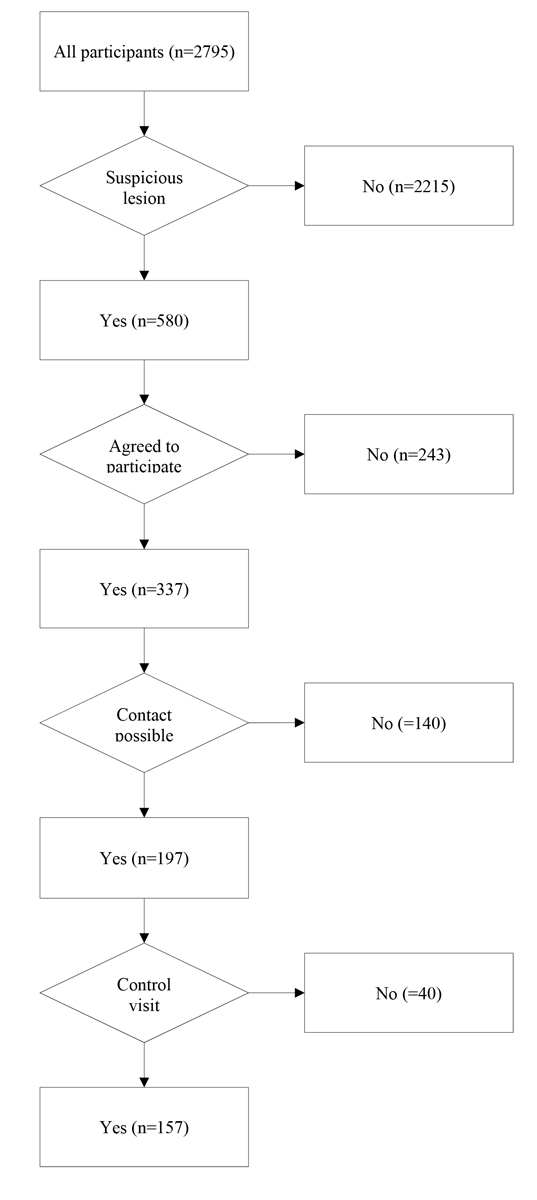
Figure 1 Follow-up of participants Swiss Euromelanoma 2016.
DOI: https://doi.org/10.4414/smw.2017.14511
Skin cancer is a non-negligible burden to healthcare and patients alike. Epidemiological data are collected on a regular basis to estimate the extent of the disease. Various prevention approaches have been introduced to reduce the burden of skin cancers. Primary prevention focuses on spread of information about and reduction of skin cancer-related risk factors and behaviour, namely reducing sun exposure, avoidance of sunburn and artificial tanning or use of sunscreen when ultraviolet radiation (UV) exposure is unavoidable. Furthermore, it tries to raise awareness among the public of warning signs of skin cancer [1–3]. Secondary prevention aims to diagnose and treat skin cancer at a potentially curable stage, to improve prognosis and thus reduce the burden of melanoma on healthcare resources and patients [1, 2].
Euromelanoma is a pan-European campaign for skin cancer prevention, which was initiated in 1999 and has now spread to 29 European countries. This campaign is targeted to both primary and secondary prevention of malignant melanoma (MM) and nonmelanoma skin cancers (NMSCs) by increasing the public awareness of skin tumours via media campaigns and by providing free skin examinations to the general public once a year, at the end of May before the summer holiday season [1–4].
As Switzerland has one of the highest incidences of cutaneous melanoma in Europe [5, 6], a National Skin Cancer-Screening Day has been organised there since 2001, on a yearly base [5, 7]. In 2006, the Swiss Society for Dermatology and Venerology (SSDV), in collaboration with the Swiss Cancer League, shifted its skin cancer prevention activities towards a Euromelanoma Screening Week Campaign to promote primary prevention measures by use of media advertising to a large public and the direct education of the patient at the screening day itself [5, 7]. The current study aimed to evaluate the results from the Swiss skin cancer screening day 2016 and investigate the number of skin cancer diagnoses based on the suspicious lesions detected.
A free-of-charge skin examination was offered within the annual Euromelanoma skin cancer prevention campaign and organised by the SSDV (from 30 May 2016 to 3 June 2016). In the National Skin Cancer Campaign 2016, 93 medical centres (69 dermatological practices and 24 general practices) were involved. Participating physicians (dermatologists and general practitioners) in hospitals or in private practices conducted the screening examinations. Participating doctors chose whether they wanted to see patients by appointment or if people could turn up at their practice freely.
The examination process was structured by using the standardised European questionnaire developed in 2008 [7, 8] (see appendix 1). The questionnaire consists of three sections:
Patients were informed about the aim of the study (for quality assessment) and study procedures, and could leave their e-mail address or phone number when they agreed to participate. Ethics approval was not necessary according to Swiss Human Research Act (https://www.admin.ch/opc/en/classified-compilation/20061313/index.html, accessed April 8, 2016). All questionnaires were sent to the SSDV office. After 3 to 6 months, all screened persons participating in the study who had a suspicious lesion were contacted either by e-mail or telephone. In the case of no-response, the patient was contacted for a second time. Patients who gave their permission were asked whether they had followed the physician’s recommendation. Finally, the patients were asked about the definite diagnosis. All results of the questionnaire and the follow-up data were collected in a file.
For descriptive purposes, data were presented as means with standard deviations (SDs) or numbers with percentages for continuous and categorical variables respectively. Prevalences (i.e., detection rates) of selected skin cancers and other precancerous conditions within the study sample were presented along with their exact (Clopper-Pearson) 95% confidence intervals (CIs). The ratios between study prevalences and known estimates from the general Swiss population (i.e., prevalence ratios), where available, were computed, with exact 95% CIs and p-values. Detection rate is defined here as the percentage of subjects in the overall study population who had a positive diagnosis of skin cancer or other precancerous conditions after clinical assessment.
All tests were considered statistically significant at p-value <0.05. The analysis was carried out using Matlab software, ver. 7.8 (The MathWorks Inc., Natick, MA, USA).
The participating physicians examined 2795 individuals (Female: 63.2%, Male: 36.8%) with mean (SD) age of 51.65 (18.25) years, covering all of Switzerland’s geographic regions. Figure 1 presents the entire workflow. A total 2215 (79.3%) screened individuals required no further treatment. Suspicious lesions were found in 580 (20.7%) patients. Out of these 580 patients, 243 (41.9%) patients did not agree to be contacted again to assess quality 3 to 6 months later. From the 337 who were willing to participate in the study, 140 (41.5%) were not reachable because of either incorrect contact details or no reply. Of the 197 available patients, 40 (20.3%) patients declared not having followed the physician’s recommendation of referral to a dermatologist. The remaining 157 (79.7%) participants had a check-up visit at a dermatologist.
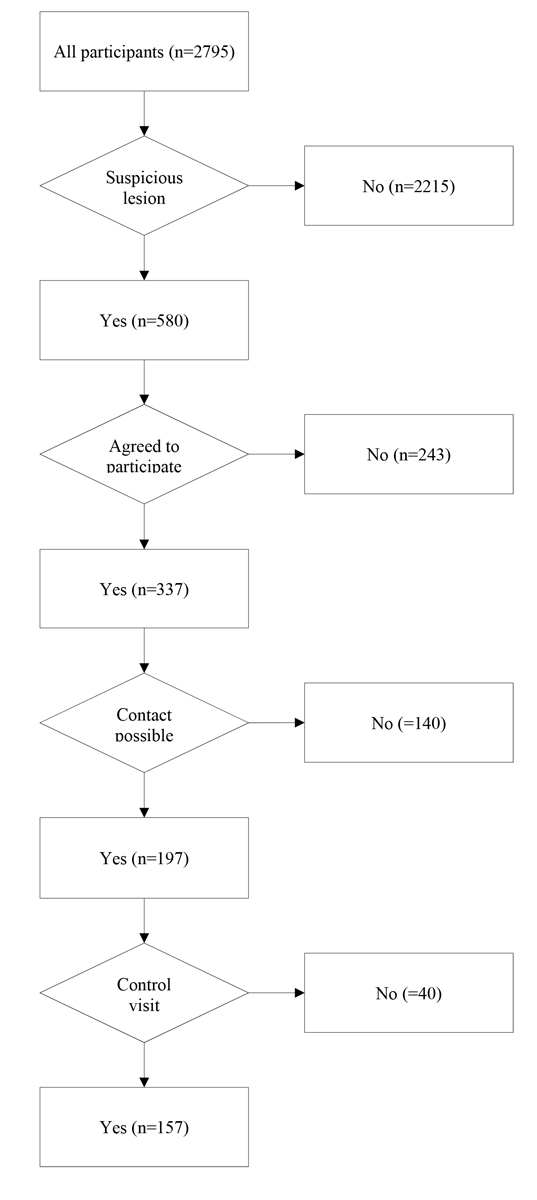
Figure 1 Follow-up of participants Swiss Euromelanoma 2016.
A total of 81 out of 157 lesions were reported to be biopsied. Among these 157 cases were found 6 MM (6/6 biopsied), 21 basal cell carcinomas (BCCs) (17/21 biopsied), 2 squamous cell carcinomas (SCCs) (2/2 biopsied), 44 actinic keratoses (8/44 biopsied) and 3 dysplastic/atypical naevi (3/3 biopsied). Seventy-four cases were without pathological findings (41/74 biopsied) and in 7 cases the diagnosis was not communicated. Detection rates differed between the various types of skin cancer. The malignant melanoma detection rate was 1:466 and the detection rate for BCC was 1:133. SCC detection rate was the lowest at 1:1398. (table 1)
Table 1 Distribution of diagnosis, biopsies and detection rate during Swiss Euromelanoma 2016†.
| Diagnosis | No. of reported cases | No. of biopsies | Detection rate*‡ | ||||
|---|---|---|---|---|---|---|---|
| n | % | % | |||||
| MM | 6 | 3.8 | 6 | 0.21 | |||
| BCC | 21 | 13.4 | 17 | 0.75 | |||
| SCC | 2 | 1.3 | 2 | 0.07 | |||
| AK | 44 | 28.0 | 8 | 1.57 | |||
| Atypical naevus, Dysplastic naevus | 3 | 1.9 | 3 | 0.11 | |||
| Not specified | 7 | 4.5 | 4 | 0.25 | |||
| Negative | 74 | 47.1 | 41 | 2.65 | |||
AK = actinic keratosis; BCC = basal cell carcinoma; MM = malignant melanoma; NMSC = non-melanoma skin cancer; SCC = squamous cell carcinoma † based on recorded data of 157 patients * Detection rate can be defined here as the percentage of subjects in the overall study population who had a positive diagnosis of skin cancer or other precancerous conditions after clinical assessment. ‡ Detection rates of MM, SCC and BCC in the Swiss National Skin Cancer Campaign in 2008 were 0.3, 0.15 and 0.38%, respectively.
The description of the epidemiological data is based on the 157 (91 female, 66 male) participants with a suspicious lesion who underwent a referral to a dermatologist. The majority of the 157 patients were female (58.0%) and the mean age was 58.8 years for both genders. The skin phototypes I, II, III or IV were reported for 8.9%, 15.9%, 47.1% and 23.6% of the patients, respectively. Overall, 69.4% had never had a skin cancer screening before. Most of the participants (47.8%) attended the screening for a general skin examination; 40.1% gave a high number of naevi as a reason to participate in the campaign and about one fifth of the patients (21.7%) were concerned about a specific or newly appeared lesion. (table 2)
Table 2 Reasons for participation in the campaign and previous skin cancer screenings†.
| No. of participants | ||
|---|---|---|
| n | % | |
| Reason for participation ‡ | ||
| Many naevi | 63 | 40.1% |
| New or change in naevi | 34 | 21.7% |
| Personal history of skin cancer | 15 | 9.6% |
| Family history of skin cancer | 14 | 8.9% |
| General skin examination | 75 | 47.8% |
| Previous skin examination | ||
| Yes | 46 | 29.3% |
| No | 109 | 69.4% |
| Not specified | 2 | 1.3% |
† Based on recorded data of 157 patients ‡ Multiple answers allowed
Table 3 shows the distribution of sun-related risk factors and history of skin cancer. Most patients showed neither a positive family history (88.5%) nor a personal history (91.7%) of skin cancer; 46.5% had fewer than 25 naevi and a minority of 5.7% presented more than 100 naevi. Regarding sun-seeking behaviour, 41.4% of the participants confirmed a sunburn under the age of 18 years (38.2% had no sunburn). Sunscreen was reported to always be applied when sunbathing by 59.9%, 21.7% of the participants sometimes used sun protection and 13.4% never sunbathed. Reportedly, 23.6% never went on vacation to highly sun-exposed areas, 45.9% stayed in such regions for up to 2 weeks and 28.7% more than 2 weeks per year.
Table 3 Distribution of the risk factors family history of skin cancer, sunburn in childhood, use of sunscreen and vacation in areas with high sun exposure†.
| Risk factors †‡ | No. of participants | |
|---|---|---|
| n | % | |
| Family history of skin cancer | ||
| Yes | 12 | 7.6% |
| No | 139 | 88.5% |
| Personal history of skin cancer | ||
| MM | 6 | 3.8% |
| NMSC | 6 | 3.8% |
| No | 144 | 91.7% |
| Sunburn in childhood | ||
| Yes | 65 | 41.4% |
| No | 60 | 38.2% |
| Use of sunscreen during 1-hour exposure | ||
| Never | 13 | 8.3% |
| Sometimes | 76 | 48.4% |
| Always | 66 | 42.0% |
| Use of sunscreen while sunbathing | ||
| Never | 6 | 3.8% |
| Sometimes | 34 | 21.7% |
| Always | 94 | 59.9% |
| Vacation in sun exposed areas | ||
| Never | 37 | 23.6% |
| Up to 2 weeks per year | 72 | 45.9% |
| More than 2 weeks per year | 45 | 28.7% |
| MM = malignant melanoma; NMSC = nonmelanoma skin cancer † Based on recorded data of 157 patients ‡ Numbers do not always add up to the total because of missing data. |
||
Prevalence estimates of skin cancers and other precancerous conditions, in detail, and comparisons with known estimates from the general population are reported in table 4. Overall. 6 patients in the sampling population had a diagnosis of MM with an estimated prevalence of 21.5 × 10 000 (95% CI 7.9–46.7). Regarding NMSC, the observed prevalence of BCC was 75.1 × 10 000 (95% CI 46.6–114.6), and the prevalence of SCC was 10.7 × 10 000 (95% CI 2.2–31.3). For other precancerous conditions, the estimated prevalence of actinic keratosis in our sample was 157.4 × 10 000 (95% CI 114.6–210.8, and the prevalence of dysplastic naevus was 10.7 × 10 000 (95% CI 2.2–31.3).
Table 4 Prevalence estimates of skin cancers and other pre-cancerous conditions, in detail, and comparisons with known estimates from the general population†.
|
Total
(n = 77) |
Pr × 10 000 in the overall study population
(n = 2795) (95% CI) |
Pr × 10 000 in the general population |
Pr ratio#
(95% CI) |
p-value | ||
|---|---|---|---|---|---|---|
| n | % | |||||
| BCC | 21 | 13.4% | 75.1 (46.6–114.6) | 8.0* | 9.4 (5.8–14.3) | <0.001 |
| SCC | 2 | 1.3% | 10.7 (2.2–31.3) | 3.0* | 3.6 (0.7–10.4) | 0.06 |
| MM | 6 | 3.8% | 21.5 (7.9–46.7) | 3.3‡ | 6.4 (2.4–14.0) | <0.001 |
| AK | 44 | 28.0% | 157.4 (114.6–210.8) | 140 (120–180)§ | 1.1 (0.8–1.6) | 0.53 |
| Dysplastic naevus | 3 | 1.9% | 10.7 (2.2–31.3) | NA | – | – |
AK = actinic keratosis; BCC = basal cell carcinoma; CI = confidence interval; MM = malignant melanoma; NA = not available; Pr = prevalence; SCC = squamous cell carcinoma † Based on recorded data of 157 patients * Levi F et al. 2001 [9] ‡ 2012 EUCAN 1-yr Pr estimates for Switzerland § Naldi L et al. 2006 [10] # Prevalence: the relative frequency of a condition of interest in the sampled population
Skin cancer is one of the most common cancers in Switzerland [11]. In this study, data collected during the Swiss Euromelanoma screening day 2016 were analysed to provide a current picture of the impact of the campaign and a basis for future measures to improve the screening event.
The detection rates of melanoma in Euromelanoma programmes varied substantially across participating countries (from 0.1 to 1.9%) [3]. The results of the 2016 Swiss Euromelanoma Day showed a detection rate for melanoma of 0.21%, which is compatible to similar European and American studies [1–3, 12, 13]. However, compared with the Swiss Euromelanoma evaluation conducted in 2008 with the same methodology and public awareness strategy on 1312 screened individuals [7], the melanoma detection rate was found to be lower (0.21 vs 0.30%).
Although the main focus of the Euromelanoma Day is the early diagnosis of melanoma [14], our campaign also detected some patients with NMSC; the BCC detection rate was higher and SCC detection rate lower in 2016 compared with 2008(0.75 vs 0.38% and 0.07 vs 0.15%, respectively) [7]. Furthermore, comparisons of prevalence estimates of skin cancers and other precancerous conditions between the current study and the general population showed that 6 patients in the sampling population had a diagnosis of MM with an estimated prevalence of 21.5 × 10 000. The observed prevalence was significantly higher than in the general population (prevalence ratio 6.4; p <0.001). Regarding NMSC, the observed prevalence of BCC was 75.1 × 10 000, and the prevalence of SCC was 10.7 × 10 000. Compared with general population estimates, the prevalence of BCC was significantly higher (prevalence ratio 9.4; p <0.001) [9]. For other precancerous conditions, the estimated prevalence of actinic keratosis in our sample was 157.4 × 10 000, similarly to previous estimates from another study [10], while the prevalence of dysplastic naevus was 10.7 × 10 000.
In 2016, 70.7% of the persons screened had a skin phototype III or higher, which was similar to data reported by individual Euromelanoma countries in previous years [3]. Additionally, in concordance with Euromelanoma Day campaigns in other countries, women were more likely than men to participate in the Swiss screenings [3, 14]. Women are probably more conscious about the risk factors and more accustomed to attending cancer screening campaigns [14]. Sun exposure is a known risk factor of skin cancers. Three quarters of all participants go on vacation to destinations with high solar radiation on a yearly basis. This behaviour results in elevated intermittent sun exposure. Awareness of the need for adequate sun protection while sunbathing seems to be high. The impact of unintended sun exposure appears to be taken less seriously, however. Twenty percent fewer screened persons used sun screen when exposed to sunlight for one hour than sunbathers. The elevated numbers of BCCs and MMs could be explained by widespread intermittent sun exposure. These findings reveal a continuing need of public education about UV radiation as a risk factor, not only when sunbathing but also when exposure is not intended.
Skin cancer screening of an unselected population is controversial: the Cancer Council Australia does not recommend routine skin screening for average-risk individuals, whereas the American Cancer Society supports this type of regular screening [15]. Skin cancer screening could be accompanied by psychosocial harms, cosmetic harms, or overdiagnosis [16]. However, it was shown that skin cancer screening might be able to reduce disease-specific mortality [17–22].
The success of the Euromelanoma days depends on many factors, including the number of dermatologists who participate, as well as the costs of the screening and information campaigns. Furthermore, the characteristics of the population screened during Euromelanoma were influenced by the message broadcasted and local rules of participation [3].
Our current study was certainly not without limitations, because the individuals screened were relatively older than the Swiss population, with a predominance of women. Another possible limitation of the study is that not all of the subjects with suspect lesions were followed up, because they did not give permission to be contacted for further evaluation. This might have lowered our detection rate estimates. Nevertheless, the observed rates are significantly higher, at least for MM and BCC, than the reference general population, showing a positive impact of a national campaign of screening on detection rates.
All in all, skin cancer prevention initiatives are highly cost-effective and may also be cost-saving [23]. Although the direct benefits of skin cancer screening may be greatest among subgroups most likely to develop fatal melanoma [16], indirect consequences of screening campaigns should not be underestimated. The impact of skin cancer diagnoses on the awareness of the social circle of a patient can hardly be measured. This spread of consciousness of skin cancer might influence the risk factor-related behaviour and secondary prevention can thus reinforce primary prevention efforts. Therefore, considering the morbidity, mortality and financial and social impact of skin cancer, the capacity to raise awareness of risk factors, skin cancer prevention methods and educating high-risk and at-risk individuals, we may assume that a National Screening Day does have a crucial impact on the public health system.
The questionnaires are available as separate files for downloading at https://smw.ch/en/article/doi/smw.2017.14511/.
The authors thank all participating dermatologists, physicians, sponsors, SSDV and First Aid Marketing staff for their kind effort and professional support in Euromelanoma 2016 in Switzerland. The authors thank Dr Max Gabutti for translation.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Suppa M , Altomare G , Cannavò SP , Capizzi R , Catricalà C , Colombo E , et al.; Italian investigators for the Euromelanoma prevention campaign. The Italian Euromelanoma Day: evaluation of results and implications for future prevention campaigns. Int J Dermatol. 2014;53(6):699–706. doi:.https://doi.org/10.1111/j.1365-4632.2012.05783.x
2 Stratigos AJ , Forsea AM , van der Leest RJ , de Vries E , Nagore E , Bulliard JL , et al. Euromelanoma: a dermatology-led European campaign against nonmelanoma skin cancer and cutaneous melanoma. Past, present and future. Br J Dermatol. 2012;167(Suppl 2):99–104. doi:.https://doi.org/10.1111/j.1365-2133.2012.11092.x
3 van der Leest RJ , de Vries E , Bulliard JL , Paoli J , Peris K , Stratigos AJ , et al. The Euromelanoma skin cancer prevention campaign in Europe: characteristics and results of 2009 and 2010. J Eur Acad Dermatol Venereol. 2011;25(12):1455–65. doi:.https://doi.org/10.1111/j.1468-3083.2011.04228.x
4 Forsea AM , del Marmol V ; Euromelanoma Working Group. Impact, challenges and perspectives of Euromelanoma, a pan-European campaign of skin cancer prevention. J Eur Acad Dermatol Venereol. 2013;27(10):1317–9.
5 Bulliard JL , Panizzon RG , Levi F . Prévention du métanome en Suisse: où en sommes-nous ? [Melanoma prevention in Switzerland: where do we stand?]. Rev Med Suisse. 2006;2(63):1122–5. Article in French.
6 Hunger RE , Seyed Jafari SM , Angermeier S , Shafighi M . Excision of fascia in melanoma thicker than 2 mm: no evidence for improved clinical outcome. Br J Dermatol. 2014;171(6):1391–6. doi:.https://doi.org/10.1111/bjd.13478
7 Bulliard JL , Maspoli M , Panizzon RG , Hohl D , Gueissaz F , Levi F . Evaluation of the Euromelanoma skin cancer screening campaign: the Swiss experience. J Eur Acad Dermatol Venereol. 2008;22(3):365–6. doi:.https://doi.org/10.1111/j.1468-3083.2007.02316.x
8 Suppa M , Neri L , Bianchi L , Capizzi R , Carbone A , Catricalà C , et al. The first skin cancer screening day at the Italian parliament: a Euromelanoma initiative. Int J Dermatol. 2015;54(1):42–9. doi:.https://doi.org/10.1111/ijd.12677
9 Levi F , Te VC , Randimbison L , Erler G , La Vecchia C . Trends in skin cancer incidence in Vaud: an update, 1976-1998. Eur J Cancer Prev. 2001;10(4):371–3. doi:.https://doi.org/10.1097/00008469-200108000-00011
10 Naldi L , Chatenoud L , Piccitto R , Colombo P , Placchesi EB , La Vecchia C ; Prevalence of Actinic Keratoses Italian Study (PraKtis) Group. Prevalence of actinic keratoses and associated factors in a representative sample of the Italian adult population: Results from the Prevalence of Actinic Keratoses Italian Study, 2003-2004. Arch Dermatol. 2006;142(6):722–6. doi:.https://doi.org/10.1001/archderm.142.6.722
11 Seyed Jafari SM , Jäckle P , Michel A , Angermeier S , Hunger R , Shafighi M . Prognostic value of sentinel lymph node biopsy in melanomas of different Breslow’s thickness. Swiss Med Wkly. 2016;146:w14358.
12 Seidenari S , Benati E , Ponti G , Borsari S , Ferrari C , Albertini G , et al. Italian Euromelanoma Day Screening Campaign (2005-2007) and the planning of melanoma screening strategies. Eur J Cancer Prev. 2012;21(1):89–95. doi:.https://doi.org/10.1097/CEJ.0b013e3283498e14
13 Geller AC , Zhang Z , Sober AJ , Halpern AC , Weinstock MA , Daniels S , et al. The first 15 years of the American Academy of Dermatology skin cancer screening programs: 1985-1999. J Am Acad Dermatol. 2003;48(1):34–41. doi:.https://doi.org/10.1067/mjd.2003.9
14 Paoli J , Danielsson M , Wennberg AM . Results of the ‘Euromelanoma Day’ screening campaign in Sweden 2008. J Eur Acad Dermatol Venereol. 2009;23(11):1304–10. doi:.https://doi.org/10.1111/j.1468-3083.2009.03316.x
15 Tripp MK , Watson M , Balk SJ , Swetter SM , Gershenwald JE . State of the science on prevention and screening to reduce melanoma incidence and mortality: The time is now. CA Cancer J Clin. 2016;66(6):460–80. doi:.https://doi.org/10.3322/caac.21352
16 Wernli KJ , Henrikson NB , Morrison CC , Nguyen M , Pocobelli G , Blasi PR . Screening for Skin Cancer in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2016;316(4):436–47. doi:.https://doi.org/10.1001/jama.2016.5415
17 Geller AC , Greinert R , Sinclair C , Weinstock MA , Aitken J , Boniol M , et al. A nationwide population-based skin cancer screening in Germany: proceedings of the first meeting of the International Task Force on Skin Cancer Screening and Prevention (September 24 and 25, 2009). Cancer Epidemiol. 2010;34(3):355–8. doi:.https://doi.org/10.1016/j.canep.2010.03.006
18 Katalinic A , Waldmann A , Weinstock MA , Geller AC , Eisemann N , Greinert R , et al. Does skin cancer screening save lives?: an observational study comparing trends in melanoma mortality in regions with and without screening. Cancer. 2012;118(21):5395–402. doi:.https://doi.org/10.1002/cncr.27566
19 Katalinic A , Kunze U , Schäfer T . Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig-Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer). Br J Dermatol. 2003;149(6):1200–6. doi:.https://doi.org/10.1111/j.1365-2133.2003.05554.x
20 Shellenberger R , Nabhan M , Kakaraparthi S . Melanoma screening: A plan for improving early detection. Ann Med. 2016;48(3):142–8. doi:.https://doi.org/10.3109/07853890.2016.1145795
21 Boniol M , Autier P , Gandini S . Melanoma mortality following skin cancer screening in Germany. BMJ Open. 2015;5(9):e008158. doi:.https://doi.org/10.1136/bmjopen-2015-008158
22 Lakhani NA , Saraiya M , Thompson TD , King SC , Guy GP, Jr . Total body skin examination for skin cancer screening among U.S. adults from 2000 to 2010. Prev Med. 2014;61:75–80. doi:.https://doi.org/10.1016/j.ypmed.2014.01.003
23 Gordon LG , Rowell D . Health system costs of skin cancer and cost-effectiveness of skin cancer prevention and screening: a systematic review. Eur J Cancer Prev. 2015;24(2):141–9. doi:.https://doi.org/10.1097/CEJ.0000000000000056
Sven Lieberherr and S. Morteza Seyed Jafari contributed equally to this work.
No financial support and no other potential conflict of interest relevant to this article was reported.