Physicians’ experience with follow-up care of childhood cancer survivors – challenges and needs
DOI: https://doi.org/10.4414/smw.2017.14457
Gisela
Michela, Micol E.
Gianinazzia, Janine
Vetscha, Luzius
Madera, Judith E.
Lupatschb, Nicolas X.
von der Weidc, Corina S.
Rueeggad
aDepartment of Health Sciences and Health Policy,
bInstitute of Social and Preventive Medicine,
cDepartment of Paediatric Oncology and Haematology,
dOslo Centre for Biostatistics and Epidemiology, Department of Biostatistics, Institute of Basic Medical Sciences,
Physicians’ experience with follow-up care of childhood cancer survivors – challenges and needs
w14457
Summary
BACKGROUND
Regular follow-up care is essential for childhood cancer survivors, but we know little about physicians’ experience with it. We aimed to describe: (1) involvement of Swiss physicians in follow-up care; (2) content of follow-up care provided; (3) problems encountered; and (4) additional resources needed.
MATERIALS AND METHODS: Within this cross-sectional survey we sent adapted questionnaires via professional associations to a sample of medical oncologists (MOs), paediatric oncologists (POs), general practitioners (GPs) and paediatricians (P) in Switzerland. Only oncologists involved in follow-up care were asked to report problems. GPs and Ps not involved in follow-up could indicate why. All physicians were asked about the content of follow-up care provided and additional resources needed.
RESULTS
A total of 183 physicians responded (27 MO, 13 PO, 122 GP, 21 P). Involved in follow-up were 81% of MOs, 85% of POs, 39% of GPs and 81% of Ps. Follow-up content differed between oncologists (MO and PO) and generalists (GP and P), with generalists examining or informing less in regard to the former cancer. POs reported more problems than MOs: many POs reported problems with transition of survivors to adult care (91%), and because of financial resources (73%) and time restraints (73%). MOs reported most problems during transition (23%). Not being aware of a survivor was the most common reason for GPs and Ps not participating in follow-up (74%). All groups reported a need for standardised protocols (85–91%) and specialised training (55–73%). GPs (94%) and Ps (100%) additionally desired more support from oncologists.
CONCLUSIONS
To improve quality and efficiency of follow-up care a national follow-up care model including standardised protocols and guidelines needs to be developed.
Introduction
Childhood cancer survivors are former patients who were diagnosed with cancer before the age of 15 years and have survived at least 5 years after diagnosis [1]. An adolescent and young adult (AYA) cancer survivor is defined as a former patient diagnosed between 15 and 39 years of age who survived at least 5 years after diagnosis [1].
High-quality, standardised follow-up care (regular medical check-ups to identify and treat late adverse outcomes early, and advice on health behaviour) of childhood and AYA cancer survivors will be a public health concern for two main reasons. First, there is an increasing population of childhood and AYA cancer survivors thanks to improvements of treatment in past decades [2]. The population of childhood cancer survivors was estimated to be 379 112 in the United States in 2010 [3] and 4902 in Switzerland in 2015 (including only Swiss residents diagnosed at age 0–14 years) [4]. Second, these survivors are at increased risk for developing late effects of the cancer and the treatments received [5, 6]. A recent study estimated that 95.5% of childhood cancer survivors suffered from any chronic health condition and 80.5% from a serious or life-threatening chronic condition by the age of 45 years [7].
Because of this increasing population with special medical needs, many international groups advocate systematic, risk-stratified and evidence-based long-term follow-up care for childhood and AYA cancer survivors, and specific recommendations have been published [8–12]. This is important to prevent, or detect early, cancer recurrence, second malignancies and other health and psychosocial problems due to the cancer or its treatment [1]. However, systematic implementation of these recommendations is still lacking in most countries, including Switzerland, and loss to follow-up of survivors remains a major problem [13–16].
In developed countries, about 1 in 500 young adults between the age of 20 and 39 years is estimated to be a childhood cancer survivor [2, 3, 17]. It is therefore essential that at some stage, not only specialists such as paediatric and medical oncologists, but also primary care physicians such as paediatricians and general practitioners (GPs), are involved in the follow-up care of childhood and AYA cancer patients [3, 18–20]. This will help to reduce the financial burden and preserve specialists’ valuable time for care of acute cancer patients. To develop such efficient models of follow-up care including specialists and generalists, the experience and needs of involved stakeholders (physicians, survivors, parents of survivors) need to be assessed. Whereas the view of survivors and parents has been investigated in the past [21–29], we still know little about the perception of physicians and their involvement in follow-up care [30]. Only three studies involved healthcare professionals’ view and only one of these included GPs [31–33]. The studies suggested greater nurse and primary care involvement, risk-stratified follow-up care, transition to adult care, increase in psychosocial support and model-based follow-up care as future directions to be pursued [30].
We therefore investigated: (1) the involvement of physicians from different specialities in follow-up care of childhood and AYA cancer survivors; (2) the content of the follow-up care they provide; (3) the problems they encountered; and (4) additional resources they would need to provide optimal care.
Materials and methods
The Childhood Cancer Follow-Up Study (CCFU)
The CCFU is a nested project of the population-based Swiss Childhood Cancer Survivor Study (SCCSS), which had the overall aim of investigating the long-term effects of childhood cancer and its treatment [34]. The CCFU is a questionnaire survey with the specific aim of gaining in-depth knowledge on preferences and needs for the organisation of follow-up care of childhood cancer survivors in Switzerland [35]. For this purpose, relevant stakeholders (survivors, survivors’ parents, physicians) were contacted with questionnaires. This paper evaluates the questionnaire to physicians sent between 2011 and 2012.
Sample and procedure
We included four groups of physicians frequently involved in follow-up care in Switzerland: medical oncologists, paediatric oncologists, GPs and paediatricians. Medical oncologists and paediatric oncologists were considered specialists (oncologists), GPs and paediatricians generalists (primary care physicians). We developed adapted, semistructured questionnaires for each group (see appendix 1 for a translated version of all the questions used in the current study, provided in separate download file). The questionnaire to the generalists was short and included 17 questions; the questionnaire to the specialists had additional more detailed questions on follow-up care, ending up with 32 items.
We used different strategies to contact the physicians depending on the availability of and access to databases of physicians in the respective specialty and individual contact information. Medical oncologists received an e-mail with the study invitation and a link to an online survey from the Swiss Society of Medical Oncology (n = 241). From the Swiss Paediatric Oncology Group we received a list with all paediatric oncologists in Switzerland (n = 40). They were contacted from the study centre by e-mail with the study invitation and a link to the online survey. To contact GPs and paediatricians, we used an address list of all members of the Hausärzte Schweiz: Berufsverband der Haus- und Kinderärztinnen Schweiz (Swiss Professional Association of General Practitioners and Paediatricians), which unites the Swiss Society of General Practitioners (SGAM), the Swiss Society of General Internal Medicine (SGIM) and the Swiss Society of Paediatrics (SSP). We received 6312 addresses and drew a random sample of 700 German- and 300 French-speaking physicians (reflecting the proportion of the Swiss and German speaking population of Switzerland), using the STATA (version 13.1; College Station, TX) command to draw random samples without replacement. In addition, we contacted the GPs (n = 114) of survivors who provided the name and address of their doctor (and consent to contact them) in an earlier questionnaire of the Swiss Childhood Cancer Survivor Study [34]. The GPs and paediatricians were contacted by mail and sent a paper-based questionnaire. They could also complete the questionnaire online if preferred.
Questions on follow-up care
We assessed the following information to describe physicians’ (1) involvement in, (2) content of, (3) problems with, and (4) needs for optimal follow-up care of, childhood and AYA cancer survivors (appendix 1). First, we asked all physicians to report any experience with childhood (diagnosed at age ≤15years) and AYA (diagnosed at age 16–25years) cancer patients and whether they were involved in follow-up care. Second, we asked all physicians who were involved in follow-up care, which types of cancer they follow up and what services they routinely provide in their follow-up care. Third, to assess problems in the provision of follow-up care, we asked generalists who were not involved in follow-up to indicate the reasons why; we asked oncologists who were involved in follow-up to report the problems they encountered on the patient level and on the institution level. Fourth, we asked all physicians who were involved in follow-up, what additional resources they would need to provide optimal care.
Other information assessed
We assessed physicians’ age at the time of the study, time since specialisation, sex, work situation (hospital; private practice; both) and work setting (urban; rural).
Statistical analyses
Statistical analysis was performed with STATA version 13.1. We performed complete case analysis. We used means and range or numbers and proportions to describe the study population, overall and stratified by specialisation (medical oncologists, paediatric oncologists, GPs, paediatricians). To address aim 1, we used numbers and proportions to describe the involvement of physicians in follow-up care of childhood and AYA cancer survivors, overall and stratified by specialisation. We calculated p-values comparing all four specialisations using univariable logistic regression (if the variable of interest was binary) or univariable multinomial logistic regression (if the variable of interest had more than two categories). Chi-square statistics were used for comparisons within specialists and generalists. For aim 2, we used numbers and proportions to describe the content of follow-up care stratified by specialisation. Chi-square statistics were used to compare the content of follow-up care between the medical specialisations. For aims 3 and 4, we used numbers, proportions and 95% confidence intervals to describe the problems encountered, reasons for not engaging in follow-up care and additional resources needed for optimal care, all stratified by medical specialisation.
Results
Study Population
Out of the 1395 physicians contacted, 183 (13%) responded. Of those 183, 27 (15%) were medical oncologists, 13 (7%) paediatric oncologists, 122 (67%) GPs and 21 (12%) paediatricians (table 1). The mean age of the physicians at the time of the study was 54.3 years (range 33–81), mean time since specialisation 20.1 years (range 1–52), and 76% were male. The working situation differed between specialisations (p <0.001), with all paediatric oncologists and half of the medical oncologists working exclusively in a hospital, whereas the generalists mainly worked in private practices. The work setting also differed (p = 0.010), with oncologists working almost exclusively in urban areas (92% of medical oncologists and 100% of paediatric oncologists), compared with 69% GPs and 85% paediatricians.
Table 1 Characteristics of physicians who participated in the study.
|
Total
(n = 183)
|
Medical oncologists
(n = 27)
|
Paediatric oncologists
(n = 13)
|
General practitioners*
(n = 122)
|
Paediatricians
(n = 21)
|
p-value
|
|
Mean
|
Range
|
Mean
|
Range
|
Mean
|
Range
|
Mean
|
Range
|
Mean
|
Range
|
| Age at study (years) |
54.3 |
33–81 |
53.7 |
39–69 |
50.2 |
40–81 |
54.8 |
33–74 |
54.6 |
43–68 |
0.339
†
|
| Time since specialisation (years) |
20.1 |
1–52 |
18.8 |
5–31 |
15.7 |
4–52 |
20.7 |
1–44 |
20.8 |
7–37 |
0.345
†
|
|
n
|
%‡
|
n
|
%‡
|
n
|
%‡
|
|
%‡
|
n
|
%‡
|
|
| Sex |
|
|
|
|
|
|
|
|
|
|
|
| Male |
139 |
76.0 |
21 |
77.8 |
9 |
69.2 |
95 |
77.9 |
14 |
66.7 |
|
| Female |
44 |
24.0 |
6 |
22.2 |
4 |
30.8 |
27 |
22.1 |
7 |
33.3 |
0.658§
|
| Work situation |
|
|
|
|
|
|
|
|
|
|
|
| Hospital |
30 |
16.9 |
15 |
55.6 |
13 |
100 |
2 |
1.7 |
0 |
0 |
|
| Own or group practice |
135 |
75.8 |
4 |
14.8 |
0 |
0 |
113 |
96.6 |
18 |
85.7 |
|
| Both |
13 |
7.3 |
8 |
29.6 |
0 |
0 |
2 |
1.7 |
3 |
14.3 |
<0.001¶
|
| Work location |
|
|
|
|
|
|
|
|
|
|
|
| Urban |
128 |
22.9 |
24 |
92.3 |
12 |
100 |
75 |
69.4 |
17 |
85.0 |
|
| Rural |
38 |
77.1 |
2 |
7.7 |
0 |
0 |
33 |
30.6 |
3 |
15.0 |
0.010§
|
| Involved in FU care of child/AYA cancer survivors‖
|
|
|
|
|
|
|
|
|
|
|
|
| Yes |
98 |
53.6 |
22 |
81.5 |
11 |
84.6 |
48 |
39.3 |
17 |
81.0 |
|
| No |
85 |
46.4 |
5 |
18.5 |
2 |
15.4 |
74 |
60.7 |
4 |
19.0 |
<0.001§
|
Involvement in follow-up care
Overall, 22 (82%) medical oncologists, 11 (85%) paediatric oncologists, 48 (39%) GPs, and 17 (81%) paediatricians had been involved in follow-up care of young cancer survivors (table 1). Among specialists, 4 (15%) medical oncologists and 11 (85%) paediatric oncologists were involved in follow-up care of childhood cancer survivors (p<0.001; table 2). Twenty-two (82%) medical oncologists and 10 (77%) paediatric oncologists were involved in follow-up of AYA cancer survivors (p = 0.736). Among generalists, 16 (13%) GPs and 8 (38%) paediatricians were currently involved in follow-up care of childhood cancer survivors (p = 0.005), and 21 (17%) and 1 (5%) in follow-up of AYA cancer survivors (p = 0.144).
Table 2 Physicians’ experience with childhood, adolescent and young adult cancer patients and their follow-up care.
|
Medical oncologists
(n = 27)
|
Paediatric oncologists
(n = 13)
|
General practitioners
(n = 122)
|
Paediatricians
(n = 21)
|
p-value†
|
|
n
|
%*
|
n
|
%*
|
n
|
%*
|
n
|
%*
|
| Experience with cancer patients in general (only oncologists)‡
|
|
|
|
|
n.a.‡
|
n.a.‡
|
n.a.‡
|
n.a.‡
|
|
| Inpatient treatment of new patients |
19 |
70.3 |
12 |
92.3 |
|
|
|
|
0.219 |
| Outpatient treatment of new patients |
24 |
88.8 |
11 |
84.6 |
|
|
|
|
0.217 |
| FU care ≤5 years since diagnosis |
22 |
81.5 |
12 |
92.3 |
|
|
|
|
0.681 |
| FU care 5-10 years since diagnosis |
22 |
81.5 |
12 |
92.3 |
|
|
|
|
0.681 |
| Long-term follow-up care ≥10 years since diagnosis |
16 |
59.3 |
10 |
76.9 |
|
|
|
|
0.416 |
| Other experience with cancer patients |
2 |
7.4 |
3 |
23.1 |
|
|
|
|
0.192 |
| Experience with follow up care of cancer patients (only oncologists)‡
|
|
|
|
|
n.a.‡
|
n.a.‡
|
n.a.‡
|
n.a.‡
|
|
| FU care childhood cancer |
4 |
14.8 |
11 |
84.6 |
|
|
|
|
<0.001 |
| FU care AYA cancer |
22 |
81.5 |
10 |
76.9 |
|
|
|
|
0.736 |
| FU care adult cancer |
24 |
88.9 |
4 |
30.8 |
|
|
|
|
<0.001 |
| No experience |
3 |
11.5 |
2 |
15.4 |
|
|
|
|
0.735 |
| Experience with childhood/AYA cancer (only generalists)‡
|
n.a.‡
|
n.a.‡
|
n.a.‡
|
n.a.‡
|
|
|
|
|
|
| Ever diagnosed a childhood/AYA cancer patient |
|
|
|
|
33 |
27.1 |
15 |
71.4 |
<0.001 |
| Involved in FU care >2 years ago |
|
|
|
|
33 |
27.1 |
14 |
66.7 |
<0.001 |
| Currently involved in FU care of childhood cancer |
|
|
|
|
16 |
13.1 |
8 |
38.1 |
0.005 |
| Currently involved in FU care of AYA cancer |
|
|
|
|
21 |
17.2 |
1 |
4.8 |
0.144 |
| Other experience with childhood/AYA cancer |
|
|
|
|
18 |
14.8 |
5 |
23.8 |
0.297 |
| No experience with childhood/AYA cancer |
|
|
|
|
75 |
61.5 |
1 |
4.8 |
<0.001 |
Content of follow-up care
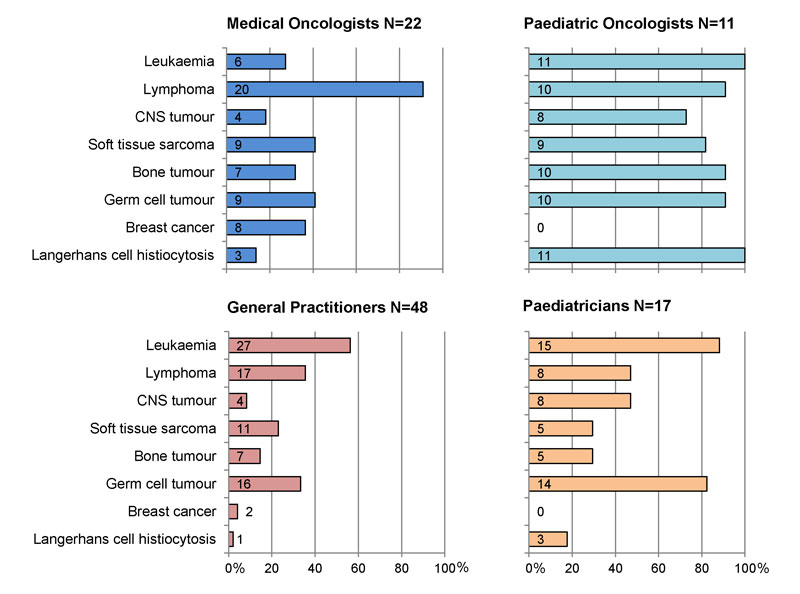
The types of cancers included in follow-up care differed between the specialisations (all p-values comparing the prevalence of each diagnosis between the medical specialisations ≤0.002, fig. 1). Most medical oncologists followed up survivors of lymphoma (n = 20, 95% of 22 medical oncologists involved in follow-up). Paediatric oncologists followed up survivors of all types of cancer, except breast cancer. Most GPs reported following up survivors of leukaemia (n = 27, 56% of 48 GPs), lymphoma (n = 17, 35%) and germ cell tumours (n = 16, 33%). Paediatricians mostly saw survivors of leukaemia (n = 15, 88% of 17 paediatricians) and germ cell tumours (n = 14, 82%) for follow-up care.
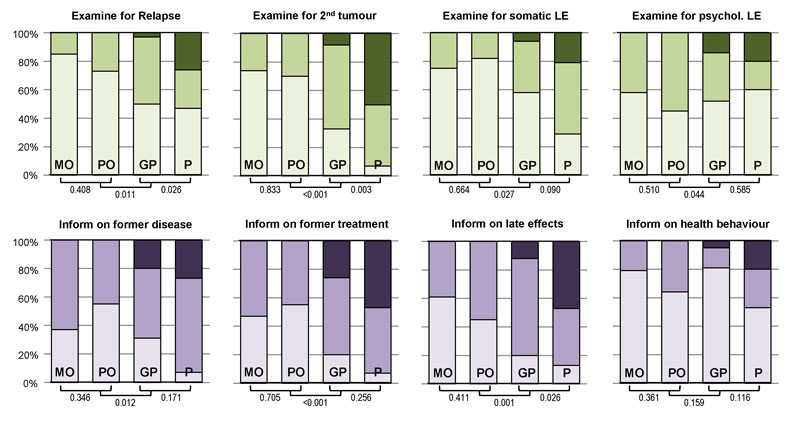
In general, oncologists, independent of whether medical or paediatric, offered follow-up care of similar content (all p-values >0.300; fig. 2). The content of follow-up provided by GPs and paediatricians was also comparable (5 out of 8 p-values >0.05). However, follow-up care provided by oncologists differed significantly from the care provided by generalists (all p <0.05, except for information on health behaviours). Compared with generalists, more oncologists examined survivors for relapse, second tumours and late somatic effects, and informed them about their former disease, former treatment and possible late effects. Differences were less pronounced for the examination of psychological late effects; counselling on healthy behaviour did not differ between oncologists and generalists.
Problems encountered and reasons for not engaging in follow-up care
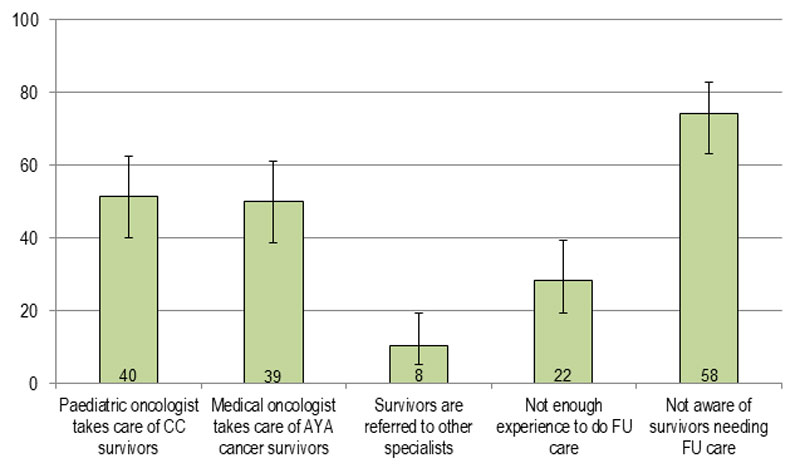
Generalists could indicate reasons for not engaging in follow-up care (total n = 78; fig. S1 in appendix 2). Most stated that they were not aware of survivors needing follow up (n = 58, 74% of 78). Other reasons were that paediatric (n = 40, 51%) or medical (n = 39, 50%) oncologists were taking care of these patients; or not having enough experience to provide follow-up care (n = 22, 28%).
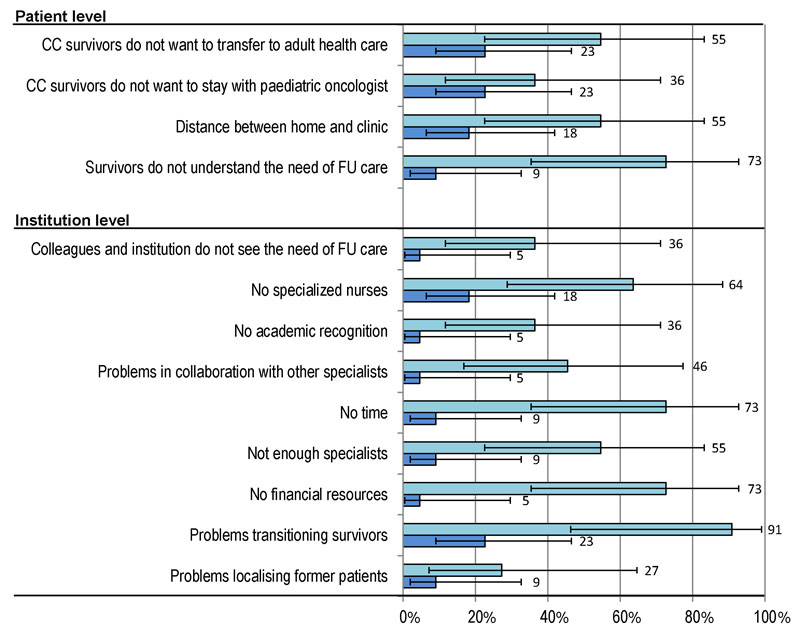
Oncologists who were involved in follow-up care were asked to indicate problems they encountered (fig. 3). Overall, more paediatric than medical oncologists reported problems. The most frequent problem for paediatric oncologists (n = 11) on the patient level was that survivors did not understand the need for follow-up (73%, n = 8). On the institution level they reported problems with transitioning patients to adult care (91%, n = 10), lack of time and financial resources (both 73%, n = 8), and lack of specialised nurses (64%, n = 7). Medical oncologists (n = 22) reported, on the patient level, that childhood cancer survivors often wish not to transfer to adult oncologists (23%, n = 5), and found the distance between home and clinic too long (18%, n = 4). On the institution level, they reported problems with transitioning patients (23%, n = 5) and lack of specialised nurses (18%, n = 4).
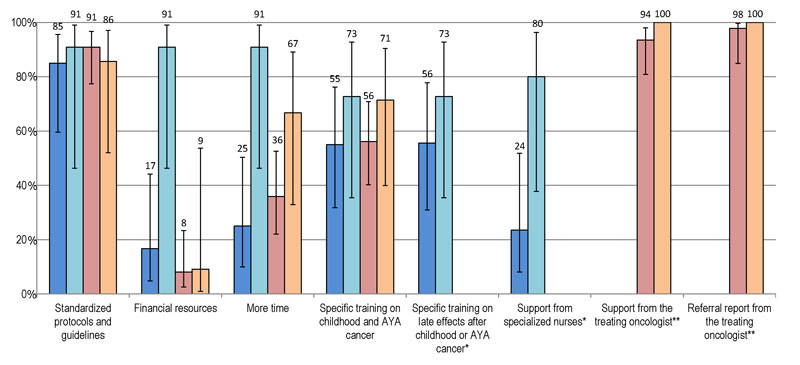
Additional resources needed for optimal care
In all four groups of specialisation, most physicians reported that they desired standardised protocols and guidelines (85–91% variation between groups; fig. 4), followed by the need for specific training (55–73%). Paediatric oncologists additionally wished for more financial resources (91%). GPs and paediatricians would appreciate support from the treating oncologist (94% of GPs and 100% of paediatricians) and a referral report from the oncologist (98% GPs and 100% paediatricians).
Discussion
We found that, among our responders, most medical and paediatric oncologists, as well as paediatricians, have been involved in follow-up care of young cancer survivors, but less than half of GPs reported doing so. The types of cancer diagnoses seen, as well as the content of follow-up care provided, differed between oncologists and generalists. All physicians, independent of their specialisation stated the need for standardised protocols and guidelines (85-91%). GPs and paediatricians also desired more support from the treating oncologists (94 and 100%, respectively) and a referral report with the medical history and recommendations for follow up (98 and 100%, respectively).
A major strength of our study is that we assessed the opinion of different medical specialists at the same time and with similar questions (some adaptions between specialisations were necessary). This allowed us to compare directly the experiences, problems and needs of different medical specialists regarding follow up of childhood and AYA cancer survivors. We put a lot of effort into different mailing strategies in order to contact all members or a random sample of the respective medical speciality. This was rather difficult in Switzerland, because no national registry with all active physicians exists. The questionnaire focussed explicitly on follow-up care, therefore many in-depth questions could be asked.
This study also has limitations. Because we had no access to a database of active physicians with contact information, we had to send most of our questionnaires via professional associations. We therefore do not know how many physicians really received our questionnaire and we were not able to send reminders to increase response, which makes it difficult to judge the representativeness of our sample. In our study, physicians involved in follow-up might have been more interested in responding to the questionnaire. Therefore, our results might not reflect the true participation of Swiss physicians in follow-up care of childhood and AYA cancer survivors. Because we have no information on nonresponders we cannot tell how selection bias might have affected the results. However, most of our results focus on physicians who are involved in follow-up care, and we think that these results are less prone to selection bias. Also, the different contact strategies might have affected the response behaviour: physicians might be more reluctant to answer a general e-mail from the medical association than a personally addressed letter. However, research on selection and response bias has shown that a low response rate does not necessarily introduce response bias [36, 37]. In a methodological study, Groves and colleagues explained this phenomenon by the fact that every person is potentially either a responder or a nonresponder, depending on various characteristics and circumstances, and nonresponse bias may cancel out across subgroups [36, 37]. Finally, because we stratified our results by specialisation and because Switzerland is a small country, we ended up with small numbers of oncologists.
Follow-up care of the growing population of childhood cancer survivors will become a public health concern [2, 3, 5, 7]. It is therefore important to provide high-quality and cost-effective care for this population with increased medical needs [38–41]. A model of care including not only specialists but also primary care physicians might prevent over- or undertreatment of survivors and thereby reduce loss to follow up [42–44]. Our results showed that GPs and paediatricians are involved in follow-up care of childhood and AYA cancer survivors. For optimal care, however, they need standardised protocols and guidelines, support from the treating oncologist and a referral letter including the medical history of the patient and recommendations for follow-up. Similar results were found by Nathan and colleagues, where 85% of the contacted US and Canadian family physicians desired support of the oncologist or follow-up guidelines [45]. Also, Blaauwbroek and colleagues reported that GPs from the northern Netherlands were willing to participate in follow-up care of childhood cancer survivors if adequate guidelines and medical information were provided, and communication lines between the paediatric oncologists and GPs were clear [46].
This need for support and guidelines might reflect uncertainty of generalists about care for childhood cancer survivors. In our study, 28% of generalists stated that they did not provide follow-up care owing to lack of experience. Other studies reported the same lack of knowledge among primary care physicians regarding health problems of survivors, optimal surveillance and provision of information [33, 45]. A recent study found that, among a random sample of specialists for internal medicine, most reported being uncomfortable with the care of childhood cancer survivors and unfamiliar with available guidelines [47]. This lack of knowledge among GPs and paediatricians might be reflected in our study in the content of follow-up care they provided, which differed from the services of oncologists. GPs and paediatricians examined mostly general physical and mental health and informed patients about health behaviours rather than cancer-specific issues.
To overcome these problems, we have various suggestions that could be implemented in Switzerland or other countries with a similar healthcare system in order to develop a shared-care model including oncologists and generalists. Generalists need to be educated and provided with guidelines sufficiently to feel comfortable in examining and discussing cancer-related issues. This was tried in a pilot project and proved effective in terms of feasibility and interest of primary care physicians [43]. One specialised primary care physician for a certain catchment area might be able to provide adequate follow-up care for all survivors in the area and involve other specialists if needed.
Furthermore each survivor should receive a personal survivorship care plan, a so called “survivorship passport” [48]. This personalised passport contains important information about the cancer-specific diagnoses, treatments and follow-up care recommendations [49, 50]. The specified follow-up tasks can then be adopted by either specialists or primary care physicians based on their competencies. Thanks to the survivorship passport, the tasks can be efficiently organised and loss to follow-up, as well as overtreatment, of survivors can be reduced. The passport is advocated by Childhood Cancer Switzerland, PanCare (Pan-European Network for Care of Survivors after Childhood and Adolescent Cancer) and ENCCA (European Network for Cancer Research in Children and Adolescents) and is planned to be introduced in Swiss hospitals in autumn 2017 [49, 50].
Conclusion
In Switzerland, many physicians, except GPs, reported being involved in follow-up of childhood and adolescent cancer survivors. To improve quality and efficiency of follow-up, care a national model including standardised protocols and guidelines needs to be developed in accordance with international efforts to standardise follow-up care.
Appendix 1 Translated English version of the questions
This appendix is provided as a separate file for downloading at: https://smw.ch/en/article/doi/smw.2017.14457/
Appendix 2 Supplemental figure
Acknowledgements
We thank the physicians for participating in our survey and the study team of the Childhood Cancer Follow-Up Study (Fabienne Liechti, Anna Hohn, Philip Laeuppi).
References
1
www.cancer.gov 2016 [cited 2016; Available from: www.cancer.gov]
2
Gatta
G
,
Botta
L
,
Rossi
S
,
Aareleid
T
,
Bielska-Lasota
M
,
Clavel
J
, et al.; EUROCARE Working Group. Childhood cancer survival in Europe 1999-2007: results of EUROCARE-5--a population-based study. Lancet Oncol. 2014;15(1):35–47. https://doi.org/10.1016/S1470-2045(13)70548-5
3
Ward
E
,
DeSantis
C
,
Robbins
A
,
Kohler
B
,
Jemal
A
. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):83–103. https://doi.org/10.3322/caac.21219
4Pfeiffer V, Redomond S, Kouonen R, Sommer G, Spycher B, Schindler M, et al. Swiss Childhood Cancer Registry. Annual Report 2014-2015. Bern: University of Bern Institute of Social and Preventive Medicine; 2016.
5
Oeffinger
KC
,
Mertens
AC
,
Sklar
CA
,
Kawashima
T
,
Hudson
MM
,
Meadows
AT
, et al.; Childhood Cancer Survivor Study. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355(15):1572–82. https://doi.org/10.1056/NEJMsa060185
6
Alvarez
JA
,
Scully
RE
,
Miller
TL
,
Armstrong
FD
,
Constine
LS
,
Friedman
DL
, et al.
Long-term effects of treatments for childhood cancers. Curr Opin Pediatr. 2007;19(1):23–31. https://doi.org/10.1097/MOP.0b013e328013c89e
7
Hudson
MM
,
Ness
KK
,
Gurney
JG
,
Mulrooney
DA
,
Chemaitilly
W
,
Krull
KR
, et al.
Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309(22):2371–81. https://doi.org/10.1001/jama.2013.6296
8
Landier
W
,
Bhatia
S
,
Eshelman
DA
,
Forte
KJ
,
Sweeney
T
,
Hester
AL
, et al.
Development of risk-based guidelines for pediatric cancer survivors: the Children’s Oncology Group Long-Term Follow-Up Guidelines from the Children’s Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol. 2004;22(24):4979–90. https://doi.org/10.1200/JCO.2004.11.032
9Children’s Oncology Group. Long-Tem Follow-Up Program Resource Guide. Wendy Landler, editor 2008.
10
Wallace
WHB
,
Blacklay
A
,
Eiser
C
,
Davies
H
,
Hawkins
M
,
Levitt
GA
, et al.; Late Effects Committee of the United Kingdom Children’s Cancer Study Group (UKCCSG). Developing strategies for long term follow up of survivors of childhood cancer. BMJ. 2001;323(7307):271–4. https://doi.org/10.1136/bmj.323.7307.271
11
Wallace
WHB
,
Thompson
L
,
Anderson
RA
; Guideline Development Group. Long term follow-up of survivors of childhood cancer: summary of updated SIGN guidance. BMJ. 2013;346:f1190. https://doi.org/10.1136/bmj.f1190
12
Kremer
LCM
,
Mulder
RL
,
Oeffinger
KC
,
Bhatia
S
,
Landier
W
,
Levitt
G
, et al.; International Late Effects of Childhood Cancer Guideline Harmonization Group. A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer. 2013;60(4):543–9. https://doi.org/10.1002/pbc.24445
13
Steele
JR
,
Wall
M
,
Salkowski
N
,
Mitby
P
,
Kawashima
T
,
Yeazel
MW
, et al.
Predictors of risk-based medical follow-up: a report from the Childhood Cancer Survivor Study. J Cancer Surviv. 2013;7(3):379–91. https://doi.org/10.1007/s11764-013-0280-z
14
Rebholz
CE
,
von der Weid
NX
,
Michel
G
,
Niggli
FK
,
Kuehni
CE
; Swiss Pediatric Oncology Group (SPOG). Follow-up care amongst long-term childhood cancer survivors: a report from the Swiss Childhood Cancer Survivor Study. Eur J Cancer. 2011;47(2):221–9. https://doi.org/10.1016/j.ejca.2010.09.017
15
Skinner
R
,
Wallace
WHB
,
Levitt
G
. Long-term follow-up of children treated for cancer: why is it necessary, by whom, where and how?
Arch Dis Child. 2007;92(3):257–60. https://doi.org/10.1136/adc.2006.095513
16
Essig
S
,
Skinner
R
,
von der Weid
NX
,
Kuehni
CE
,
Michel
G
. Follow-up programs for childhood cancer survivors in Europe: a questionnaire survey. PLoS One. 2012;7(12):e53201. https://doi.org/10.1371/journal.pone.0053201
17Mitter V, Michel G, Woelfli P, et al. The Swiss Childhood Cancer Registry. Annual Report 2011/2012. Bern: Institute of Social and Preventive Medicine, University of Bern; 2013.
18
Oeffinger
KC
,
Mertens
AC
,
Hudson
MM
,
Gurney
JG
,
Casillas
J
,
Chen
H
, et al.
Health care of young adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Ann Fam Med. 2004;2(1):61–70. https://doi.org/10.1370/afm.26
19
Haddy
RI
,
Haddy
TB
. Lifetime follow-up care after childhood cancer. J Am Board Fam Med. 2010;23(5):647–54. https://doi.org/10.3122/jabfm.2010.05.100031
20
Guilcher
GMT
,
Fitzgerald
C
,
Pritchard
S
. A questionnaire based review of long-term follow-up programs for survivors of childhood cancer in Canada. Pediatr Blood Cancer. 2009;52(1):113–5. https://doi.org/10.1002/pbc.21701
21
Kinahan
KE
,
Sharp
LK
,
Arntson
P
,
Galvin
K
,
Grill
L
,
Didwania
A
. Adult survivors of childhood cancer and their parents: experiences with survivorship and long-term follow-up. J Pediatr Hematol Oncol. 2008;30(9):651–8. https://doi.org/10.1097/MPH.0b013e31817e4a6a
22
Earle
EA
,
Davies
H
,
Greenfield
D
,
Ross
R
,
Eiser
C
. Follow-up care for childhood cancer survivors: a focus group analysis. Eur J Cancer. 2005;41(18):2882–6. https://doi.org/10.1016/j.ejca.2005.08.028
23
Absolom
K
,
Eiser
C
,
Michel
G
,
Walters
SJ
,
Hancock
BW
,
Coleman
RE
, et al.
Follow-up care for cancer survivors: views of the younger adult. Br J Cancer. 2009;101(4):561–7. https://doi.org/10.1038/sj.bjc.6605213
24
Absolom
K
,
Greenfield
D
,
Ross
R
,
Horne
B
,
Davies
H
,
Glaser
A
, et al.
Predictors of clinic satisfaction among adult survivors of childhood cancer. Eur J Cancer. 2006;42(10):1421–7. https://doi.org/10.1016/j.ejca.2006.01.053
25
Michel
G
,
Greenfield
D
,
Absolom
K
,
Eiser
C
; Late Effects Group Sheffield. Satisfaction with follow-up consultations among younger adults treated for cancer: the role of quality of life and psychological variables. Psychooncology. 2011;20(8):813–22. https://doi.org/10.1002/pon.1783
26
Michel
G
,
Greenfield
DM
,
Absolom
K
,
Ross
RJ
,
Davies
H
,
Eiser
C
; Late Effects Group Sheffield. Follow-up care after childhood cancer: survivors’ expectations and preferences for care. Eur J Cancer. 2009;45(9):1616–23. https://doi.org/10.1016/j.ejca.2009.02.026
27
Michel
G
,
Gianinazzi
ME
,
Eiser
C
,
Bergstraesser
E
,
Vetsch
J
,
von der Weid
N
, et al.; Swiss Paediatric Oncology Group. Preferences for long-term follow-up care in childhood cancer survivors. Eur J Cancer Care (Engl). 2016;25(6):1024–33. https://doi.org/10.1111/ecc.12560
28
Christen
S
,
Vetsch
J
,
Mader
L
,
Dehler
S
,
Korol
D
,
Kuehni
C
, et al.
Preferences for the organization of long-term follow-up in adolescent and young adult cancer survivors. Support Care Cancer. 2016;24(8):3425–36. https://doi.org/10.1007/s00520-016-3157-7
29
Vetsch
J
,
Rueegg
CS
,
Mader
L
,
Bergstraesser
E
,
Diezi
M
,
Kuehni
CE
, et al.; Swiss Paediatric Oncology Group. Parents’ preferences for the organisation of long-term follow-up of childhood cancer survivors. Eur J Cancer Care (Engl). 2017;e12649. https://doi.org/10.1111/ecc.12649
30
Aslett
H
,
Levitt
G
,
Richardson
A
,
Gibson
F
. A review of long-term follow-up for survivors of childhood cancer. Eur J Cancer. 2007;43(12):1781–90. https://doi.org/10.1016/j.ejca.2007.04.009
31
Taylor
A
,
Hawkins
M
,
Griffiths
A
,
Davies
H
,
Douglas
C
,
Jenney
M
, et al.
Long-term follow-up of survivors of childhood cancer in the UK. Pediatr Blood Cancer. 2004;42(2):161–8. https://doi.org/10.1002/pbc.10482
32
Oeffinger
KC
,
Eshelman
DA
,
Tomlinson
GE
,
Buchanan
GR
. Programs for adult survivors of childhood cancer. J Clin Oncol. 1998;16(8):2864–7. https://doi.org/10.1200/JCO.1998.16.8.2864
33
Mertens
AC
,
Cotter
KL
,
Foster
BM
,
Zebrack
BJ
,
Hudson
MM
,
Eshelman
D
, et al.
Improving health care for adult survivors of childhood cancer: recommendations from a delphi panel of health policy experts. Health Policy. 2004;69(2):169–78. https://doi.org/10.1016/j.healthpol.2003.12.008
34
Kuehni
CE
,
Rueegg
CS
,
Michel
G
,
Rebholz
CE
,
Strippoli
MP
,
Niggli
FK
, et al.; Swiss Paediatric Oncology Group (SPOG). Cohort profile: the Swiss childhood cancer survivor study. Int J Epidemiol. 2012;41(6):1553–64. https://doi.org/10.1093/ije/dyr142
35
Gianinazzi
ME
,
Essig
S
,
Rueegg
CS
,
von der Weid
NX
,
Brazzola
P
,
Kuehni
CE
, et al.; Swiss Paediatric Oncology Group (SPOG). Information provision and information needs in adult survivors of childhood cancer. Pediatr Blood Cancer. 2014;61(2):312–8. https://doi.org/10.1002/pbc.24762
36
Groves
RM
. Nonresponse Rates and Nonresponse Bias in Household Surveys. Public Opin Q. 2006;70(5):646–75. https://doi.org/10.1093/poq/nfl033
37
Groves
RM
,
Singer
E
,
Corning
A
. Leverage-saliency theory of survey participation: description and an illustration. Public Opin Q. 2000;64(3):299–308. https://doi.org/10.1086/317990
38
McBride
ML
,
Lorenzi
MF
,
Page
J
,
Broemeling
AM
,
Spinelli
JJ
,
Goddard
K
, et al.
Patterns of physician follow-up among young cancer survivors: report of the Childhood, Adolescent, and Young Adult Cancer Survivors (CAYACS) research program. Can Fam Physician. 2011;57(12):e482–90.
39
Langer
T
,
Henze
G
,
Beck
JD
; For the German Late Effects Study Group in the German Society Pediatric Oncology and Hematology (GPOH). Basic methods and the developing structure of a late effects surveillance system (LESS) in the long-term follow-up of pediatric cancer patients in Germany. Med Pediatr Oncol. 2000;34(5):348–51. https://doi.org/10.1002/(SICI)1096-911X(200005)34:5<348::AID-MPO6>3.0.CO;2-U
40
Holmqvist
AS
,
Moëll
C
,
Hjorth
L
,
Lindgren
A
,
Garwicz
S
,
Wiebe
T
, et al.
Increased health care utilization by survivors of childhood lymphoblastic leukemia is confined to those treated with cranial or total body irradiation: a case cohort study. BMC Cancer. 2014;14(1):419. https://doi.org/10.1186/1471-2407-14-419
41
Rebholz
CE
,
Reulen
RC
,
Toogood
AA
,
Frobisher
C
,
Lancashire
ER
,
Winter
DL
, et al.
Health care use of long-term survivors of childhood cancer: the British Childhood Cancer Survivor Study. J Clin Oncol. 2011;29(31):4181–8. https://doi.org/10.1200/JCO.2011.36.5619
42
Blaauwbroek
R
,
Barf
HA
,
Groenier
KH
,
Kremer
LC
,
van der Meer
K
,
Tissing
WJ
, et al.
Family doctor-driven follow-up for adult childhood cancer survivors supported by a web-based survivor care plan. J Cancer Surviv. 2012;6(2):163–71. https://doi.org/10.1007/s11764-011-0207-5
43
Blaauwbroek
R
,
Tuinier
W
,
Meyboom-de Jong
B
,
Kamps
WA
,
Postma
A
. Shared care by paediatric oncologists and family doctors for long-term follow-up of adult childhood cancer survivors: a pilot study. Lancet Oncol. 2008;9(3):232–8. https://doi.org/10.1016/S1470-2045(08)70034-2
44
Singer
S
,
Gianinazzi
ME
,
Hohn
A
,
Kuehni
CE
,
Michel
G
. General practitioner involvement in follow-up of childhood cancer survivors: a systematic review. Pediatr Blood Cancer. 2013;60(10):1565–73. https://doi.org/10.1002/pbc.24586
45
Nathan
PC
,
Daugherty
CK
,
Wroblewski
KE
,
Kigin
ML
,
Stewart
TV
,
Hlubocky
FJ
, et al.
Family physician preferences and knowledge gaps regarding the care of adolescent and young adult survivors of childhood cancer. J Cancer Surviv. 2013;7(3):275–82. https://doi.org/10.1007/s11764-013-0271-0
46
Blaauwbroek
R
,
Zwart
N
,
Bouma
M
,
Meyboom-de Jong
B
,
Kamps
WA
,
Postma
A
. The willingness of general practitioners to be involved in the follow-up of adult survivors of childhood cancer. J Cancer Surviv. 2007;1(4):292–7. https://doi.org/10.1007/s11764-007-0032-z
47
Suh
E
,
Daugherty
CK
,
Wroblewski
K
,
Lee
H
,
Kigin
ML
,
Rasinski
KA
, et al.
General internists’ preferences and knowledge about the care of adult survivors of childhood cancer: a cross-sectional survey. Ann Intern Med. 2014;160(1):11–7. https://doi.org/10.7326/M13-1941
48
Poplack
DG
,
Fordis
M
,
Landier
W
,
Bhatia
S
,
Hudson
MM
,
Horowitz
ME
. Childhood cancer survivor care: development of the Passport for Care. Nat Rev Clin Oncol. 2014;11(12):740–50. https://doi.org/10.1038/nrclinonc.2014.175
49Lack P. Ein Pass für das Leben nach dem Krebs. Basel: Childhood Cancer Switzerland; 2016.
50Niederer A. Leben nach dem Krebs - Neuer Pass soll Nachsorge verbessern. Zurich: NZZ; 2016.