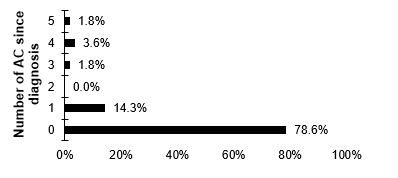
Figure 1 number of adrenal crisis per patient.
DOI: https://doi.org/10.4414/smw.2018.14586
Primary and secondary adrenal insufficiency are dangerous clinical conditions leading to significant morbidity or even mortality in situations with inadequate glucocorticoid replacement treatment. A previous Swedish registry study in patients with primary adrenal insufficiency showed a two-fold increase in standardised mortality rate, most likely in relation to inappropriate glucocorticoid replacement therapy leading to adrenal crises [1]. The incidence of adrenal crisis varies between different study types. The largest retrospective analysis was performed in the UK, and included 841 patients with primary adrenal insufficiency. The study indicated an incidence of 8 crises per 100 patient-years. In this study, vomiting and/or diarrhoea were the most important precipitating factors for an adrenal crisis, besides influenza-like illness and other respiratory infections [2]. In another retrospective study, based on German hospital records, 6.3 adrenal crises per 100 patient-years were reported [3] and in the following prospective German study with a follow-up of 2 years, 8.3 crises per 100 patient-years were documented. In this study, four patients died during the follow-up [4].
Patients’ knowledge about the disease and corresponding education are critical to prevent adrenal crises. Preventive measures include possession of an emergency card and an emergency kit (supply of hydrocortisone vials), as well as the instruction about utilisation of the kit [5]. There is no consistency between European countries on how many patients have an emergency kit. In a study from the UK, 68% of the patients had a supply of injectable hydrocortisone at home [2]. In a Dutch study, 95% of the patients had vials of hydrocortisone at home. In contrast, a study from Germany showed that only 29.6% were equipped with an emergency kit [3].
Apart from being equipped with the card and kit, patients should be trained to recognise symptoms of an emerging adrenal crisis [6] and instructed in glucocorticoid therapy adjustment in typical situations requiring a change in route of administration (parenteral in the case of severe vomiting) and of dose in the case of fever, and physical and sometimes psychological stress [6–8].
A few studies investigated the knowledge of patients with adrenal insufficiency [7–11]. By use of questionnaires based on different clinical situations, the knowledge of the patients could be objectively tested. Globally, only about half of the patients could correctly answer the questions [7–11].
In Switzerland, data on the frequency of adrenal crises, possible risk factors and the quality of preventive measures to avoid crises are not available. We therefore assessed incidence and risk factors for adrenal crisis in patients with primary or secondary adrenal insufficiency. Preventive measures (presence of emergency card, kit and spare hydrocortisone tablets) were documented. In addition, self-perceived subjective knowledge and objectively assessed knowledge of their disease was assessed using adapted questionnaires from previous studies [8, 9].
All adult patients with primary or secondary adrenal insufficiency who attended the Division of Endocrinology, Diabetology and Metabolism at the Inselspital (University Hospital) in Bern between May and June 2016, and December 2016 and January 2017 were prospectively included in a questionnaire-based interview. Each patient was interviewed only once. People with iatrogenic adrenal insufficiency and adrenogenital syndrome were excluded from the study. The trial was approved by the local review board (Kantonale Ethikkommission, Bern) and all subjects gave written informed consent.
Patients completed detailed questionnaires about their personal and medical background. In addition, the frequency and circumstances of adrenal crises experienced and the availability of an emergency card, kit and spare hydrocortisone tablets were documented. Importantly, the adrenal crisis that led to the diagnosis was not included, since at that point the patient was not yet informed about the newly diagnosed disease and, therefore, the patient’s knowledge could not be evaluated. Documentation of an adrenal crisis was confirmed from hospital notes where available. Potential risk factors for adrenal crises were recorded.
Afterwards, in order to quantify the patients subjective knowledge they were asked to estimate their self-perceived understanding of the disease on a five-point scale with the items “very bad”, “bad”, “neither good nor bad”, “good” and “very good”. The same scale was used for the evaluation of satisfaction with the initial counselling and the endocrine care during follow-up. The objective assessment of knowledge comprised two questionnaires that were adapted from Harsch et al. (part A [9];) and Flemming et al. (part B [8]). The questions and correct answers are shown in table 1 and table 2. For every fully correctly answered question one point was given. We then evaluated the following possible factors predicting a poor test performance: age at diagnosis, gender, level of education, presence of internet access, primary vs secondary adrenal insufficiency, hydrocortisone dose and previous adrenal crisis. For this evaluation, the patients were divided into two groups according to their performance. The line was drawn at the 50 percentile mark of the total points. The maximum score was 10 out of 12 points. One group therefore included the patients with 0 to 5 points in the two questionnaires. This group was called “worse-performance group”. The other group consisted of the patients with 6 to 10 points and was considered as the “better-performance group”.
Table 1 Questions Part A, which assessed knowledge about the biomedical background of cortisone replacement.
| Questions | Answers |
|---|---|
| 1. Is cortisone replacement therapy with hydrocortisone alone possible, or alternatively with other synthetic steroids? | Other synthetic steroids are feasible |
| 2. Which modes of application of cortisone are possible? | Oral, intravenous, intramuscular, subcutaneous and suppository |
| 3. Are the doses of cortisone replacement therapy comparable to the cortisol production of a healthy adrenal gland? | The doses are comparable |
| 4. In which situations must the replacement dose be raised? | Infection with raised temperature, surgery, vomiting, diarrhoea |
| 5. What are the clinical signs of an under-substitution with cortisone? | Marked tiredness, fever, loss of power and energy |
| 6. What are the precursors of an adrenal crisis? | Marked tiredness, fever, loss of power and energy |
Table 2 Questions part B, assessing the knowledge about dose adaptation in different hypothetical situations.
| Questions (What do you do in the following situations?) | Answers |
|---|---|
| 1. Increased mental pressure at home or at work (death of a relative, examination at an university) | I take 5 or 10 mg more hydrocortisone |
| 2. Common cold with fever <38° Celsius | I double the usual dose for 3–4 days (until recovery) |
| 3. Influenza / raised temperature between 38.5 and 39.5°C | I double to triple every usual dose until recovery |
| 4. Single vomiting right after the ingestion of the usual morning dosage | I take the morning dose once again |
| 5. Repeated vomiting or diarrhoea | I need cortisone as a self-injection or injected by relatives/medical assistance or I phone my family doctor / endocrinologist |
| 6. Repeated vomiting or diarrhoea, with fever | I need cortisone as a self-injection or injected by relatives/medical assistance or I phone my family doctor / endocrinologist |
Categorical variables are presented as numbers (percentages) and continuous variables are expressed as means ± standard deviation (SD). First, the predefined potential risk factors for an adrenal crisis (age at diagnosis, gender, tertiary education, body mass index [BMI], internet access, secondary adrenal insufficiency, hydrocortisone dose and test performance) were investigated with binary logistic regression analysis. Odds ratios with 95% confidence intervals (CIs) were calculated for the whole group of patients, and then, as there were fewer than 10 patients with primary adrenal insufficiency, analysed for only the subgroup with secondary adrenal insufficiency. Secondly, we searched for potential risk factors leading to a poor performance in the objective knowledge test. We did this for the two parts (A + B) together and also for each part separately. We used the same predefined list of risk factors for poor knowledge (age at diagnosis, female sex, tertiary education, duration of illness, internet access, secondary adrenal insufficiency, experienced an adrenal crisis) for all patients. The above-mentioned risk factors were investigated by means of binary logistic regression analyses. All p-values are considered statistically significant at a level of <0.05. SPSS, Version 23, was used for the analyses.
Of 62 adult patients asked, 56 finally participated in a questionnaire-based interview. Six patients did not want to be included in the study because of lack of time or interest. Fifty-four (96.4%) of the patients were followed up at the Division of Endocrinology at the Inselspital Bern, the other two were previously in the care of a private endocrinologist or had no regular appointments before. Clinical characteristics are presented in table 3. In brief; a majority (60%) of the patients were male, had secondary adrenal insufficiency, spoke mostly German or French, had at least professional tertiary education, were regular internet users and had annual follow-ups.
Table 3 Characteristics of 56 patients with adrenal insufficiency.
| Sex | |
| Female | 22 (39.3%) |
| Male | 34 (60.7%) |
| Age (years) | 51.9 ± 16.5 (19–83) |
| Body mass index (kg/m2) | 28.8 ± 5.1 (19.7–46.25) |
| Cause of adrenal insufficiency | |
| Primary | 10 (17.9%) |
| Secondary | 46 (82.1%) |
| Age at diagnosis (years) | 41.8 ± 17.0 (2–76) |
| Duration of AI (years) | 9.7 ± 8.9 (0.1–37.2) |
| History of AC since primary diagnosis of AI | 12 (21.4%) |
| Types of glucocorticoid replacement | |
| Hydrocortisone | 54 (86.5%) |
| Cortisone acetate | 1 (1.8%) |
| Prednisone | 1 (1.8%) |
| Dose of replacement therapy (mg/day) | |
| Hydrocortisone | 19.0 ± 4.7 (10.0–35.0) |
| Cortisone acetate | 25 ± 0 |
| Prednisone | 5 ± 0 |
| Fludrocortisone dose in pAI patients (mg/day) | 0.15 ± 0.13 (0.05–0.50) |
| Educational background | |
| Compulsory | 10 (17.9%) |
| Professional training | 23 (41.1%) |
| Higher professional training | 15 (26.8%) |
| University / CoHE | 8 (14.3%) |
| German/French as first language | 46 (82.1%) |
| Appointments with an endocrinologist | |
| More often than quarterly | 7 (12.5%) |
| Quarterly | 8 (14.3%) |
| Biannually | 11 (19.6%) |
| Annually | 29 (51.8%) |
| Regular use of the internet | 47 (83.9%) |
AC = adrenal crisis; AI = adrenal insufficiency; pAI = primary AI; CoHE: college of higher education Data for numerical variables are given as number with percentage in brackets. Continuous variables are presented as mean ± standard and ranges in brackets
A total of 24 adrenal crises in 12 patients (21.4%) were recorded, of which 5 crises occurred in the last 2 years. Of the 12 patients with an adrenal crisis, 4 had primary and 8 secondary adrenal insufficiency. This results in 4.4 adrenal crises per 100 disease-years. Medical records or file notes confirmed the diagnosis of 17 adrenal crises. Two patients with a confirmed adrenal crisis had primary and five had secondary adrenal insufficiency. A reported adrenal crisis could not be confirmed in two patients with primary and three with secondary adrenal insufficiency. The maximum number of adrenal crises per patient is summarised in figure 1. Twenty-one adrenal crisis resulted in a short hospitalisation and three were treated by a general practitioner. Self-injection or treatment by relatives were not performed.
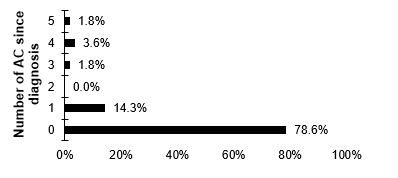
Figure 1 number of adrenal crisis per patient.
Precipitating factors for confirmed crises (17 adrenal crises, 70.8%) are shown in figure 2a. Vomiting/diarrhoea (gastroenteritis) and influenza were the events most frequently associated with the occurrence of adrenal crisis, besides noncompliance with therapy and unknown factors. Where we were not able to confirm the adrenal crisis by medical records (7 crises, 20.2%), the most prevalent reasons were gastroenteritis and unknown reasons (fig. 2b).
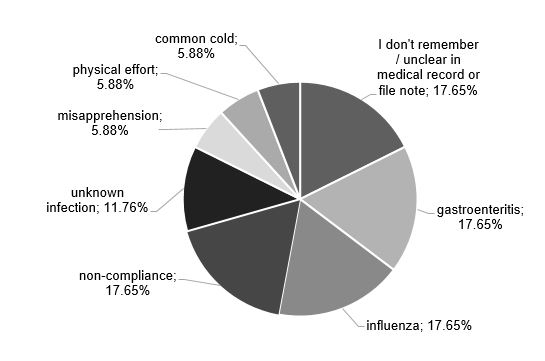
Figure 2a Precipitating factors for the adrenal crises reported by the patients and confirmed by medical records or file note.
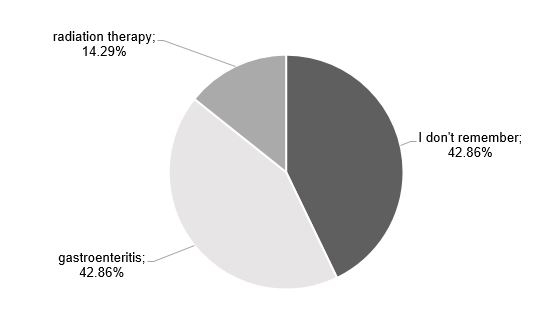
Figure 2b Precipitating factors for the adrenal crises reported only by the patients.
The results of the preventive measures for adrenal crisis are summarised in table 4. Fifty-three (96.4%) of the patients were equipped with an emergency card and 46 (82.1%) carried the card with them. Nine (16.1%) owned an emergency kit. Thirty-six (64.3%) did not have their hydrocortisone for the day with them, and 32 (57.1%) did not have spare hydrocortisone with them (table 4).
Table 4 Characteristics of equipment and preventive measures in 56 patients with adrenal insufficiency.
| Possess an emergency card | 53 (94.6%) |
| Carry the emergency card | 46 (82.1%) |
| Possess an emergency set | 9 (16.1%) |
| Carry the emergency kit | 3 (5.4%) |
| Carry the HC required for the day with them | 36 (64.3%) |
| Carry spare HC (emergency HC) with them | 32 (57.1%) |
| Adapted HC dose in the last 2 years | |
| Yes | 23 (41.1%) |
| No | 16 (28.6%) |
| The patient was not asked this question in the interview | 17 (30.4%) |
| Asked by the physician about dose adaptation in the last 2 years? | |
| Yes | 35 (62.5%) |
| No | 9 (16.1%) |
| The patient was not asked this question in the interview | 12 (21.4%) |
| Ever asked by the physician about dose adaptation? | |
| Yes | 36 (64.3%) |
| No | 8 (14.3%) |
| The patient was not asked this question in the interview | 12 (21.4%) |
HC = hydrocortisone Data are given as numbers with percentage in brackets.
The risk factor analysis is summarised in table 5. Internet access in patients with secondary adrenal insufficiency was associated with a lower incidence of adrenal crisis compared with patients without internet access. If corrected for the possible confounder of age, this remained statistically significant. The other possible risk factors were not associated with a significant risk for an adrenal crisis.
Table 5 Risk factors for adrenal crisis in all patients with adrenal insufficiency and in a subgroup of those with secondary adrenal insufficiency (binary logistic regression).
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| All patients (n = 56) | |||
| Age at diagnosis (years) | 0.992 | 0.955–1.031 | 0.691 |
| Female sex | 1.750 | 0.483–6.342 | 0.394 |
| Tertiary education | 0.481 | 0.053–4.340 | 0.514 |
| BMI (kg/m2) | 0.903 | 0.773–1.054 | 0.197 |
| Internet acces | 0.256 | 0.056–1.171 | 0.079 |
| sAI | 0.316 | 0.072–1.383 | 0.126 |
| Glucocorticoid dose (mg) | 1.039 | 0.914–1.180 | 0.560 |
| Test performance | 1.088 | 0.815–1.454 | 0.567 |
| Patients with sAI (n = 46) | |||
| Age at diagnosis (years) | 0.984 | 0.942–1.028 | 0.469 |
| Female sex | 1.154 | 0.238–5.605 | 0.859 |
| Tertiary education | 0.762 | 0.079–7.371 | 0.814 |
| Body mass index (kg/m2) | 0.809 | 0.635–1.030 | 0.085 |
| Internet access | 0.152 | 0.028–0.809 | 0.027 |
| Glucocorticoid dose (mg) | 1.125 | 0.947–1.335 | 0.181 |
| Test performance | 1.117 | 0.763–1.635 | 0.569 |
pAI = primary adrenal insufficiency; sAI = secondary adrenal insufficiency
After the first counselling at the time of adrenal insufficiency diagnosis, 9 patients (16.1%) felt not well informed, 33 patients (58.9%) felt well informed and 14 (25%) did not remember. Half of the patients (n = 28) searched for additional information after the diagnosis was established. Among these, 4 (14.2%) read leaflets of self-help groups, 8 (28.5%) booklets/guidebooks, 26 (92.8%) searched the internet, 5 (17.8%) discussed with other patients with adrenal insufficiency and 2 (7.1%) listened to lectures or speeches (multiple answers were possible). Twelve patients (21.4%) would have liked additional information, six (10.7%) would have liked written information (books, booklets, guidebooks), three (5.4%) would have liked to learn in interactive groups, eight (8.6%) would have liked to learn with an internet-based tool and three (5.4%) would have liked to receive more information from their endocrinologist.
The satisfaction with the care at the Inselspital as follows: 40 (71.4%) were very satisfied, 14 (25.0%) were satisfied, and two (3.6%) were neither satisfied nor dissatisfied with the care.
The self-perceived understanding was rated as follows: one patient (1.8%) considered his knowledge as very bad, two (3.6%) rated is as bad, five (8.9%) answered with neither bad nor good, 39 (69.6%) stated that they are well-informed and nine (16.1%) rated themselves as very well informed.
The results of the questionnaires used to objectively assess knowledge are shown in figure 3.
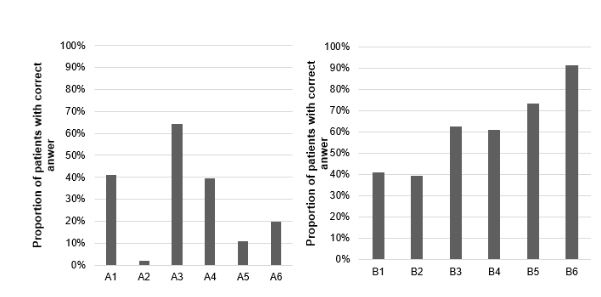
Figure 3 (a: left) Right answers (in %) to the questions of test A, shown in “Material and methods” and in table 1 . (b: right) Right answers (in %) to the questions of test B, shown in “Material and methods” and in table 2.
The average score in part A was 1.7 ± 1.0 points (range 0–4), in part B 3.6 ± 1.6 points (range 0–6), and in total (A + B) 5.3 ± 2.3 points (range 1–10). In part A 28.9%, in part B 60.1% and in total (A + B) 44.4% of the total possible points were achieved.
Twenty-nine patients (51.7%) obtained 0 to 5.0 points in parts A and B combined and were then classified as the “worse-performance group”. Twenty-seven patients (48.3%) scored 6 to 10 points and were classified as the “better-performance group”. We could not identify any risk factors for a poor performance in the overall knowledge test (table 6). In the analysis of part A alone, 42 patients (75.0%) scored 0 to 2 points and were then classified as the worse-performance group, 14 patients (25.0%) scored 3 to 4 points and were classified as the better-performance group. People with secondary adrenal insufficiency had a statistically increased risk of belonging to the worse performance group (table 7). In this subanalysis, the binary logistic regression analysis for internet access as a risk factor was not possible because of a subgroup with a zero value (table 8). In the analysis of part B alone, 25 patients (44.6%) scored 0 to 3 points and were then classified as the worse-performance group, 31 patients (55.4%) scored 4 to 6 points and were then classified as the better-performance group. No risk factors for a poor performance in part B could be identified (table 9).
Table 6 Factors contributing to a good overall test performance.
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| All patients (n = 56) | |||
| Age at diagnosis (years) | 1.003 | 0.972–1.034 | 0.870 |
| Female sex | 2.063 | 0.694–6.139 | 0.193 |
| Tertiary education | 1.970 | 0.422–9.186 | 0.388 |
| Duration of illness (years) | 0.977 | 0.919–1.038 | 0.447 |
| Internet access | 1.198 | 0.286–5.025 | 0.805 |
| sAI | 0.330 | 0.076–1.438 | 0.140 |
| AC experienced | 1.680 | 0.462–6.115 | 0.431 |
AC = adrenal crisis; sAI = secondary adrenal insufficiency. Odds ratio = risk for belonging to the better performance group, binary logistic regression
Table 7 Factors contributing to a good test performance in Part A.
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| All patients (n = 56) | |||
| Age at diagnosis (years) | 0.984 | 0.947–1.022 | 0.394 |
| Female sex | 1.800 | 0.530–6.116 | 0.346 |
| Tertiary education | 1 | 0.178–5.632 | 1.000 |
| Duration of illness (years) | 0.982 | 0.914–1.056 | 0.632 |
| Internet access | Error * | ||
| sAI | 0.140 | 0.032–0.615 | 0.009 |
| AC experienced | 0.533 | 0.102–2.796 | 0.457 |
AC =: adrenal crisis; sAI: = secondary adrenal insufficiency Odds ratio = risk for belonging to the better performance group, binary logistic regression * see table 8
Table 8 Explanation of error in table 7.
| Do you have an internet access / do you use the internet regularly? | |||
|---|---|---|---|
| No | Yes | Total | |
| Group 1 (worse) | 9 | 33 | 42 |
| Group 2 (better) | 0 | 14 | 14 |
| Total | 9 | 47 | 56 |
Table 9 Factors contributing to a good test performance in Part B.
| Odds ratio | 95% confidence interval | p-value | |
|---|---|---|---|
| All patients (n=56) | |||
| Age at diagnosis (years) | 0.994 | 0.963–1.026 | 0.704 |
| Female sex | 1.284 | 0.434–3.797 | 0.651 |
| Tertiary education | 1.410 | 0.302–6.577 | 0.662 |
| Duration of illness (years) | 0.964 | 0.906–1.025 | 0.237 |
| Internet access | 0.990 | 0.236–4.160 | 0.990 |
| sAI | 0.468 | 0.107–2.036 | 0.311 |
| AC experienced | 1.167 | 0.321–4.247 | 0.815 |
AC =: adrenal crisis; sAI: = secondary adrenal insufficiency Odds ratio = risk for belonging to the better performance group, binary logistic regression
The main findings of this study can be summarised as follows:
The incidence of adrenal crisis in educated patients was still high, but lower than recent data from Germany and the UK suggest [2–4]. In most of the cases the crisis resulted in a short hospitalisation, which is consistent with the literature [4]. The most frequent clinical conditions leading to a confirmed adrenal crisis were gastroenteritis and influenza, in keeping with the literature [2]. However, in about one sixth of patients an adrenal crisis occurred because of noncompliance and, in addition, one sixth of the patients reported unknown reasons for a crisis or the medical record / file note did not reveal the reason. In the unconfirmed adrenal crises, the reason mostly remained unclear or was gastroenteritis.
Nearly all patients with adrenal insufficiency carried their emergency card with them, consistent with previous reports [3, 4, 7–12]. However, in our study, spare hydrocortisone tablets were not available for nearly 50% of the patients and only 16.1% were equipped with an emergency kit. Previous studies suggested more frequent possession of an emergency kit [2, 11], whereas data on the immediate availability of oral hydrocortisone are not reported to our knowledge. This finding is, therefore, new and concerning, since oral medication can be critical in covering the time until emergency therapy can be administered.
In our study, reduced internet access significantly increased the risk for an adrenal crisis in patients with secondary adrenal insufficiency. This finding is intriguing and new. It may indicate that internet access facilitates the search for additional information about the disease, in keeping with the fact that additional sources of information were searched for by about 50% of the patients in the current study. Alternatively, the availability of internet access could be a marker for patients who wish to be generally better informed. Previous studies have identified several risk factors for adrenal crisis: steroid replacement of more than 4 years’ duration, the presence of a mental disorder and untreated hypogonadism, concomitant diseases and secondary adrenal insufficiency were risk factors in all patients [3, 13]. Age at diagnosis was a risk factor in the subgroup with primary adrenal insufficiency and female sex were risk factors in the subgroup with secondary adrenal insufficiency [3]. Our present study did not confirm these risk factors, possibly owing to the small number of patients in the subgroups.
The current data indicate that the self-perceived understanding of the disease was considered good to very good and the initial counselling was reported to be satisfactory. However, results of objective testing of knowledge were disappointing, in particular with regard to the understanding of the disease and dose adaptation in different clinical conditions. The latter results were comparable to results of previous studies [7–11] with one exception: the Swiss patients scored worse for knowledge about the biomedical background of the disease than those in the study of Harsch et al. (28.9 vs 52%) [9]. Remarkably, there was a substantial number of patients who scored badly in questions A2 (see fig. 3), suggesting that they are not aware that multiple routes of application beyond the commonly used one are available. In addition, the patients scored badly in question A5 (fig. 3) indicating that patient education should focus on early symptoms of adrenal crisis and the consequent therapeutic actions.
In the subanalysis of part A, secondary adrenal insufficiency statistically increased the risk for a worse performance. Consequently, the education should focus on patients with secondary adrenal insufficiency. Several factors may have contributed to the unsatisfactory performance: (1) patients in a stable condition – as in our study – are seen only once a year, thereby decreasing the opportunity to review key elements of dose adaptation; (2) The mean follow-up of the patients in this study was quite long and it is conceivable that basic knowledge of the initial counselling was not remembered anymore. Interestingly, poor knowledge was not directly associated with an increased risk for adrenal crisis, most probably because of the small sample size. However, in a German prospective study, patients who experienced an adrenal crisis during follow-up were more likely to correctly adjust their hydrocortisone dose in the future than patients who did not experience a crisis [4], indicating that there is a probably a relationship between adrenal crises and knowledge of the disease.
Our study has several limitations. First, the sample size was rather small, with predominantly patients with secondary adrenal insufficiency. Firm conclusions on patients with primary adrenal insufficiency have, therefore, to be drawn with caution. However, since nearly all adrenal crises resulted in a hospitalisation (and most of the diagnoses could be confirmed by consulting the hospital files), we believe that at least the number of reported adrenal crises is valid. Secondly, it was a retrospective analysis, where in particular the circumstances of adrenal crisis could not always be retrieved or remembered with certainty by the patients and is, therefore, a possible source of bias. Thirdly, the patients were mainly followed up in the outpatient clinic of the University Hospital of Bern. These results cannot be extrapolated to the quality of care of patients in Switzerland in general.
In conclusion, there is still a significant number of adrenal crises in patients with primary and secondary adrenal insufficiency. The current data suggest that there is a need for an improvement in education with regard to preventive measures and understanding of the disease. The method of instruction (individual, group teaching, internet-based tools [12]) remains to be defined. Whether such measures will result in a decrease in the rate of adrenal crisis has to be determined in prospective studies.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Bergthorsdottir R , Leonsson-Zachrisson M , Odén A , Johannsson G . Premature mortality in patients with Addison’s disease: a population-based study. J Clin Endocrinol Metab. 2006;91(12):4849–53. doi:.https://doi.org/10.1210/jc.2006-0076
2 White K , Arlt W . Adrenal crisis in treated Addison’s disease: a predictable but under-managed event. Eur J Endocrinol. 2010;162(1):115–20. doi:.https://doi.org/10.1530/EJE-09-0559
3 Hahner S , Loeffler M , Bleicken B , Drechsler C , Milovanovic D , Fassnacht M , et al. Epidemiology of adrenal crisis in chronic adrenal insufficiency: the need for new prevention strategies. Eur J Endocrinol. 2010;162(3):597–602. doi:.https://doi.org/10.1530/EJE-09-0884
4 Hahner S , Spinnler C , Fassnacht M , Burger-Stritt S , Lang K , Milovanovic D , et al. High incidence of adrenal crisis in educated patients with chronic adrenal insufficiency: a prospective study. J Clin Endocrinol Metab. 2015;100(2):407–16. doi:.https://doi.org/10.1210/jc.2014-3191
5 Allolio B . Extensive expertise in endocrinology. Adrenal crisis. Eur J Endocrinol. 2015;172(3):R115–24. doi:.https://doi.org/10.1530/EJE-14-0824
6 Hahner S , Allolio B . Therapeutic management of adrenal insufficiency. Best Pract Res Clin Endocrinol Metab. 2009;23(2):167–79. doi:.https://doi.org/10.1016/j.beem.2008.09.009
7 Braatvedt GD , Newrick PG , Corrall RJ . Patients’ self administration of hydrocortisone. BMJ. 1990;301(6764):1312. doi:.https://doi.org/10.1136/bmj.301.6764.1312
8 Flemming TG , Kristensen LO . Quality of self-care in patients on replacement therapy with hydrocortisone. J Intern Med. 1999;246(5):497–501. doi:.https://doi.org/10.1046/j.1365-2796.1999.00538.x
9 Harsch IA , Schuller A , Hahn EG , Hensen J . Cortisone replacement therapy in endocrine disorders - quality of self-care. J Eval Clin Pract. 2010;16(3):492–8.
10 Peacey SR , Pope RM , Naik KS , Hardern RD , Page MD , Belchetz PE . Corticosteroid therapy and intercurrent illness: the need for continuing patient education. Postgrad Med J. 1993;69(810):282–4. doi:.https://doi.org/10.1136/pgmj.69.810.282
11 Repping-Wuts HJ , Stikkelbroeck NM , Noordzij A , Kerstens M , Hermus AR . A glucocorticoid education group meeting: an effective strategy for improving self-management to prevent adrenal crisis. Eur J Endocrinol. 2013;169(1):17–22. doi:.https://doi.org/10.1530/EJE-12-1094
12 Downie WW , Leatham PA , Rhind VM , Wright V . Steroid cards: patient compliance. BMJ. 1977;1(6058):428. doi:.https://doi.org/10.1136/bmj.1.6058.428
13 Quinkler M , Hahner S . What is the best long-term management strategy for patients with primary adrenal insufficiency? Clin Endocrinol (Oxf). 2012;76(1):21–5. doi:.https://doi.org/10.1111/j.1365-2265.2011.04103.x
No financial support and no other potential conflict of interest relevant to this article was reported.