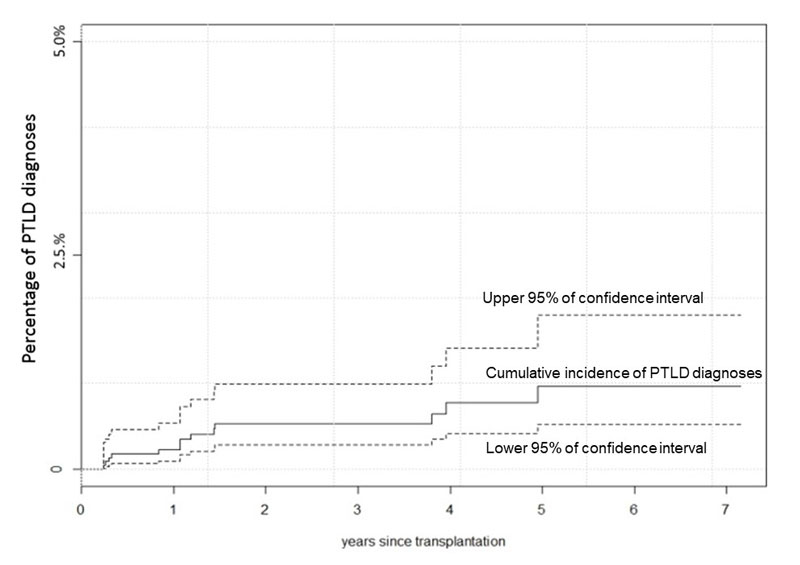
Figure 1 Post-transplant lymphoproliferative disorder cumulative incidence rate according to time after transplantation for solid organ transplant patients in the Swiss Transplant Cohort Study.
DOI: https://doi.org/10.4414/smw.2018.14596
Solid organ transplant recipients have an elevated cancer risk due to immunosuppression and subsequent oncogenic viral infections [1]. Post-transplant lymphoproliferative disorder (PTLD) is a potentially life-threatening complication in up to 20% of transplanted patients [2], with non-Hodgkin’s lymphoma accounting for 93% of cases [3]. PTLD development after solid organ transplantation is estimated to be from 1 to 20%, with the highest incidence for intestinal and multivisceral transplants (up to 20%), followed by lung and heart transplants (up to 10%), and the lowest incidence for renal and liver transplants (up to 5%) [4].
The pathogenesis of PTLD is based on the immunosuppression-associated reduction of CD8+ T cells responsible for protective cytotoxic immunity to viruses [5], resulting in an imbalance in Epstein-Barr virus (EBV)-positive B cells, virus-specific cytotoxic T cells and regulatory T cells. This facilitates the proliferation of EBV-positive B cells and development of PTLD [6]. According to the World Health Organization (WHO) classification 2008 (updated in 2016), PTLDs are subdivided into (a) early lesions (plasmacytic hyperplasia, infectious mononucleosis-like PTLD and florid follicular hyperplasia), (b) polymorphic PTLD (polyclonal lymphatic proliferations with histoarchitectural tissue effacement), and (c) monomorphic PTLD including B- and T-cell lymphoma resembling PTLD and Hodgkin’s type of PTLD [6–8].
Since the likelihood of PTLD is strictly related to the degree of immunosuppression and infection with EBV, prevention is mainly achieved by limited patient exposure to aggressive immunosuppressive regimens [9], rapid withdrawal and tapering of agents required for graft tolerance, and antiviral prophylaxis [10]. Options for initial treatment of PTLD encompass reduction of immunosuppression [11], immunotherapy with the anti-CD20 monoclonal antibody rituximab [12], chemotherapy [13], radiation therapy [14], or a combination thereof.
Little is known about the outcome of PTLDs in Switzerland under treatment over time. We hypothesised that there could be a difference in the cumulative incidence of PTLDs between Switzerland and other countries, related to differences in population, risk factors, management or access to healthcare. For a better understanding and a useful management of these disorders we conducted a retrospective study describing cumulative incidence, histological subtypes, risk factors and outcome in our country.
We conducted a retrospective evaluation of solid organ transplant patients in Switzerland using two sequential cohorts. A first case series before the Swiss Transplant Cohort Study, the pre-STCS cohort, started with data gathered from PTLD patients in five transplant centres in Switzerland (Geneva University Hospital, Lausanne University Hospital, Zurich University Hospital, Basel University Hospital and St Gallen State Hospital) between January 1986 (date of transplantation) and April 2008. Only one transplant centre in Switzerland did not participate in the data gathering for the pre-STCS case series, which was not expected to have changed significantly the final results.
The pre-STCS case series mostly cross-referenced the data of solid organ transplant patients with the data of lymphoma patients diagnosed in each centre. Some data of the pre-STCS case series were provided by Swiss Transplant [15]. The data for the pre-STCS cohort were gathered specifically for this study and were not in a national registry.
The second cohort, the Swiss Transplant Cohort Study (STCS) [16] started in May 2008. The STCS covers solid organ transplantation on a national scale in a complete and comprehensive way. The last patient of this cohort included in this study was diagnosed with PTLD in December 2014 Six percent of solid organ transplant patients nationwide did not give consent for their data to be included in the STCS. Also, we lost a few patients in the follow-up period.
We included the pre-STCS case series because of the low number of PTLD patients in the STCS cohort.
Only patients aged ≥18 years old at the time of transplantation and undergoing SOT from 1986 met the inclusion criteria for this study.
PTLD was defined as lymphoproliferative disorder developing at least 1 month after transplantation and no later than 2 years after loss of graft function [17].
For each transplant recipient, pre-STCS or STCS, data included demographic characteristics, serology results for EBV (EBV IgG) and cytomegalovirus (CMV IgG). Information on the initial immunosuppressive regimen prescribed prior to hospital discharge, 6 and 12 months after the solid organ transplant, and at the time of the PTLD diagnosis were also obtained.
Transplant centres reported on the occurrence of PTLD during follow-up, which were categorised according to the 2008 WHO classification. PTLDs diagnosed within 1 year of transplant were defined as early-onset PTLD and those diagnosed after 1 year were defined as late-onset PTLD.
All patients with PTLD were staged retrospectively according to the Ann Arbor staging system, and International Prognostic Index (IPI) [18] scores were calculated wherever possible. Performance status and response to treatment were determined retrospectively and were extracted from clinical reports. Approval for the study was obtained from the institutional review boards of all five participating transplant centres.
Owing to the retrospective nature of the study, with cases of PTLD diagnosed back to 1990, it was not possible to do a central review of the pathology. PTLDs were categorised according to the 2008 WHO classification, with information retrieved from charts.
EBV was identified in PTLD tissue specimens by in-situ hybridisation for EBV (EBER; Epstein-Barr virus encoded RNA). This information was retrieved from charts.
Overall survival was estimated using the Kaplan-Meier method, and was determined from the date of PTLD diagnosis to the date of death from any cause or last follow-up. A p-value <0.05 was considered statistically significant, and all p-values were two-sided. The survival analysis accounted for loss to follow up, graft loss and the varying observation time of each patient. No fixed denominator was applied.
During the pre-STCS period 8708 solid organ transplants were performed nationwide [19] and 2942 were performed during the STCS period. After exclusion of patients younger than 18 years, 79 patients were diagnosed with PTLD in five transplant centres in Switzerland. In total, 62 patients undergoing solid organ transplantation in January 1986 or later and having a diagnosis of PTLD up to April 2008 were included in the pre-STCS case series. Seventeen patients were included in the STCS cohort with a solid organ transplant not before May 2008 and a PTLD diagnosed by December 2014. The interval between transplantation and PTLD occurrence ranged between 2 and 281 months (table 1) and some patients of the pre-STCS case series were diagnosed with PTLD during the period of the STCS cohort. The observation period of the two cohorts ended in December 2014.
Table 1 Time from transplantation to post-transplant lymphoproliferative disorders (PTLD) diagnosis (months) with histological substratification.
| WHO Classification of PTLD | Pre-STCS | STCS | Pre-STCS+STCS | |
|---|---|---|---|---|
| Early | Median | 75 | No case | 75 |
| Range | 64–85 | No case | 64–85 | |
| Polymorphic | Median | 14 | 10 | 13 |
| Range | 5–237 | 2–28 | 2–237 | |
| Monomorphic | Median | 96 | 17 | 81 |
| Range | 3–281 | 3–59 | 3–281 | |
| Hodgkin's | Median | 67 | No case | 67 |
| Range | 26–228 | No case | 26–228 | |
| All histologies | Median | 90 | 14 | 59 |
| Range | 3–281 | 2–59 | 2–281 | |
STCS = Swiss Transplant Cohort Study
The baseline characteristics of PTLD patients are presented in table 2. The median age of patients at transplantation was similar in both cohorts, namely 43 years (range 18–69) in the pre-STCS case series and 44 years (18–61) years in the STCS. Our data showed a strong male predominance in both cohorts, in accordance with the gender distribution of transplanted patients in the STCS, with 63.2% male patients [20].
Table 2 Basic demographic characteristics.
| Characteristics |
Pre-STCS
(n = 62) |
STCS
(n = 17) |
|||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Sex | Male | 51 | 82 | 11 | 65 |
| Female | 11 | 18 | 6 | 35 | |
| Age at first transplantation, years | Median | 43 | – | 44 | – |
| Average | 43 | – | 46 | – | |
| Range | 18–69 | – | 18–61 | – | |
| 18–35 | 18 | 29 | 4 | 24 | |
| 36–53 | 30 | 48 | 6 | 35 | |
| >53 | 14 | 23 | 7 | 41 | |
| Organ transplanted | Kidney | 38 | 61 | 6 | 35 |
| Heart | 9 | 15 | 2 | 12 | |
| Lung | 5 | 8 | 6 | 35 | |
| Liver | 8 | 13 | 1 | 6 | |
| Pancreas + kidney | 1 | 2 | 1 | 6 | |
| Liver + kidney | 0 | 0 | 0 | 0 | |
| Heart + kidney | 1 | 2 | 0 | 0 | |
| Bowel and pancreas | 0 | 0 | 1 | 6 | |
| Histology | Early | 2 | 3 | 0 | 0 |
| Polymorphic | 8 | 13 | 7 | 41 | |
| Monomorphic (all) | 47 | 76 | 10 | 59 | |
| Monomorphic DLBCL | 37 | 60 | 7 | 41 | |
| Monomorphic Burkitt lymphoma | 4 | 6 | 0 | 0 | |
| Monomorphic other | 6 | 10 | 0 | 0 | |
| Hodgkin’s disease | 5 | 8 | 0 | 0 | |
| Age at PTLD diagnosis, years | Median | 53 | – | 45 | – |
| Mean | 51 | – | 48 | – | |
| Range | 22–75 | – | 18–65 | – | |
| 18–35 | 9 | 15 | 3 | 18 | |
| 36–53 | 22 | 35 | 7 | 41 | |
| >53 | 31 | 50 | 7 | 41 | |
| Time of onset of PTLD | Within 1 year after transplant | 9 | 15 | 8 | 47 |
| More than 1 year after transplant | 53 | 85 | 9 | 53 | |
| Ann Arbor stage | Stage I–II | 30 | 48 | 11 | 65 |
| Stage III–IV | 32 | 52 | 6 | 35 | |
| IPI | 0–2 | 36 | 58 | 12 | 71 |
| 3–5 | 20 | 32 | 5 | 29 | |
| Insufficient data | 6 | 10 | 0 | 0 | |
| EBV serostatus before transplant patient | Positive (EBV IgG or PCR) | 25 | 40 | 11 | 65 |
| Negative (EBV IgG or PCR) | 5 | 8 | 4 | 24 | |
| Insufficient data | 32 | 52 | 2 | 12 | |
| EBV serostatus before PTLD diagnosis, patient | Positive | 36 | 58 | 16 | 94 |
| Negative | 9 | 15 | 0 | 0 | |
| Insufficient data | 17 | 27 | 1 | 6 | |
| Tumour EBV status | Positive | 27 | 44 | 14 | 82 |
| Negative | 26 | 42 | 1 | 6 | |
| Insufficient data | 9 | 15 | 2 | 12 | |
| Initial maintenance immunosuppression at transplantation | CYA ±– AZA | 35 | 56 | 6 | 35 |
| TAC + other | 11 | 18 | 9 | 53 | |
| AZA without CYA | 0 | 0 | 0 | 0 | |
| Steroids | 0 | 0 | 2 | 12 | |
| Other | 2 | 3 | 0 | 0 | |
| NA | 14 | 23 | 0 | 0 | |
| Maintenance immunosuppression at the time of the PTLD diagnosis | CYA ± AZA | 32 | 52 | 6 | 35 |
| TAC + other | 15 | 24 | 9 | 53 | |
| AZA without CYA | 2 | 3 | 1 | 6 | |
| Steroids | 4 | 6 | 1 | 6 | |
| Other | 2 | 3 | 0 | 0 | |
| NA | 7 | 11 | 0 | 0 | |
| Age at death, years | Median | 63 | – | 63 | – |
| Mean | 59 | – | 57 | – | |
| Range | 24–82 | – | 42–66 | – | |
| Follow up duration on months since transplantation | Median | 141 | – | 33 | – |
| Mean | 151 | – | 37 | – | |
| Range | 19–283 | – | 6–63 | – | |
AZA without CYA = azathioprine without ciclosporin; CYA ± AZA = ciclosporin with or without azathioprine; DLBCL = diffuse large B-cell lymphoma; EBV = Epstein-Barr virus; IPI = International Prognostic Index; NA = not available; PCR = polymerase chain reaction; PTLD = post-transplant lymphoproliferative disorder; STCS = Swiss Transplant Cohort Study; TAC + other = tacrolimus with other immunosuppression
After 1 year, 0.22% (95% confidence interval [CI] 0.09–0.53%) of STCS patients were diagnosed with PTLD and at 5 years 0.96% (95% CI 0.52–1.80%, fig. 1) were diagnosed.
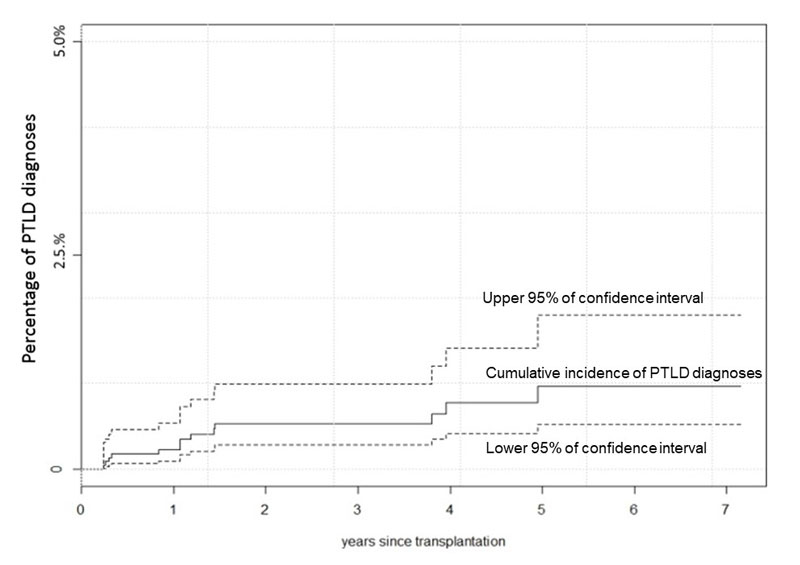
Figure 1 Post-transplant lymphoproliferative disorder cumulative incidence rate according to time after transplantation for solid organ transplant patients in the Swiss Transplant Cohort Study.
For the pre-STCS case series, the exact number of transplanted patients and their survival is unknown since not all cases were recorded. Therefore, we do not know the incidence rate of PTLD for this cohort, nor any effects of potential risk factors. For the STCS cohort, it was not possible to calculate the incidence rate because of the low number of cases.
In both cohorts the majority of cases were monomorphic (76% for pre-STCS and 59% for the STCS) or polymorphic (13% for pre-STCS and 41% for the STCS) subtypes (table 2). The high variability may be in part explained by underreporting of early stage PTLD that resolves with reduction of immunosuppression alone [21]. Seventy-nine percent of the monomorphic PTLDs were diffuse large B-cell lymphoma (DLBCL) in the pre-STCS case-series and 69% for the STCS.
The EBV serostatus D/R (donor/recipient) in the STCS period was known in only 13/17 patients, and was D+/R+ in 11 patients and D+/R− in 2 cases. Sufficient PTLD tissue was available for analysis of EBV status (by means of EBER in situ hybridisation) in 68 cases of both cohorts (table 2). For early-onset PTLDs (PTLD diagnosed before 1 year after the transplant), 100% were EBV positive in the pre-STCS case series and 86% in the STCS (table 3). For late-onset PTLDs (PTLD diagnosed more than 1 year after the transplant) at least 34% of patients with an identifiable EBV status were EBV positive in the pre-STCS and at least 80% for STCS patients (table 3).
Table 3 Early versus late onset post-transplant lymphoproliferative disorder (PTLD).
| Cohort | Pre-STCS | STCS | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Onset of PTLD | Early | Late | Early | Late | |||||
| Absolute no. | % of early | Absolute no. | % of late | Absolute no. | % of early | Absolute no. | % of late | ||
| Total | 9 | 15 | 53 | 85 | 7 | 41 | 10 | 59 | |
| PTLD in organ transplant | 3 | 33 | 3 | 6 | 4 | 57 | 2 | 20 | |
| Immunosuppressant at PTLD diagnosis | CYA ± AZA | 7 | 78 | 25 | 47 | 3 | 43 | 3 | 30 |
| TAC + other | 2 | 22 | 13 | 25 | 2 | 29 | 7 | 70 | |
| AZA without CYA | 0 | 0 | 2 | 4 | 1 | 14 | 0 | 0 | |
| Steroids | 0 | 0 | 4 | 8 | 1 | 14 | 0 | 0 | |
| Other | 0 | 0 | 2 | 4 | 0 | 0 | 0 | 0 | |
| NA | 0 | 0 | 7 | 13 | 0 | 0 | 0 | 0 | |
| Histology subtype | Early | 0 | 0 | 2 | 4 | 0 | 0 | 0 | 0 |
| Polymorphic | 3 | 33 | 4 | 8 | 3 | 43 | 4 | 40 | |
| Monomorphic | 6 | 67 | 42 | 79 | 4 | 57 | 6 | 60 | |
| Hodgkin’s disease | 0 | 0 | 5 | 9 | 0 | 0 | 0 | 0 | |
| Latency PTLD diagnosis to death in months | Median | 38 | – | 63 | – | 63 | – | 62 | – |
| Mean | 38 | – | 61 | – | 58 | – | 58 | – | |
| Range | 24–51 | – | 36–82 | – | 42–64 | – | 43–66 | – | |
| Total duration of follow up since TPL in months | Median | 83 | – | 150 | – | 23 | – | 47 | – |
| Mean | 97 | – | 160 | – | 25 | – | 46 | – | |
| Range | 19–189 | – | 20–310 | – | 6–59 | – | 30–63 | – | |
| Outcome at the end of the follow up | Dead | 2 | 22 | 9 | 17 | 4 | 57 | 3 | 30 |
| Alive | 5 | 56 | 26 | 49 | 0 | 0 | 1 | 10 | |
| NA | 2 | 22 | 18 | 34 | 3 | 43 | 6 | 60 | |
| Tumour EBV status | Positive | 9 | 100 | 18 | 34 | 6 | 86 | 8 | 80 |
| Negative | 0 | 0 | 26 | 49 | 0 | 0 | 1 | 10 | |
| Insufficient data | 0 | 0 | 9 | 17 | 1 | 14 | 1 | 10 | |
AZA without CYA = azathioprine without ciclosporin; CYA ± AZA = ciclosporin with or without azathioprine; DLBCL = diffuse large B-cell lymphoma; EBV = Epstein-Barr virus NA = not available; STCS = Swiss Transplant Cohort Study; TAC + other = tacrolimus with other immunosuppression; TPL = transplantation
Early onset PTLD more often involved the transplanted organ (in 33% of early onset PTLDs for the pre-STCS and in 57% of early PTLD for the STCS, table 3) and were more often associated with the use of calcineurin inhibitors such as ciclosporin and tacrolimus (in 100% of early PTLD for the pre-STCS and in 72% of early PTLD for the STCS). In both early and late onset, monomorphic subtypes were most common, but in the early-onset PTLD the proportion of polymorphic subtypes was higher than in late onset PTLDs in the pre-STCS case series (table 3).
In the pre-STCS case series, median survival was shorter in patients with early-onset PTLD (38 months) than in patients with late onset PTLD (63 months), in contrast to the STCS cohort where they were about equal (table 3). However, the follow-up for the STCS cohort was significantly shorter (table 2). Despite incomplete data for the pre-STCS cohort, the percentage of patients who had died at the end of the follow up was 17% for patients with early-onset PTLD and 22% for patients with late-onset PTLD, which was not notably different (table 3). Furthermore, owing to shorter follow-up of STCS- patients and the low number or patients, survival in early and late onset PTLD cannot be compared with pre-STCS-patients.
Data of induction immunosuppression at time of transplantation was reported only for STCS patients. In this cohort, 11 patients (65%) received basiliximab, 4 patients (23%) received antithymocyte globulin (ATG), 1 patient (6%) received ATG and intravenous immunoglobulin (IVIG) and 1 patient (6%) received basiliximab and ATG.
Initial maintenance immunosuppression at the time of transplantation included a calcineurin inhibitor (ciclosporin and tacrolimus) for at least 74% of the pre-STCS case series and in 88% of the STCS patients (table 2).
At the time of PTLD occurrence, 76% of patients of the pre-STCS case series and 88% of the patients of the STCS were on calcineurin inhibitors (table 2).
For the pre-STCS case series, the median follow-up after PTLD diagnosis was 141 months with a range of 19 to 283 months (table 2). This follow-up continued even during the STCS period. However, the median follow-up for the STCS cohort starting in May 2008, was only of 33 months (range 6–63).
The overall survival rates at 1, 5 and 10 years after diagnosis were of 80% (95% CI 68–87%), 56% (95% CI 42–68%) and 51% (95% CI 37–63%), respectively, for the two cohorts (fig. 2). However, the median age at death was similar, 63 years, for the pre-STCS and STCS cohorts (table 2).
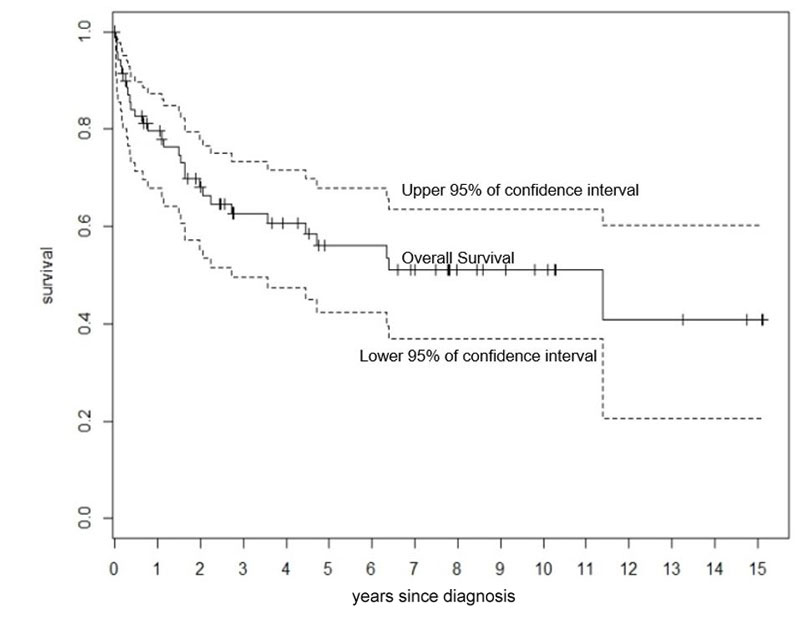
Figure 2 Overall Survival from post-transplant lymphoproliferative disorder diagnosis for both cohorts combined.
There was no censoring at any time and no loss to follow up. We did not censor any graft loss patient.
In this study, we found for the STCS cohort (between 2008 and 2014) a low cumulative incidence of PTLD in Switzerland, with only 0.96% at 5 years, irrespective of the type of organ that was transplanted. Our findings are at variance with other studies that have described higher cumulative incidences of PTLD, as quoted in numerous national trials and large cohorts.
In a population-based cohort study in Denmark between 1990 and 2011, Maksten et al. found a cumulative incidence of 1.4% at 5 years in renal transplants [17]. However, this study differed from ours by including young patients, with 17.1% being less than 17 years old. Paediatric patients are known to have a higher incidence of PTLD, because of the higher rate of EBV seronegativity in this population [22]. This could partly explain the difference of cumulative incidence between studies. In another study including 1,206 recipients of liver transplants between 1985 and 2004 at a single institution, 37 recipients developed a PTLD and Kremers et al. found a cumulative incidence of 2.1% at 5 years [23]. In contrast, the STCS surprisingly has only 1 liver recipient with PTLD, possibly owing to late onset PTLD after liver transplants and shorter follow-up of the SCTS cohort. Moreover, in the Kremers study, 16 and 32% of the patients were treated with the monoclonal antibody muromonab OKT3 and with high-dose steroids, which is known to be a significant risk factor for the development of PTLD. In a retrospective analysis between 1991 and 2011, Kremer et al. found a 5-year cumulative incidence of PTLD of 5.9% in lung transplant recipients [24]. They observed that the PTLD incidence decreased between 1991 and 2011: Between 2001 and 2011, the annual incidence of PTLD after transplantation ranged from 0 to 3%. A decrease of PTLD incidence over time, which could at least in part explain the low cumulative incidence of PTLD in our study, was also observed by Kumarasinghe et al. in a retrospective study between 1984 and 2013 including 70 heart and lung recipients [25]. It is noteworthy that the incidence of PTLD tends to be higher in thoracic organ transplant recipients who have long-term profound immunosuppression required to prevent the more serious consequences of transplant rejection. In the thoracic organ transplant cohort of Kumarasinghe et al., the incidence of PTLD was 7.2% between 1984 and 1990 but only 1.99% between 2006 and 2010. This decrease was attributed to changing induction immunosuppression protocols, particularly avoiding T cell-depleting therapy (i.e., ATG).
The relationship between maintenance therapy and PTLD remains a matter of debate in the literature [26–28]. In our study, as maintenance immunosuppression at the time of transplantation, 74% of the pre-STCS case-series and 88% of the STCS patients were receiving calcineurin inhibitors (ciclosporin and tacrolimus) and 76% and 88%, respectively, at the time of PTLD diagnosis (table 2). Moreover, the agents used for maintenance immunosuppression have changed over time (for instance, using tacrolimus instead of ciclosporin), had a heterogeneous pattern reflecting among other factors the different organs transplanted, and the intensity of the immunosuppression could not be reported reliably in the retrospective setting. Consequently, we could not identify significantly the correlation between the type of maintenance and the development of PTLD.
The low cumulative incidence at 5 years might as well reflect the efforts made to minimise the number of EBV negative recipients with EBV donors. According to the study directed by Walker et al. [29], the incidence rate of PTLD for EBV-seronegative recipients is 24 times higher than in EBV-seropositive recipients. In our patients, the interpretation of the EBV serology status was not possible in the pre-STCS case-series, due to incomplete data. The STCS cohort included in total 2,621 patients with a SOT in the period of time studied. But only 13 patients with a PTLD met the inclusion criteria. Those 13 PTLD cases had either a positive-positive or negative-positive recipient/donor EBV status, which emphasised the importance in prevention of screening and matching correctly the EBV status, which can be a difficult or impossible task if there is a scarcity of organ donors.
As final comment regarding the low cumulative incidence of PTLD at 5 years in the STCS cohort, it is unclear if the cumulative incidence for the same cohort is also lower at 10 years, or even later. Indeed, the median follow-up after transplantation was only 33 months in the STCS cohort (table 1), which is a limitation. According the data of Maksten et al., the incidence of PTLD after kidney transplantation changed over time, showing a bimodal pattern with highest incidence rates in the first year and more than 10 years after transplantation [17]. Nevertheless, the incidence of PTLD differs with the organ transplanted. According to Kumarasinghe et al., the median time from heart and lung transplantation to PTLD diagnosis is only 3.2 years, probably due to higher immunosuppression required for transplanted thoracic organs [25].
Interestingly, the comparison of the two cohorts show that the median age at transplantation and the median age at death are almost the same. In contrast, the median age at PTLD diagnosis was 53 years for the patients of the pre-STCS and 45 years for the patients of the STCS cohort (table 2). We speculate that earlier detection of the PTLD could be attributed to a better awareness and better clinical and radiological screening for PTLD among SOT patients. Furthermore, many transplant centres have incorporated EBV monitoring into the routine follow-up evaluation of patients at high risk for PTLD [30]. However, this difference of age at the time of PTLD diagnosis could be in part the result of underreporting of early PTLD disorders that can be treated with reduction of immunosuppression only in the pre-STCS case series.
The 5-year overall survival of the pre-STCS and STCS combined was 56%, which is superior to the 48% reported in an Irish retrospective study between 1991 and 2010 of kidney transplant recipient patients with a PTLD diagnosis [31]. Unfortunately, our study did not have enough patients either for a statistical evaluation of mortality or to explain why a group of patients diagnosed earlier with a PTLD presents a similar median age at death as a group of patients diagnosed later. If the median age of death is the same, the cause of death was probably different. Putatively, some deaths were not related to the PTLD diagnosis but to other causes, such as infections. This aspect could not be elucidated in this study.
This study had strengths. Firstly, it was a nationwide cohort study of PTLD in Switzerland. Secondly, our patient series was considerable, including 79 cases of PTLD. Thirdly, our follow-up was extensive for the pre-STCS case-series with a median of 11.6 years.
In conclusion, we found at 5 years a cumulative incidence of PTLD, disregarding any type of organ transplanted, of only 0.96% between 2008 and 2014 in Switzerland, which is lower than described in the literature. We speculate that reduction of the risk factors such as notably reducing the recipient/donor EBV mismatch by allocating EBV negative transplants to EBV negative recipients and the usage of less T cell immunosuppression led to those results. Secondly, the two successive cohorts show that PTLD tends to be diagnosed earlier, possibly owing to a better identification of the disease. However, the median age at death stayed the same. The causes of death and the reason for the decline in incidence of PTLD over time could not be clarified by this study. Open questions need to be answered with further studies of larger cohorts to improve our understanding of PTLD occurrence and development in transplant patients.
This study was conducted in the framework of the Swiss Transplant Cohort Study, supported by the Swiss National Science Foundation and the Swiss University Hospitals (G15) and transplant centres. R. Steiner declares having received 8500 CHF from the Swiss Transplant Cohort Study (STCS) for the gathering of the data. The other authors have declared no funding for this study and no conflict of interest.
1 Engels EA , Pfeiffer RM , Fraumeni JF, Jr , Kasiske BL , Israni AK , Snyder JJ , et al. Spectrum of cancer risk among US solid organ transplant recipients. JAMA. 2011;306(17):1891–901. doi:.https://doi.org/10.1001/jama.2011.1592
2 Morscio J , Tousseyn T . Recent insights in the pathogenesis of post-transplantation lymphoproliferative disorders. World J Transplant. 2016;6(3):505–16. doi:.https://doi.org/10.5500/wjt.v6.i3.505
3 Penn I . Cancers complicating organ transplantation. N Engl J Med. 1990;323(25):1767–9. doi:.https://doi.org/10.1056/NEJM199012203232510
4 Petrara MR , Giunco S , Serraino D , Dolcetti R , De Rossi A . Post-transplant lymphoproliferative disorders: from epidemiology to pathogenesis-driven treatment. Cancer Lett. 2015;369(1):37–44. doi:.https://doi.org/10.1016/j.canlet.2015.08.007
5 Kotton CN , Fishman JA . Viral infection in the renal transplant recipient. J Am Soc Nephrol. 2005;16(6):1758–74. doi:.https://doi.org/10.1681/ASN.2004121113
6 Tiede C , Maecker-Kolhoff B , Klein C , Kreipe H , Hussein K . Risk factors and prognosis in T-cell posttransplantation lymphoproliferative diseases: reevaluation of 163 cases. Transplantation. 2013;95(3):479–88. doi:.https://doi.org/10.1097/TP.0b013e3182762e07
7 Swerdlow SH , Campo E , Pileri SA , Harris NL , Stein H , Siebert R , et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–90. doi:.https://doi.org/10.1182/blood-2016-01-643569
8 Swerdlow SH , Campo E , Pileri SA , Harris NL , Stein H , Siebert R , et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–90. doi:.https://doi.org/10.1182/blood-2016-01-643569
9 Shapiro R , Scantlebury VP , Jordan ML , Vivas C , Tzakis AG , Ellis D , et al. FK506 in pediatric kidney transplantation--primary and rescue experience. Pediatr Nephrol. 1995;9(S1, Suppl):S43–8. doi:.https://doi.org/10.1007/BF00867683
10 Funch DP , Walker AM , Schneider G , Ziyadeh NJ , Pescovitz MD . Ganciclovir and acyclovir reduce the risk of post-transplant lymphoproliferative disorder in renal transplant recipients. Am J Transplant. 2005;5(12):2894–900. doi:.https://doi.org/10.1111/j.1600-6143.2005.01115.x
11 Tsai DE , Hardy CL , Tomaszewski JE , Kotloff RM , Oltoff KM , Somer BG , et al. Reduction in immunosuppression as initial therapy for posttransplant lymphoproliferative disorder: analysis of prognostic variables and long-term follow-up of 42 adult patients. Transplantation. 2001;71(8):1076–88. doi:.https://doi.org/10.1097/00007890-200104270-00012
12 Choquet S , Leblond V , Herbrecht R , Socié G , Stoppa AM , Vandenberghe P , et al. Efficacy and safety of rituximab in B-cell post-transplantation lymphoproliferative disorders: results of a prospective multicenter phase 2 study. Blood. 2006;107(8):3053–7. doi:.https://doi.org/10.1182/blood-2005-01-0377
13 Taylor AL , Bowles KM , Callaghan CJ , Wimperis JZ , Grant JW , Marcus RE , et al. Anthracycline-based chemotherapy as first-line treatment in adults with malignant posttransplant lymphoproliferative disorder after solid organ transplantation. Transplantation. 2006;82(3):375–81. doi:.https://doi.org/10.1097/01.tp.0000228906.31675.fb
14 Koffman BH , Kennedy AS , Heyman M , Colonna J , Howell C . Use of radiation therapy in posttransplant lymphoproliferative disorder (PTLD) after liver transplantation. Int J Cancer. 2000;90(2):104–9. doi:.https://doi.org/10.1002/(SICI)1097-0215(20000420)90:2<104::AID-IJC6>3.0.CO;2-0
15 https://www.swisstransplant.org/en/swisstransplant/publications/annual-figures. Accessed 13 October 2016.
16 http://www.stcs.ch/internal/reports/2015_11_19_final_stcs_annual.pdf Accessed 13 October 2016.
17 Maksten EF , Vase MØ , Kampmann J , d’Amore F , Møller MB , Strandhave C , et al. Post-transplant lymphoproliferative disorder following kidney transplantation: a population-based cohort study. Transpl Int. 2016;29(4):483–93. doi:.https://doi.org/10.1111/tri.12744
18 International Non-Hodgkin’s Lymphoma Prognostic Factors Project. A predictive model for aggressive non-Hodgkin’s lymphoma. N Engl J Med. 1993;329(14):987–94. doi:.https://doi.org/10.1056/NEJM199309303291402
19Swisstransplant. Annual reports. https://www.swisstransplant.org/fr/swisstransplant/publications/rapports-annuels/ Accessed on: 12 June 2016.
20Koller M, Stampf S, Rick J, Bianco S, Branca S, Achermann R, et al.; on behalf of the STCS. Swiss Transplant Cohort Study report (May 2008 – December 2016). Available at: http://www.stcs.ch/internal/documents/stcs_annual_report_june_2017.pdf. Accessed on: 15 September 2017
21 Mynarek M , Schober T , Behrends U , Maecker-Kolhoff B . Posttransplant lymphoproliferative disease after pediatric solid organ transplantation. Clin Dev Immunol. 2013;2013:814973. doi:.https://doi.org/10.1155/2013/814973
22 McDonald RA , Smith JM , Ho M , Lindblad R , Ikle D , Grimm P , et al.; CCTPT Study Group. Incidence of PTLD in pediatric renal transplant recipients receiving basiliximab, calcineurin inhibitor, sirolimus and steroids. Am J Transplant. 2008;8(5):984–9. doi:.https://doi.org/10.1111/j.1600-6143.2008.02167.x
23 Kremers WK , Devarbhavi HC , Wiesner RH , Krom RA , Macon WR , Habermann TM . Post-transplant lymphoproliferative disorders following liver transplantation: incidence, risk factors and survival. Am J Transplant. 2006;6(5 Pt 1):1017–24. doi:.https://doi.org/10.1111/j.1600-6143.2006.01294.x
24 Kremer BE , Reshef R , Misleh JG , Christie JD , Ahya VN , Blumenthal NP , et al. Post-transplant lymphoproliferative disorder after lung transplantation: a review of 35 cases. J Heart Lung Transplant. 2012;31(3):296–304. doi:.https://doi.org/10.1016/j.healun.2011.10.013
25 Kumarasinghe G , Lavee O , Parker A , Nivison-Smith I , Milliken S , Dodds A , et al. Post-transplant lymphoproliferative disease in heart and lung transplantation: Defining risk and prognostic factors. J Heart Lung Transplant. 2015;34(11):1406–14. doi:.https://doi.org/10.1016/j.healun.2015.05.021
26 Bichari W , Bartiromo M , Mohey H , Afiani A , Burnot A , Maillard N , et al. Significant risk factors for occurrence of cancer after renal transplantation: a single center cohort study of 1265 cases. Transplant Proc. 2009;41(2):672–3. doi:.https://doi.org/10.1016/j.transproceed.2008.12.013
27 Pourfarziani V , Taheri S , Lessan-Pezeshki M , Nourbala MH , Simforoosh N , Nemati E , et al. Lymphoma after living donor kidney transplantation: an Iranian multicenter experience. Int Urol Nephrol. 2008;40(4):1089–94. doi:.https://doi.org/10.1007/s11255-008-9377-0
28 Bustami RT , Ojo AO , Wolfe RA , Merion RM , Bennett WM , McDiarmid SV , et al. Immunosuppression and the risk of post-transplant malignancy among cadaveric first kidney transplant recipients. Am J Transplant. 2004;4(1):87–93. doi:.https://doi.org/10.1046/j.1600-6135.2003.00274.x
29 Walker RC , Marshall WF , Strickler JG , Wiesner RH , Velosa JA , Habermann TM , et al. Pretransplantation assessment of the risk of lymphoproliferative disorder. Clin Infect Dis. 1995;20(5):1346–53. doi:.https://doi.org/10.1093/clinids/20.5.1346
30 Tsai DE , Douglas L , Andreadis C , Vogl DT , Arnoldi S , Kotloff R , et al. EBV PCR in the diagnosis and monitoring of posttransplant lymphoproliferative disorder: results of a two-arm prospective trial. Am J Transplant. 2008;8(5):1016–24. doi:.https://doi.org/10.1111/j.1600-6143.2008.02183.x
31 OʼRegan JA , Prendeville S , McCaughan JA , Traynor C , OʼBrien FJ , Ward FL , et al. Posttransplant Lymphoproliferative Disorders in Irish Renal Transplant Recipients: Insights From a National Observational Study. Transplantation. 2017;101(3):657–63. doi:.https://doi.org/10.1097/TP.0000000000001201
This study was conducted in the framework of the Swiss Transplant Cohort Study, supported by the Swiss National Science Foundation and the Swiss University Hospitals (G15) and transplant centres. R. Steiner declares having received 8500 CHF from the Swiss Transplant Cohort Study (STCS) for the gathering of the data. The other authors have declared no funding for this study and no conflict of interest.