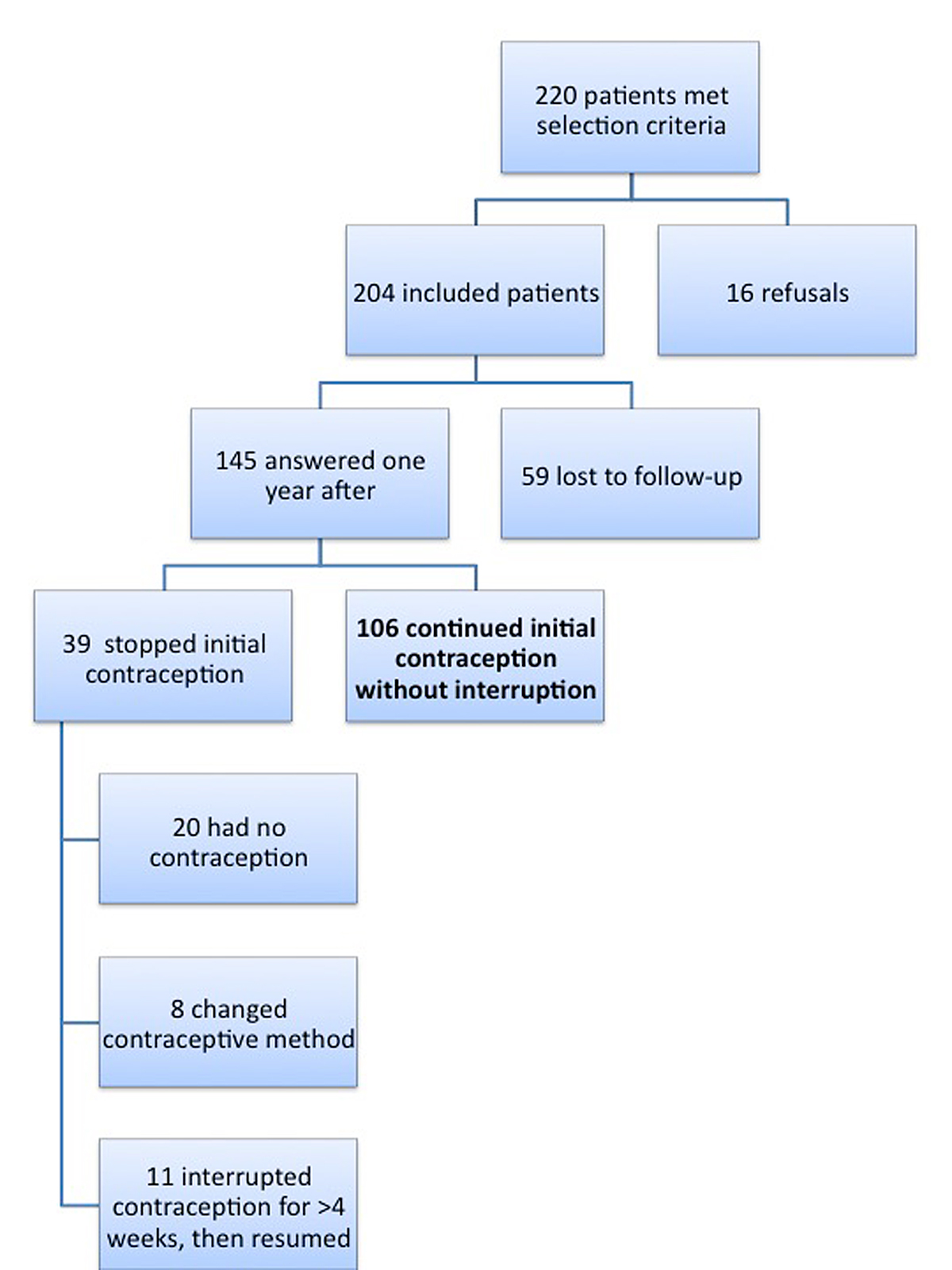
Figure 1 Distribution of patients from recruitment to results.
DOI: https://doi.org/10.4414/smw.2017.14504
long-acting reversible contraception
combined oral contraception
progesterone-only pill
depot medroxyprogesterone acetate
intrauterine device
Adolescence is a challenging step in life: teenagers face anatomical and hormonal changes, alongside developing their independence. Difficulty in self-projection into the long-term future, as well as the need to break rules and take risks, are part of this transition age. With the development of a romantic and sexual life, contraception is needed despite possible difficulties with adherence [1, 2]. A large panel of contraceptive methods can now be suggested to teenagers: combined oestrogen-progestogen methods (oral pill, vaginal ring or transdermal patch), progestogen-only pills, trimestral injections of progestogen or long-acting reversible contraception (LARC) methods including subdermal progestogen implants and intra-uterine devices (with progestogens or copper). Guaranteeing confidentiality from family or peers is crucial to allowing access to the largest number of patients [3]. A successful doctor-patient relationship participates in creating a trustworthy environment for prescription, thus increasing satisfaction and adherence [3–7]. In Switzerland, the adolescent birth rate is very low at 2.1/1000, as is adolescent abortion rate at 3.4/1000 [8]. Among other factors that can explain these low rates are education at school and easy access to health centres.
The literature shows great variations in continuation rates depending on the studied population (country, parity, age, socioeconomic status, etc.), and the methodology used to measure continuation (number of follow-up visits, free contraception, message reminders, etc.) [1, 9–22]. However, continuation seems to be influenced by the contraceptive method, with decreasing rate from LARC, with a 79.8 to 100% continuation rate 1 year later, to oestrogen-progestogen pills (12–72.7%), and finally to vaginal rings and transdermal patches (0–31%) [1, 9, 10, 15, 20, 21]. Other identified factors known to have a negative impact on contraception continuation are smoking or school dropout [11–14, 17, 23].
Currently there is growing evidence recommending the use of LARC methods by adolescents, including as a first-line method [9, 11, 24–28]. In Switzerland, the proportion of adolescents who choose these contraceptive methods is unknown.
As risks of unintended pregnancy increase with every change of contraceptive method [1], we aimed to measure continuity and factors that influence it. Thus, the primary objective of our study was to determine contraceptive continuation rates among adolescents in Switzerland. Further outcomes were to report the prescribed contraceptive methods and to assess possible predictive factors of discontinuation.
The Cantonal Ethic Committee of Human Research approved our study protocol on 24.01.2013. (Protocol 324/12). The CHUV (Centre Hospitalier Universitaire Vaudois) supported all financial costs; we received no private sponsoring. The recruitment centres did not receive any compensation for their work, nor did patients receive any compensation for their participation.
We conducted a prospective observational cohort study with an exploratory purpose and consecutively recruited adolescent girls consulting in order to start contraception, not necessarily for the first time in their lifetime. Recruitment took place in the University Hospital of Lausanne (adolescent gynaecology unit and a senior consultant’s practice) and in seven sexual health centres, of which one was also located in Lausanne and the other six in small and middle-sized cities in the Canton of Vaud. The study began in March 2013 with the aim of including the convenience sample of 200 patients. Inclusion criteria were: age 12 to 19 years and de novo prescription of a contraceptive method: combined oral contraception (COC), progesterone-only pill (PP), vaginal ring, transdermal patch, depot medroxyprogesterone acetate (DMPA), LARC methods such as an intrauterine device (IUD) or a subdermal etonorgestrel implant]. Exclusion criteria were: (1) methods prescribed for other indications than contraception (such as COC for dysmenorrhoea or hormonal IUD for hypermenorrhoea), (2) contraceptive prescription already in place, (3) suspicion of pregnancy, (4) desire for pregnancy within a year, (5) lack of capacity of discernment, and (6) poor comprehension of the French language.
Each participant signed a written informed consent form and allowed the investigator to contact her 1 year later. It is important to emphasise that in Switzerland adolescents can receive contraception without informing their legal representative; to respect this practical reality, informed consent from the legal representative was not necessary for participation in the study.
We wanted to measure the adherence to the method initially prescribed because our clinical experience shows that risks of pregnancy increase not only in the case of contraception interruption but also upon contraceptive method change. If an adolescent changes method, it is usually a sign that the first prescribed contraception method was not optimal from her point of view. That is why “discontinuers” were defined as patients who either did not use contraception anymore 1 year later, who had interrupted their contraception for more than 4 weeks, or who had changed contraceptive method.
Upon inclusion, we recorded the following data: age, nationality, gravidity and parity, prescribed contraceptive method, number of sexual partners over the last month, smoking, occupation, and place of residence (living alone, at parents’ home, at partner’s home, or community centre). We also recorded whether the legal representative knew about the contraception or not, in order to measure the impact of confidentiality on compliance. These data were also recorded for patients who refused to participate, in order to determine the representativeness of the included subjects compared with those others who matched the selection criteria.
One year later, we conducted a semi-structured interview with each patient by telephone, email or postal mail, depending on their preference. The questionnaire was in French and is provided in appendix 1, available as a separate file for downloading. To increase the reliability of answers, contact was made by the principal investigator, who did not take part in the screening of patients nor in their follow-up. Questions focused on contraception continuation, change of contraceptive method, satisfaction, forgotten pills, noticed side effects, and patients’ opinion regarding efficacy and price of their contraception and discretion of their doctor. As some characteristics could have changed during the year, we also repeated questions about sexual partners, smoking, occupation, place of residence and the legal representative’s knowledge of the contraception. Finally, we asked about pregnancies during the time of the study. In order to measure their satisfaction, patients could choose between “very unsatisfied”, “unsatisfied”, “neither satisfied nor unsatisfied”, “satisfied” or “very satisfied”.
To avoid bias regarding adherence, we chose to contact patients for one single interview instead of several times, which could have artificially increased adherence. We nevertheless asked if they had had follow-up visits in the meantime.
Associations between contraception continuation and its potential predictive factors were assessed separately at the time of inclusion into the study and 1 year later. Except for age, all of the assessed predictive factors were categorical variables. Therefore, their associations with contraception continuation (continuers versus discontinuers) were estimated and tested by means of contingency tables and Fisher’s exact tests. Age was compared between the continuation and the discontinuation groups by means of a Student t-test, after visual checking that the distribution was Gaussian. The statistical package Stata, version 13 (StataCorp LP, College Station, Texas) was used for the calculations.
Two hundred and four patients were included up to June 2014. In figure 1 we detail the distribution of patients from the time of selection until the questionnaire 1 year later. Only 7.3% of the patients who met the selection criteria refused to participate in the study. These were more likely to declare having no sexual relations at the time of recruitment than those who accepted the study (60 vs 17.4%, p = 0.001 with Fisher’s exact test). This was the only significant difference between the two groups.
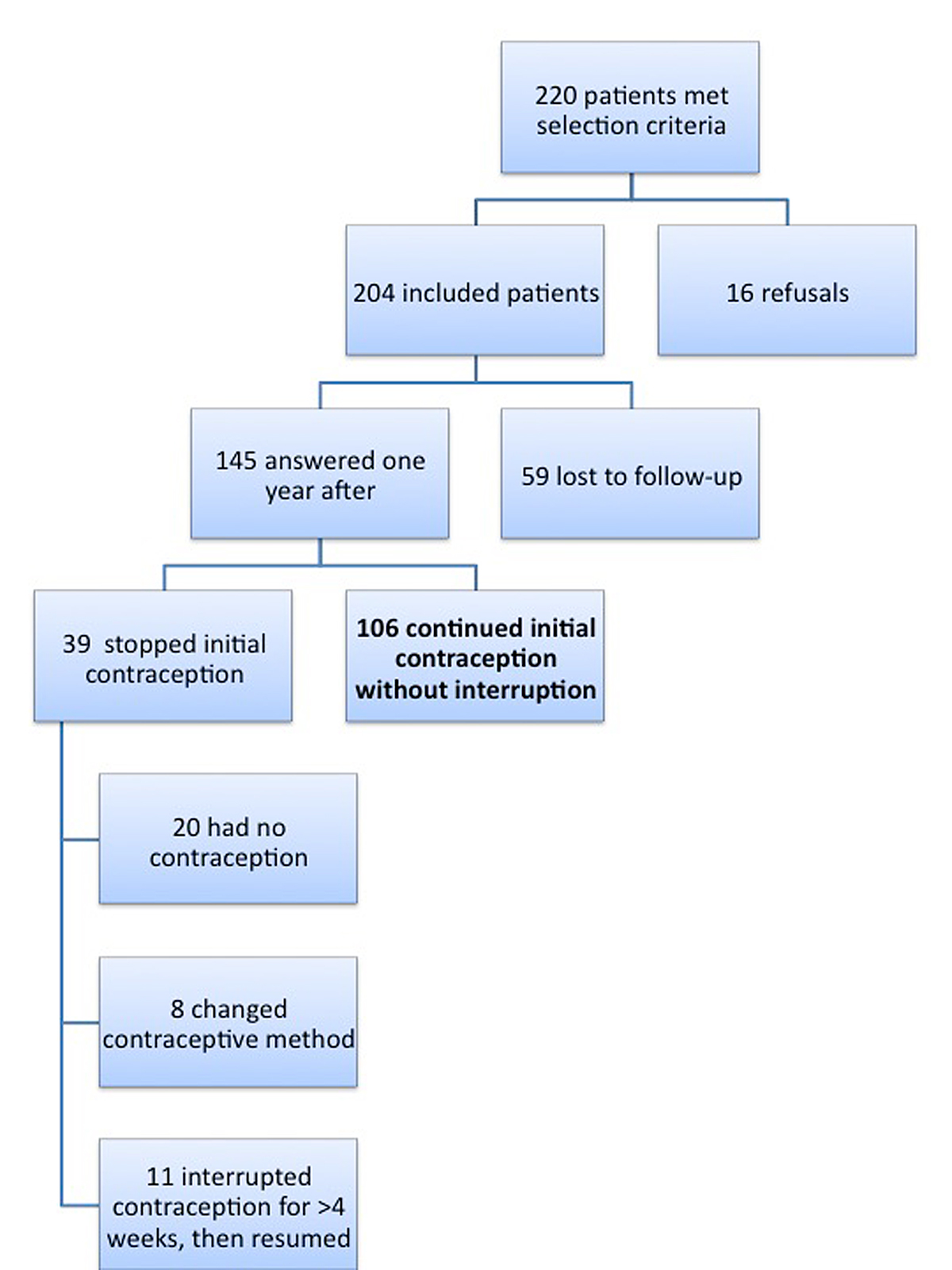
Figure 1 Distribution of patients from recruitment to results.
The characteristics of the included patients are detailed in table 1. In figure 2 we show the number of adolescent girls per age group. Most COCs were second generation pills. Smokers did not give preference to a method with a lesser thromboembolic risk as they amounted to 42.9% of the group using a method without oestrogen.
Table 1 Characteristics of included patients.
| Mean age in years | 17.28 (range 14–19) |
| Nationality | |
| Swiss | 138 (69.35%) |
| Portuguese | 19 (9.55%) |
| Other | 42 (21.10%) |
| Unknown | 5 |
| Gravidity | |
| 0 | 203 (100%) |
| Unknown | 1 |
| Number of sexual partners | |
| None | 35 (17.41%) |
| One | 159 (79.1%) |
| More than one | 7 (3.48%) |
| Unknown | 3 |
| Smoking | |
| Yes | 77 (38.31%) |
| No | 124 (61.69%) |
| Unknown | 3 |
| Activity | |
| Studies (school, college, university) | 124 (61.39%) |
| Apprenticeship | 59 (29.21%) |
| Employee | 7 (3.47%) |
| Without | 12 (5.94%) |
| Unknown | 2 |
| Place of residence | |
| Parents’ home | 189 (93.56%) |
| Partner’s home | 1 (0.5%) |
| Alone | 4 (1.98%) |
| Community centre | 6 (2.97%) |
| Other | 2 (0.99%) |
| Unknown | 2 |
| Legal representative informed about contraception | |
| Yes | 129 (65.15%) |
| No | 69 (34.35%) |
| Unknown | 6 |
| Contraceptive method | |
| COC | 175 (85.78%) |
| PP | 9 (4.41%) |
| Ring | 5 (2.45%) |
| Patch | 2 (0.98%) |
| DMPA | 7 (3.43%) |
| Implant | 2 (0.98%) |
| IUD | 4 (1.96%) |
COC = combined oral contraception; PP = progesterone-only pill; Ring = vaginal ring; patch = transdermal patch; DMPA = depot medroxyprogesterone acetate; implant = subdermal etonorgestrel implant; IUD = intra-uterine device Unknown factors were not included in the percentages.

Figure 2 Number of adolescent girls per age group.
One year later, 71% of included patients answered the questionnaire. The characteristics of the subjects lost to follow-up are listed in table 2. The only significant difference was nationality; Swiss nationals answered more frequently than non-Swiss after 1 year ater (75.2 vs 55.2% in the lost to follow-up group, p value = 0.007).
Table 2 Characteristics of patients lost to follow-up.
| Mean age (years) | 17.35 |
| Nationality | |
| Swiss | 32 (55.17%) |
| Other | 26 (44.83%) |
| Unknown | 1 |
| Gravidity | |
| 0 | 59 (100%) |
| Number of sexual partners | |
| None | 8 (13.56%) |
| One | 49 (83.05%) |
| More than one | 2 (3.39%) |
| Smoking | |
| Yes | 23 (40.35%) |
| No | 34 (59.65%) |
| Unknown | 2 |
| Activity | |
| Studies (school, college, university) | 35 (59.32%) |
| Apprenticeship | 16(27.12%) |
| Employee | 2 (3.39%) |
| Without | 6 (10.17%) |
| Place of residence | |
| Parents’ home | 54 (91.53%) |
| Partner’s home | 0 |
| Alone | 1 (1.69%) |
| Community centre | 2 (3.39%) |
| Other | 2 (3.39%) |
| Legal representative informed about contraception | |
| Yes | 38 (66.67%) |
| No | 19 (33.33%) |
| Unknown | 2 |
| Contraceptive method | |
| COC | 50 (84.75%) |
| PP | 4 (6.78%) |
| Ring | 1 (1.69%) |
| Patch | 1 (1.69%) |
| DMPA | 3 (5.08%) |
| Implant | 0 |
| IUD | 0 |
COC = combined oral contraception; PP = progesterone-only pill; Ring = vaginal ring; patch = transdermal patch; DMPA = depot medroxyprogesterone acetate; implant = subdermal etonorgestrel implant; IUD = intra-uterine device Unknown factors were not included in the percentages.
The 1-year continuation rate was 73.1%. In table 3 we report the characteristics of contraception continuers and discontinuers for each recorded variable. The factors that differed significantly between discontinuers and continuers were: the contraceptive method prescribed at inclusion, and sexual activity and place of residence 1 year later. Age, nationality, smoking, occupation, sexual relations at the time of inclusion, place of residence upon inclusion, and the legal representative’s knowing about the contraception were not significantly different between these two groups.
Table 3 Comparison of continuers with discontinuers for each factor.
|
Total patients who answered
n = 145 |
Continuers
n = 106 |
Discontinuers
n = 39 |
p-value | |
|---|---|---|---|---|
| At inclusion | ||||
| Mean age (years) | 17.27 | 17.36 | 17.03 | 0.215 |
| Nationality | 0.277 | |||
| Swiss | 106 (75.18%) | 80 (77.67%) | 26 (68.42%) | |
| Non-Swiss | 35 (24.82%) | 23 (23.33%) | 12 (31.58%) | |
| Unknown | 4 | 3 | 1 | |
| Method | 0.011 | |||
| COC | 125 (86.21%) | 94 (88.68%) | 31 (79.49%) | |
| PP | 5 (3.45%) | 3 (2.83%) | 2 (5.13%) | |
| Ring | 4 (2.76%) | 0 | 4 (10.26%) | |
| Patch | 1 (0.69%) | 0 | 1 (2.56%) | |
| DMPA | 4 (2.76%) | 3 (2.83%) | 1 (2.56%) | |
| Implant | 2 (1.28%) | 2 (1.89%) | 0 | |
| IUD | 4 (2.76%) | 4 (3.77%) | 0 | |
| Sexual partners | 0.859 | |||
| None | 27 (19%) | 21 (20.39%) | 6 (15.38%) | |
| One | 110 (77.46%) | 78 (75.73%) | 32 (82.05%) | |
| More than one | 5 (3.52%) | 4 (3.89%) | 1 (2.56%) | |
| Unknown | 3 | 3 | 0 | |
| Activity | 0.573 | |||
| Studies | 89 (62.24%) | 67 (63.81%) | 22 (57.89%) | |
| Apprenticeship | 43 (30.07%) | 31 (29.52%) | 12 (31.58%) | |
| Working | 5 (3.5%) | 4 (3.81%) | 1 (2.63%) | |
| Without | 6 (4.2%) | 3 (2.86%) | 3 (7.89%) | |
| Unknown | 2 | 1 | 1 | |
| Place of residence | 0.416 | |||
| Parents’ home | 135 (94.41%) | 101 (95.28%) | 34 (91.89%) | |
| Partner’s home | 1 (0.7%) | 1 (0.94%) | 0 | |
| Alone | 3 (2.1%) | 1 (0.94%) | 2 (5.41%) | |
| Community centre | 4 (2.8%) | 3 (2.98%) | 1 (2.7%) | |
| Unknown | 2 | 0 | 2 | |
| Smoking | 0.330 | |||
| Yes | 54 (37.50%) | 37 (34.91%) | 17 (44.74%) | |
| No | 90 (62.50%) | 69 (65.09%) | 21 (55.26%) | |
| Unknown | 1 | 0 | 1 | |
| Legal representative informed | 0.241 | |||
| Yes | 91 (64.54%) | 69 (67.65%) | 22 (56.41%) | |
| No | 50 (35.46%) | 33 (32.35%) | 17 (43.59%) | |
| Unknown | 4 | 4 | 0 | |
| Consultation | 0.265 | |||
| Family planning | 124 (85.52%) | 90 (84.91%) | 34 (87.18%) | |
| Adolescent unit | 10 (6.9%) | 6 (5.66%) | 4 (10.26%) | |
| Private practice | 11 (7.59%) | 10 (9.43%) | 1 (2.56%) | |
| One year after | ||||
| Sexual partners | 0.001 | |||
| None | 37 (25.69%) | 20 (19.05%) | 17 (43.59%) | |
| One | 104 (72.22%) | 84 (80%) | 20 (51.28%) | |
| More than one | 3 (2.08%) | 1 (0.95%) | 2 (5.13%) | |
| Unknown | 1 | 1 | 0 | |
| Activity | 0.940 | |||
| Studies | 74 (51.03%) | 55 (51.89%) | 19 (48.72%) | |
| Apprenticeship | 56 (38.62%) | 40 (37.74%) | 16 (41.03%) | |
| Working | 9 (6.21%) | 7 (6.6%) | 2 (5.13%) | |
| Without | 6 (4.14%) | 4 (3.77%) | 2 (5.13%) | |
| Place of residence | 0.020 | |||
| Parents’ home | 119 (85.00%) | 90 (87.38%) | 29 (78.38%) | |
| Partner’s home | 6 (4.29%) | 6 (5.83%) | 0 | |
| Alone | 6 (4.29%) | 3 (2.91%) | 3 (8.11%) | |
| Community centre | 4 (2.86%) | 3 (2.91%) | 1 (2.7%) | |
| Other | 5 (3.57%) | 1 (0.97%) | 4 (10.81%) | |
| Unknown | 5 | 3 | 2 | |
| Smoking | 0.696 | |||
| Yes | 51 (35.17%) | 36 (33.96%) | 15 (38.46%) | |
| No | 94 (64.83%) | 70 (66.04%) | 24 (61.54%) | |
| Legal representative informed | 0.148 | |||
| Yes | 120 (86.96%) | 93 (89.42%) | 27 (79.41%) | |
| No | 18 (13.04%) | 11 (10.58%) | 7 (20.59%) | |
| Unknown | 7 | 2 | 5 |
COC = combined oral contraception; PP = progesterone-only pill; Ring = vaginal ring; patch = transdermal patch; DMPA = depot medroxyprogesterone acetate; implant = subdermal etonorgestrel implant; IUD = intra-uterine device Unknown factors were not included in the percentages.
Continuation rates according to methods were: 0% for patch and ring, 60% for PP, 75% for DMPA, 75.2% for COC and 100% for LARC methods. Among patients who continued contraception, 93.4% considered themselves satisfied or very satisfied with their contraception. One out of four agreed or totally agreed with the proposition “my contraception is expensive”. Some continuers (16.7%) agreed or totally agreed with the proposition “I often forgot to take my contraception”. One fifth (19.8%) reported adverse side effects, mostly irregular bleeding or mood changes.
Among patients who chose LARC, two had an implant, two a hormonal IUD and two a copper IUD. Four of the six had informed their legal representative. One year after, five of the six felt satisfied or very satisfied with their contraception, none complained about side effects, and none agreed with the proposition “my contraception is expensive”.
In the discontinuer group, various reasons for interruption were reported: 54.3% no longer had sexual relations, 34.3% noticed adverse side effects, 22.9% had changed contraceptive method, 22.9% often forgot to take their contraception, 20% found the contraception too expensive and 8.8% feared inefficacy of the method. The side effects reported in this group were mostly weight gain, acne and headaches.
Fifty-two percent of continuers and 44% of discontinuers reported at least one follow-up visit during the study period.
Two patients reported a pregnancy during the study period. Both pregnancies were unintended and terminated. These patients initially had a COC prescription and changed after the abortion, one choosing a patch, the other an IUD.
The purpose of our study was to learn more about adolescents’ long-term contraception use in Switzerland. Our adolescent contraception continuation rate was 73.1%. This is high compared with large prospective cohort American studies. Raine [1] found a continuation rate of 18.5% and Rosenstock [9] 44% for non-LARC methods. Suhonen [15] had a comparable continuation rate of 79.8% for hormonal IUD and 72.7% for COC in a prospective randomised study of Scandinavian 18- to 25-year-old women. In our study, we defined discontinuers as adolescents who changed contraception or interrupted it transitorily before resuming it. Therefore, if we consider all the adolescents in our study who had contraception in place 1 year later, the percentage is even higher at 86.2%. This high rate is a first measurable explanation of the low level of teenage pregnancies in Switzerland. However, continuation rates varied depending on the initial contraceptive method prescribed. We did not find other predictive factors of discontinuation in our study, but given our relatively small sample of patients, we might have insufficient power to detect some of them.
Another factor we studied was the impact of tobacco. In our study, the answering and continuation rates of smokers were comparable to those of nonsmokers. This contrasts with the observations of Westhoff [17], who also studied adolescents using COC and reported that smoking negatively influenced adherence. A hypothesis to explain this difference is that the percentage of smokers was only 18% in their study versus 38% in ours, and that the smoking population is probably different in the United States, given the more negative image of tobacco in American society.
Regarding the thromboembolic risks of combined oestrogen-progestogens, and despite recent controversies, we found COC to be the most frequently prescribed contraceptive method. Our selection criteria may explain why only a small proportion of the patients in our study used IUD, as they excluded adolescents already on contraception. Moreover, following current recommendations encouraging the use of LARC in adolescents [25], it is likely that the proportion of IUDs prescribed has grown since the start of our study.
Another influencing factor studied was school dropouts, since Maslyanskaya [23] found a link between these and continuation rates. However, in our study, there were very few school dropouts and adolescents in a professional environment did not have a different contraception continuation rate from those enrolled in school or college.
Furthermore, the legal representative’s knowledge of contraceptive use did not influence participation in the study nor contraception continuation. Unfortunately, this variable is rarely reported in other studies.
Even though very few adolescents chose a patch or a ring as contraception, continuation was very low, possibly due to general misunderstanding of how to use these products or their side effects. Similar results have been found previously [1, 9, 10, 15, 20, 21]. More evidence is needed. In the meantime, medical professionals should be careful when prescribing these methods to young patients.
The first reason given by our adolescent subjects to explain interruption of contraception was the end of their romantic and sexual relationship. Financial considerations certainly increase this phenomenon in our country, as women bear the costs of their contraception. This is not an issue when a LARC method has been chosen and paid for at the beginning. A particular feature of adolescents’ sexuality is that it is frequently unpredictable, unplanned and associated with a feeling of invulnerability; that is why it is important that teenagers continue their contraception method despite a short pause in sexual relations. One fifth of discontinuers were, in fact, subjects who changed contraceptive methods, illustrating their dissatisfaction regarding the first prescribed method. This could impair compliance and lead to contraceptive failure, particularly for non-LARC methods.
Our study has some weaknesses. Firstly, we note the small number of patients using methods other than COC, which prevents reliable comparisons between different contraceptive methods or conclusions regarding the other methods. Secondly, LARC methods were rarely prescribed. However, our encouraging results regarding continuation and satisfaction, in accordance with literature data, led our institution to suggest them increasingly to adolescents. Also, many foreign patients were lost to follow-up, which could have led to a bias regarding the statistical impact of nationality on continuation rates. Lastly, another weakness and possible bias is that the continuation rate was self-declared.
The main strength of our study is that it is the first prospective study on this topic in Switzerland. Also, we noted a high answer rate 1 year after prescription. Moreover, the lack of intervention or subvention is consistent with “real-life” conditions, allowing a practical application of our results in effective contraception counselling.
This study underlines adolescents high adherence to contraception in Switzerland, which is not altered by confidentiality. The results also underline the necessity of making teenagers aware of the importance of continuing contraception despite romantic breakups. The significant impact of the type of contraceptive method on continuation rate stresses the importance of individualised counselling for young patients, even in a country where teen pregnancy is low. Expanding the survey to other parts of Switzerland or to other similar countries could bring more powerful results and give practitioners other interesting tools to help individualized counselling.
This research has been presented at the 14th Congress / 2nd Global Conference of the European Society of Contraception and Reproductive Health, 4–7 May 2016, as a poster; and at the Annual Congress of the Société Suisse de Gynécologie-Obstétrique, 22–24 June 2016, as a poster and an oral presentation.
The questionnaire is available as a separate file at https://smw.ch/en/article/doi/smw.2017.14504.
Special thanks to Pr. Pierre-André Michaud for his advice, and Vanessa Kraege for her support. The authors also wish to thank all the young women who took part in the study.
The Centre Hospitalier Universitaire Vaudois (CHUV) supported all financial costs. The Cantonal Ethic Committee of Human Research approved the study protocol on 24.01.2013 (Protocol No. 324/12).
Dr M. Jacot-Guillarmod is a member of the Jaydess® Advisory Board – Bayer Healthcare.
1 Raine TR , Foster-Rosales A , Upadhyay UD , Boyer CB , Brown BA , Sokoloff A , et al. One-year contraceptive continuation and pregnancy in adolescent girls and women initiating hormonal contraceptives. Obstet Gynecol. 2011;117(2 Pt 1):363–71. doi:.https://doi.org/10.1097/AOG.0b013e31820563d3
2 Rahman M , Berenson AB , Herrera SR . Perceived susceptibility to pregnancy and its association with safer sex, contraceptive adherence and subsequent pregnancy among adolescent and young adult women. Contraception. 2013;87(4):437–42. doi:.https://doi.org/10.1016/j.contraception.2012.09.009
3 Bitzer J , Abalos V , Apter D , Martin R , Black A ; Global CARE (Contraception: Access, Resources, Education) Group. Targeting factors for change: contraceptive counselling and care of female adolescents. Eur J Contracept Reprod Health Care. 2016;21(6):417–30. doi:.https://doi.org/10.1080/13625187.2016.1237629
4 Dehlendorf C , Grumbach K , Schmittdiel J , Steinauer J . Shared decision making in contraceptive counselling. Contraception. 2017;95(5):452–5. doi:.https://doi.org/10.1016/j.contraception.2016.12.010
5 Carter WB , Inui TS , Kukull WA , Haigh VH . Outcome-based doctor-patient interaction analysis: II. Identifying effective provider and patient behavior. Med Care. 1982;20(6):550–66. doi:.https://doi.org/10.1097/00005650-198206000-00002
6 Adherence strategies. Improve bedside manner, affect patient adherence. Communication makes a difference. Aids Alert. 2005;20(5):57–9.
7 Merki-Feld GS , Gruber IM . Intention to use a combined contraceptive method and decision after counselling in Switzerland--Swiss data from the European CHOICE study. Eur J Contracept Reprod Health Care. 2012;17(2):119–27. Published online December 27, 2011. doi:.https://doi.org/10.3109/13625187.2011.630114
8Office fédéral de la Statistique [Internet] – Interruptions de grossesse[cited 2016 sept 19] - Available from http://www.bfs.admin.ch/bfs/portal/fr/index/themen/14/02/03/key/03.html and http://www.svss-uspda.ch/fr/suisse/adolescentes.htm
9 Rosenstock JR , Peipert JF , Madden T , Zhao Q , Secura GM . Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012;120(6):1298–305. doi:.https://doi.org/10.1097/AOG.0b013e31827499bd
10 Yoost JL , Hertweck SP , Barnett SN . The effect of an educational approach to pregnancy prevention among high-risk early and late adolescents. J Adolesc Health. 2014;55(2):222–7. Published online March 18, 2014. doi:.https://doi.org/10.1016/j.jadohealth.2014.01.017
11 Alton TM , Brock GN , Yang D , Wilking DA , Hertweck SP , Loveless MB . Retrospective review of intrauterine device in adolescent and young women. J Pediatr Adolesc Gynecol. 2012;25(3):195–200. doi:.https://doi.org/10.1016/j.jpag.2012.01.005
12 Dempsey AR , Johnson SS , Westhoff CL . Predicting oral contraceptive continuation using the transtheoretical model of health behavior change. Perspect Sex Reprod Health. 2011;43(1):23–9. Published online December 22, 2010. doi:.https://doi.org/10.1363/4302311
13 Sucato GS , Land SR , Murray PJ , Cecchini R , Gold MA . Adolescents’ experiences using the contraceptive patch versus pills. J Pediatr Adolesc Gynecol. 2011;24(4):197–203. Published online March 30, 2011. doi:.https://doi.org/10.1016/j.jpag.2011.02.001
14 Lete I , Pérez-Campos E , Correa M , Robledo J , de la Viuda E , Martínez T , et al. Continuation rate of combined hormonal contraception: a prospective multicenter study. J Womens Health (Larchmt). 2012;21(5):490–5. Published online October 26, 2011. doi:.https://doi.org/10.1089/jwh.2011.2967
15 Suhonen S , Haukkamaa M , Jakobsson T , Rauramo I . Clinical performance of a levonorgestrel-releasing intrauterine system and oral contraceptives in young nulliparous women: a comparative study. Contraception. 2004;69(5):407–12. doi:.https://doi.org/10.1016/j.contraception.2003.11.008
16 Berenson AB , Tan A , Hirth JM , Wilkinson GS . Complications and continuation of intrauterine device use among commercially insured teenagers. Obstet Gynecol. 2013;121(5):951–8. doi:.https://doi.org/10.1097/AOG.0b013e31828b63a0
17 Westhoff C , Jones K , Robilotto C , Heartwell S , Edwards S , Zieman M , et al. Smoking and oral contraceptive continuation. Contraception. 2009;79(5):375–8. doi:.https://doi.org/10.1016/j.contraception.2008.12.003
18 Alton TM , Brock GN , Yang D , Wilking DA , Hertweck SP , Loveless MB . Retrospective review of intrauterine device in adolescent and young women. J Pediatr Adolesc Gynecol. 2012;25(3):195–200. doi:.https://doi.org/10.1016/j.jpag.2012.01.005
19 Lim SW , Rieder J , Coupey SM , Bijur PE . Depot medroxyprogesterone acetate use in inner-city, minority adolescents: continuation rates and characteristics of long-term users. Arch Pediatr Adolesc Med. 1999;153(10):1068–72. doi:.https://doi.org/10.1001/archpedi.153.10.1068
20 Berenson AB , Wiemann CM , Rickerr VI , McCombs SL . Contraceptive outcomes among adolescents prescribed Norplant implants versus oral contraceptives after one year of use. Am J Obstet Gynecol. 1997;176(3):586–92. doi:.https://doi.org/10.1016/S0002-9378(97)70552-0
21 Zibners A , Cromer BA , Hayes J . Comparison of continuation rates for hormonal contraception among adolescents. J Pediatr Adolesc Gynecol. 1999;12(2):90–4. doi:.https://doi.org/10.1016/S1083-3188(00)86633-4
22 Castaño PM , Bynum JY , Andrés R , Lara M , Westhoff C . Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstet Gynecol. 2012;119(1):14–20. doi:.https://doi.org/10.1097/AOG.0b013e31823d4167
23 Maslyanskaya S , Coupey S , Chhabra R , Khan UI . Predictors of early discontinuation of effective contraception by teens at High risk of pregnancy. J Pediatr Adolesc Gynecol. 2016;29(3):269–75.
24 Peipert JF , Zhao Q , Allsworth JE , Petrosky E , Madden T , Eisenberg D , et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117(5):1105–13. doi:.https://doi.org/10.1097/AOG.0b013e31821188ad
25 Committee on adolescent health care long acting reversible contraception working group, The American College of Obstetricians and Gynecologists ; Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group, The American College of Obstetricians and Gynecologists. Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2012;120(4):983–8. doi:.https://doi.org/10.1097/AOG.0b013e3182723b7d
26 Diedrich JT , Klein DA , Peipert JF . Long-Acting Reversible Contraception in Adolescents: A systematic Review and Meta-analysis. Am J Obstet Gynecol. Am J Obstet Gynecol. 2017;216(4):364.e1–12.
27 Patseadou M , Michala L . Usage of the levonorgestrel-releasing intrauterine system (LNG-IUS) in adolescence: what is the evidence so far? Arch Gynecol Obstet. 2017;295(3):529–41. doi:.https://doi.org/10.1007/s00404-016-4261-0
28 Usinger KM , Gola SB , Weis M , Smaldone A . Intrauterine Contraception Continuation in Adolescents and Young Women: A Systematic Review. J Pediatr Adolesc Gynecol. 2016;29(6):659–67. Published online July 4, 2016. doi:.https://doi.org/10.1016/j.jpag.2016.06.007
The Centre Hospitalier Universitaire Vaudois (CHUV) supported all financial costs. The Cantonal Ethic Committee of Human Research approved the study protocol on 24.01.2013 (Protocol No. 324/12).
Dr M. Jacot-Guillarmod is a member of the Jaydess® Advisory Board – Bayer Healthcare.