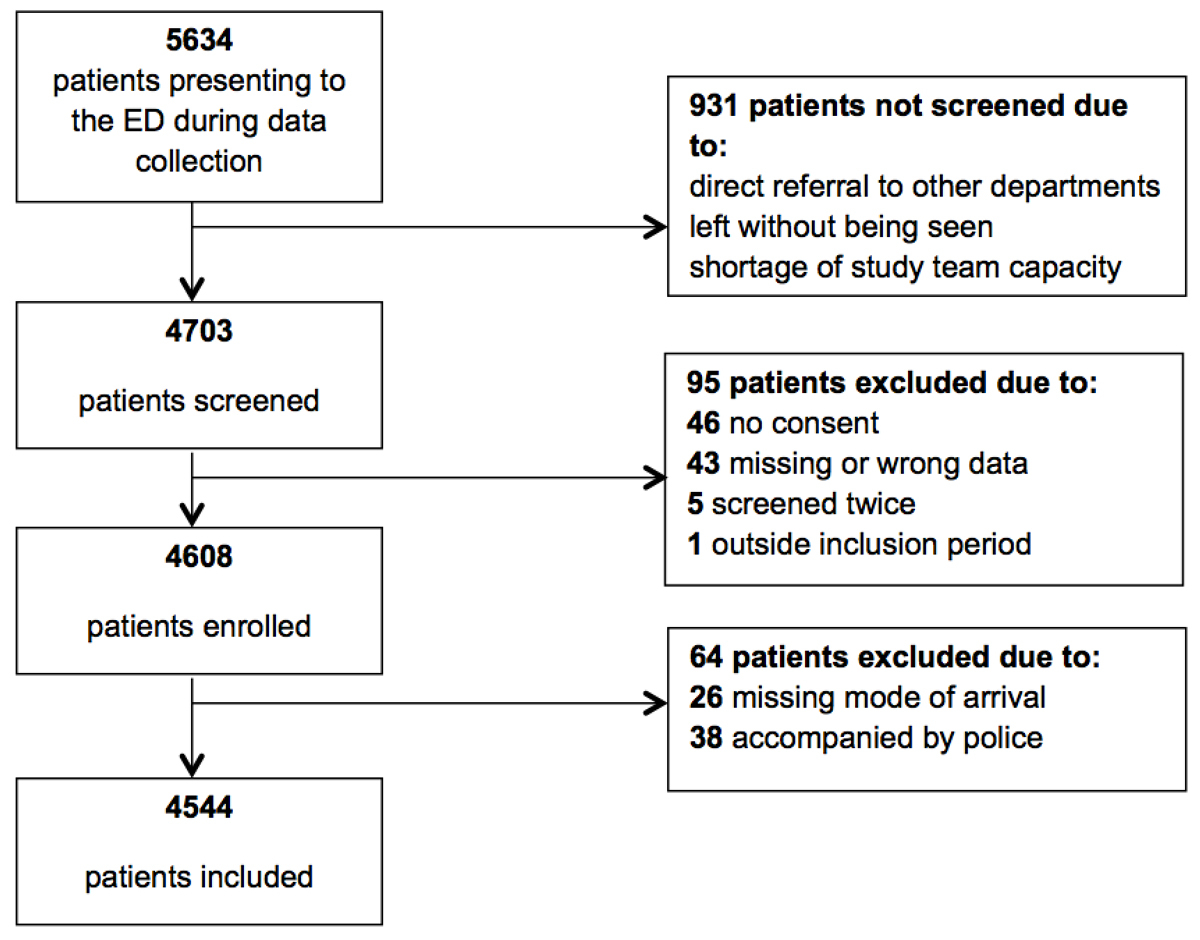
Figure 1 Overview of inclusion of patients.
DOI: https://doi.org/10.4414/smw.2017.14554
Emergency medical services (EMS) are difficult to compare between different healthcare systems. Therefore, it is important to gather knowledge about the performance of individual EMS, as well as the population referred by the service. Since the large majority of primary EMS deployments are referrals to emergency departments (EDs), data about the group of patients referred by EMS to EDs are of great importance to hospitals and emergency physicians. Healthcare providers need to be aware of risks inherent to specific groups of patients, such as migrants, the elderly, or EMS patients, because of early risk stratification and resource allocation. In order to refine strategies optimising resource allocation in the ED, different approaches have been tested, including various front-end interventions intended to improve patient flow through the ED while ensuring safety [1–3]. The introduction of triage liaison physicians, team triage and triage-based protocols has been shown to improve patient outcomes [3–5]. However, transporting clinical tools to new settings is not an easy task, and triage still shows great variation in procedure and outcome [6]. The early identification of patients at risk could therefore benefit certain groups, such as EMS-referred patients, if resources can be allocated immediately.
To date, there is conflicting evidence as to whether EMS referral is an independent predictor of outcome. Some studies showed that EMS/ambulance patients are often older, have lower incomes and are more severely ill [7]. Little is known about outcomes in EMS patients. Higher admission rates, greater use of resources, longer ED length of stay (LOS), and higher mortality have been reported [7–10]. Only a few studies could show an association between EMS referral and long-term mortality – this knowledge being restricted to patients with myocardial infarction or acute chest pain [11–13]. It has never been shown in a general EMS population. We therefore conducted a prospective study in an ED “all-comer” population in order to test the hypothesis that EMS referral is an independent predictor of admission to hospital and intensive care unit (ICU), acute morbidity, use of resources, length of stay in the ED, total length of stay, follow up presentations, and mortality in patients presenting to the ED.
This prospective observational study was conducted in the ED of University Hospital Basel, Switzerland. The hospital has 700 beds and an annual census of over 50 000 adult emergency patients. The ED is responsible for all acute patients, except for paediatric, ophthalmological and gynaecological patients, who are treated nearby. Data collection took place from 21 October to 11 November 2013, and from 1–23 February 2015. Ethical approval of the study was given by the local ethics committee (http://www.eknz.ch, Ref. No. 236/13)
During the study periods, all patients presenting to the ED were eligible. Patients lacking information about mode of arrival/referral, patients accompanied by the police and patients who did not give consent were excluded.
During the study period, data were collected consecutively 24 hours a day, 7 days a week. A study team consisting of medically trained staff received instruction on how to gather data from the hospital’s electronic health records and how to systematically interview patients, patients’ proxies, emergency physicians and emergency nurses. Printed questionnaires were used to report all results; a copy of the questionnaire is provided in appendix 1, available in a separate file for downloading. Data in the questionnaires were check-boxed on a machine-readable product provided by HCRI (Health Care Research Institute AG, Zurich, Switzerland). Validation was done by an internal review of each individual form, followed by an external validation by the company providing the technology. For retrospective chart review, the guidelines from Worster et al. were fulfilled for 8 out of 12 criteria (except for criteria 5, 6, 7, and 8) [14]. Disagreements were resolved by discussion in the group of authors.
All patients presenting to the ED were registered in the electronic health record. Each patient was personally attended by a member of the study team during the whole ED stay. All data collected were immediately recorded on the questionnaire. Every patient was triaged, in accordance with the German version of the Emergency Severity Index (ESI) [6], by either an emergency nurse or an emergency physician [3]. Patients, patients’ proxies, and emergency physicians and nurses were interviewed immediately after triage. Finally, all examinations requested by emergency physicians were recorded. End of ED work-up (defining ED-LOS) was defined as transfer to another department or discharge.
Data about the patient’s characteristics (age, gender, origin) and disposition (hospitalisation, ICU admission) as well as in-hospital mortality and follow-up presentations were retrieved from the electronic health record. An individual patient ID number was used to match the study database with the electronic health record database. After matching, the study database was anonymised.
One-year follow-up was obtained from the electronic health record and by telephone calls with the patient, proxies, primary-care physicians, or by written communication with the primary-care physician. For patients with residency in Basel, the date of death was retrieved from the registry office. Date of death (dd.mm.yyyy) or “period of death” (month.year) were recorded in the database.
EMS referral was defined as all ambulance transports or transfers, all air ambulance transports or transfers, and all patient transfers from other hospitals in the surrounding area (50–70 km) presenting primarily to the ED before admission. All patients referred from hospitals outside Switzerland (for example, in Germany or France) arriving by ambulance and undergoing ED evaluation were also included.
Mode of arrival/referral was assigned to one of nine categories: self-referred, referred by a primary-care physician, referred by other physician (e.g., specialist), referred by other hospital / care centre, referred by other medical care facilities, referred by outpatient clinic, referred by EMS with or without an emergency physician (air medical transport included), or accompanied by police.
Disease severity ratings were reported at the time of presentation, and defined as the subjective impression of disease severity reported on a numeric rating scale (NRS) from 0 (not sick at all) to 10 (extremely sick). Patient’s impression was expressed as the answer to the question: “How ill do you feel right now?” The impressions of emergency physicians and nurses, and patients’ proxies were expressed as the answer to the question: “How ill does this patient look right now?”
ESI category was defined as the priority to be seen according to the ESI triage algorithm.
Hospital admission was defined as transfer to another department or hospital directly after the end of ED work-up. A minimum of one overnight stay in a registered hospital bed was required.
ICU admission was defined as any admission to a medical, surgical or intermediate care unit, as well as any stroke unit or neurosurgical intensive care, occurring either as immediate transfer from the ED or during the patient’s index hospital stay.
Acute morbidity was defined, as previously described [15], as any acute condition that requires immediate specific medical therapy, invasive procedures, prolonged monitoring, or any fracture.
Resources were defined as the total number of examinations (X-ray, ultrasound, echocardiography, duplex sonography, endoscopy, computed tomography (CT) scan, magnetic resonance imaging, interventional radiology, or consultation by a specialist) requested during ED workup.
Emergency department length of stay (ED LOS) was defined as time in minutes between time of arrival and time of discharge or transfer to other departments or hospitals.
Total length of stay was defined as the time in days spent in hospital during the index hospitalisation.
Follow up presentations were defined as all presentations to University Hospital Basel within a year from first presentation. All outpatient visits and all hospitalisations accounted for follow-up presentations.
In-hospital mortality was death occurring in the ED or during the index hospitalisation.
One-year mortality was defined as any death occurring within a year from presentation. To calculate 1-year mortality, presentation day and exact date of death were required. For patients with more than one presentation during the study period, one case was randomly selected to calculate the 1-year mortality. Random selection was performed in a computerised and automated fashion. For patients with an unknown exact date, but known “period of death” (e.g., March 2015), date of death was defined as the first day of the period of death (in the previous example 1 March 2015). Bias effect was assessed through extreme-case scenario simulation and analysis of difference.
Overall sample characteristics were determined in the descriptive analysis. Homogeneity of variance was tested using Levene’s Test. Chi-squared tests, exact Fisher test and student T-tests with corresponding p-values were used for comparison between EMS referral and non-EMS referral.
Univariate and multivariate (age and gender adjusted) regression models were performed to estimate the association between EMS referral and the various response variables. For binary response variables (hospital admission, ICU admission, acute morbidity, in-hospital mortality, and 1-year mortality), logistic regression models were used. Results were expressed as the ratio of odds (ORs) with 95% confidence intervals (CIs) and corresponding p-value. For metric response variables, linear regression models (ED LOS, in-hospital LOS) and Poisson regression model (resources, follow up presentation) were used. For linear regression models, results were expressed as differences of means with 95% CIs and corresponding p-values. For ED LOS, the values were also log-transformed and results were expressed as geometric mean ratios (GMRs) with 95% CIs and corresponding p-values. For Poisson regression models, a quasi-Poisson distribution was used and results were expressed as inference rate ratios (IRRs) with 95% CIs and corresponding p-values.
For all calculations, a p-value below 0.05 was considered to be significant.
Statistical analysis was performed using the statistics software package SPSS (IBM SPSS Statistics 22) for distributions and R (version 3.3.1) for regression analyses.
Of all 5634 patients presenting to the ED during the study period, 4703 (83.5%) were screened for inclusion. Questionnaires of 4608 patients were validated. Twenty-six patients were excluded because of missing data about mode of arrival. Thirty-eight patients were excluded because they were accompanied by police. Finally, 4544 (80.6%) patients were included (fig. 1), and of these 94.3% completed the 1-year follow up.
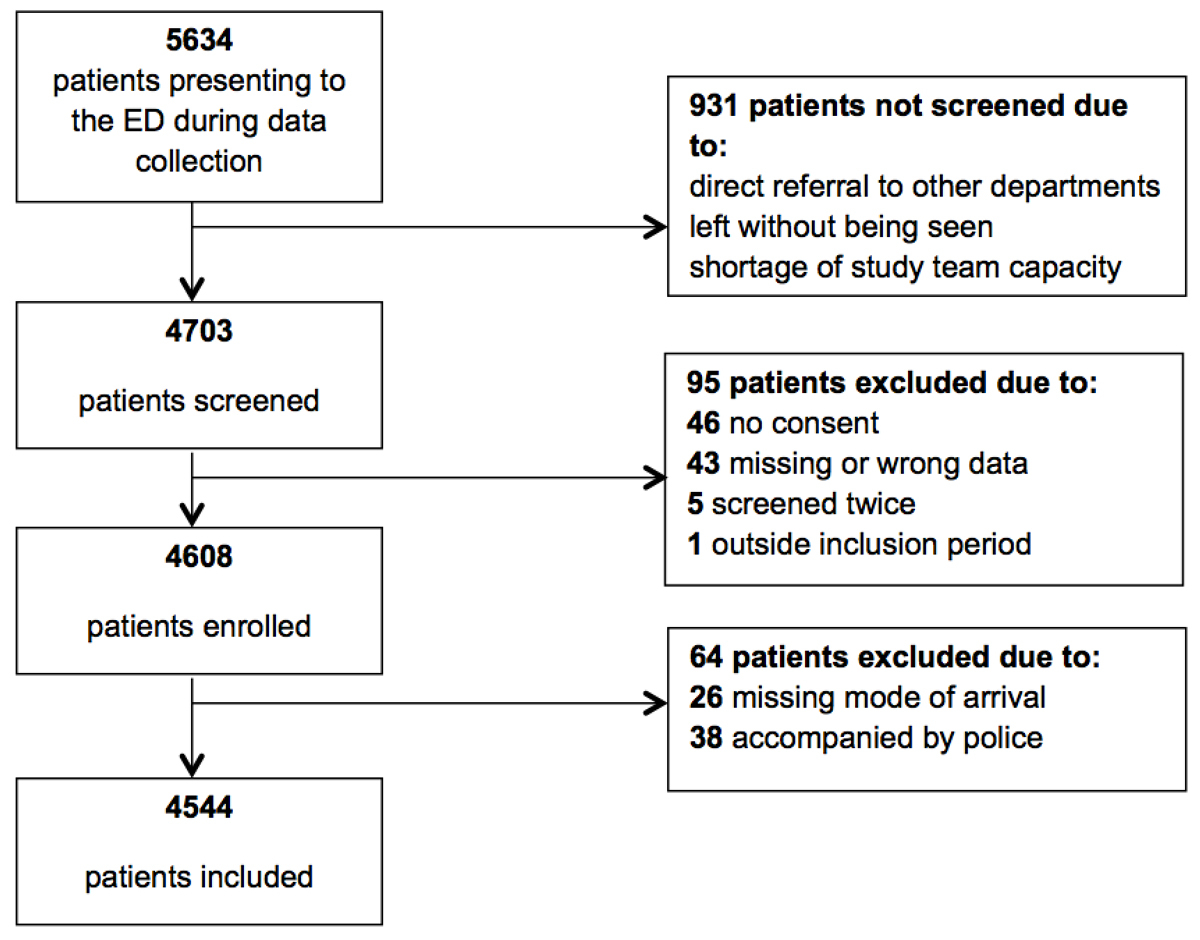
Figure 1 Overview of inclusion of patients.
Median age was 51 years and 51.5% of the patients were male. The majority of patients were assigned ESI categories 2 to 4 (94.5%), with the highest prevalence in ESI category 3 (38.8%). EMS referral without an emergency physician (19.8%) and with an emergency physician (air and ground transport, 3%) was reported for almost one fourth of the included patients. Of the walk-in patients (77.2%), the vast majority (83.5%) were self-referred (table 1).
Table 1 Characteristics of 4544 included patients.
| Age in years, median (range) | 51 | (14–106) |
| Male sex, n (%) | 2338 | (51.5) |
| Origin | ||
| Middle/North Europe, n (%) | 3086 | (67.9) |
| Mediterranean, n (%) | 435 | (9.6) |
| Southeast Europe, n (%) | 244 | (5.4) |
| Eastern Europe, n (%) | 159 | (3.5) |
| Turkey, n (%) | 282 | (6.2) |
| Africa, n (%) | 116 | (2.6) |
| Asia, n (%) | 141 | (3.1) |
| North America/Australia, n (%) | 24 | (0.5) |
| Central/South America, n (%) | 42 | (0.9) |
| No data, n (%) | 15 | (0.3) |
| ESI | ||
| 1, n (%) | 93 | (2.0) |
| 2, n (%) | 1001 | (22.0) |
| 3, n (%) | 1765 | (38.8) |
| 4, n (%) | 1530 | (33.7) |
| 5, n (%) | 144 | (3.2) |
| No data, n (%) | 11 | (0.2) |
| Mode of arrival | ||
| Self-referred, n (%) | 2929 | (64.5) |
| Referred by PCP, n (%) | 324 | (7.1) |
| Referred by other physician/specialist, n (%) | 81 | (1.8) |
| Referred by other hospital / care centre, n (%) | 147 | (3.2) |
| Referred by other medical care facilities, n (%) | 24 | (0.5) |
| Referred by outpatient clinic, n (%) | 3 | (0.1) |
| EMS with EP, n (%) | 136 | (3.0) |
| EMS without EP, n (%) | 900 | (19.8) |
EMS = emergency medical services; EP emergency physician; ESI = Emergency Severity Index; PCP = primary-care physician
One third of all included patients (33.5%) were admitted to hospital, 6.5% were admitted to intensive care, and 40.7% experienced acute morbidity. Mean number of resources used per patient was 1.84 (±1.33), mean time spent in the ED was 226.9 (±171.7) minutes, and mean time in days spent in hospital was 7.15 (±7.7). The mean number of follow-up presentations was 2.15 (±2.98). Of all patients, 1.6% died in hospital and 6.2% died within a year from presentation.
EMS patients were significantly older than walk-in patients (67.3 ± 20.6 vs 48.8 ± 20.5 years, p <0.001). Significantly more female patients were in the EMS group (52 vs 48%, p = 0.012). Mean ESI category showed a significantly higher acuity in EMS patients (2.55 ± 0.76) than in walk-in patients (3.31 ± 0.82, p < 0.001) (table 2). Disease severity ratings (DSR) of emergency physicians and nurses were significantly higher for EMS patients, but the ratings of patients and proxies were not (supplementary table S1 and fig. S1 in appendix 2).
Table 2 Outcomes stratified by mode of arrival and results of the multivariate analysis (adjusted for age and gender).
|
All patients
(n = 4544) |
EMS patients
(n = 1038) |
Walk-in patients
(n =3506) |
p-value | Multivariate analysis | ||
|---|---|---|---|---|---|---|
|
EMS patients
(reference = walk-in patients) |
p-value | |||||
| Age, mean years (SD) | 53.0 (21.9) | 67.3 (20.6) | 48.8 (20.5) | <0.001* | – | - |
| Male sex, n (%) | 2338 (51.5) | 497 (48.0) | 1841 (52.5) | 0.012** | – | - |
| ESI, mean category (SD) | 3.14 (0.87) | 2.55 (0.76) | 3.31 (0.82) | <0.001* | – | - |
| Admission to hospital, n (%) | 1523 (33.5) | 687 (66.3) | 836 (23.8) | – | 3.8 (3.2–4.5)† | <0.001 |
| ICU admission, n (%) | 296 (6.5) | 174 (16.8) | 122 (3.5) | – | 4.2 (3.2–5.5)† | <0.001 |
| Acute morbidity, n (%) | 1848 (40.7) | 624 (60.2) | 1224 (34.9) | – | 1.6 (1.4–1.9)† | <0.001 |
| Resources, mean number (SD) | 1.84 (1.33) | 2.61 (1.24) | 1.61 (1.27) | – | 1.3 (1.3–1.4)‡ | <0.001 |
| ED LOS, mean time (SD) | 226.9 (171.7) | 270.9 (179.7) | 213.8 (167.0) | – | 1.2 (1.1–1.2)§ | <0.001 |
| In-hospital mortality, n (%) | 73 (1.6) | 55 (5.3) | 18 (0.5) | – | 6.4 (2.9–15.6)† | <0.001 |
| One-year mortality, n (%) | 280 (6.2) | 164 (15.8) | 116 (3.3) | – | 2.3 (1.7–3.0)† | <0.001 |
ED = emergency department; EMS emergency medical services; ESI Emergency Severity Index; ICU = intensive care unit; LOS length of stay; SD = standard deviation ED LOS is length of stay in the ED defined as time in minutes between ED presentation and discharge or transfer * Calculated using Student's T-test; ** calculated using χ2-test; † results of logistic regression model, expressed as odds ratios (95% CI); ‡ results of Poisson regression model, expressed as inference rate ratios (95% CI); § results of log-transformed linear regression model, expressed as geometric mean ratios (95% CI)
In multivariate logistic, linear, and Poisson regression models, adjusted for age and gender, a significant positive correlation was found for admission to hospital (OR 3.8, 95% CI 3.2–4.5; p <0.001) and ICU admission (OR 4.2, 95% CI 3.2–5.5, p < 0.001). For resources, a significant linear positive correlation was found (IRR 1.3, 95% CI 1.3–1.4; p <0.001). For ED LOS, a significant positive correlation was found (GMR 1.2, 95% CI 1.1–1.2; p <0.001). For total length of stay, a non-significant positive correlation was found (B 0.1, 95% CI −0.7 – 0.9; p = 0.88). For follow up presentations, a significant, negative correlation was found (IRR 0.8, 95% CI 0.7–0.9 p <0.001). A significant positive correlation was found for in-hospital mortality (OR 6.4, 95% CI 2.9–15.6; p <0.001), and 1-year mortality (OR 2.3, 95% CI 1.7–3.0; p < 0.001) (supplementary table S2).
Univariate analyses showed similar results (data not shown).
The main findings of our study are the positive associations between EMS referral and admission to hospital and ICU, use of resources, length of stay and mortality.
First, the odds of being admitted to hospital and intensive care for EMS patients were about four-fold higher than for walk-in patients. Second, the use of resources and the ED LOS were significantly higher. Third, acute morbidity, defined as immediate requirement for medical attention, was significantly higher in EMS patients. Fourth, and most importantly, EMS patients suffer from an over six-fold increase in in-hospital mortality. This poor outcome holds true for the 1-year follow-up, with an odds ratio of 2.3 for adjusted mortality. These findings are new in terms of a prospective observation in a general EMS population, but can be compared to special EMS populations: a retrospective study on Dutch sepsis patients found an association between EMS referrals with sepsis and admission to both hospital and ICU [16]. An American database analysis, focusing on low acuity patients, reported that ambulance patients are four times more likely to be hospitalised than walk-in patients [17]. Additionally, the association between EMS referral and use of resources, as well as ED LOS, has previously been reported: one study showed that EMS patients used more resources [9]. Another study demonstrated that EMS patients spent more time in the ED [10]. Several studies provided evidence of an association between EMS referral and in-hospital mortality [7, 8, 18, 19], and several authors have shown an association with long-term mortality [11, 12, 20]. However, some of these studies were retrospective [7, 8, 19], with all the inherent problems, such as inclusion bias, and others focused on special groups, such as acute chest pain [11, 12], or trauma [19].
The stronger association between EMS referral and in-hospital mortality as compared to 1-year mortality suggests that for most EMS patients the exposure to an increased risk of mortality appears to be limited to the index presentation. Other publications [13, 18] demonstrated a similar pattern of early versus late mortality for EMS patients suffering from acute myocardial infarction.
The higher mortality in EMS patients may lead to the following conclusions in light of two distinct issues:
First, EMS use can be judged to be appropriate on the basis of adverse outcome. The issue of ambulance misuse has been widely discussed [21, 22]. It may be argued that EMS use depends on acuity of symptoms, such as in patients with suspected myocardial infarction [20]. Alternatively, a higher perceived severity of illness could trigger the use of EMS [23]. However, in our cohort, the patients’ disease severity ratings were not significantly different in EMS patients (table S1 and fig. S1), as opposed to physicians’ and nurses’ disease severity ratings.
Second, the adverse outcomes in EMS patients could be taken as an argument for refining triage tools. At present, none of the widely used tools use EMS referral as a rationale for up-triage. However, considering that the unadjusted odds for short-term mortality are 13.1 (6.3–30.6), this issue should be investigated. Taking the US triage tool as reference, ESI 2 mortality is about twofold higher than ESI 3 mortality, and ESI 2 mortality is lower than the EMS referred patients’ mortality [6].
To summarise our findings, we could confirm our hypothesis that EMS patients are more prone to adverse outcomes. To the best of our knowledge, this is the first prospective study showing an association between EMS referral and 1-year mortality for an all-comer population. Further research should focus on evaluating early interventions, such as reducing ED LOS or up-triaging, in EMS patients in order to reduce adverse outcomes.
Our study had several limitations. First, this was a single-centre study with a limitation to external validity. However, the outcomes shown are comparable to other European studies, in spite of their retrospective or selective nature [11, 12, 16]. Second, in our analysis we only adjusted for age and gender, and other confounders could have been considered. However, as 1-year mortality in an emergency population is driven to about 60% by age and gender [24], we believe that the main confounders have been addressed. Third, admission is an outcome influenced by the healthcare system, culture, and socioeconomic factors. Furthermore, intensive care – due to high cost – may be restricted in certain cases, and is certainly dependent on available resources. However, our admission rates are comparable to reported data in other academic centres, such as Wisconsin, US [25], Limerick, Ireland [26], and the region of New South Wales, Australia [27]. Fourth, we did not analyse or adjust for outcomes according to a prehospital triage score, such as the National Advisory Committee for Aeronautics (NACA) score. Fifth, exact dates of death could not be identified in all patients. In these cases, the date of death was defined as the closest possible date to the day of presentation to the ED. Therefore, long-term mortality could be overestimated. However, we also simulated the inverse scenario with a maximal difference of four patients (0.1%). Finally, we cannot exclude an inclusion bias, since 16.5% of the patients presenting to the ED could not be screened, mostly because of crowding and patients who left without being seen. Therefore, the number of low-acuity patients could be underestimated.
The questionnaire is available as a separate file at: https://smw.ch/en/article/doi/smw.2017.14554/
Table S1 Results of group comparison for mean disease severity ratings of physicians, nurses, patients and patient’s proxies on a numeric rating scale from 0 to 10.
| Disease severity ratings | All patients | EMS patients | Walk-in patients | p-value* | Missing† |
|---|---|---|---|---|---|
| Emergency physician, mean (SD) | 3.9 (2.3) | 5.1 (2.4) | 3.5 (2.1) | <0.001 | 65 (1.4) |
| Emergency nurse, mean (SD) | 4.2 (2.3) | 5.5 (2.3) | 3.8 (2.1) | <0.001 | 77 (1.7) |
| Patient, mean (SD) | 5.1 (2.8) | 5.3 (2.6) | 5.0 (2.8) | 0.236 | 3351(73.7) |
| Patient's proxies, mean (SD) | 6.0 (2.4) | 6.3 (2.5) | 6.0 (2.4) | 0.373 | 4179 (92.0) |
EMS = emergency medical services; SD = standard deviation * Calculated using Student's T-test; † number (%) of the 4544 included patients
Table S2 Results of univariate and multivariate analysis (adjusted for age and gender).
| Univariate | Multivariate | |||
|---|---|---|---|---|
| EMS patients (reference = walk-in patients) | p-value | EMS patients (reference = walk-in patients) | p-value | |
| Admission to hospital* | 6.3 (5.4–7.3) | <0.001 | 3.8 (3.2–4.5) | <0.001 |
| ICU-admission* | 5.6 (4.4–7.2) | <0.001 | 4.2 (3.2–5.5) | <0.001 |
| Acute morbidity* | 2.4 (2.1–2.8) | <0.001 | 1.6 (1.4–1.9) | <0.001 |
| Resources† | 1.6 (1.6–1.7) | <0.001 | 1.3 (1.3–1.4) | <0.001 |
| ED LOS‡ | 1.4 (1.3–1.5) | <0.001 | 1.2 (1.1–1.2) | <0.001 |
| total LOS§ | 0.3 (−0.5 – 1.0) | 0.5 | 0.1 (−0.7 – 0.9) | 0.88 |
| Follow up presentations† | 0.9 (0.8–1.0) | 0.05 | 0.8 (0.7–0.9) | <0.001 |
| In-hospital mortality* | 13.1 (6.3–30.6) | <0.001 | 6.4 (2.9–15.6) | <0.001 |
| One-year mortality* | 5.6 (4.4–7.2) | <0.001 | 2.3 (1.7–3.0) | <0.001 |
ED = emergency department; EMS = emergency medical services; ESI = Emergency Severity Index; LOS = length of stay ED LOS is length of stay in the ED defined as time in minutes between ED presentation and discharge or disposition; total LOS is length of stay in hospital defined as time in days of index hospitalisation; Follow up presentations are all presentation to University Hospital Basel in the 365 days after the initial presentation. * Results of logistic regression model, expressed as odds ratios (95% CI); † results of Poisson regression model, expressed as inference rate ratios (95% CI); ‡ results of log-transformed linear regression model, expressed as geometric mean ratios (95% CI); § results of linear regression model, expressed as estimates (95% CI)
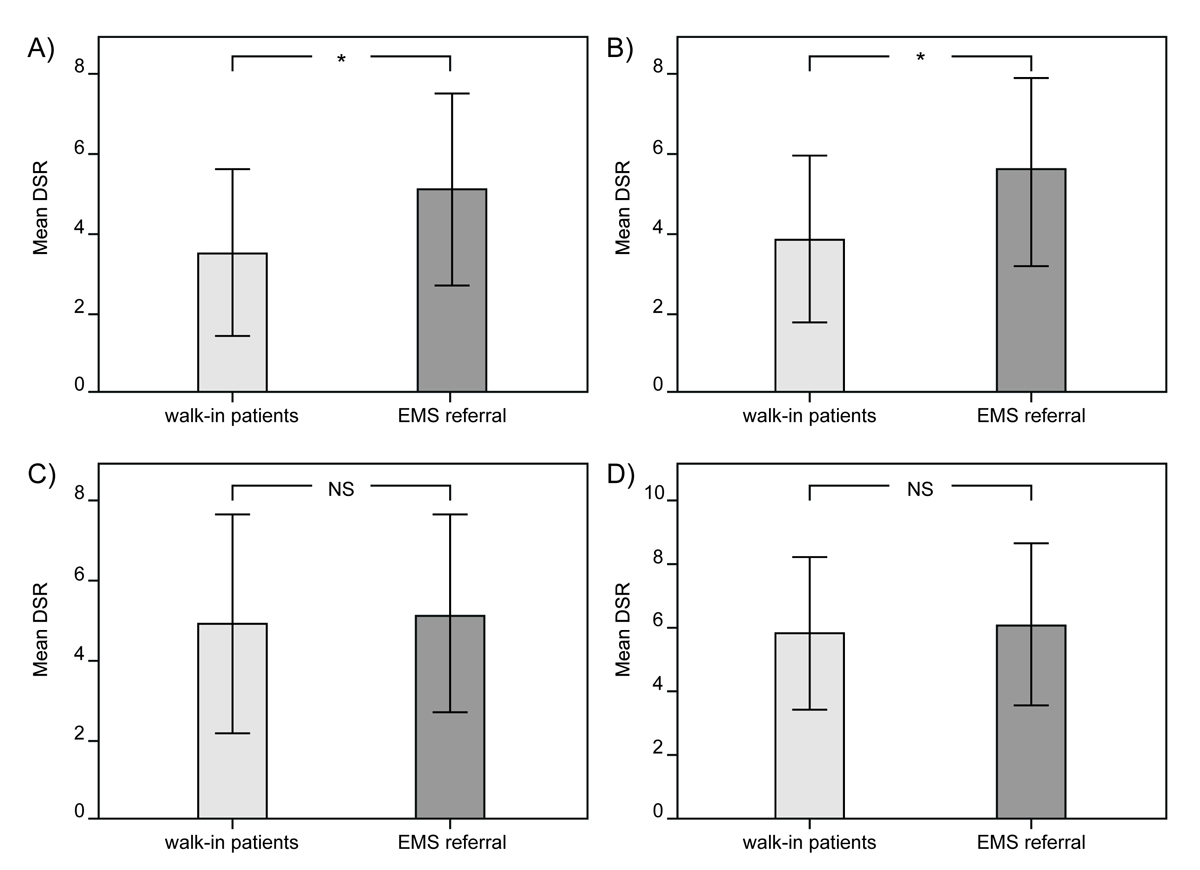
Figure S1 Results of group comparison between EMS referral and walk-in patients for mean disease severity ratings. Comparison of mean disease severity ratings (DSR) between EMS referral and walk-in patients of: (A) emergency physicians, (B) emergency nurses, (C) patients, and (D) patient’s proxies between EMS referral and walk-in patients. * p <0.001; NS = nonsignificant.
We thank the HCRI team for guaranteeing the quality of the data. We thank the medical students for data collection and follow up assessments. We would like to thank Christian Müller, EUDOX Basel, Switzerland for professional statistical analyses.
There were no financial relationships with any organisation that might have an interest in this work. The sponsor of the study was the scientific fund of the University Hospital Basel Emergency Department. It had no influence on the design or the conduct of the study, nor in the interpretation and in the analysis of the data.
The authors did not receive support from any organisation for the presented work. There are no conflicts of interest
1 Ro YS , Shin SD , Song KJ , Cha WC , Cho JS . Triage-based resource allocation and clinical treatment protocol on outcome and length of stay in the emergency department. Emerg Med Australas. 2015;27(4):328–35. doi:.https://doi.org/10.1111/1742-6723.12426
2 Wiler JL , Gentle C , Halfpenny JM , Heins A , Mehrotra A , Mikhail MG , et al. Optimizing emergency department front-end operations. Ann Emerg Med. 2010;55(2):142–160.e1. doi:.https://doi.org/10.1016/j.annemergmed.2009.05.021
3 Lauks J , Mramor B , Baumgartl K , Maier H , Nickel CH , Bingisser R . Medical Team Evaluation: Effect on Emergency Department Waiting Time and Length of Stay. PLoS One. 2016;11(4):e0154372. doi:.https://doi.org/10.1371/journal.pone.0154372
4 Nestler DM , Fratzke AR , Church CJ , Scanlan-Hanson L , Sadosty AT , Halasy MP , et al. Effect of a physician assistant as triage liaison provider on patient throughput in an academic emergency department. Acad Emerg Med. 2012;19(11):1235–41. doi:.https://doi.org/10.1111/acem.12010
5 Soremekun OA , Capp R , Biddinger PD , White BA , Chang Y , Carignan SB , et al. Impact of physician screening in the emergency department on patient flow. J Emerg Med. 2012;43(3):509–15. doi:.https://doi.org/10.1016/j.jemermed.2012.01.025
6 Grossmann FF , Nickel CH , Christ M , Schneider K , Spirig R , Bingisser R . Transporting clinical tools to new settings: cultural adaptation and validation of the Emergency Severity Index in German. Ann Emerg Med. 2011;57(3):257–64. doi:.https://doi.org/10.1016/j.annemergmed.2010.07.021
7 Ruger JP , Richter CJ , Lewis LM . Clinical and economic factors associated with ambulance use to the emergency department. Acad Emerg Med. 2006;13(8):879–85. doi:.https://doi.org/10.1111/j.1553-2712.2006.tb01742.x
8 Anselmi L , Meacock R , Kristensen S , Doran T , Sutton M . Arrival by ambulance explains variation in mortality by time of admission: retrospective study of admissions to hospital following emergency department attendance in England. BMJ Qual Saf. 2017;26(8):613–21.
9 Marinovich A , Afilalo J , Afilalo M , Colacone A , Unger B , Giguère C , et al. Impact of ambulance transportation on resource use in the emergency department. Acad Emerg Med. 2004;11(3):312–5. doi:.https://doi.org/10.1111/j.1553-2712.2004.tb02218.x
10 Downing A , Wilson RC , Cooke MW . Which patients spend more than 4 hours in the Accident and Emergency department? J Public Health (Oxf). 2004;26(2):172–6. doi:.https://doi.org/10.1093/pubmed/fdh141
11 Herlitz J , Hjälte L , Karlson BW , Suserud BO , Karlsson T . Characteristics and outcome of patients with acute chest pain in relation to the use of ambulances in an urban and a rural area. Am J Emerg Med. 2006;24(7):775–81. doi:.https://doi.org/10.1016/j.ajem.2006.03.016
12 Herlitz J , Karlson BW , Bång A , Lindqvist J . Characteristics and outcome for patients with acute chest pain in relation to whether or not they were transported by ambulance. Eur J Emerg Med. 2000;7(3):195–200. doi:.https://doi.org/10.1097/00063110-200009000-00006
13 Boothroyd LJ , Lambert LJ , Segal E , Ross D , Kouz S , Maire S , et al. Comparison of outcomes of ambulance users and nonusers in ST elevation myocardial infarction. Am J Cardiol. 2014;114(9):1289–94. doi:.https://doi.org/10.1016/j.amjcard.2014.07.060
14 Worster A , Bledsoe RD , Cleve P , Fernandes CM , Upadhye S , Eva K . Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448–51. doi:.https://doi.org/10.1016/j.annemergmed.2004.11.021
15 Rohacek M , Nickel CH , Dietrich M , Bingisser R . Clinical intuition ratings are associated with morbidity and hospitalisation. Int J Clin Pract. 2015;69(6):710–7. doi:.https://doi.org/10.1111/ijcp.12606
16 Groenewoudt M , Roest AA , Leijten FM , Stassen PM . Septic patients arriving with emergency medical services: a seriously ill population. Eur J Emerg Med. 2014;21(5):330–5. doi:.https://doi.org/10.1097/MEJ.0000000000000091
17 Durant E , Fahimi J . Factors associated with ambulance use among patients with low-acuity conditions. Prehosp Emerg Care. 2012;16(3):329–37. doi:.https://doi.org/10.3109/10903127.2012.670688
18 So DY , Ha AC , Turek MA , Maloney JP , Higginson LA , Davies RF , et al. Comparison of mortality patterns in patients with ST-elevation myocardial infarction arriving by emergency medical services versus self-transport (from the prospective Ottawa Hospital STEMI Registry). Am J Cardiol. 2006;97(4):458–61. doi:.https://doi.org/10.1016/j.amjcard.2005.08.069
19 Huber S , Crönlein M , von Matthey F , Hanschen M , Seidl F , Kirchhoff C , et al.; TraumaRegister DGU. Effect of private versus emergency medical systems transportation in trauma patients in a mostly physician based system- a retrospective multicenter study based on the TraumaRegister DGU®. Scand J Trauma Resusc Emerg Med. 2016;24(1):60. doi:.https://doi.org/10.1186/s13049-016-0252-1
20 Johansson I , Strömberg A , Swahn E . Ambulance use in patients with acute myocardial infarction. J Cardiovasc Nurs. 2004;19(1):5–12. doi:.https://doi.org/10.1097/00005082-200401000-00004
21 Richards JR , Ferrall SJ . Inappropriate use of emergency medical services transport: comparison of provider and patient perspectives. Acad Emerg Med. 1999;6(1):14–20. doi:.https://doi.org/10.1111/j.1553-2712.1999.tb00088.x
22 Horibata K , Takemura Y . Inappropriate use of ambulance services by elderly patients with less urgent medical needs. Tohoku J Exp Med. 2015;235(2):89–95. doi:.https://doi.org/10.1620/tjem.235.89
23 Toloo GS , FitzGerald GJ , Aitken PJ , Ting JYS , McKenzie K , Rego J , et al. Ambulance use is associated with higher self-rated illness seriousness: user attitudes and perceptions. Acad Emerg Med. 2013;20(6):576–83. doi:.https://doi.org/10.1111/acem.12149
24 Nickel CH , Ruedinger J , Misch F , Blume K , Maile S , Schulte J , et al. Copeptin and peroxiredoxin-4 independently predict mortality in patients with nonspecific complaints presenting to the emergency department. Acad Emerg Med. 2011;18(8):851–9. doi:.https://doi.org/10.1111/j.1553-2712.2011.01126.x
25 Gorski JK , Batt RJ , Otles E , Shah MN , Hamedani AG , Patterson BW . The Impact of Emergency Department Census on the Decision to Admit. Acad Emerg Med. 2017;24(1):13–21.
26 Fogarty EM , Cummins F . The effect of admitted patients in the emergency department on rates of hospital admissions. Emerg Med J. 2013;30(9):766–7. doi:.https://doi.org/10.1136/emermed-2012-201780
27 Dinh MM , Berendsen Russell S , Bein KJ , Chalkley D , Muscatello D , Paoloni R , et al. Trends and characteristics of short-term and frequent representations to emergency departments: A population-based study from New South Wales, Australia. Emerg Med Australas. 2016;28(3):307–12. doi:.https://doi.org/10.1111/1742-6723.12582
The authors had full access to all data used for the study and take responsibility for the integrity of the data and the accuracy of the analysis. R. Bingisser and C.H. Nickel conceived the study, designed the trial, and obtained research funding. R. Bingisser and C.H. Nickel supervised the conduct of the trial and data collection.
K. Weigel, A. Malinovska and F. Schmid undertook recruitment of patients and managed the data, including quality control. C. Müller, EUDOX Basel, Switzerland, provided statistical advice on study design and analysed the data. He was paid for his contributions; R. Bingisser chaired the data quality committee. T. Bosia drafted the manuscript, and all authors contributed substantially to its revision. R. Bingisser takes responsibility for the paper as a whole.
There were no financial relationships with any organisation that might have an interest in this work. The sponsor of the study was the scientific fund of the University Hospital Basel Emergency Department. It had no influence on the design or the conduct of the study, nor in the interpretation and in the analysis of the data.
The authors did not receive support from any organisation for the presented work. There are no conflicts of interest