Impact of growing cohorts of adults with congenital heart disease on clinical workload: a 20-year experience at a tertiary care centre
DOI: https://doi.org/10.4414/smw.2017.14443
Maria
Padrutt, Isabelle
Bracher, Francesca
Bonassin, Bruno Santos
Lopes, Christiane
Gruner, Simon F.
Stämpfli, Thomas
Wolber, Oliver
Kretschmar, Angela
Oxenius, Gabriella
De Pasquale, Theresa
Seeliger, Thomas F.
Lüscher, Christine Attenhofer
Jost, Matthias
Greutmann
Department of Cardiology, University Heart Centre, Zurich,
Impact of growing cohorts of adults with congenital heart disease on clinical workload: a 20-year experience at a tertiary care centre
Summary
BACKGROUND
Population based studies show a steady increase in adult patients with congenital heart defects. The aim of this study was to assess the evolution of such a patient cohort and its burden on clinical care at a dedicated tertiary care centre.
METHODS
All patients with congenital heart disease followed up by a dedicated multidisciplinary team at our institution were identified (n = 1725). Disease characteristics, the increase in patient numbers and interventions and the increase in selected complications were analysed and compared between the first (1996–2005) and second (2006–2015) decades of the study period.
RESULTS
Between the two decades of the study period, the number of patients in follow-up increased by 109%, the number of patients who died or underwent transplantation more than doubled and the number of outpatient visits increased by 195%. One fourth of all patients underwent at least one surgical procedure and 14% had at least one percutaneous intervention. The increase in surgical procedures between the two decades was 27% and the increase in percutaneous interventions 159%. Between the two decades the number of patients requiring direct current cardioversion increased from 32 to 95 (+197%), the number of patients requiring admission for infective endocarditis increased from 7 to 29 (+314%) and the number of women followed up during pregnancy increased from 18 to 115 (+539%).
CONCLUSION
As a result of the increasing number and complexity of adult survivors with congenital heart disease more resources will be needed to cope with the demands of this novel cohort of complex patients in adult cardiology.
Background
Congenital heart defects are the most common birth defects, affecting about 1% of newborns [1–3]. Only a few decades ago the majority of affected patients with complex defects died in early childhood [1]. This has changed dramatically with the invention of open-heart surgery and improved cardiology care. In the contemporary era, about 90% of affected children are expected to survive to adulthood [4]. This has led to rapidly increasing new cohorts of adult survivors with congenital heart disease [5]. These adults are not cured and many remain at high risk of cardiovascular complications [6, 7]. Patients with defects of moderate or great disease complexity are at particularly increased risk of premature death as young adults [8]. Specialist care of adults with congenital heart disease in multidisciplinary tertiary care centres has been shown to improve outcomes and is thus recommended by international guidelines [9–13].
The impact of increasing patient numbers and recommended specialist care of these patients on the workload at specialised tertiary care centres has not been well studied. Such data may be important to help healthcare authorities and hospital administrations to allocate appropriate resources to cope with the needs of this novel group of complex patients in adult cardiology.
The aims of this study were, therefore, to describe the evolution of cohorts of adults with congenital heart disease at a single tertiary care centre over a 20-year period and to analyse the impact of increasing patient numbers on the workload of specialist care teams.
Methods
Patient cohorts
All patients who had been followed up by a dedicated team of specialists for adult congenital heart disease at a single tertiary care centre between 1996 and 2015 were identified from the clinical database. The evolution of patient numbers and the characteristics of the heart defects were reported. Defects were classified in accordance with previously published disease classification; simple defects, defects of moderate complexity and defects of great complexity were distinguished [1]. Patients with Marfan syndrome and related disorders, as well as selected patients with noncongenital heart disease followed up by the dedicated team of specialists in congenital heart disease (mainly pregnant women with acquired heart disease), were also included into the study cohort as they contributed to the increasing workload. The rationale for including pregnant women with acquired heart disease was the fact that at most centres care for these patients is provided by the dedicated congenital heart disease teams.
Within this patient cohort we analysed the number of surgical and interventional procedures that were performed at our institution during the study period. As surrogates for the complexity of patient care, we analysed the number of patients requiring direct current cardioversion and the number of patients requiring admission for infective endocarditis. Furthermore, we reported the increasing number of women who were followed up during pregnancy, as their care increases the overall in- and outpatient workload substantially.
Changes in patient numbers or numbers of procedures over time are reported either as changes from the first to the second decade of the study period (1996–2005 vs 2006–2015), or as changes between 5-year periods (1996–2000, 2001–2005, 2006–2010 and 2011–2015) as more appropriate and illustrative for individual characteristics.
The study was approved by the local ethics board.
Statistics
Continuous data are presented as mean ± standard deviation or median with range as appropriate. Categorical data are presented as number with percentage. For comparison between groups, chi squared tests, Fisher’s exact test, Student’s t-test or the Mann-Whitney test was used, as appropriate. Two-sided p-values <0.05 were considered statistically significant.
Results
Patient cohorts
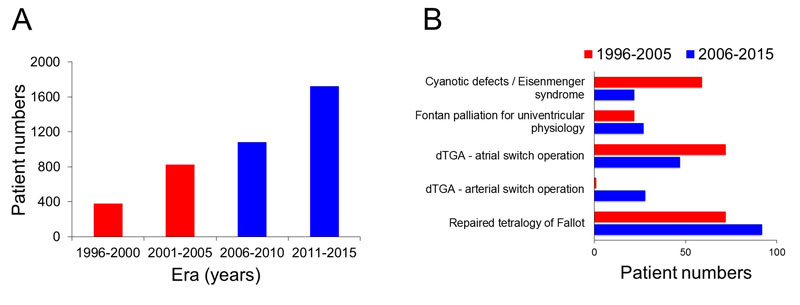
A total of 2045 patients with congenital heart disease were identified from our administrative database. We excluded 250 patients who were followed up by general cardiologists not specialised in adult congenital heart disease. These patients had mainly simple defects (73%), particularly isolated aortic valve disease (41%), or small or repaired shunt lesions (24%). We also excluded 70 patients who were referred for surgery only and had never been seen in the outpatient clinic. This left 1725 patients in the study cohort, of whom 1371 (79%) were under the exclusive care of the team at our centre and 354 (21%) were under shared care with nonspecialist cardiologists in private practice or local hospitals. Within the study cohort, 912 of 1725 patients (53%) were male. The median age at first visit was 26.4 (10.9–82.1) years. Only two patients were younger than 16 years at their first clinic visit, both referred for family screening. The majority of patients had defects of moderate or great complexity. The overall proportion of patients with mild, moderate and great disease complexity did not significantly change over time. Type and frequency of defects are summarised in table 1 and the increase in patient numbers during the study period is illustrated in figure 1, panel A. The number of patients under follow-up increased from 827 to 1725 (+109%) between the first and the second decade of the study period and from 379 to 1725 (+355%) from the first (1996–2000) to the last 5-year period (2011–2015) of the study. Changes in referral patterns of selected important congenital heart defects during the study period are depicted in figure 1, panel B. The median age at last clinic visit was 32.5 (16.0–88.6) years.
Table 1 Type and frequency of congenital heart defects within the study cohort.
|
Type of defect
|
n (%)
|
Simple defects
n = 600 (35%) |
|
| Isolated aortic valve disease |
162 (9.4) |
| Isolated mitral valve disease |
41 (2.4) |
| Small secundum type atrial septal defect |
39 (2.3) |
| Repaired secundum type atrial septal defect |
85 (4.9) |
| Repaired sinus venosus defect |
16 (0.9) |
| Small ventricular septal defect |
51 (3.0) |
| Repaired ventricular septal defect |
52 (3.0) |
| Small patent ductus arteriosus |
14 (0.8) |
| Isolated pulmonary valve stenosis |
47 (2.7) |
| Non-congenital heart disease*
|
59 (3.4) |
| Left ventricular non-compaction |
19 (1.1) |
| Other defects of mild complexity |
21 (1.2) |
Defects of moderate complexity
n = 749 (43%) |
|
| Sinus venosus defect |
13 (0.8) |
| Coarctation of the aorta |
127 (7.4) |
| Ebstein anomaly |
38 (2.2) |
| Infundibular pulmonary stenosis |
28 (1.6) |
| Atrioventricular septal defect |
77 (4.5) |
| Supravalvar aortic stenosis |
11 (0.6) |
| Subvalvar aortic stenosis |
20 (1.2) |
| Hypertrophic cardiomyopathy |
16 (0.9) |
| Repaired tetralogy of Fallot |
164 (9.5) |
| Repaired double outlet right ventricle |
18 (1.0) |
| Marfan syndrome and related disorders |
50 (2.9) |
| Shone’s complex†
|
19 (1.1) |
| Other defects of moderate complexity |
162 (9.4) |
Defects of great complexity
n = 376 (22%) |
|
| Repaired pulmonary atresia |
28 (1.6) |
| Cyanotic heart disease |
31 (1.8) |
| Eisenmenger syndrome |
50 (2.9) |
| Fontan procedure for univentricular heart |
49 (2.8) |
| Transposition of the great arteries - atrial switch operation |
119 (6.9) |
| Transposition of the great arteries - arterial switch operation |
29 (1.7) |
| Transposition of the great arteries - Rastelli repair |
8 (0.5) |
| Congenitally corrected transposition of the great arteries |
26 (1.5) |
| Common arterial trunk |
10 (0.6) |
| Other defects of great complexity |
26 (1.5) |
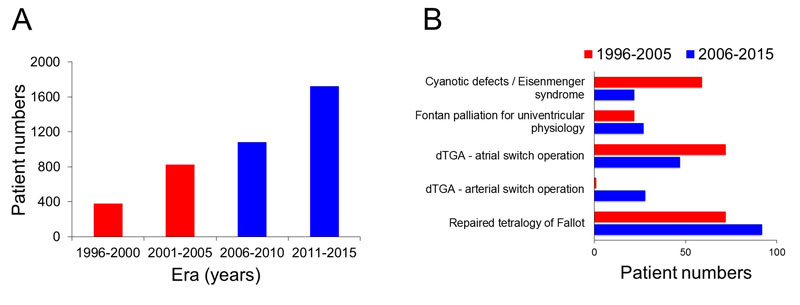
Figure 1 Evolution of patient numbers during the study period (red bars represent the first and blue bars the second decade of the study period). Panel A: Numbers of patients at the end of each 5-year era of the study period. Panel B: Comparison of newly referred patients with selected congenital heart defects, between the first and second decade of the study period.
dTGA = d-transposition of the great arteries
Evolution of cardiac surgery and percutaneous interventions during the study period
During the 20-year study period, 432 of 1725 patients (25%) had at least one cardiac surgical procedure at our institution and 115 patients (7%) had more than one and up to five surgical procedures. The total number of heart operations was 601, and 183 of the operations using cardiopulmonary bypass were redo-surgery. The number of surgical procedures within the first decade of the study period was 264, compared with 335 within the second decade of the study period, an increase of 27%.
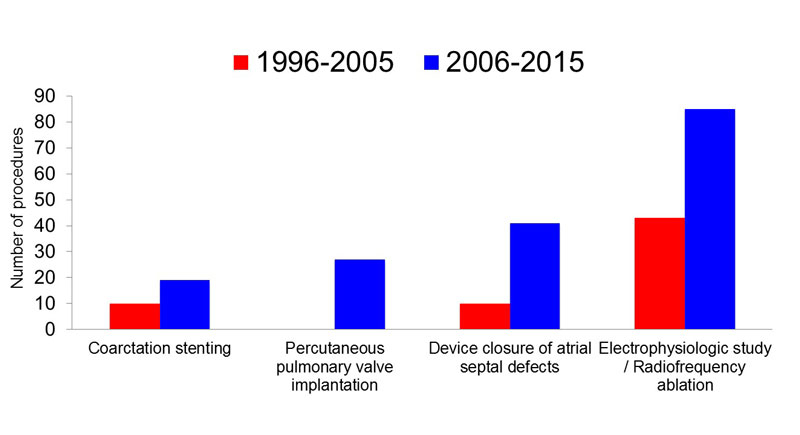
The increase in percutaneous interventions was even more pronounced. During the study period, 233 patients (14%) had at least one percutaneous intervention and 47 patients (3%) had more than one and up to five interventions. The number of percutaneous interventions increased from 84 procedures within the first decade of the study period to 218 procedures within the second decade of the study period, an increase of 159%. The most common procedures were electrophysiological studies / radiofrequency ablations (128 procedures), device closure of atrial septal defects (51 procedures), coarctation stenting (29 procedures) and percutaneous pulmonary valve implantation (27 procedures). The increase among these frequent procedures during the study period is illustrated in figure 2.
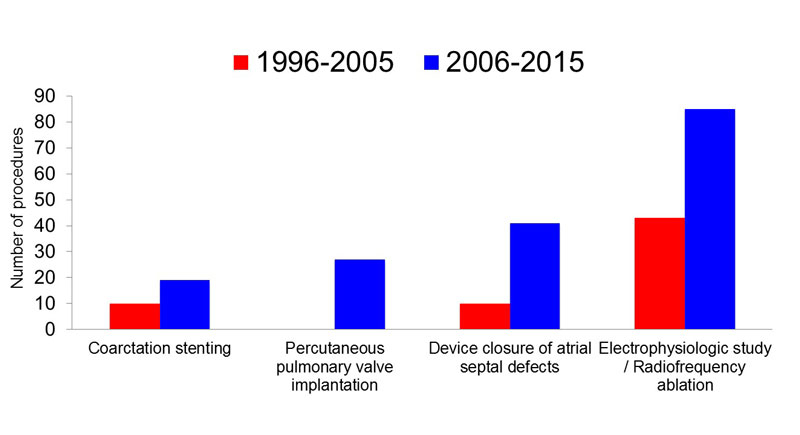
Figure 2 Increase in number of selected procedures between the first and the second decade of the study period.
Evolution of cardiac outpatient visits, morbidity and mortality during the study period
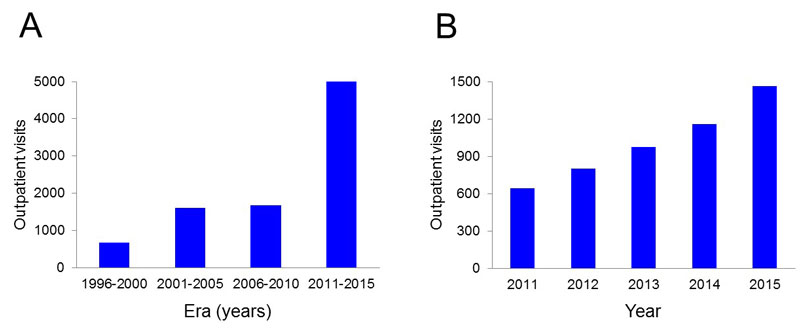
The number of outpatient visits increased constantly during the study period, as depicted in figure 3.
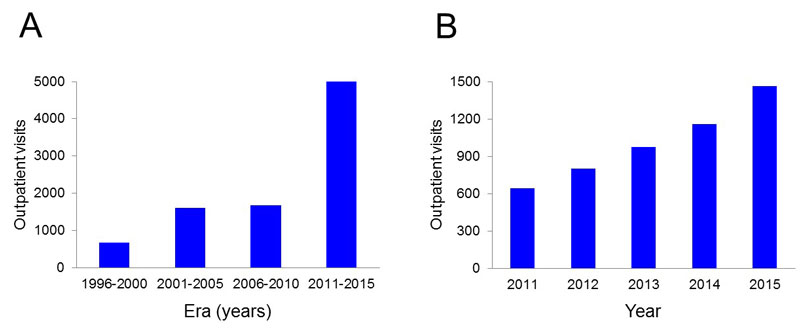
Figure 3 Number of outpatient visits during the study period. Panel A: Number of outpatient visits per 5-year intervals. Panel B: Number of outpatient visits per year over the last 5 years of the study period.
While the number of patients under care increased by 109% from 2005 to 2015, the number of outpatient visits increased by 195%. Of patients seen within the last 5 years of the study period, 68% had moderate or great disease complexity, which reflects the disease complexity within the entire study cohort (65% of patients with lesions of moderate or great complexity). During the study period, follow-up policy and frequency of follow-up visits for the different congenital heart defects had not changed at our centre and followed recommended guidelines. The reason for the increasing numbers of outpatient visits are mainly increasing numbers of patients under follow-up, as illustrated in figure 1, as well as increasing numbers of unplanned and emergency visits. This is indirectly illustrated by an increasing proportion of patients requiring electrical cardioversion and patients suffering from infective endocarditis (see next paragraph).
A total of 92 patients (5%) died or underwent heart transplantation during the study period. Median age at death or transplantation was 42.9 (17.4–88.6) years. The median age at death remained unchanged over the study period. The number of patients who died more than doubled between the first decade of the study period (29 deaths) and the second decade (63 deaths). The majority of patients died from their cardiac disease. Of those for whom the cause of death was known (83%), sudden death (39%), heart failure (17%) and perioperative death (12%) were the most common causes. Among patients who died during the study period, 53% had defects of great, 27% of moderate and 20% of simple complexity. Among deceased patients, those with a diagnosis of Eisenmenger syndrome (16%), atrial switch operations for transposition of the great arteries (12%), unrepaired cyanotic defects (9%) and patients with repaired tetralogy of Fallot (9%) contributed most to the overall mortality burden. Among individual disease entities, mortality was highest in patients with Eisenmenger syndrome (30%), followed by unrepaired cyanotic defects (26%), patients with congenitally corrected transposition of the great arteries (19%), patients after atrial switch operations (9%), Fontan palliation (6%) and repaired tetralogy of Fallot (5%).
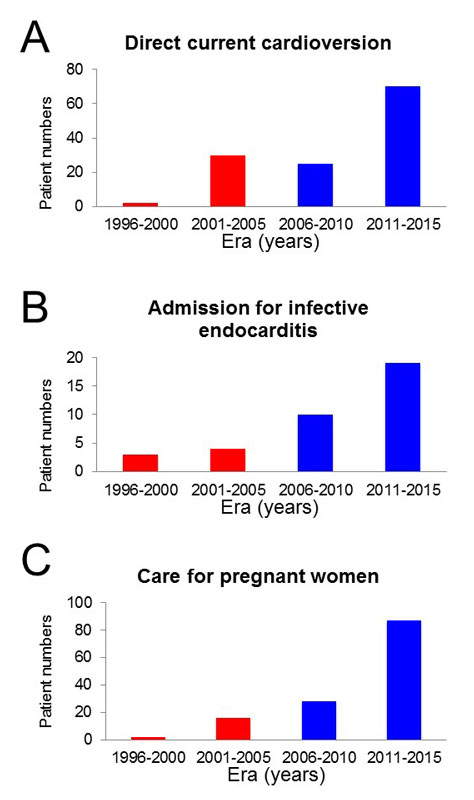
Figure 4 depicts the number of direct current cardioversions, the number of admissions for infective endocarditis and the number of women followed during pregnancy during the study period, which act as surrogates for the increasing morbidity and complexity among adults within our cohort. The majority of women followed up during pregnancy were patients with repaired congenital heart defects (94%); a few had cardiomyopathy or acquired valvar heart disease.
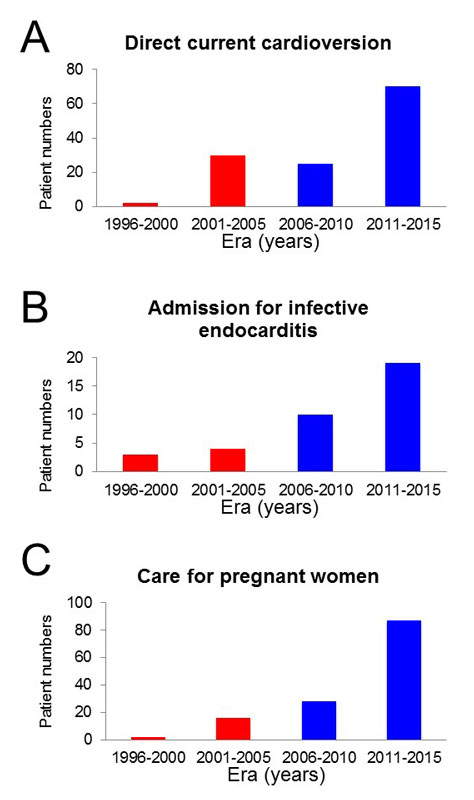
Figure 4 Number of direct current cardioversions (panel A), number of admissions for infective endocarditis (panel B) and number of women followed during pregnancy (panel C).
Within the first decade of the study period, 3.1% of patients under follow-up required a cardioversion versus 5.4% of patients in the second decade, a relative increase of 74%. The frequency of patients with infective endocarditis increased from 1.1% within the first decade to 1.7% in the second decade of the study period, a relative increase of 54%. Among patients suffering from infective endocarditis, there was a trend towards higher disease complexity compared with those without endocarditis (proportion of patients with defects of moderate/great complexity 81% in the group with endocarditis vs 65% in those without endocarditis, p = 0.061). Patients requiring electrical cardioversion had lesions of moderate/great disease complexity more frequently than those not requiring electrical cardioversion (82% vs 65%, p = 0.01). There was no difference in distribution of disease complexity among women followed up during a pregnancy (proportion of patients with defects of moderate/great complexity 58% in the group of pregnant women vs 66% of those without pregnancy, p = 0.12).
Discussion
As a result of successful surgical repair and palliation most patients born with congenital heart disease now survive to adulthood, and recent population-based studies have shown a rapidly emerging and growing cohort of adults with congenital heart disease [4, 5]. After surgical repair, most patients go through a stable period, with a low risk of morbidity and mortality during childhood and adolescence [14]. These patients are, however, not cured. Many remain at substantially increased risk of cardiac morbidity and have an increased risk of premature death as young and middle-aged adults [6–8].
In this study we depicted the evolution of the adult patient population with congenital heart disease at a tertiary care centre over a 20-year period, and the impact of these growing patient numbers on workload for the multidisciplinary teams. The increasing workload is driven by both the increasing number of patients in follow-up and the increasing morbidity risks with the ageing of these cohorts, as illustrated by the increasing proportion of patients requiring cardioversion or suffering from infective endocarditis. Previous work by Marelli and colleagues, providing population based data from Canada, has shown an increase in the prevalence of adults with congenital heart disease of 57% between the years 2000 and 2010 [5]. During the same period, the number of patients followed up at our centre increased by 186%, followed by an additional increase of 59% during the subsequent 5 years between 2011 and 2015. This is important as it shows that the number of patients followed up at tertiary care centres increased more rapidly than the overall prevalence of adults with congenital heart disease. This probably reflects adherence to guideline recommendations that adults with congenital heart disease should be followed up by multidisciplinary teams at dedicated tertiary care centres [11–13]. Recent studies have suggested improved outcomes for patients followed up at tertiary care centres [9, 10].
Increasing morbidity and mortality
A large proportion of patients in our cohort required surgical or interventional procedures during adult life; hence, the numbers of operations, and particularly the number of percutaneous interventions, steadily increased. This underscores the notion that many adults with repaired congenital heart defects have important residual lesions requiring redo-interventions in adulthood. Particularly striking is the increasing number of electrophysiological procedures and radiofrequency ablations, as well as the increasing number of direct current cardioversions. This highlights the high prevalence of arrhythmias in adults with congenital heart disease, by far the most common cardiovascular complication in this patient group [7]. The number of patients within our cohort who died more than doubled between the first and the second decade of the study period. This is an important marker of increasing workload; because most patients who died had multiple previous hospital admissions and, typically, intensive in- and outpatient care before their demise, these patients require a great deal of personnel and time resources [15]. Given that the majority of patients within our cohort were still young at the end of the study period, it is likely that, with the ageing of these cohorts, the number of young and middle-aged adults reaching the end stage of their disease will rapidly increase [8]. Heart failure was among the leading causes of death in our cohort. With ageing of the patient cohorts, heart failure will certainly become much more frequent and will substantially contribute to in- and outpatient workload. Heart transplantation or advanced heart failure treatment (including ventricular assist devices) may be an option for some of these patients, but for many there will probably be no such option and end-of-life support for patients and their families will become an important part of specialist care [8, 16, 17]. Patients dying under our care will thus substantially add to the overall workload of our in- and outpatient services. Given that most women survive to childbearing age, the number of women who embark on pregnancy is steadily increasing. Depending on the type of defect, residual lesions and other individual disease characteristics, these women may be at increased risk for complications during pregnancy and require intensive counselling and follow-up during pregnancy, as well as in the peri- and postpartum periods [18].
There has been a rapid increase in hospital admissions of patients with infective endocarditis. With the increasing number of patients who undergo implantation of prosthetic heart valves, particularly in the pulmonary position, the cohort of patients suffering from infective endocarditis will probably continue to further increase in the future [19].
Evolution of adult patient cohorts
As expected, major differences in the evolution of cohorts with different types of congenital heart defects was observed. As most cyanotic defects have been successfully repaired or palliated since the 1980s, only few patients with unrepaired cyanotic defects entered the adult cohort after the year 2000. The same is true for patients with Eisenmenger syndrome, which is defined by irreversible pulmonary hypertension as the consequence of an unrepaired shunt lesion with eventual shunt reversal. As patients with shunt lesions are usually detected early in life and operated on in a timely manner, Eisenmenger syndrome in young adults has become rare. This observation supports findings from previous studies [8].
Interestingly, the number of patients with Fontan palliation who entered the adult cohort was almost as high within the first decade of the study period as in the second decade. This is surprising, as the Fontan palliation for univentricular hearts was first proposed in the 1970s and widely introduced into the surgical armamentarium only in the 1980s. The high number of Fontan patients who entered the adult cohort at our institution before 2000 is probably a consequence of the fact that the surgical programme at our institution was led by Professor Åke Senning, one of the pioneers in surgical repair of congenital heart disease, and thus the Fontan palliation was introduced relatively early at our institution.
As expected, patients with repaired transposition of the great arteries who entered the adult cohort within the second decade of the study period had mainly undergone arterial switch repair, which replaced the atrial switch repair (Senning or Mustard procedures) in the 1980s. The number of patients with repaired tetralogy of Fallot remained relatively unchanged between the first and the second decade of the study period.
Limitations
This was a retrospective analysis of patients identified from our clinical database. Patient with erroneous diagnostic coding may thus have been missed. We restricted our analysis to patients followed up by the dedicated multi-disciplinary team for adults with congenital heart disease at our institution. Patients followed up by general cardiologists within tertiary care centres may add to the overall burden of patient care and further increase the need for resources. Some of the fluctuations of patient numbers, number of procedures and outpatient visits may reflect changes in staff over the 20-year study period.
Although the experience at our centre probably mirrors the experience at other tertiary care centres, different referral patterns and different organisation of care will inevitably lead to differences in the evolution of patient cohorts.
Conclusions
The increasing number of adult survivors with congenital heart disease leads to an over-proportional increase in patients followed at dedicated tertiary care centres. These patients are not cured, have a high risk of cardiovascular complications, many require redo-surgery or interventions and many have an increased risk of premature death. There is and will be a rapidly increasing need for more resources to cope with the increasing workload for this new cohort of complex patients in adult cardiology. Our data may help healthcare authorities and hospital administrations to allocate appropriate resources.
Authors’ contribution
Maria Padrutt and Isabelle Bracher contributed equally to the manuscript
References
1
Warnes
CA
,
Liberthson
R
,
Danielson
GK, Jr
,
Dore
A
,
Harris
L
,
Hoffman
JI
, et al.
Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37(5):1170–5. https://doi.org/10.1016/S0735-1097(01)01272-4
2
Hoffman
JI
,
Kaplan
S
. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39(12):1890–900. https://doi.org/10.1016/S0735-1097(02)01886-7
3
van der Linde
D
,
Konings
EE
,
Slager
MA
,
Witsenburg
M
,
Helbing
WA
,
Takkenberg
JJ
, et al.
Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. 2011;58(21):2241–7. https://doi.org/10.1016/j.jacc.2011.08.025
4
Moons
P
,
Bovijn
L
,
Budts
W
,
Belmans
A
,
Gewillig
M
. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. 2010;122(22):2264–72. https://doi.org/10.1161/CIRCULATIONAHA.110.946343
5
Marelli
AJ
,
Ionescu-Ittu
R
,
Mackie
AS
,
Guo
L
,
Dendukuri
N
,
Kaouache
M
. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014;130(9):749–56. https://doi.org/10.1161/CIRCULATIONAHA.113.008396
6
Greutmann
M
,
Tobler
D
. Changing epidemiology and mortality in adult congenital heart disease: looking into the future. Future Cardiol. 2012;8(2):171–7. https://doi.org/10.2217/fca.12.6
7
Kaemmerer
H
,
Fratz
S
,
Bauer
U
,
Oechslin
E
,
Brodherr-Heberlein
S
,
Zrenner
B
, et al.
Emergency hospital admissions and three-year survival of adults with and without cardiovascular surgery for congenital cardiac disease. J Thorac Cardiovasc Surg. 2003;126(4):1048–52. https://doi.org/10.1016/S0022-5223(03)00737-2
8
Greutmann
M
,
Tobler
D
,
Kovacs
AH
,
Greutmann-Yantiri
M
,
Haile
SR
,
Held
L
, et al.
Increasing mortality burden among adults with complex congenital heart disease. Congenit Heart Dis. 2015;10(2):117–27. https://doi.org/10.1111/chd.12201
9
Mylotte
D
,
Pilote
L
,
Ionescu-Ittu
R
,
Abrahamowicz
M
,
Khairy
P
,
Therrien
J
, et al.
Specialized adult congenital heart disease care: the impact of policy on mortality. Circulation. 2014;129(18):1804–12. https://doi.org/10.1161/CIRCULATIONAHA.113.005817
10
Wray
J
,
Frigiola
A
,
Bull
C
; Adult Congenital Heart disease Research Network (ACoRN). Loss to specialist follow-up in congenital heart disease; out of sight, out of mind. Heart. 2013;99(7):485–90. https://doi.org/10.1136/heartjnl-2012-302831
11
Silversides
CK
,
Marelli
A
,
Beauchesne
L
,
Dore
A
,
Kiess
M
,
Salehian
O
, et al.
Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: executive summary. Can J Cardiol. 2010;26(3):143–50. https://doi.org/10.1016/S0828-282X(10)70352-4
12
Warnes
CA
,
Williams
RG
,
Bashore
TM
,
Child
JS
,
Connolly
HM
,
Dearani
JA
, et al.; American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease); American Society of Echocardiography; Heart Rhythm Society; International Society for Adult Congenital Heart Disease; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Develop Guidelines on the Management of Adults With Congenital Heart Disease). Developed in Collaboration With the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52(23):e143–263. https://doi.org/10.1016/j.jacc.2008.10.001
13
Baumgartner
H
,
Bonhoeffer
P
,
De Groot
NM
,
de Haan
F
,
Deanfield
JE
,
Galie
N
, et al.; Task Force on the Management of Grown-up Congenital Heart Disease of the European Society of Cardiology (ESC); Association for European Paediatric Cardiology (AEPC); ESC Committee for Practice Guidelines (CPG). ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010;31(23):2915–57. https://doi.org/10.1093/eurheartj/ehq249
14
Khairy
P
,
Ionescu-Ittu
R
,
Mackie
AS
,
Abrahamowicz
M
,
Pilote
L
,
Marelli
AJ
. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56(14):1149–57. https://doi.org/10.1016/j.jacc.2010.03.085
15
Tobler
D
,
Greutmann
M
,
Colman
JM
,
Greutmann-Yantiri
M
,
Librach
LS
,
Kovacs
AH
. End-of-life care in hospitalized adults with complex congenital heart disease: care delayed, care denied. Palliat Med. 2012;26(1):72–9. https://doi.org/10.1177/0269216311407694
16
Tobler
D
,
Greutmann
M
,
Colman
JM
,
Greutmann-Yantiri
M
,
Librach
LS
,
Kovacs
AH
. End-of-life in adults with congenital heart disease: a call for early communication. Int J Cardiol. 2012;155(3):383–7. https://doi.org/10.1016/j.ijcard.2010.10.050
17
Tobler
D
,
de Stoutz
N
,
Greutmann
M
. Supportive and palliative care for adults dying from congenital heart defect. Curr Opin Support Palliat Care. 2011;5(3):291–6. https://doi.org/10.1097/SPC.0b013e3283492aa3
18
Greutmann
M
,
Pieper
PG
. Pregnancy in women with congenital heart disease. Eur Heart J. 2015;36(37):2491–9. https://doi.org/10.1093/eurheartj/ehv288
19
O’Byrne
ML
,
Glatz
AC
,
Mercer-Rosa
L
,
Gillespie
MJ
,
Dori
Y
,
Goldmuntz
E
, et al.
Trends in pulmonary valve replacement in children and adults with tetralogy of fallot. Am J Cardiol. 2015;115(1):118–24. https://doi.org/10.1016/j.amjcard.2014.09.054