Beliefs, endorsement and application of homeopathy disclosed: a survey among ambulatory care physicians
DOI: https://doi.org/10.4414/smw.2017.14505
Stefan
Markun, Marc
Maeder, Thomas
Rosemann, Sima
Djalali
Institute of Primary Care, University of Zurich, University Hospital Zurich, Switzerland
Summary
BACKGROUND
Explanation models for the effectiveness of homeopathy are not supported by natural sciences and the aggregated evidence from clinical trials is unconvincing. From this standpoint, placebo effects seem the most obvious explanation for the therapeutic effects experienced in homeopathy. Still, many physicians continue to prescribe homeopathic treatments.
OBJECTIVES
Whether physicians who prescribe homeopathic treatments aim to achieve placebo effects or actually believe in specific effects is poorly understood. However, this distinction has important educational and ethical implications. Therefore, we aimed to describe the use of homeopathy among physicians working in outpatient care, factors associated with prescribing homeopathy, and the therapeutic intentions and attitudes involved.
METHODS
All physicians working in outpatient care in the Swiss Canton of Zurich in the year 2015 (n = 4072) were approached. Outcomes of the study were: association of prescribing homeopathy with medical specialties (odds ratios [OR] and 95% confidence intervals [95% CI] from multivariable logistic regression); intentions behind prescriptions (to induce specific or nonspecific/placebo effects); level of agreement with specific attitudes; and views towards homeopathy including explanatory models, rating of homeopathy’s evidence base, the endorsement of indications, and reimbursement of homeopathic treatment by statutory health insurance providers.
RESULTS
The participation rate was 38%, mean age 54 years, 61% male, and 40% specialised in general internal medicine. Homeopathy was prescribed at least once a year by 23% of the respondents. Medical specialisations associated with prescribing homeopathy were: no medical specialisation (OR 3.9; 95% CI 1.7-9.0), specialisation in paediatrics (OR 3.8 95% CI 1.8-8.0) and gynaecology/obstetrics (OR 3.1 95% CI 1.5-6.7). Among prescribers, only 50% clearly intended to induce specific homeopathic effects, only 27% strongly adhered to homeopathic prescription doctrines, and only 23% thought there was scientific evidence to prove homeopathy’s effectiveness. Seeing homeopathy as a way to induce placebo effects had the strongest endorsement among prescribers and non-prescribers of homeopathy (63% and 74% endorsement respectively). Reimbursement of homeopathic remedies by statutory health insurance was rejected by 61% of all respondents.
CONCLUSION
Medical specialties use homeopathy with significantly varying frequency and only half of the prescribers clearly intend to achieve specific effects. Moreover, the majority of prescribers acknowledge that effectiveness is unproven and give little importance to traditional principles behind homeopathy. Medical specialties and associated patient demands but also physicians’ openness towards placebo interventions may play a role in homeopathy prescriptions. Education should therefore address not only the evidence base of homeopathy, but also ethical dilemmas with placebo interventions.
Introduction
Since its creation, homeopathy has appeared to divide the medical community between supporters and opponents, and has spurred discussion about its effectiveness. Up to now, the mainstays of homeopathic doctrine have contradicted established principles of natural sciences, and comprehensible models consistently explaining how homeopathy could cause specific effects are lacking [1]. Nonetheless, homeopathy remains popular not only among the general public, but also among a considerable proportion of medical professionals [2–4]. In Switzerland, as in other countries, homeopathy is even integrated into national health systems and health plans [5–8].
Scientifically, most accepted explanations for people’s perception of the beneficial effects of homeopathy are built around placebo effects, i.e. either simply by knowing that they are receiving treatment, or from the effects of homeopathic consultation [9, 10]. Interestingly, several studies have addressed attitudes towards placebo treatments both from the caregivers’ and patients’ points of view, and found high acceptance if certain conditions are met [11, 12]. Instead of or (depending on their beliefs) in addition to specific effects, physicians may therefore use homeopathy intentionally or without reflection to achieve placebo effects.
Distinctions between intentions and beliefs behind homeopathic prescriptions are important from ethical and educational perspectives. Prescribing homeopathy solely with the intention of achieving placebo effects and without informing the patient to this effect is considered deceitful, and is prohibited by ethical authorities. However, if the prescribing physician believes in the specific effects of homeopathy, the matter of deception ceases to exist, and there are no further ethical implications to consider. In order to believe in specific effects, physicians somehow need to give credibility to the concept either by their own appraisal of the evidence base, or by believing in any of the explanatory models for the effectiveness of homeopathy (the most eminent being the Law of Similars including the method of “potentization” by ultra-dilution).
Little is currently known about the beliefs and intentions of physicians who prescribe homeopathy. While in public, homeopathy is commonly discussed by extreme proponents and adversaries, the point of view of the majority of physicians is unknown. Knowledge about these perspectives, however, is needed to foster a productive dialogue and discuss the role of homeopathy in real-life clinical practice. Therefore, the aims of this study were:
- To provide data on use of homeopathy in outpatient care including factors associated with prescribing homeopathy (i.e., medical specialties). Among prescribers, to determine whether there was an intention to induce specific or non-specific/placebo effects and the degree of adherence to classical homeopathic doctrine.
- Among all respondents: to quantify existing beliefs in explanatory models for homeopathy and rate the evidence base of homeopathy’s effectiveness
- Among all respondents: to assess the endorsement of different indications and justifications of homeopathy use, including the political view of whether homeopathy should be reimbursed by statutory health insurance providers.
Materials and methods
Design and participants
A cross-sectional mixed modes survey among all practice-based physicians in the Canton of Zurich from every medical specialisation was performed between November and December 2015. Mixed modes means that addressees were contacted by letter but could choose to return the completed questionnaire either by mail (postpaid envelopes were provided), fax, or using an online survey platform (Surveymonkey®). Eligible physicians were identified using the local physicians’ association’s (Aerztegesellschaft des Kantons Zürich, AGZ) registry. The search was restricted to physicians at least partly working in outpatient care (and excluding physicians solely working in inpatient settings). From this registry, address data were used to send a postal letter containing the paper survey, along with a stamped and addressed envelope and an explanatory letter. The letter contained a link to give access to the online survey platform. Responses received via mail were entered into the online database by study staff members, in order to compile all data within a single spreadsheet. Four weeks after the initial circulation, non-respondents received another invitation. After eight weeks, the survey was closed. As an incentive to encourage participation, a prize draw for a weekend at a local spa (total value CHF 1000) was launched. Participation in the draw was possible without responding to the survey. According to Swiss federal law, surveys among physicians do not require the approval of an ethical committee.
Questionnaire
The questionnaire was self-administered and specifically designed for the study purposes. It included knowledge from previous surveys on homeopathy use by general practitioners in Germany [13]. The questionnaire was German and was composed of 24 items: homeopathy application behaviour (items 1 to 8); observation of and beliefs in efficacy (items 9 and 10); endorsement of indications for homeopathy (item 11); justifications to use homeopathy (item 12); appraisal of evidence (items 13 and 14); patient factors (items 15 and 16), physicians’ demographics and working environment (items 17 to 23); and view on reimbursement of homeopathy by statutory health insurance providers (item 24). 14 items were designed as multiple-choice questions with a set of minimum 2 and maximum 5 answer options. One item was designed as a multiple response item, and 3 items were related to a 5-point Likert scale. The original questionnaire is provided in appendix A
, which is available in a separate file for downloading. It was pilot-tested by 11 physicians representing the target group. Testers completed the questionnaire and marked or noted uncertainties, or any general comments. Improvements were made according to the feedback provided.
Outcomes
Outcomes of the study were:
- − Use of homeopathy among physicians measured by the proportion of participants prescribing homeopathy (subsequently referred to as
- − Prescribers’ intentions to induce specific or non-specific/placebo effects and their level of adherence to homeopathic doctrine (see definitions below)
- − Beliefs of all respondents in explanatory models for homeopathy, their ratings of the evidence base of homeopathy’s effectiveness, and the need for more research
- − All respondents’ endorsement of different indications for homeopathy as first- or second-line treatment, their agreement with different statements justifying use of homeopathy, and their political view of whether homeopathy should be reimbursed by statutory health insurance providers.
Definitions
In the following, specific outcome measures are defined, and a number of homeopathy-specific terms (italics) are used. Detailed explanations of these terms is provided in appendix B.
Prescribers of homeopathy
All participants having prescribed homeopathic remedies or having referred patients to homeopathic treatment by other therapists within the preceding 12 months were classified as prescribers. All others were classified as non-prescribers.
Adherence to homeopathic doctrine
Adherence to homeopathic doctrine was a composite outcome of answers to questions on attitudes to use of treatment, namely consideration of miasm theory, remedy preparation, and remedy selection techniques.
Strong adherence was assumed in physicians who revealed either that they consider miasm theory for their treatments, or that they predominantly use single remedies and choose homeopathic remedies according to the techniques of total consideration, hierarchisation and repertorisation of patient symptoms. Moderate adherence was assumed in physicians either predominantly prescribing complex remedies or selecting remedies according to proven indications but not considering miasm theory. Non-adherence was assumed when neither miasm theory nor the above-mentioned preparations and selection techniques were considered in treatment.
Intentions behind prescriptions
Prescribers’ intentions when prescribing homeopathic treatment were assessed based on beliefs in explanatory models for the effectiveness of homeopathy. Prescribers were asked to rate different proposed models on a 5-point Likert scale (strongly agree to strongly disagree). If participants agreed or strongly agreed with at least one of the following explanatory models for efficacy, they were assumed to intend specific effects from using homeopathic remedies: Law of Similars, water memory, cybernetic model, chaos theory or quantum physics. Intending placebo effects was assumed if participants disagreed or strongly disagreed with the above explanatory models, and if they agreed or strongly agreed with at least one following explanatory models: placebo effect, strengthening the relationship between patient and physician, satisfaction of patient expectations, or transference/counter-transference model. Not intending any effects was assumed if prescribers disagreed or strongly disagreed with all explanatory models. The remaining respondents were those giving least one “undecided” (but no higher) rating to any beliefs in explanation models. Therefore such respondents seem to hold weak beliefs in effects, or at least do not rule them out completely. These respondents we classified as having ambiguous intentions when prescribing homeopathy.
Statistics
We describe categorical variables with counts and proportions, numerical variables with means and standard deviations (SD) or median and interquartile range (IQR) as appropriate. For bivariate group comparisons, we used Fisher’s exact test or chi-squared test for categorical variables, and the Wilcoxon rank sum test or Student’s t-test for numerical variable according to distributions.
Association of categorisation as a prescriber of homeopathy and physician’s medical specialisation were examined using multivariable logistic regression. We adjusted for age, perceived proportion of patients requesting homeopathy, perceived proportion of patients with symptoms that could not be treated satisfactorily (we hypothesise this to be a key factor in explaining physicians’ use of homeopathy), organisation of workplace (single-handed or group practice/emergency department/hospital ward), socioeconomic status of practice postal code regions (average per capita income from public taxation register [14]). We report odds-ratios (OR), 95% confidence intervals (CI), and p values. A p level of <0.05 is considered statistically significant. All statistical analyses were performed with R (version 3.2.0, The R Foundation for Statistical Computing, Vienna, Austria).
Results
Participants
All 4072 physicians from the AGZ database registered as working full- or part-time in outpatient care were addressed and all except 14 letters were deliverable. We received 1531 responses corresponding to a response rate of 37.7%. However, 19 respondents made an opt-out statement on their questionnaire and were excluded from analysis. Thus, the responses of a total of 1512 participants were analysed (see flowchart of in- and exclusions in appendix C). Mean age of the participants was 54.1 (SD 9.25) years and 61.0% of the participants were male. Detailed characteristics of survey participants are given in table 1.
Table 1 Characteristics of survey participants.
|
Variable
|
Category / unit
|
Mean or n
|
(SD) or %
|
| Total n |
Survey participants |
1512 |
100% |
| Age |
Years |
54.1 |
(9.25) |
| Sex |
Male |
923 |
61.0% |
| Principal workplace |
Single-handed practice |
562 |
37.2% |
| Group practice |
717 |
47.4% |
| Outpatient care or ED at hospital |
71 |
4.7% |
| Hospital ward |
138 |
9.1% |
| Missing |
24 |
1.6% |
| Medical board certification |
General or internal medicine |
604 |
39.9% |
| Psychiatry |
231 |
15.3% |
| Paediatrics |
85 |
5.6% |
| Gynaecology |
80 |
5.3% |
| No further medical specialisation |
65 |
4.3% |
| Child and adolescent psychiatry |
55 |
3.6% |
| Ophthalmology |
47 |
3.1% |
| Surgery |
44 |
2.9% |
| Otorhinolaryngology |
38 |
2.5% |
| Dermatology |
34 |
2.2% |
| Anaesthesiology |
31 |
2.1% |
| Neurology |
31 |
2.1% |
| Others |
157 |
10.4% |
| Missing |
10 |
0.7% |
| Work with patients |
Number of patients per week |
66.5 |
(46.6) |
| Hours working with patients per week |
35.2 |
(13.03) |
Use of homeopathy and associations with medical specialties
From all participants, 22.8% (n = 345/1512) were classified as prescribers and 76.7% (n = 1160/1512) were classified as non-prescribers of homeopathy. In 0.5% of cases (n = 7/1512) missing data made such categorisation impossible. The prescriber proportions and percentages of patients treated with homeopathy by medical specialty are presented in table 2. Thirty-seven (2.4%) participants had already acquired a certificate in homeopathy and another 35 (2.3%) were currently acquiring or planning to gain this certificate. Prescribers estimated that they used homeopathy in a median of 5% (IQR 1−20%) of their patients.
Table 2 Homeopathy prescribing among medical specialties.
|
Total respondents
(n)
|
Respondents categorised as prescribers
(n and %)
|
% of patients treated with homeopathy by prescribers (median and IQR)*
|
| No further medical specialisation |
65 |
28 (43.1%) |
12.5% (0–52.5%) |
| Paediatrics |
85 |
33 (38.8%) |
4% (0–11.25%) |
| Anaesthesiology |
31 |
10 (32.3%) |
45% (0–65%) |
| Gynaecology and obstetrics |
81 |
26 (32.1%) |
10% (0–10%) |
| General internal medicine |
603 |
150 (24.9%) |
5% (0–30%) |
| Child and adolescent psychiatry |
55 |
12 (21.8%) |
0% (0–5%) |
| Otorhinolaryngology |
37 |
7 (18.9%) |
1% (0–7.5%) |
| Surgery |
44 |
8 (18.2%) |
25% (0–52.5%) |
| Psychiatry and psychotherapy |
232 |
42 (18.1%) |
5% (0–17.5%) |
| Others |
164 |
22 (13.4%) |
7.5% (0–20%) |
| Neurology |
31 |
3 (9.7%) |
1% (1–1%) |
| Ophthalmology |
47 |
4 (8.5%) |
5% (5–5%) |
| Dermatology and venereology |
34 |
1 (2.9%) |
1% (1–1%) |
When it came to associations of prescribing homeopathy with medical specialties, in the multivariate regression model we found a strong positive association for paediatricians (OR = 3.8, 95% CI = 1.8–8.0) and gynaecologists/obstetricians (OR = 3.1, 95% CI = 1.5–6.7), but the strongest positive association was found for those without further medical specialisation (i.e., a Swiss “Praktischer Arzt”: OR = 3.9, 95%CI = 1.7–9.0). Significant associations were noted with the following control variables: perceived proportion of patients with unsatisfactorily treatable symptoms, perceived proportion of patients requesting homeopathy, respondent sex, organisation of workplace, but not physicians’ age and socio-economic status of practice postal code regions (see table 3 for details).
Table 3 Associations with categorisation as prescriber of homeopathy in multivariate logistic regression model.
|
Odds ratio (95% CI)
|
p-value
|
| No further medical specialisation |
3.9 (1.7–8.96) |
0.001 |
| Paediatrics |
3.8 (1.82–8) |
<0.001 |
| Anaesthesiology |
2.3 (0.78–7.06) |
0.13 |
| Gynaecology and obstetrics |
3.1 (1.47–6.67) |
0.003 |
| General internal medicine |
1.7 (0.93–2.97) |
0.09 |
| Child and adolescent psychiatry |
0.9 (0.36–2.35) |
0.86 |
| Otorhinolaryngology |
1.8 (0.67–5.02) |
0.24 |
| Surgery |
1.5 (0.52–4.47) |
0.45 |
| Psychiatry and psychotherapy |
0.9 (0.46–1.78) |
0.77 |
| Neurology |
<0.1 (NA) |
0.97 |
| Ophthalmology |
0.9 (0.26–2.8) |
0.80 |
| Dermatology and venereology |
0.2 (0.03–1.79) |
0.16 |
| Age (OR per increase in one year) |
1 (0.99–1.02) |
0.54 |
| Female sex (ref = male) |
1.8 (1.32–2.46) |
<0.001 |
| Practice type: single practice (ref = hospital-run clinic) |
2 (1.2–3.47) |
0.009 |
| Practice type: group practice (ref = hospital-run clinic) |
1.6 (0.97–2.7) |
0.07 |
| Average per capita income in practice municipality |
1 (1–1) |
0.41 |
| Perceived % of patients with unsatisfactorily treatable symptoms (OR per increase of 1%*) |
1.02 (1.01–1.02) |
<0.001 |
| Perceived % of patients requesting homeopathic treatment (OR per increase of 1%*) |
1.06 (1.04–1.07) |
<0.001 |
Intentions behind prescriptions and level of adherence to homeopathic doctrine
According to the predefined classification criteria, 50.4% of the prescribing physicians intended specific effects from homeopathy, 21.4% intended non-specific/placebo effects, 16.5% had ambiguous intentions, and 1.2% didn’t intend any effects at all. Incomplete responses prohibited this classification in 10.4% of participants. Applying the criteria for adherence to homeopathic doctrine, we found that 27.2% of the prescribers showed strong adherence to homeopathic doctrine, 54.4% moderate adherence, and 18.4% non-adherence. Detailed results of use of homeopathy are given in table 4.
Table 4 Usage of homeopathy among prescribers.
|
Variable
|
Category/unit
|
Median or n
|
% or IQR
|
| Total n |
Prescribers of homeopathy |
345 |
100% |
| % of patients receiving homeopathy prescriptions |
Median and IQR |
5 |
1–20 |
| Homeopathic remedies sold in practice |
Yes |
139 |
40.3% |
| Self-manufacture of homeopathic remedies |
Yes |
7 |
2.0% |
| Predominant preparation prescribed |
Predominant use of single remedies |
137 |
39.7% |
| Predominant use of complex remedies |
58 |
16.8% |
| No consideration of preparation |
80 |
23.2% |
| Missing |
70 |
20.3% |
| Consideration of concepts to select homeopathic remedies |
Hierarchisation and repertorisation |
73 |
21.2% |
| Proven indications |
137 |
39.7% |
| Not considering established concepts |
64 |
18.6% |
| Missing |
71 |
20.6% |
| Consideration of miasms |
Yes |
65 |
18.8% |
| No |
126 |
36.5% |
| I don't know what miasms are |
112 |
32.5% |
| Missing |
42 |
12.2% |
Beliefs in explanatory models and rating of the evidence available
Prescribers of homeopathy agreed most often with the Law of Similars to explain the efficacy of homeopathy (41.7%). Placebo effects came in second place (35.1%) followed by other interpersonal effects (satisfaction of patient expectations, strengthening of relationship between patient and physician, transference/counter-transference). Quantum physics and water memory were seen as explanatory models by 19% of prescribers. Agreement with each explanatory model is shown in table 5. By contrast, non-prescribers agreed in 0.9−6.7% of cases with explanatory models for specific effects, and in 40.3−72.4% of cases with explanatory models advocating interpersonal or placebo effects. Among prescribers, 22.6% thought the evidence base of homeopathy proved effectiveness, versus 2.6% of the non-prescribers. The need for more research in homeopathy was expressed by 76.0% of the prescribers and 42.4% of the non-prescribers.
Table 5 Agreement with explanatory models for effectiveness of homeopathy.
|
Explanatory model
|
Prescribers agreed or strongly agreed
(n = 345)
|
Non-prescribers agreed or strongly agreed
(n = 1160)
|
| Law of Similars |
41.7% |
6.7% |
| Placebo effect |
35.1% |
72.4% |
| Satisfaction of patients’ expectations |
34.7% |
57.6% |
| Strengthening of relationship between patient and physician |
33.2% |
48.6% |
| Transference/counter-transference model |
24.0% |
40.3% |
| Quantum physics |
19.3% |
2.2% |
| Water memory |
19.0% |
2.2% |
| Cybernetic model |
8.7% |
0.9% |
| Chaos theory |
3.5% |
1.4% |
Endorsement of indications, justification and view on reimbursement
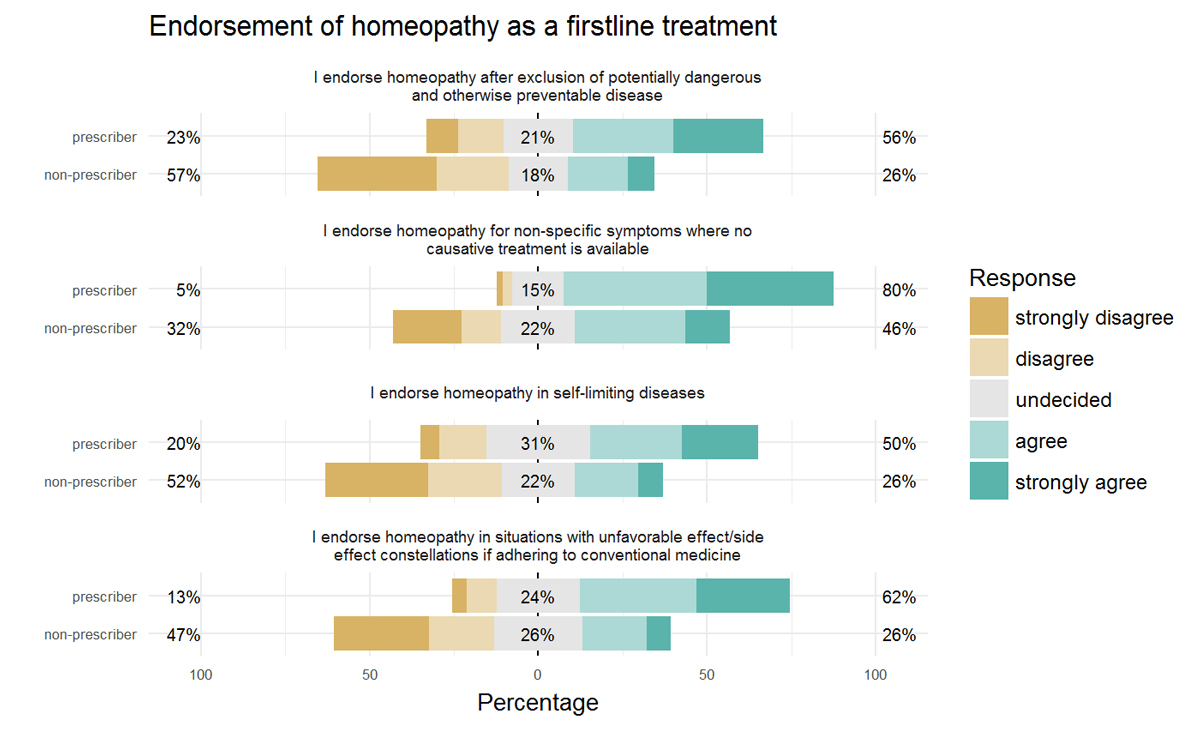
Endorsement of homeopathy as a first-line treatment was greatest for non-specific symptoms where no causative treatment was available (agreement from 53.8% of participants). The least endorsement was seen regarding self-limiting diseases (agreement from 31.4% of participants). Figure 1 shows endorsement of all indications for homeopathy as a first-line treatment stratified by prescribers and non-prescribers.
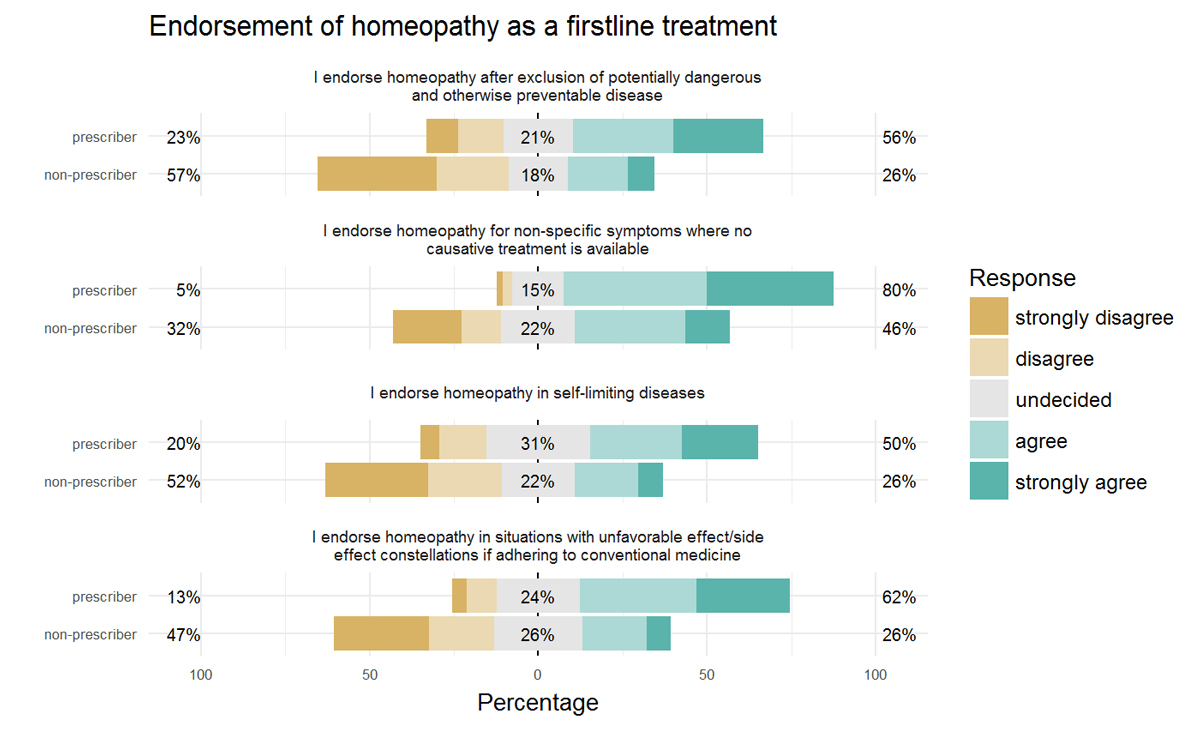
Figure 1 Endorsement of homeopathy as a first-line treatment by prescribers and non-prescribers; bars represent prescribers’ and non-prescribers’ responses to 5-point Likert scale items; colours represent the proportions of individual response categories. The horizontal position of the bars represents the summarised tendency of the responses (left = % disagree, centre = % undecided, right = % agree). Reading an example for the first item of the plot, “Endorsement of homeopathy as a first line therapy after exclusion of potentially dangerous and otherwise preventable diseases”: 23% of prescribers either strongly disagreed or disagreed, 21% remained undecided, 56% agreed or strongly agreed; agreement and strong agreement rates were similar. Non-prescribers’ response proportions are almost precisely inversely distributed.
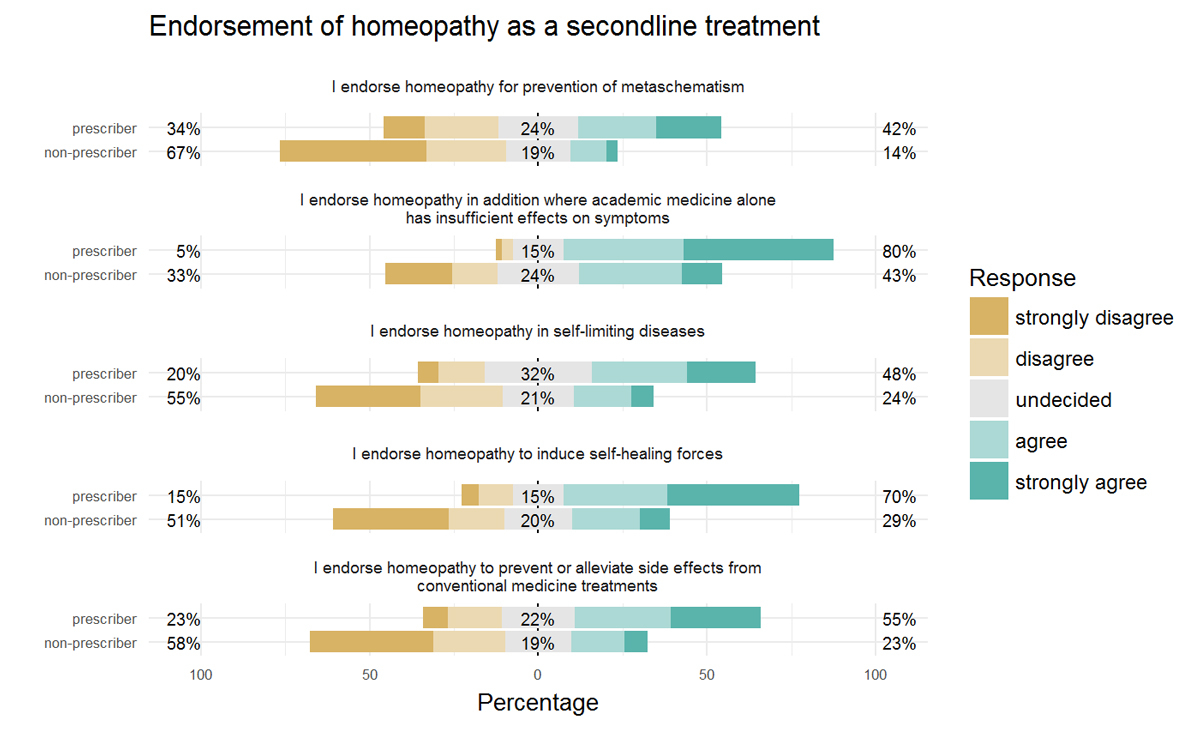
Endorsement of homeopathy as a second-line treatment was greatest in situations where conventional medicine alone had insufficient effects on symptoms (agreement from 51.2% of participants). The least endorsement was seen regarding the prevention of metaschematism (see appendix B) with 20.6% of participants showing agreement. Figure 2 shows endorsement of homeopathy as a second-line treatment, stratified according to prescribers and non-prescribers.
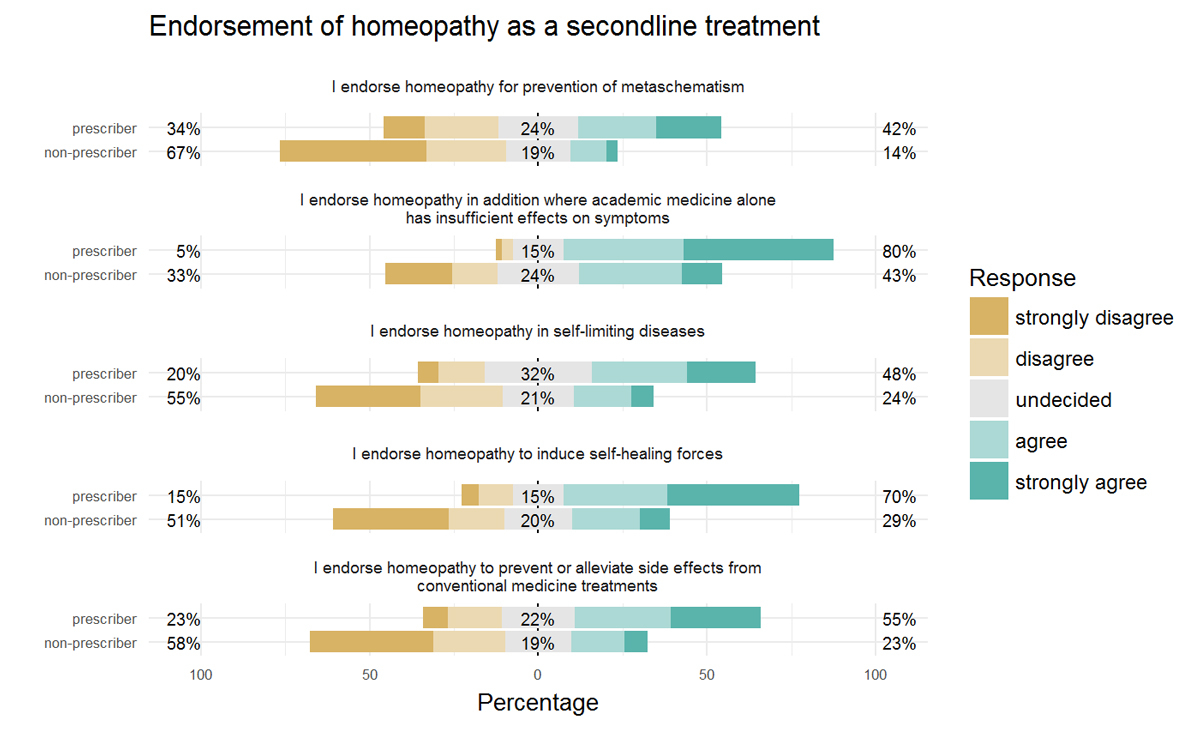
Figure 2 Endorsement of homeopathy as second-line treatment by prescribers and non-prescribers: bars represent prescribers’ and non-prescribers’ responses to 5-point Likert scale items; colours represent the proportions of individual response categories. The horizontal position of the bars represents the summarised tendency of the responses (left = % disagree, centre = % undecided, right = % agree).
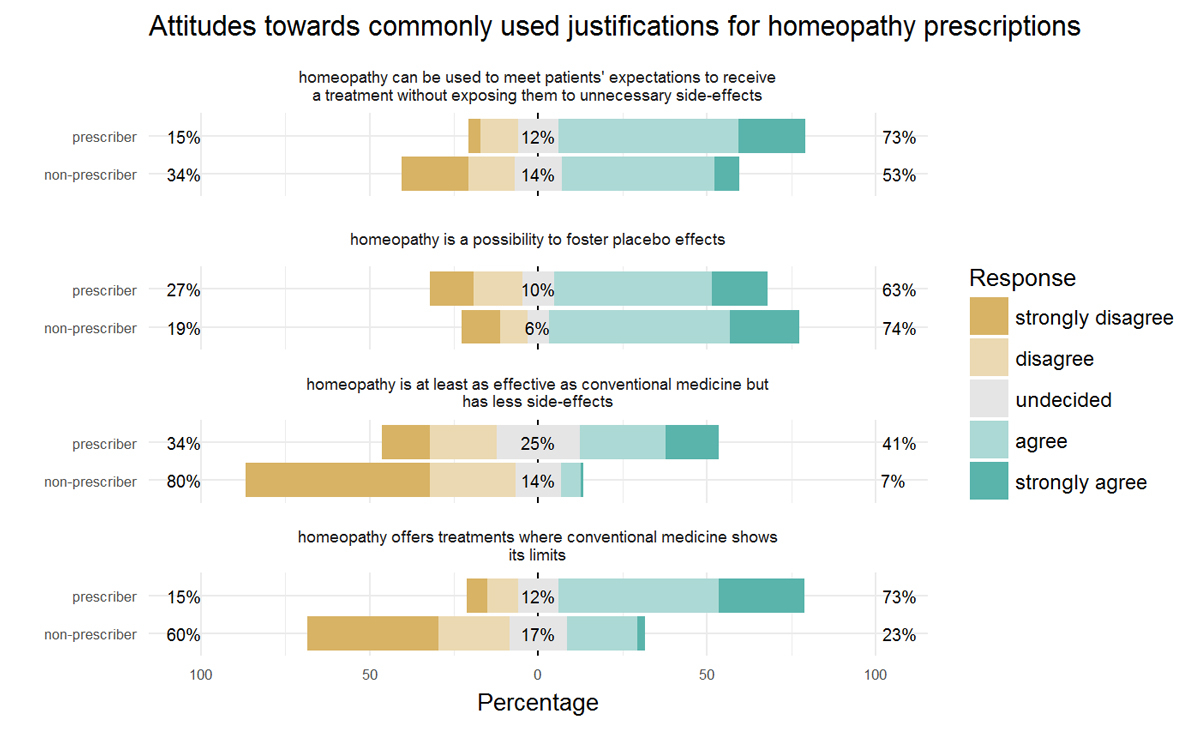
Among commonly used justifications for homeopathy use, the greatest agreement from participants referred to homeopathy’s possible role in fostering placebo effects. Overall, 71.6% of participants agreed with this statement and differences between prescribers and non-prescribers were smallest compared to all other Likert-type items in this chapter. To consider homeopathy to be at least as effective as conventional medicine but with fewer side effects was the least accepted statement, with only 14.6% of participants showing agreement. This item featured the greatest between-group difference of all items in this chapter. Figure 3 visualises attitudes towards commonly used arguments to justify homeopathy use, stratified by prescribers and non-prescribers.
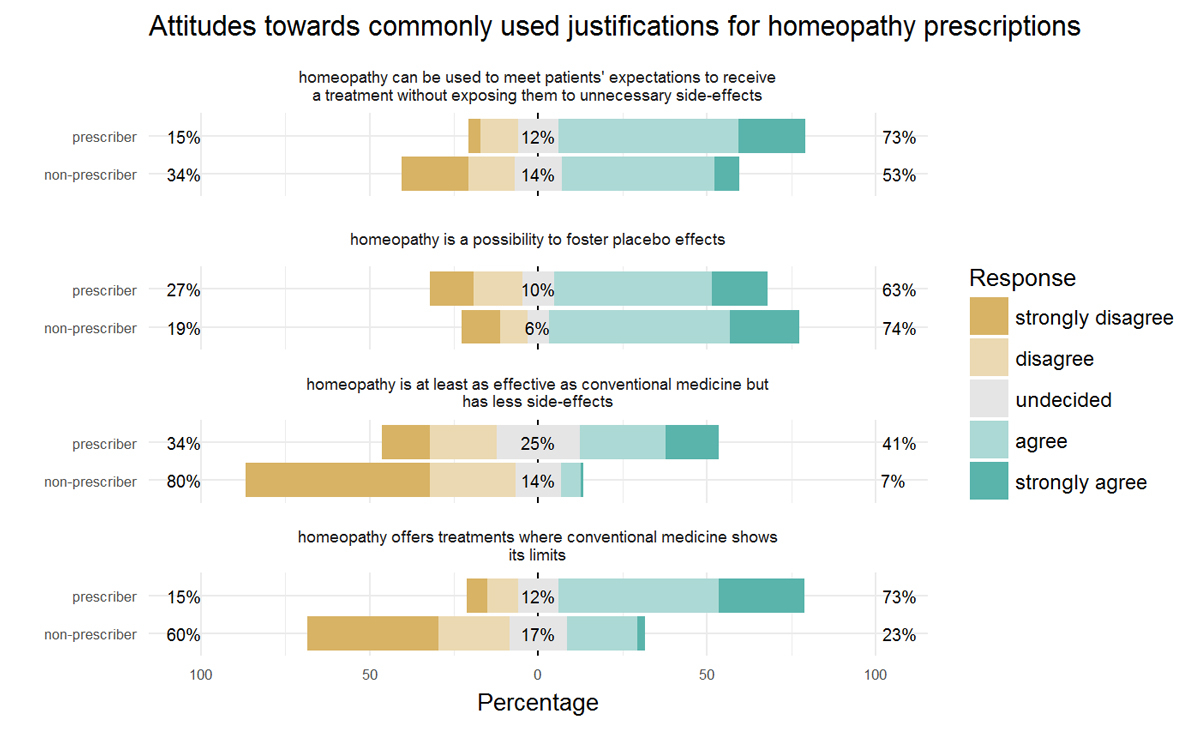
Figure 3 Attitudes towards commonly used justifications for prescriptions of homeopathy; bars represent prescribers’ and non-prescribers’ responses to 5-point Likert scale items; colours represent the proportions of individual response categories. The horizontal position of the bars represents the summarised tendency of the responses (left = % disagree, centre = % undecided, right = % agree).
A prolongation of the legal decree assuring reimbursement of homeopathic remedies by statutory health insurance was welcomed by 29.3%, and rejected by 61.0% of the participants. 9.6% were undecided.
Discussion
This cross-sectional survey among practice-based physicians aimed to explore homeopathy’s use across medical specialties and assess physicians’ views and attitudes towards homeopathy. The results show that one out five physicians prescribed homeopathic treatment at least once a year and that prescribing homeopathy was associated with specific medical certifications. Half of the prescribing physicians clearly intended specific effects with homeopathy and a fifth clearly intended non-specific/placebo effects only. Over 4000 practice-based physicians in the Canton of Zurich (full census) were approached and the response rate was 37.7%. Gender distribution and medical specialisation of participants corresponded to the expected proportions based on the corresponding census data of Swiss ambulatory care [15, 16]. The proportion of practising homeopaths identified among physicians in the outpatient sector was in the middle of the expected range from other countries’ reports [2–4, 8, 17, 18].
Hahnemann’s Law of Similars continues to be the predominantly believed explanatory model for homeopathy, with almost half of the prescribing physicians supporting this thesis. In contrast, all explanatory models containing non-specific effects (such as placebo) ranked next on the scale, and are believed by a quarter to a third of the prescribers. Other more recent explanatory models for specific effects (such as water memory) gained the least credibility among prescribers. The majority of prescribers were also clearly detached from homeopathic doctrine with only one in four still distinguishing different qualities of preparations and applying traditional techniques for remedy selection, or considering the theory of miasms. The majority of prescribers made more liberal use of homeopathy, and either partially or completely disregarded the doctrine. Ultimately and most astoundingly, only one in five prescribers rated evidence that proves the effectiveness of homeopathy. In summary, these findings allow for the interpretation that a majority of prescribing physicians use homeopathy liberally, have heterogeneous confidence in the underlying theories explaining homeopathy, and acknowledge that there is no evidence for specific effects of homeopathy. An important proportion of the prescribing physicians may therefore be vulnerable to the criticism of using homeopathy to practice placebo medicine. This, however, seems to apply only to about one in five prescribing physicians openly intending non-specific effects only. One out of six prescribers seems to be ambiguous (i.e., sceptical about believing in any effects of homeopathy but apparently not ruling them out completely). These physicians therefore have no exclusive or straightforward intention of achieving only non-specific effects, and possibly retain a low level of confidence that specific effects might still occur.
In this study, we found that the perceived prevalence of patients with symptoms that could not be treated satisfactorily with conventional medicine was indeed strongly associated with prescribing homeopathy. Three out of four prescribers thought homeopathy to offer treatment options when conventional medicine showed limits. Such limits are manifold and include non-existing treatments, or treatments just unavailable or unknown to the respective physician, or the potential of adverse reactions and harm. This points to a possible explanation regarding our finding of specific medical specialties being more inclined to homeopathy. Gynaecologists/obstetricians and paediatricians treat pregnant women and children who are both especially vulnerable to adverse effects from conventional treatments. Naturally, these physicians more often need to withhold effective but potentially harmful treatments because the risks outweigh the potential benefits. Prescribing homeopathy instead might be a delicate but understandable path in such situations, allowing a treatment for demanding patients (ut aliquid fiat) but without exposing them to potential harm (primum nihil nocere). This hypothesis is supported by three out of four prescribing physicians who use homeopathy as an opportunity to meet patients’ expectations without exposing them to unnecessary side-effects. Working in a single-doctor practice and responding to patients’ requests for homeopathy were also associated with prescribing homeopathy, which suggests that social phenomena are also associated with homeopathy prescriptions. This might also hold true for the association between prescribing homeopathy and the female sex, a finding in line with previous observations [19–21]. Altogether however, these associations are still poorly understood and hypotheses need to be formulated and tested in dedicated studies before firm conclusions can be drawn.
Interestingly, most non-prescribers did not reject homeopathy outright, but acknowledged placebo- and other interpersonal effects inherent to homeopathic treatments. Many non-prescribers even endorsed use of homeopathy in the case of certain indications, particularly in situations where the possibilities of conventional medicine were exhausted or did not exist. These findings possibly reflect a certain openness of most physicians to accept homeopathy as a placebo intervention, an attitude that two thirds of prescribers and three quarters of the non-prescribers directly agreed upon in our survey. This, however, also points to the need for specific and practicable ethical guidance, which will assist physicians who risk being perceived as deceitful by their patients.
Certain strengths and limitations to this study must be acknowledged. The response rate was 37.7% and even if physicians’ demographics matched the latest census data, we cannot exclude bias from selective answering. Strict opponents of homeopathy in particular may have tended to refuse survey participation. Thus, our survey likely overestimates use and endorsement of homeopathy among physicians. Simultaneously, however, proportions within the group of homeopathy prescribers would suffer less from this possible selective-answering bias. Furthermore, this is a full census and the absolute numbers produced in this survey can still be faithfully used as minimal estimations (e.g., “At least 345 out of 4072 physicians in the canton of Zurich prescribed homeopathy at least once a year.”). Another limitation originates from missing items in specific sections of the questionnaire. The questions that required understanding of homeopathic doctrine were left out by up to 20% of the participants. Here we assume selective omission by physicians unfamiliar with homeopathy, therefore we expect real-life adherence to homeopathic doctrine to be even lower than this study shows. Ultimately, this study summarises a broad spectrum of attitudes and views on homeopathy represented by a broad spectrum of physicians. Thereby this study might contribute to the on-going political debate concerning homeopathy that usually and unproductively tends to be dominated by extreme proponents and extreme adversaries.
We conclude that medical specialties use homeopathy with significantly varying frequency and only half of the prescribers clearly intend specific effects when issuing homeopathic treatments. Hypotheses need to be tested to determine why exactly physicians give credibility to the concept of homeopathy despite training in natural sciences, and why exactly physicians prescribe homeopathy when they don’t even expect specific effects to be achieved. Not only does knowledge about natural sciences pay a role in perceptions of homeopathy, but so too does physicians’ openness towards placebo interventions. Educational efforts should therefore address not only the evidence base of homeopathy, but also ethical dilemmas with placebo interventions.
Appendix A Questionnaire
Appendix B Glossary
Appendix C Flowchart
The appendices are available as a separate file at https://smw/en/article/doi/smw.2017.14505.
Acknowledgments
The physicians’ association of the Canton of Zurich (Aerztegesellschaft des Kantons Zürich, AGZ) provided address data for outpatient care physicians settled in the Canton. The association had influence neither on the collection or analysis of data nor on the decision to publish or the preparation of the manuscript.
References
1
Maddox
J
,
Randi
J
,
Stewart
WW
. “High-dilution” experiments a delusion. Nature. 1988;334(6180):287–91. doi:.https://doi.org/10.1038/334287a0
2
Linde
K
,
Alscher
A
,
Friedrichs
C
,
Wagenpfeil
S
,
Karsch-Völk
M
,
Schneider
A
. Belief in and use of complementary therapies among family physicians, internists and orthopaedists in Germany - cross-sectional survey. Fam Pract. 2015;32(1):62–8.
3
White
AR
,
Resch
KL
,
Ernst
E
. Complementary medicine: use and attitudes among GPs. Fam Pract. 1997;14(4):302–6. doi:.https://doi.org/10.1093/fampra/14.4.302
4
von Ammon
K
,
Frei-Erb
M
,
Cardini
F
,
Daig
U
,
Dragan
S
,
Hegyi
G
, et al.
Complementary and alternative medicine provision in Europe--first results approaching reality in an unclear field of practices. Forsch Komplement Med. 2012;19(s2, Suppl 2):37–43. doi:.https://doi.org/10.1159/000343129
5
Clarke
TC
,
Black
LI
,
Stussman
BJ
,
Barnes
PM
,
Nahin
RL
. Trends in the use of complementary health approaches among adults: United States, 2002-2012. Natl Health Stat Rep. 2015;(79):1–16.
6
Jong
MC
,
van de Vijver
L
,
Busch
M
,
Fritsma
J
,
Seldenrijk
R
. Integration of complementary and alternative medicine in primary care: what do patients want?
Patient Educ Couns. 2012;89(3):417–22. doi:.https://doi.org/10.1016/j.pec.2012.08.013
7
Poitevin
B
. Integrating homoeopathy in health systems. Bull World Health Organ. 1999;77(2):160–6.
8
Piolot
M
,
Fagot
JP
,
Rivière
S
,
Fagot-Campagna
A
,
Debeugny
G
,
Couzigou
P
, et al.
Homeopathy in France in 2011-2012 according to reimbursements in the French national health insurance database (SNIIRAM). Fam Pract. 2015;32(4):442–8.
9
Brien
S
,
Lachance
L
,
Prescott
P
,
McDermott
C
,
Lewith
G
. Homeopathy has clinical benefits in rheumatoid arthritis patients that are attributable to the consultation process but not the homeopathic remedy: a randomized controlled clinical trial. Rheumatology (Oxford). 2011;50(6):1070–82. doi:.https://doi.org/10.1093/rheumatology/keq234
10
Busato
A
,
Künzi
B
. Differences in the quality of interpersonal care in complementary and conventional medicine. BMC Complement Altern Med. 2010;10(1):63. doi:.https://doi.org/10.1186/1472-6882-10-63
11
Fent
R
,
Rosemann
T
,
Fässler
M
,
Senn
O
,
Huber
CA
. The use of pure and impure placebo interventions in primary care - a qualitative approach. BMC Fam Pract. 2011;12(1):11. doi:.https://doi.org/10.1186/1471-2296-12-11
12
Hull
SC
,
Colloca
L
,
Avins
A
,
Gordon
NP
,
Somkin
CP
,
Kaptchuk
TJ
, et al.
Patients’ attitudes about the use of placebo treatments: telephone survey. BMJ. 2013;347(jul02 1):f3757. doi:.https://doi.org/10.1136/bmj.f3757
13
Linde
K
,
Friedrichs
C
,
Alscher
A
,
Blank
WA
,
Schneider
A
,
Fässler
M
, et al.
Use of placebos and nonspecific and complementary treatments by German physicians--rationale and development of a questionnaire for a nationwide survey. Forsch Komplement Med. 2013;20(5):361–7. doi:.https://doi.org/10.1159/000356230
14Kanton Zürich, Direktion der Justiz und des Innern, Statistisches Amt: Gemeindefinanzporträt Kanton Zürich [Average per capita income in municipalities of the Canton of Zurich, data from 2011 to 2014, Download 06 April 2016]. http://www.statistik.zh.ch/internet/justiz_inneres/statistik/de/daten/finanzportraet.html; Accessed 23 May 2016.
15Interactive query tool based on the full census of Swiss physicians: Statistics of the Canton Zurich [Interaktives Abfragetool zur FMH-Ärztestatistik: Statistik des Kantons Zürich]. http://aerztestatistik.myfmh2.fmh.ch/; Accessed 19 May 2016.
16
Hostettler
S
,
Kraft
E
. FMH-Ärztestatistik 2015: Zuwanderung grundlegend für Versorgungssystem. SÄZ. 2016;97(12–13):448–53.
17
Wardle
J
,
Adams
J
,
Sibbritt
D
. Homeopathy in rural Australian primary health care: a survey of general practitioner referral and practice in rural and regional New South Wales, Australia. Homeopathy. 2013;102(3):199–206. doi:.https://doi.org/10.1016/j.homp.2013.03.002
18
Astin
JA
,
Marie
A
,
Pelletier
KR
,
Hansen
E
,
Haskell
WL
. A review of the incorporation of complementary and alternative medicine by mainstream physicians. Arch Intern Med. 1998;158(21):2303–10. doi:.https://doi.org/10.1001/archinte.158.21.2303
19
Verhoef
MJ
,
Sutherland
LR
. Alternative medicine and general practitioners. Opinions and behaviour. Can Fam Physician. 1995;41:1005–11.
20
Salomonsen
LJ
,
Fønnebø
V
,
Norheim
AJ
,
Pederson
EJ
. Attitudes about acupuncture and homeopathy among doctors in research positions: a survey. J Altern Complement Med. 2005;11(2):229–31. doi:.https://doi.org/10.1089/acm.2005.11.229
21
von Studnitz
FS
,
Eulenburg
C
,
Mueck
AO
,
Buhling
KJ
. The value of complementary and alternative medicine in the treatment of climacteric symptoms: results of a survey among German gynecologists. Complement Ther Med. 2013;21(5):492–5. doi:.https://doi.org/10.1016/j.ctim.2013.07.005