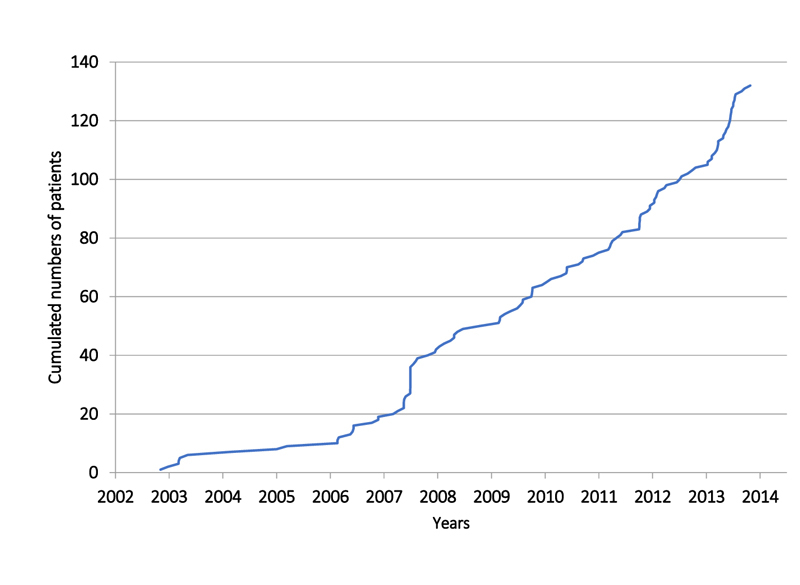
Figure 1 Cumulative number of patients during the length of the study.
DOI: https://doi.org/10.4414/smw.2017.14499
The trafficking and sale of narcotics frequently involves the intra-abdominal transport of large quantities of drugs, usually cocaine or heroin (“body packing”), more rarely methamphetamine or drug mixtures such as cocaine-levamisole and heroin-piracetam, or, when there is a risk of being arrested, the oral ingestion of minor quantities of narcotics dedicated for immediate resale (“body stuffing”) [1]. Body packing, body stuffing and body pushing are three distinct modes of internal drug concealment. Despite the fact that there is currently no study that evaluated these three populations separately, it is believed that the risks and complications are different in the three groups. Body packing refers to the planned ingestion of multiple packages of narcotics; in our setting, they are usually made of latex, averaging a size of 5 × 1.5 cm, with a total weight of sometimes as much as 1 kg [2]. In other settings or countries, condoms, aluminium foil or other materials are used for package creation [3]. The medical risks involved with body packing are mainly linked to intestinal obstruction (or perforation), pyloric or intestinal. More rarely, at least with “professionally” produced packages, they may rupture, leading to the risk of immediate death of the body packer once the large quantity of cocaine has been absorbed into the bloodstream. Rupture is nevertheless rare as these packets are usually made “professionally” to resist intestinal transit, owing to the costs of the merchandise contained [4–6].
Body stuffing refers to the oral ingestion of small quantities of narcotics known as “boulettes” in French, usually in an emergency, by local street dealers, when faced with potential police arrest. The quantities of narcotics within these small balls are usually less than or equal to 1 g. Usually, this type of packaging simply consists of multiple layers of cellophane, and thus is considered to have poor resistance to intestinal transit and is more prone to rupture or to leak. The rupture or leakage of narcotics from these packages leads to an acute intoxication, with the appearance of a sympathomimetic toxidrome in the case of cocaine or opioid toxidrome in the case of heroin.
Finally, the insertion of small reservoirs containing narcotics into body cavities (think “Kinder Surprise”), known as body pushing, is usually done by street dealers as a means to stock narcotics for later resale.
Police and judicial authorities regularly ask medical or medico-legal professionals in areas near borders (airports in particular) to assist with identifying potential body packers or body stuffers. If this is confirmed, they are often requested to monitor and/or treat in the case of acute intoxication. Referral to these departments for diagnostic purposes (in the case of body packers) is usually from local police or border patrol. Aside from the history of the presenting complaint, the physical examination (other than digital rectal/vaginal examination) is often normal in the absence of an acute intoxication or intestinal obstruction.
A review of the literature regarding the management of body packers suggested a series of diagnostic procedures [3, 7–12], including, but not limited to, abdominal X-ray [13], abdominal ultrasound [14], magnetic resonance imaging (MRI) [12] and/or abdominal computed tomography (CT) to confirm the diagnosis [15, 16]. As a result of its far better sensitivity, abdominal CT is preferred to abdominal X-ray and ultrasound [6, 15–17]. Owing to poor sensitivity, urinary screening for narcotics, once considered useful [2, 18], has now been abandoned. Once the presence of packages in the intestinal tract has been confirmed, the management of these patients varies considerably between countries. In certain nations, such as the United States of America, these patients are observed in a prison and are only admitted to the hospital in the event of intoxication or intestinal obstruction [9], whereas in Europe, these cases are usually referred to hospitals until complete expulsion of all narcotics [8, 19, 20].
The management of body stuffers is, on the other hand, much less documented in current literature, and recommendations are rare. Because of the reduced size of the ingested packages, diagnosis requires an abdominal CT, abdominal X-ray being much less sensitive at 50% [4, 21]. Owing to the higher risk of rupture or leakage, initial urinary screening has been suggested by some [18]; others have proposed prophylactic use of activated charcoal [22].
This study aimed to describe the characteristics of body packing and body stuffing cases in our institution, as well as identify complications and medical management of such patients, over the course of 12 years. By combining our experience with a review of the literature, we will then suggest a rational protocol/strategy for the management of these patients.
The Emergency Department of the University Hospital of Lausanne (Centre Hospitalier Universitaire Vaudois – CHUV) admits an average of 40 000 patients every year. It serves as a referral centre for the cantonal police, border agents and prison services for the canton of Vaud (population 700 000) in the case of a medical or surgical problem with a suspect or prisoner. In this regard, any person suspected of trafficking or dealing narcotics (and who may be potentially carrying narcotics packages) who is arrested by the police or border patrol is brought to our emergency department for confirmatory imaging and patient management. Swiss Law authorises the judicial authorities to order a CT scan for patients suspected of the above-mentioned crimes, as a means of confirmation. If the patient (suspect) refuses, the management is then delegated to the judicial authorities and the patient is discharged.
Our emergency department and the department of diagnostic imaging have developed a standardised diagnostic procedure for these patients, involving a standardised CT scan imaging process [15]. Once the presence of drug packages within the digestive system has been confirmed, a standardised management procedure includes continuous surveillance until elimination of the full count of narcotic packs [15]. The patient is observed within our emergency department by judicial order until the complete evacuation of drug packages.
Every patient admitted to the Emergency Department of the CHUV from 1 September 2002 to 31 December 2014 for suspected body stuffing or body packing necessitating a diagnostic evaluation or clinical observation, was included for retrospective analysis. These patients were observed within our department until complete evacuation of intra-abdominal narcotic packets, or until passage of at least three stools free from drug packages (if the number of evacuated packets was less than the count on CT).
This study aimed to review sociodemographic and medical parameters (vital signs, symptoms and clinical signs, laboratory results, treatment and complications) of all patients, with a review of the length of observation and orientation following medical discharge, based on the analysis of the administrative and medical records of each patient. Each CT scan was reviewed in order to classify the patients into body packers (packages longer than 2.5 cm), body stuffers (spherical packets <2.5 cm), or an indeterminate/mixed category.
The analysis focused on the description of the above described characteristics, with a special focus on the length of stay in relation to the medical characteristics and the nature, number and position of ingested foreign bodies. The distribution of these results is expressed in terms of mean, median and range, and the different subgroups were analysed using the nonparametric Wilcoxon test (non-normal distribution).
The study was submitted to and accepted by the Ethics Committee of the Canton of Vaud (CER No 324/14).
From 1 September2002 to 31 December 2014, 148 patients were admitted to the Emergency Department of the CHUV after proven diagnosis of body stuffing, body pushing or body packing by use of abdominal CT without contrast, upon order of the police or judicial authorities. All these patients underwent the examination as ordered by the Prosecutor, police or judicial authorities because of suspected narcotics dealing or trafficking. In addition to these 148 patients, one patient refused the CT scan but admitted having ingested three drug packages; this patient was observed in our hospital until evacuation of the packages.
Of the 149 patients, 16 body pushers were excluded when narcotic packages were visualised within the rectum or the vagina, and thus were rapidly expelled. One additional patient was excluded because of prehospital death from bronchoaspiration of one packet following his arrest (asphyxia); his body was nonetheless brought to our emergency department.
Table 1 describes the sociodemographic characteristics of the remaining132 patients and characteristics of the narcotics. Ninety-three per cent of patients were male and 83% from the African continent. Among the 132 patients, 36 (27%) were classified as body packers, 83 (63%) as body stuffers and 13 (10%) as indeterminate/mixed (because of difficulty in interpreting size or mix of sizes on CT).
Table 1 Sociodemographic characteristics of patients (n = 132) and characteristics of the ingested substances.
| Age (years), mean / median / range | 25.9 / 24.0 / 18–61 |
| Gender, n (%) | |
| Male | 123 (93%) |
| Female | 9 (7%) |
| Country of origin, n (%) | |
| African | 109 (83%) |
| European | 14 (11%) |
| Dominican Republic | 1 (1%) |
| Switzerland | 1 (1%) |
| Unknown | 7 (5%) |
| Number of drug packages, mean / median / range | |
| Total (n = 132) | 16 / 10 / 1–100 |
| Body packers (n = 36) | 34 / 20 / 1–100 |
| Body stuffers (n = 83) | 9 / 8 / 1–29 |
| Indeterminate/mix (n = 13) | 14 / 8 / 2–70 |
| Anatomical location of drug packages on CT images, n (%) | |
| Mouth-oesophagus-stomach | 54 (41%) |
| Small intestine-colon-rectum | 78 (59%) |
| Substances ingested (according to the patient)*, n (%)] | |
| Cocaine | 79 (60%) |
| Methamphetamine | 1 (1%) |
| Heroin | 1 (1%) |
| Not identified | 52 (39%) |
* The total is 133, as one patient was carrying both cocaine and methamphetamine.
During the 12-year study period, a statistically significant increase in the number of patients per year was noted (p <0.01) (fig. 1).
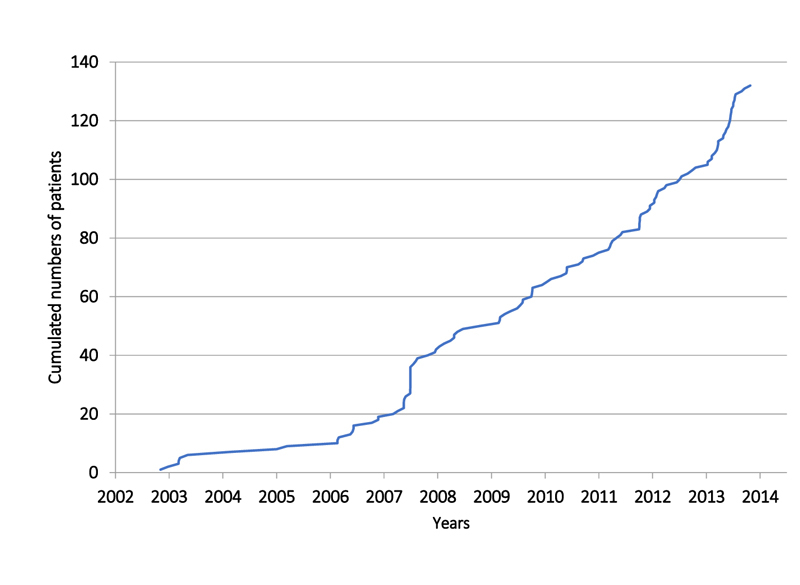
Figure 1 Cumulative number of patients during the length of the study.
The majority of patients were carrying a relatively restricted number of boulettes or packages (<25) within their digestive tract (table 1). The mean intra-abdominal package count was 16 boulettes and/or large packages, with a maximum of 100 large packages in one body packer (approximately 1 kg of narcotics). Body stuffers transported a significantly lower number of boulettes than body packers (mean 8.7 vs 34.2, p<0.001).
According to the information given by the patients, the majority of drug packages contained cocaine (60%), followed by methamphetamine (0.7%) and heroin (0.7%). In 39% of these patients, the patient did not reveal the nature of the narcotics.
Table 2 represents the clinical characteristics of patients at admission, as well as the nature of their admission and medical management.
Table 2 Clinical characteristics of 132 patients at admission, details of specific therapies and mean length of stay.
| Clinical observations |
Total patients
(n = 132) |
Body packers
(n = 36) |
Body stuffers
(n = 83) |
Indeterminate/mix
(n = 13) |
|---|---|---|---|---|
| SBP ≥140 mm Hg or DBP ≤90 mm Hg, n (%) | 67 (51%) | 15 (42%) | 43 (52%) | 9 (69%) |
| HR >100/min, n (%) | 19 (14%) | 7 (19%) | 11 (13%) | 1 (8%) |
| Abdominal pain, n (%) | 11 (8%) | 8 (22%) | 2 (2%) | 1 (8%) |
| Chest pain, n (%) | 7 (5%) | 1 (3%) | 5 (6%) | 1 (8%) |
| Convulsive episode, n (%) | 1 (0.8%) | 0 | 1 (1.2%) | 0 |
| Acute intoxication, n (%) | 0 | 0 | 0 | 0 |
| Osmotic laxatives, n (%) | 54 (41%) | 10 (28%) | 39 (47%) | 5 (38%) |
| + Senna | 1 | |||
| + Enema | 1 | |||
| Laparotomy*, n (%) | 3 (2%) | 3 (8%) | 0 | 0 |
| Antidote administration, n (%) | 0 | 0 | 0 | 0 |
| Length of stay (hours) | ||||
| Mean | 51.2 | 57.3 | 53,3 | 20,6 |
| Median | 42.2 | 46.7 | 42.2 | 20.2 |
| Range | 1.0–307.6 | 9.0–229.8 | 3.5–307.6 | 1.0–42.9 |
SBP= Systolic Blood Pressure; DBP = Diastolic Blood Pressure; HR = Heart Rate * Surgical indications for each of the 3 patients: intra-gastric stagnation of packets >24h00, intra-gastric stagnation of packets >5 days, intragastric packet >5cm.
Half (51%) of the patients were slightly hypertensive upon arrival in our emergency department; a mild tachycardia was also noted in 14% of cases. Nonspecific abdominal or thoracic pain was reported by a minority of cases. Body packers were more frequently subject to nonspecific abdominal pain than body stuffers (22 vs 2%, p <0.001).
One body-stuffer patient had a convulsive episode of unknown origin, which was treated successfully with antiepileptics without recurrence. The rupture of a drug package was never reported in our data, including the patient with an epileptic episode. No acute intoxication was noted; there were no deaths.
An ECG was recorded in 77 patients, of whom 26 (34%) had some abnormality consistent with early repolarisation. A urinary toxicology screen was done in two patients, with one positive for cocaine (this patient also had hypertension, though the patient was deemed not to be intoxicated). Blood tests (full blood count and/or urea/creatinine/electrolytes) were performed in 54 patients (41%); the results did not influence the therapeutic management.
No patient received an antidote. In light of slow intestinal transit, 55 patients (42%) received osmotic laxatives. Three body packers (2.3%) also required a surgical gastrotomy for various indications (packages too voluminous or gastric stagnation of packages). There were no postoperative complications in any of the three patients.
The mean length of stay in the emergency department was 51.2 hours. Location of the drug packages had no effect on the mean length of stay (MOS); MOS was 61.9 hours and 43.8 hours for locations in the stomach and lower intestine, respectively (p = 0.13). Nevertheless, the MOS was consequently prolonged for the three patients requiring surgical intervention (mean 158.1 hours, p <0.01). The MOS was not correlated with hypertension (mean 53.7 hours) or tachycardia (46.9 hours) on admission. The MOS was also independent of the number of ingested drug packages (fig. 2).
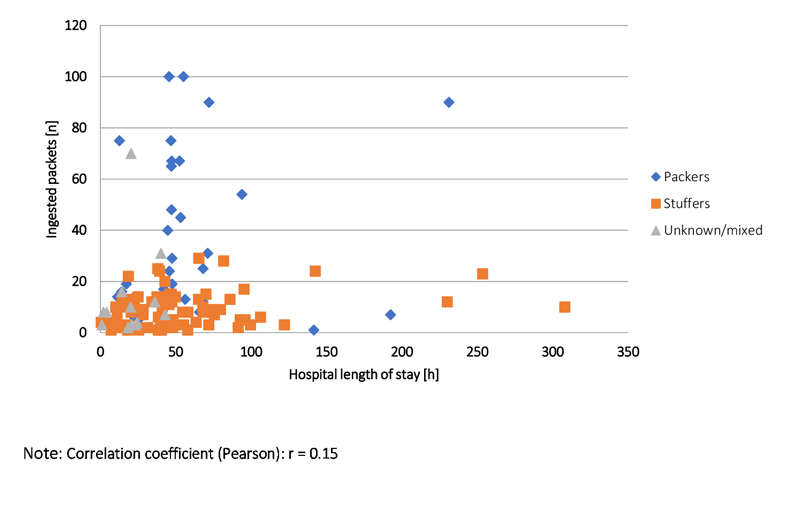
Figure 2 Length of stay (hours) in relation to calculated number of packages on computed tomography.
A second CT scan was undertaken in 19 patients (14%); one patient required a total of three CT scans over 7 consecutive days.
Body packers did not have a longer MOS than body stuffers (57.3 vs 53.3 hours, respectively, p = 0.54).
Our study of 132 body packers (n = 36, 27%) and body stuffers (n = 83, 63%) conclusively showed a very low prevalence of complications; in particular, intradigestive rupture of packaging and ileus were not seen within our patient cohort. Nevertheless, surgical intervention was required in three body packers (2.3%) owing to gastric stasis of packages. Although length of stay was longer in the presence of intragastric packages (61.9 vs 43.8 hours), this difference was not statistically significant (p = 0.13), and no increase in the length of stay was noted in relation to the number of ingested drug packages, the presence of chest pain or nonspecific clinical signs such as tachycardia or mild hypertension. Results of blood tests and/or an ECG, done as a standard measure, did not influence the medical management of these otherwise asymptomatic patients. The hypertension and/or tachycardia observed in a large number of patients were not associated with rupture of packaging or other signs suggestive of a toxidrome, and were more probably associated with the stress of police arrest.
Because of the large number of body stuffers and thanks to a standardised medical observation guideline, our study allowed for a good appreciation of the clinical characteristics and evolution of these patients. Our results confirmed those of the literature in terms of characteristics of portage, and onset of symptoms or complications, in particular regarding the high frequency of clinically insignificant mild hypertension or tachycardia [4, 22]. Although not statistically significant, the presence of intragastric drug packages seemed to prolong the delay before complete expulsion of the drug packages. The rate of rupture of drug packages was nil in our cohort (composed mostly of body stuffers), in contrast to a reported rate of 1.4% [6]; it seems to depend mostly on the quality of the packaging, which differs according to the country of origin [2]. Nonetheless, in light of the ever-present risk of rupture of packages, and the subsequent imminent risk of death [4–6, 23], in-hospital surveillance seems necessary for all body packers and body stuffers until expulsion of all the drug packages, as is practiced in France and Germany [19]. In our setting, the diagnostic procedure always includes the use of a CT scan to confirm the internal concealment of drugs, as a result of the low sensitivity of plain X-ray to reveal the presence of small packages of drugs in the body stuffers [6, 15–17]. Moreover, CT scan also allows an accurate estimation of the number of packages, unlike a plain X-ray.
Some authors have suggested an in-hospital observation period of 6 hours, arguing that this constitutes a safe minimum [22], although this was not confirmed in other studies. In the event of a sympathomimetic toxidrome occurring in a body packer, immediate surgical intervention is recommended in light of the high mortality due to rupture of a cocaine packet [4, 6, 23]. In the case of uncertainty regarding rupture of cocaine packets, a urinary screening test could be performed to confirm the intoxication. Gas chromatography or mass spectroscopy analysis are, of course, more precise ways to confirm the rupture or leak of the package; these tests are, however, frequently not readily available for clinical use.
The risks of intragastric stasis, obstruction, or intestinal perforation in body packers are well documented [9, 18, 23–25]. The rate of laparotomy varies widely in the literature owing to the large variation in the indications to perform such an intervention. No consensus exists regarding the necessity for surgical therapy in cases of gastric stasis >48 hours, with the indication varying on a case-by-case basis favouring the most conservative approach [19, 25]. Endoscopic retrieval is not recommended because of the risk of iatrogenic rupture of the packaging [11].
Finally, for all body packers or body stuffers, the administration of osmotic laxatives (lactulose) or polyethylene-glycol (PEG) is suggested, together with activated charcoal in body stuffers [26]. In our patient cohort, nearly half of the patients received osmotic laxatives, which were well tolerated. The administration of gastric prokinetic agents such as erythromycin has also been suggested [26]. Additionally, a nonclinical study has shown that paraffin- and/or mineral-oil-based laxatives rendered latex porous and thus increased the risk for rupture [27]. Owing to doubt as to whether full expulsion of packets has occurred, a second CT scan was performed in 14% of patients prior to medical discharge. Table 3 summarises the diagnostic and therapeutic recommendations derived from our data and the review of the literature.
Table 3 Characteristics of and recommendations for the management of body packers, body stuffers and body pushers
| Body packers | Body stuffers | Body pushers | |
|---|---|---|---|
| Nature of the package | Oblong latex drug packages (4–5 × 0–1.5 cm) | Spherical balls made of cling- film or cellophane (0 1–2 cm) | Variable, like “Kinder Surprise” eggs, or multi-packs of balls/boulettes |
| Frequent baseline clinical symptoms | Abdominal Pain | None, possibly anxiety with hypertension and tachycardia | None |
| Diagnostic confirmation | Abdominal X-ray or CT | Abdominal CT | Clinical exam., possibly abdominal X-ray |
| Counting of the packets | Abdominal CT | Abdominal CT | Not indicated |
| Clinical monitoring “focus” | Abdominal | Toxicological | None |
| Preventive therapy | Prokinetics (erythromycin), osmotic laxatives, polyethylene- glycol | Activated charcoal, osmotic laxatives, polyethylene- glycol | None |
| Main complications | Intestinal obstruction or perforation, occasionally deadly overdoses | Overdoses, occasionally deadly | None |
| Treatment of complications | Surgical extraction of the packages | Treatment of the cocaine or heroin intoxication (naloxone) | None |
| Appropriate surveillance location | Appropriate prison ward or hospital | Hospital | None |
| Length of Surveillance | Until full expulsion | Until full expulsion | None |
CT = computed tomography
Many limitations need to be considered with regard to this study. Its retrospective character meant that there was a lack of certain information from the medical charts. Nonetheless, this would not be relevant to the identification of complications or significant treatment. This allows us to viably state our observations, and also validate our (medical) standardised management guidelines.
In conclusion, we can state from this cohort study of 132 body packers and body stuffers that the management of this category of patients is rarely associated with serious complications, and that duration of hospital stay is long, on average 2 days before the full elimination of boulettes/packages, in particular in the presence of intragastric packages.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Booker RJ , Smith JE , Rodger MP . Packers, pushers and stuffers--managing patients with concealed drugs in UK emergency departments: a clinical and medicolegal review. Emerg Med J. 2009;26(5):316–20. doi:.https://doi.org/10.1136/emj.2008.057695
2 Bogusz MJ , Althoff H , Erkens M , Maier RD , Hofmann R . Internally concealed cocaine: analytical and diagnostic aspects. J Forensic Sci. 1995;40(5):811–5. doi:.https://doi.org/10.1520/JFS15390J
3 Cappelletti S , Piacentino D , Sani G , Bottoni E , Fiore PA , Aromatario M , et al. Systematic review of the toxicological and radiological features of body packing. Int J Legal Med. 2016;130(3):693–709. doi:.https://doi.org/10.1007/s00414-015-1310-3
4 June R , Aks SE , Keys N , Wahl M . Medical outcome of cocaine bodystuffers. J Emerg Med. 2000;18(2):221–4. doi:.https://doi.org/10.1016/S0736-4679(99)00198-5
5 Norfolk GA . The fatal case of a cocaine body-stuffer and a literature review - towards evidence based management. J Forensic Leg Med. 2007;14(1):49–52. doi:.https://doi.org/10.1016/j.jcfm.2005.12.002
6 Schaper A , Hofmann R , Bargain P , Desel H , Ebbecke M , Langer C . Surgical treatment in cocaine body packers and body pushers. Int J Colorectal Dis. 2007;22(12):1531–5. doi:.https://doi.org/10.1007/s00384-007-0324-9
7Hoffman RS, Nelson L. Internal concealment of drugs of abuse (body packing). Available from: https://www.uptodate.com/contents/internal-concealment-of-drugs-of-abuse-body-packing
8 Hugli O , Schmidt S , Trueb L , Yersin B . [Cocaine: new traffic mode, new detection method and new algorithm]. Rev Med Suisse. 2008;4(167):1747–53. Article in French.
9 Mandava N , Chang RS , Wang JH , Bertocchi M , Yrad J , Allamaneni S , et al. Establishment of a definitive protocol for the diagnosis and management of body packers (drug mules). Emerg Med J. 2011;28(2):98–101. doi:.https://doi.org/10.1136/emj.2008.059717
10 Traub SJ , Hoffman RS , Nelson LS . Body packing--the internal concealment of illicit drugs. N Engl J Med. 2003;349(26):2519–26. doi:.https://doi.org/10.1056/NEJMra022719
11 Wong GCK , Lai KK , Chung CH . Management of body packers in the emergency department. Hong Kong J Emerg Med. 2005;12:112–8.
12 Reginelli A , Russo A , Urraro F , Maresca D , Martiniello C , D’Andrea A , et al. Imaging of body packing: errors and medico-legal issues. Abdom Imaging. 2015;40(7):2127–42. doi:.https://doi.org/10.1007/s00261-015-0469-x
13 Marc B , Baud FJ , Aelion MJ , Gherardi R , Diamant-Berger O , Blery M , et al. The cocaine body-packer syndrome: evaluation of a method of contrast study of the bowel. J Forensic Sci. 1990;35(2):345–55. doi:.https://doi.org/10.1520/JFS12835J
14 Meijer R , Bots ML . Detection of intestinal drug containers by ultrasound scanning: an airport screening tool? Eur Radiol. 2003;13(6):1312–5.
15 Schmidt S , Hugli O , Rizzo E , Lepori D , Gudinchet F , Yersin B , et al. Detection of ingested cocaine-filled packets--diagnostic value of unenhanced CT. Eur J Radiol. 2008;67(1):133–8. doi:.https://doi.org/10.1016/j.ejrad.2007.07.017
16 Yang RM , Li L , Feng J , Lai SS , Lin BQ , Yu T , et al. Heroin body packing: clearly discerning drug packets using CT. South Med J. 2009;102(5):470–5. doi:.https://doi.org/10.1097/SMJ.0b013e31819ecacc
17 Shahnazi M , Sanei Taheri M , Pourghorban R . Body packing and its radiologic manifestations: a review article. Iran J Radiol. 2011;8(4):205–10. doi:.https://doi.org/10.5812/iranjradiol.4757
18 Gherardi RK , Leporc P , Dupeyron J-P , Baud FJ , Marc B , Diamant-Berger O . Detection of drugs in the urine of body-packers. Lancet. 1988;1(8594):1076–8. doi:.https://doi.org/10.1016/S0140-6736(88)91897-1
19 de Prost N , Lefebvre A , Questel F , Roche N , Pourriat JL , Huchon G , et al. Prognosis of cocaine body-packers. Intensive Care Med. 2005;31(7):955–8. doi:.https://doi.org/10.1007/s00134-005-2660-y
20 Glovinski PV , Lauritsen ML , Bay-Nielsen M , Brandstrup B , Bisgaard T . Asymptomatic body packers should be treated conservatively. Dan Med J. 2013;60(11):A4723.
21 Flach PM , Ross SG , Ampanozi G , Ebert L , Germerott T , Hatch GM , et al. “Drug mules” as a radiological challenge: sensitivity and specificity in identifying internal cocaine in body packers, body pushers and body stuffers by computed tomography, plain radiography and Lodox. Eur J Radiol. 2012;81(10):2518–26. doi:.https://doi.org/10.1016/j.ejrad.2011.11.025
22 Moreira M , Buchanan J , Heard K . Validation of a 6-hour observation period for cocaine body stuffers. Am J Emerg Med. 2011;29(3):299–303. doi:.https://doi.org/10.1016/j.ajem.2009.11.022
23 Álvarez Llano L , Rey Valcalcel C , Al-Lal Y-M , Pérez Díaz M-D , Stafford A , Turégano Fuentes F . The role of surgery in the management of “body packers”. Eur J Trauma Emerg Surg. 2014;40(3):351–5. doi:.https://doi.org/10.1007/s00068-014-0388-5
24 de Bakker JK , Nanayakkara PW , Geeraedts LM, Jr , de Lange ES , Mackintosh MO , Bonjer HJ . Body packers: a plea for conservative treatment. Langenbecks Arch Surg. 2012;397(1):125–30. doi:.https://doi.org/10.1007/s00423-011-0846-z
25 Beckley I , Ansari NA , Khwaja HA , Mohsen Y . Clinical management of cocaine body packers: the Hillingdon experience. Can J Surg. 2009;52(5):417–21.
26 Traub SJ , Su M , Hoffman RS , Nelson LS . Use of pharmaceutical promotility agents in the treatment of body packers. Am J Emerg Med. 2003;21(6):511–2. doi:.https://doi.org/10.1016/S0735-6757(03)00171-2
27 Visser L , Stricker B , Hoogendoorn M , Vinks A . Do not give paraffin to packers. Lancet. 1998;352(9137):1352. doi:.https://doi.org/10.1016/S0140-6736(98)08302-0
No financial support and no other potential conflict of interest relevant to this article was reported.