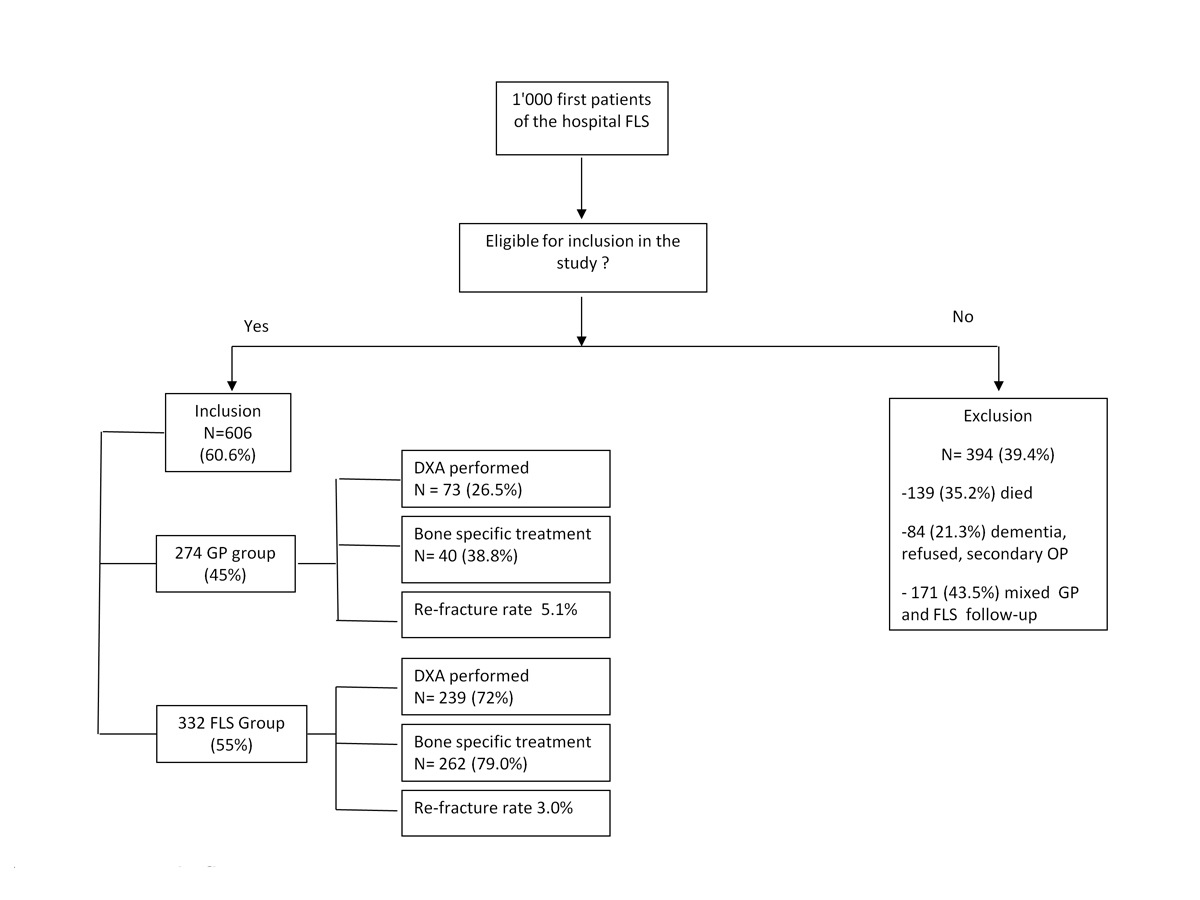
Figure 1 Study flowchart.
DOI: https://doi.org/10.4414/smw.2018.14579
With the aging of the population and the recognised huge economic burden of osteoporotic fractures [1–3], multidisciplinary expert management of acute osteoporotic fractures through what was called a Fracture Liaison Service (FLS) was proposed. The International Osteoporosis Foundation subsequently supported a “Capture the Fracture” campaign to encourage the creation of FLS programmes worldwide and thereby improve both the detection and subsequent management of osteoporosis-related fractures [4]. The two major objectives of an FLS are: (1) to reduce the 80% of adult low-trauma fracture patients not currently screened and/or treated for osteoporosis (“the treatment gap”); and (2) to enhance communication between different healthcare providers to facilitate the treatment of fragility fractures. Today, FLSs are widely considered the most efficient way to identify patients with a major osteoporotic fracture, assess their bone status, and select the most appropriate treatment and follow-up schedule [4]. The FLS models can be divided into four groups on the basis of the management type proposed [5]: type A is defined as a service that identifies, investigates and initiates treatment; type B is a service that identifies and investigates patients, but refers them back to the primary care physician for treatment initiation; type C is a service that identifies patients at risk and informs them and their primary care physician, but does not undertake any assessment or treatment of the patients; and type D is a service that identifies patients at risk, informs and educates them but takes no further part in others stakeholders in the patient‘s care. Compared with the others type of FLS, type A is associated with a greater reduction in future fracture risk, more bone health assessments and lower mortality, and is cost-effective and cost-saving, [6].
In 2008, an FLS was created at the Centre Hospitalier Universitaire Vaudois (CHUV), Lausanne, Switzerland. Lausanne is a city of more than 133 800 people, and is the main city of the state of Vaud, which had a population of 778 251 at the end of 2016. The CHUV is the biggest public hospital in the canton of Vaud, and the only university hospital. The orthopaedic capacity is 100 beds. After detection by the FLS, inpatients are free to be managed by either the FLS team or their general practitioner. Management by the FLS team is considered to be FLS type A.
The first aim of this study was to compare osteoporosis management (diagnosis and treatment) of patients registered with the FLS between the two forms of management (FLS or GP). We compared these results with data recorded previously in the Osteocare study, before the creation of the FLS. The second aim was to compare one- and five-year new fracture and mortality rates between patients managed by the FLS team and those managed by their GP. To accomplish this, we elected to prospectively follow up the first 1000 consecutive patients registered in the FLS.
The FLS first came into being at the CHUV in October 2008. Since that time, all consecutive patients hospitalised for one or more low-trauma fractures have been registered by a dedicated nurse (present 30% of full-time in the orthopaedic unit) at the time of their admission into the orthopaedic unit. During hospitalisation, a physician specialising in bone diseases meets each registered patient, apart from patients with dementia, who are not stable, or who refused. Depending on the patient’s estimated risk of future osteoporotic fractures, specific management is proposed; this may consist of monitoring only or monitoring plus treatment. All baseline data are entered into a dedicated database. Patients are then allowed to choose whether they wish to be evaluated, treated and followed up by the FLS or by their own GP.
The standardised FLS protocol includes dual X-ray absorptiometry (DXA, Hologic Inc., Bedford, MA) for assessment of bone mineral density, a vertebral fracture assessment (VFA), prescription of treatment and scheduling of follow-up. Such monitoring may include: (1) a clinical and biological evaluation 3 months after the fracture; (2) further clinical and biological evaluations every year thereafter; and (3) follow-up with DXA plus VFA assessment every 2 years. DXA and VFA interpretation follow the International Society of Clinical Densitometry (ISCD) recommendations. Follow-up by the GP is not standardised. The FLS team at CHUV evaluates roughly 600 patients hospitalised for a fragility fracture every year.
Between 2004 and 2006, the Osteocare Study Group performed a nationwide survey of 4966 patients who presented consecutively with one or more fractures at any one of eight designated hospitals in Switzerland [7], as either an in- or an outpatient. The CHUV participated in this study. After data were recorded by a study nurse, an information letter was sent to the GP about any suspected osteoporotic fractures. Data on osteoporosis management were recorded on a second occasion.
Inclusion criteria for the current study were: being seen by the CHUV FLS for an osteoporotic fracture; being alive at the time of hospital discharge; and having provided written informed consent to participate in the study. Exclusion criteria were: severe dementia, an already known secondary cause of osteoporosis, refusal to participate, and follow-up by both their GP and the FLS team. One year after each patient’s acute fracture was registered by the FLS, data were collected on osteoporosis management and course/events. Patients followed up by their GP were sent a written questionnaire, and the institutional database was used to collect information on all patients followed up by the FLS. Data collected at 1 year of follow-up included the number and results of DXA evaluations over the preceding year; any osteoporosis treatment rendered (including: none; vitamin D and/or calcium; and bone-active drugs like bisphosphonate, denosumab and teriparatide); any new non-traumatic fractures; and mortality. Data on fractures at 5 years of follow-up were also collected for patients followed up by the FLS. In addition, patients who had died by 1 and 5 years of follow-up were identified in the institutional database, from information obtained from family members, and from regional death records, as needed.
Differences between the two patient groups – those followed up by the FLS and those followed up by their GP – were identified with Student’s t-tests for continuous variables and Pearson’s chi-squared analysis for categorical variables, and statistical significance was considered for a two-sided test with p-value ≤0.05. All statistical analysis were performed using Stata/IC 14.0 (StataCorp, College Station, Texas, USA) for Windows.
The first 1000 consecutive patients were registered with the CHUV FLS between 17 October 2008 and 27 October 2011. Figure 1 is a flow chart depicting subject recruitment and follow-up. A total of 606 patients were included (60.6%), 394 were excluded (139 died, 171 had a mixed GP and FLS follow-up, and 84 refused to participate, or had dementia or secondary osteoporosis). Overall, 55% (n = 332) of the patients chose to be followed up by the FLS team, and 45% (n = 274) elected to be managed by their GP. About 80% were women in both groups. The mean age was 78.5 years. Patients were older in GP group than in the FLS group (79.9 vs 75.4 years, p <0.05). The proportion of patients with hip fractures was greater in the GP group (51.5 vs 36.5% in the FLS group, p = 0.003). In the initial nationwide survey Osteocare, the mean age was 73.9 years and 26.4% of the patients had a hip fracture. Baseline characteristics of the 606 registered patients are summarised in table 1. In the nationwide survey, 30.7% had an upper limb fracture, 26.4% a lower limb fracture and 19.5% an axial fracture [7].
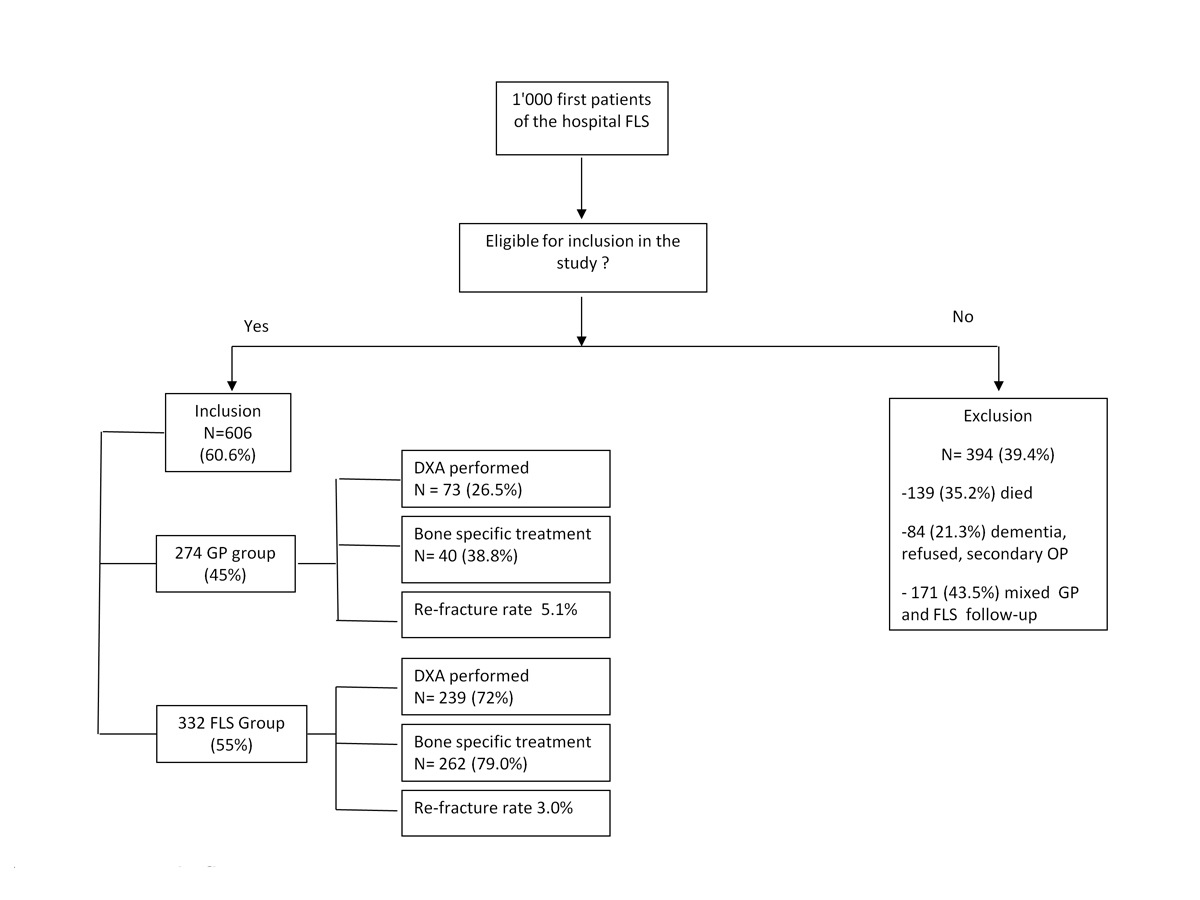
Figure 1 Study flowchart.
Table 1 Characteristics of the 606 patients included.
|
GP group
(n = 274) |
FLS group
(n = 332) |
p-value | Nationwide survey | |
|---|---|---|---|---|
| Mean age (years) | 79.5 | 75.5 | <0.05 | 73.9 |
| % of women | 81% | 83% | ||
| Hip | 51.5% | 39.5% | 0.003 | 26.4% |
| Spine | 8.4% | 12.7% | 0.092 | |
| Pelvis | 5.8% | 9.6% | 0.085 | |
| Humerus | 12.4% | 11.5% | 0.617 | |
| Radius | 5.5% | 7.5% | 0.310 | |
| Others | 16.4% | 19.3% | 0.303 |
FLS = Fracture Liaison Service; GP = general practitioner
The diagnostic workup for osteoporosis differed between the groups, with 72.0% (n = 239) having DXA in FLS-managed group and 26.5% (n = 73) in the GP-managed group (p <0.01). In the previous nationwide survey the percentage was 31.4%. Based on the definition of osteoporosis proposed by the World health Organization and the lowest measured T-score, 50.3% in the FLS group and 57.5% in the GP group had osteoporosis (p <0.05). This percentage was 46.0% in the nationwide survey. An additional 38% in FLS group versus 18% in the GP group had osteopenia (p <0.05). This was 35.1% in the nationwide survey. Normal DXA results were found in 11.7% of the FLS group, 5.5% in the GP group (p <0.05) and 14.4% in the nationwide survey. Nineteen percent of GP-managed patients had no available DXA evaluation results, whereas DXA results were available for all patients in the FLS group (table 2). In the nationwide survey, 4.5% of the subjects lacked DXA results.
Table 2 Dual X-ray absorptiometry results.
|
GP group
(n = 274) |
FLS group
(n = 332) |
Nationwide survey | |
|---|---|---|---|
| DXA performed | |||
| Yes | 26.5% | 72.0%* | 31.4% |
| No | 45.5%* | 28.0% | |
| Unknown | 28.0% | 0.0% | |
| DXA normal | 5.5% | 11.7%* | 14.4% |
| DXA osteopenia | 18.0% | 38.0%* | 35.1% |
| DXA osteoporosis | 57.5% | 50.3%* | 46.0% |
| Result not known | 19.0% | 0.0%* | 4.5% |
DXA = dual X-ray absorptiometry results; FLS = Fracture Liaison Service; GP = general practitioner * p <0.05
The percentage of patients receiving a prescription for some osteoporosis-specific therapy (i.e., a bone-active drug) was 79.0% in the FLS group and 38.8% in the GP group (p <0.001). Only 21.6% of the patients had a bone-active drug prescribed in the nationwide survey. In all groups, the majority of patients were prescribed a bisphosphonate (table 3).
Table 3 Treatment proposed after the fracture
| GP group | FLS group | |
|---|---|---|
| Treatment proposed | (n = 274) | (n = 332) |
| Yes | 44.1% | 100% |
| No | 32.5% | 0% |
| Unknown | 23.4% | 0% |
| Type of treatment | (n = 103) | (n = 332) |
| Calcium and/or vitamin D alone | 63 (61.2%) | 70 (21.0%) |
| Zoledronate | 16 (15.6%) | 141 (42.5%) |
| Alendronate | 2 (1.9%) | 51 (15.3%) |
| Ibandronate IV | 16 (15.6%) | 33 (10.0%) |
| Risedronate | 3 (2.9%) | 3 (0.9%) |
| Teriparatide | 2 (1.9%) | 20 (6.0%) |
| Denosumab | 1 (0.9%) | 13 (4.0%) |
| Pamidronate | 0 | 1 (0.3%) |
FLS = Fracture Liaison Service; GP = general practitioner
Data on incident fractures were available for 100% (n = 332) and 78% (n = 214) of patients in the FLS and GP groups, respectively; 15.1% had a second low-trauma fracture. The most commonly affected site was the hip. At 1 year, a new fracture had occurred in 5.4% and 5.1% of patients managed by the FLS and the GP, respectively (p = 0.80). A vertebral fracture was documented in eight patients at 1 year, all in the FLS group; this included one patient with three clinical vertebral fractures, and seven patients with one to three new asymptomatic fractures detected by VFA. After exclusion of vertebral fractures, which were screened for systematically by the FLS team but not by GPs, at least one new nonvertebral fracture was documented in 3.0% of patients in the FLS group and 5.1% in the GP group (p <0.05) (table 4). The proportions of patients with a new fracture who were given an osteoporosis-specific treatment (a bisphosphonate, denosumab, or teriparatide) were the same in both groups. After between 1 and 5 years of follow-up, data were available only for the FLS patients, among whom 40 had a new fracture, including vertebral fractures (12.3%).
Table 4 New fractures.
|
GP group
(n = 214) |
FLS group
(n = 332) |
p-value | |
|---|---|---|---|
| New fracture (with VF) | 5.1% | 5.4% | 0.80 |
| New fracture (without VF) | 5.1% | 3.0% | <0.05 |
FLS = Fracture Liaison Service; GP = general practitioner; VF = vertebral fracture
Over the first year after registration with the FLS, 7 patients followed up by the FLS team died compared with 19 followed up by their GP (2.1 vs 6.9%, p = 0.04). The mean times to death were 0.68 years (range 0.36–0.85) and 0.50 years (range 0.07–0.96), respectively (p = 0.05). Over a mean follow-up period of 5.62 years (range 3.84–6.86), 145 of the 606 patients died (24%): 53/332 in the FLS group and 92/274 in the GP group (16.0 vs 33.6%, p = 0.001). When adjusted for age and fracture site, these differences were not statistically significant (table 5).
Table 5 Mortality after 1 year and after a mean follow-up of 5.62 years.
|
GP group
(n = 274) |
FLS group
(n = 332) |
p-value | Adjusted p-value* | |
|---|---|---|---|---|
| After 1 year | 6.9% | 2.1% | 0.04 | NS |
| After 5.62 years | 33.6% | 16.0% | 0.001 | NS |
FLS = Fracture Liaison Service; GP = general practitioner; NS = not significant * p-value adjusted for age and hip fracture.
The key results of our study showed that the diagnosis and treatment of osteoporosis is more frequent for patients followed by the FLS team than for those followed by their GP after their acute low trauma fracture and both of them have increased relative to rates reported before the FLS creation. Relative to the GP management patients, FLS followed patients had fewer nonvertebral refractures and a decreased risk of death. These results are important in a country where the incidence of osteoporotic fractures is high [8] and where osteoporosis is associated with an increase morbidity and mortality [9, 10].
Although effective treatments for osteoporosis are currently available, the “treatment gap” between patients who should receive a bone-active drug and those who are effectively treated is increasing worldwide, with more than 50% of women and 36% of men undertreated in Switzerland [11, 12]. Patients at high risk for fragility fractures should be treated, especially after an osteoporotic fracture has occurred. Fracture liaison services are the most efficient way to enhance osteoporotic fracture detection.
Compared with the results of the nationwide survey, since the FLS implementation a higher proportion of patients had a DXA evaluation and the prescription of an active osteoporosis-specific treatment. These increases were greater in patients managed by the FLS team than in those managed by their GP. In fact, among patients managed by their GP, only the proportion receiving osteoporosis-specific therapy increased compared with the nationwide survey, and not the percentage having DXA,. These results are consistent with other publications. FLS type A versus GP has been shown to more effectively increase the number of DXA evaluations from 6% to a maximum of 85%, depending on the site of the fracture and the study [13–18]. In our study, even after a low-trauma fracture, only 50 to 53% of patients were in the osteoporotic range, with more than 50% having either osteopenia or a normal result, which is consistent with others’ data [13, 17, 19, 20]. Osteoporotic fracture risk is not well detected by the measurement of bone mineral density alone.
The frequency of prescription of an active osteoporotic drug increased and reached 79% in the FLS, but remained low in the GP group (39%). Our results are comparable to other publications, confirming the more appropriate care by a type A FLS [13, 15, 16, 21, 22]. The remaining difficulty is adherence to the treatment, which seems to be better with intravenous, bisphosphonates. Indeed, adherence to osteoporosis medication is well known to decline with time, but seems to be better with an annual intravenous infusion. In our study, we did not record adherence to oral medication, but most patients received intravenous medication (52.5% in the FLS group, 31.2% in the GP group) [6].
In our study, a significantly higher proportion of patients had new nonvertebral fragility fractures in the GP group compared with patients treated and followed by the FLS. These results are comparable to other studies [21, 23] and are relevant, since “less intense” FLS models have not demonstrated any improvement on refracture rates [6]. However, data about vertebral fractures are not known and, among published studies evaluating the rate of new fractures after FLS implementation, the majority excluded vertebral fractures [23, 24]. We documented eight vertebral fractures in the FLS group (seven of which were asymptomatic) versus none in the GP group in the first year. This reflects the routine DXA and VFA evaluations performed in the FLS group (not or rarely performed by the GPs) rather than any true inter-group difference in fracture incidence and highlights the persistent challenge of the diagnosis of vertebral fractures: more than 50% are misdiagnosed [25–28], even in a FLS [28, 29]. Education, teaching [30], and implementation of systematic VFA in addition to DXA could decrease this level of misdiagnosis. Nevertheless, even if the VFA has a high specificity, the sensitivity remains low, and osteoporotic patients with new back pain should have a spinal X-Ray in order to confirm a new vertebral fracture [31]. This diagnosis reflects the severity of the disease and has an impact on the choice of the treatment.
In terms of death, we failed to identify any statistically significant difference between the FLS and GP groups, after adjusting for age and previous fracture site. However, these results might be biased for several reasons. For example, since the CHUV is a university-based hospital, it is reasonable to expect that patients with more comorbid conditions would be more likely to choose follow-up by the FLS team. Since we did not collect data on comorbid conditions, we cannot rule this possibility out. Few FLS studies have used mortality as an outcome. However, some of them have described a 20 to 35% decrease in mortality [23, 32].
Our study has limitations. First, for patients followed by their GP, data were collected by asking patients (or family members) to complete a questionnaire. It appeared clear that most of these patients were not well informed about their management. For example, 28% of patients did not know if they had undergone a DXA evaluation, 19% of those having DXA did not know the results and 23.4% did not know if they had received osteoporosis-specific medication. It is well known that reduced familiarity with treatment decreases adherence [33–36]. This point underlines the importance of increasing patients’ education through the FLS and through GP education. A second limitation pertains to patient age and the sites of fracture. Older patients were more likely to have hip fractures and to be followed up by their GP, as already observed in other studies [21, 22]. As such, we failed to observe any significant decrease in the 1-year rate of death in the FLS group relative to patients followed up by their GP when the analysis was adjusted for age and fracture site.
These limitations aside, several finding are worthy of notice. First, the management of osteoporosis in our hospital’s catchment area improved from 2004–2006 (date of the nationwide survey) to 2011. All results were highly significant when the patient was managed by our type A FLS, and prescription of specific treatment increased when the patient decided to be followed up by the GP. We had previously informed local GPs about the results of the nationwide survey, and about our reasons for establishing a fracture liaison service type A at our hospital. We informed them when we started the CHUV FLS. Potentially, either or both of these actions had some positive impact upon their osteoporosis management. These results are in accordance with the literature and could by be easily generalisable in the others osteoporosis centres through Switzerland.
In conclusion, our study adds further support to the fact that fracture liaison services enhance the detection and subsequent management of patients with a major osteoporotic fracture. Such services may also reduce the incidence of future fractures. Detection of vertebral fractures remains low, and an FLS dedicated to spine management (FLS spine) are currently in development.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Svedbom A , Ivergård M , Hernlund E , Rizzoli R , Kanis JA . Epidemiology and economic burden of osteoporosis in Switzerland. Arch Osteoporos. 2014;9(1):187. doi:.https://doi.org/10.1007/s11657-014-0187-y
2 Rosengren BE , Karlsson MK . The annual number of hip fractures in Sweden will double from year 2002 to 2050: projections based on local and nationwide data. Acta Orthop. 2014;85(3):234–7. doi:.https://doi.org/10.3109/17453674.2014.916491
3 Friedman SM , Mendelson DA . Epidemiology of fragility fractures. Clin Geriatr Med. 2014;30(2):175–81. doi:.https://doi.org/10.1016/j.cger.2014.01.001
4 Åkesson K , Marsh D , Mitchell PJ , McLellan AR , Stenmark J , Pierroz DD , et al.; IOF Fracture Working Group. Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24(8):2135–52. doi:.https://doi.org/10.1007/s00198-013-2348-z
5 Ganda K , Puech M , Chen JS , Speerin R , Bleasel J , Center JR , et al. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int. 2013;24(2):393–406. doi:.https://doi.org/10.1007/s00198-012-2090-y
6 Walters S , Khan T , Ong T , Sahota O . Fracture liaison services: improving outcomes for patients with osteoporosis. Clin Interv Aging. 2017;12:117–27. doi:.https://doi.org/10.2147/CIA.S85551
7 Suhm N , Lamy O , Lippuner K ; OsteoCare study group. Management of fragility fractures in Switzerland: results of a nationwide survey. Swiss Med Wkly. 2008;138(45-46):674–83. https://smw.ch/en/article/doi/smw.2008.12294/.
8 Hernlund E , Svedbom A , Ivergård M , Compston J , Cooper C , Stenmark J , et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8(1-2):136. doi:.https://doi.org/10.1007/s11657-013-0136-1
9 Lippuner K , Johansson H , Kanis JA , Rizzoli R . Remaining lifetime and absolute 10-year probabilities of osteoporotic fracture in Swiss men and women. Osteoporos Int. 2009;20(7):1131–40. doi:.https://doi.org/10.1007/s00198-008-0779-8
10Office fédéral de la santé publique. Ostéoporose et chutes des personnes âgées, une approche de santé publique. Berne: Office fédéral de la santé publique; 2004.
11 Kanis JA , Borgström F , Compston J , Dreinhöfer K , Nolte E , Jonsson L , et al. SCOPE: a scorecard for osteoporosis in Europe. Arch Osteoporos. 2013;8(1-2):144. doi:.https://doi.org/10.1007/s11657-013-0144-1
12 Kanis JA , Svedbom A , Harvey N , McCloskey EV . The osteoporosis treatment gap. J Bone Miner Res. 2014;29(9):1926–8. doi:.https://doi.org/10.1002/jbmr.2301
13 Shipman KE , Stammers J , Doyle A , Gittoes N . Delivering a quality-assured fracture liaison service in a UK teaching hospital-is it achievable? Osteoporos Int. 2016;27(10):3049–56. doi:.https://doi.org/10.1007/s00198-016-3639-y
14 Murray AW , McQuillan C , Kennon B , Gallacher SJ . Osteoporosis risk assessment and treatment intervention after hip or shoulder fracture. A comparison of two centres in the United Kingdom. Injury. 2005;36(9):1080–4. doi:.https://doi.org/10.1016/j.injury.2005.03.012
15 Majumdar SR , Beaupre LA , Harley CH , Hanley DA , Lier DA , Juby AG , et al. Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med. 2007;167(19):2110–5. doi:.https://doi.org/10.1001/archinte.167.19.2110
16 Ruggiero C , Zampi E , Rinonapoli G , Baroni M , Serra R , Zengarini E , et al. Fracture prevention service to bridge the osteoporosis care gap. Clin Interv Aging. 2015;10:1035–42.
17 Cosman F , Nicpon K , Nieves JW . Results of a fracture liaison service on hip fracture patients in an open healthcare system. Aging Clin Exp Res. 2017;29(2):331–4. doi:.https://doi.org/10.1007/s40520-016-0545-2
18 Dell R , Greene D , Schelkun SR , Williams K . Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am. 2008;90(Suppl 4):188–94. doi:.https://doi.org/10.2106/JBJS.H.00628
19 Siris ES , Miller PD , Barrett-Connor E , Faulkner KG , Wehren LE , Abbott TA , et al. Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA. 2001;286(22):2815–22. doi:.https://doi.org/10.1001/jama.286.22.2815
20 Popp AW , Meer S , Krieg MA , Perrelet R , Hans D , Lippuner K . Bone mineral density (BMD) and vertebral trabecular bone score (TBS) for the identification of elderly women at high risk for fracture: the SEMOF cohort study. Eur Spine J. 2016;25(11):3432–8.
21 Van der Kallen J , Giles M , Cooper K , Gill K , Parker V , Tembo A , et al. A fracture prevention service reduces further fractures two years after incident minimal trauma fracture. Int J Rheum Dis. 2014;17(2):195–203. doi:.https://doi.org/10.1111/1756-185X.12101
22 Dehamchia-Rehailia N , Ursu D , Henry-Desailly I , Fardellone P , Paccou J . Secondary prevention of osteoporotic fractures: evaluation of the Amiens University Hospital’s fracture liaison service between January 2010 and December 2011. Osteoporos Int. 2014;25(10):2409–16. doi:.https://doi.org/10.1007/s00198-014-2774-6
23 Huntjens KM , van Geel TA , van den Bergh JP , van Helden S , Willems P , Winkens B , et al. Fracture liaison service: impact on subsequent nonvertebral fracture incidence and mortality. J Bone Joint Surg Am. 2014;96(4):e29. doi:.https://doi.org/10.2106/JBJS.L.00223
24 Nakayama A , Major G , Holliday E , Attia J , Bogduk N . Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int. 2016;27(3):873–9. doi:.https://doi.org/10.1007/s00198-015-3443-0
25 Casez P , Uebelhart B , Gaspoz JM , Ferrari S , Louis-Simonet M , Rizzoli R . Targeted education improves the very low recognition of vertebral fractures and osteoporosis management by general internists. Osteoporos Int. 2006;17(7):965–70. doi:.https://doi.org/10.1007/s00198-005-0064-z
26 Delmas PD , van de Langerijt L , Watts NB , Eastell R , Genant H , Grauer A , et al.; IMPACT Study Group. Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20(4):557–63. doi:.https://doi.org/10.1359/JBMR.041214
27 Sosa M , Saavedra P , Gómez-de-Tejada MJ , Navarro MD , Jódar E , García E , et al. High prevalence of undiagnosed vertebral fractures in patients suffering from hip fracture at their hospital admission: weak concordance among observers. Aging Clin Exp Res. 2015;27(6):835–9. doi:.https://doi.org/10.1007/s40520-015-0365-9
28 Reniu AC , Ong T , Ajmal S , Sahota O . Vertebral fracture assessment in patients presenting with a non-hip non-vertebral fragility fracture: experience of a UK Fracture Liaison Service. Arch Osteoporos. 2017;12(1):23. doi:.https://doi.org/10.1007/s11657-017-0318-3
29 Gehlbach SH , Bigelow C , Heimisdottir M , May S , Walker M , Kirkwood JR . Recognition of vertebral fracture in a clinical setting. Osteoporos Int. 2000;11(7):577–82. doi:.https://doi.org/10.1007/s001980070078
30 Aubry-Rozier B , Fabreguet I , Iglesias K , Lamy O , Hans D . Impact of level of expertise versus the statistical tool on vertebral fracture assessment (VFA) readings in cohort studies. Osteoporos Int. 2017;28(2):523–7. doi:.https://doi.org/10.1007/s00198-016-3757-6
31 Lee JH , Lee YK , Oh SH , Ahn J , Lee YE , Pyo JH , et al. A systematic review of diagnostic accuracy of vertebral fracture assessment (VFA) in postmenopausal women and elderly men. Osteoporos Int. 2016;27(5):1691–9. doi:.https://doi.org/10.1007/s00198-015-3436-z
32 Hawley S , Javaid MK , Prieto-Alhambra D , Lippett J , Sheard S , Arden NK , et al.; REFReSH study group. Clinical effectiveness of orthogeriatric and fracture liaison service models of care for hip fracture patients: population-based longitudinal study. Age Ageing. 2016;45(2):236–42. doi:.https://doi.org/10.1093/ageing/afv204
33 Wu F , Laslett LL , Wills K , Oldenburg B , Jones G , Winzenberg T . Effects of individualized bone density feedback and educational interventions on osteoporosis knowledge and self-efficacy: a 12-yr prospective study. J Clin Densitom. 2014;17(4):466–72. doi:.https://doi.org/10.1016/j.jocd.2014.07.008
34 Winzenberg T , Oldenburg B , Frendin S , De Wit L , Riley M , Jones G . The effect on behavior and bone mineral density of individualized bone mineral density feedback and educational interventions in premenopausal women: a randomized controlled trial [NCT00273260] [NCT00273260]. BMC Public Health. 2006;6(1):12. doi:.https://doi.org/10.1186/1471-2458-6-12
35 Sale JE , Gignac MA , Frankel L , Hawker G , Beaton D , Elliot-Gibson V , et al. Patients reject the concept of fragility fracture--a new understanding based on fracture patients’ communication. Osteoporos Int. 2012;23(12):2829–34. doi:.https://doi.org/10.1007/s00198-012-1914-0
36 Giangregorio L , Dolovich L , Cranney A , Adili A , Debeer J , Papaioannou A , et al. Osteoporosis risk perceptions among patients who have sustained a fragility fracture. Patient Educ Couns. 2009;74(2):213–20. doi:.https://doi.org/10.1016/j.pec.2008.08.001
No financial support and no other potential conflict of interest relevant to this article was reported.