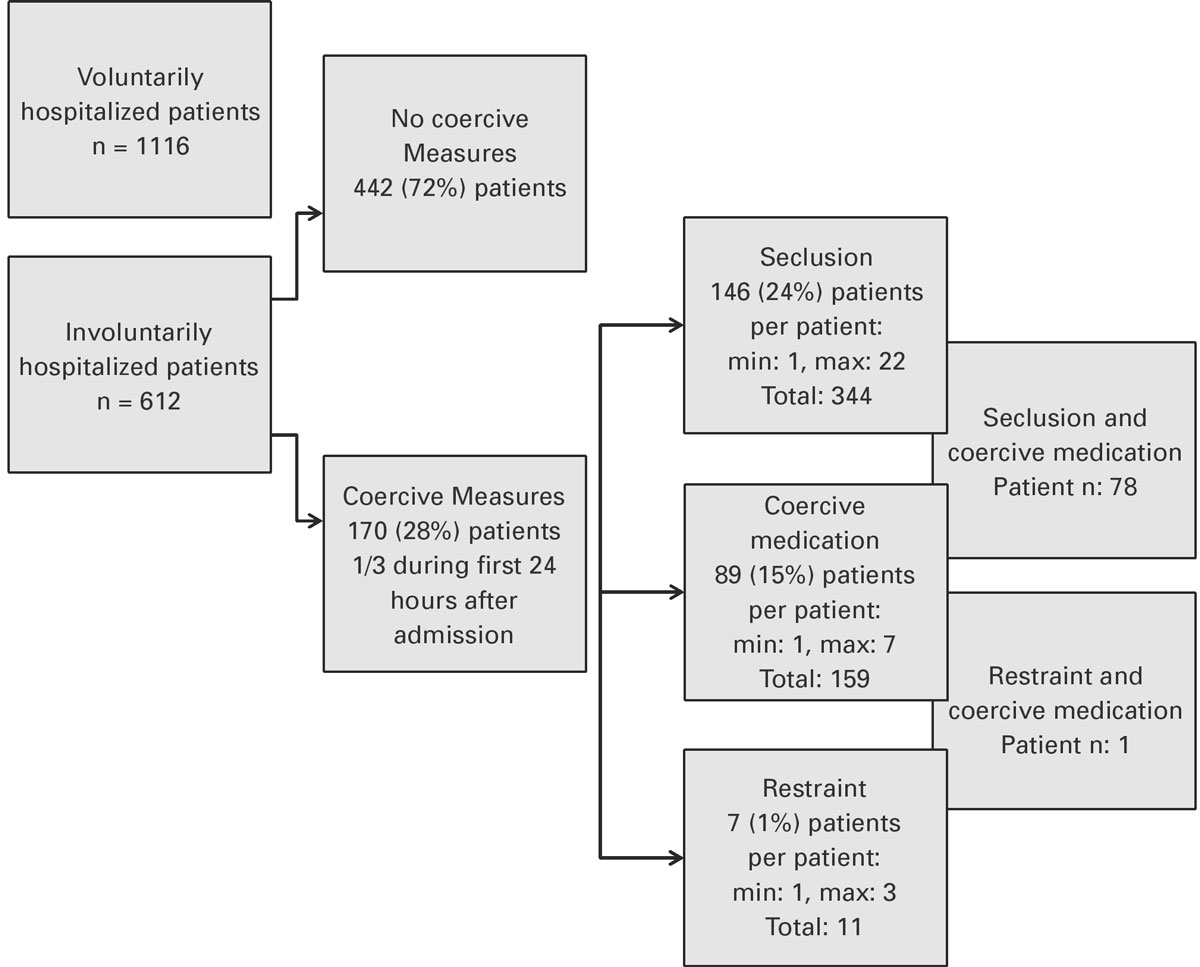
Figure 1 Prevalence of coercive measures at the University Hospital of Psychiatry Zurich.
The cumulative duration of seclusion in the 14 patients with the longest episodes of seclusion (10% of those patients with episodes of seclusion) was 1773 hours, which accounts for 57% of the total duration of seclusion (for detailed information about the duration of coercive measures see table 2). In those patients with restraint, one patient with an episode of 54 hours accounted for 40% of the total time under restraint.
Table 2 Duration of coercive measures during a 6 month period.
| Per patient | Per measure | |||||
|---|---|---|---|---|---|---|
| Minimum | Maximum | Mean | Standard deviation | Median | Mean | |
| Duration of seclusion in hours 146 patients, 344 measures |
0.5 | 655 | 21 | 60 | 7.25 | 9 |
| Duration of restraint in hours 7 patients, 11 measures |
0.25 | 54 | 19 | 17 | 17 | 12 |
Male gender was significantly associated with the use of coercion. More detailed analysis showed that this was the case for coercive medication and seclusion, whereas the use of restraint did not differ significantly between males and females. Age did not show significant differences between the group of patients who received coercive measures and those without such measures. Retention of patients who were admitted voluntarily at first was significantly correlated with the use of coercion. In patients with involuntary commitment, those referred by emergency medicine physicians were significantly more often exposed to coercion, whereas the group referred from hospital physicians showed the lowest rates of coercive measures. Patients who were referred because of harm to self or others and those whose admission involved the police force were more frequently treated with coercion. A primary diagnosis of psychotic disorder or personality disorder was significantly associated with coercion. In the patients with personality disorders, 70% met the criteria for cluster B [43], with most of them having borderline personality disorders. Nearly half of all patients meeting cluster B criteria, received at least one coercive measure. The type of coercive measure used did not differ between patients with personality disorder and those with other diagnoses. A secondary substance use disorder was significantly associated with coercion (n = 218, chi-square 17.76, p <0.01). Antipsychotics and benzodiazepines were prescribed significantly more often in patients who experienced coercion during their hospitalisation. Other pharmacological groups, such as antidepressants, mood stabilisers, replacement therapy and stimulants showed no significant differences between the groups. For detailed information see table 3.
Table 3 Comparison of patients’ characteristics with/without coercion of clinical and procedural parameters.
|
Total
(n = 612) |
No coercion
(n = 442) |
Coercion
(n = 170) |
χ2 | df | p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||||
| Gender | 7.12 | 1 | 0.008 | ||||||
| Male | 314 | 51 | 212a | 67 | 102b | 33 | |||
| Age at admission | 7.38 | 0.117 | |||||||
| <30 years | 127 | 21 | 89 | 70 | 38 | 30 | |||
| 30–39 years | 111 | 18 | 71 | 64 | 40 | 36 | |||
| 40–49 years | 91 | 15 | 72 | 79 | 19 | 21 | |||
| 50–59 years | 94 | 15 | 67 | 71 | 27 | 29 | |||
| >60 years | 189 | 31 | 143 | 76 | 46 | 24 | |||
| Retained patients | 27.40 | 1 | <0.001 | ||||||
| Yes | 39 | 6 | 14a | 36 | 25b | 64 | |||
| Referring physician | 19.75 | 4 | <0.001 | ||||||
| Psychiatrist | 274 | 40 | 171a | 69 | 76a | 31 | |||
| Emergency physician | 135 | 22 | 86a | 64 | 49b | 36 | |||
| Hospital physician | 142 | 23 | 122a | 86 | 20b | 14 | |||
| General physician | 66 | 11 | 46a | 70 | 20 a | 30 | |||
| Other | 22 | 4 | 17a | 77 | 5a | 23 | |||
| Reason for involuntary commitment | 69.97 | 3 | <0.001 | ||||||
| Harm to self | 337 | 55 | 287a | 85 | 50b | 15 | |||
| Harm to others | 118 | 19 | 60a | 51 | 58b | 49 | |||
| Harm to self and others | 134 | 22 | 77a | 57 | 57b | 43 | |||
| Other | 23 | 4 | 18a | 78 | 5a | 22 | |||
| Psychiatric diagnosis | 65.48 | 6 | <0.001 | ||||||
| Organic disorder (F0) | 109 | 18 | 82a | 75 | 27a | 25 | |||
| Substance use disorder (F1) | 94 | 15 | 82a | 87 | 12b | 13 | |||
| Psychotic disorder (F2) | 225 | 37 | 136a | 60 | 89b | 40 | |||
| Affective disorder (F3) | 80 | 13 | 60a | 75 | 20a | 25 | |||
| Neurotic disorder (F4) | 67 | 11 | 66a | 99 | 1b | 1 | |||
| Personality disorder (F6) | 21 | 3 | 9a | 43 | 12b | 57 | |||
| Other | 16 | 3 | 7a | 44 | 9b | 56 | |||
| Police involved at admission | 20.40 | 1 | <0.001 | ||||||
| Yes | 187 | 31 | 112a | 60 | 75b | 40 | |||
| Former involuntary commitment | 27.78 | 1 | <0.001 | ||||||
| Yes | 270 | 44 | 166a | 61 | 104b | 39 | |||
| Antipsychotics | 59.14 | 1 | <0.001 | ||||||
| Yes | 457 | 75 | 293a | 64 | 164b | 36 | |||
| Antidepressant | 4.79 | 1 | 0.029 | ||||||
| Yes | 222 | 36 | 172a | 78 | 50b | 22 | |||
| Benzodiazepines | 26.34 | 1 | <0.001 | ||||||
| Yes | 454 | 74 | 303a | 67 | 151b | 33 | |||
df = degrees of freedom Missing values of all variables are less than 1.8%. Identical letters indicate no statistically significant difference by Bonferroni-adjusted chi-square post-hoc tests at p <0.05.
Time until issue of a day pass, time until revocation of involuntary commitment and total duration of hospitalisation were significantly longer in the group of patients exposed to coercion. This was also the case when controlled for gender, age, former admissions and the psychiatric diagnosis F2 by rank regression analyses. Patients who experienced coercive measures also had significantly more former admissions than those without coercion (for details see table 4). Also, the number of re-hospitalisations during the 6 months was significantly higher in those patients with coercion (n = 612, chi-square 9.73, p <0.01). The individual hospital wards did not differ significantly in the rates of coercion (n = 612, chi-square 18.60, p = 0.181).
Table 4 Comparison of group with/without coercion of procedural aspects during hospitalisation.
| Coercion | Mann-Whitney U | Z | p-value | Cohen’s r | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No (n = 442) | Yes (n = 170) | |||||||||||
| Minimum | Maximum | Mean | Median | Minimum | Maximum | Mean | Median | |||||
| Number of former admissions | 0 | 69 | 4 | 0 | 0 | 67 | 9 | 2 | 27771.5 | 5.249 | <0.001 | 0.21 |
| Time until revocation of IC | 0 | 88 | 15 | 10 | 1 | 230 | 31 | 25 | 20859.5 | 8.453 | <0.001 | 0.34 |
| Duration of hospitalisation | 0 | 138 | 21 | 13 | 1 | 245 | 37 | 31 | 21871.5 | 8.015 | <0.001 | 0.32 |
| Time until issue of day passes | 0 | 109 | 10 | 5 | 0 | 161 | 18 | 11 | 23864.0 | 6.918 | <0.001 | 0.28 |
IC = involuntary commitment
Our study showed that there are some clinical and procedural characteristics of patients that are associated with the usage of coercive measures in Switzerland. We were also able to show that 28% of the involuntarily hospitalised patients (10% of all inpatients) experienced coercive measures in the largest psychiatric hospital in Switzerland.
As well as the percentage of patients in which coercion was used, it is important to analyse the number and length of coercive measures in the patients affected. The number of coercive measures per affected patient in Zurich (3) was higher than in various European countries where a mean number of 1.5 coercive measures per affected patient [44]. The complexity of the interpretation of coercive measures can be illustrated by a comparison with a German study, which revealed a prevalence of coercive measures of 9.5% in all treated patients [12]. This is comparable to data in this study. But further analysis showed that in this study 5.4 coercive measures per patient were applied. The mean duration per patient was also lower in Zurich, with 20 hours compared with 50.6 hours in Germany.
In this study we showed that seclusion was the most commonly used coercive measure. This differs from countries such as Germany, where seclusion is rarely used relative to restraint [13]. The low numbers of restraints at the University Hospital of Psychiatry Zurich may explained by knowledge about their harmful side effects [45–47]. But differences in the attitude towards coercive measures, which had been shown in earlier studies, [48, 49] could also account for this difference and future studies should aim to gain more understanding about this phenomenon. When we compared the wards for their usage of coercive measures, no significant between-ward variance was found. This contrasts with former findings [29], where such a variance was described. Our finding may be explained by the fact that the entire hospital adheres to the same strategy in the treatment of involuntarily hospitalised patients. The wards distribute patients at “high-risk” with a good balance, and interpersonal bias might be reduced through combined staff training from all wards, which is a standard procedure at the University Hospital of Psychiatry Zurich.
Patients who were admitted because of danger to others were more likely to be subjected to coercion, which was also shown in other studies [50, 51] and might be an explanation for the significant association between police involvement at admission and the use of coercion. Our data revealed that, during inpatient treatment, harm to others was the most common reason for seclusion or coercive medication. The fact that male gender is a risk factor for coercive measures has already been described [36], but it is important to remember that other studies have shown females to be more often exposed to coercion [35].
As in other studies, our study showed that patients with schizophrenia or other psychotic disorders were significantly more likely to experience coercion. Paranoid ideation, hallucinations and anxiety (some of the main symptoms in these disorders) might be associated with an increased stress level and reduced coping strategies in conflicts, resulting in danger and the use of coercive measures [43]. Personality disorders were also significantly associated with use of coercive measures. The big group of Cluster B personality disorders in these patients might be caused by impaired impulse control and excessive emotions [43], which also might lead to threatening situations on the wards. Interestingly, a substance use disorder as primary diagnosis was not significantly associated with use of coercive measures, but when given as a secondary diagnosis a significant association was shown. Withdrawal and craving might lead to higher vulnerability to stress with less coping strategies available. In patients with a dual diagnosis, withdrawal might combine with symptoms caused by another disorder, which increases sensitivity in patients.
A recovery-oriented patient-centred deescalating attitude from the staff`s side may be helpful to meet the needs of this group of patients [52]. Clarity and communication skills have been shown to create an environment where patients feel secure and are better able to engage in a therapeutic relationship. In some situations informal coercion may also be a potent way to avoid legal coercion [53]. Its use should nevertheless be considered within the team and the patient [54].
Some limitations have to be mentioned regarding this study. The analysis was based on retrospectively collected data, and it was not possible to assess the subjective perspectives of patients and hospital staff in a standardised form. Also, in some cases when patients were secluded and took medication, the documentation of the situation did not explicitly reveal if the application of medication was voluntary, or if either informal or legal coercion was used. As it was not possible to gain more information we decided to document the occurrence of coercive medication only if it was declared as coercive medication in the patient’s documentation file. Owing to the retrospective character of the study, the clinical course and severity of the patients’ psychopathological symptoms could not be assessed in a standardised, way which limits the comparability of patients. Clinic culture and organisational aspects as potential influencing factors were not included in the analysis which might also be a limitation in this study.
Despite these limitations, this study was able to show that there is a group of patients who are at risk for receiving coercion. We also showed that more than half of the coercive measures (in number and duration) were used in a small group of patients. Further studies should focus on interventions that could help to reduce the number of coercive measures and their duration. Further studies investigating the prevalence of coercive measures should analyse different measurement parameters to ensure comparability of the results (number of coercive measures in voluntarily and involuntarily hospitalised patients, number of coercive measures per patient, duration per patient, duration per measure). Furthermore, it should be an aim of future studies to analyse reasons for the prolonged hospitalisation in patients who experience coercion compared with those without coercion, especially because one argument for the use of coercive measures is that they help to defuse a crisis.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Zinkler M , Priebe S . Detention of the mentally ill in Europe--a review. Acta Psychiatr Scand. 2002;106(1):3–8. doi:.https://doi.org/10.1034/j.1600-0447.2002.02268.x
2 Lay B , Salize HJ , Dressing H , Rüsch N , Schönenberger T , Bühlmann M , et al. Preventing compulsory admission to psychiatric inpatient care through psycho-education and crisis focused monitoring. BMC Psychiatry. 2012;12(1):136. doi:.https://doi.org/10.1186/1471-244X-12-136
3 Jäger M , Ospelt I , Kawohl W , Theodoridou A , Rössler W , Hoff P . Qualität unfreiwilliger Klinikeinweisungen in der Schweiz. Praxis (Bern). 2014;103(11):631–9. doi:.https://doi.org/10.1024/1661-8157/a001670
4Salize HJ, Dressing H, Peitz M. Compulsory Admission and Involuntary Treatment of Mentally Ill Patients – Legislation and Practice in EU-Member States. 2002; Available from: http://ec.europa.eu/health/ph_projects/2000/promotion/fp_promotion_2000_frep_08_en.pdf.
5 Soininen P , Välimäki M , Noda T , Puukka P , Korkeila J , Joffe G , et al. Secluded and restrained patients’ perceptions of their treatment. Int J Ment Health Nurs. 2013;22(1):47–55. doi:.https://doi.org/10.1111/j.1447-0349.2012.00838.x
6 Molewijk B , Kok A , Husum T , Pedersen R , Aasland O . Staff’s normative attitudes towards coercion: the role of moral doubt and professional context-a cross-sectional survey study. BMC Med Ethics. 2017;18(1):37. doi:.https://doi.org/10.1186/s12910-017-0190-0
7 Curran WJ . Comparative analysis of mental health legislation in forty-three countries: a discussion of historical trends. Int J Law Psychiatry. 1978;1(1):79–92. doi:.https://doi.org/10.1016/0160-2527(78)90025-0
8 Hoff P . Zwangsmassnahmen in der Medizin. Schweiz Arzteztg. 2015;96(22):773–5. doi:https://doi.emh.ch/10.4414/saez.2015.03581.
9 Dressing H , Salize HJ . Zwangsunterbringung und Zwangsbehandlung psychisch Kranker in den Mitgliedsländern der Europäischen Union [Compulsory admission of mentally ill patients in European union member States]. Psychiatr Prax. 2004;31(1):34–9.
10 Lauber C , Rössler W . Zwangsaufnahme in das psychiatrische Krankenhaus im Spiegel der öffentlichen Meinung und aus Sicht von Professionellen in der Psychiatrie [Involuntary admission and the attitude of the general population, and mental health professionals]. Psychiatr Prax. 2007;34(Suppl 2):S181–5. doi:.https://doi.org/10.1055/s-2006-952002
11 Steinert T , Lepping P , Bernhardsgrütter R , Conca A , Hatling T , Janssen W , et al. Incidence of seclusion and restraint in psychiatric hospitals: a literature review and survey of international trends. Soc Psychiatry Psychiatr Epidemiol. 2010;45(9):889–97. doi:.https://doi.org/10.1007/s00127-009-0132-3
12 Steinert T , Martin V , Baur M , Bohnet U , Goebel R , Hermelink G , et al. Diagnosis-related frequency of compulsory measures in 10 German psychiatric hospitals and correlates with hospital characteristics. Soc Psychiatry Psychiatr Epidemiol. 2007;42(2):140–5. doi:.https://doi.org/10.1007/s00127-006-0137-0
13 Martin V , Bernhardsgrütter R , Göbel R , Steinert T . Ein Vergleich von Schweizer und deutschen Kliniken in Bezug auf die Anwendung von Fixierung und Isolierung [The use of mechanical restraint and seclusion: comparing the clinical practice in Germany and Switzerland]. Psychiatr Prax. 2007;34(Suppl 2):S212–7. doi:.https://doi.org/10.1055/s-2006-952005
14 Wierdsma AI , van Baars AW , Mulder CL . Psychiatrische voorgeschiedenis en nazorg bij dwangopneming. Zorggebruik als indicator van de kwaliteit van zorg bij inbewaringstellingen in Rotterdam [Psychiatric past history and health care after compulsory admission. Care use as an indicator of the quality of care for patients in compulsory care in Rotterdam]. Tijdschr Psychiatr. 2006;48(2):81–93.
15 Knutzen M , Bjørkly S , Eidhammer G , Lorentzen S , Mjøsund NH , Opjordsmoen S , et al. Characteristics of patients frequently subjected to pharmacological and mechanical restraint--a register study in three Norwegian acute psychiatric wards. Psychiatry Res. 2014;215(1):127–33. doi:.https://doi.org/10.1016/j.psychres.2013.10.024
16 Bilanakis N , Kalampokis G , Christou K , Peritogiannis V . Use of coercive physical measures in a psychiatric ward of a general hospital in Greece. Int J Soc Psychiatry. 2010;56(4):402–11. doi:.https://doi.org/10.1177/0020764009106620
17 El-Badri SM , Mellsop G . A study of the use of seclusion in an acute psychiatric service. Aust N Z J Psychiatry. 2002;36(3):399–403. doi:.https://doi.org/10.1046/j.1440-1614.2002.01003.x
18 Migon MN , Coutinho ES , Huf G , Adams CE , Cunha GM , Allen MH . Factors associated with the use of physical restraints for agitated patients in psychiatric emergency rooms. Gen Hosp Psychiatry. 2008;30(3):263–8. doi:.https://doi.org/10.1016/j.genhosppsych.2007.12.005
19 Larue C , Dumais A , Drapeau A , Ménard G , Goulet MH . Nursing practices recorded in reports of episodes of seclusion. Issues Ment Health Nurs. 2010;31(12):785–92. doi:.https://doi.org/10.3109/01612840.2010.520102
20 Happell B , Gaskin CJ . Exploring patterns of seclusion use in Australian mental health services. Arch Psychiatr Nurs. 2011;25(5):e1–8. doi:.https://doi.org/10.1016/j.apnu.2011.04.001
21 Hendryx M , Trusevich Y , Coyle F , Short R , Roll J . The distribution and frequency of seclusion and/or restraint among psychiatric inpatients. J Behav Health Serv Res. 2010;37(2):272–81. doi:.https://doi.org/10.1007/s11414-009-9191-1
22 Zhu XM , Xiang YT , Zhou JS , Gou L , Himelhoch S , Ungvari GS , et al. Frequency of physical restraint and its associations with demographic and clinical characteristics in a Chinese psychiatric institution. Perspect Psychiatr Care. 2014;50(4):251–6. doi:.https://doi.org/10.1111/ppc.12049
23 Salize HJ , Dressing H . Epidemiology of involuntary placement of mentally ill people across the European Union. Br J Psychiatry. 2004;184(02):163–8. doi:.https://doi.org/10.1192/bjp.184.2.163
24 Riecher-Rössler A , Rössler W . Compulsory admission of psychiatric patients--an international comparison. Acta Psychiatr Scand. 1993;87(4):231–6. doi:.https://doi.org/10.1111/j.1600-0447.1993.tb03363.x
25 Faulkner LR , McFarland BH , Bloom JD . An empirical study of emergency commitment. Am J Psychiatry. 1989;146(2):182–6. doi:.https://doi.org/10.1176/ajp.146.2.182
26 Odawara T , Narita H , Yamada Y , Fujita J , Yamada T , Hirayasu Y . Use of restraint in a general hospital psychiatric unit in Japan. Psychiatry Clin Neurosci. 2005;59(5):605–9. doi:.https://doi.org/10.1111/j.1440-1819.2005.01422.x
27 Korkeila JA , Tuohimäki C , Kaltiala-Heino R , Lehtinen V , Joukamaa M . Predicting use of coercive measures in Finland. Nord J Psychiatry. 2002;56(5):339–45. doi:.https://doi.org/10.1080/080394802760322105
28Deutsche Gesellschaft für Psychiatrie und Psychotherapie. Psychosomatik und Nervenheilkunde. Praxisleitlinien in Psychiatrie und Psychotherapie Band 2: Therapeutische Maßnahmen bei aggressivem Verhalten in der Psychiatrie und Psychotherapie. Ed. Gaebel W, Falkau P. Berlin: Springer; 2010.
29 Husum TL , Bjørngaard JH , Finset A , Ruud T . A cross-sectional prospective study of seclusion, restraint and involuntary medication in acute psychiatric wards: patient, staff and ward characteristics. BMC Health Serv Res. 2010;10(1):89. doi:.https://doi.org/10.1186/1472-6963-10-89
30 Keski-Valkama A , Sailas E , Eronen M , Koivisto AM , Lönnqvist J , Kaltiala-Heino R . The reasons for using restraint and seclusion in psychiatric inpatient care: A nationwide 15-year study. Nord J Psychiatry. 2010;64(2):136–44. doi:.https://doi.org/10.3109/08039480903274449
31National Institute for Mental Health in England. Results of a national census of inpatients in mental health hospitals and facilities in England and Wales. Available from: http://www.wales.nhs.uk/documents/04021695.pdf
32 Beck NC , Durrett C , Stinson J , Coleman J , Stuve P , Menditto A . Trajectories of seclusion and restraint use at a state psychiatric hospital. Psychiatr Serv. 2008;59(9):1027–32. doi:.https://doi.org/10.1176/ps.2008.59.9.1027
33 Knutzen M , Mjosund NH , Eidhammer G , Lorentzen S , Opjordsmoen S , Sandvik L , et al. Characteristics of psychiatric inpatients who experienced restraint and those who did not: a case-control study. Psychiatr Serv. 2011;62(5):492–7. doi:.https://doi.org/10.1176/ps.62.5.pss6205_0492
34 Dumais A , Larue C , Drapeau A , Ménard G , Giguère Allard M . Prevalence and correlates of seclusion with or without restraint in a Canadian psychiatric hospital: a 2-year retrospective audit. J Psychiatr Ment Health Nurs. 2011;18(5):394–402. doi:.https://doi.org/10.1111/j.1365-2850.2010.01679.x
35 Sercan M , Bilici R . [Restraint variables in a regional mental health hospital in Turkey]. Turk Psikiyatr Derg. 2009;20(1):37–48.
36 Kalisova L , Raboch J , Nawka A , Sampogna G , Cihal L , Kallert TW , et al. Do patient and ward-related characteristics influence the use of coercive measures? Results from the EUNOMIA international study. Soc Psychiatry Psychiatr Epidemiol. 2014;49(10):1619–29. doi:.https://doi.org/10.1007/s00127-014-0872-6
37 Jarrett M , Bowers L , Simpson A . Coerced medication in psychiatric inpatient care: literature review. J Adv Nurs. 2008;64(6):538–48. doi:.https://doi.org/10.1111/j.1365-2648.2008.04832.x
38 Fiorillo A , Giacco D , De Rosa C , Kallert T , Katsakou C , Onchev G , et al. Patient characteristics and symptoms associated with perceived coercion during hospital treatment. Acta Psychiatr Scand. 2012;125(6):460–7. doi:.https://doi.org/10.1111/j.1600-0447.2011.01809.x
39 Whitehead PD , Liljeros F . Heavy-tailed distribution of seclusion and restraint episodes in a state psychiatric hospital. J Am Acad Psychiatry Law. 2011;39(1):93–9.
40 Flammer E , Steinert T , Eisele F , Bergk J , Uhlmann C . Who is Subjected to Coercive Measures as a Psychiatric Inpatient? A Multi-Level Analysis. Clin Pract Epidemol Ment Health. 2013;9(1):110–9. doi:.https://doi.org/10.2174/1745017901309010110
41Gassmann J. Wirksamkeit des Rechtsschutzes bei psychiatrischen Zwangseinweisungen in der Schweiz. 2011. p. 1-51. Available from: https://www.humanrights.ch/upload/pdf/140217_Wirksamkeit_des_Rechtschutzes_bei_psychiatrischen_Zwangseinweisungen_in_der_Schweiz_2011.pdf
42 Patel MX , de Zoysa N , Bernadt M , Bindman J , David AS . Are depot antipsychotics more coercive than tablets? The patient’s perspective. J Psychopharmacol. 2010;24(10):1483–9. doi:.https://doi.org/10.1177/0269881109103133
43American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5). 2013: American Psychiatric Pub.
44 Raboch J , Kalisová L , Nawka A , Kitzlerová E , Onchev G , Karastergiou A , et al. Use of coercive measures during involuntary hospitalization: findings from ten European countries. Psychiatr Serv. 2010;61(10):1012–7. doi:.https://doi.org/10.1176/ps.2010.61.10.1012
45 Hatta K , Shibata N , Ota T , Usui C , Ito M , Nakamura H , et al. Association between physical restraint and drug-induced liver injury. Neuropsychobiology. 2007;56(4):180–4. doi:.https://doi.org/10.1159/000119736
46 Strout TD . Perspectives on the experience of being physically restrained: an integrative review of the qualitative literature. Int J Ment Health Nurs. 2010;19(6):416–27. doi:.https://doi.org/10.1111/j.1447-0349.2010.00694.x
47 Smith SB . Restraints: retraumatization for rape victims? J Psychosoc Nurs Ment Health Serv. 1995;33(7):23–8.
48 Hottinen A , Välimäki M , Sailas E , Putkonen H , Joffe G , Noda T , et al. Underaged patients’ opinions toward different containment measures: a questionnaire survey in Finnish adolescent psychiatry. J Child Adolesc Psychiatr Nurs. 2012;25(4):219–23. doi:.https://doi.org/10.1111/jcap.12006
49 Dack C , Ross J , Bowers L . The relationship between attitudes towards different containment measures and their usage in a national sample of psychiatric inpatients. J Psychiatr Ment Health Nurs. 2012;19(7):577–86. doi:.https://doi.org/10.1111/j.1365-2850.2011.01832.x
50 Steinert T , Schmid P . Effect of voluntariness of participation in treatment on short-term outcome of inpatients with schizophrenia. Psychiatr Serv. 2004;55(7):786–91. doi:.https://doi.org/10.1176/appi.ps.55.7.786
51 Gudjonsson GH , Rabe-Hesketh S , Szmukler G . Management of psychiatric in-patient violence: patient ethnicity and use of medication, restraint and seclusion. Br J Psychiatry. 2004;184(03):258–62. doi:.https://doi.org/10.1192/bjp.184.3.258
52 Fiorillo A , De Rosa C , Del Vecchio V , Jurjanz L , Schnall K , Onchev G , et al. How to improve clinical practice on involuntary hospital admissions of psychiatric patients: suggestions from the EUNOMIA study. Eur Psychiatry. 2011;26(4):201–7. doi:.https://doi.org/10.1016/j.eurpsy.2010.01.013
53 Hotzy F , Jaeger M . Clinical Relevance of Informal Coercion in Psychiatric Treatment-A Systematic Review. Front Psychiatry. 2016;7:197. doi:.https://doi.org/10.3389/fpsyt.2016.00197
54 Appelbaum PS , Le Melle S . Techniques used by assertive community treatment (ACT) teams to encourage adherence: patient and staff perceptions. Community Ment Health J. 2008;44(6):459–64. doi:.https://doi.org/10.1007/s10597-008-9149-4
No financial support and no other potential conflict of interest relevant to this article was reported.