
Figure 1 Computed tomography image of periappendicular abscess after drainage.
DOI: https://doi.org/10.4414/smw.2017.14422
Acute appendicitis is one of the most critical causes of an “acute abdomen”, and appendectomy is the most common surgical intervention performed worldwide to treat “acute abdomen” [1]. Several recent studies have assessed conservative treatment with antibiotics for uncomplicated appendicitis [2–4], but the results have not indicated that conservative management is clearly superior to appendectomy. Thus, surgery remains the gold standard for uncomplicated appendicitis [2–4]. However, the treatment guidelines are less clear in cases of complicated appendicitis.
Perityphlitic abscess formation occurs in 2–7% of patients with perforated appendicitis, representing about 1% of all patients presenting with appendicitis [1, 5]. A surgical approach is generally recommended for patients in whom perityphlitic or appendicular abscess is associated with generalised peritonitis [6]. However, in cases without generalised peritonitis it is unclear whether the benefits of emergency appendectomy outweigh the potential benefits of a primarily conservative approach with antibiotics and drainage followed by an interval appendectomy (IA). Emergency appendectomy may be technically challenging in such patients, because of local inflammation. It may also be associated with an elevated risk of ileocaecal resection and postoperative complications [7–9]. A conservative approach, with radiologically guided drainage and antibiotic treatment as the first step and appendectomy as the second step, has the advantage of lower peri- and postoperative morbidity [7–9]. Although the conservative approach for perityphlitic abscess without generalised peritonitis is increasingly accepted in clinical settings, there is still little high-quality evidence to support its use in the literature.
In our department, we routinely carry out the two-step approach in patients with appendicitis and perityphlitic abscess formation but without generalised peritonitis. Our aim in the present study was to report our experience at a single centre by evaluating outcome and complications after the two-step procedure.
We retrospectively analysed data from the prospective inpatient database of our hospital for patients presenting with appendicitis from January 2007 to December 2015. We included data for all patients who were diagnosed with appendicitis and perityphlitic abscess (diameter ≥3 cm) but with no signs of general peritonitis and who underwent the following two-step treatment procedure. Step 1 comprised administration of intravenous antibiotics and, if feasible, radiologically guided abscess drainage (fig. 1). Intravenous antibiotics were followed by oral antibiotic treatment. Step 2 comprised elective IA. Although all eligible patients underwent the described treatment procedure, decisions such as the duration of intravenous and oral antibiotic treatment and the feasibility of drainage were made by the treating physicians and not dictated by a protocol. Diagnosis and drainage were performed with ultrasonography (US) or computed tomography (CT). We noted demographic data, duration of antibiotic treatment, duration of drainage, details about the surgical intervention, length of hospital stay, complications (in accordance with Dindo et al. [10]), and microbiological and histological findings. Based on our results and on a review of the current literature, we developed a decision flowchart for the management of patients with suspected complicated appendicitis (fig. 2).

Figure 1 Computed tomography image of periappendicular abscess after drainage.
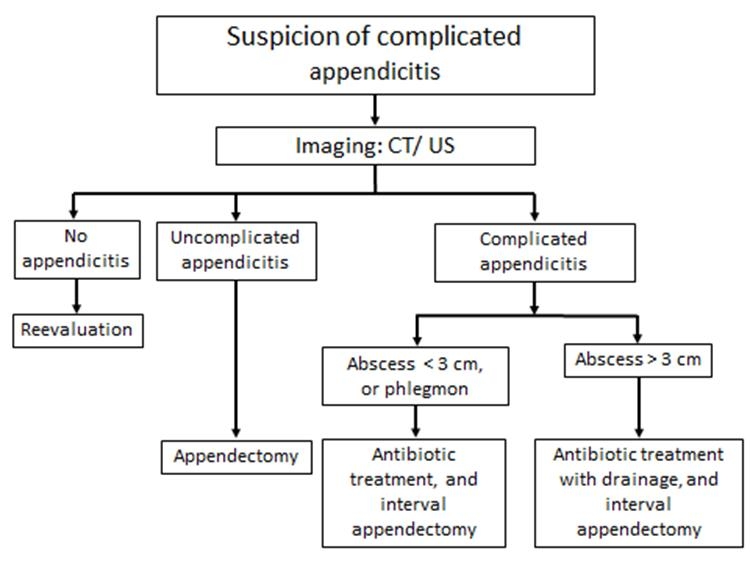
Figure 2 Decision flowchart for patients with suspected complicated appendicitis but without generalised peritonitis.
CT = computed tomography; US = ultrasound
During the study period, 15 out of a total of 1480 patients with acute appendicitis (1%) were eligible for the two-step procedure. Demographic and treatment data are summarised in table 1. A flow chart describing our management of suspected complicated appendicitis is shown in figure 2. The treating physicians made the decision to perform imaging studies when complicated appendicitis was suspected. Suspicion of complicated appendicitis was mainly based on the presence of one or more of the following conditions: deterioration of the general condition of the patient, presence of localised or generalised peritonitis, body temperature >38°C, symptoms for >48 hours, white blood cell count >11 × 109 cells/l and C-reactive protein concentration >50 mg/l. All 15 patients were initially treated with intravenous piperacillin-tazobactam, a broad-spectrum antibiotic agent. After they had received the results of the drain cultures, clinicians chose to continue treatment in 14 patients by administering antibiotics that were less broad spectrum for a median duration of 15 days (10–28 days): amoxicillin-clavulanate in five patients and ceftriaxone plus metronidazole in nine patients.
Table 1 Demographic data and baseline characteristics for patients with perityphlitic abscess formation (n = 15).
| Variable | |
|---|---|
| Age (years) | 43 (16–81) |
| Male gender | 9 (60%) |
| ASA class I | 10 (67%) |
| ASA class II | 5 (33%) |
| CRP (mg/l) | 123 (14–270) |
| WBC count (× 109 cells/l) | 15 (6–25) |
| Duration of symptoms (days) | 18 (2–30) |
| Percutaneously drainable | 12 (80%) |
| Drainage modality, CT | 11 (92%) |
| Drainage modality, US | 1 (8%) |
| Duration of drainage (days) | 6 (4–13) |
| Duration of antibiotic treatment (days) | 15 (10–28) |
ASA = American Association of Anesthesiology; CRP = C-reactive protein ; computed tomography (CT); ultrasound (US); WBC = white blood cell Data are given as total number and percentage for categorical variables, and as median and range for continuous variables.
Because of anatomical constraints or abscesses that could not be reached, clinicians decided that drainage was not feasible in three patients whose abscess diameters were 3–6 cm. These patients were treated with antibiotics alone and subsequent IA, and had an uneventful course. Drainage was feasible in 12 out of 15 patients (80%) who fulfilled the criteria for percutaneous drainage. There were no periprocedural complications. Median duration of drainage was 6 days (range 4–13 days), and the median length of hospital stay for step 1 was 7 days (range 5–14 days). In all patients, elective IA was performed after a median of 13 weeks (range 6–22 weeks). The median operative time was 70 minutes (range 23–135 minutes), and the median hospital stay for step 2 was 2 days (range 2–12 days).
Two complications occurred (13%); the first occurred after step 1, and the second occurred after step 2. In the first, abscess recurrence with new onset of appendicitis and perforation was noted 2 months after drainage. In this patient, initial intravenous antibiotic treatment was interrupted after 4 days owing to an allergic reaction and replaced early by oral antibiotic treatment. Initial treatment was successful with complete cessation of symptoms and normalisation of laboratory tests (white blood cell count 7 vs 18 × 109 cells/l, C-reactive protein <5 vs 208 mg/l). However, after the recurrence was detected, the patient underwent immediate laparoscopic appendectomy with an uneventful follow-up. Histopathological examination revealed acute inflammation with focal activity and perforation. In the second complication, the patient underwent reoperation after IA, where a stercolith in a small abscess was found. Following that, a second look operation and lavage had to be performed because of signs of early peritonitis on postoperative day two. A slight fibrinous peritonitis was found without any signs of perforation and the postoperative follow-up was then uneventful.
Histology did not reveal any malignancies in resected specimens. At follow-up outpatient examinations 2–6 weeks after IA, all patients were doing well without abdominal or other complaints.
Our study revealed that the two-step procedure described above for appendicitis with perityphlitic abscess formation was highly successful and associated with a low complication rate. This two-step procedure is also supported by recent meta-analyses, which showed that patients similar to those included in the present study were more likely to have postoperative complications or require colonic resection after emergency appendectomy [7–9].
Conservative initial treatment approaches toward perityphlitic abscess formation remain controversial in the literature. Recently, Mentula et al. reported a higher rate of uneventful recovery after initial appendectomy (90%) compared with conservative treatment (50%) [11]. However, in these 30 conservatively treated patients the approach differed from our procedure in that we did not attempt to drain in two patients (7%). Mentula et al. did not succeed in introducing drainage in nine patients (30%), and punctured abscesses without leaving a drain in place in 16 patients (50%) [11]. In contrast to this previous report, in which there was a low rate of drainage left in place (10%) [11], 80% of our patients underwent drainage. Additionally, Mentula et al. [11] included patients with abscesses as small as 2 cm in diameter, whereas in our patient cohort only patients with abscesses ≥3 cm were included.
In our study, two patients experienced complications, which were classified as grade IIIb in accordance with the Dindo–Clavien classification [10]. The first complication was a recurrence of appendicitis with a new perforation; thus, 1 out of 15 (7%) patients who initially underwent successful conservative treatment had recurrent appendicitis and abscess formation. This result is comparable to that of other reports [7, 9] and is better than the results reported by Mentula et al., who had recurrence rates of 27% and 10% for conservative and surgical treatment, respectively [11]. The second complication was a second-look operation after IA due to early peritonitis after a stercolith in a small abscess was found at the initial operation. Although IA is supported by most (53–75%) surgeons [12, 13], in the literature its necessity remains a topic of controversy. IA following initial conservative treatment has been associated with an elevated morbidity of 10–12% in studies that included patients who initially underwent conservative treatment for complicated appendicitis followed by IA [7, 14]. However, these morbidity rates may have been overestimated since there were marked differences among studies and protocols, some of which included patients who did not undergo drainage or who underwent open appendectomy. The morbidity rate (7%) of IA in the present study was lower than others in the literature [7, 14], suggesting that drainage together with laparoscopic IA might be associated with lower morbidity. Moreover, our results are confirmed by those of You et al., who used a similar protocol and also reported only one complication (7%) out of 15 patients who underwent laparoscopic IA after drainage [15].
An important point to address is appendicular neoplasm as a cause of complicated appendicitis. Carpenter et al. found a neoplasm rate of 28% in patients >40 years of age who underwent IA for complicated appendicitis [16]. Two other studies also found considerable risks of appendicular malignancy, of 29% and 12%, respectively, associated with IA after complicated appendicitis [17, 18]. In view of these results and the reported low morbidity associated with IA, the risk of malignancy should be considered and IA evaluated, especially in patients >40 years of age. In order to assess the exact risk of underlying neoplasm, larger studies using the two-step procedure have to be performed [19].
Compared with previous studies, in our study the frequency of patients with perityphlitic abscess formation who were eligible for the two-step procedure was slightly lower [7–9]. However, the cited studies evaluated phlegmon formation as well as abscesses of various sizes [7–9]. We excluded patients with perityphlitic phlegmons and abscesses with a diameter of <3 cm. This patient selection seems justified, because smaller abscesses can be treated successfully with antibiotics alone [20–22]. However, the monocentric retrospective setting and our strict patient selection criteria resulted in relatively few cases, which may somewhat decrease the strength of our conclusions.
We found that the median length of hospital stay for the first step of the procedure was 7 days, which is in accordance with the literature [7, 15, 23]. However, recent reports suggest that shortened antibiotic regimens may be appropriate in cases in which the source of infection is adequately controlled [24]. The median length of hospital stay after IA in our study was 2 days, which is relatively low compared with other reports [14, 15, 23]. Limitations of the present study include its retrospective, single-centre design. Moreover, the number of patients who met the inclusion criteria was relatively low. However, our results are consistent with those reported in the literature with respect to the safety and efficacy of this type of two-step approach. A prospective, multicentre evaluation in Switzerland is planned to confirm the superiority of our proposed two-step procedure (see fig. 2). In conclusion, management of appendicular abscesses ≥3 cm by conservative treatment is highly successful. In the view of a potentially increased rate of appendicular neoplasm in combination with abscess formation, the role of interval appendectomy has to be evaluated in larger trials.
The authors listed above certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
1 Grundmann RT , Petersen M , Lippert H , Meyer F . Das akute (chirurgische) Abdomen – Epidemiologie, Diagnostik und allgemeine Prinzipien des Managements. [The acute (surgical) abdomen - epidemiology, diagnosis and general principles of management]. Z Gastroenterol. 2010;48(6):696–706. . Article in German.https://doi.org/10.1055/s-0029-1245303
2 Mason RJ , Moazzez A , Sohn H , Katkhouda N . Meta-analysis of randomized trials comparing antibiotic therapy with appendectomy for acute uncomplicated (no abscess or phlegmon) appendicitis. Surg Infect (Larchmt). 2012;13(2):74–84. https://doi.org/10.1089/sur.2011.058
3 Rocha LL , Rossi FM , Pessoa CM , Campos FN , Pires CE , Steinman M . Antibiotics alone versus appendectomy to treat uncomplicated acute appendicitis in adults: what do meta-analyses say? World J Emerg Surg. 2015;10(1):51. https://doi.org/10.1186/s13017-015-0046-1
4 Varadhan KK , Humes DJ , Neal KR , Lobo DN . Antibiotic therapy versus appendectomy for acute appendicitis: a meta-analysis. World J Surg. 2010;34(2):199–209. https://doi.org/10.1007/s00268-009-0343-5
5 Bradley EL, 3rd , Isaacs J . Appendiceal abscess revisited. Arch Surg. 1978;113(2):130–2. https://doi.org/10.1001/archsurg.1978.01370140020003
6 Sartelli M , Viale P , Catena F , Ansaloni L , Moore E , Malangoni M , et al. 2013 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2013;8(1):3. https://doi.org/10.1186/1749-7922-8-3
7 Andersson RE , Petzold MG . Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246(5):741–8. https://doi.org/10.1097/SLA.0b013e31811f3f9f
8 Olsen J , Skovdal J , Qvist N , Bisgaard T . Treatment of appendiceal mass--a qualitative systematic review. Dan Med J. 2014;61(8):A4881.
9 Simillis C , Symeonides P , Shorthouse AJ , Tekkis PP . A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery. 2010;147(6):818–29. https://doi.org/10.1016/j.surg.2009.11.013
10 Dindo D , Demartines N , Clavien PA . Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae
11 Mentula P , Sammalkorpi H , Leppäniemi A . Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg. 2015;262(2):237–42. https://doi.org/10.1097/SLA.0000000000001200
12 Ahmed I , Deakin D , Parsons SL . Appendix mass: do we know how to treat it? Ann R Coll Surg Engl. 2005;87(3):191–5. https://doi.org/10.1308/1478708051649
13 Corfield L . Interval appendicectomy after appendiceal mass or abscess in adults: what is “best practice”? Surg Today. 2007;37(1):1–4. https://doi.org/10.1007/s00595-006-3334-2
14 Lai HW , Loong CC , Chiu JH , Chau GY , Wu CW , Lui WY . Interval appendectomy after conservative treatment of an appendiceal mass. World J Surg. 2006;30(3):352–7. https://doi.org/10.1007/s00268-005-0128-4
15 You KS , Kim DH , Yun HY , Jang LC , Choi JW , Song YJ , et al. The value of a laparoscopic interval appendectomy for treatment of a periappendiceal abscess: experience of a single medical center. Surg Laparosc Endosc Percutan Tech. 2012;22(2):127–30. https://doi.org/10.1097/SLE.0b013e318244ea16
16 Carpenter SG , Chapital AB , Merritt MV , Johnson DJ . Increased risk of neoplasm in appendicitis treated with interval appendectomy: single-institution experience and literature review. Am Surg. 2012;78(3):339–43.
17 Furman MJ , Cahan M , Cohen P , Lambert LA . Increased risk of mucinous neoplasm of the appendix in adults undergoing interval appendectomy. JAMA Surg. 2013;148(8):703–6. https://doi.org/10.1001/jamasurg.2013.1212
18 Wright GP , Mater ME , Carroll JT , Choy JS , Chung MH . Is there truly an oncologic indication for interval appendectomy? Am J Surg. 2015;209(3):442–6. https://doi.org/10.1016/j.amjsurg.2014.09.020
19 Botes SN , Ibirogba SB , McCallum AD , Kahn D . Schistosoma prevalence in appendicitis. World J Surg. 2015;39(5):1080–3. https://doi.org/10.1007/s00268-015-2954-3
20 Jeffrey RB, Jr , Federle MP , Tolentino CS . Periappendiceal inflammatory masses: CT-directed management and clinical outcome in 70 patients. Radiology. 1988;167(1):13–6. https://doi.org/10.1148/radiology.167.1.3347712
21 Siewert B , Tye G , Kruskal J , Sosna J , Opelka F , Raptopoulos V , et al. Impact of CT-guided drainage in the treatment of diverticular abscesses: size matters. AJR Am J Roentgenol. 2006;186(3):680–6. https://doi.org/10.2214/AJR.04.1708
22 Zerem E , Salkic N , Imamovic G , Terzić I . Comparison of therapeutic effectiveness of percutaneous drainage with antibiotics versus antibiotics alone in the treatment of periappendiceal abscess: is appendectomy always necessary after perforation of appendix? Surg Endosc. 2007;21(3):461–6. https://doi.org/10.1007/s00464-006-9005-y
23 Brown CV , Abrishami M , Muller M , Velmahos GC . Appendiceal abscess: immediate operation or percutaneous drainage? Am Surg. 2003;69(10):829–32.
24 Sawyer RG , Claridge JA , Nathens AB , Rotstein OD , Duane TM , Evans HL , et al. Trial of short-course antimicrobial therapy for intraabdominal infection. N Engl J Med. 2015;372(21):1996–2005. https://doi.org/10.1056/NEJMoa1411162
The authors listed above certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.