Overuse of antimicrobial prophylaxis in low-risk patients undergoing transurethral resection of the prostate
DOI: https://doi.org/10.4414/smw.2018.14594
Kathrin
Bauschab, Jan A.
Rothbc, Hans-H.
Seifertab, Andreas F.
Widmerbc
aDepartment of Urology, University Hospital Basel, Switzerland
bUniversity of Basel, Switzerland
cDivision of Infectious Diseases and Hospital Epidemiology, University Hospital and University of Basel, Switzerland
Summary
OBJECTIVE
To evaluate the current antimicrobial prophylaxis practices for low-risk patients undergoing transurethral resection of the prostate (TURP) or photoselective vaporisation of the prostate (PVP) in comparison with the antimicrobial prophylaxis recommendations of the European Association of Urology (EAU), which have been shown to effectively reduce infectious complications and antimicrobial resistance rates.
METHODS
In May 2017, we sent an anonymous online -survey to board-certified urologists in Germany, Austria and Switzerland, by use of the database directory of the respective urology associations. Besides demographical questions, urologists were asked about their sources of information on antimicrobial prophylaxis prescription and their prescribing patterns before, during and after surgery in patients without an indwelling catheter or significant bacteriuria undergoing TURP or PVP.
RESULTS
Overall, 374 of 5825 urologists responded, of whom 76% (286/374) performed TURP and 16% (60/374) PVP. For TURP and PVP, respectively: (i) 42% (119/286) and 33% (20/60) reported routine use of preoperative antimicrobial prophylaxis, which does not conform to guideline recommendations; (ii) 43% (124/286) and 52% (31/60) reported prescribing non-recommended perioperative antimicrobial prophylaxis regimens; and (iii) 60% (172/286) and 65% (39/60) routinely extended antimicrobial prophylaxis after surgery for up to one week. In summary, of the urologists who responded to the questionnaire, 74% (211/286) reported nonadherence to guidelines on antimicrobial prophylaxis for TURP.
CONCLUSION
A low adherence to guidelines for low-risk patients undergoing TURP or PVP was reported. Given these preliminary data, there is an urgent need to monitor adherence to antimicrobial prophylaxis guidelines in urology to reduce antimicrobial resistance rates.
Introduction
Transurethral resection of the prostate (TURP) is a frequent urological procedure, with single-dose antimicrobial prophylaxis being routinely recommended to reduce postoperative urinary tract infections. Antimicrobial prophylaxis is ideally administered as a single dose of trimethoprim/sulfamethoxazole (TMP/SMX), an amino-penicillin or a cephalosporin [1, 2]. Photoselective vaporisation of the prostate (PVP) has become an important alternative to TURP, especially for patients taking platelet aggregation inhibitors or oral anticoagulants [3], but no international recommendations for antimicrobial prophylaxis have, so far, been established for PVP. Remarkably, little is known about antimicrobial prophylaxis prescribing patterns in TURP and PVP in routine clinical practice. Furthermore, the frequency of antimicrobial resistance in urological patients is much higher than for patients in other departments, possibly through inappropriate use of antimicrobial agents and prolonged prophylaxis [4]; this may apply in particular to low-risk patients without indwelling urinary catheters and/or significant bacteriuria.
By applying the antimicrobial prophylaxis recommendations of the European Association of Urology (EAU), we aimed to differentiate current antimicrobial prophylaxis practices among urologists for low-risk patients undergoing TURP or PVP.
Methods
In May 2017, we sent an anonymous online questionnaire to all board-certified urologists in Germany, Austria and Switzerland by means of the database directory of the respective urology associations; a reminder of participation was sent 2 weeks later to nonrespondents. Besides demographic questions, urologists were asked about their sources of information on antimicrobial prophylaxis prescription (multiple answers). Questions regarding prescribing patterns pre-, peri- and postoperatively in patients without indwelling catheter or significant bacteriuria undergoing TURP or PVP were included (single answer). Perioperative antimicrobial prophylaxis was defined as a prophylactic regimen administered ≤60 minutes before surgical incision (and possibly continued during surgery), with preoperative and postoperative prophylaxis being administered >60 minutes before surgical incision and at any time point after completion of surgery, respectively. In accordance with the EAU guidelines, we defined guideline adherence as a single dose of TMP/SMX, an amino-penicillin or a cephalosporin administered ≤60 minutes before surgical incision (and possibly continued during surgery). Nonadherence was defined as any other prophylaxis agent routinely given perioperatively, as well as preoperative and postoperative antimicrobial prophylaxis administered >60 minutes before surgical incision and at any time-point after completion of surgery. Only fully completed questionnaires were included in the final analysis.
Results
A total 5825 urologists received the online questionnaire; 6.4% (374/5825) completed the survey. The majority of urologists worked at university hospitals (30%, 111/374) with most of the participants having worked as a urologist for 10 to 19 years (28%, 106/374); 76% (286/374) performed TURP and 16% (60/374) PVP. For TURP and/or PVP, 64% (241/374) of urologists primarily used international guidelines as a basis for antimicrobial prophylaxis recommendations, followed by in-house guidelines (52%, 194/374), local resistance rates (36%, 133/374) and experience (29%, 108/374).
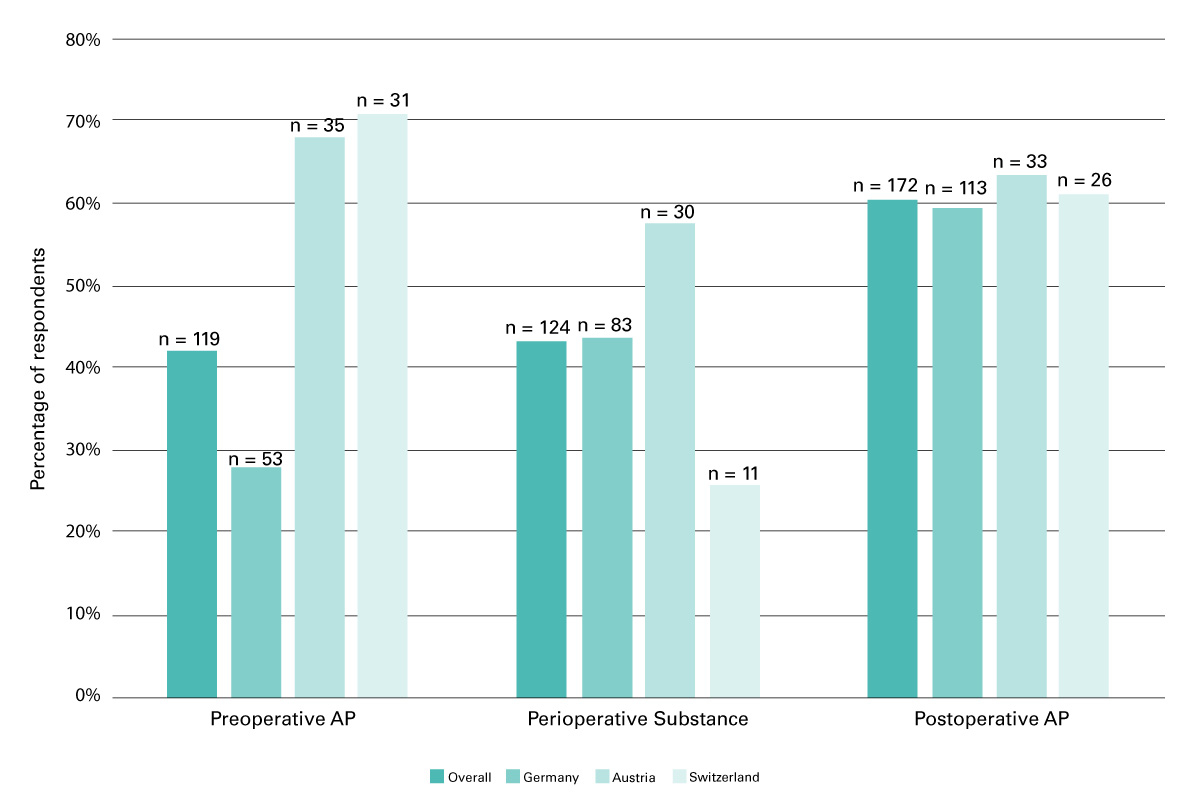
The overall rate of nonadherence to EAU guidelines for TURP was 74% (211/286). For each TURP and PVP, 42% (119/286) and 33% (20/60) of the respondents reported routine use of preoperative antimicrobial prophylaxis, which is not recommended; 43% (124/286) and 52% (31/60) reported prescribing non-recommended perioperative prophylaxis regimens (defined as substances other than TMP/SMX, an amino-penicillin or a cephalosporin), and 60% (172/286) and 60% (36/60) routinely continued the prophylaxis after surgery, which is not recommended by current guidelines (fig. 1).
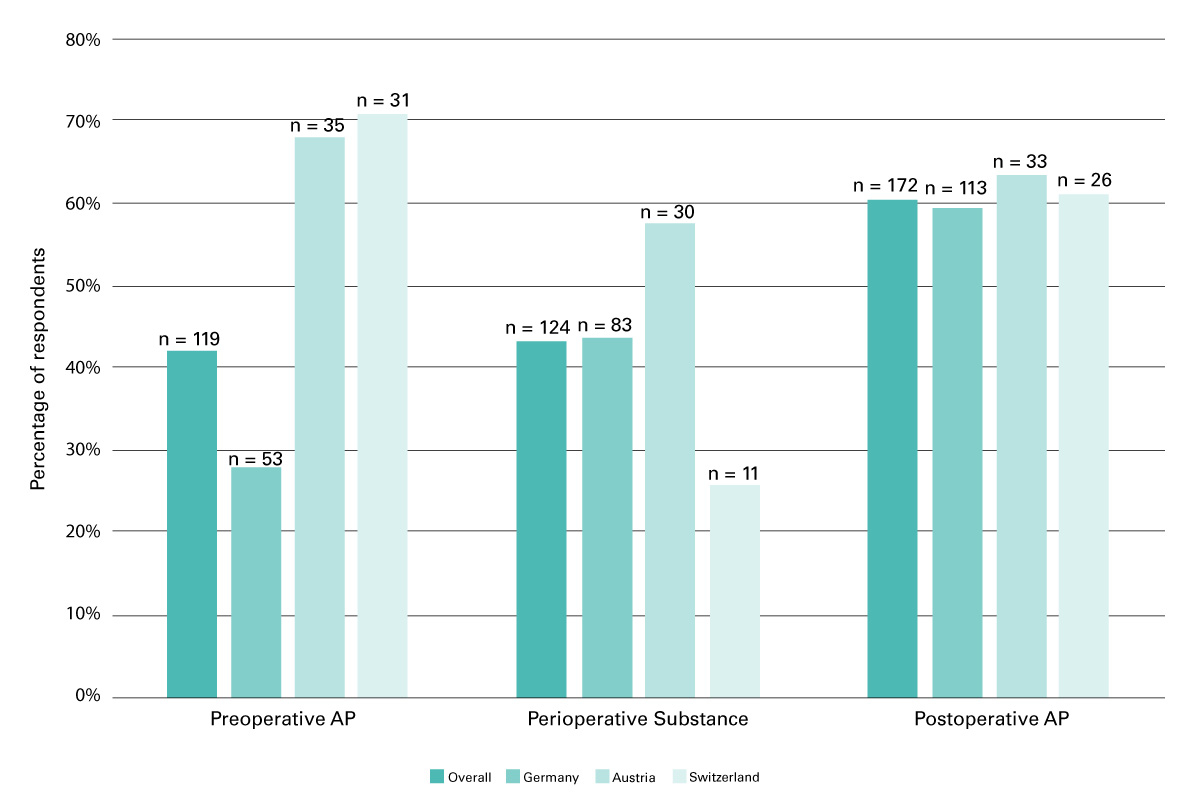
Figure 1
Nonadherence to the European Association of Urology (EAU) guidelines for pre-, peri- and postoperative antimicrobial prophylaxis (AP) in low-risk patients undergoing transurethral resection of the prostate; survey results (n = 286 urologists). Overall, 42% (119/286) of urologists routinely used preoperative antimicrobial prophylaxis, 43% (124/286) prescribed non-recommended perioperative prophylaxis agents, and 60% (172/286) routinely extended prophylaxis after surgery. In contrast to postoperative use, nonadherence rates for pre- and perioperative antimicrobial prophylaxis differed significantly between Germany, Austria and Switzerland (p = 0.853 vs p <0.001 and p = 0.007; chi-squared test).
In all three countries, noncompliance rates did not significantly differ between university hospitals (72%, 80/111) and non-university hospitals (75%, 196/263) (p = 0.622).
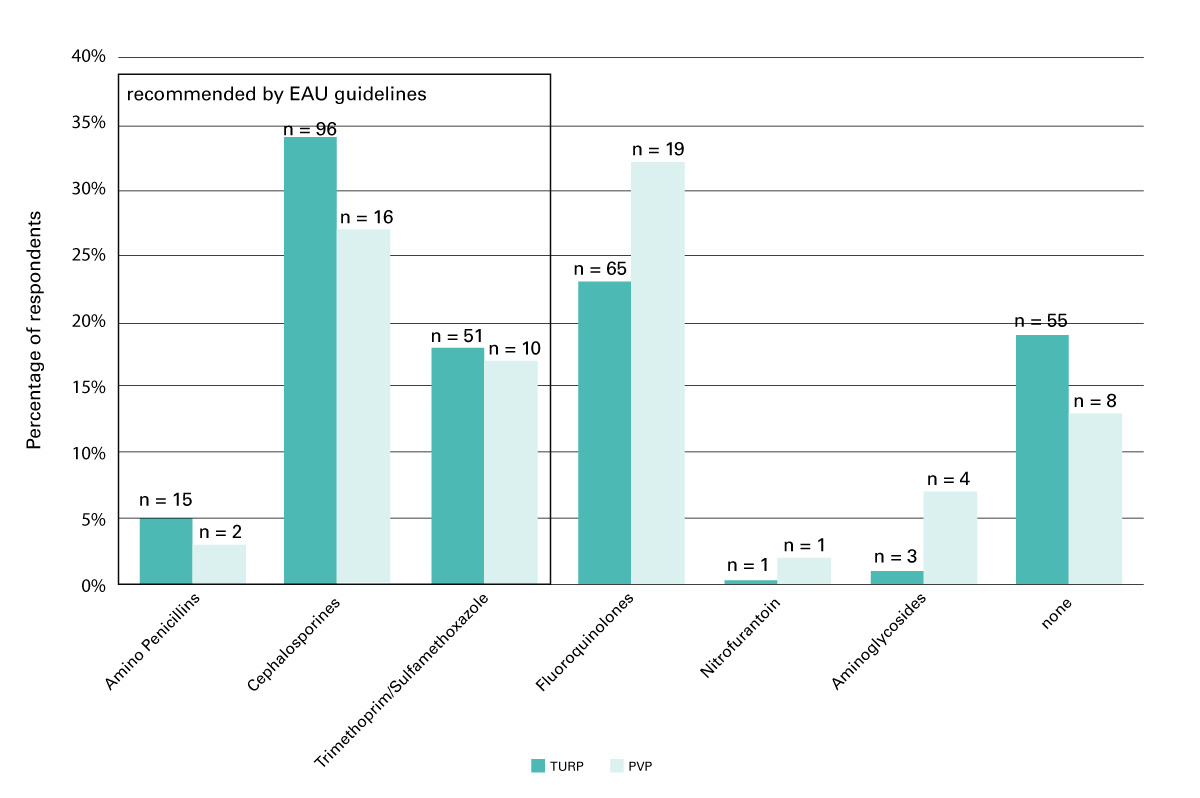
Among all participating urologists, cephalosporins were the most frequently chosen agents for perioperative antimicrobial prophylaxis (34%, 96/286), followed by fluoroquinolones (23%, 65/286), TMP/SMX (18%, 51/286) and amino-penicillins (5%, 15/286). Interestingly, 19% (55/286) of urologists reported using perioperative antimicrobial prophylaxis (fig. 2). In Switzerland, TMP/SMX was the most commonly used regimen (63%, 27/43), whereas in Germany and Austria cephalosporins were preferred (41%, 78/191; 27%, 14/52). In PVP, fluoroquinolones were primarily chosen, by 32% (19/60) of the participating urologists. In total, in TURP, 43% (124/286) of urologists reported prescribing non-recommended perioperative prophylaxis regimens (fig. 1); in PVP, 52% (31/60) did not prescribe any prophylaxis regimen, which is in line with the EAU guidelines on TURP.
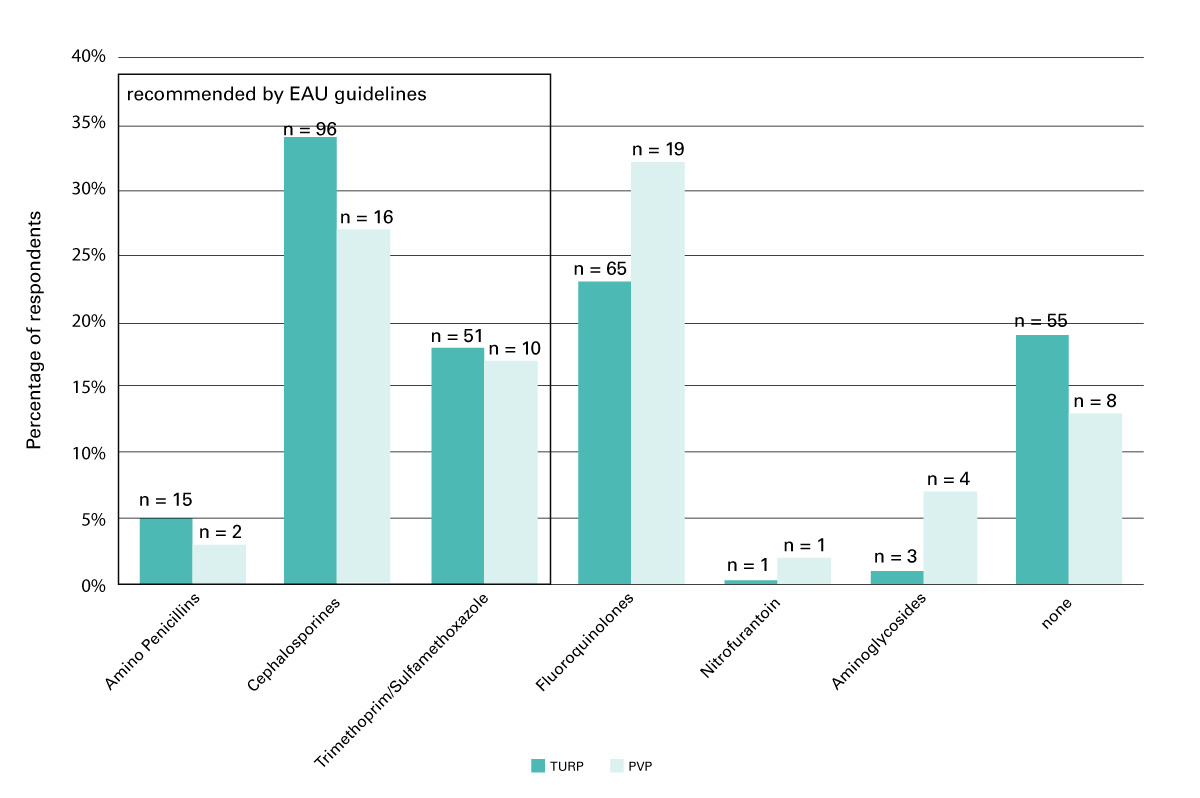
Figure 2
Perioperative antimicrobial prophylactic regimens. Despite the guidelines of the European Association of Urology (EAU), fluoroquinolones (23%, 65/286) were second choice in transurethral resection of the prostate (TURP; 23%, 65/286) and first choice in photoselective vaporisation of the prostate (PVP; 32%, 19/60).
In TURP and PVP, fluoroquinolones were the most frequently chosen preoperative antimicrobial prophylaxis agents (12%, 35/286; 22%, 13/60).
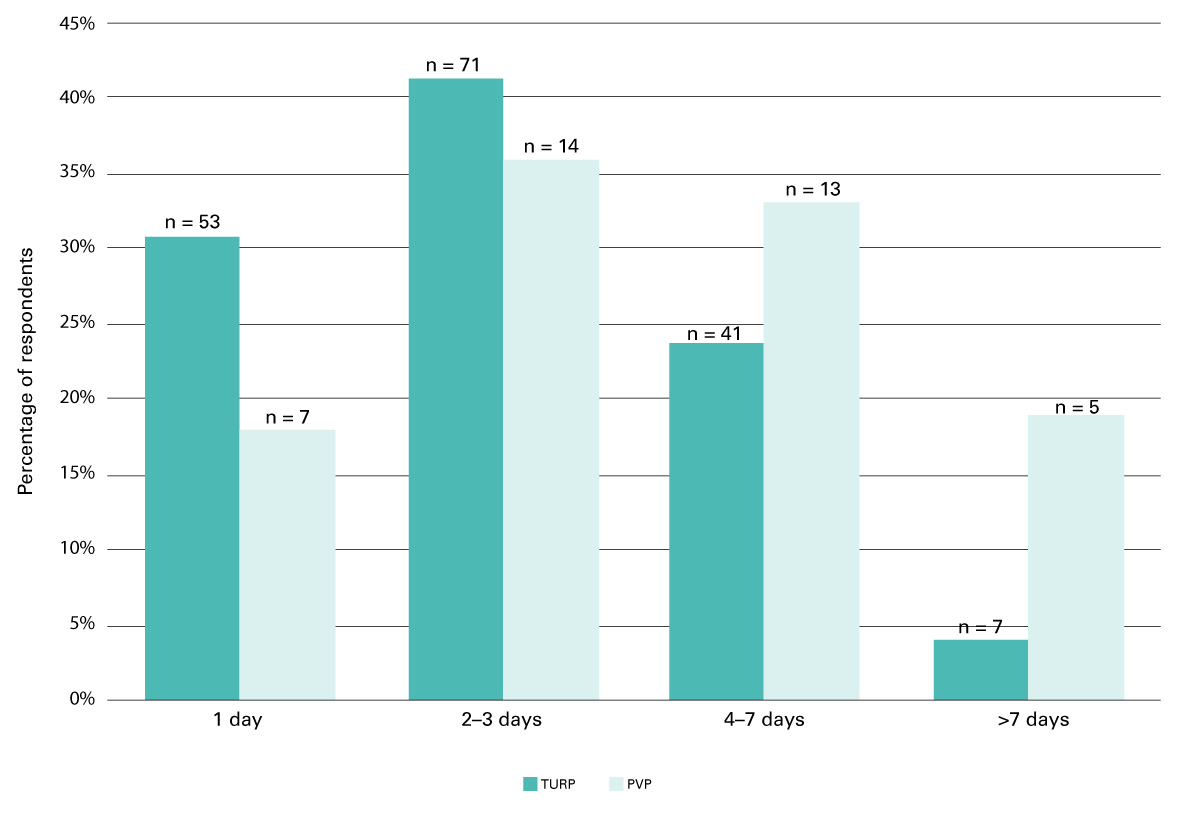
Furthermore, 60% (172/286) and 65% (39/60) of urologists extended antimicrobial prophylaxis after TURP and PVP, respectively (fig. 1). Reported reasons for prolonged prophylaxis were prostate volume over 30 g, intraoperative findings such as opening of venous sinus and operation duration of more than 1 hour. Antimicrobial prophylaxis was predominantly given for additional 2–3 days (fig. 3).
Postoperatively, fluoroquinolones were most frequently used, in both TURP (38%, 65/172) and PVP (82%, 32/39).
Discussion
In this survey-based study focusing on TURP and PVP in low-risk patients, we have found diverging antimicrobial prophylaxis practices, which were often not recommended by current EAU guidelines [1]. Generally, urine is free from bacteria, but TURP and PVP are performed in mostly elderly patients, often with indwelling transurethral catheters and a history of urinary tract infections or prostatitis [2]. Therefore, TURP has been defined as a “clean-contaminated” intervention according to the World Health Organization [5] and, consequently, routine antimicrobial prophylaxis, ideally administered as a single dose of TMP/SMX, an amino-penicillin or cephalosporin, is recommended by EAU guidelines [1]. Several meta-analyses of randomised controlled clinical trials provided strong evidence that antimicrobial prophylaxis in TURP is effective in reducing postoperative bacteriuria, urinary tract infections and sepsis [6–8].
Almost 15 years ago, a similar survey demonstrated that more than half of urologists used more than one dose of an antimicrobial agent as prophylaxis in patients with an indwelling catheter [9]. Despite ever rising antimicrobial resistance rates, our study results in low-risk patients without preoperative catheter or significant bacteriuria are in line with these findings. Even recent studies show wide variation in terms of antimicrobial prophylaxis duration and regimen, which is in contrast to the EAU guidelines [10].
Even though a single-dose antimicrobial prophylaxis is recommended in TURP, preoperative prophylaxis was regularly used by more than one third of the urologists, postoperative antimicrobial prophylaxis in two thirds, and fluoroquinolones were regularly given pre-, peri- and postoperatively. A prospective study by Wagenlehner et al. showed that the application of fluoroquinolones during urological surgery may increase antimicrobial resistance rates even with a single dose of antimicrobial prophylaxis: Escherichia coli resistance rates to fluoroquinolones before antimicrobial prophylaxis was 3% (3/91) versus 12% (5/42) after single dose prophylaxis (p = 0.052) [11]. Antimicrobial resistance rates to fluoroquinolones correlate with higher consumption [4]. Similarly, resistance rates of Escherichia coli isolated from urological patients are much higher compared with non-urological patients (33 vs 15%, p <0.05) [12].
Whereas studies have shown that adherence to antimicrobial prophylaxis guidelines results in healthcare cost savings [13], recent studies have also demonstrated that adherence to EAU guidelines reduces antimicrobial resistance rates by lowering the total antimicrobial consumption without increasing postoperative infections [14]. Therefore, it is even more alarming that wide overuse of antimicrobial prophylaxis in TURP was demonstrated in our study – even in low-risk patients without a preoperative catheter or significant bacteriuria; the guideline nonadherence may be explained by a lack of awareness of rising antimicrobial resistance rates in urology and its associated complications. Higher compliance with current antimicrobial prophylaxis guidelines may only be achieved by large antibiotic stewardship programmes in these countries.
Our study has limitations. First, it was not based on direct observations, which did not allow accounting for recall and reporting biases. Second, our survey results may not adequately represent antimicrobial prophylaxis practices among German, Austrian and Swiss urologists, as the overall response rate was low (around 6%). However, it is conceivable that compliance with antimicrobial prophylaxis in nonrespondents is not considerably higher than in those respondents who are less interested in this topic.
In conclusion, a low adherence to guidelines for low-risk patients undergoing TURP or PVP was reported. Given this preliminary data, there is an urgent need to monitor adherence to guideline recommendations of antimicrobial prophylaxis in urology.
Acknowledgements
We thank the German, Swiss and Austrian urological association for distribution of the survey. Thanks to Marc Dangel and Stefan Heinz for technical advice.
References
1Bonkat G, Pickard R, Bartoletti R, et al. EAU Guidelines on Urological Infections. Perioperative antibacterial prophylaxis in urology. In: Complete European Association of Urology Guidelines. Edn. presented at the EAU Annual Congress London 2017. 2017. pp 35–9.
2
Reich
O
,
Gratzke
C
,
Bachmann
A
,
Seitz
M
,
Schlenker
B
,
Hermanek
P
, et al.; Urology Section of the Bavarian Working Group for Quality Assurance. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol. 2008;180(1):246–9. http://uroweb.org/guideline/urological-infections/ doi:.https://doi.org/10.1016/j.juro.2008.03.058
3
Ruszat
R
,
Wyler
S
,
Forster
T
,
Reich
O
,
Stief
CG
,
Gasser
TC
, et al.
Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol. 2007;51(4):1031–8, discussion 1038–41. doi:.https://doi.org/10.1016/j.eururo.2006.08.006
4
Blaettler
L
,
Mertz
D
,
Frei
R
,
Elzi
L
,
Widmer
AF
,
Battegay
M
, et al.
Secular trend and risk factors for antimicrobial resistance in Escherichia coli isolates in Switzerland 1997-2007. Infection. 2009;37(6):534–9. doi:.https://doi.org/10.1007/s15010-009-8457-0
5World Health Organization. Global guidelines on the prevention of surgical site infection. Geneva: World Health Organization; 2016. Available from: http://www.who.int/gpsc/global-guidelines-web.pdf
6
Alsaywid
BS
,
Smith
GH
. Antibiotic prophylaxis for transurethral urological surgeries: Systematic review. Urol Ann. 2013;5(2):61–74. doi:.https://doi.org/10.4103/0974-7796.109993
7
Berry
A
,
Barratt
A
. Prophylactic antibiotic use in transurethral prostatic resection: a meta-analysis. J Urol. 2002;167(2 Pt 1):571–7.
8
Qiang
W
,
Jianchen
W
,
MacDonald
R
,
Monga
M
,
Wilt
TJ
. Antibiotic prophylaxis for transurethral prostatic resection in men with preoperative urine containing less than 100,000 bacteria per ml: a systematic review. J Urol. 2005;173(4):1175–81. doi:.https://doi.org/10.1097/01.ju.0000149676.15561.cb
9
Wilson
JR
,
Puri
R
,
Prescott
S
,
Urwin
GH
. The catheterized patient undergoing transurethral resection of the prostate: a survey of the current practice of British urologists. BJU Int. 2003;92(6):589–91. doi:.https://doi.org/10.1046/j.1464-410X.2003.04429.x
10
Çek
M
,
Tandoğdu
Z
,
Naber
K
,
Tenke
P
,
Wagenlehner
F
,
van Oostrum
E
, et al.; Global Prevalence Study of Infections in Urology Investigators. Antibiotic prophylaxis in urology departments, 2005-2010. Eur Urol. 2013;63(2):386–94. doi:.https://doi.org/10.1016/j.eururo.2012.09.038
11
Wagenlehner
F
,
Stöwer-Hoffmann
J
,
Schneider-Brachert
W
,
Naber
KG
,
Lehn
N
. Influence of a prophylactic single dose of ciprofloxacin on the level of resistance of Escherichia coli to fluoroquinolones in urology. Int J Antimicrob Agents. 2000;15(3):207–11. doi:.https://doi.org/10.1016/S0924-8579(00)00182-5
12
Bonkat
G
,
Müller
G
,
Braissant
O
,
Frei
R
,
Tschudin-Suter
S
,
Rieken
M
, et al.
Increasing prevalence of ciprofloxacin resistance in extended-spectrum-β-lactamase-producing Escherichia coli urinary isolates. World J Urol. 2013;31(6):1427–32. doi:.https://doi.org/10.1007/s00345-013-1031-5
13
Bantar
C
,
Sartori
B
,
Vesco
E
,
Heft
C
,
Saúl
M
,
Salamone
F
, et al.
A hospitalwide intervention program to optimize the quality of antibiotic use: impact on prescribing practice, antibiotic consumption, cost savings, and bacterial resistance. Clin Infect Dis. 2003;37(2):180–6. doi:.https://doi.org/10.1086/375818
14
Cai
T
,
Verze
P
,
Brugnolli
A
,
Tiscione
D
,
Luciani
LG
,
Eccher
C
, et al.
Adherence to European association of urology guidelines on prophylactic antibiotics: An important step in antimicrobial stewardship. Eur Urol. 2016;69(2):276–83. doi:.https://doi.org/10.1016/j.eururo.2015.05.010