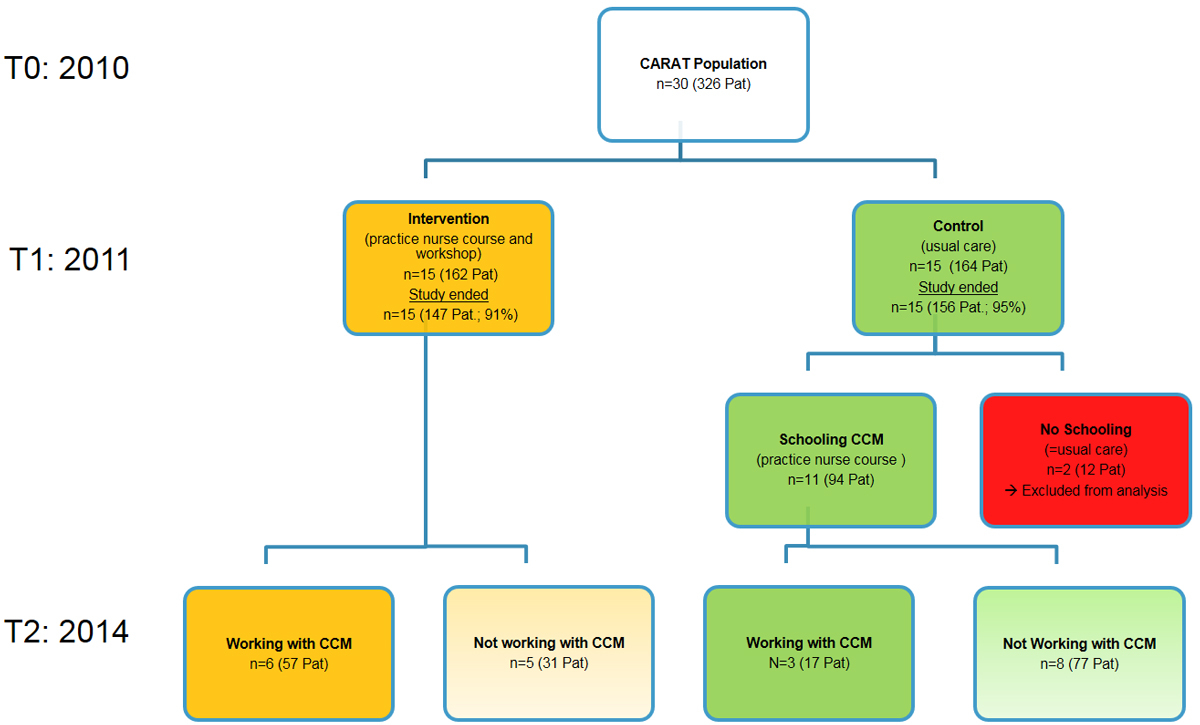
Figure 1 Implementation of the Chronic Care Models over 4 years.
CARAT = Chronic CARe for diabetes trial; n = number of primary care practices; Pat = patients; CCM = Chronic Care Model
DOI: https://doi.org/10.4414/smw.2017.14522
In most European countries, an increasing mismatch can be observed between, on the one hand, rising numbers of patients with chronic diseases [1] and, on the other hand, a shortage of general practitioners, who are mainly responsible for treating these patients [2]. In order to nevertheless enable complex health care and cope with rising costs, team-based approaches have been developed for treatment of the chronically ill. The cluster-randomised CARAT trial (Chronic CARe for diAbeTes) [3–6] showed that implementing the Chronic Care Model (CCM) in diabetes care via involvement of specially trained practice nurses [7, 8] is feasible in small primary care practices (PCPs), improves the cardiovascular risk profile and is perceived by patients to be better structured care, at least on the short term. Little is known on the long-term effects of such an intervention.
The aim of this study was, therefore, to assess the feasibility and practicability of implementing the CCM in small PCPs in the long term. We assessed the proportion of patients still treated according to CCM 3 years after completion of the CARAT trial, as well as reasons for discontinuing the use of the CCM, and the development of clinical outcomes over time (glycosylated haemoglobin [HbA1c], blood pressure, low density lipoprotein [LDL]-cholesterol and compliance with CCM (assessed by use of Patient Assessment of Chronic Illness Care [PACIC]).
We performed a cross-sectional questionnaire survey among the participants who completed the cluster-randomised controlled CARAT trial [3–6], 3 years after its finalisation.
Detailed information about design and methods, baseline characteristics and results of the trial have been published previously [3–6]. The eligibility criteria for the CARAT trial were PCPs participating in routine primary care of unselected patients. The inclusion criteria for patients were adulthood (age >18 years), diagnosis of type 2 diabetes according to international diagnostic criteria [9] and at least one HbA1c level of ≥7.0% measured within the preceding year. Exclusion criteria were insufficient language skills to read and understand informed consent, patient information and the questionnaires, patients who contacted the practice for emergencies only or as a substitute practice (i.e., no continuous patient-doctor relationship), and a life expectancy less than 6 months. Fifteen PCPs were randomised to the intervention and 15 to the control group. Recruitment of PCPs took place between November 2009 and February 2010. Recruitment of patients and baseline assessments took place between January and April 2010 (T0). The intervention ran from April 2010 until May 2011, and follow-up assessments were conducted 1 year after baseline assessments (T1). The intervention aimed at providing team care according to the CCM by means of involving a trained practice nurse in the care of diabetic patients. Therefore, practice nurses of the intervention group were trained soon after randomisation in a 6-day educational course “Treatment of long term patients – module diabetes,” organised by the Union of Swiss Practice Nurses [10]. The course provided medical knowledge about the treatment of diabetes patients and general communication skills, and it empowered practice nurses for their role in a team providing structured care for chronically ill patients. The practice nurses also learned how to perform visits and follow-up consultations by means of a monitoring tool developed for the study [3]. In addition, PCPs and practice nurses from the intervention group participated in two 4-hour interactive workshops. The first workshop took place soon after randomisation and addressed the implementation of the team approach in practice and evidenced-based therapy of diabetes. The second workshop took place after 6 study months, and covered professional exchange between practice nurses and PCPs regarding implementation experience and management of cardiovascular risk factors. The intervention included practice nurses that were involved in the care of type 2 diabetes patients. Practice nurses planned independent consultations with patients. The monitoring tool guided them through the consultations, and provided the opportunity to record relevant parameters and assistance for self-management support in order to help the patient in selecting appropriate, concrete behavioural goals, in developing plans for reaching those goals, and in evaluating the progress and adequacy of those plans. The monitoring tool addressed clinical parameters (e.g., HbA1c, blood pressure and LDL-cholesterol levels), examinations (e.g., food control, neurological tests and eye examinations), adherence to prescribed drugs, self-care goals, and other recommendations. The clinical aim of the tool was to ensure that treatment recommendations were followed. The assessed parameters were classified regarding their clinical urgency and importance into a traffic light scheme (green, amber, and red), and the practice nurses forwarded the tool to the PCPs. Therefore, the PCPs obtained an immediate overview on the current situation of the patients. We recommended practice nurse consultations every 4 months, but frequency could be adapted according to the clinical situation of the patient.
The study protocol for the CARAT study was approved by the ethics committee of the Kanton Zurich and received an unrestricted positive vote on 25 January 2010 [4].
The current follow-up study among the 30 originally participating PCPs of the CARAT trial (303 type 2 diabetes patients) was performed in 2014, 3 years after the end of the trial (T2). Recruitment of participants took place between April and October 2014. After completion of the CARAT trial, the practice nurses of the control group were given the opportunity to participate in the same diabetes management course that the intervention group had participated in. In contrast to the training of the CARAT intervention group, no common workshops were provided for the general practitioners. For the data analysis, we considered all the participating PCPs from the intervention group. Since the focus of the current follow-up was to evaluate the effect of implementing the CCM in the long term, only PCPs from the original control group whose practice nurses had completed the diabetes management course were included. Thirteen of the 15 practice nurses of the control group had participated in the course, two had not. Their data, including the associated 12 patients, could therefore not be taken into consideration for the follow up evaluation.
The current follow up study included two types of questionnaire, one filled out by the practice team and one by the patients (appendices 1 and 2 ). In the CARAT trial, PCPs had created a list with the study participants and their corresponding code. According to this list, which remained at the participating PCPs, the practices were able to recruit the CARAT patients for the current follow-up. Both questionnaires were marked with this patient code and sent to the University of Zurich in a stamped envelope independently by the patients and practice teams. The university had no access to the patients’ names; anonymity was therefore ensured.
The questionnaire filled out by the practice team (general practitioner and/or practice nurse) consisted of a qualitative and quantitative section. The qualitative section included questions about the structure of care the PCP is currently working with. The aim was to assess whether patients are still treated according to the intention of the CARAT study, meaning that the practice nurse is essentially involved in the treatment of diabetic patients according to the CCM. We also assessed whether the traffic light scheme is used as a monitoring tool. The reasons for a negative answer to these questions were assessed by means of free text. The quantitative section included clinical and laboratory follow-up parameters on the specific study patient (within the previous 6 months). The primary and secondary outcomes of the original CARAT study were analysed over a period of 4 years, meaning that we compared the baseline data (T0 in 2010) with the current findings (T2 in 2014), according to the original randomisation and the current modus operandi concerning CCM (fig. 1).
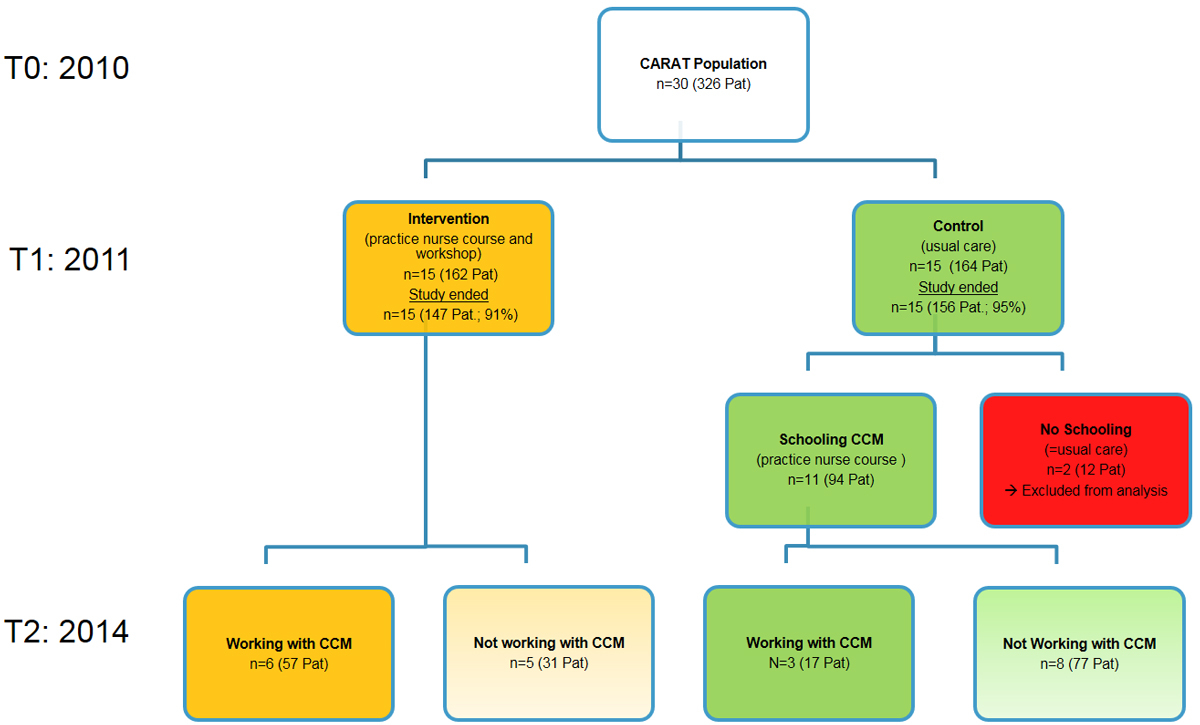
Figure 1 Implementation of the Chronic Care Models over 4 years.
CARAT = Chronic CARe for diabetes trial; n = number of primary care practices; Pat = patients; CCM = Chronic Care Model
The questionnaires filled out by the patients consisted mainly of the PACIC [11, 12], which aims at evaluating the subjectively experienced compliance of medical care with the CCM.
The study outcomes were: proportion of patients still treated according to CCM, possible reasons for discontinuation, development of clinical parameters between T0 and T2 (HbA1c, blood pressure, LDL-cholesterol, and compliance with CCM [assessed with PACIC]).
In order to systematically summarise and analyse the qualitative data concerning structure of care, we performed a framework analysis [13]. Clinical data and PACIC were analysed according to the intention to treat method (last observation carried forward). Characteristics of PCPs and patients are presented as means and standard deviations (SDs) or confidence intervals (CIs) for continuous variables, and frequencies and percentages for categorical data. After testing if the clinical data is well modelled by a normal distribution (Shapiro-Wilk test and distributional diagnostic plots), either parametric or nonparametric independent comparison tests were used. For variables that were not normally distributed, Wilcoxon rank sum tests were used to compare the clinical outcomes between the different groups. If the hypothesis that the sample comes from a population that has a normal distribution was not rejected, parametric tests were conducted. To compare difference scores (T2 minus T0) and scores at T2 on clinical variables between PCPs of the intervention- and control-group, as well as between PCPs still using or not using the CCM, two sample-independent Student t-tests were conducted. The following parameters were not normally distributed: HbA1c at T2, HbA1c T2−T0, systolic blood pressure at T2, LDL-cholesterol at T2, LDL-cholesterol T2−T0. The following parameters were normally distributed: systolic blood pressure T2−T0, diastolic blood pressure at T2, diastolic blood pressure T2−T0. For analysis of the change in clinical parameters, the paired t-test, followed by a Wilcoxon signed rank if not normally distributed, was performed. A chi-square test of independence was used to examine the relation between target levels and time (T0, T2) as well as to examine the relation between initial randomisation and CCM usage. The significance level was set at 0.05 (two sided). Statistical analyses were performed using SPSS (Version 22) and Stata (version 13.0, StataCorp, 2010).
From the 30 PCPs and 326 type 2 diabetes patients originally participating in the CARAT trial, 30 PCPs and 303 patients completed the study. Baseline characteristics of the CARAT patients are listed in table 1. For the current follow up, 24 PCPs (80%) and 194 patients (64.0%) agreed to participate. Six PCPs with 67 patients refused to participate owing to time and personnel shortages. The detailed study population and dropouts are listed in figure 2. All practice nurses of the intervention group were trained in implementing elements of CCM into practice during the trial. In the control group, all practice nurses apart from two were trained in the CCM after completion of the trial. Characteristics of these two PCPs, including 12 patients, could therefore not be taken into consideration for the current follow up evaluation, leaving 22 PCPs (73.3%) with 182 patients (60.1%) for further analyses. Eleven (45.8%) had been originally randomised to the intervention group of the CARAT trial, and 13 (54.2%) to the control group (fig. 2).
Table 1 Baseline patient characteristics and clinical measures.
| Mean ± SD or n (%) | |
|---|---|
| Age (years) | 67.1 ± 10.6 |
| Male gender | 187 (57.4%) |
| Living together with partner/family | 246 (78.3%) |
| Still working | 100 (32.2%) |
| Education (years) | 11.6 ± 3.2 |
| Smoking status | |
| Current smoker | 36 (11.5%) |
| Former smoker | 129 (41.1%) |
| Never smoker | 149 (47.4%) |
| Duration of diabetes (years) | 9.9 ± 7.6 |
| Glycated haemoglobin (%) | 7.7 ± 1.3 |
| Self-monitoring of blood glucose | |
| None | 65 (19.9%) |
| Daily (≥1) | 133 (40.8%) |
| Weekly (≥1) | 101 (31.0%) |
| Monthly (≥1) | 27 (8.3%) |
| Number of consultations last year | 8.07 ± 6.0 |
| Systolic blood pressure (mm Hg) | 139.1 ± 17.6 |
| Diastolic blood pressure (mm Hg) | 80.9 ± 10.5 |
| Pulse | 73.7 ± 11.9 |
| Body-mass index (kg/m2) | 30.6 ± 5.6 |
| Low-density lipoprotein-cholesterol | 2.7 ± 1.1 |
| Number of comorbidities | 2.66 ± 1.6 |
| Hypertension | 231 (71.3%) |
| Hyperlipidaemia | 208 (66.7%) |
| Obesity | 173 (53.1%) |
| Coronary heart disease | 66 (20.4%) |
| Depression | 38 (11.7%) |
| Asthma / chronic obstructive pulmonary disease | 32 (9.8%) |
| Heart failure | 22 (6.8%) |
| Stroke | 17 (5.2%) |
| Cancer | 13 (4.2%) |
| Antidiabetic therapy | 312 (96.6%) |
| None | 12 (3.7%) |
| Only oral* | 208 (64.4) |
| Only insulin* | 26 (8.0) |
| Combined (insulin and oral)* | 77 (23.8) |
| Any antihypertensive agent* | 246 (76.2) |
| Any antiplatelet/anticoagulation therapy* | 179 (55.4) |
| Any lipid-lowering therapy* | 182 (56.3) |
| Any antidepressants* | 37 (11.5) |
| Number of drugs total | 4.8 (2.1) |
| PACIC summary score | 3.18 ± 0.85 |
| Patient activation | 3.83 ± 1.13 |
| Delivery system / practice design | 3.87 ± 0.82 |
| Goal setting / tailoring | 2.86 ± 0.98 |
| Problem solving / contextual | 3.26 ± 1.22 |
| Follow-up / coordination | 2.66 ± 1.05 |
* More than one drug possible
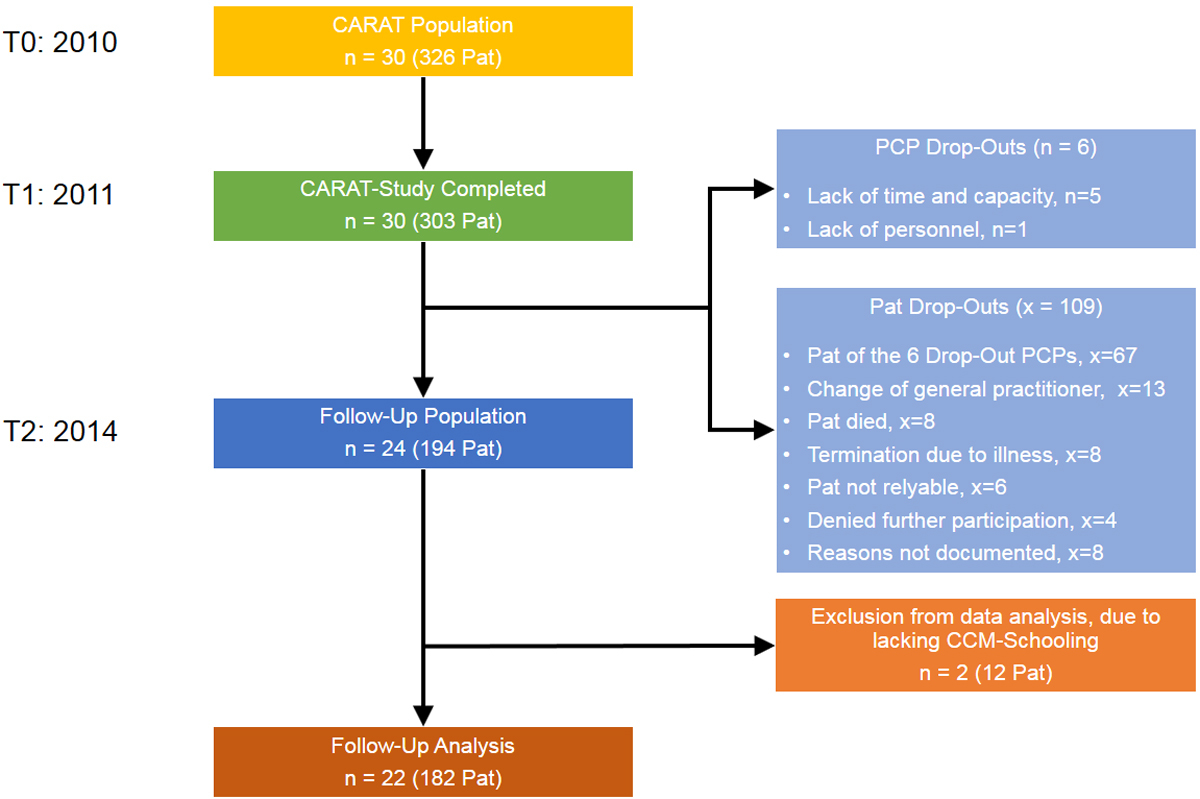
Figure 2 Study population and drop-outs.
CARAT = Chronic CARe for diabetes trial; n = number of primary care practices; x = number of patients; Pat = patients; CCM = Chronic Care Model; PCP = primary care practice
Thirteen of the 22 PCPs (59.1%) did not treat 108 of the 182 patients (59.3%) according to the CCM. The 11 PCPs originally randomised into the intervention group were more likely to still treat their 88 patients according to CCM than the 11 practices (94 patients) originally randomised to the control group (chi-square 48.402, degrees of freedom [DF] 192, p <0.001, fig. 1). The main reasons for currently not using the CCM for the treatment of diabetic patients were personnel and organisational problems (n = 9), mainly due to commonly occurring changes in the employment structure of the practice nurses, the associated lack of capacity / missing resources and lacking accommodation. The second most common reason was financial problems (n = 4), since the billing process of practice nurses involved in patient treatment is not settled in the current insurance structures, where only physicians’ work can be billed. Additionally, general practitioners were not willing to transfer treatment responsibility (n = 4) because of the fear of losing control or of low workload, or patients did not want to be treated according to the CCM (n = 4). Lack of benefits combined with additional work and costs were mentioned only once (multiple statements possible). In general, PCPs treated their patients consistently, meaning that all patients of the same PCP were treated according to the CCM or not.
Two PCPs (9.1%, one originally intervention and one control group) with 11 patients (6%) still used the traffic light scheme as a monitoring tool. The main reason for currently not using the scheme was the utilisation of an alternative tool (n = 12), mainly the use of an electronic patient record with a linked diabetes monitoring system, a practice own scheme, or cooperation with hospitals and their schemes. Five PCPs stated that the scheme was confusing and complex. Five PCPs stated it was pointless using it if the study nurse was not involved in the treatment of patients. Three PCPs did not know about the scheme (multiple statements possible).
Overall, the absolute HbA1c did not change significantly over 4 years (T0 mean 7.74%, SD 1.34% vs T2 mean 7.58%, SD 1.32%; DF 154, p = 0.249). By the time of the current follow-up, no significant difference between patients from the original intervention compared with the control group was found (control mean 7.51%, SD1.49% vs intervention mean 7.65%, SD 1.13%; DF 153, p = 0.092). There was a significant difference in the change in HbA1c according to randomisation; the original intervention group showed significantly lower changes in HbA1c (intervention T2−T0 mean 0.43%, SD 1.85% vs control T2−T0 mean 0.10%, SD 1.21%; DF 153, p = 0.04) (table 2). Additionally, a significant difference in HbA1c was detected at the time of follow up, depending on whether the PCP treated their patients according to the CCM or the classical model: patients treated according to CCM displayed lower values (CCM T2 mean 7.40%, SD 1.33% vs no CCM T2 mean 7.73%, SD 1.29%; DF 153, p = 0.025) (table 3). The change of HbA1c according to implementation of the CCM showed a trend in favour of PCPs using the CCM (CCM T2−T0 mean −0.28%, SD 1.41% vs no CCM T2−T0 mean −0.05%, SD 1.70%; DF 153, p = 0.071) (table 3). If the target for HbA1c levels was set at 7.5%, the target was reached significantly more often at the time of the current follow up than at baseline (52 vs 26%, chi-square 7.945, p = 0.005, data not shown). This finding was independent of initial randomisation (44 vs 42%, chi-square 0.351, p = 0.554) or current implementation of the CCM as a treatment concept (44 vs 42%, chi-square 2.233, p = 0.135). If the target for HbA1c levels was set according to the initial study protocol at <7% (based on the guideline valid at that time) no significant improvement over time could be found (15 vs 21%, chi-square 1.164, p = 0.281). Practices initially randomised to the intervention group (33 vs 20%, chi-square 5.642, p = 0.018) and practices still working with the CCM achieved this target level significantly more often (32 vs 21%, chi-square 6.888, p = 0.009).
Table 2 Changes in clinical parameters and PACIC according to randomisation to the initial intervention or control group.
|
T0
total population mean (SD) |
T2
total population mean (SD) |
Difference
T2−T0 total population mean (SD) |
Difference
T2−T0 intervention mean (SD) |
Difference
T2−T0 control mean (SD) |
(Difference T2−T0 intervention) − (Difference T2−T02 control)
mean (CI) |
T2
intervention mean (SD) |
T2
control mean (SD) |
T2 intervention – T2 control
mean (CI) |
|
|---|---|---|---|---|---|---|---|---|---|
| HbA1c (%) n = 155 |
7.74 (1.34) |
7.58 (1.32) |
0.16 (1.57) |
−0.43 (1.85) |
0.10 (1.21) |
−0.53* (−1.02, −0.03) |
7.51 (1.49) |
7.65 (1.13) |
−0.14 (−0.55, 0.27) |
| SBP (mm Hg) n = 156 |
140.34 (17.91) |
136.90 (17.83) |
−3.44 (21.02) |
−3.27 (22.45) |
−3.60 (19.73) |
0.34 (−6.33, 7.01) |
138.36 (20.57) |
135.54 (14.83) |
2.82 (−2.82, 8.46) |
| DBP (mm Hg) n = 156 |
81.65 (10.17) |
77.16 (9.27) |
−4.49* (12.04) |
−5.75 (12.80) |
−3.33 (11.25) |
−2.41 (−6.21, 1.39) |
78.51 (8.93) |
75.91 (9.45) |
2.59 (−0.32, 5.51)) |
| LDL (mmol/l) n = 147 |
2.58 (1.09) |
2.52 (0.99) |
−0.06 (1.06) |
−0.02 (1.10) |
−0.12 (1.02) |
0.14 (−0.21, 0.48) |
2.69 (1.03) |
2.37 (0.92) |
0.32 (0.00, 0.63)† |
| PACIC Sum n = 110 |
3.28 (0.83) |
3.18 (0.88) |
0.10 (0.76) |
0.16 (0.72) |
−0.27 (0.73) |
0.43* (0.15, 0.72) |
3.32 (0.89) |
3.12 (0.87) |
0.19 (−0.13, 0.52) |
| PACIC pat. act. n = 122 |
3.94 (1.05) |
3.78 (1.05) |
−0.17 (0.99) |
−0.04 (1.03) |
−0.25 (0.96) |
0.21 (−0.16, 0.58) |
3.76 (1.03) |
3.76 (1.06) |
−0.00 (−0.38, 0.38) |
| PACIC del. sys. n = 122 |
4.01 (0.72) |
3.73 (0.87) |
0.28* (0.89) |
−0.05 (0.98) |
−0.43 (0.81) |
0.38* (0.05, 0.71) |
3.82 (0.86) |
3.66 (0.85) |
0.16 (−0.15, 0.47) |
| PACIC goal set. n = 120 |
3.03 (0.97) |
2.97 (1.00) |
0.06 (0.97) |
0.17 (1.00) |
−0.21 (0.93) |
0.39* (0.02, 0.75) |
3.04 (1.02) |
2.95 (0.98) |
0.09 (−0.27, 0.46) |
| PACIC prob. sol. n = 121 |
3.42 (1.22) |
3.48 (1.20) |
0.05 (1.05) |
0.40 (0.94) |
−0.17 (1.07) |
0.57* (0.17, 0.95) |
3.65 (1.08) |
3.34 (1.26) |
0.31 (−0.13, 0.74) |
| PACIC foll.-up. n = 113 |
2.63 (1.00) |
2.54 (1.05) |
−0.09 (0.94) |
0.05 (1.16) |
−0.18 (0.79) |
0.23 (−0.15, 0.60) |
2.76 (1.20) |
2.42 (0.97) |
0.34 (−0.07, 0.74) |
| CI = 95% confidence interval; control = patients of the original control group; DBP = diastolic blood pressure; intervention = patients of the original intervention group; LDL = low density lipoprotein-cholesterol; PACIC = Patient Assessment of Care for Chronic Conditions; PACIC pat. act = PACIC-subscale patient activation; PACIC del. sys = PACIC subscale delivery system design; PACIC goal set = PACIC subscale goal setting; PACIC prob. sol = PACIC subscale problem solving; PACIC follow.-up = PACIC subscale follow-up; SBP = systolic blood pressure; SD = standard deviation; T0 = baseline CARAT study 2010; T2 = follow-up 2014 * p <0.05 † CI of t-test; since LDL is not normally distributed significance test was performed by means of the two-sample Wilcoxon rank-sum (Mann-Whitney) test, where p = 0.0763. |
|||||||||
Table 3 Changes in clinical parameters and PACIC Score according to treatment with the Chronic Care Model.
|
T2
working with CCM mean (SD) |
T2
working without CCM mean (SD) |
T2 with CCM –
T2 without CCM mean (CI) |
Difference
T2−T0 with CCM mean (SD) |
Difference
T2−T0 without CCM mean (SD) |
(Difference
T2−T0 with CCM) − (Difference T2−T0 without CCM) mean (CI) |
|
|---|---|---|---|---|---|---|
| HbA1c (%) n = 155 |
7.40 (1.33) |
7.73 (1.29) |
−0.33* (−0.74, 0.08)† |
−0.28 (1.41) |
−0.05 (1.69) |
−0.23 (−0.73, 0.26) |
| SBP (mm Hg) n = 156 |
137.24 (19.99) |
136.61 (15.91) |
0.63 (−5.05, 6.30) |
−3.77 (22.65) |
−3.16 (19.67) |
−0.61 (−7.30, 6.08) |
| DBP (mm Hg) n = 156 |
77.48 (8.88) |
76.89 (9.62) |
0.58 (−2.36, 3.53) |
−4.86 (12.16) |
−4.19 (12.00) |
−0.67 (−4.50, 3.16) |
| LDL (mmol/l) n = 147 |
2.52 (0.88) |
2.53 (1.07) |
−0.01 (−0.33, 0.31) |
0.07 (1.05) |
−0.16 (1.05) |
0.23 (−0.12, 0.57) |
| PACIC Sum n = 110 |
3.16 (0.89) |
3.23 (0.83) |
−0.06 (−0.38, 0.27) |
0.06 (0.73) |
−0.22 (0.76) |
0.28 (0.01, 0.57) |
| PACIC pat. act. n = 122 |
3.68 (1.07) |
3.81 (1.03) |
−0.13 (−0.51, 0.24) |
−0.04 (1.07) |
−0.25 (0.92) |
0.22 (−0.15, 0.59) |
| PACIC del. syst. n = 122 |
3.71 (0.78) |
3.73 (0.91) |
−0.03 (−0.33, 0.28) |
−0.16 (0.92) |
−0.37 (0.87) |
0.21 (−0.12, 0.54) |
| PACIC goal set. n = 120 |
2.96 (1.05) |
3.00 (0.96) |
−0.04 (−0.40, 0.32) |
0.14 (0.96) |
−0.2 (0.96) |
0.34 (−0.02, 0.70) |
| PACIC prob. sol. n = 121 |
3.41 (1.15) |
3.50 (1.23) |
−0.09 (−0.53, 0.34) |
0.27 (1.02) |
−0.10 (1.06) |
0.37 (−0.02, 0.76) |
| PACIC foll.-up. n = 113 |
2.59 (1.12) |
2.52 (1.04) |
0.07 (−0.33, 0.47) |
−0.03 (1.05) |
−0.14 (0.87) |
0.11 (−0.26, 0.48) |
| CCM = Chronic Care Model; CI = 95% confidence interval; control = patients of the original control group; DBP = diastolic blood pressure; intervention = patients of the original intervention group; LDL = low density lipoprotein-cholesterol; PACIC = Patient Assessment of Care for Chronic Conditions; PACIC pat. act = PACIC-subscale patient activation; PACIC del. sys = PACIC subscale delivery system design; PACIC goal set = PACIC subscale goal setting; PACIC prob. sol = PACIC subscale problem solving; PACIC follow.-up = PACIC subscale follow-up; SBP = systolic blood pressure; SD = standard deviation; T0 = baseline CARAT study 2010; T2 = follow-up 2014 * p <0.05 † CI of t-test; since Hba1c is not normally distributed significance testing was performed by means of the two-sample Wilcoxon rank-sum (Mann-Whitney) test, where p = 0.0246. |
||||||
Diastolic blood pressure was significantly lower at the current follow-up compared with baseline measures (T0 mean 81.65, SD 10.17 mm Hg vs T2 mean 77.16, SD 9.27 mm Hg; DF 155, p<0.001), whereas the systolic blood pressure did not change significantly (table 2). These findings, as well as achievement of target levels, were independent of original randomisation or treatment concept (tables 2 and 3 ). Target level achievement rates did not change when analysed with the updated or initial target levels of <140/90 mm Hg or <130/80 mm Hg. respectively (data not shown).
No significant difference in LDL-cholesterol levels was found between practices still working with the CCM and practices working with the traditional treatment concept, as well as for randomisation to the original intervention or control group (tables 2 and 3 ). If the target LDL-cholesterol level was 2.6 mmol/l, it was reached significantly more often at the follow-up than at baseline (59 vs 20%, chi-square 16.985, p <0.001, data not shown), independent of initial randomisation (39 vs 48%, chi-square 0.381, p = 0.537) or treatment according to CCM (41 vs 46%, chi-square 0.293, p = 0.588).
The PACIC sum score improved significantly in practices originally randomied to the intervention group compared with the control group (intervention T2−T0 mean 0.16, SD 0.72 vs control T2−T0 mean −0.27, SD 0.73; DF 108, p = 0.003) (table 2). PACIC sum score did not differ between practices currently still working with CCM and practices working with the traditional treatment concept: CCM mean 0.06, SD 0.73 vs non-CCM mean −0.22, SD 0.76; p = 0.057 (table 3). These positive findings were confirmed in three of the five PACIC subscales according to original randomisation: delivery system design (intervention T2−T0 mean −0.05, SD 0.98 vs control T2−T0 mean −0.43, SD 0.81; DF 115, p = 0.024), goal setting (intervention T2−T0 mean 0.17, SD 1.00 vs control T2−T0 mean −0.21, SD 0.93; DF 110, p = 0.037) and problem solving (intervention T2−T0 mean 0.40, SD 0.94 vs control T2−T0 mean −0.17, SD 1.07; DF 110, p = 0.005) (table 2). A trend was found in favour of CCM practices in the subscales goal setting (CCM T2−T0 mean 0.14, SD 0.96 vs no CCM T2−T0 mean −0.2, SD 0.96; DF 110, p = 0.07) and problem solving (CCM T2−T0 mean 0.27, SD 1.02 vs no CCM T0−T2 mean −0.10, SD 1.06; DF 110, p = 0.067) (table 3). For the subscale delivery system design, a significant improvement could be shown (T0 mean 4.01, SD 0.72 vs T2 mean 3.73, SD 0.87; DF 116, p = 0.004). For patient activation a trend in favour of the follow-up was found (T0 mean 3.94, SD 1.05 vs T2 mean 3.78, SD 1.05; DF 114, p = 0.057) (table 2).
Three years after the completion of the randomised controlled CARAT trial, which assessed the effect of implementing the CCM via involvement of a trained practice nurse in the care for type 2 diabetes patients, approximately 40% of PCPs that participated in the follow up continued using the novel treatment model. PCPs originally randomised to the intervention group of the CARAT study were significantly more likely to be still using the CCM. The main reasons for discontinuation were organisational and financial aspects, and the general practitioner not wanting to transfer treatment responsibility. HbA1c and PACIC changes over the long term showed significantly positive effects in favour of PCPs originally randomised to the intervention group and PCPs continuing to treat patients according to the CCM.
The CARAT trial has already shown that the implementation of the CCM, via a specially trained practice nurse exhibiting the central role in the treatment of diabetic patients in Swiss PCP, is possible and feasible [4, 6]. The current long-term follow up confirmed these findings. The treatment concept over 4 years of observation was, however, sustained by less than half of the PCPs. This number is possibly even overestimated owing to selection bias, when considering that the six PCPs that refused participation in the follow up possibly also did not continue treating patients according to CCM. PCPs originally randomised to the intervention group were more likely to continue working with the CCM. This finding can be explained by following considerations: PCPs of the former intervention group had, unlike the former control group, participated in two interactive workshops during the CARAT trial, besides training of the practice nurses. In these workshops, the general practitioners too were trained in the concepts of the CCM. These workshops also offered recurring opportunities to discuss experiences with and organisational barriers to implementing the CCM with other teams, and solutions were jointly developed. The results of the current follow up suggest that training the entire team involved in patient treatment increases understanding and implementation of the CCM, emphasising that this model requires good collaboration between the patients, practice nurse and general practitioner.
The steady increase in chronically ill people in an aging population, paired with lack of appropriately prepared medical staff, puts the continuous and structured treatment of such patients in the spotlight, with a focus on increasing the effectiveness and quality of patient-centred care, as well as cost reduction [14–16]. The concept of task shifting or skill mix as a solution for the shortage of general practitioners has been investigated for a number of different outcomes [17]. For financial aspects especially, such a restructuring of care has become attractive [18, 19]. A meta-analysis by Martinez-Gonzales et al. concluded that care of the chronically ill coordinated by specially trained nurses is at least equivalent to a physician-dominated care structure [20]. Other studies have shown that task shifting might be associated with an increased number and length of consultations, although the frequency and quality of referrals, examinations and prescriptions are comparable to physician-led care [21]. An additional meta-analysis confirmed that nurse-led care achieves similar results to physician-led care if it follows structured therapy protocols [22].
This switch from physician- to nurse-led care presumes a fundamental rethinking of the strongly enrooted and hierarchical patient-physician and physician-practice nurse relationship. In these new models, the practice nurse occupies a more central role in the treatment process, accompanied by an increased authority in the eyes of the patient and of the physician. This change of dogma implies that the physician is capable of transferring the control and authority of patient treatment. Our study showed that this circumstance is a barrier to implementing the CCM in the long term. Our study also showed that from the patients’ perspective there are relevant barriers to the altered patient-physician relationship and to the elements of the CCM that are designed to promote personal responsibility and patient self-management. Some patients prefer seeing complete responsibility for their illness with the physician, which renders the implementation of the CCM nearly impossible. It seems, therefore, wise to implement the concepts of the CCM as soon as possible into patient treatment, in order to promote acceptance and associated motivation.
In addition, current financial barriers hinder the long-term implementation of the CCM. On the one hand, certain financial investments in personnel, training and premises have to be made. On the other hand, the remuneration of specially trained practice nurses is not clearly settled in the Swiss reimbursement system. Many hopes lie in the currently pending revision of the Swiss Standard Billing Rate for outpatient medical care in Switzerland (Tarmed), which plans separate entries of services rendered by the practice nurse.
As shown by numerous studies, the implementation of the CCM can lead to improvement in chronic diseases [23–25], but it has not been proven consistently in all studies. Possible explanations for this inconsistency are offered by the implementation model from Grol and Wensing [26], which groups existing barriers into seven levels: innovation, specialist, patient, social, organisational, economic and political. Our findings are in line with the recently published systematic review from Busetto et al. [27], which showed that most barriers occur on the organisational level, and could be overcome on the social level by means of an increase in personnel and measures improving satisfaction of employees.
Improvement of diabetes care constitutes a massive challenge in medicine. Stellefson et al. have shown improved health of patients with diabetes in general practice with implementation of the CCM elements [28]. The use of single elements was shown not to be crucial, but rather the combination of multiple elements. An improved cardiovascular risk profile could not be achieved by consulting a specialist in the treatment of type 2 diabetes patients [29]. The guidelines for the treatment of diabetic patients, including goal HbA1c, have been modified on the basis of more recent real-life data, taking into consideration that, depending on age and comorbidities, too strict therapy leads to increased morbidity and mortality [30–32].
The baseline HbA1c level of the CARAT population was already relatively low (mean 7.74%) and in the current follow up even lower (mean 7.58%). Therefore, among our study population there was little room for improvement in the HbA1c, without taking the risk of hypoglycaemia into account. Nevertheless, the study showed a significantly lower HbA1c in the original intervention group compared with the original control group 4 years after the intervention. In addition, HbA1c was significantly lower at the time of the current follow up in practices that treat their patients according to the CCM. These two findings undermine the sustained effect of such an intervention, in line with other studies [24], and suggest that a treatment strategy according to the CCM might even lead to a stronger effect in patients who have poorer diabetes control than our population.
The finding that no relevant differences existed between the intervention group and the control group with respect to blood pressure and LDL-cholesterol can be possibly attributed to selection bias, as only general practitioners who have a corresponding interest in the subject were included in the control group. A significant effect on diastolic blood pressure only was found over time, not affected by randomisation or use of CCM. The reason therefore probably lies in the already low values (baseline mean 140.34/81.65 mm Hg, follow up mean136.90/77.16 mm Hg), which met the suggested guideline values of <140/85 mm Hg [32] and which hindered further improvements without risking of side effects. Diverse other studies among patients with less well controlled blood pressure have shown that, by means of task shifting to a trained nurse, a significant effect on systolic blood pressure can be achieved [33]. Also, the lack of significant effects on LDL-cholesterol levels can be explained by the low baseline values (mean 2.58 mmol/l). The improved PACIC scores, independent of original randomisation or use of the CCM, are in line with findings from a meta-analysis that showed that the care by a trained nurse had positive effects on patient satisfaction and hospitalisation rate [34].
Our data originated from a real-life setting in small, mostly single-handed PCPs in Switzerland. The findings are therefore presumably applicable to most European countries with small single-handed practices that are not experienced in involving practice nurses as central agents in patient care. Nevertheless, one has to take into consideration that the extent of medical knowledge and clinical training of practice nurses in Switzerland might not be comparable to those from other European countries. The implementation of elements of the CCM has shown manifold positive effects on diverse chronic diseases, among them diabetes mellitus [35–39]. The benefit of its implementation in small PCPs, which is the most common practice form in most of Europe, has rarely been proven [4, 40]. Our study confirmed that the implementation of the CCM is possible with moderate efforts, including in the long term. The return rate of our follow up was representative at 64.03%.
A possible limitation of our study is that changes during the period of observation, such as new clinical guidance on diabetes care, or the implementation or development of electronic patient records linked with diabetes monitoring systems in the observed PCPs, may have influenced our findings. Furthermore, lack of anonymity/blinding and recall bias are natural limitations of our study. According to our inclusion criteria, only patients with a continuous relation to their general practitioner were eligible to participate, meaning that patients who contacted the practice for emergencies only or as a substitute practice were excluded. Therefore, a certain selection bias was introduced to the study, since it was at the discretion of the participating team (practice nurse and general practitioner) to decide whether the patients was considered a “regular customer”. On the other hand, introducing this selection seems clinically sensible since chronic care is the issue of interest in our study. In addition, a certain selection bias among the participating PCPs has to be considered, since it seems likely that only general practitioners interested in new treatment concepts were willing to participate in the study. However, this renders our findings even more interesting, in terms of barriers to continuing to work with these innovative models in the long term mentioned by such a motivated clientele.
Diabetes care according to the CCM, including the involvement of trained practice nurses, is a reasonable tool to improve care in the long term. CCM training of the whole team is essential to overcome organisational challenges. Continual team education, technical decision support, and recognition of the importance of these new structures by healthcare policy makers might improve the long-term clinical effect of the team approach.
The questionnaire is available as a separate file for downloading at: https://smw.ch/en/article/doi/smw.2017.14522/
The questionnaire is available as a separate file for downloading at https://smw.ch/en/article/doi/smw.2017.14522/
We thank the general practitioners, practice nurses and patients who made this study possible with their enthusiastic participation.
This study was supported by grants from the Swiss Academy for Medical Sciences, SAMW (grant numbers RRMA 8-09 and RRMA 13/10), from Menarini AG, Switzerland and from Margrit und Ruth Stellmacher Foundation. The writing of the report and the decision to submit the article for publication was entirely independent of the funders. The study funders had not input into the study design or analysis, not the interpretation of data.
1 Shaw JE , Sicree RA , Zimmet PZ . Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87(1):4–14. doi:.https://doi.org/10.1016/j.diabres.2009.10.007
2OECD/WHO. OECD Reviews of health systems: Switzerland 2011. OECD Publishing; 2011.
3 Chmiel C , Birnbaum B , Gensichen J , Rosemann T , Frei A . Das Diabetes-Ampelschema - Entwicklung eines Instruments für das hausärztliche Case Management bei Patienten mit Diabetes mellitus. Praxis (Bern). 2011;100(24):1457–73. Article in German. doi:.https://doi.org/10.1024/1661-8157/a000751
4 Frei A , Chmiel C , Schläpfer H , Birnbaum B , Held U , Steurer J , et al. The Chronic CARe for diAbeTes study (CARAT): a cluster randomized controlled trial. Cardiovasc Diabetol. 2010;9(1):23. doi:.https://doi.org/10.1186/1475-2840-9-23
5 Frei A , Herzog S , Woitzek K , Held U , Senn O , Rosemann T , et al. Characteristics of poorly controlled Type 2 diabetes patients in Swiss primary care. Cardiovasc Diabetol. 2012;11(1):70. doi:.https://doi.org/10.1186/1475-2840-11-70
6 Frei A , Senn O , Chmiel C , Reissner J , Held U , Rosemann T . Implementation of the chronic care model in small medical practices improves cardiovascular risk but not glycemic control. Diabetes Care. 2014;37(4):1039–47. doi:.https://doi.org/10.2337/dc13-1429
7 Epping-Jordan JE , Pruitt SD , Bengoa R , Wagner EH . Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004;13(4):299–305. doi:.https://doi.org/10.1136/qshc.2004.010744
8 Wagner EH , Austin BT , Davis C , Hindmarsh M , Schaefer J , Bonomi A . Improving chronic illness care: translating evidence into action. Health Aff (Millwood). 2001;20(6):64–78. doi:.https://doi.org/10.1377/hlthaff.20.6.64
9 American Diabetes Association. Standards of medical care in diabetes--2010. Diabetes Care. 2010;33(Suppl 1):S11–61. doi:. Corrected in: Diabetes Care 2010:33(3):692. https://doi.org/10.2337/dc10-S011
10Schweizerischer Verband medizinischer Praxisassistentinnen. Available from: http://www.sva.ch/no_cache/bildung/weiterbildung/diabetes.html .
11 Glasgow RE , Wagner EH , Schaefer J , Mahoney LD , Reid RJ , Greene SM . Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care. 2005;43(5):436–44. doi:.https://doi.org/10.1097/01.mlr.0000160375.47920.8c
12 Rosemann T , Laux G , Droesemeyer S , Gensichen J , Szecsenyi J . Evaluation of a culturally adapted German version of the Patient Assessment of Chronic Illness Care (PACIC 5A) questionnaire in a sample of osteoarthritis patients. J Eval Clin Pract. 2007;13(5):806–13. doi:.https://doi.org/10.1111/j.1365-2753.2007.00786.x
13Ritchie JLJ. Qualitative research practice: a guide for social science students and researchers. London: Sage Publishing; 2003.
14Global Health Workforce Alliance and World Health Organization. A universal truth: No health without a workforce. Geneva: World health Organization: 2013.
15 Chopra M , Munro S , Lavis JN , Vist G , Bennett S . Effects of policy options for human resources for health: an analysis of systematic reviews. Lancet. 2008;371(9613):668–74. doi:.https://doi.org/10.1016/S0140-6736(08)60305-0
16 Cooper RA . New directions for nurse practitioners and physician assistants in the era of physician shortages. Acad Med. 2007;82(9):827–8. doi:.https://doi.org/10.1097/ACM.0b013e31812f7939
17 Laurant M , Harmsen M , Wollersheim H , Grol R , Faber M , Sibbald B . The impact of nonphysician clinicians: do they improve the quality and cost-effectiveness of health care services? Med Care Res Rev. 2009;66(6, Suppl):36S–89S. doi:.https://doi.org/10.1177/1077558709346277
18 Kreitzer MJ , Kligler B , Meeker WC . Health professions education and integrative healthcare. Explore (NY). 2009;5(4):212–27. doi:.https://doi.org/10.1016/j.explore.2009.05.012
19 Norman I , Normand C , Watson R , Draper J , Jowett S , Coster S . Calculating the costs of work-based training: the case of NHS Cadet Schemes. Int J Nurs Stud. 2008;45(9):1310–8. doi:.https://doi.org/10.1016/j.ijnurstu.2007.10.004
20 Martínez-González NA , Rosemann T , Tandjung R , Djalali S . The effect of physician-nurse substitution in primary care in chronic diseases: a systematic review. Swiss Med Wkly. 2015;145:w14031.
21 Martínez-González NA , Rosemann T , Djalali S , Huber-Geismann F , Tandjung R . Task-Shifting From Physicians to Nurses in Primary Care and its Impact on Resource Utilization: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Med Care Res Rev. 2015;72(4):395–418. doi:.https://doi.org/10.1177/1077558715586297
22 Martínez-González NA , Tandjung R , Djalali S , Rosemann T . The impact of physician-nurse task shifting in primary care on the course of disease: a systematic review. Hum Resour Health. 2015;13(1):55. doi:.https://doi.org/10.1186/s12960-015-0049-8
23 Drewes HW , Steuten LM , Lemmens LC , Baan CA , Boshuizen HC , Elissen AM , et al. The effectiveness of chronic care management for heart failure: meta-regression analyses to explain the heterogeneity in outcomes. Health Serv Res. 2012;47(5):1926–59. doi:.https://doi.org/10.1111/j.1475-6773.2012.01396.x
24 Elissen AM , Steuten LM , Lemmens LC , Drewes HW , Lemmens KM , Meeuwissen JA , et al. Meta-analysis of the effectiveness of chronic care management for diabetes: investigating heterogeneity in outcomes. J Eval Clin Pract. 2013;19(5):753–62.
25 Lemmens KM , Lemmens LC , Boom JH , Drewes HW , Meeuwissen JA , Steuten LM , et al. Chronic care management for patients with COPD: a critical review of available evidence. J Eval Clin Pract. 2013;19(5):734–52.
26 Grol R , Wensing M . What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust. 2004;180(6, Suppl):S57–60.
27 Busetto L , Luijkx KG , Elissen AM , Vrijhoef HJ . Context, mechanisms and outcomes of integrated care for diabetes mellitus type 2: a systematic review. BMC Health Serv Res. 2016;16(1):18. doi:.https://doi.org/10.1186/s12913-015-1231-3
28 Stellefson M , Dipnarine K , Stopka C . The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:120180. doi:.https://doi.org/10.5888/pcd10.120180
29 Smith SM , Paul G , Kelly A , Whitford DL , O’Shea E , O’Dowd T . Peer support for patients with type 2 diabetes: cluster randomised controlled trial. BMJ. 2011;342(feb15 1):d715. doi:.https://doi.org/10.1136/bmj.d715
30 Rydén L , Standl E , Bartnik M , Van den Berghe G , Betteridge J , de Boer M-J , et al.; Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC); European Association for the Study of Diabetes (EASD). Guidelines on diabetes, pre-diabetes, and cardiovascular diseases: executive summary. Eur Heart J. 2007;28(1):88–136.
31 Boyd CM , Vollenweider D , Puhan MA . Informing evidence-based decision-making for patients with comorbidity: availability of necessary information in clinical trials for chronic diseases. PLoS One. 2012;7(8):e41601. doi:.https://doi.org/10.1371/journal.pone.0041601
32 Rydén L , Grant PJ , Anker SD , Berne C , Cosentino F , Danchin N , et al., Document Reviewers. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J. 2013;34(39):3035–87. doi:.https://doi.org/10.1093/eurheartj/eht108
33 Martínez-González NA , Tandjung R , Djalali S , Huber-Geismann F , Markun S , Rosemann T . Effects of physician-nurse substitution on clinical parameters: a systematic review and meta-analysis. PLoS One. 2014;9(2):e89181. doi:.https://doi.org/10.1371/journal.pone.0089181
34 Martínez-González NA , Djalali S , Tandjung R , Huber-Geismann F , Markun S , Wensing M , et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14(1):214. doi:.https://doi.org/10.1186/1472-6963-14-214
35 Adams SG , Smith PK , Allan PF , Anzueto A , Pugh JA , Cornell JE . Systematic review of the chronic care model in chronic obstructive pulmonary disease prevention and management. Arch Intern Med. 2007;167(6):551–61. doi:.https://doi.org/10.1001/archinte.167.6.551
36 Parchman ML , Pugh JA , Wang CP , Romero RL . Glucose control, self-care behaviors, and the presence of the chronic care model in primary care clinics. Diabetes Care. 2007;30(11):2849–54. doi:.https://doi.org/10.2337/dc06-2516
37 Parchman ML , Zeber JE , Romero RR , Pugh JA . Risk of coronary artery disease in type 2 diabetes and the delivery of care consistent with the chronic care model in primary care settings: a STARNet study. Med Care. 2007;45(12):1129–34. doi:.https://doi.org/10.1097/MLR.0b013e318148431e
38 Sunaert P , Bastiaens H , Nobels F , Feyen L , Verbeke G , Vermeire E , et al. Effectiveness of the introduction of a Chronic Care Model-based program for type 2 diabetes in Belgium. BMC Health Serv Res. 2010;10(1):207. doi:.https://doi.org/10.1186/1472-6963-10-207
39 Piatt GA , Orchard TJ , Emerson S , Simmons D , Songer TJ , Brooks MM , et al. Translating the chronic care model into the community: results from a randomized controlled trial of a multifaceted diabetes care intervention. Diabetes Care. 2006;29(4):811–7. doi:.https://doi.org/10.2337/diacare.29.04.06.dc05-1785
40 Nutting PA , Dickinson WP , Dickinson LM , Nelson CC , King DK , Crabtree BF , et al. Use of chronic care model elements is associated with higher-quality care for diabetes. Ann Fam Med. 2007;5(1):14–20. doi:.https://doi.org/10.1370/afm.610
This study was supported by grants from the Swiss Academy for Medical Sciences, SAMW (grant numbers RRMA 8-09 and RRMA 13/10), from Menarini AG, Switzerland and from Margrit und Ruth Stellmacher Foundation. The writing of the report and the decision to submit the article for publication was entirely independent of the funders. The study funders had not input into the study design or analysis, not the interpretation of data.