Figure 1 Prevalence of age-related enuresis – yellow rectangle [8, 9], and parent-reported sleep apnoea from various Western countries – blue line [4].
DOI: https://doi.org/10.4414/smw.2017.14400
antidiuretic hormone
attention-deficit hyperactivity disorder
atrial natriuretic peptide
brain natriuretic peptide
health-related quality of life
obstructive sleep apnoea syndrome
sleep-disordered breathing
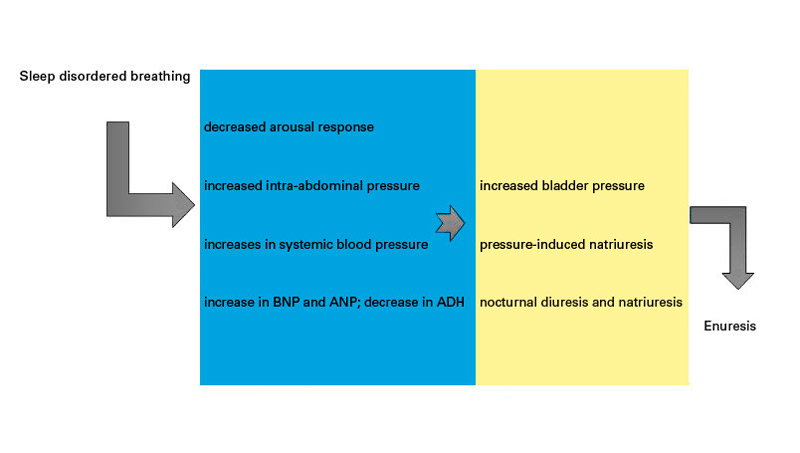
Obstructive sleep-disordered breathing (SDB) is a syndrome of upper airway dysfunction that occurs during sleep and is characterised by snoring and/or increased respiratory effort. Obstructive sleep apnoea syndrome (OSAS) is characterised by witnessed apnoea, unrefreshing sleep and excessive daytime sleepiness [1]. The prevalence of OSAS is approximately 0.7 to 3% in children [2–5]. The first peak occurs in children between 2 and 8 years of age and the second peak during adolescence [6]. A follow-up study has shown that only 12% of children aged 5 to 9 years had OSAS resolution at 7 months of follow-up without treatment [7]. A summary of the age-related prevalence of childhood OSAS is shown in figure 1.
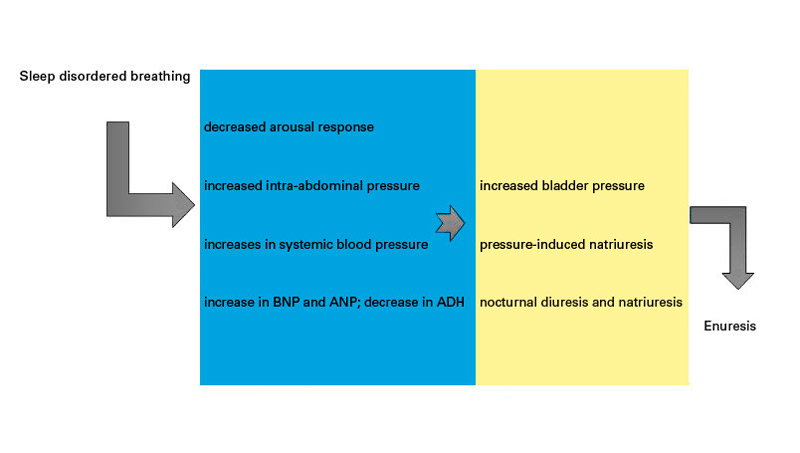
Figure 1 Prevalence of age-related enuresis – yellow rectangle [8, 9], and parent-reported sleep apnoea from various Western countries – blue line [4].
OSAS is a complex, multifactorial disorder. Adenotonsillar hypertrophy is considered an important factor associated with OSAS [10, 11]. Accordingly, adenotonsillectomy can achieve a significant improvement in the severity of obstructive SDB [12]. Other factors are linked to characteristic facial features [13–17]. Correction of craniofacial deformities in children with malocclusion has been shown to improve OSAS [18]. Other putative factors include ethnicity (African-American), prematurity and Down’s syndrome [19], obesity [20, 21], and craniofacial anomaly in syndromic patients (achondroplasia) [22]. In a recent multicentre retrospective study [12], children with chronic asthma were found to be at higher risk of residual OSAS.
OSAS results in snoring, episodic oxyhaemoglobin desaturation, hypercapnia and sleep disruption [11, 23]. Snoring in children has been associated with cortical arousal [24] and multiple neurobehavioural consequences [25–29]. OSAS children have significantly greater morbidity [30]. Children with SDB can have a dolico facial pattern [31] and rhinosinus involvement [32]. They frequently experience decreases in mean neuronal metabolites in the left hippocampus [33], a reduction of middle cerebral artery blood flow velocity [34], prefrontal cortex dysregulation [35], grey matter density deficit in prefrontal regions, reduced attention and visual fine-motor coordination scores [36], and a blunted daytime cerebral blood flow response to hypercapnia [37]. Possible consequences include deficits in Intelligence Quotient and executive functions [35, 38], daytime sleepiness [39, 40], impairment of health-related quality of life (HRQoL) [41, 42], increased internalising (over-control of emotions) and externalising symptoms (interpersonal relationships) [43], psychosocial, cognitive and behavioural impairments [44, 45] that persist even with OSAS resolution [46], poorer academic performance [47] – not yet detected at preschool age [48], periodic limb movements [49] and exacerbation of attention-deficit hyperactivity disorder (ADHD) [50, 51]. An improvement in behaviour, cognitive function, and quality of life has been frequently observed following adenotonsillectomy [52–56]. Autonomic activation from frequent cortical arousal has been reported [57–59]. The respiratory events trigger a greater acute cardiovascular response, including surges in blood pressure and heart rate [60–62], altered cardiovascular and hemodynamic function [63], and an alteration of both antidiuretic hormone (ADH) and brain natriuretic peptide (BNP) levels [64]. A significantly higher value of oxidative stress markers has also been observed in children with SDB [65] along with a higher intra-ocular pressure level [66].
Nocturnal enuresis is a complex disorder characterised by intermittent incontinence that occurs exclusively during sleep. Nocturnal enuresis is applicable to children who are at least 5 years old [67]. There are two subtypes, monosymptomatic nocturnal enuresis and non-monosymptomatic nocturnal enuresis, depending on the absence or presence of symptoms of lower urinary tract and bladder dysfunction [67]. Primary nocturnal enuresis applies to children who have not had a previous dry period for at least 6 months [68]. Secondary nocturnal enuresis refers to children who have had a previous dry period of >6 months [67]. Nocturnal enuresis is one of the most common problems in childhood, with a prevalence of between 2 and 15% [67, 69–71]. The overall prevalence of nocturnal enuresis declines with increasing age, from 15% in 5-year-old children to 0.5% in those aged ≥18 years [8, 9], with an annual healing rate of approximately 15% [72, 73]. A summary of the prevalence of childhood nocturnal enuresis is shown in figure 1.
Although several aetiologies have been proposed for nocturnal enuresis [74, 75], a clear pathogenesis remains mostly unknown [76]. Reduced functional bladder capacity [77], detrusor overactivity [78–80] and elevated arousal thresholds [78, 81, 82] have been implicated. Butler et al. proposed a three-system model that lists excessive nocturnal urine production, nocturnal bladder overactivity and failure to awaken in response to bladder sensation as underlying factors [69, 83]. Abnormal function of the autonomic nervous system [84–87] and the central dopaminergic pathways [88] may alter the control of bladder function. Moreover, nocturnal polyuria [89–91] due to decreased ADH release has also been reported [92–94]. Children with nocturnal enuresis may have decreased ADH secretion [95, 96] and higher BNP values [97] during sleep. Circadian variations [98] may be involved in the impaired regulation of water and electrolytes, micturition, and bladder capacity [93, 99].
Sleep problems in children with enuresis have been studied for a long time. Immaturity of the sleep mechanism has been proposed as a cause [100]. Previously, sleep differences between children with nocturnal enuresis and their dry peers were not clearly and consistently observed [86, 100–104]. The enuretic event was found to be a predominantly non-rapid eye movement (non-REM) sleep phenomenon, with bladder voiding occurring at any stage of sleep and throughout the night [82, 100, 105–107]. Recent observations have shown that children with nocturnal enuresis have disturbed sleep [108, 109]. In particular, they have increased deep sleep, higher arousal thresholds and daytime sleepiness [81, 108–111], sleep fragmentation, frequent cortical arousals [78, 89, 111], and periodic limb movements [89, 110, 112]. High arousal thresholds have been considered one of the leading causes of nocturnal enuresis. Deep sleep prevents arousals when the bladder is full [75, 81, 113]. Sleep fragmentation leads to sleep deprivation, thus affecting endocrine, metabolic, immune, inflammatory and cardiovascular regulation [87, 114].
Several studies have confirmed that children with nocturnal enuresis have low HRQoL [111, 115–117]. Behavioural disorders affect 20 to 40% of children with nocturnal enuresis [118]. They have higher levels of daytime sleepiness [111], daytime internal and external behaviour problems and impaired neuropsychological functioning [83, 119–122]. Nocturnal enuresis generates significant impairment of self-esteem [123] and an impaired HRQoL that worsens over time [117, 124]; their mothers also have lower quality-of-life scores [125]. In these children, periodic limb movements during sleep are associated with a lower HRQoL [126]. They frequently display an ADHD pattern [127–130] and develop conduct disorders [131]. In children with monosymptomatic nocturnal enuresis, magnetic resonance imaging revealed substantial structural abnormalities in the thalamus, medial frontal gyrus, anterior cingulate cortex and insula, which are involved in the micturition control network [132].
Practical consensus guidelines for the management of primary nocturnal enuresis do not mention [133], or mention only marginally, SDB in children with nocturnal enuresis, particularly in those who have treatment resistance and comorbidities [67, 134]. Subjects with habitual snoring are at greater risk of primary nocturnal enuresis than those without snoring, regardless of OSA severity [135]. Therefore, the aims of this paper were to look for published material and to possibly find a putative link between nocturnal enuresis and SDB. In particular, we were trying to answer the following questions:
We conducted an electronic search in Medline (with PubMed interface), Scopus and the ISI Web of Science using [“sleep disordered breathing” OR “sleep apnea”] AND “enuresis” AND “children” in title/abstract/keywords for relevant articles in English. The studies on children with genetic diseases (e.g., achondroplasia), or neurological and endocrinological (e.g., growth hormone deficiency) conditions were excluded. All the articles that were retrieved by our search criteria were systematically reviewed by two authors (MZ and LN). The bibliographies of the selected articles were also examined to identify other pertinent articles.
Firstly, we looked for studies that aimed to answer our four questions (see above) Regarding the fourth question, we looked for studies on the outcome of treatment for obstructive SDB in children with enuresis according to the PRISMA guidelines [136]. We also examined the strength of the evidence (grade of recommendation) according to the Oxford Centre for Evidence-Based Medicine (2011) and the Centre for Evidence-Based Medicine (2009).
A flow chart of our criteria and results are summarized in figure 2. A total of 181 published articles were found; 98 of these were assessed for eligibility, but 24 of them had to be excluded after an attentive reading of the title, abstract and/or full text because the information did not concern the four questions that were the basis of our research. Finally, we found 17 studies regarding the urological outcome of treatment for obstructive SDB in children with enuresis.
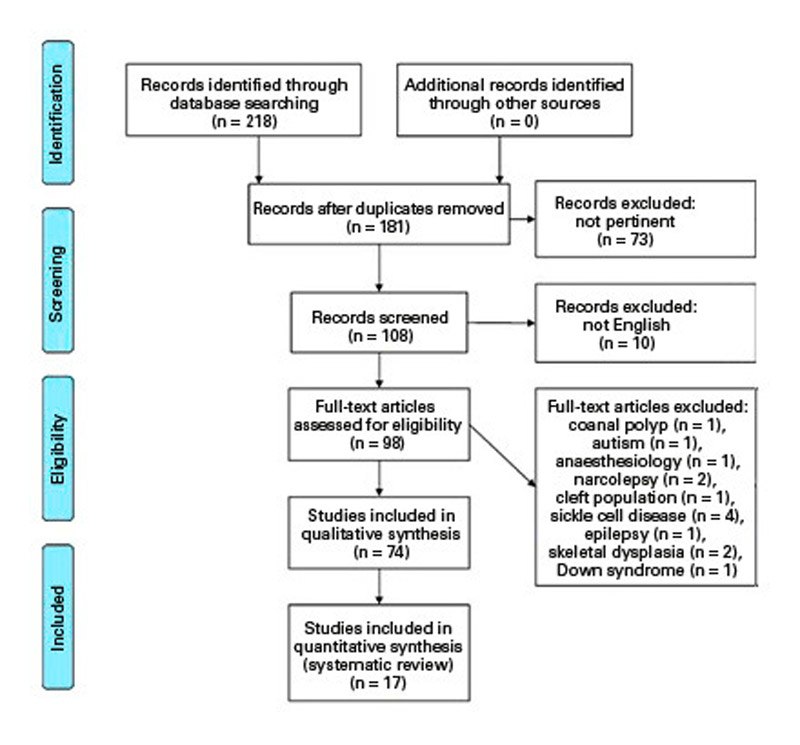
Figure 2 Search criteria for relevant articles and results.
The possible relationship between nocturnal enuresis and obstructive SDB was reported nearly 40 years ago [137–139]. The prevalence of nocturnal enuresis among children with upper airway obstruction was found to be high [140–142], particularly in those not responding to standard treatment with desmopressin and/or an alarm [143]. Several studies have associated childhood nocturnal enuresis with coexistent obstructive SDB [141, 142, 144–147], particularly in children who also have daytime incontinence [148]. Moreover, patients with refractory nocturnal enuresis have a significantly higher prevalence of OSAS, with no difference between sexes [149]. In only one study was the association found only in girls [150]. Facial pattern (dolicofacial) and abnormal head posture was observed in children with nocturnal enuresis, features closely linked to OSAS [151].
Children with nocturnal enuresis and OSAS had a higher arousal index than enuretic children without OSAS [152]. Therefore, the prevalence of nocturnal enuresis could not be directly related to severity of OSAS [141, 152]. The presence of both upper airway narrowing and nocturnal enuresis exhibited the highest sensitivity for detecting children with OSAS [153]. Overweight and monosymptomatic nocturnal enuresis have been associated with OSAS, but not with each other [154]. Nocturnal enuresis has been significantly associated with the presence of moderate-to-severe OSAS in a fully adjusted model considering tonsillar hypertrophy, obesity, gender and age [155]. Residual OSAS after surgery has been significantly associated with coexistent nocturnal enuresis [156].
The most important symptoms and signs – breathing through the mouth, tonsillar size and nasal congestion – correlated with nocturnal enuresis in children who do not respond to standard treatment [152]. Children with therapy-resistant enuresis and without a history of snoring or sleep apnoea showed subclinical signs of disordered respiration, respiratory arousals and a high frequency of hypopnoeas [157].
The frequency of nocturnal enuresis is also greater in children with habitual snoring [97, 152, 158–160]. Snoring in children with monosymptomatic nocturnal enuresis increases their risk of behavioural and psychosocial problems, with impaired HRQoL [161]. Nocturnal enuresis and obstructive SDB, ranging in severity from snoring to OSAS, have both been associated with impaired HRQoL [117, 119, 161]. HRQoL was found to be similar between children with obstructive SDB, with and without enuresis, thus suggesting that the presence of SDB, rather than the presence of nocturnal enuresis, is the major contributing factor to HRQoL impairment [64]. Excessive autonomic activation, hyperactive behaviour and enuresis during sleep have been reported in children with symptoms of obstructive SDB [26].
SDB is frequent in children with monosymptomatic nocturnal enuresis [143, 148]. More specifically, nocturnal enuresis has been reported in 8 to 47% of children with obstructive SDB [141, 143, 162–164]. Recently, of 87 children (aged 9.5 ± 2.6 years) out of 140 enuretic participants in a prospective study who underwent polysomnography, 6 were diagnosed with severe apnoea, 40.7% had mild/moderate apnoea; a family history of nocturnal enuresis and constipation were both extremely frequent. The authors suggested a multidisciplinary approach of the problem [165].
Complete resolution of nocturnal enuresis has been reported in 31 to 76% of OSAS children within months of surgical intervention [9, 166]; interestingly, in about half of them nocturnal enuresis disappeared within 1 month [167, 168]. Spontaneous resolution of nocturnal enuresis has been used to explain nocturnal enuresis remission after adenotonsillectomy [167, 169]. Compared with the 15% annual rate of spontaneous resolution, this resolution rate after surgery should be considered significantly higher than expected [72, 170].
Children who wet the bed are more difficult to arouse from sleep than children who do not [106]. Obstructive SDB may promote nocturnal enuresis by decreasing the arousal response [171], but whether decreased arousal response contributes to both OSA and nocturnal enuresis is questionable [110, 142, 172, 173]. Daytime urodynamics are similar in children with and without nocturnal enuresis [174]. Therefore, increased intra-abdominal pressure caused by respiratory efforts against an obstructed airway has been implicated in the pathogenesis of nocturnal enuresis because of increasing bladder pressure [175].
Urinary excretion of sodium and diastolic blood pressure have been found to increase in parallel with the severity of obstructive SDB [176]. At the end of nocturnal obstructive events, repetitive increases in systemic blood pressure occur, and these can lead to pressure-induced natriuresis [177, 178]. On the contrary, natriuresis and polyuria are completely suppressed by effective treatment of OSAS [70, 144].
SDB can affect the secretion of urinary hormones such as atrial natriuretic peptide (ANP) and ADH. Nocturnal increase in ANP and a decrease in ADH are responsible for the nocturnal diuresis and natriuresis associated with OSA. It has been observed that adults with OSAS have elevated ANP and decreased levels of ADH [179–181], and the normal nocturnal decrease in urine output does not occur [182–184]. ADH normalises after adenotonsillectomy [183]. In patients with OSA, plasma ANP is negatively correlated with cumulative apnoea duration and lowest arterial oxygen saturation (SaO2), whereas a positive correlation has been observed with the highest change in intrathoracic pressure [179]. Upper airway obstruction leads to negative intrathoracic pressure swings, increases systemic venous return, generates high preload at the right ventricle and ultimately enhances the left cardiac ventricle afterload [185, 186]. Acute overload of the cardiac ventricles may promote the release of ANP from ventricular myocytes, which then induces vasodilation and natriuresis [187]. nocturnal enuresis may eventually be triggered by sleep apnoea because an accentuated negative intrathoracic pressure during sleep leads to abnormal secretion of ANP [144].
Enuretic children with obstructive SDB displayed a greater increase in BNP values [97], which correlated with obstructive SDB severity [188]. After successful treatment of OSA-induced ANP secretion, urine output and sodium excretion decreased, whereas renin and aldosterone values increased [179, 181, 189, 190]. Adenotonsillectomy for OSAS is accompanied by a reduction of morning venous BNP levels in childhood [191]. Significant increases in plasma ADH and significant decreases in plasma BNP were observed in all children, with no difference between responders and nonresponders to surgery for OSAS [174]. A significant increase in plasma ADH and a significant decrease in plasma BNP were also recorded after adenotonsillectomy in all children, with no difference between those who became dry and those who remained wet [192].
A summary of the putative mechanisms for pathogenesis of enuresis in patients with sleep disordered breathing is shown in figure 3.
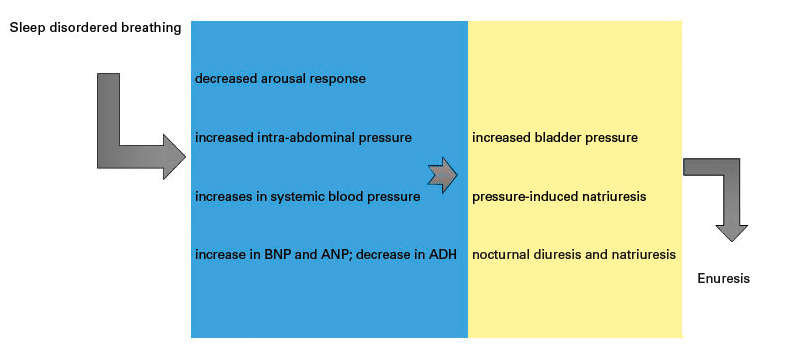
Figure 3 Putative mechanisms for pathogenesis of enuresis in patients with sleep disordered breathing
ADH = antidiuretic hormone; ANP = atrial natriuretic peptide; BNP = brain natriuretic peptide
A summary of the studies concerning the urological outcome of treatment for obstructive SDB in children with enuresis is shown in table 1.
Table 1 Urological outcome of the treatment for sleep disordered breathing in children with enuresis.
| Authors [ref.] | Population | Intervention | Outcome | Study design | Strength of the evidence (therapy) |
|---|---|---|---|---|---|
| Alexopoulos et al., 2005 [193] | 8-year-old boy and 7-year-old girl with primary NE, chronic nasal obstruction, and loud snoring | Nasal budesonide | Resolution of enuresis (2–4 weeks) | Case reports | 4 |
| Firoozi F et al., 2006 [9] | 86 patients; 42% with NE | A&T | 12 patients (33%) had complete resolution, 11 (31%) had significant improvement and 13 (36%) showed no change | Prospective population-based study | 2c |
| Basha S et al., 2005 [162] | 326 patients aged 2–18 years over a 44-month period; 32.8% children with a positive history of enuresis of whom 53.3% agreed to participate in the second phase of the study | Tonsillectomy or adenoidectomy | 61.4% of the children were free of enuresis, 22.8% had a decrease in enuresis, and 15.8% had no change in enuresis. | Retrospective chart review with prospective collection of data | 2c |
| Cinar U et al., 2001 [140] | 321 children (5–16 years), 35% had NE | A&T | 64/111 were evaluated postoperatively: after 3 months. 63% were free of their complaints; 4% reported a decrease in the frequency of NE; 24/111 had no change in their complaints | Population-based study | 2c |
| Weider DJ et al., 1991 [142] | 115 children (3–19 years) | A&T | Significant decrease in or complete cure of nocturnal enuresis in 87 (76%) | Population-based study | 2c |
| Leiberman et al., 2006 [166] | All relevant published data by the Soroka University Medical Center compared with MEDLINE linked literature | A&T | Reduction of nocturnal enuresis | Narrative (review article) | - |
| Weissbach et al., 2006 [167] | 161 children (4–18 years of age); 42 had enuresis; | A&T | 27 of these 42 underwent A&T: in 41% enuresis totally disappeared within 1 month | Retrospective review of clinical data | 2c |
| Kovacevic L et al., 2013 [168] | 417 children (5–18 years of age); 24% had NE | Tonsillectomy and/or adenoidectomy | 49% responded to A&T; of these, 61% resolved within 1 month postoperatively | Observational, pilot study | 2c |
| Kovacevic L et al., 2014 [192] | 46 children (8.79 ± 2.41 years) | A&T | 43.5% of patients became dry; those who became dry had more frequent arousal episodes from apnoea events | Prospective study | 2c |
| Ahmadi MS et al., 2013 [194] | 97 children aged 3–12 years | A&T | 3 months after A&T, NE had resolved completely in 60.7% children and had shown relative improvement in 26.2% children | Prospective cohort study | 2c |
| Jeyakumar A et al., 2012 [195] | 14 studies, 3 550 children (18 months to 19 years) had SDB, one-third had a diagnosis of NE | A&T | Preoperative prevalence of NE was 31%; postoperative prevalence of NE was 16% | Systematic review | 3a |
| Kalorin CM et al., 2010 [169] | 326 toilet-trained children 3–15 years old; 257 in the tonsillectomy group and 69 in the control group | Tonsillectomy | Cure rates for NE and daytime incontinence at 3 and 6 months postoperatively, respectively, were 40% and 50% in the tonsillectomy group (p = 0.60), and 35% and 48% in the control group | Prospective study | 2c |
| Kovacevic L et al., 2015 [64] | 30 children in the study group vs 30 age-matched controls before and 4 weeks after T&A | T&A | Improvement was shown for HRQoL in children with both SDB and NE (study group) and children with SDB without NE (controls) | Prospective study | 2c |
| Park S, et al. 2016 [196] | 183 children (8.17 ± 2.84 years), 9.3% with NE. | A&T | After A&T, 76.5% showed complete resolution of NE | Prospective study | 2c |
| Nevéus T et al., 2014 [157] | 34 children (10.7 ± 1.8 years) | Orthodontic widening of the palate | Proportions of responders, intermediate responders and nonresponders during treatment were 21.2%, 27.3% and 51.5%, respectively | Clinical trial | 2c |
| Timms DJ, 1990 [197] | 10 children (6.5–15.5 years) | RME | NE ceased within a few months of maxillary expansion | Prospective study | 4 |
| Kurol J, Modin H, 1998 [198] | 10 children (8–13 years) | RME | Within 1 month of RME of 3 to 5 mm, 4 children were completely dry and 3 showed notable improvement | Prospective study | 4 |
A&T = adenotonsillectomy; HRQoL = health-related quality of life; NE = nocturnal enuresis; RME = rapid maxillary expansion; SDB = sleep-disordered breathing
Administration of nasal corticosteroids was associated with resolution of nocturnal enuresis in two children with mild obstructive SDB [193]. Moreover, tonsillectomy and/or adenotonsillectomy have been frequently associated with a high resolution rate of childhood nocturnal enuresis [9, 140, 142, 162, 166–168, 192, 194–196], although this evidence could not be confirmed in one study [169], which considered grading of tonsillar hypertrophy, but not OSAS grading by polysomnography. adenotonsillectomy significantly improved the HRQoL in all children with obstructive SDB and nocturnal enuresis, regardless of nocturnal enuresis outcomes [64].
Rapid maxillary expansion produces an immediate change in transverse dimensions of the nasal cavity, circum-maxillary sutures and aperture width [199]. The positive impact of rapid maxillary expansion on respiration could possibly explain its antienuretic effect in some patients who might have a coexistent OSAS and a nocturnal respiratory problem [157, 200]. In children with obstructive SDB and therapy-resistant nocturnal enuresis, rapid maxillary expansion may prove to be a harmless and curative therapy for both problems [148, 197, 198].
Some limitations of these studies should be addressed. In particular, none of the outcome studies were peer reviewed, randomised or quasi-randomised (e.g., controlled before-and-after studies, interrupted time series) and controlled. On the contrary, the studies were mostly retrospective/prospective/observational. The strength of an evidence analysis showed that 12 out of the 17 studies were of 2c level. Moreover, some studies (table 1) included children under 5 years old [142, 162, 167, 169, 194, 195] and the improvement in these younger children may be related to natural development.
Nocturnal enuresis and obstructive SDB are both frequent problems of sleep that coexist in childhood. nocturnal enuresis is diagnosed and treated by a primary paediatrician or family practitioner; if the diagnosis is doubtful, the children may be referred to a paediatric urologist. Other studies found that children with OSAS had frequent bedwetting. Although a vast amount of information is now available regarding the relationship between nocturnal enuresis and obstructive SDB, many of the published studies were uncontrolled, retrospective or prospective cohort studies (grade C recommendation). A correlation between the two conditions is frequently reported, and resolution of nocturnal enuresis following medical or surgical treatment for obstructive SDB is emphasised. Both disorders have an underlying sleep disturbance characterised by altered arousal response and sleep fragmentation. The pathophysiology of enuretic events is seemingly linked to nocturnal obstructive events, causing increased intra-abdominal pressure, altered systemic blood pressure that induces natriuresis and polyuria by altering ADH, ANP and BNP levels. Treatment of obstructive SDB, mainly due to tonsil and adenoid hypertrophy, leads to significant resolution of nocturnal enuresis in most patients, accompanied by normalisation of ADH, ANP and BNP levels, and concomitant improvement of HRQoL.
In summary, since our information comes from observational studies, there is a need to further explore these correlations in controlled studies. In the meantime, symptoms of OSAS such as snoring, sleep apnoea and restless sleep should be sought for all children with nocturnal enuresis. Confirmed obstructive SDB should be treated promptly; the persistence of nocturnal enuresis afterwards would require treatment following the standard protocol.
No financial support and no other potential conflict of interest relevant to this article was reported.
1 Kaditis AG , Alonso Alvarez ML , Boudewyns A , Alexopoulos EI , Ersu R , Joosten K , et al. Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J. 2016;47(1):69–94.https://doi.org/10.1183/13993003.00385-2015
2 Anuntaseree W , Rookkapan K , Kuasirikul S , Thongsuksai P . Snoring and obstructive sleep apnea in Thai school-age children: prevalence and predisposing factors. Pediatr Pulmonol. 2001;32(3):222–7.https://doi.org/10.1002/ppul.1112
3 Brunetti L , Rana S , Lospalluti ML , Pietrafesa A , Francavilla R , Fanelli M , et al. Prevalence of obstructive sleep apnea syndrome in a cohort of 1,207 children of southern Italy. Chest. 2001;120(6):1930–5.https://doi.org/10.1378/chest.120.6.1930
4 Lumeng JC , Chervin RD . Epidemiology of pediatric obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):242–52.https://doi.org/10.1513/pats.200708-135MG
5 Montgomery-Downs HE , O’Brien LM , Holbrook CR , Gozal D . Snoring and sleep-disordered breathing in young children: subjective and objective correlates. Sleep. 2004;27(1):87–94.
6 Chang SJ , Chae KY . Obstructive sleep apnea syndrome in children: Epidemiology, pathophysiology, diagnosis and sequelae. Korean J Pediatr. 2010;53(10):863–71.https://doi.org/10.3345/kjp.2010.53.10.863
7 Chervin RD , Ellenberg SS , Hou X , Marcus CL , Garetz SL , Katz ES , et al.; Childhood Adenotonsillectomy Trial. Prognosis for Spontaneous Resolution of OSA in Children. Chest. 2015;148(5):1204–13.https://doi.org/10.1378/chest.14-2873
8 Byrd RS , Weitzman M , Lanphear NE , Auinger P . Bed-wetting in US children: epidemiology and related behavior problems. Pediatrics. 1996;98(3 Pt 1):414–9.
9 Firoozi F , Batniji R , Aslan AR , Longhurst PA , Kogan BA . Resolution of diurnal incontinence and nocturnal enuresis after adenotonsillectomy in children. J Urol. 2006;175(5):1885–8, discussion 1888.https://doi.org/10.1016/S0022-5347(05)00935-3
10 Burg CJ , Friedman NR . Diagnosis and treatment of sleep apnea in adolescents. Adolesc Med State Art Rev. 2010;21(3):457–79, viii. [viii.].
11 Schechter MS ; Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea Syndrome. Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109(4):e69.https://doi.org/10.1542/peds.109.4.e69
12 Bhattacharjee R , Kheirandish-Gozal L , Spruyt K , Mitchell RB , Promchiarak J , Simakajornboon N , et al. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: a multicenter retrospective study. Am J Respir Crit Care Med. 2010;182(5):676–83.https://doi.org/10.1164/rccm.200912-1930OC
13 Guilleminault C , Pelayo R , Leger D , Clerk A , Bocian RC . Recognition of sleep-disordered breathing in children. Pediatrics. 1996;98(5):871–82.
14 Behlfelt K , Linder-Aronson S , McWilliam J , Neander P , Laage-Hellman J . Cranio-facial morphology in children with and without enlarged tonsils. Eur J Orthod. 1990;12(3):233–43.https://doi.org/10.1093/ejo/12.3.233
15 Oulis CJ , Vadiakas GP , Ekonomides J , Dratsa J . The effect of hypertrophic adenoids and tonsils on the development of posterior crossbite and oral habits. J Clin Pediatr Dent. 1994;18(3):197–201.
16 Cheng MC , Enlow DH , Papsidero M , Broadbent BH, Jr , Oyen O , Sabat M . Developmental effects of impaired breathing in the face of the growing child. Angle Orthod. 1988;58(4):309–20.
17 Kushida CA , Efron B , Guilleminault C . A predictive morphometric model for the obstructive sleep apnea syndrome. Ann Intern Med. 1997;127(8 Pt 1):581–7.https://doi.org/10.7326/0003-4819-127-8_Part_1-199710150-00001
18 Villa MP , Bernkopf E , Pagani J , Broia V , Montesano M , Ronchetti R . Randomized controlled study of an oral jaw-positioning appliance for the treatment of obstructive sleep apnea in children with malocclusion. Am J Respir Crit Care Med. 2002;165(1):123–7.https://doi.org/10.1164/ajrccm.165.1.2011031
19 Côté V , Ruiz AG , Perkins J , Sillau S , Friedman NR . Characteristics of children under 2 years of age undergoing tonsillectomy for upper airway obstruction. Int J Pediatr Otorhinolaryngol. 2015;79(6):903–8.https://doi.org/10.1016/j.ijporl.2015.04.003
20 Van Eyck A , Van Hoorenbeeck K , De Winter BY , Van Gaal L , De Backer W , Verhulst SL . Sleep-disordered breathing and pulmonary function in obese children and adolescents. Sleep Med. 2014;15(8):929–33.https://doi.org/10.1016/j.sleep.2014.03.024
21 Alonso-Álvarez ML , Cordero-Guevara JA , Terán-Santos J , Gonzalez-Martinez M , Jurado-Luque MJ , Corral-Peñafiel J , et al. Obstructive sleep apnea in obese community-dwelling children: the NANOS study. Sleep. 2014;37(5):943–9.
22 Schlüter B , De Sousa G , Trowitzsch E , Andler W . Diagnostics and management of sleep-related respiratory disturbances in children with skeletal dysplasia caused by FGFR3 mutations (achondroplasia and hypochondroplasia). Georgian Med News. 2011;196–197(196-197):63–72.
23 Goldstein NA , Pugazhendhi V , Rao SM , Weedon J , Campbell TF , Goldman AC , et al. Clinical assessment of pediatric obstructive sleep apnea. Pediatrics. 2004;114(1):33–43.https://doi.org/10.1542/peds.114.1.33
24 Montgomery-Downs HE , O’Brien LM , Gulliver TE , Gozal D . Polysomnographic characteristics in normal preschool and early school-aged children. Pediatrics. 2006;117(3):741–53.https://doi.org/10.1542/peds.2005-1067
25 Blunden S , Lushington K , Lorenzen B , Martin J , Kennedy D . Neuropsychological and psychosocial function in children with a history of snoring or behavioral sleep problems. J Pediatr. 2005;146(6):780–6.https://doi.org/10.1016/j.jpeds.2005.01.043
26 Brockmann PE , Urschitz MS , Noehren A , Sokollik C , Schlaud M , Poets CF . Risk factors and consequences of excessive autonomic activation during sleep in children. Sleep Breath. 2011;15(3):409–16.https://doi.org/10.1007/s11325-010-0349-0
27 Urschitz MS , Eitner S , Guenther A , Eggebrecht E , Wolff J , Urschitz-Duprat PM , et al. Habitual snoring, intermittent hypoxia, and impaired behavior in primary school children. Pediatrics. 2004;114(4):1041–8.https://doi.org/10.1542/peds.2003-1145-L
28 O’Brien LM , Mervis CB , Holbrook CR , Bruner JL , Smith NH , McNally N , et al. Neurobehavioral correlates of sleep-disordered breathing in children. J Sleep Res. 2004;13(2):165–72.https://doi.org/10.1111/j.1365-2869.2004.00395.x
29 Beebe DW , Rausch J , Byars KC , Lanphear B , Yolton K . Persistent snoring in preschool children: predictors and behavioral and developmental correlates. Pediatrics. 2012;130(3):382–9.https://doi.org/10.1542/peds.2012-0045
30 Tarasiuk A , Greenberg-Dotan S , Simon-Tuval T , Freidman B , Goldbart AD , Tal A , et al. Elevated morbidity and health care use in children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2007;175(1):55–61.https://doi.org/10.1164/rccm.200604-577OC
31 Kikuchi M , Higurashi N , Miyazaki S , Itasaka Y , Chiba S , Nezu H . Facial pattern categories of sleep breathing-disordered children using Ricketts analysis. Psychiatry Clin Neurosci. 2002;56(3):329–30.https://doi.org/10.1046/j.1440-1819.2002.01002.x
32 Arens R , Sin S , Willen S , Bent J , Parikh SR , Freeman K , et al. Rhino-sinus involvement in children with obstructive sleep apnea syndrome. Pediatr Pulmonol. 2010;45(10):993–8.https://doi.org/10.1002/ppul.21284
33 Halbower AC , Degaonkar M , Barker PB , Earley CJ , Marcus CL , Smith PL , et al. Childhood obstructive sleep apnea associates with neuropsychological deficits and neuronal brain injury. PLoS Med. 2006;3(8):e301.https://doi.org/10.1371/journal.pmed.0030301
34 Hogan AM , Hill CM , Harrison D , Kirkham FJ . Cerebral blood flow velocity and cognition in children before and after adenotonsillectomy. Pediatrics. 2008;122(1):75–82.https://doi.org/10.1542/peds.2007-2540
35 Beebe DW , Gozal D . Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. J Sleep Res. 2002;11(1):1–16.https://doi.org/10.1046/j.1365-2869.2002.00289.x
36 Chan KC , Shi L , So HK , Wang D , Liew AWC , Rasalkar DD , et al. Neurocognitive dysfunction and grey matter density deficit in children with obstructive sleep apnoea. Sleep Med. 2014;15(9):1055–61.https://doi.org/10.1016/j.sleep.2014.04.011
37 Busch DR , Lynch JM , Winters ME , McCarthy AL , Newland JJ , Ko T , et al. Cerebral Blood Flow Response to Hypercapnia in Children with Obstructive Sleep Apnea Syndrome. Sleep. 2016;39(1):209–16.https://doi.org/10.5665/sleep.5350
38 Esposito M , Antinolfi L , Gallai B , Parisi L , Roccella M , Marotta R , et al. Executive dysfunction in children affected by obstructive sleep apnea syndrome: an observational study. Neuropsychiatr Dis Treat. 2013;9:1087–94.https://doi.org/10.2147/NDT.S47287
39 Gozal D , Kheirandish-Gozal L . Obesity and excessive daytime sleepiness in prepubertal children with obstructive sleep apnea. Pediatrics. 2009;123(1):13–8.https://doi.org/10.1542/peds.2008-0228
40 Gozal D , Wang M , Pope DW, Jr . Objective sleepiness measures in pediatric obstructive sleep apnea. Pediatrics. 2001;108(3):693–7.https://doi.org/10.1542/peds.108.3.693
41 Rosen CL , Palermo TM , Larkin EK , Redline S . Health-related quality of life and sleep-disordered breathing in children. Sleep. 2002;25(6):657–66.
42 Mitchell RB , Kelly J . Behavior, neurocognition and quality-of-life in children with sleep-disordered breathing. Int J Pediatr Otorhinolaryngol. 2006;70(3):395–406.https://doi.org/10.1016/j.ijporl.2005.10.020
43 Xanthopoulos MS , Gallagher PR , Berkowitz RI , Radcliffe J , Bradford R , Marcus CL . Neurobehavioral functioning in adolescents with and without obesity and obstructive sleep apnea. Sleep. 2015;38(3):401–10.
44 Beebe DW . Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents. Pediatr Clin North Am. 2011;58(3):649–65.https://doi.org/10.1016/j.pcl.2011.03.002
45 Owens JA . Neurocognitive and behavioral impact of sleep disordered breathing in children. Pediatr Pulmonol. 2009;44(5):417–22.https://doi.org/10.1002/ppul.20981
46 Biggs SN , Walter LM , Jackman AR , Nisbet LC , Weichard AJ , Hollis SL , et al. Longitudinal Impact of Resolution of Snoring in Young Children on Psychosocial Functioning. J Pediatr. 2015;167(6):1272–9.e1.https://doi.org/10.1016/j.jpeds.2015.09.016
47 Galland B , Spruyt K , Dawes P , McDowall PS , Elder D , Schaughency E . Sleep Disordered Breathing and Academic Performance: A Meta-analysis. Pediatrics. 2015;136(4):e934–46.https://doi.org/10.1542/peds.2015-1677
48 Pietropaoli N , Supino MC , Vitelli O , Rabasco J , Evangelisti M , Forlani M , et al. Cognitive function in preschool children with sleep-disordered breathing. Sleep Breath. 2015;19(4):1431–7.https://doi.org/10.1007/s11325-015-1157-3
49 Chervin RD . Periodic leg movements and sleepiness in patients evaluated for sleep-disordered breathing. Am J Respir Crit Care Med. 2001;164(8 Pt 1):1454–8.https://doi.org/10.1164/ajrccm.164.8.2011062
50 Chervin RD , Dillon JE , Bassetti C , Ganoczy DA , Pituch KJ . Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep. 1997;20(12):1185–92.
51 Amiri S , AbdollahiFakhim S , Lotfi A , Bayazian G , Sohra BP our M , Hemmatjoo T . Effect of adenotonsillectomy on ADHD symptoms of children with adenotonsillar hypertrophy and sleep disordered breathing. Int J Pediatr Otorhinolaryngol. 2015;79(8):1213–7.https://doi.org/10.1016/j.ijporl.2015.05.015
52 Garetz SL . Behavior, cognition, and quality of life after adenotonsillectomy for pediatric sleep-disordered breathing: summary of the literature. Otolaryngol Head Neck Surg. 2008;138(1, Suppl):S19–26.https://doi.org/10.1016/j.otohns.2007.06.738
53 Mitchell RB , Kelly J . Outcomes and quality of life following adenotonsillectomy for sleep-disordered breathing in children. ORL J Otorhinolaryngol Relat Spec. 2007;69(6):345–8.https://doi.org/10.1159/000108366
54 Flanary VA . Long-term effect of adenotonsillectomy on quality of life in pediatric patients. Laryngoscope. 2003;113(10):1639–44.https://doi.org/10.1097/00005537-200310000-00003
55 Goldstein NA , Fatima M , Campbell TF , Rosenfeld RM . Child behavior and quality of life before and after tonsillectomy and adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002;128(7):770–5.https://doi.org/10.1001/archotol.128.7.770
56 Mitchell RB , Kelly J , Call E , Yao N . Quality of life after adenotonsillectomy for obstructive sleep apnea in children. Arch Otolaryngol Head Neck Surg. 2004;130(2):190–4.https://doi.org/10.1001/archotol.130.2.190
57 McNamara F , Issa FG , Sullivan CE . Arousal pattern following central and obstructive breathing abnormalities in infants and children. J Appl Physiol (1985). 1996;81(6):2651–7.
58 Tauman R , O’Brien LM , Holbrook CR , Gozal D . Sleep pressure score: a new index of sleep disruption in snoring children. Sleep. 2004;27(2):274–8.
59 Brietzke SE , Katz ES , Roberson DW . Pulse transit time as a screening test for pediatric sleep-related breathing disorders. Arch Otolaryngol Head Neck Surg. 2007;133(10):980–4.https://doi.org/10.1001/archotol.133.10.980
60 Walter LM , Nixon GM , Davey MJ , Anderson V , Walker AM , Horne RS . Autonomic dysfunction in children with sleep disordered breathing. Sleep Breath. 2013;17(2):605–13.https://doi.org/10.1007/s11325-012-0727-x
61 Walter LM , Biggs SN , Nisbet LC , Weichard AJ , Muntinga M , Davey MJ , et al. Augmented cardiovascular responses to episodes of repetitive compared with isolated respiratory events in preschool children with sleep-disordered breathing. Pediatr Res. 2015;78(5):560–6.https://doi.org/10.1038/pr.2015.147
62 Katz ES , Lutz J , Black C , Marcus CL . Pulse transit time as a measure of arousal and respiratory effort in children with sleep-disordered breathing. Pediatr Res. 2003;53(4):580–8.https://doi.org/10.1203/01.PDR.0000057206.14698.47
63 Kontos A , van den Heuvel C , Pamula Y , Martin J , Lushington K , Baumert M , et al. Delayed brachial artery dilation response and increased resting blood flow velocity in young children with mild sleep-disordered breathing. Sleep Med. 2015;16(12):1451–6.https://doi.org/10.1016/j.sleep.2015.08.004
64 Kovacevic L , Lu H , Wolfe-Christensen C , Abdulhamid I , Thottam PJ , Lulgjuraj M , et al. Adenotonsillectomy Normalizes Hormones and Urinary Electrolytes in Children With Nocturnal Enuresis and Sleep-Disordered Breathing. Urology. 2015;86(1):158–61.https://doi.org/10.1016/j.urology.2015.04.011
65 Loffredo L , Zicari AM , Occasi F , Perri L , Carnevale R , Angelico F , et al. Endothelial dysfunction and oxidative stress in children with sleep disordered breathing: role of NADPH oxidase. Atherosclerosis. 2015;240(1):222–7.https://doi.org/10.1016/j.atherosclerosis.2015.03.024
66 Simsek A , Bayraktar C , Dogan S , Uckardes F , Reyhan AH , Sarikaya Y , et al. Retinal Nerve Fiber Layer Thickness Alteration in Apneic Children. Optom Vis Sci. 2016;93(1):63–9.
67 Austin PF , Bauer SB , Bower W , Chase J , Franco I , Hoebeke P , et al. The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children’s Continence Society. Neurourol Urodyn. 2016;35(4):471–81.https://doi.org/10.1002/nau.22751
68 Lottmann HB , Alova I . Primary monosymptomatic nocturnal enuresis in children and adolescents. Int J Clin Pract Suppl. 2007;61(155):8–16.https://doi.org/10.1111/j.1742-1241.2007.01464.x
69 Butler RJ , Holland P . The three systems: a conceptual way of understanding nocturnal enuresis. Scand J Urol Nephrol. 2000;34(4):270–7.https://doi.org/10.1080/003655900750042022
70 Hjalmas K , Arnold T , Bower W , Caione P , Chiozza LM , von Gontard A , et al. Nocturnal enuresis: an international evidence based management strategy. J Urol. 2004;171(6 Pt 2):2545–61.https://doi.org/10.1097/01.ju.0000111504.85822.b2
71 Lee SD , Sohn DW , Lee JZ , Park NC , Chung MK . An epidemiological study of enuresis in Korean children. BJU Int. 2000;85(7):869–73.https://doi.org/10.1046/j.1464-410x.2000.00617.x
72 Forsythe WI , Redmond A . Enuresis and spontaneous cure rate. Study of 1129 enuretis. Arch Dis Child. 1974;49(4):259–63.https://doi.org/10.1136/adc.49.4.259
73 Kuehhas FE , Djakovic N , Hohenfellner M . Infantile Enuresis: Current State-of-the-Art Therapy and Future Trends. Rev Urol. 2011;13(1):1–5.
74 Nevéus T . Diagnosis and management of nocturnal enuresis. Curr Opin Pediatr. 2009;21(2):199–202.https://doi.org/10.1097/MOP.0b013e3283229b12
75 Wille S . Nocturnal enuresis: sleep disturbance and behavioural patterns. Acta Paediatr. 1994;83(7):772–4.https://doi.org/10.1111/j.1651-2227.1994.tb13136.x
76 Robson WL . Clinical practice. Evaluation and management of enuresis. N Engl J Med. 2009;360(14):1429–36.https://doi.org/10.1056/NEJMcp0808009
77 Dehoorne JL , Walle CV , Vansintjan P , Raes AM , De Guchtenaere ARP , Van Laecke E , et al. Characteristics of a tertiary center enuresis population, with special emphasis on the relation among nocturnal diuresis, functional bladder capacity and desmopressin response. J Urol. 2007;177(3):1130–7.https://doi.org/10.1016/j.juro.2006.10.093
78 Yeung CK , Diao M , Sreedhar B . Cortical arousal in children with severe enuresis. N Engl J Med. 2008;358(22):2414–5.https://doi.org/10.1056/NEJMc0706528
79 Charalampous S , Printza N , Hashim H , Bantouraki M , Rompis V , Ioannidis E , et al. Bladder wall thickness and urodynamic correlation in children with primary nocturnal enuresis. J Pediatr Urol. 2013;9(3):334–8.https://doi.org/10.1016/j.jpurol.2012.04.008
80 Ryu DS , Lee HW , Kwak KW , Park KH , Baek M . Role of Urodynamic Study in Nocturnal Enuresis: Urodynamic Findings and Treatment Outcome Correlation in Children with Pharmacotherapy-resistant Monosymptomatic Nocturnal Enuresis or Severe Non-monosymptomatic Nocturnal Enuresis. Low Urin Tract Symptoms. 2014;6(2):88–93.https://doi.org/10.1111/luts.12024
81 Wolfish NM , Pivik RT , Busby KA . Elevated sleep arousal thresholds in enuretic boys: clinical implications. Acta Paediatr. 1997;86(4):381–4.https://doi.org/10.1111/j.1651-2227.1997.tb09027.x
82 Wolfish N . Sleep arousal function in enuretic males. Scand J Urol Nephrol Suppl. 1999;202(33):24–6.https://doi.org/10.1080/003655999750169402
83 Butler RJ . Childhood nocturnal enuresis: developing a conceptual framework. Clin Psychol Rev. 2004;24(8):909–31.https://doi.org/10.1016/j.cpr.2004.07.001
84 Fujiwara J , Kimura S , Tsukayama H , Nakahara S , Haibara S , Fujita M , et al. Evaluation of the autonomic nervous system function in children with primary monosymptomatic nocturnal enuresis--power spectrum analysis of heart rate variability using 24-hour Holter electrocardiograms. Scand J Urol Nephrol. 2001;35(5):350–6.https://doi.org/10.1080/003655901753224396
85 Unalacak M , Aydin M , Ermis B , Ozeren A , Sogut A , Demirel F , et al. Assessment of cardiac autonomic regulation in children with monosymptomatic nocturnal enuresis by analysis of heart rate variability. Tohoku J Exp Med. 2004;204(1):63–9.https://doi.org/10.1620/tjem.204.63
86 Bader G , Nevéus T , Kruse S , Sillén U . Sleep of primary enuretic children and controls. Sleep. 2002;25(5):579–83.
87 Kruse A , Mahler B , Rittig S , Djurhuus JC . Increased nocturnal blood pressure in enuretic children with polyuria. J Urol. 2009;182(4, Suppl):1954–60.https://doi.org/10.1016/j.juro.2009.04.079
88 Yoshimura N , Miyazato M , Kitta T , Yoshikawa S . Central nervous targets for the treatment of bladder dysfunction. Neurourol Urodyn. 2014;33(1):59–66.https://doi.org/10.1002/nau.22455
89 Dhondt K , Van Herzeele C , Roels SP , Raes A , Groen L-A , Hoebeke P , et al. Sleep fragmentation and periodic limb movements in children with monosymptomatic nocturnal enuresis and polyuria. Pediatr Nephrol. 2015;30(7):1157–62.https://doi.org/10.1007/s00467-015-3044-3
90 Kamperis K , Rittig S , Bower WF , Djurhuus JC . Effect of indomethacin on desmopressin resistant nocturnal polyuria and nocturnal enuresis. J Urol. 2012;188(5):1915–22.https://doi.org/10.1016/j.juro.2012.07.019
91 Kamperis K , Rittig S , Jørgensen KA , Djurhuus JC . Nocturnal polyuria in monosymptomatic nocturnal enuresis refractory to desmopressin treatment. Am J Physiol Renal Physiol. 2006;291(6):F1232–40.https://doi.org/10.1152/ajprenal.00134.2006
92 Rittig S , Knudsen UB , Nørgaard JP , Pedersen EB , Djurhuus JC . Abnormal diurnal rhythm of plasma vasopressin and urinary output in patients with enuresis. Am J Physiol. 1989;256(4 Pt 2):F664–71.
93 Rittig S , Schaumburg HL , Siggaard C , Schmidt F , Djurhuus JC . The circadian defect in plasma vasopressin and urine output is related to desmopressin response and enuresis status in children with nocturnal enuresis. J Urol. 2008;179(6):2389–95.https://doi.org/10.1016/j.juro.2008.01.171
94 Dossche L , Raes A , Hoebeke P , De Bruyne P , Vande Walle J . Circadian Rhythm of Glomerular Filtration and Solute Handling Related to Nocturnal Enuresis. J Urol. 2016;195(1):162–7.https://doi.org/10.1016/j.juro.2015.07.079
95 Wille S . Primary nocturnal enuresis in children. Background and treatment. Scand J Urol Nephrol Suppl. 1994;156:1–48.
96 Aikawa T , Kasahara T , Uchiyama M . The arginine-vasopressin secretion profile of children with primary nocturnal enuresis. Eur Urol. 1998;33(Suppl 3):41–4.https://doi.org/10.1159/000052242
97 Sans Capdevila O , Crabtree VM , Kheirandish-Gozal L , Gozal D . Increased morning brain natriuretic peptide levels in children with nocturnal enuresis and sleep-disordered breathing: a community-based study. Pediatrics. 2008;121(5):e1208–14.https://doi.org/10.1542/peds.2007-2049
98 Van Hoeck K , Bael A , Lax H , Hirche H , van Gool JD . Circadian variation of voided volume in normal school-age children. Eur J Pediatr. 2007;166(6):579–84.https://doi.org/10.1007/s00431-006-0286-x
99 De Guchtenaere A , Vande Walle C , Van Sintjan P , Raes A , Donckerwolcke R , Van Laecke E , et al. Nocturnal polyuria is related to absent circadian rhythm of glomerular filtration rate. J Urol. 2007;178(6):2626–9.https://doi.org/10.1016/j.juro.2007.08.028
100 Inoue M , Shimojima H , Chiba H , Tsukahara N , Tajika Y , Taka K . Rhythmic slow wave observed on nocturnal sleep encephalogram in children with idiopathic nocturnal enuresis. Sleep. 1987;10(6):570–9.
101 Nørgaard JP , Hansen JH , Nielsen JB , Rittig S , Djurhuus JC . Nocturnal studies in enuretics. A polygraphic study of sleep-EEG and bladder activity. Scand J Urol Nephrol Suppl. 1989;125:73–8.
102 Gillin JC , Rapoport JL , Mikkelsen EJ , Langer D , Vanskiver C , Mendelson W . EEG sleep patterns in enuresis: a further analysis and comparison with normal controls. Biol Psychiatry. 1982;17(8):947–53.
103 Mazza M , Faia V , Paciello N , Della Marca G , Mazza S . Sleep disorders in childhood: a review. Clin Ter. 2002;153(3):189–93.
104 Hunsballe JM . Increased delta component in computerized sleep electroencephalographic analysis suggests abnormally deep sleep in primary monosymptomatic nocturnal enuresis. Scand J Urol Nephrol. 2000;34(5):294–302.https://doi.org/10.1080/003655900750048305
105 Mikkelsen EJ , Rapoport JL , Nee L , Gruenau C , Mendelson W , Gillin JC . Childhood enuresis. I. Sleep patterns and psychopathology. Arch Gen Psychiatry. 1980;37(10):1139–44.https://doi.org/10.1001/archpsyc.1980.01780230057008
106 Nevéus T , Stenberg A , Läckgren G , Tuvemo T , Hetta J . Sleep of children with enuresis: a polysomnographic study. Pediatrics. 1999;103(6 Pt 1):1193–7.https://doi.org/10.1542/peds.103.6.1193
107 Nørgaard JP , Hansen JH , Wildschiøtz G , Sørensen S , Rittig S , Djurhuus JC . Sleep cystometries in children with nocturnal enuresis. J Urol. 1989;141(5):1156–9.
108 Nevéus T . Enuretic sleep: deep, disturbed or just wet? Pediatr Nephrol. 2008;23(8):1201–2.https://doi.org/10.1007/s00467-008-0859-1
109 Nevéus T . The role of sleep and arousal in nocturnal enuresis. Acta Paediatr. 2003;92(10):1118–23.https://doi.org/10.1111/j.1651-2227.2003.tb02469.x
110 Dhondt K , Raes A , Hoebeke P , Van Laecke E , Van Herzeele C , Vande Walle J . Abnormal sleep architecture and refractory nocturnal enuresis. J Urol. 2009;182(4, Suppl):1961–6.https://doi.org/10.1016/j.juro.2009.05.103
111 Cohen-Zrubavel V , Kushnir B , Kushnir J , Sadeh A . Sleep and sleepiness in children with nocturnal enuresis. Sleep. 2011;34(2):191–4.
112 Dhondt K , Baert E , Van Herzeele C , Raes A , Groen L-A , Hoebeke P , et al. Sleep fragmentation and increased periodic limb movements are more common in children with nocturnal enuresis. Acta Paediatr. 2014;103(6):e268–72.https://doi.org/10.1111/apa.12610
113 Nevéus T , Läckgren G , Stenberg A , Tuvemo T , Hetta J . Sleep and night-time behaviour of enuretics and non-enuretics. Br J Urol. 1998;81(s3, Suppl 3):67–71.https://doi.org/10.1046/j.1464-410x.1998.00011.x
114 Mahler B , Kamperis K , Schroeder M , Frøkiær J , Djurhuus JC , Rittig S . Sleep deprivation induces excess diuresis and natriuresis in healthy children. Am J Physiol Renal Physiol. 2012;302(2):F236–43.https://doi.org/10.1152/ajprenal.00283.2011
115 Gozmen S , Keskin S , Akil I . Enuresis nocturna and sleep quality. Pediatr Nephrol. 2008;23(8):1293–6.https://doi.org/10.1007/s00467-008-0817-y
116 Kushnir J , Cohen-Zrubavel V , Kushnir B . Night diapers use and sleep in children with enuresis. Sleep Med. 2013;14(10):1013–6.https://doi.org/10.1016/j.sleep.2013.02.018
117 Üçer O , Gümüş B . Quantifying subjective assessment of sleep quality, quality of life and depressed mood in children with enuresis. World J Urol. 2014;32(1):239–43.https://doi.org/10.1007/s00345-013-1193-1
118 von Gontard A , Baeyens D , Van Hoecke E , Warzak WJ , Bachmann C . Psychological and psychiatric issues in urinary and fecal incontinence. J Urol. 2011;185(4):1432–7.https://doi.org/10.1016/j.juro.2010.11.051
119 Wolfe-Christensen C , Veenstra AL , Kovacevic L , Elder JS , Lakshmanan Y . Psychosocial difficulties in children referred to pediatric urology: a closer look. Urology. 2012;80(4):907–13.https://doi.org/10.1016/j.urology.2012.04.077
120 Bourke R , Anderson V , Yang JS , Jackman AR , Killedar A , Nixon GM , et al. Cognitive and academic functions are impaired in children with all severities of sleep-disordered breathing. Sleep Med. 2011;12(5):489–96.https://doi.org/10.1016/j.sleep.2010.11.010
121 Beebe DW . Neural and neurobehavioral dysfunction in children with obstructive sleep apnea. PLoS Med. 2006;3(8):e323.https://doi.org/10.1371/journal.pmed.0030323
122 Abou-Khadra MK , Amin OR , Ahmed D . Association between sleep and behavioural problems among children with enuresis. J Paediatr Child Health. 2013;49(2):E160–6.https://doi.org/10.1111/jpc.12017
123 Hjälmås K . Nocturnal enuresis: basic facts and new horizons. Eur Urol. 1998;33(Suppl 3):53–7.https://doi.org/10.1159/000052245
124 Ertan P , Yilmaz O , Caglayan M , Sogut A , Aslan S , Yuksel H . Relationship of sleep quality and quality of life in children with monosymptomatic enuresis. Child Care Health Dev. 2009;35(4):469–74.https://doi.org/10.1111/j.1365-2214.2009.00940.x
125 Egemen A , Akil I , Canda E , Ozyurt BC , Eser E . An evaluation of quality of life of mothers of children with enuresis nocturna. Pediatr Nephrol. 2008;23(1):93–8.https://doi.org/10.1007/s00467-007-0605-0
126 Van Herzeele C , Dhondt K , Roels SP , Raes A , Groen L-A , Hoebeke P , et al. Periodic limb movements during sleep are associated with a lower quality of life in children with monosymptomatic nocturnal enuresis. Eur J Pediatr. 2015;174(7):897–902.https://doi.org/10.1007/s00431-014-2474-4
127 Baeyens D , Roeyers H , Demeyere I , Verté S , Hoebeke P , Vande Walle J . Attention-deficit/hyperactivity disorder (ADHD) as a risk factor for persistent nocturnal enuresis in children: a two-year follow-up study. Acta Paediatr. 2005;94(11):1619–25.https://doi.org/10.1080/08035250510041240
128 Baeyens D , Roeyers H , Van Erdeghem S , Hoebeke P , Vande Walle J . The prevalence of attention deficit-hyperactivity disorder in children with nonmonosymptomatic nocturnal enuresis: a 4-year followup study. J Urol. 2007;178(6):2616–20.https://doi.org/10.1016/j.juro.2007.07.059
129 von Gontard A , Moritz AM , Thome-Granz S , Freitag C . Association of attention deficit and elimination disorders at school entry: a population based study. J Urol. 2011;186(5):2027–32.https://doi.org/10.1016/j.juro.2011.07.030
130 Hechtman L . Assessment and diagnosis of attention-deficit/hyperactivity disorder. Child Adolesc Psychiatr Clin N Am. 2000;9(3):481–98.
131 Park S , Kim BN , Kim JW , Hong S-B , Shin M-S , Yoo HJ , et al. Nocturnal enuresis is associated with attention deficit hyperactivity disorder and conduct problems. Psychiatry Investig. 2013;10(3):253–8.https://doi.org/10.4306/pi.2013.10.3.253
132 Lei D , Ma J , Shen X , Du X , Shen G , Liu W , et al. Changes in the brain microstructure of children with primary monosymptomatic nocturnal enuresis: a diffusion tensor imaging study. PLoS One. 2012;7(2):e31023.https://doi.org/10.1371/journal.pone.0031023
133 Vande Walle J , Rittig S , Bauer S , Eggert P , Marschall-Kehrel D , Tekgul S ; American Academy of Pediatrics; European Society for Paediatric Urology; European Society for Paediatric Nephrology; International Children’s Continence Society. Practical consensus guidelines for the management of enuresis. Eur J Pediatr. 2012;171(6):971–83.https://doi.org/10.1007/s00431-012-1687-7
134 Marcus CL , Brooks LJ , Ward SD , Draper KA , Gozal D , Halbower AC , et al.; American Academy of Pediatrics. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714–55.https://doi.org/10.1542/peds.2012-1672
135 Kaditis A , Kheirandish-Gozal L , Gozal D . Algorithm for the diagnosis and treatment of pediatric OSA: a proposal of two pediatric sleep centers. Sleep Med. 2012;13(3):217–27.https://doi.org/10.1016/j.sleep.2011.09.009
136 Liberati A , Altman DG , Tetzlaff J , Mulrow C , Gøtzsche PC , Ioannidis JPA , et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100.https://doi.org/10.1371/journal.pmed.1000100
137 Grundfast KM , Wittich DJ, Jr . Adenotonsillar hypertrophy and upper airway obstruction in evolutionary perspective. Laryngoscope. 1982;92(6 Pt 1):650–6.https://doi.org/10.1288/00005537-198206000-00011
138 Nowak KC , Weider DJ . Pediatric nocturnal enuresis secondary to airway obstruction from cleft palate repair. Clin Pediatr (Phila). 1998;37(11):653–7.https://doi.org/10.1177/000992289803701102
139 Guilleminault C , Eldridge FL , Tilkian A , Simmons FB , Dement WC . Sleep apnea syndrome due to upper airway obstruction: a review of 25 cases. Arch Intern Med. 1977;137(3):296–300.https://doi.org/10.1001/archinte.1977.03630150020008
140 Cinar U , Vural C , Cakir B , Topuz E , Karaman MI , Turgut S . Nocturnal enuresis and upper airway obstruction. Int J Pediatr Otorhinolaryngol. 2001;59(2):115–8.https://doi.org/10.1016/S0165-5876(01)00463-3
141 Brooks LJ , Topol HI . Enuresis in children with sleep apnea. J Pediatr. 2003;142(5):515–8.https://doi.org/10.1067/mpd.2003.158
142 Weider DJ , Sateia MJ , West RP . Nocturnal enuresis in children with upper airway obstruction. Otolaryngol Head Neck Surg. 1991;105(3):427–32.
143 Stone J , Malone PS , Atwill D , McGrigor V , Hill CM . Symptoms of sleep-disordered breathing in children with nocturnal enuresis. J Pediatr Urol. 2008;4(3):197–202.https://doi.org/10.1016/j.jpurol.2007.11.011
144 Umlauf MG , Chasens ER . Bedwetting--not always what it seems: a sign of sleep-disordered breathing in children. J Spec Pediatr Nurs. 2003;8(1):22–30.https://doi.org/10.1111/j.1744-6155.2003.tb00180.x
145 Goodwin JL , Kaemingk KL , Fregosi RF , Rosen GM , Morgan WJ , Smith T , et al. Parasomnias and sleep disordered breathing in Caucasian and Hispanic children - the Tucson children’s assessment of sleep apnea study. BMC Med. 2004;2(1):14.https://doi.org/10.1186/1741-7015-2-14
146 Barone JG , Hanson C , DaJusta DG , Gioia K , England SJ , Schneider D . Nocturnal enuresis and overweight are associated with obstructive sleep apnea. Pediatrics. 2009;124(1):e53–9.https://doi.org/10.1542/peds.2008-2805
147 Brooks LJ . Enuresis and sleep apnea. Pediatrics. 2005;116(3):799–800, author reply 800 . [author reply].https://doi.org/10.1542/peds.2005-1261
148 Bascom A , Penney T , Metcalfe M , Knox A , Witmans M , Uweira T , et al. High risk of sleep disordered breathing in the enuresis population. J Urol. 2011;186(4, Suppl):1710–4.https://doi.org/10.1016/j.juro.2011.04.017
149 El-Mitwalli A , Bediwy AS , Zaher AA , Belal T , Saleh AB . Sleep apnea in children with refractory monosymptomatic nocturnal enuresis. Nat Sci Sleep. 2014;6:37–42.
150 Su MS , Li AM , So HK , Au CT , Ho C , Wing YK . Nocturnal enuresis in children: prevalence, correlates, and relationship with obstructive sleep apnea. J Pediatr. 2011;159(2):238–42.e1.https://doi.org/10.1016/j.jpeds.2011.01.036
151 Carotenuto M , Esposito M , Pascotto A . Facial patterns and primary nocturnal enuresis in children. Sleep Breath. 2011;15(2):221–7.https://doi.org/10.1007/s11325-010-0388-6
152 Sakellaropoulou AV , Hatzistilianou MN , Emporiadou MN , Aivazis VT , Goudakos J , Markou K , et al. Association between primary nocturnal enuresis and habitual snoring in children with obstructive sleep apnoea-hypopnoea syndrome. Arch Med Sci. 2012;8(3):521–7.https://doi.org/10.5114/aoms.2012.28809
153 Xu Z , Cheuk DK , Lee SL . Clinical evaluation in predicting childhood obstructive sleep apnea. Chest. 2006;130(6):1765–71.https://doi.org/10.1016/S0012-3692(15)50899-4
154 Barone JG , Hanson C , DaJusta DG , Gioia K , England SJ , Schneider D . Nocturnal enuresis and overweight are associated with obstructive sleep apnea. Pediatrics. 2009;124(1):e53–9.https://doi.org/10.1542/peds.2008-2805
155 Alexopoulos EI , Malakasioti G , Varlami V , Miligkos M , Gourgoulianis K , Kaditis AG . Nocturnal enuresis is associated with moderate-to-severe obstructive sleep apnea in children with snoring. Pediatr Res. 2014;76(6):555–9.https://doi.org/10.1038/pr.2014.137
156 Huang YS , Guilleminault C , Lee LA , Lin CH , Hwang FM . Treatment outcomes of adenotonsillectomy for children with obstructive sleep apnea: a prospective longitudinal study. Sleep. 2014;37(1):71–6.
157 Nevéus T , Leissner L , Rudblad S , Bazargani F . Respiration during sleep in children with therapy-resistant enuresis. Acta Paediatr. 2014;103(3):300–4.https://doi.org/10.1111/apa.12515
158 Ersu R , Arman AR , Save D , Karadag B , Karakoc F , Berkem M , et al. Prevalence of snoring and symptoms of sleep-disordered breathing in primary school children in istanbul. Chest. 2004;126(1):19–24.https://doi.org/10.1378/chest.126.1.19
159 Gozal D , O’Brien LM . Snoring and obstructive sleep apnoea in children: why should we treat? Paediatr Respir Rev. 2004;5(Suppl A):S371–6.https://doi.org/10.1016/S1526-0542(04)90066-8
160 Alexopoulos EI , Kostadima E , Pagonari I , Zintzaras E , Gourgoulianis K , Kaditis AG . Association between primary nocturnal enuresis and habitual snoring in children. Urology. 2006;68(2):406–9.https://doi.org/10.1016/j.urology.2006.02.021
161 Wolfe-Christensen C , Kovacevic LG , Mirkovic J , Lakshmanan Y . Lower health related quality of life and psychosocial difficulties in children with monosymptomatic nocturnal enuresis--is snoring a marker of severity? J Urol. 2013;190(4, Suppl):1501–4.https://doi.org/10.1016/j.juro.2013.01.060
162 Basha S , Bialowas C , Ende K , Szeremeta W . Effectiveness of adenotonsillectomy in the resolution of nocturnal enuresis secondary to obstructive sleep apnea. Laryngoscope. 2005;115(6):1101–3.https://doi.org/10.1097/01.MLG.0000163762.13870.83
163 Wang RC , Elkins TP , Keech D , Wauquier A , Hubbard D . Accuracy of clinical evaluation in pediatric obstructive sleep apnea. Otolaryngol Head Neck Surg. 1998;118(1):69–73.https://doi.org/10.1016/S0194-5998(98)70377-8
164 Brouilette R , Hanson D , David R , Klemka L , Szatkowski A , Fernbach S , et al. A diagnostic approach to suspected obstructive sleep apnea in children. J Pediatr. 1984;105(1):10–4.https://doi.org/10.1016/S0022-3476(84)80348-0
165 Nascimento Fagundes S , Azevedo Soster L , Lebl AS , Rodrigues Pereira RP , Tanaka C , Pereira RF , et al. Impact of a multidisciplinary evaluation in pediatric patients with nocturnal monosymptomatic enuresis. Pediatr Nephrol. 2016;31(8):1295–303.https://doi.org/10.1007/s00467-016-3316-6
166 Leiberman A , Stiller-Timor L , Tarasiuk A , Tal A . The effect of adenotonsillectomy on children suffering from obstructive sleep apnea syndrome (OSAS): the Negev perspective. Int J Pediatr Otorhinolaryngol. 2006;70(10):1675–82.https://doi.org/10.1016/j.ijporl.2006.06.002
167 Weissbach A , Leiberman A , Tarasiuk A , Goldbart A , Tal A . Adenotonsilectomy improves enuresis in children with obstructive sleep apnea syndrome. Int J Pediatr Otorhinolaryngol. 2006;70(8):1351–6.https://doi.org/10.1016/j.ijporl.2006.01.011
168 Kovacevic L , Jurewicz M , Dabaja A , Thomas R , Diaz M , Madgy DN , et al. Enuretic children with obstructive sleep apnea syndrome: should they see otolaryngology first? J Pediatr Urol. 2013;9(2):145–50.https://doi.org/10.1016/j.jpurol.2011.12.013
169 Kalorin CM , Mouzakes J , Gavin JP , Davis TD , Feustel P , Kogan BA . Tonsillectomy does not improve bedwetting: results of a prospective controlled trial. J Urol. 2010;184(6):2527–32.https://doi.org/10.1016/j.juro.2010.08.040
170 Klackenberg G . Nocturnal enuresis in a longitudinal perspective. A primary problem of maturity and/or a secondary environmental reaction? Acta Paediatr Scand. 1981;70(4):453–7.https://doi.org/10.1111/j.1651-2227.1981.tb05722.x
171 Berry RB , Kouchi KG , Der DE , Dickel MJ , Light RW . Sleep apnea impairs the arousal response to airway occlusion. Chest. 1996;109(6):1490–6.https://doi.org/10.1378/chest.109.6.1490
172 Phillipson EA , Bowes G , Sullivan CE , Woolf GM . The influence of sleep fragmentation on arousal and ventilatory responses to respiratory stimuli. Sleep. 1980;3(3-4):281–8.
173 Downey R , Bonnet MH . Performance during frequent sleep disruption. Sleep. 1987;10(4):354–63.
174 Nørgaard JP , Rittig S , Djurhuus JC . Nocturnal enuresis: an approach to treatment based on pathogenesis. J Pediatr. 1989;114(4 Pt 2):705–10.https://doi.org/10.1016/S0022-3476(89)80885-6
175 Arai H , Furuta H , Kosaka K , Kaneda R , Koshino Y , Sano J , et al. Polysomnographic and urodynamic changes in a case of obstructive sleep apnea syndrome with enuresis. Psychiatry Clin Neurosci. 1999;53(2):319–20.https://doi.org/10.1046/j.1440-1819.1999.00550.x
176 Kaditis AG , Alexopoulos EI , Evangelopoulos K , Kostadima E , Varlami V , Boultadakis E , et al. Correlation of urinary excretion of sodium with severity of sleep-disordered breathing in children: a preliminary study. Pediatr Pulmonol. 2010;45(10):999–1004.https://doi.org/10.1002/ppul.21285
177 O’Driscoll DM , Foster AM , Davey MJ , Nixon GM , Horne RS . Can actigraphy measure sleep fragmentation in children? Arch Dis Child. 2010;95(12):1031–3.https://doi.org/10.1136/adc.2009.166561
178 Staessen JA , Birkenhäger W , Bulpitt CJ , Fagard R , Fletcher AE , Lijnen P , et al. The relationship between blood pressure and sodium and potassium excretion during the day and at night. J Hypertens. 1993;11(4):443–7.https://doi.org/10.1097/00004872-199304000-00016
179 Krieger J , Follenius M , Sforza E , Brandenberger G , Peter JD . Effects of treatment with nasal continuous positive airway pressure on atrial natriuretic peptide and arginine vasopressin release during sleep in patients with obstructive sleep apnoea. Clin Sci (Lond). 1991;80(5):443–9.https://doi.org/10.1042/cs0800443
180 Ichioka M , Hirata Y , Inase N , Tojo N , Yoshizawa M , Chida M , et al. Changes of circulating atrial natriuretic peptide and antidiuretic hormone in obstructive sleep apnea syndrome. Respiration. 1992;59(3):164–8.https://doi.org/10.1159/000196049
181 Lin CC , Tsan KW , Lin CY . Plasma levels of atrial natriuretic factor in moderate to severe obstructive sleep apnea syndrome. Sleep. 1993;16(1):37–9.
182 Rodenstein DO , D’Odemont JP , Pieters T , Aubert-Tulkens G . Diurnal and nocturnal diuresis and natriuresis in obstructive sleep apnea. Effects of nasal continuous positive airway pressure therapy. Am Rev Respir Dis. 1992;145(6):1367–71.https://doi.org/10.1164/ajrccm/145.6.1367
183 Yue Z , Wang M , Xu W , Li H , Wang H . Secretion of antidiuretic hormone in children with obstructive sleep apnea-hypopnea syndrome. Acta Otolaryngol. 2009;129(8):867–71.https://doi.org/10.1080/00016480802441762
184 Ljunggren M , Lindahl B , Theorell-Haglöw J , Lindberg E . Association between obstructive sleep apnea and elevated levels of type B natriuretic peptide in a community-based sample of women. Sleep. 2012;35(11):1521–7.
185 Garpestad E , Parker JA , Katayama H , Lilly J , Yasuda T , Ringler J , et al. Decrease in ventricular stroke volume at apnea termination is independent of oxygen desaturation. J Appl Physiol (1985). 1994;77(4):1602–8.
186 Bonsignore MR , Marrone O , Romano S , Pieri D . Time course of right ventricular stroke volume and output in obstructive sleep apneas. Am J Respir Crit Care Med. 1994;149(1):155–9.https://doi.org/10.1164/ajrccm.149.1.8111575
187 Yoshimura M , Yasue H , Morita E , Sakaino N , Jougasaki M , Kurose M , et al. Hemodynamic, renal, and hormonal responses to brain natriuretic peptide infusion in patients with congestive heart failure. Circulation. 1991;84(4):1581–8.https://doi.org/10.1161/01.CIR.84.4.1581
188 Kaditis AG , Alexopoulos EI , Hatzi F , Kostadima E , Kiaffas M , Zakynthinos E , et al. Overnight change in brain natriuretic peptide levels in children with sleep-disordered breathing. Chest. 2006;130(5):1377–84.https://doi.org/10.1378/chest.130.5.1377
189 Baruzzi A , Riva R , Cirignotta F , Zucconi M , Cappelli M , Lugaresi E . Atrial natriuretic peptide and catecholamines in obstructive sleep apnea syndrome. Sleep. 1991;14(1):83–6.
190 Follenius M , Krieger J , Krauth MO , Sforza F , Brandenberger G . Obstructive sleep apnea treatment: peripheral and central effects on plasma renin activity and aldosterone. Sleep. 1991;14(3):211–7.
191 Kaditis AG , Chaidas K , Alexopoulos EI , Varlami V , Malakasioti G , Gourgoulianis K . Effects of adenotonsillectomy on R-R interval and brain natriuretic peptide levels in children with sleep apnea: a preliminary report. Sleep Med. 2011;12(7):646–51.https://doi.org/10.1016/j.sleep.2011.01.014
192 Kovacevic L , Wolfe-Christensen C , Lu H , Toton M , Mirkovic J , Thottam PJ , et al. Why does adenotonsillectomy not correct enuresis in all children with sleep disordered breathing? J Urol. 2014;191(5, Suppl):1592–6.https://doi.org/10.1016/j.juro.2013.10.032
193 Alexopoulos EI , Kaditis AG , Kostadima E , Gourgoulianis K . Resolution of nocturnal enuresis in snoring children after treatment with nasal budesonide. Urology. 2005;66(1):194.https://doi.org/10.1016/j.urology.2005.01.021
194 Ahmadi MS , Amirhassani S , Poorolajal J . The effect of adenotonsillectomy on pediatric nocturnal enuresis: a prospective cohort study. Iran J Otorhinolaryngol. 2013;25(70):37–40.
195 Jeyakumar A , Rahman SI , Armbrecht ES , Mitchell R . The association between sleep-disordered breathing and enuresis in children. Laryngoscope. 2012;122(8):1873–7.https://doi.org/10.1002/lary.23323
196 Park S , Lee JM , Sim CS , Kim JG , Nam JG , Lee T-H , et al. Impact of adenotonsillectomy on nocturnal enuresis in children with sleep-disordered breathing: A prospective study. Laryngoscope. 2016;126(5):1241–5.https://doi.org/10.1002/lary.25934
197 Timms DJ . Rapid maxillary expansion in the treatment of nocturnal enuresis. Angle Orthod. 1990;60(3):229–33, discussion 234.
198 Kurol J , Modin H , Bjerkhoel A . Orthodontic maxillary expansion and its effect on nocturnal enuresis. Angle Orthod. 1998;68(3):225–32.
199 Bazargani F , Feldmann I , Bondemark L . Three-dimensional analysis of effects of rapid maxillary expansion on facial sutures and bones. Angle Orthod. 2013;83(6):1074–82.https://doi.org/10.2319/020413-103.1
200 Halicioğlu K , Kiliç N , Yavuz İ , Aktan B . Effects of rapid maxillary expansion with a memory palatal split screw on the morphology of the maxillary dental arch and nasal airway resistance. Eur J Orthod. 2010;32(6):716–20.https://doi.org/10.1093/ejo/cjp164
Study conception and design: Marco Zaffanello; Collection of data: Marco Zaffanello, Emma Gasperi, Giorgio Piacentini, Giuseppe Lippi, Vassilios Fanos; Analysis and interpretation of data: Marco Zaffanello, Giorgio Piacentini, Giuseppe Lippi, Vassilios Fanos; Drafting of manuscript: Marco Zaffanello, Giorgio Piacentini, Giuseppe Lippi, Vassilios Fanos; Critical revision: Luana Nosetti, Giuseppe Lippi, Giorgio Piacentini
No financial support and no other potential conflict of interest relevant to this article was reported.