Safety and effectiveness of labour induction after caesarean section using balloon catheter or oxytocin
DOI: https://doi.org/10.4414/smw.2017.14532
Anda-Petronela
Radana, Sofia
Amylidi-Mohra, Beatrix
Mosimanna, Cedric
Simillionb, Luigi
Raioa, Martin
Muellerabc, Daniel
Surbekab
aDepartment of Obstetrics and Gynaecology, University Hospital and University of Bern, Switzerland
bDepartment of Biomedical Research, University of Bern, Switzerland
cDepartment of Obstetrics, Gynecology, and Reproductive Sciences, Yale University School of Medicine, New Haven, USA
Summary
AIMS OF THE STUDY
Induction of labour after previous caesarean section (CS) is a challenge for obstetricians due to the increased risk of uterine rupture. Common methods for labour induction are balloon catheters and oxytocin as they are considered safe. However, the effectiveness remains unclear as currently available data are limited. Therefore, we aimed to determine safety and effectiveness of balloon catheter or oxytocin for labour induction after CS.
METHODS
We included 179 consecutive women with a previous CS and labour induction in this retrospective study. We performed labour induction using a balloon catheter in case of a Bishop score of <6 and intact membranes, or oxytocin in the case of a Bishop score of >6 and/or premature rupture of membranes. The primary outcome was the rate of successful vaginal deliveries. We adjusted for multiple factors that may have impacted on the rate of vaginal delivery as well. The secondary outcomes were the rate of maternal and neonatal morbidities.
RESULTS
We detected a vaginal delivery success rate of 45.8% in the catheter and of 63.9% in the oxytocin group. We identified previous vaginal birth as an independent predictive factor for successful vaginal delivery in both groups. Induction using oxytocin was a negative predictive factor for neonatal admissions. Multivariate analysis showed that post-term pregnancy decreased the likelihood of vaginal delivery. We did not detect any factors predicting uterine rupture or uterine dehiscence, which occurred with similar frequency in both groups. Finally, the neonatal admission rate was less likely with higher gestational age and oxytocin as an induction method, whereas previous vaginal birth increased the risk.
CONCLUSIONS
Our study indicates that induction of labour with balloon catheter or oxytocin seems to be safe in women with previous CS. Labour induction using a balloon catheter in women with previous CS and unfavourable cervix has a disappointingly low success rate. We identified factors influencing vaginal delivery success rates. Women with previous CS and indications for labour induction should be informed about vaginal birth success rates and the alternative of elective repeat CS needs to be discussed.
Introduction
The caesarean section (CS) rate is increasing. Several factors are contributing to rising CS rates with previous CS being important among these [1, 2]. The dogma “once a caesarean – always a caesarean” [3] existed in the 1970s, and public health authorities and obstetric societies tried to reverse the trend by promoting vaginal birth after caesarean (VBAC). These efforts led to a sharp increase in the VBAC prevalence to approximately 30% in the US in the late 1990s [4]. However, large retrospective studies have showed a small but significant increase in adverse neonatal outcomes and perinatal death in VBAC compared to repeated CS [5]. As a consequence, the VBAC trend reversed rapidly and VBAC prevalence has dropped below 10% in the US.
Despite this trend, VBAC may be safe for many women and an individual risk-benefit analysis is necessary. This is particularly important if labour induction is performed as in case of approximately 20% of women attempting VBAC [4, 6]. This continuing debate is further heated up as the Royal College of Obstetricians and Gynaecologists and the American College of Obstetricians and Gynecologists disagree about the safety of labour induction using prostaglandins after CS [4–10]. Therefore, counselling our patients about labour induction and management strategies is difficult. Furthermore, patients attempting labour induction after CS should be offered not only a safe, but also an effective method [11]. In general, labour induction can be achieved by using several approaches.
Prostaglandins (PGE2) are an effective tool for cervix ripening and induction of labour. However, in the case of VBAC, higher uterine rupture rates compared to spontaneous onset of labour, amniotomy and/or oxytocin were noted [12]. Misoprostol is very effective, but generally contraindicated in women with previous CS due to a high uterine rupture risk. Given the higher uterine rupture risk, the use of prostaglandins for labour induction after CS is not used in our institution [7, 12, 13].
Oxytocin administration is considered a safe method, but may be less effective with an unfavourable Bishop score [14]. An eligible alternative is mechanical induction of labour using a balloon catheter (single or double balloon device). Although this method is widely used, available data on safety and effectiveness after labour induction is scarce [15–17]. Given that balloon catheters and oxytocin are valid options for labour induction in patients attempting VBAC and have lower uterine rupture risk [18], we performed a retrospective cohort study to assess the safety and effectiveness of labour induction after CS using balloon catheters or oxytocin. Given that multiple factors may influence VBAC success, we aimed to determine single and multi-variant parameters in our cohort as well [19].
Material and methods
We performed a retrospective cohort study at our tertiary referral centre at the University Hospital of Bern. We included all consecutive singleton pregnancies delivered between January 2003 and December 2014 who underwent VBAC and labour induction after 24 weeks of gestation. We excluded all pregnancies with lethal congenital anomalies and pregnancies with antepartum intrauterine fetal demise, as well as patients with additional surgical procedures that led to opening of the uterine cavity, such as myomectomy. Importantly, patients with spontaneous onset of labour were not taken into consideration.
We performed labour induction either by using a transcervical balloon catheter for cervical ripening, or by administrating oxytocin, depending on the Bishop score and membrane rupture status. The Bishop score is an obstetric cervix scoring method assessing the following parameters on digital vaginal examination: cervical dilation, effacement, position and consistency, and fetal position. It is an accurate, cost- effective cervical evaluation method prior to induction of labour [20]. In patients with a Bishop score > 6 with intact membranes or with ruptured membranes, we used oxytocin. We administrated 5 IU oxytocin in 500 ml of a sodium chloride and glucose solution as follows: begin with 12 ml/h and increase the dosage every 15 minutes by 21ml/h until development of regular contractions or until reaching the maximum dosage of 120 ml/h, for maximum of 6 hours. In patients with a Bishop score <6 and intact membranes, we inserted the balloon catheter transcervically and inflated it with sterile 0.9% saline solution (60 ml in the single balloon Foley catheter and maximum 80 ml in each balloon of a double device Cook® catheter). There was no traction applied on the catheter. The catheter remained in place until spontaneously expelled or until start of active labour. If neither happened, the catheter was removed after 24 hours and oxytocin was administered. If the cervix remained unfavourable after 6 hours of oxytocin infusion, induction was classified as unsuccessful and subsequently CS was performed. Artificial rupture of membranes (ARM) was performed whenever technically feasible and progressive cervical dilatation was missing. We performed ARM by using an amniotic membrane perforator. We are aware that other centres have different internal guidelines or use different techniques and protocols for the induction of labour after CS, so the results may have a limited external validity.
The primary outcome of the study was successful vaginal delivery, either spontaneous or assisted. We defined assisted vaginal delivery as vaginal delivery using vacuum or forceps. Spontaneous and assisted delivery were also assessed as independent outcomes in the subsequent statistical analysis. Secondly, we evaluated the incidence of maternal and fetal adverse outcomes as well as the influence of maternal factors on the delivery mode. We assessed the following maternal data: maternal age, gestational age at the point of labour induction, parity, previous vaginal delivery, indications for labour induction and previous CS, and need for oxytocin infusion during labour. We assessed the following adverse maternal outcomes: intrapartum infection and postpartum haemorrhage, defined as a total blood loss of >500 ml in the case of vaginal delivery and a total blood loss of >1000 ml in the case of CS. In addition, we defined uterus rupture as the uterus content reaching the abdominal cavity. The uterine dehiscence (“incomplete” uterine rupture) was noted when the surgeon identified a thin or incomplete uterine rupture (absence of myometrium between the amniotic membrane and peritoneum). We assessed the following fetal outcomes: fetal weight, APGAR score after 5 minutes, arterial pH values and neonatal admission after birth. We divided the correlations into clinically significant and non-significant. Clinically non-significant correlations were defined as correlations having no impact on the decision process (induction of labour after CS). One example is the risk of “no perineal laceration”, as this is not the primary goal of labour induction. Another example is the fetal weight. It is expected that the fetal weight is higher if we induce labour due to post-term pregnancy.
The study was approved by the Ethics Committee of the Canton of Bern.
To calculate the impact of the induction method on delivery mode, we used Fisher's exact test. To obtain a confidence interval for the true log-odds ratio, we calculated the log-odds ratio for 10,000 bootstrap replicates. To detect individual correlations (one-to-one correlations), both within the predictive variables and between the predictive and outcome variables, we fitted a simple generalised linear model (glm) for each variable pair, where one variable is the dependent and the other the independent. Notably, using glms allows assessment of correlations between both numerical and categorical variables. Each model obtained was compared using a χ2-test to a null model that only assumes a constant value for the dependent variable. The resulting p-value was corrected for multiple testing using the Benjamini-Hochberg method. Only correlation models with an adjusted p-value of 0.01 were retained. Finally, we used a compound model to determine which combinations of predictive variables gave the best prediction for each of the outcome variables. This analysis revealed more subtle correlations that were not selected by the one-to-one analysis. We accomplished this analysis by matching all models consisting of any combination of the predictive variables for each outcome variable. We used the glmulti package [21] to fit and evaluate all possible models. The performance of each model was evaluated using the corrected Akaike information criterion [22]. For each outcome variable, the best performing model was selected and a p-value was calculated by comparing it against a null-model, as described above. Evaluating each of the models using a p-value was necessary as there was no guarantee that the model with the best AICC score would perform better than the null model. The p-values obtained were again corrected using the Benjamini-Hochberg method and only the models with a corrected p-value of 0.01 were retained. The results were presented using network visualisation to obtain a comprehensive overview of all the correlations that were detected during this analysis.
Results
Patients’ basic characteristics
We summarised the patients’ basic characteristics in table 1. Given that the two patient groups investigated (induction using oxytocin or balloon catheter) are primarily defined by the Bishop score and membrane-rupture status, we detected differences between the two groups in terms of basic characteristics. For example, multiparous women were more common in the oxytocin group than in the catheter group. Birth weight was higher in the catheter group than in the oxytocin group, as the main indication for catheter induction was post-term pregnancy. Although a direct comparison between these groups is not possible, the safety and effectiveness of labour induction after CS can still be assessed.
Table 1 Patient’s basic characteristics and materno-fetal outcomes in the cohorts (induction method catheter and oxytocin after caesarean section).
|
Catheter group
|
Oxytocin group
|
|
Patients’ basic characteristics
|
| Age (years), mean (SD) |
33.19 (± 4.77) |
31.83 (± 4.99) |
| Gestational age (weeks/days), mean (SD) |
40.26 (± 1.30) |
38.70 (± 2.74) |
| At least one prior vaginal delivery, n (%) |
22 (20.56%) |
19 (26.38%) |
| Primiparous (has given birth only once), n (%) |
85 (79.43%) |
53 (73.61%) |
| Multiparous (has given birth more than once), n (%) |
22 (20.6%) |
19 (26.38%) |
| Grand multipara (has given birth at least five times), n (%) |
2 (1.86%) |
0 (0.00%) |
| Duration between previous CS and induction of labour (years), mean (SD) |
4.19 (± 3.35) |
4.53 (± 3.25) |
|
Maternal and neonatal outcomes
|
| Vaginal delivery, n (%) |
49 (45.79%) |
46 (63.88%) |
| Caesarean section, n (%) |
58 (54.21%) |
26 (36.12%) |
| Vaginal assisted delivery, n (%) |
12 (16.66%) |
12 (16.66%) |
| Episiotomy, n (%) |
17 (15.88%) |
15 (20.83%) |
| High-grade perineal laceration (3 and 4), n (%) |
4 (3.73%) |
1 (1.38%) |
| Cervical laceration, n (%) |
0 (0.00%) |
1 (1.38%) |
| Peridural anaesthesia, n (%) |
43 (40.18%) |
35 (48.61%) |
| Uterine rupture, n (%) |
1 (0.93%) |
1 (1.38%) |
| Uterine dehiscence, n (%) |
5 (4.67%) |
4 (5.55%) |
| Birth weight (g) mean (SD) |
3515.83 (± 464.73) |
3206.25 (± 659.47) |
| Birth weight > 4000 g, n (%) |
11 (10.28%) |
6 (8.33%) |
| APGAR-score after 5 minutes mean (SD) |
8.88 (± 0.73) |
8.60 (± 1.00) |
| APGAR-Score < 7, n (%) |
0 (0.00%) |
2 (2.77%) |
| pH mean (SD) |
7.24 (± 0.07) |
7.26 (±0.071) |
| pH <7.20, n (%) |
21 (19.62%) |
8 (11.11%) |
| pH <7.00, n (%) |
1 (0.93%) |
0 (0.0%) |
| Neonatal admissions, n (%) |
7 (6.54%) |
10 (13.88%) |
|
Indication(s) of labour induction*
|
| Post-term, n (%) |
43 (40.18%) |
15 (20.83%) |
| Gestational hypertension/ preeclampsia, n (%) |
7 (6.54%) |
0 (0.00%) |
| Oligo-/polyhydramnios, n (%) |
9 (8.41%) |
1 (1.38%) |
| Pregnancy cholestasis, n (%) |
6 (5.60%) |
1 (1.38%) |
| Patient’s request, n (%) |
13 (12.14%) |
2 (2.77%) |
| (Gestational) diabetes, n (%) |
14 (13.08%) |
3 (7.14%) |
| Fetal distress, n (%) |
4 (3.73%) |
4 (5.55%) |
| PROM/PPROM, n (%) |
2 (1.86%) |
42 (58.33%) |
| Others, n (%) |
9 (8.41%) |
4 (5.55%) |
|
Indication for previous CS*
|
| Failed induction of labour, n (%) |
5 (4.67%) |
2 (2.77%) |
| Labour dystocia, n (%) |
11 (10.28%) |
7 (9.72%) |
| Abnormal progression of labour, n (%) |
18 (16.82%) |
10 (13.88%) |
| Fetal distress, n (%) |
21 (19.62%) |
17 (23.61%) |
| Breech presentation, n (%) |
16 (14.95%) |
12 (16.66%) |
| Others, n (%) |
25 (23.36%) |
16 (22.22%) |
| Unknown |
13 (12.14%) |
8 (11.11%) |
Impact of the induction method on delivery mode
The main goal of our study was to determine the success rate of vaginal delivery after induction of labour (balloon catheter or oxytocin) in women with a scarred uterus. The secondary goal was to detect factors that may influence the delivery mode as well as multiple parameters relating to maternal and neonatal outcomes.
As summarised in table 1, we detected a vaginal delivery success rate of 63.9% (46/72) in the oxytocin group, which is in line with previous reports [15, 19, 23]. In the catheter group, we detected a success rate of 45.8% (49/107), which was lower than expected [15, 23–25].
Maternal and fetal outcomes are summarised in table 1 as well. We detected uterine rupture of 0.9% (1/107) in the catheter and 1.4% (1/72) in the oxytocin group. The incomplete uterine rupture (uterine dehiscence) was 4.67% (5/107) in the catheter group and 5.55% (4/72) in the oxytocin group. Notably, neither of these observations was significant. The neonatal admission rate was 6.54% (7/107) in the catheter, and 13.88% (10/72), in the oxytocin group.
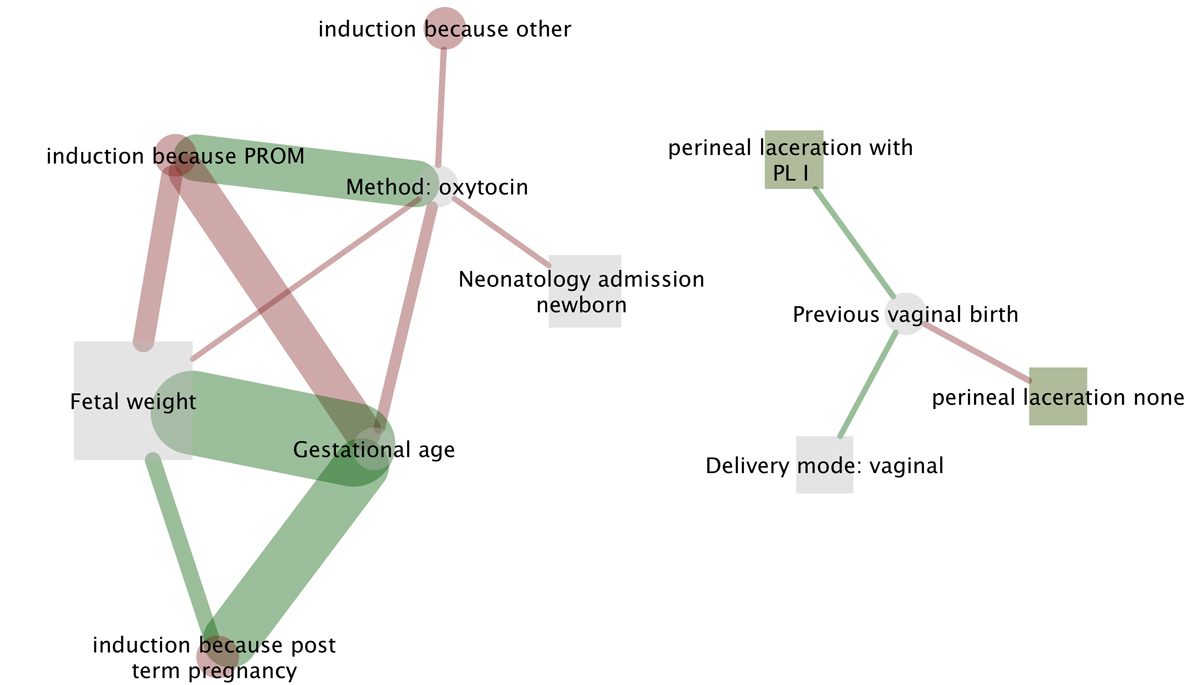
One-to-one correlations and delivery mode
To further dissect which factors contribute to the vaginal delivery success rate, we searched for one-to-one correlations. We detected several apparent and clinically not significant one-to-one correlations such as fetal weight and gestational age, or gestational age and post-term pregnancy (table 2 and fig. 1 solid lines). Premature rupture of membranes (PROM) as an indication for labour induction correlated positively with oxytocin as an induction method as well. Importantly, we detected two clinically significant correlations: previous vaginal birth as a single predictive factor for vaginal delivery (independent of induction method) and induction method (oxytocin) as a negative predictive factor for neonatal admissions (see fig. 1 full lines). To further dissect which variables (multiple) predict vaginal birth success rate and impact on outcomes (neonatal and maternal), we used a compound model.
Table 2 Significant one-to-one correlations in the investigated cohorts (induction method catheter and oxytocin after caesarean section).
|
Variable 1
|
Variable 2
|
Coefficient
|
p-value
|
Adj. p-value
|
| Fetal weight (g) |
Gestational age (days) |
182.422 |
2.21E-34 |
1.12E-31 |
| Gestational age (days) |
Induction because post-term pregnancy |
2.634 |
1.71E-23 |
4.33E-21 |
| Induction method oxytocin |
Induction because PROM |
4.356 |
3.13E-20 |
5.27E-18 |
| Gestational age (days) |
Induction because PROM |
-2.572 |
1.13E-16 |
1.43E-14 |
| Fetal weight (g) |
Induction because PROM |
-570.658 |
1.25E-10 |
1.27E-08 |
| Fetal weight (g) |
Induction because post-term pregnancy |
462.599 |
1.56E-08 |
1.32E-06 |
| Gestational age (days) |
Induction method oxytocin |
-1.497 |
7.87E-07 |
5.69E-05 |
| Induction method oxytocin |
Induction because other |
-1.47 |
8.90E-05 |
5.25E-03 |
| Previous vaginal birth |
Perineal laceration none |
-1.501 |
9.33E-05 |
5.25E-03 |
| Induction method oxytocin |
Neonatal admission |
-1.388 |
1.51E-04 |
7.50E-03 |
| Previous vaginal birth |
Perineal laceration I° |
1.695 |
1.68E-04 |
7.50E-03 |
| Delivery mode: vaginal |
Previous vaginal birth |
1.443 |
1.78E-04 |
7.50E-03 |
| Fetal weight (g) |
Induction method oxytocin |
-309.582 |
2.29E-04 |
8.91E-03 |
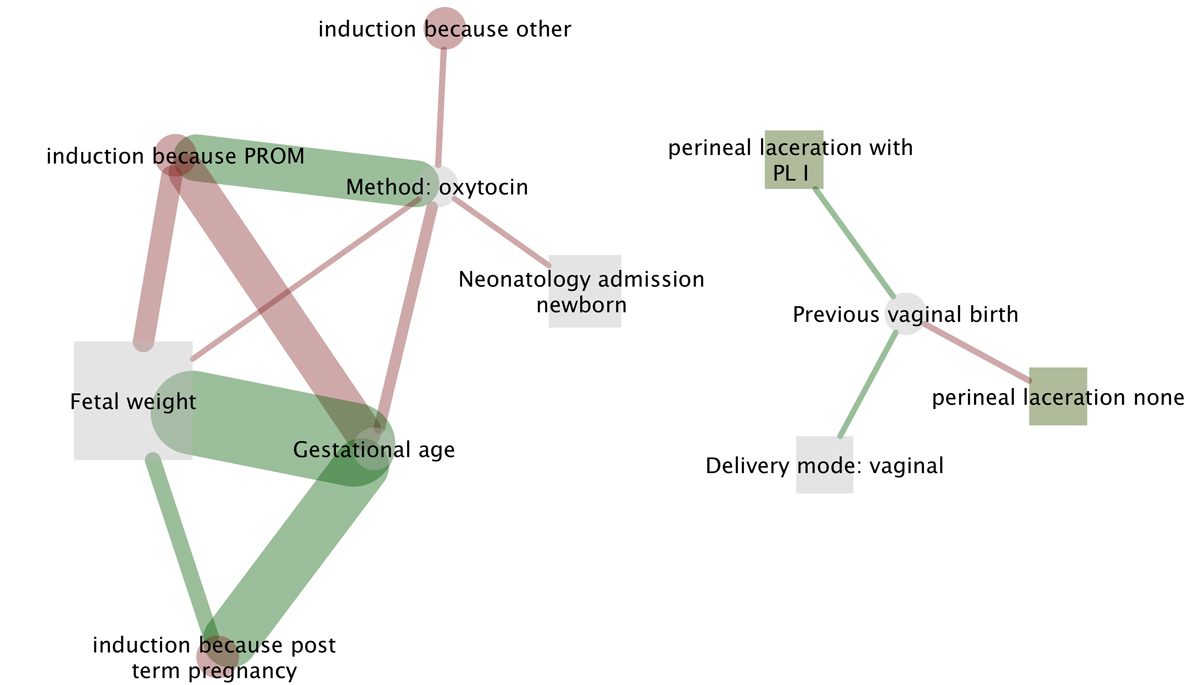
Figure 1
All significant one-to-one correlations in the cohorts (induction method catheter and oxytocin after caesarean section; for details see
table 2
). Each edge represents a statistically significant relationship between two variables. Positive correlations are indicated by the colour green (for example the gestational age correlates positively with the fetal weight: the more advanced the gestational age, the higher the fetal weight). Negative correlations are indicated by the colour red (for example, labour induction because of PROM is correlated to a lower birth weight). Predictive variables (factors) are indicated with circles and outcome variables with squares (for example induction because post-term pregnancy is a predictive factor for higher fetal weight). The size of the squares reflects the overall significance.
Multiple correlations and materno-fetal outcomes
Figure 2 (dashed lines) summarises all the detected and significant multiple correlations in our cohort. To understand the impact of the data on clinical practice, we divided it into clinically significant (table 3) and clinically not significant correlations (supplementary table S1 in appendix 1). Notably, the coefficient describes a positive or negative impact of the variables. Indeed, vaginal delivery success was more likely if previous vaginal delivery was noted and oxytocin as the induction method used. Additionally, post-term pregnancy as an indication for labour induction and other reasons for previous CS decreased the likelihood of vaginal delivery success. Interestingly, vaginal operative delivery was more likely if previous CS was performed due to abnormal labour progression or labour dystocia, whereas oxytocin as an induction method and previous vaginal birth decreased this likelihood. These observations suggest that previous vaginal birth process impact on the vaginal success rate in current pregnancy.

Figure 2
All significant and multiple correlations in the cohort. (Induction method catheter and oxytocin after caesarean section; for details see table 3 – clinically significant correlations and table S1 – clinically not relevant correlations). Each edge represents a statistically significant relationship between multiple variables. Positive correlations are indicated by the colour green (for example, previous vaginal birth increases the likelihood of vaginal delivery and a first degree perineal tear). Negative correlations are indicated by the colour red (for example, previous vaginal birth decreases the likelihood of secondary CS and vaginal assisted delivery due to abnormal labour progression). Predictive variables (factors) are indicated with circles and outcome variables with squares (for example higher gestational age results in increased fetal weight and higher risk for secondary CS due to abnormal labour progression). The size of the squares reflects the overall significance. Finally, variables related to the same indication or outcome variable (each reason for induction or type of perineal laceration) have the same node colour.
Table 3 Detailed analysis of clinically significant compound models in the cohorts investigated (induction method catheter and oxytocin after caesarean section).
|
Variable
|
p-value
|
Coefficient
|
|
Significant variables imparting vaginal delivery
|
| Induction method: oxytocin |
1.69E-02 |
0.567 |
| Previous vaginal birth |
2.65E-04 |
1.401 |
| Induction because: post-term pregnancy |
6.66E-02 |
-0.62 |
| Previous caesarean section because: other |
1.82E-02 |
-0.795 |
|
Significant variables imparting vaginal operative delivery because: other
|
| Induction method oxytocin |
7.73E-02 |
-38.211 |
| Previous CS because: breech presentation |
5.02E-02 |
59.452 |
| Previous CS because: labour dystocia |
2.23E-02 |
40.711 |
| Previous CS because: abnormal labour progression |
1.66E-02 |
39.637 |
|
Significant variables imparting vaginal operative delivery because: abnormal labour progression
|
| Induction method oxytocin |
5.006E |
1.366 |
| Previous vaginal birth |
1.47E-02 |
-18.129 |
| Induction because: patients request |
2.00E-01 |
-18.426 |
| Previous CS because: breech presentation |
3.84E-02 |
-17.744 |
| Previous CS because: labour dystocia |
1.15E-01 |
1.673 |
|
Significant variables imparting neonatal admission
|
| Induction method oxytocin |
1.51E-04 |
-3.339 |
| Gestational age (days) |
9.14E-07 |
-0.577 |
| Previous vaginal birth |
9.47E-02 |
0.821 |
| Induction because: other |
8.81E-02 |
-1.046 |
| Previous caesarean section because: breech presentation |
1.62E-03 |
1.46 |
| Previous caesarean section because: labour dystocia |
5.20E-02 |
-1.793 |
|
Significant variables imparting secondary CS because: abnormal labour progression
|
| Induction method oxytocin |
1.55E-03 |
-1.054 |
| Gestational age (days) |
1.06E-02 |
0.384 |
| Previous vaginal birth |
1.63E-03 |
-2.358 |
We identified single and multiple factors impacting on the VBAC success rate. Previous vaginal delivery and oxytocin as the induction method are the most prominent.
Discussion
We report that, in our cohort, induction of labour with oxytocin seems to be a safe method. It also seems to be an effective method for women with previous CS and a potential alternative to repeated CS. We detected a VBAC success rate of 63.9% when oxytocin was used, which is in line with previous reports [15, 19, 23]. Further, induction with a balloon catheter seems to be safe as well, but associated with a lower vaginal delivery success rate of only 45.8%. However, almost half of our patients delivered vaginally. Depending on a patient’s preference, this presents a valid basis for repeated CS. As many healthcare providers offer primary CS to patients with unfavourable Bishop scores, and increase the CS rate unnecessarily as a result, our study provides support that induction using oxytocin or balloon catheter is possible. We are aware that a direct comparison between the groups is limited due to different inclusion criteria. However, patients attempting VBAC need to be counselled about the advantages and disadvantages prior to labour induction. Often, the cervical ripening score is not available at the initial counselling time point, but all potential options and success rates need to be addressed. We are aware that other centres have different internal guidelines or use different techniques and protocols for the induction of labour after CS, so the results may have a limited external validity.
An unexpected finding in our study was that the vaginal delivery success rate in the catheter group was lower compared to previous studies [23–26]. Nevertheless, a recent study reported a vaginal delivery success rate after catheter induction in women with unfavourable cervix of approximately 50%, which is in line with our results [17]. These various success rates suggest that multiple factors need to be accounted for prior to labour induction. Factors that may impact on VBAC success rate are fetal weight, maternal age, indication for previous CS, or previous vaginal delivery [3, 27]. In our cohort, previous vaginal delivery had the biggest impact on vaginal delivery success rate (fig. 1: one-to-one correlation solid line and fig. 2: multiple correlations dashed lines). This is in line with previous reports showing that previous vaginal delivery is the most important success predictor for VBAC success, whereas labour dystocia as a previous CS indication represent a negative prediction factor [28]. Interestingly, abnormal labour progression and labour dystocia as indications for previous CS did not impact the CS rate in our cohort, but rather increased assisted vaginal operative delivery rates (fig. 1 and table 3). We hypothesise that this may be due to different obstetric practices between institutions. Besides previous vaginal delivery, oxytocin as an induction method increases the likelihood of vaginal delivery as well. The question of whether oxytocin should be applied only to a favourable cervix is still unanswered, as a recent study reported a higher vaginal delivery success rate compared to catheter devices [17]. Additional prospective and multi-centre studies are necessary, especially as maternal morbidities such as uterus rupture after oxytocin use were reported [29].
The safety of both the mother and neonate is the main goal in patients attempting VBAC and labour induction. In our cohort, we observed a higher incidence of neonatal admissions after labour induction using oxytocin. However, (8/10) neonatal admissions were due to premature rupture of membranes (PROM), one due to fetal distress, and one due to trisomy 21 and fetal distress, which explains the differences. Notably, no long-term complications were noted. Together, the neonatal admission rate confirms the importance of proper equipped perinatal units when labour is induced after previous CS. It includes not only trained obstetricians but the timely availability of a neonatologist at the unit as well.
The most severe maternal complication after labour induction on a scarred uterus is uterus rupture [27, 30–33]. Given increasing awareness of uterine dehiscence and/or thin lower uterine segment after CS, we defined uterine rupture and uterine dehiscence according to current standards. Although our analyses did not detect any predicting factors associated with uterine rupture, there remains a controversial discussion about the incidence of uterus rupture after labour induction and spontaneous onset of birth [12, 18, 34–38]. There is always a small risk of uterine rupture when VBAC is attempted. The risk in the case of spontaneous labour onset is approximately 0.5–0.7%, and in the case of labour induction approximately 0.8% without prostaglandins and 2.7% with prostaglandins compared to repeat CS [12, 18]. Whether oxytocin or balloon catheter is the safest choice is still unanswered by the present study, mainly due to the rare occurrence of this event. In this regard, an important problem is that the definition of “thin uterine segment” or uterine dehiscence is not standardised. In our cohort, the incidence of uterine rupture was rare and comparable to previous studies [12, 13, 15, 19, 39]. However, thin uterine segment was noted to be more common (table 1). We have to acknowledge that this study is not designed to detect these kinds of changes. Besides its retrospective design, the patient inclusion timeline is the main limitation of our study. For example, during the time investigated, we changed our internal guidelines from single to double-device catheter, which may bias the internal validity of our findings. Additionally, the number of patients induced using the double-balloon catheter was not large enough to detect differences between single and double balloon catheter devices. Studies comparing these two catheter devices are needed [40]. Further limitations arise due to the retrospective design of our study. For example, certain factors that may have influenced the VBAC success rate in our multivariate analysis were not present. These include body-mass index, ethnicity, and exact Bishop score after 24h catheter induction. On the other hand, the advantages of our study are the large total number of patients included, the exclusion of patients with spontaneous onset of labour, and the single and multi-variant assessment of factors contributing to VBAC success. Together, our study provides important information contributing to proper counselling of our patients.
Together, prior to labour induction, patients need to be counselled extensively and included in the process of decision making. Again, as in case of vaginal delivery success rate, the patient population must be considered, and additional factors assessed. These include indication(s) of previous CS, previous vaginal birth, maternal age, or thickness of the lower uterine segment measured by ultrasound [9]. Importantly, patients need to be counselled not only about the risks of VBAC, but also about the CS related morbidities as well. These include infection, increased blood loss, intraoperative lesions [41, 42], thromboembolic events, and abnormal placentation risk in following pregnancies [43, 44].
Appendix 1 Supplementary table
Table S1 Detailed analysis of clinically non-significant compound models in the investigated cohorts (induction method catheter and oxytocin after caesarean section).
|
Variable
|
p-value
|
Coefficient
|
|
Selected variables for the pHa model
|
| Age (years) |
5.840E-03 |
-0.003 |
| Gestational age (days) |
1.221E-01 |
-0.008 |
| Induction because: of post term pregnancy |
3.639E-02 |
0.028 |
| Previous CS because: labour dystocia |
4.088E-02 |
-0.040 |
|
Selected variables for the APGAR5 model
|
| Age (years) |
6.508E-02 |
-0.026 |
| Gestational age (days) |
1.796E-02 |
0.072 |
| Induction because: diabetes |
2.065E-02 |
0.477 |
| Previous CS because: abnormal progression of labour |
8.003E-02 |
0.311 |
Author contributions
MM and DS contributed equally to the study
References
1
Mueller
M
,
Kolly
L
,
Bauman
M
,
Imboden
S
,
Surbek
D
. Analysis of caesarean section rates over time in a single Swiss centre using a ten-group classification system. Swiss Med Wkly. 2014;144:w13921. https://smw.ch/en/article/doi/smw.2014.13921
2
Hamilton
BE
,
Martin
JA
,
Osterman
MJ
,
Curtin
SC
,
Matthews
TJ
. Births: Final Data for 2014. Natl Vital Stat Rep. 2015;64(12):1–64.
3
Christmann-Schmid
C
,
Raio
L
,
Scheibner
K
,
Müller
M
,
Surbek
D
. Back to “once a caesarean: always a caesarean”? A trend analysis in Switzerland. Arch Gynecol Obstet. 2016;294(5):905–10. doi:.https://doi.org/10.1007/s00404-016-4055-4
4
American College of Obstetricians and Gynecologists Committee on Obstetric Practice. ACOG Committee Opinion No. 342: induction of labor for vaginal birth after cesarean delivery. Obstet Gynecol. 2006;108(2):465–8. doi:.https://doi.org/10.1097/00006250-200608000-00045
5
Menacker
F
,
Declercq
E
,
Macdorman
MF
. Cesarean delivery: background, trends, and epidemiology. Semin Perinatol. 2006;30(5):235–41. doi:.https://doi.org/10.1053/j.semperi.2006.07.002
6Anonymous. RCOG Clinical Effectiveness Support Unit. Induction of labour. Evidence-based Clinical Guideline Number 9. Royal College of Obstetricians and Gynaecologists: London: RCOG Press, 2001..
7
Greene
MF
. Vaginal birth after cesarean revisited. N Engl J Med. 2004;351(25):2647–9. doi:.https://doi.org/10.1056/NEJMe048277
8
Caughey
AB
,
Cahill
AG
,
Guise
JM
,
Rouse
DJ
; American College of Obstetricians and Gynecologists (College); Society for Maternal-Fetal Medicine. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210(3):179–93. doi:.https://doi.org/10.1016/j.ajog.2014.01.026
9
Surbek
D
,
Rath
W
. Vaginale Geburt nach vorausgegangener Sectio - riskant? [Vaginal birth after previous caesarean section – a risk?]. Geburtshilfe Frauenheilkd. 2006;66(12):1131–3. doi:.https://doi.org/10.1055/s-2006-924757
10
Rath
W
,
Surbek
D
. Geburtseinleitung bei Zustand nach Sectio. [Induction of labor after previous caesarean section]. Geburtshilfe Frauenheilkd. 2006;66(12):1143–9. doi:.https://doi.org/10.1055/s-2006-924756
11
Martel
MJ
,
MacKinnon
CJ
; Clinical Practice Obstetrics Committee, Society of Obstetricians and Gynaecologists of Canada. Guidelines for vaginal birth after previous Caesarean birth. J Obstet Gynaecol Can. 2005;27(2):164–88. doi:.https://doi.org/10.1016/S1701-2163(16)30188-8
12
Ravasia
DJ
,
Wood
SL
,
Pollard
JK
. Uterine rupture during induced trial of labor among women with previous cesarean delivery. Am J Obstet Gynecol. 2000;183(5):1176–9. doi:.https://doi.org/10.1067/mob.2000.109037
13
Ziyauddin
F
,
Hakim
S
,
Beriwal
S
. The transcervical foley catheter versus the vaginal prostaglandin e2 gel in the induction of labour in a previous one caesarean section - a clinical study. J Clin Diagn Res. 2013;7(1):140–3.
14
Grobman
WA
,
Gilbert
S
,
Landon
MB
,
Spong
CY
,
Leveno
KJ
,
Rouse
DJ
, et al.
Outcomes of induction of labor after one prior cesarean. Obstet Gynecol. 2007;109(2 Pt 1):262–9. doi:.https://doi.org/10.1097/01.AOG.0000254169.49346.e9
15
Bujold
E
,
Blackwell
SC
,
Gauthier
RJ
. Cervical ripening with transcervical foley catheter and the risk of uterine rupture. Obstet Gynecol. 2004;103(1):18–23. doi:.https://doi.org/10.1097/01.AOG.0000109148.23082.C1
16
Jozwiak
M
,
Dodd
JM
. Methods of term labour induction for women with a previous caesarean section. Cochrane Database Syst Rev. 2013;3(3):CD009792.
17
Shah
U
,
Bellows
P
,
Drexler
K
,
Hawley
L
,
Davidson
C
,
Sangi-Haghpeykar
H
, et al.
Comparison of induction of labor methods for unfavorable cervices in trial of labor after cesarean delivery. J Matern Fetal Neonatal Med. 2017;30(9):1010–5. doi:.https://doi.org/10.1080/14767058.2016.1197903
18
Lydon-Rochelle
M
,
Holt
VL
,
Easterling
TR
,
Martin
DP
. Risk of uterine rupture during labor among women with a prior cesarean delivery. N Engl J Med. 2001;345(1):3–8. doi:.https://doi.org/10.1056/NEJM200107053450101
19
Sananès
N
,
Rodriguez
M
,
Stora
C
,
Pinton
A
,
Fritz
G
,
Gaudineau
A
, et al.
Efficacy and safety of labour induction in patients with a single previous caesarean section: a proposal for a clinical protocol. Arch Gynecol Obstet. 2014;290(4):669–76. doi:.https://doi.org/10.1007/s00404-014-3287-4
20
Kolkman
DG
,
Verhoeven
CJ
,
Brinkhorst
SJ
,
van der Post
JA
,
Pajkrt
E
,
Opmeer
BC
, et al.
The Bishop score as a predictor of labor induction success: a systematic review. Am J Perinatol. 2013;30(8):625–30. doi:.https://doi.org/10.1055/s-0032-1331024
21
Calcagno
V
,
de Mazancourt
C
. An r package for easy automated model selection with (generalized) linear models. J Stat Softw. 2010;34(1):1–29.
22
Hurvich
CM
,
Tsai
CL
. A corrected akaike information criterion for vector autoregressive model selection. J Time Ser Anal. 1993;14(3):271–9. doi:.https://doi.org/10.1111/j.1467-9892.1993.tb00144.x
23
Ferradas
E
,
Alvarado
IL
,
Gabilondo
MA
,
Diez-Itza
I
,
García-Adanez
J
. Double balloon device compared to oxytocin for induction of labour after previous caesarean section. Open J Obstet Gynecol. 2013;03(01):212–6. doi:.https://doi.org/10.4236/ojog.2013.31A039
24
Meetei
LT
,
Suri
V
,
Aggarwal
N
. Induction of labor in patients with previous cesarean section with unfavorable cervix. Journal of Medical Society.
2014;28(1):29–33. doi:.https://doi.org/10.4103/0972-4958.135223
25
Ten Eikelder
ML
,
Neervoort
F
,
Oude Rengerink
K
,
van Baaren
GJ
,
Jozwiak
M
,
de Leeuw
JW
, et al.
Induction of labour with a Foley catheter or oral misoprostol at term: the PROBAAT-II study, a multicentre randomised controlled trial. BMC Pregnancy Childbirth. 2013;13(1):67. doi:.https://doi.org/10.1186/1471-2393-13-67
26
Kehl
S
,
Weiss
C
,
Rath
W
. Balloon catheters for induction of labor at term after previous cesarean section: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2016;204:44–50. doi:.https://doi.org/10.1016/j.ejogrb.2016.07.505
27
Delaney
T
,
Young
DC
. Spontaneous versus induced labor after a previous cesarean delivery. Obstet Gynecol. 2003;102(1):39–44.
28
Landon
MB
,
Leindecker
S
,
Spong
CY
,
Hauth
JC
,
Bloom
S
,
Varner
MW
, et al.; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. The MFMU Cesarean Registry: factors affecting the success of trial of labor after previous cesarean delivery. Am J Obstet Gynecol. 2005;193(3 Pt 2):1016–23. doi:.https://doi.org/10.1016/j.ajog.2005.05.066
29
Cahill
AG
,
Waterman
BM
,
Stamilio
DM
,
Odibo
AO
,
Allsworth
JE
,
Evanoff
B
, et al.
Higher maximum doses of oxytocin are associated with an unacceptably high risk for uterine rupture in patients attempting vaginal birth after cesarean delivery. Am J Obstet Gynecol. 2008;199(1):32.e1–5. doi:.https://doi.org/10.1016/j.ajog.2008.03.001
30
Guise
JM
,
McDonagh
MS
,
Osterweil
P
,
Nygren
P
,
Chan
BK
,
Helfand
M
. Systematic review of the incidence and consequences of uterine rupture in women with previous caesarean section. BMJ. 2004;329(7456):19–25. doi:.https://doi.org/10.1136/bmj.329.7456.19
31
Landon
MB
,
Spong
CY
,
Thom
E
,
Hauth
JC
,
Bloom
SL
,
Varner
MW
, et al.; National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Risk of uterine rupture with a trial of labor in women with multiple and single prior cesarean delivery. Obstet Gynecol. 2006;108(1):12–20. doi:.https://doi.org/10.1097/01.AOG.0000224694.32531.f3
32
Ben-Aroya
Z
,
Hallak
M
,
Segal
D
,
Friger
M
,
Katz
M
,
Mazor
M
. Ripening of the uterine cervix in a post-cesarean parturient: prostaglandin E2 versus Foley catheter. J Matern Fetal Neonatal Med. 2002;12(1):42–5. doi:.https://doi.org/10.1080/jmf.12.1.42.45
33
Isono
W
,
Nagamatsu
T
,
Uemura
Y
,
Fujii
T
,
Hyodo
H
,
Yamashita
T
, et al.
Prediction model for the incidence of emergent cesarean section during induction of labor specialized in nulliparous low-risk women. J Obstet Gynaecol Res. 2011;37(12):1784–91. doi:.https://doi.org/10.1111/j.1447-0756.2011.01607.x
34
Buhimschi
CS
,
Buhimschi
IA
,
Patel
S
,
Malinow
AM
,
Weiner
CP
. Rupture of the uterine scar during term labour: contractility or biochemistry?
BJOG. 2005;112(1):38–42. doi:.https://doi.org/10.1111/j.1471-0528.2004.00300.x
35
Hendler
I
,
Bujold
E
. Effect of prior vaginal delivery or prior vaginal birth after cesarean delivery on obstetric outcomes in women undergoing trial of labor. Obstet Gynecol. 2004;104(2):273–7. doi:.https://doi.org/10.1097/01.AOG.0000134784.09455.21
36
Zelop
CM
,
Shipp
TD
,
Repke
JT
,
Cohen
A
,
Caughey
AB
,
Lieberman
E
. Uterine rupture during induced or augmented labor in gravid women with one prior cesarean delivery. Am J Obstet Gynecol. 1999;181(4):882–6. doi:.https://doi.org/10.1016/S0002-9378(99)70319-4
37
Flamm
BL
,
Anton
D
,
Goings
JR
,
Newman
J
. Prostaglandin E2 for cervical ripening: a multicenter study of patients with prior cesarean delivery. Am J Perinatol. 1997;14(3):157–60. doi:.https://doi.org/10.1055/s-2007-994118
38
McDonagh
MS
,
Osterweil
P
,
Guise
JM
. The benefits and risks of inducing labour in patients with prior caesarean delivery: a systematic review. BJOG. 2005;112(8):1007–15. doi:.https://doi.org/10.1111/j.1471-0528.2005.00623.x
39
Cheuk
QK
,
Lo
TK
,
Lee
CP
,
Yeung
AP
. Double balloon catheter for induction of labour in Chinese women with previous caesarean section: one-year experience and literature review. Hong Kong Med J. 2015;21(3):243–50.
40
De Bonrostro Torralba
C
,
Tejero Cabrejas
EL
,
Marti Gamboa
S
,
Lapresta Moros
M
,
Campillos Maza
JM
,
Castán Mateo
S
. Double-balloon catheter for induction of labour in women with a previous cesarean section, could it be the best choice?
Arch Gynecol Obstet. 2017;295(5):1135–43. doi:.https://doi.org/10.1007/s00404-017-4343-7
41
McMahon
MJ
,
Luther
ER
,
Bowes
WA, Jr
,
Olshan
AF
. Comparison of a trial of labor with an elective second cesarean section. N Engl J Med. 1996;335(10):689–95. doi:.https://doi.org/10.1056/NEJM199609053351001
42
Rageth
JC
,
Juzi
C
,
Grossenbacher
H
; Swiss Working Group of Obstetric and Gynecologic Institutions. Delivery after previous cesarean: a risk evaluation. Obstet Gynecol. 1999;93(3):332–7.
43
Paré
E
,
Quiñones
JN
,
Macones
GA
. Vaginal birth after caesarean section versus elective repeat caesarean section: assessment of maternal downstream health outcomes. BJOG. 2006;113(1):75–85. doi:.https://doi.org/10.1111/j.1471-0528.2005.00793.x
44
Nisenblat
V
,
Barak
S
,
Griness
OB
,
Degani
S
,
Ohel
G
,
Gonen
R
. Maternal complications associated with multiple cesarean deliveries. Obstet Gynecol. 2006;108(1):21–6. doi:.https://doi.org/10.1097/01.AOG.0000222380.11069.11