Perinatal mental disorders in Switzerland: prevalence estimates and use of mental-health services
DOI: https://doi.org/10.4414/smw.2017.14417
Anke
Bergera, Nicole
Bachmannb, Andri
Signorellc, Rebekka
Erdind, Stephan
Oelhafena, Oliver
Reichc, Eva
Cignaccoa
aBern University of Applied Sciences, Health Department, Discipline of Research in Midwifery, Bern,
bUniversity of Applied Sciences and Arts Northwestern Switzerland, School of Social Work, Institute for Social Work and Health, Olten,
cHelsana Group, Department of Health Sciences, Zurich,
dZurich University of Applied Sciences, Winterthur,
Perinatal mental disorders in Switzerland: prevalence estimates and use of mental-health services
Summary
BACKGROUND
Perinatal mental disorders (PMDs) are the most common complication of pregnancy and the first postpartum year. Since PMD prevalence and use of mental-health services by perinatal women in Switzerland are unknown, we analysed existing health statistics.
METHODS
We used statistics from a large health insurance company, hospitals and freelance midwives. We assessed the annual rates of mental healthcare use in perinatal women (n = 13 969). We ascertained the annual rates of PMD treatment in obstetric inpatients (n = 89 699), and annual rates of PMD records by freelance midwives (n = 57 951). In 15 104 women who gave birth in 2012 or 2013, we assessed use of mental-healthcare before and during pregnancy, and in the postpartum year. For the same sample, we determined proportions of medication and consultation treatments. We used multiple regression analysis to estimate the influence of PMD on overall healthcare costs of mandatory health insurance.
RESULTS
The annual rate of mental-healthcare use by perinatal women was 16.7%. The annual rate of PMD treatment in obstetric inpatients was 1.1%. The annual rate of PMD records in the midwifery care setting was 2.9%. Women with PMD use mental health services mainly in non-obstetric outpatient settings. Medication was the most frequent treatment. Primary care providers and mental health specialists contributed almost equally to consultation treatments. PMD during pregnancy raised overall costs of healthcare in the postpartum year by 1214 Swiss francs.
CONCLUSIONS: Health-system research and perinatal healthcare should take into consideration the high prevalence of PMD. Real PMD prevalence may be even higher than our data suggest and could be assessed with a survey using our model of PMD prevalence.
Introduction
Perinatal mental disorders (PMDs) are mental and behavioural disorders that appear during pregnancy or the first year after birth. PMDs affect up to 20% of women [1–5], but reported prevalence rates vary widely depending on method of assessment, the population and number of PMDs considered. PMD can have severe consequences, including suicide risk [6], obstetric complications [7] and chronic mental illness [8]. Children of affected women can develop persistent emotional, behavioural and cognitive problems [9]. In Great Britain, long-term costs of inadequate treatment of PMD were estimated to be about 10 000 British pounds per birth, and most of these costs relate to the child [10]. Despite high prevalence and adverse outcomes, PMD is often undiagnosed and untreated. In high-income countries, 36 to 50% of severe cases of mental disorder are untreated in the general population [11] and the rate may be even higher in perinatal populations [5, 12–14]. In the perinatal period women often hide symptoms because they fear the stigma connected to mental illness [15] or are afraid they may be considered inadequate mothers [16]. Mental-health services specifically for perinatal women are rare and often hard to access [17, 18]. Such services must take into account obstetric conditions, consider the health of the unborn or breastfed infant, bonding and attachment processes and parenting behaviour [9].
Great Britain developed comprehensive guidelines for detecting, assessing and treating PMD, in order to improve mental-health services for perinatal women and ensure adequate treatment [19]. Australia developed guidelines for detecting and treating perinatal depression in primary care [20]. The Swiss health agenda has not focused on perinatal mental health [21, 22]. PMD prevalence in Switzerland is unknown. Studies that used small inpatient samples report 12.5 to 14% of “depression symptoms” in postpartum women during the first week, or 17 months after birth, and 37% of antenatal depression in migrants [23–25]. Freelance midwives recorded “maternal distress” in 2.6% of a large sample within the first 10 days after birth [26]. Mental health services for perinatal women were assessed once, in 2007, when most cantons (65%) did not provide such specialised services in obstetric hospitals [18]. Outpatient general mental-health services are widely available in Switzerland and patients can access most of them directly. However, we do not know how many perinatal women use either specialised or general, inpatient or outpatient mental-health services. Nor are data available on the healthcare costs of PMD. This creates a substantial knowledge gap in perinatal mental health in Switzerland.
Objectives
To inform health system researchers and perinatal healthcare providers, we obtained data on PMD prevalence and use of mental health services by perinatal women from existing Swiss databases. We had four specific objectives:
- To estimate annual prevalence rates of PMD based on (a) the mental health care use by perinatal women, (b) treatment of PMD in obstetric inpatients and (c) records of PMD in the midwifery homecare setting.
- To ascertain if prevalence and women’s trajectories of mental healthcare use changed in a period that started before pregnancy and included the perinatal periods.
- To quantify the relative contributions of medication and consultation to PMD treatment.
- To estimate the influence of PMD during pregnancy on overall health insurance costs in the first postpartum year.
Materials and methods
Databases and design
We obtained data from the following sources (appendix 1):
- The Helsana group (INS), one of the largest statutory health insurance companies in Switzerland. In 2014, Helsana enrolled 1.2 million Swiss residents with mandatory insurance, which is 15% of the general population (2014). INS contains data on health insurance claims for all services covered by mandatory health insurance.
- Medical Statistics of Hospitals (MED) [27], the annual mandatory survey of all inpatients in Switzerland. MED accounts for about 97% of births in Switzerland and contains ICD-10 diagnoses for treatments during the patient’s hospital stay [28].
- Statistics of Freelance Midwives (MID) [29]. MID is an annual survey of the services of freelance midwives and is mandatory for midwives affiliated with the Swiss Confederation of Midwives. MID contains PMD records by midwives and represents 71% of postpartum women in Switzerland (2014).
We used the three different databases to look at mental health of perinatal women from different perspectives (objectives 1–4). For objective 1, we obtained a dataset from each database. We drew a second INS dataset for all other objectives. The datasets of all databases are similar in that they represent or almost cover the population of perinatal women in Switzerland. However, they differ in healthcare setting, specific population and length of postpartum sub-periods, according to the availability of data. For reasons of data protection, it is not possible to identify individuals and aggregate them across datasets. We analysed the datasets independently. We detail inclusion and exclusion criteria for all datasets in appendix 1.
Settings
INS data include all healthcare settings – inpatient and outpatient – that provide mental-health care and are covered by mandatory health insurance. MED data are drawn from inpatient obstetric settings in hospitals and midwife-lead birth centres. MID data are mainly drawn from outpatient obstetric settings, i.e. women’s homes and midwives’ practices, but also include midwife-led birth centres and hospital-affiliated midwives [29].
Populations and periods
For objective 1, we included from INS all perinatal women of the year 2014. For the second INS dataset (objectives 2–4) we included women who gave birth in 2012 or 2013 (fig. S1, appendix 2). We included a 3-month period before pregnancy to identify changes due to the perinatal state. We divided pregnancy and the postpartum year into trimesters to obtain trimester prevalence rates across all periods. From MED (objective 1), we analysed data from 2012, since there is always a 2-year lag in MED data. We included women who were inpatients during pregnancy, for birth and the following (average) 5 days [30], or were hospitalised in the postpartum period. Inpatient stays during pregnancy or after the birth indicate complications that required treatment in an obstetric hospital, whereas women hospitalised for the birth are usually healthy. For the MID data (objective 1) we included women who received freelance midwifery care in 2014. Pregnant and early postpartum women with midwifery care are usually healthy. Beyond 10 days after birth midwifery care required medial prescription, indicating the presence of complications that were treatable by the midwife.
Endpoints
The endpoints of the study indicated different aspects of PMD prevalence. “Use of mental-health services” is the endpoint derived from INS data. It reflects a broad spectrum of PMD from minor to the most severe cases because the data cover all mental-health services that are part of mandatory health insurance. The MED endpoint is “PMD treatment in obstetric hospitals”. It indicates PMD that was diagnosed and treated during the inpatient stay in an obstetric hospital. It reflects acute cases prominent in this setting. The endpoint of MID is “PMD record in freelance midwifery care”. It is based on the assessment of each midwife.
Data analysis
For objective 1, we calculated annual prevalence rates of the three endpoints and stratified MED and MID by perinatal sub-periods. For objective 2, we calculated 3-month prevalence rates of the use of mental-health services, including the trimester before pregnancy. We calculated the conditional percentages of women who used mental-health services across the trimester before pregnancy, the entire pregnancy and postpartum year. For objective 3, we stratified use of mental-health services by medication and five types of consultation treatments, again for the trimester before pregnancy, entire pregnancy and first postpartum year. Women who received more than one type of treatment appear more than once in the calculations. To account for the different lengths of the periods, we present percentage proportions of all treatments within each period. For objective 4, we calculated costs of care in the first postpartum year using multiple linear regression. We used quantitative and categorical variables as predictors. To control for differences in health status, we considered pharmacy-based cost groups (PCGs) for the year before birth. PCGs are widely used to check for confounding by chronic diseases when information on clinical diagnosis is missing [31].
We determined 95% confidence intervals (CIs). We used R 3.1.2 for analysis of INS and MID, and SPSS 20.0 (IBM Corp, USA) for the MED analysis.
Ethical statement
In compliance with Swiss Federal Law on data protection (Human Research Act, Article 2), data were anonymised and irreversibly de-identified to protect patient, physician, midwife and hospital privacy. Because data were retrospective, pre-existing, and de-identified, this study did not need approval from the ethics committee.
Results
Populations
Table 1 shows the number of women included for each dataset and population (nall). Mean age (standard deviation) of women in the INS dataset was 32.1 (5.0) years, in MED 31.1 (5.1) years and in MID 32.0 (4.9) years. In the MID sample, 58.3% of women were Swiss and 41.0% had another nationality; 50.6% were primiparous and 49.4% were multiparous.
Table 1 Annual prevalence rates of three indicators of perinatal mental disorders.
|
Data
|
Year
|
Indicator of PMD
|
Sampling period
|
%PMD
|
95% CI
|
nPMD
|
nall
|
| INS |
2014 |
Use of mental health care |
Pregnancy and postpartum year
|
16.7
|
16.1–17.4
|
2336
|
13 969
|
| MED |
2012 |
Mental health treatments in obstetric hospital |
Pregnancy*, birth up to 5 days postpartum and postpartum year*
|
1.1
|
1.1–1.2
|
1013
|
89 699
|
| Pregnancy*
|
1.5 |
1.3–1.6 |
387 |
26 530 |
|
Birth up to 5 days postpartum
|
0.7
|
0.6–0.8
|
445
|
61 142
|
| Postpartum year*
|
5.7 |
5.4–7.0 |
189 |
3301 |
| MID |
2014 |
Records of freelance midwives |
Pregnancy, birth up to 10 days postpartum and postpartum yea†
|
2.9
|
2.7–3.0
|
1660
|
57 951
|
| Pregnancy |
2.9 |
2.6–3.2 |
330 |
11 326 |
|
Birth up to 10 days postpartum
|
2.1
|
2.0–2.3
|
1152
|
54 057
|
| Beyond 10 days postpartum†
|
7.3 |
6.9–7.8 |
813 |
11 100 |
Annual prevalence estimates (objective 1)
The annual rates of the three indicators of PMD prevalence varied widely (table 1). They were highest for use of mental-health care and lowest for mental-health treatments in obstetric hospitals. Annual PMD records by freelance midwives are a small fraction of the rates of mental-health care use. Midwives referred 18.8% (n = 434) of the women they diagnosed with PMD to a mental-health specialist.
Within the obstetric inpatient setting, PMD treatment rates were lowest for the large population of women who became inpatients for the birth. Similarly, PMD record rates in midwifery care are lowest shortly after birth up to 10 days postpartum. Women with obstetric complications in later postpartum periods had highest PMD treatment rates (MED) and highest PMD records by midwives (MID).
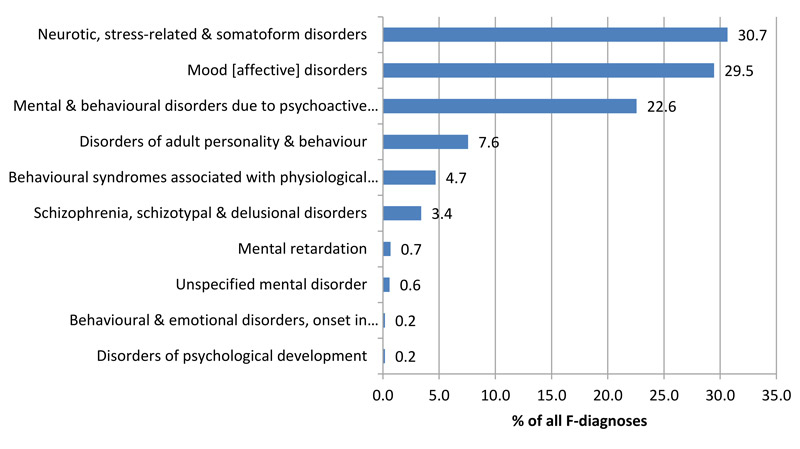
The two most common PMD diagnoses that required mental-health treatment in obstetric inpatients were neurotic, stress-related and somatoform disorders (F4) and mood (affective) disorders (F3) (fig. S2, appendix 2). Among F4 diagnoses, anxiety disorders and stress disorders were treated most frequently (table S1, appendix 2). Among F3 diagnoses, depressive episodes and recurrent depressive disorders made up almost 90%. Substance use disorders were also frequent (table S1).
Use of mental-health services across periods (objective 2)
Three-month prevalence rates
When comparing 3-month periods, use of mental-health care was highest before pregnancy, lowest in the second trimester of pregnancy and increased thereafter until the end of the postpartum year, when it returned to the prepregnancy level (table 2).
Table 2 Three-month prevalence rates of the use of mental health care.
|
Period
|
Trimester
|
%PMD
|
95% CI
|
nPMD
|
| Before pregnancy |
Last |
9.5 |
9.0–9.9 |
1433 |
| Pregnancy |
1 |
6.7 |
6.3–7.1 |
1015 |
| 2 |
5.8 |
5.4–6.1 |
870 |
| 3 |
6.8 |
6.4–7.3 |
1033 |
| Postpartum year |
1 |
6.6 |
6.2–7.0 |
997 |
| 2 |
7.6 |
7.2–8.0 |
1146 |
| 3 |
8.6 |
8.2–9.1 |
1303 |
| 4 |
8.7 |
8.3–9.2 |
1318 |
Trajectories of use
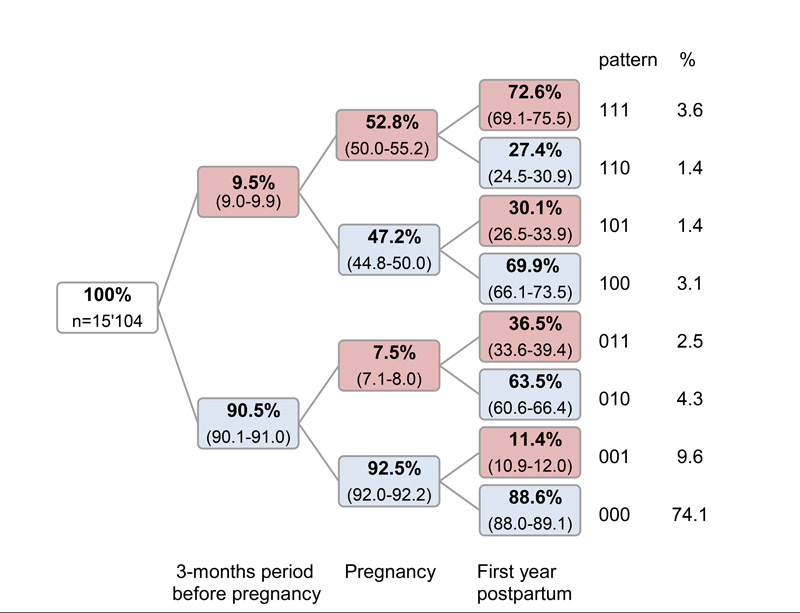
Figure 1 shows patterns of use during the 3-month period before pregnancy, during the entire pregnancy and during the postpartum year. Most of the women (74.1%) did not use mental-health services in any period (pattern 000). Most of the women who used mental-health care, attended only in the postpartum year (001). Almost half of the women who used mental-health care before pregnancy stopped using it during pregnancy. A third of the women who had stopped using mental-health treatment during pregnancy resumed use of mental-health care in the postpartum year. A small group (3.6%) of women used mental-health care in all three periods (111).
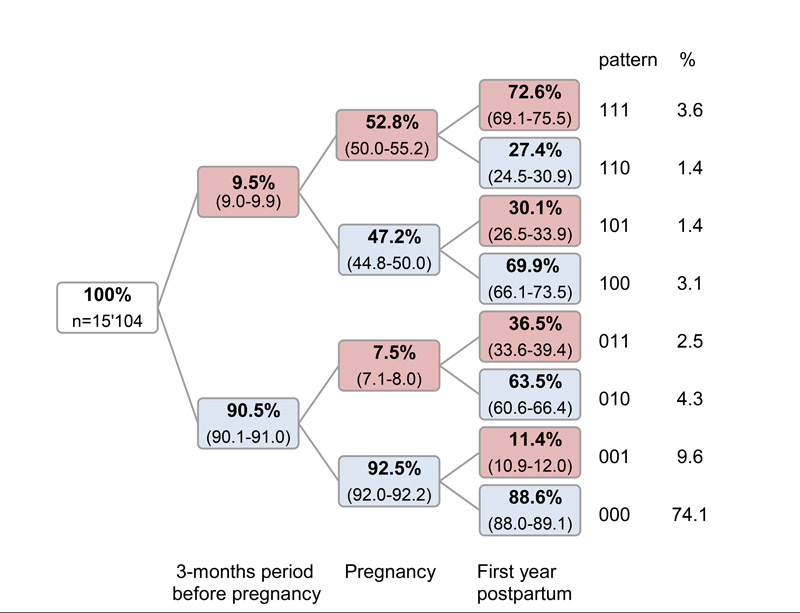
Figure 1 Trajectories of the use of mental healthcare for perinatal women in Switzerland, expressed as conditional percentages of women using mental health services (%) in consecutive periods. Red box or code 1: use of mental health services, blue box or code 0: no use of mental health services. The period patterns indicate three consecutive periods from left to right, e.g., the pattern 001 indicates use of mental health service postpartum, but not before pregnancy or during pregnancy. Helsana health insurance data.
Types of mental-health services (objective 3)
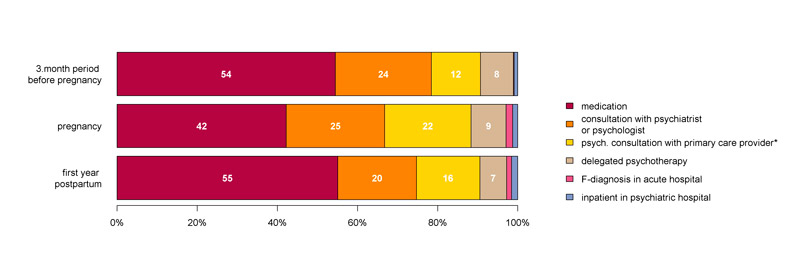
Medication was the most frequent treatment used in each perinatal period. In the last trimester before pregnancy, 6.8% (95% CI 6.4–7.2) of perinatal women used medication. To adjust for differences in period lengths, we present each treatment as a proportion of all treatments within a period (fig. 2). During pregnancy, the proportion of medication use declined and the proportion of primary care consultations increased. Consultations with mental-health specialists remained almost the same. During pregnancy and in the postpartum year, primary care providers contributed almost as much as specialists to mental-health care. Delegated psychotherapy accounted for 7–9% of all mental-health treatments. Psychiatric hospitals contributed 0.2% of all treatments in the last trimester before pregnancy, 1.7% during pregnancy and 1.2% in the postpartum year.
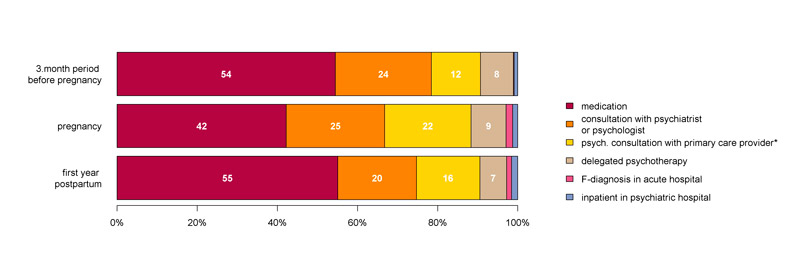
Figure 2 Proportions of medication and five types of consultation by period. For women who gave birth in Switzerland 2012 or 2013 (n = 15 104), Helsana health insurance data.
*Services summarised here also include a minor fraction provided by gynaecologists and other care providers.
PMD and healthcare costs (objective 4)
Age of the women, pharmaceutical cost group markers, managed care, high franchise, complicated vaginal birth or complicated caesarean section, and mental illness during pregnancy were variables that influenced costs within mandatory health insurance in the postpartum year (table 3). Mental illness during pregnancy raised costs in the postpartum year by CHF 1214, which was more than the other factors.
Table 3 Costs of health care in the postpartum year as influenced by perinatal mental disorder during pregnancy and other predictors (Multiple Linear Regression)..
|
Predictor variable
|
Coefficient
|
95% CI
|
p-value
|
| Intercept = 233.5 |
| Age of women |
28.0 |
12.7–43.3 |
<0.001 |
| Pharmaceutical cost group*
|
1182.0 |
1119.8–12 442 |
<0.001 |
| Managed care |
−285.8 |
−442.5– −129.1 |
<0.001. |
| Private insurance |
45.5 |
−179.8–270.8 |
n.s. |
| Latin canton |
32.3 |
−140.1–204.7 |
n.s. |
| High franchise (CHF >500) |
−353.2 |
−515.0– −191.4 |
<0.001 |
| Caesarean section |
35.5 |
−157.9–228.9 |
n.s. |
| Vaginal birth with complications |
353.2 |
150.3–556.0 |
<0.001 |
| Caesarean section with complications |
477.2 |
244.0–710.3 |
<0.001 |
| PMD during pregnancy*
|
1214.4 |
974.8–1454.0 |
<0.001 |
Discussion
Main findings
We found that 16.7% of perinatal women per year, every sixth women, used mental-health services in Switzerland. In obstetric hospitals, 1.1% of perinatal women were treated for PMD during their inpatient stay. For a small minority of women (2.9%), PMD was recorded by midwives in the home care setting. Medication was the most common treatment for PMD. Women with PMD consulted mainly with mental-health specialists, but primary care providers contributed almost as much as specialists to mental-health care in the perinatal period in the postpartum year, Mental illness in pregnancy was associated with an increase of CHF 1214 in basic health insurance costs.
Strengths and limitations
We know of no other study that estimates PMD prevalence in Switzerland. The study was strengthened by the use of data from large populations. The INS population represents about 15% of perinatal women in Switzerland, MED covers 98% of births and MID covers 71% of all early postpartum women in Switzerland, so the chance of selection bias is small, and MID and MED almost comprise the Swiss perinatal population. The analyses of the three different databases create a comprehensive picture of PMD prevalence: this includes a broad range of PMD and healthcare settings, brings together women from all perinatal periods, with and without obstetric complications. For the entire perinatal period, populations of the different datasets are very comparable.
The study is limited by the fact that the datasets are not completely unique: Some are from the same years and women can appear in more than one dataset when they switch services. However, we analysed the data independently. MED and MID almost comprise the entire perinatal population, but are from different years.
Criteria for PMD were limited because the available databases are not designed to provide PMD diagnoses. MED contains only the most prominent cases of PMD that appear and are treated during inpatient stays in obstetric hospitals. Diagnoses in MID rely on individual assessments of each midwife [29]. We could determine use of mental-health services for mandatory insurance, but not for supplementary insurance and self-paid services, and so we may have underestimated mental-health services use.
Estimates of PMD prevalence
We did not expect to find that use of mental-health services in Switzerland was so common among perinatal women, since reports of undertreatment of PMD are abundant [5, 10, 12–14, 17]. Our definition of use of mental-health services was broad and included a wide range of severities of PMD. Nevertheless, PMD may be underdiagnosed in Switzerland because systematic screening is key to detecting PMD [13, 19], but is not part of routine obstetric care in Switzerland [18, 29]. Perinatal women are cautious about reporting symptoms of mental illness to health professionals [32], and obstetricians and midwives are usually not well-trained to deal with mental illness [13, 16]. A US study that assessed PMD retrospectively using diagnostic criteria, found annual prevalence rates of 25% and 28% in past-year-pregnant and postpartum women [5]. Given the fact that our INS data cover only women who used mental-health services, we suspect that INS data underestimate PMD.
Only 1.1% per year of obstetric inpatients received mental-health treatment during their hospital stay. These women have severe forms of PMD, since their symptoms were considered clinically relevant in settings that did not specialise in mental disorders. In this population, women who came to the hospital for birth and stay there on average 5 days prevail. During this short period, postpartum mental-health problems may not manifest, or are considered by the women as transient and part of normal adjustment [17].
Apart from birth, perinatal women become inpatients in obstetric hospitals when they experience complications of pregnancy and the postpartum period. Such conditions increase the risk of PMD [1, 33, 34]. Accordingly, these women were treated for PMD more frequently than inpatients for the birth only. In the postpartum period, stress or sleep deprivation are common [35]. Women with physical complications might be more affected by these stressors than healthy women.
For further research, we suggest a pyramid model that considers different severities of PMD. The basis is women who have minor mental problems, do not seek professional help and try to cope on their own [32]. Other women experience impaired well-being and are ready to inform health professionals about their symptoms. These women use outpatient mental-health care and prevail in our INS data (fig. 2). Women with or without obstetric problems need mental-health care as inpatients in obstetric hospitals and a minority, the most severe cases, are treated in psychiatric hospitals. Because of the stigma related to PMD [15], women of all groups, including those with severe disorders, may avoid mental-health care and remain undiagnosed and untreated. True prevalence must include all these groups and can be assessed with a survey.
Use of mental-health services
By periods and women’s trajectories
The use of mental-health care was highest in the trimester before pregnancy (9.5%) – almost twice the 5% mental-health treatment rate of the general population in Switzerland in 2012 [36]. Without knowing about the impending pregnancy, women might fear stigma less and speak more about mental-health problems. The 30% drop in the 3-month prevalence rate of mental-health care use with the onset of pregnancy could reflect women who stop medication when they become pregnant [37]. This is supported by the observation that the rates decline further in the second trimester of pregnancy when almost all women are aware of their pregnancy. Our 3-month prevalence rates for healthcare use do not indicate a peak of PMD in the postpartum year, in line with a meta-analysis of depression prevalence [3], but indicate a drop with the onset of pregnancy.
The trajectories for perinatal women reflect diverse individual histories, invisible in 3-month prevalence rates. Mental health can be unaltered by pregnancy or the postpartum state, can improve for 6% and can worsen for 16.4% of women. This may create different demands in mental-health care. Women who have mental-health problems already in the trimester before pregnancy should be targeted early to help them to adjust their treatment to pregnancy, particularly in the case of psychiatric medication [19, 38]. The large group of women with PMD who did not use mental-health services before pregnancy might experience mental-health problems for the first time. Healthcare services should focus on this population, because it is not familiar with symptoms and treatment of mental disorders.
Type of care
The most frequent treatment was medication, although women seem to prefer nonpharmacological depression treatment [39]. There are medicines appropriate for treating PMD, but they still pose health risks to unborn or breastfed children [38]. Mental-health care providers should consider the woman’s need to decide about her treatment. Balanced advice should include the higher threshold for pharmacological treatment in the perinatal period, and the adverse effects and benefits of a psychological intervention [19]. Perinatal healthcare providers should be aware of the high use of medication.
Our results show that mental-health services for women with PMD are mainly provided in nonobstetric outpatient settings. We found that 9.8% of perinatal women receive mental-health consultations from a general practitioner. There is evidence that general practitioners efficaciously treated postnatal depression, particularly when it was combined with cognitive-behavioural counselling by a mental-health specialist or a trained midwife or nurse [40]. The contribution of freelance obstetricians to perinatal mental-health consultations was low. This is in line with the situation in the US, where obstetricians diagnosed, treated and referred only a minority of women with perinatal depression [41].
PMD and healthcare costs
The finding that mental illness raised overall healthcare costs for perinatal women was also the case for general populations [42, 43]. The increase due to PMD was CHF 1214 and is 15% of the average annual healthcare costs (2014) of Swiss inhabitants [44]. Depression severity is a strong predictor for using mental-health services [45]. Severe mental illnesses such as psychoses create particularly high costs [42], mainly as a result of chronic medical comorbidity and poor management of the mental illness. Overall healthcare costs for persons with chronic psychoses were CHF 4726 in 2009 [42]. Such cases – though rare in our study– may have increased the average costs.
Conclusion
Health-system researchers and perinatal healthcare providers should focus on the high prevalence of PMD, and seek to ensure that pregnant and postpartum women are adequately treated in all perinatal periods and in all settings. The high rate of mental-health service use represents women so much impaired by PMD that they actively seek professional help, or are referred to it; this rate, though high, suggests real PMD prevalence in Switzerland is even higher.
Appendix 1: Inclusion and exclusion criteria
Helsana health insurance data (INS)
To identify women who gave birth 2012 or 2013 we used the date of entry of the diagnosis group code (DRG) for birth as a proxy for the date of birth (fig. S1). We used all 12 DRG codes for vaginal birth or caesarean section (table S2). We excluded women who had given birth more than once during the time frames. Twins are treated as a single birth. To avoid observation gaps, we excluded 17 813 women who did not have continuous Helsana insurance. We proceeded similarly to identify women who were perinatal in 2014. Perinatal women were determined to have used mental health services if Helsana compensated the provider at least once for at least one of the following services:
- Psychiatric medication;
- Consultation with psychiatrist or psychological professional;
- Psychotherapeutic or psychosocial consultation;
- Delegated psychotherapy;
- Any inpatient stay with ICD-10 F-diagnosis as main or side diagnosis, F17 (tobacco use) as sole F-diagnosis was excluded;
- Inpatient stay in psychiatric hospital.
Services under criteria 3 are mainly provided by general practitioners, i.e., to 77% of perinatal women (n = 2 992). Mental health specialists (to 5.4% of women), gynaecologists (6.5% of women), general hospitals (10.8% of women) and psychiatric hospitals (0.1% of women) contributed also. Two perinatal psychiatric experts of the Psychiatric University Hospital Bern advised us on definitions of perinatal psychiatric medication, and we used the World Health Organization classification for drugs [39] (table S2).
Medical Statistics of Hospitals (MED)
In MED, the most significant health problem associated with the hospital stay is coded as the main diagnosis [37]. Further diagnoses are recorded as side diagnoses. For 2012, we selected all records of inpatients aged 15–50 years, whose main diagnosis related to pregnancy (O10–O48), childbirth (O60–O82) or the puerperium (O85–O92, O94, O98, O99) (ICD-10, n = 92 967). Of the women we selected, 3% were obstetric inpatients more than once in 2012. Using the anonymous linking code we aggregated records to individual perinatal women. Within all perinatal women, women with PMD were identified from a mental side diagnosis (ICD-10 F-diagnoses). F10–99 were considered, but women with F17 (tobacco use) as sole F-diagnosis were excluded (n = 383).
Statistics of the Freelance Midwives (MID)
In 2014, freelance midwives recorded care of 62 917 cases. Approximately 7–11% of women were recorded by more than one midwife. We refer to each record as a single woman. Though reporting the mental status during pregnancy or early postpartum period is voluntary, in 2014 it was reported in 92% of all cases. We included all cases for whom the mental health status was reported (n = 57 951). Midwives diagnose PMD on their own assessment. They can record in the survey “mental health problems” or “depression” or “postpartum depression”. We refer to all these diagnoses as PMD. We assigned women to perinatal sub-periods depending on when midwives cared for them.
Appendix 2: Supplementary figures and tables
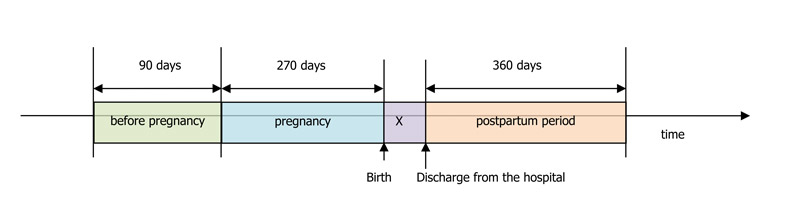
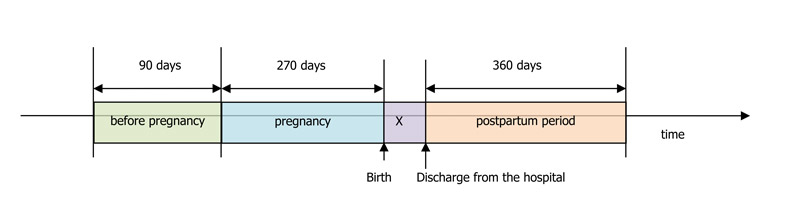
Figure S1 Definition of periods in Helsana health insurance data (INS). Lengths of periods were calculated on a 12 months per year and 30 days per month basis (360/30). X denotes the hospital inpatient stay after birth, on average 5 days 2012–2014 [30]
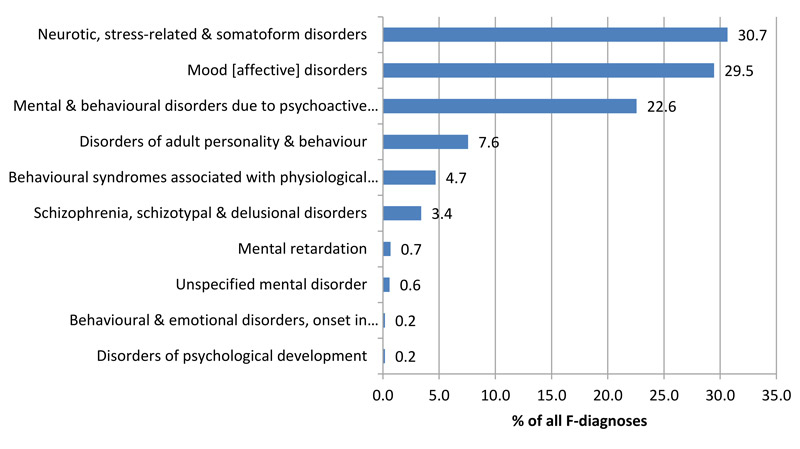
Figure S2 Percentages of diagnostic groups of mental disorders (% of all recoded F-diagnoses; n = 1174); ICD-10 F-diagnoses at the 2-character level* recorded in inpatient obstetric care. Medical Statistics of Hospitals, 2012.
* WHO. The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. 2010.
Table S1 Proportion of diagnostic groups of all perinatal mental disorders (% of all recorded F-diagnoses, n = 1174).
|
ICD-10 code*
|
Mental and behavioural disorder
|
n
|
%
|
|
F40–F48
|
Neurotic, stress-related and somatoform disorders
|
360
|
100.0
|
| F41 |
Other anxiety disorders |
172 |
47.8 |
| F43 |
Reaction to severe stress, and adjustment disorders |
154 |
42.8 |
| F40 |
Phobic anxiety disorders |
13 |
3.6 |
| F45 |
Somatoform disorders |
13 |
3.6 |
| F42 |
Obsessive-compulsive disorder |
4 |
1.1 |
| F44 |
Dissociative [conversion] disorders |
2 |
0.6 |
| F48 |
Other neurotic disorders |
2 |
0.6 |
|
F30–F39
|
Mood [affective] disorders
|
352
|
100.0
|
| F32 |
Depressive episode |
260 |
73.9 |
| F33 |
Recurrent depressive disorder |
55 |
15.6 |
| F31 |
Bipolar affective disorder |
26 |
7.4 |
| F34 |
Persistent mood [affective] disorders |
3 |
0.9 |
| F30 |
Manic episode |
1 |
0.3 |
| F38 |
Other mood [affective] disorders |
1 |
0.3 |
|
F10–F19
|
Mental and behavioural disorders due to psychoactive substance use
|
264
|
100.0
|
| F17 |
...due to use of tobacco |
74 |
28.0 |
| F11 |
...due to use of opioids |
61 |
23.1 |
| F12 |
...due to use of cannabinoids |
58 |
22.0 |
| F19 |
...due to multiple drug use and use of other psychoactive substances |
24 |
9.1 |
| F14 |
...due to use of cocaine |
20 |
7.6 |
| F10 |
...due to use of alcohol |
13 |
4.9 |
| F13 |
...due to use of sedatives or hypnotics |
9 |
3.4 |
| F15 |
...due to use of other stimulants, including caffeine |
4 |
1.5 |
| F16 |
...due to use of hallucinogens |
1 |
0.4 |
Table S2 Diagnosis Related Group codes used to identify women in Helsana health insurance data (INS), who gave birth in Switzerland 2012–2013, or were perinatal in 2014.
|
DRG*
|
Diagnosis
|
| O01A |
Caesarean section with several complicating diagnoses, duration of pregnancy up to 25th complete week or with intrauterine therapy |
| O01B |
Caesarean section with several complicating diagnoses, duration of pregnancy 26 up to 33 complete weeks, without intrauterine therapy or with complicating diagnosis, up to week 25 or thromboembolism during pregnancy with OR-procedure |
| O01C |
Caesarean section with several complicating diagnoses, duration of pregnancy > 33 complete weeks, without intrauterine therapy or with complicating diagnoses, 26 up to 33 week of pregnancy or with complex diagnose, or up to week 33 of pregnancy or with complicating diagnosis with most severe CC |
| O01D |
Caesarean section with several complicating diagnoses, pregnancy duration > 33 complete weeks, without intrauterine therapy or with complicating diagnosis, 26 up to 33 week of pregnancy or with complicating diagnosis or up to 33 week of pregnancy or with complicating diagnosis, without most severe CC |
| O01E |
Caesarean section with complicating diagnosis, pregnancy duration more than 33 complete weeks, without complex diagnosis |
| O01F |
Caesarean section without complicating diagnosis, pregnancy duration more than 33 complete weeks, without complex diagnosis |
| O02A |
Vaginal birth with complicating OR-procedure, pregnancy duration up to 33 complete weeks with intrauterine therapy |
| O02B |
Vaginal birth with complicating OR-procedure, pregnancy duration more than 33 complete weeks, without intrauterine therapy |
| O60A |
Vaginal birth with several complicating diagnoses, at least one severe, pregnancy duration up to 33 complete weeks or with complicating procedure |
| O60B |
Vaginal birth with several complicating diagnoses, at least one severe, pregnancy duration more than 33 complete weeks, without complicating procedure or thromboembolism during pregnancy without OR-procedure |
| O60C |
Vaginal birth with complicating diagnosis, severe or moderately severe |
| O60D |
Vaginal birth without complicating diagnosis |
Table S3 Definition of psychiatric medication in Helsana health insurance data (INS); at least one medication was required to classify a woman as receiving psychiatric medication.
One supply with a drug with one of the following Anatomical Therapeutic Chemical (ATC) codes*:
M03BX*, N01AH01, N01AX03, N01AX10, N02AA01, N02AA04, N02AA05, N02AA10, N02AB03, N02AC52, N02AE01, N02AX*, N03AB02, N03AF01, N03AG01, N03AX11, N03AX14, N03AX16, N05A*, N05BA*, N05CD*, N05CF*, N05CX11, N06AA*, N06AB*, N06AF*, N06AG*, N06AX*, N06C*, N07B* |
Acknowledgements
The Swiss Confederation of Midwives and the Swiss Federal Office of Statistics provided the raw data for this study. Ankica Ging (University Hospital for Psychiatry and Psychotherapy, University of Bern; Switzerland) and Barbara Gugger (Psychiatric Services of the University, University of Bern, Switzerland) offered valuable support in identifying the drugs used to treat perinatal mental disorders. The contribution of NB was funded by the Federal Administration’s “Equal Opportunity at Universities of Applied Sciences” Programme 2013–2016. Kali Tal gave us editorial assistance.
Anke Berger PhD, Bern University of Applied Sciences, Health Division, Research and Development in Midwifery, Stadtbachstrasse 64, CH-3012 Bern, anke.berger[at]bfh.ch
References:
1
Howard
LM
,
Molyneaux
E
,
Dennis
C-L
,
Rochat
T
,
Stein
A
,
Milgrom
J
. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384(9956):1775–88. doi:.https://doi.org/10.1016/S0140-6736(14)61276-9
2
Jones
I
,
Chandra
PS
,
Dazzan
P
,
Howard
LM
. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384(9956):1789–99. doi:.https://doi.org/10.1016/S0140-6736(14)61278-2
3
Gavin
NI
,
Gaynes
BN
,
Lohr
KN
,
Meltzer-Brody
S
,
Gartlehner
G
,
Swinson
T
. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005;106(5 Pt 1):1071–83. doi:.https://doi.org/10.1097/01.AOG.0000183597.31630.db
4
Grekin
R
,
O’Hara
MW
. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 2014;34(5):389–401. doi:.https://doi.org/10.1016/j.cpr.2014.05.003
5
Vesga-López
O
,
Blanco
C
,
Keyes
K
,
Olfson
M
,
Grant
BF
,
Hasin
DS
. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65(7):805–15. doi:.https://doi.org/10.1001/archpsyc.65.7.805
6
Appleby
L
,
Mortensen
PB
,
Faragher
EB
. Suicide and other causes of mortality after post-partum psychiatric admission. Br J Psychiatry. 1998;173(3):209–11. doi:.https://doi.org/10.1192/bjp.173.3.209
7
Bonari
L
,
Pinto
N
,
Ahn
E
,
Einarson
A
,
Steiner
M
,
Koren
G
. Perinatal risks of untreated depression during pregnancy. Can J Psychiatry. 2004;49(11):726–35.
8
Horwitz
SM
,
Briggs-Gowan
MJ
,
Storfer-Isser
A
,
Carter
AS
. Persistence of Maternal Depressive Symptoms throughout the Early Years of Childhood. J Womens Health (Larchmt). 2009;18(5):637–45. doi:.https://doi.org/10.1089/jwh.2008.1229
9
Stein
A
,
Pearson
RM
,
Goodman
SH
,
Rapa
E
,
Rahman
A
,
McCallum
M
, et al.
Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384(9956):1800–19. doi:.https://doi.org/10.1016/S0140-6736(14)61277-0
10Bauer A, Parsonage M, Knapp M, Iemmi V, Adelaja B. The costs of perinatal mental health problems. London: PSSRU and Centre for Mental Health, 2014.
11
Demyttenaere
K
,
Bruffaerts
R
,
Posada-Villa
J
,
Gasquet
I
,
Kovess
V
,
Lepine
JP
, et al., WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–90. doi:.https://doi.org/10.1001/jama.291.21.2581
12
Dennis
CL
,
Dowswell
T
. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013;2(2):CD001134.
13
Milgrom
J
,
Gemmill
AW
. Screening for perinatal depression. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):13–23. doi:.https://doi.org/10.1016/j.bpobgyn.2013.08.014
14
Marcus
SM
,
Flynn
HA
,
Blow
FC
,
Barry
KL
. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt). 2003;12(4):373–80. doi:.https://doi.org/10.1089/154099903765448880
15
Clement
S
,
Schauman
O
,
Graham
T
,
Maggioni
F
,
Evans-Lacko
S
,
Bezborodovs
N
, et al.
What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. 2015;45(1):11–27. doi:.https://doi.org/10.1017/S0033291714000129
16
Byatt
N
,
Biebel
K
,
Friedman
L
,
Debordes-Jackson
G
,
Ziedonis
D
,
Pbert
L
. Patient’s views on depression care in obstetric settings: how do they compare to the views of perinatal health care professionals?
Gen Hosp Psychiatry. 2013;35(6):598–604. doi:.https://doi.org/10.1016/j.genhosppsych.2013.07.011
17
Dennis
C-L
,
Chung-Lee
L
. Postpartum depression help-seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323–31. doi:.https://doi.org/10.1111/j.1523-536X.2006.00130.x
18
Amiel Castro
RT
,
Schroeder
K
,
Pinard
C
,
Blöchlinger
P
,
Künzli
H
,
Riecher-Rössler
A
, et al.
Perinatal mental health service provision in Switzerland and in the UK. Swiss Med Wkly. 2015;145:w14011.
19National Institute for Health and Care Excellence. Antenatal and postnatal mental health: Clinical management and service guidance (update). 2014, updated June 2015. Available from: https://www.nice.org.uk/guidance/cg192.
20Austin M-P. HNatGEAC. Clinical practice guidelines for depression and related disorders - anxiety, bipolar disorder and puerperalpsychosis - in the perinatal period. A guideline for primary care health professionals. Melbourne: beyondblue: the national depression initiative.; 2011 [accessed 13 Dec 2016]. Available from: http://resources.beyondblue.org.au/prism/file?token=BL/0891.
21Federal Department of Home Affairs. Health 2020 - The Federal Council’s health-policy priorities. 2013. Available from: http://www.nationalplanningcycles.org/sites/default/files/country_docs/Switzerland/nhp_swiss.pdf.
22Daniela Schuler AT. Nathalie Buscher, Paul Camenzind. Psychische Gesundheit in der Schweiz - Monitoring 2016. Obsan Bericht 72: Obsan; 2016. p. 76.
23
Bielinski-Blattmann
D
,
Lemola
S
,
Jaussi
C
,
Stadlmayr
W
,
Grob
A
. Postpartum depressive symptoms in the first 17 months after childbirth: the impact of an emotionally supportive partnership. Int J Public Health. 2009;54(5):333–9. doi:.https://doi.org/10.1007/s00038-009-0056-4
24
Gürber
S
,
Bielinski-Blattmann
D
,
Lemola
S
,
Jaussi
C
,
von Wyl
A
,
Surbek
D
, et al.
Maternal mental health in the first 3-week postpartum: the impact of caregiver support and the subjective experience of childbirth - a longitudinal path model. J Psychosom Obstet Gynaecol. 2012;33(4):176–84. doi:.https://doi.org/10.3109/0167482X.2012.730584
25
Ratcliff
BG
,
Sharapova
A
,
Suardi
F
,
Borel
F
. Factors associated with antenatal depression and obstetric complications in immigrant women in Geneva. Midwifery. 2015;31(9):871–8. doi:.https://doi.org/10.1016/j.midw.2015.04.010
26
Staehelin
K
,
Kurth
E
,
Schindler
C
,
Schmid
M
,
Zemp Stutz
E
. Predictors of early postpartum mental distress in mothers with midwifery home care--results from a nested case-control study. Swiss Med Wkly. 2013;143:w13862.
27Federal Statistical Office. Medical Statistics of Hospitals 2012. Neuchâtel: 2014.
28Federal Statistical Office. Medizinisches Kodierungshandbuch Der offizielle Leitfaden der Kodierrichtlinien in der Schweiz. Neuchâtel 2016.
29Erdin Springer R, II, van Gogh S, Schmid M, Pehlke-Milde J. Statistics of the Freelance Midwives - Tätigkeitserfassung der frei praktizierenden Hebammen der Schweiz: Bericht zur Erhebung 2014. Bern, Schweizerischer Hebammenverband;2015.
30 Federal Statistical Office. Medical Statistics of Hospitals. Neuchâtel: 2013–2015.
31
Huber
CA
,
Szucs
TD
,
Rapold
R
,
Reich
O
. Identifying patients with chronic conditions using pharmacy data in Switzerland: an updated mapping approach to the classification of medications. BMC Public Health. 2013;13(1):1030. doi:.https://doi.org/10.1186/1471-2458-13-1030
32Boots Family Trust Alliance. Perinatal mental health experiences of women and health professionals. 2013. Accessed 13 Dec 2016; available from: https://www.tommys.org/sites/default/files/Perinatal_Mental_Health_Experiences%20of%20women.pdf
33
Melville
JL
,
Gavin
A
,
Guo
Y
,
Fan
MY
,
Katon
WJ
. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol. 2010;116(5):1064–70. doi:.https://doi.org/10.1097/AOG.0b013e3181f60b0a
34
O’Hara
MW
,
Wisner
KL
. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):3–12. doi:.https://doi.org/10.1016/j.bpobgyn.2013.09.002
35
Lawson
A
,
Murphy
KE
,
Sloan
E
,
Uleryk
E
,
Dalfen
A
. The relationship between sleep and postpartum mental disorders: A systematic review. J Affect Disord. 2015;176:65–77. doi:.https://doi.org/10.1016/j.jad.2015.01.017
36Schuler DBL. Psychische Gesundheit in der Schweiz. Monitoring 2012 (Obsan Bericht 2012) Neuchâtel: Schweizerisches Gesundheitsobservatorium: 2012.
37
Petersen
I
,
Gilbert
RE
,
Evans
SJ
,
Man
SL
,
Nazareth
I
. Pregnancy as a major determinant for discontinuation of antidepressants: an analysis of data from The Health Improvement Network. J Clin Psychiatry. 2011;72(7):979–85. doi:.https://doi.org/10.4088/JCP.10m06090blu
38Schaefer C, Peters PW, Miller RK. Drugs during pregnancy and lactation: treatment options and risk assessment: Academic Press; 2014.
39
Battle
CL
,
Salisbury
AL
,
Schofield
CA
,
Ortiz-Hernandez
S
. Perinatal antidepressant use: understanding women’s preferences and concerns. J Psychiatr Pract. 2013;19(6):443–53. doi:.https://doi.org/10.1097/01.pra.0000438183.74359.46
40
Milgrom
J
,
Holt
CJ
,
Gemmill
AW
,
Ericksen
J
,
Leigh
B
,
Buist
A
, et al.
Treating postnatal depressive symptoms in primary care: a randomised controlled trial of GP management, with and without adjunctive counselling. BMC Psychiatry. 2011;11(1):95. doi:.https://doi.org/10.1186/1471-244X-11-95
41
Goodman
JH
,
Tyer-Viola
L
. Detection, treatment, and referral of perinatal depression and anxiety by obstetrical providers. J Womens Health (Larchmt). 2010;19(3):477–90. doi:.https://doi.org/10.1089/jwh.2008.1352
42
Huber
CA
,
Schneeweiss
S
,
Signorell
A
,
Reich
O
. Improved prediction of medical expenditures and health care utilization using an updated chronic disease score and claims data. J Clin Epidemiol. 2013;66(10):1118–27. doi:.https://doi.org/10.1016/j.jclinepi.2013.04.011
43
Lee
S
,
Black
D
,
Held
M
. Associations of multiplicity of comorbid health conditions, serious mental illness, and health care costs. Soc Work Health Care. 2016;55(7):518–30. doi:.https://doi.org/10.1080/00981389.2016.1183551
44Ausgaben für das Gesundheitswesen [Internet]. 2016 [cited 12 Dec 2016]. Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit.html.
45
Dey
M
,
Jorm
AF
. Social determinants of mental health service utilization in Switzerland. Int J Public Health. 2016 Sept 15. doi:. https://doi.org/10.1007/s00038-016-0898-5