Pulmonary hypertension associated with left-sided heart disease
DOI: https://doi.org/10.4414/smw.2017.14395
Micha T.
Maederac, Otto D.
Schochbc, Rebekka
Kleinerbc, Lucas
Joergac, Daniel
Weilenmannac, , on behalf of the Swiss Society for Pulmonary Hypertension
a Department of Cardiology, Kantonsspital St Gallen, Switzerland
b Department of Respiratory Medicine, Kantonsspital St Gallen, Switzerland
c Pulmonary Hypertension Unit, Kantonsspital St Gallen, Switzerland
Summary
Pulmonary hypertension associated with left-sided heart disease (PH-LHD) is the most common type of pulmonary hypertension. In patients with left-sided heart disease, the presence of pulmonary hypertension is typically a marker of more advanced disease, more severe symptoms, and worse prognosis. In contrast to pulmonary arterial hypertension, PH-LHD is characterised by an elevated pulmonary artery wedge pressure (postcapillary pulmonary hypertension) without or with an additional precapillary component (isolated postcapillary vs combined postcapillary and precapillary pulmonary hypertension). Transthoracic echocardiography is the primary noninvasive imaging tool to estimate the probability of pulmonary hypertension and to establish a working diagnosis on the mechanism of pulmonary hypertension. However, right heart catheterisation is always required if significant pulmonary hypertension is suspected and exact knowledge of the haemodynamic constellation is necessary. The haemodynamic constellation (mean pulmonary artery pressure, mean pulmonary artery wedge pressure, left ventricular end-diastolic pressure) in combination with clinical information and imaging findings (mainly echocardiography, coronary angiography and cardiac magnetic resonance imaging) will usually allow the exact mechanism underlying PH-LHD to be defined, which is a prerequisite for appropriate treatment. The general principle for the management of PH-LHD is to treat the underlying left-sided heart disease in an optimal manner using drugs and/or interventional or surgical therapy. There is currently no established indication for pulmonary arterial hypertension-specific therapies in PH-LHD, and specific therapies may even cause harm in patients with PH-LHD.
Abbreviations
- DPG
-
diastolic pressure gradient
- HFpEF
-
heart failure with preserved ejection fraction
- HFrEF
-
heart failure with reduced ejection fraction
- HFmrEF
-
heart failure with mid-range ejection fraction
- LVEDP
-
left ventricular end-diastolic pressure
- LVEF
-
left ventricular ejection fraction
- PAP
-
pulmonary artery pressure
- PAWP
-
pulmonary artery wedge pressure
- PDE-5
-
phosphodiesterase-5
- PH-LHD
-
pulmonary hypertension associated with left-sided heart disease
- PVR
-
pulmonary vascular resistance
- TPG
-
transpulmonary gradient
- TRV
-
tricuspid regurgitation velocity
Introduction
Pulmonary hypertension associated with left-sided heart disease (PH-LHD; group 2 pulmonary hypertension, table 1) is the most common type of pulmonary hypertension, probably accounting for approximately 75% of cases [1–4]. Many forms of left-sided heart disease can be associated with pulmonary hypertension, and the presence of PH-LHD is typically a marker of more advanced heart disease, more severe symptoms and worse prognosis [4]. Importantly, the haemodynamic situation in PH-LHD differs fundamentally from that of other forms of pulmonary hypertension, i.e., groups 1, 3, 4, and at least in part group 5 (table 1). Whereas the latter forms of pulmonary hypertension are characterised by a precapillary problem (with the exception of group 1ʹ, as discussed later), i.e., pulmonary arterial hypertension, group 2 pulmonary hypertension is characterised primarily by a postcapillary obstruction of the vascular bed, i.e., pulmonary venous hypertension [1]. The accurate diagnosis of PH-LHD and the identification of the exact underlying mechanism can be challenging, but is crucial as the basis on which to define the appropriate management. Misdiagnosis of pulmonary arterial hypertension in patients with PH-LHD is not uncommon and may lead to inappropriate use of pulmonary arterial hypertension-specific therapies, which can precipitate pulmonary congestion in these patients [5, 6]. In this review we present a summary of the current understanding of pathophysiology, diagnostic approach and treatment of patients with PH-LHD.
Table 1 Classification of pulmonary hypertension (PH) according to current guidelines [1]. Please see table 2, table 4 and text for details.
|
Group
|
Haemodynamic constellation
|
| 1. Pulmonary arterial hypertension |
Precapillary PH |
| 1’ Pulmonary veno-occlusive disease and/or pulmonary capillary haemangiosis |
Postcapillary PH and “capillary” PH, respectively |
| 1’’ Persistent PH of the newborn |
Precapillary PH |
| 2. PH due to left-sided heart disease |
Postcapillary PH |
| 3. PH due to lung disease and/or hypoxia |
Precapillary PH |
4. Chronic thromboembolic PH and other pulmonary
artery obstructions |
Precapillary PH |
5. PH associated with unclear and/or multifactorial
mechanisms |
Precapillary and postcapillary forms of PH |
Epidemiology
The prevalence of pulmonary hypertension in patients with left-sided heart disease depends on the method of pulmonary artery pressure (PAP) measurement (estimation with echocardiography vs right heart catheterisation), the definition of pulmonary hypertension applied (invasively assessed mean PAP >25 mm Hg vs cut-offs for echocardiographically estimated systolic PAP, e.g., ≥35 mm Hg), and the disease severity of the population studied. In a recently published study from large cohort of patients with heart failure and a reduced ejection fraction (HFrEF) undergoing cardiac catheterisation (n = 664), Gerges et al. reported a prevalence of PH-LHD (mean PAP >25 mm Hg) of 68% [7]. By design (indication for cardiac catheterisation), this was a selected population. However, invasive haemodynamic data from unselected HFrEF patients are unlikely to be available. In a community-based cohort of patients with heart failure with preserved ejection fraction (HFpEF) (n = 244), the prevalence of pulmonary hypertension, defined as an echocardiographically estimated systolic PAP >35 mm Hg, was 83% [8]. The above-mentioned study by Gerges et al. [7] also included 399 HFpEF patients with a prevalence of PH-LHD of 54%. The adverse prognostic impact of the presence of pulmonary hypertension has been documented in HFrEF [9, 10] and HFpEF [8]. In a cohort of patients with severe primary mitral regurgitation and left ventricular ejection fraction (LVEF) ≥60%, 47% had an estimated systolic PAP ≥35 mm Hg and 15% had a systolic PAP >50 mm Hg; the degree of pulmonary hypertension was an independent predictor of prognosis [11].
Pathophysiology of pulmonary hypertension associated with left-sided heart disease
The pathophysiology of PH-LHD is complex, and a number of aspects remain incompletely understood. The primary mechanism underlying PH-LHD is the backward transmission of elevated left-sided filling pressures, which develop because of systolic and/or diastolic left ventricular dysfunction, mitral regurgitation/stenosis, decreased left atrial compliance, and increased afterload due to vascular stiffness or aortic stenosis. Aspects of specific disease entities are discussed later (see section on differential diagnosis of PH-LHD). In the majority of patients with PH-LHD, pulmonary hypertension is purely passive and due to increased left atrial pressure and pulmonary venous congestion, a situation that is haemodynamically characterised by a high pulmonary artery wedge pressure (PAWP) but a low transpulmonary gradient (TPG; the difference between mean PAP and mean PAWP) and pulmonary vascular resistance (PVR; TPG/cardiac output). In some patients, however, there is an additional precapillary component due to pulmonary vasoconstriction and vascular remodelling, which may develop depending on the individual susceptibility of the pulmonary vasculature and the chronicity of left atrial pressure / PAWP elevation. These patients have not only a high left atrial pressure and PAWP, but also an elevation of PVR. The underlying mechanisms include, but are probably not restricted to, decreased nitric oxide availability, increased endothelin expression, and desensitisation to natriuretic peptide-mediated vasodilatation. Histopathological changes include thickening of the alveolar-capillary membrane, medial hypertrophy, intimal and adventitial fibrosis, and luminal occlusion of small pulmonary arterioles, whereas plexiform lesions are usually not found [3]. Studies have shown that in advanced HFrEF successful unloading of the left ventricle by implantation of an assist device not only lowers left-sided filling pressures but also PVR [12, 13], suggesting that elevated left-sided filling pressures are indeed the driver for the occurrence of a precapillary component of pulmonary hypertension, and that this phenomenon may be at least in part reversible by efficient left ventricular unloading. In PH-LHD, the features of left ventricular failure are usually more prominent than the degree of right ventricular dysfunction (“left ventricular phenotype”). However, not only pulmonary arterial hypertension but also combined postcapillary and precapillary pulmonary hypertension in the context of PH-LHD can lead to right ventricular dysfunction and failure. Therefore, PH-LHD can also present with a “right ventricular phenotype”, an echocardiographic aspect resembling pulmonary arterial hypertension [3]. This picture is thought to represent an advanced stage of an unfavourable evolution occurring in PH-LHD patients susceptible to right ventricular dysfunction and failure [3]. A number of recent studies in HFpEF patients have clearly highlighted that subtle right ventricular dysfunction and abnormal coupling of the right ventricle and the pulmonary vasculature is a common feature of patients who are thought to primarily have a left ventricle disease [14, 15]. Importantly, the degree of right ventricular dysfunction and PAP elevation are not always proportional, and right ventricular dysfunction is an important prognostic sign in HFrEF [10], HFpEF [14] and also valve disease [16].
Definitions of pulmonary hypertension associated with left-sided heart disease
As shown in table 2, PH-LHD is defined as a combination of a mean PAP ≥25 mm Hg and a mean PAWP >15 mm Hg [1]. In patients with isolated postcapillary pulmonary hypertension, the TPG (cut-off ≤12 mm Hg as used in the previous guidelines [17]), the diastolic pressure gradient (DPG, the difference between diastolic PAP and mean PAWP, cut-off <7 mm Hg), and the PVR (cut-off 3 Wood units, 240 dyn·sec·cm-5) are low. In the current guidelines [1], isolated postcapillary pulmonary hypertension is defined as a mean PAP ≥25 mm Hg, a mean PAWP >15 mm Hg, and a DPG <7 m Hg, whereas combined postcapillary and precapillary pulmonary hypertension is defined as mean PAP ≥25 mm Hg, a mean PAWP >15 mm Hg and a DPG ≥7 mm Hg (table 2). The rationale for the use of the DPG rather than the TPG is based on the assumption that the DPG is less dependent on stroke volume and loading conditions, and may be a better marker of outcomes [4, 18]. This definition has now been accepted, although results of studies on the prognostic role of DPG have been conflicting [18–20]. According to the current guidelines, a PVR of >3 WU (240 dyn·sec·cm-5), and/or a DPG ≥7 mm Hg, can also be used to differentiate between isolated postcapillary pulmonary hypertension and combined postcapillary and precapillary pulmonary hypertension [1]. The use of PVR rather than TPG has the advantage of including an element of cardiac output, which makes sense from a pathophysiological point of view as the importance of a certain TPG value depends on cardiac output: the higher the cardiac output the lower the PVR for a given TPG. On the other hand, measurement of cardiac output is subject to error and may therefore further complicate the situation [21]. In addition, the introduction of PVR in the definition of isolated postcapillary versus combined postcapillary and precapillary pulmonary hypertension has led to the situation in which a substantial proportion of patients are unclassifiable (DPG <7 mm Hg but PVR >3 WU) [22]. Thus, further refinement of these definitions can be expected.
Table 2 Haemodynamic definitions of pulmonary hypertension associated with left-sided heart disease according to [1].
|
PH-LHD (postcapillary PH): general definition
|
| Mean PAP |
≥25 mm Hg |
| Mean PAWP |
>15 mm Hg |
|
Subtypes of PH-LHD according to the presence or absence of a pre-capillary component
|
|
Isolated postcapillary PH
|
DPG
And/or PVR |
<7 mm Hg
≤3 WU |
|
Combined postcapillary and precapillary PH
|
DPG
And/or PVR |
≥7 mm Hg
>3 WU |
Comprehensive noninvasive and invasive assessment
Diagnosis of pulmonary hypertension
The first step in the assessment of the patient with possible PH-LHD is a thorough clinical assessment. The next step is a carefully performed transthoracic echocardiogram to assess the probability of the pulmonary hypertension and PH-LHD, and to define the underlying mechanisms of left-sided heart disease and the therapeutic targets. The first question for the echocardiogram is whether pulmonary hypertension is present, i.e., to make sure that mean PAP is ≥25 mm Hg. Studies have shown good correlations between invasively measured systolic PAP and echocardiographically assessed systolic PAP as estimated from the peak tricuspid regurgitation velocity (TRV; systolic PAP is 4 × peak TRV2 [according to the simplified Bernoulli equation] + central venous pressure) [23]. On the other hand, several studies have shown that estimation of systolic PAP based on peak TRV can result in significant inaccuracy in the individual patient, particularly overestimation of the true systolic PAP [24, 25]. In presence of severe tricuspid regurgitation, underestimation of systolic PAP by use of the measured peak TRV is also possible. Central venous pressure is often ignored, but this can lead to a substantial error in the case of a high central venous pressure and a relatively low peak TRV. In addition, estimation of mean PAP from peak TRV is theoretically feasible since a linear relationship between systolic PAP and mean PAP has been demonstrated (mean PAP = 0.61 × systolic PAP + 2 mm Hg [26]), but it should be realized that this is also based on TRV measurement. Therefore, echocardiography should not be used to predict systolic PAP as an exact number and, importantly, indirect signs of pulmonary hypertension must be included in the assessment of the probability of pulmonary hypertension. Thus, according to current guidelines [1] the probability of pulmonary hypertension (all forms including PH-LHD) is estimated based on peak TRV (after exclusion of pulmonary valve stenosis) and indirect signs of pulmonary hypertension including enlargement of the right cardiac chambers, deformation of the interventricular septum (“D-shape” of the left ventricle), and shortening of the pulmonary acceleration time as follows:
- Peak TRV ≤2.8 m/s, no indirect signs: low probability of pulmonary hypertension;
- Peak TRV ≤2.8 m/s but indirect signs OR peak TRV 2.9-3.4 m/s without indirect signs: intermediate probability of pulmonary hypertension;
- Peak TRV 2.9–3.4 m/s with indirect signs OR peak TRV >3.4 m/s with/without indirect signs: high probability of pulmonary hypertension.
Importantly, measures of right ventricular function including right ventricular fractional area change, tricuspid annular plane systolic excursion (as assessed with M-mode echocardiography), and right ventricular peak systolic annular velocity (as assessed with pulsed-wave tissue Doppler) provide prognostic information in conjunction with the degree of PAP elevation [10, 27].
Whether or not right heart catheterisation is performed to confirm the presence of pulmonary hypertension in a patient with left-sided heart disease depends on the clinical context. In patients with an established pathophysiology, e.g. patients with HFrEF, echocardiography is usually sufficient for detecting changes in key haemodynamic parameters including central venous pressure, left ventricular end-diastolic pressure (LVEDP) and systolic PAP in a qualitative manner. An exact assessment of haemodynamic parameters by echocardiography is not possible, however [28]. Routine right heart catheterisation to guide therapy of acutely decompensated patients is not necessary. Right heart catheterisation may be considered in patients with HFrEF if there is evidence of significant pulmonary hypertension in the euvolaemic state, if the haemodynamic constellation is not clear, and in severely compromised patients, particularly in those for whom cardiac transplantation will be considered. A significant precapillary pulmonary hypertension component is a contraindication to cardiac transplantation as this carries a high risk of early postoperative right heart failure of the allograft. In patients with suspected significant PH-LHD, but uncertainty about the underlying mechanism (see next paragraph), right heart catheterisation will be required.
Pulmonary hypertension associated with left-sided heart disease versus pulmonary arterial hypertension
Echocardiography is also an important tool for the differentiation of pulmonary arterial hypertension and PH-LHD. In general, features of pulmonary hypertension are less prominent in PH-LHD than in pulmonary arterial hypertension, which is because in PH-LHD both left-sided and right-sided filling pressures are elevated. An elevated systolic PAP in the context of a dilated left ventricle with impaired LVEF, evidence of a specific cardiomyopathy (e.g., hypertrophic cardiomyopathy or amyloid heart disease), or significant valve disease (e.g., severe mitral regurgitation or severe aortic stenosis) suggest PH-LHD. If this is not the case, PH-LHD can still be present (i.e., HFpEF) but the differentiation from pulmonary arterial hypertension is challenging. Patients with PH-LHD due to HFpEF are typically older and have more classical cardiovascular risk factors than those with pulmonary arterial hypertension [29]. Table 3 summarises clinical and echocardiographic features of pulmonary arterial hypertension versus PH-LHD [29, 30]. Figure 1 depicts key echocardiographic features used in the assessment of the patient with suspected pulmonary hypertension and for the differentiation between pulmonary arterial hypertension und PH-LHD. Although algorithms for the echocardiographic differentiation between pulmonary arterial hypertension and PH-LHD are available [30–32], and noninvasive estimation of PVR is feasible [33], an accurate noninvasive prediction of haemodynamics by means of echocardiography is not possible in this setting [34]. Accordingly, right heart catheterisation is required if the probability of pulmonary hypertension is high, first to confirm pulmonary hypertension and second to assess the underlying haemodynamic constellation.
Table 3 Clinical features and noninvasive findings favouring pulmonary arterial hypertension or postcapillary pulmonary hypertension.
|
Pulmonary arterial hypertension
|
Postcapillary pulmonary hypertension
|
|
Clinical features
|
|
|
| Age >65 years |
No |
Yes |
| Systemic blood pressure |
↓/Normal |
Normal/↑ |
| Atrial fibrillation |
No |
Yes |
| Obesity/diabetes |
No |
Yes |
| Coronary artery disease |
No |
Yes |
|
BNP/NT-proBNP
|
↑ |
↑ |
|
Chest X-ray
|
No pulmonary congestion |
Pulmonary congestion |
|
ECG
|
RV hypertrophy/strain |
LV hypertrophy/strain |
|
Echocardiography
|
|
|
| Peak TRV |
↑↑ |
↑ |
| LV size |
↓ |
↑ |
| LV wall thickness |
↓ |
↑ |
| LV eccentricity index (degree of LV “D-shape”) |
↑↑ |
↑ |
| Apex-forming right ventricle |
Yes |
No |
| Left atrial size |
↓ |
↑ |
| Mitral regurgitation |
No/little |
Little to severe |
| E/eʹ |
↓ |
↑ |
| Pulmonary flow acceleration time |
↓ |
Normal/↑ |
| Peak TRV / VTI RVOT*
|
↑ |
Normal/↓ |

Figure 1 Important echocardiographic features for the assessment of the patient with suspected pulmonary hypertension. Direct (elevated peak tricuspid regurgitation velocity) and indirect (right ventricular dilatation, hypertrophy, and dysfunction as well as right atrial dilatation) are seen in all forms of pulmonary hypertension. In general, evidence of significant pulmonary hypertension without evidence of left-sided heart disease suggests pulmonary arterial hypertension, particularly if the right ventricle and right atrium are bigger than the left ventricle and the left atrium, and there is evidence of higher right atrial than left atrial pressure (atrial septum bulged to the left). In contrast, signs of pulmonary hypertension combined with evidence of significant left-sided heart disease suggest PH-LHD, particularly if there is evidence of higher left atrial than right atrial pressure (left atrium bigger than right atrium, and atrial septum bulged to the right).
CW = continuous wave; LA = left atrium; LV = left ventricle; PW = pulsed wave; RA = right atrium; RV = right ventricle; TAPSE = tricuspid annular plane systolic excursion
Measurement of PAWP can be associated with inaccuracies, and sometimes a “proper” PAWP cannot be obtained. Therefore, the threshold to performing simultaneous right and left heart catheterisation should be low in subjects with a high likelihood of left-sided heart disease [35]. Whereas routine left heart catheterisation is not recommended in all patients with suspected pulmonary hypertension, the availability of both PAWP and LVEDP will allow the differentiation of pulmonary arterial hypertension and PH-LHD if there is doubt about the reliability of a PAWP and the exact haemodynamic characterisation of special forms of PH-LHD [35]. Assessment of patients with PH-LHD in the context of HFpEF can be particularly challenging. Although the echocardiogram may have suggested significant pulmonary hypertension, mean PAP and PAWP criteria for PH-LHD may not be fulfilled during the invasive assessment at rest. Reasons for these seemingly discrepant findings may include successful treatment with diuretics and/or afterload reduction after the echocardiogram has been obtained, or the impact of fasting before cardiac catheterisation. Patients with HFpEF are characterised by concentric left ventricular remodelling with a small left ventricular cavity and a steep end-diastolic pressure–volume relationship. In these patients with noncompliant left ventricles, relatively small changes in left ventricular volume lead to significant changes in filling pressures [36]. Thus, in a fasting or diuretic-treated patient, a fluid challenge (500 ml saline over 5 minutes) may be needed to unmask these properties of the left ventricle and to diagnose PH-LHD in the context of HFpEF [35, 37]. In addition, exercise right heart catheterisation can be very instructive on the haemodynamic profile of patients with HFpEF [36, 38, 39]. However, both administration of a fluid bolus and exercise right heart catheterisation have not been standardised, are thus not yet recommended for routine use, and should be performed only in expert centres [35].
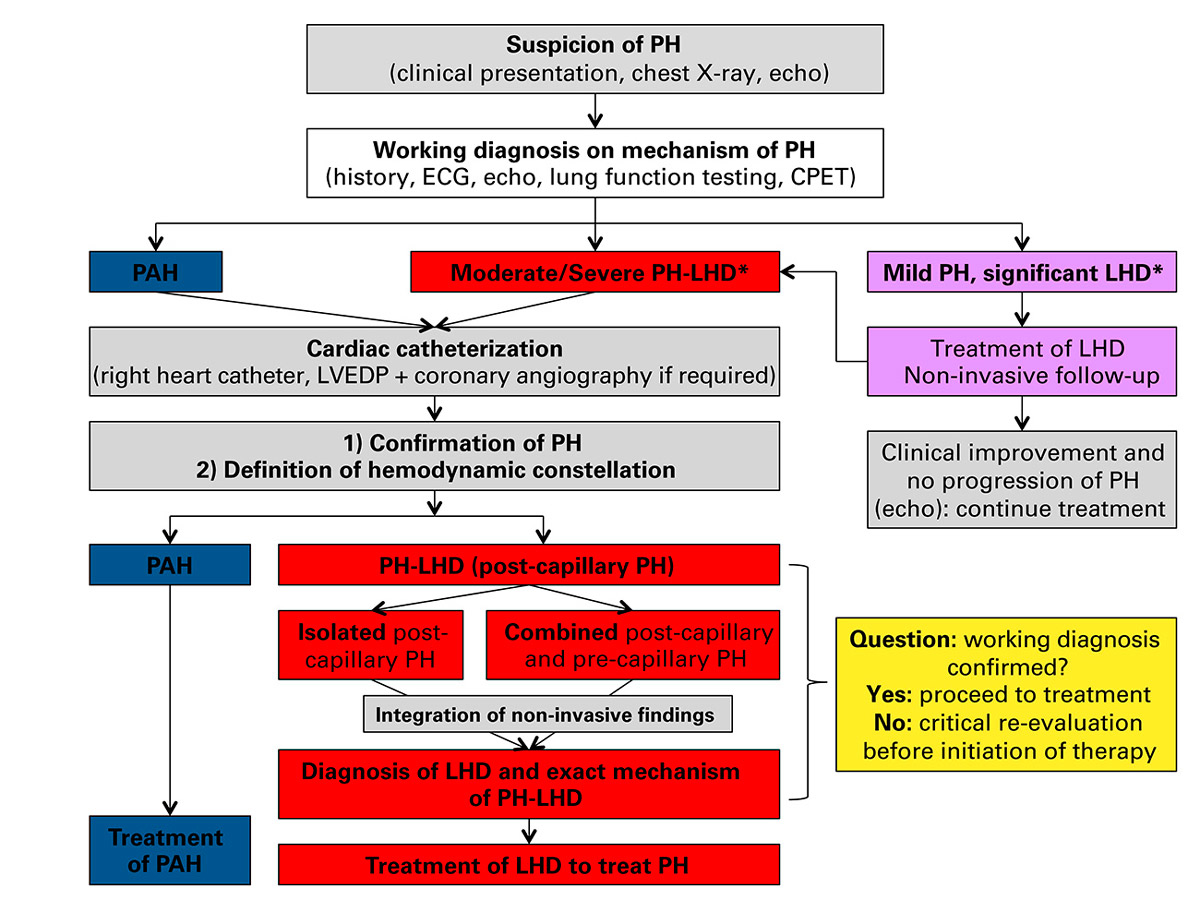
It is of utmost importance that invasive haemodynamic measurements are looked at in the light of the precatheterisation working diagnosis, which should always be established after a thorough clinical and echocardiographic assessment. This diagnostic process in a patient with suspected pulmonary hypertension is summarised in figure 2. If noninvasive and invasive haemodynamic measures are congruent, one can proceed to planning the patient’s management. However, if this was not the case, then a certain PAWP reading should not lead to the noncritical rejection of the precatheterisation working diagnosis. Rather, it should be asked whether PAWP was not correctly measured (zero level, PAWP measured at end-expiration without performing a Valsalva manoeuvre, significant difference between PAWP and LVEDP) or whether measures had been performed which had changed the haemodynamic situation between the time of echocardiography to the time of cardiac catheterisation (e.g., forced diuresis). It should be kept in mind that patients with pulmonary arterial hypertension typically have low rather than borderline PAWP levels (mean PAWP ≈ 9 mm Hg in the Study with an Endothelial Receptor Antagonist in Pulmonary arterial Hypertension to Improve cliNical outcome [SERAPHIN] [40], a classical pulmonary arterial hypertension population), and that mean PAWP readings between 12 and 15 mm Hg should already raise the suspicion for PH-LHD. Figure 2 also highlights that not every patient with echocardiographic evidence of pulmonary hypertension and clear evidence of left-sided heart disease needs right heart catheterisation.
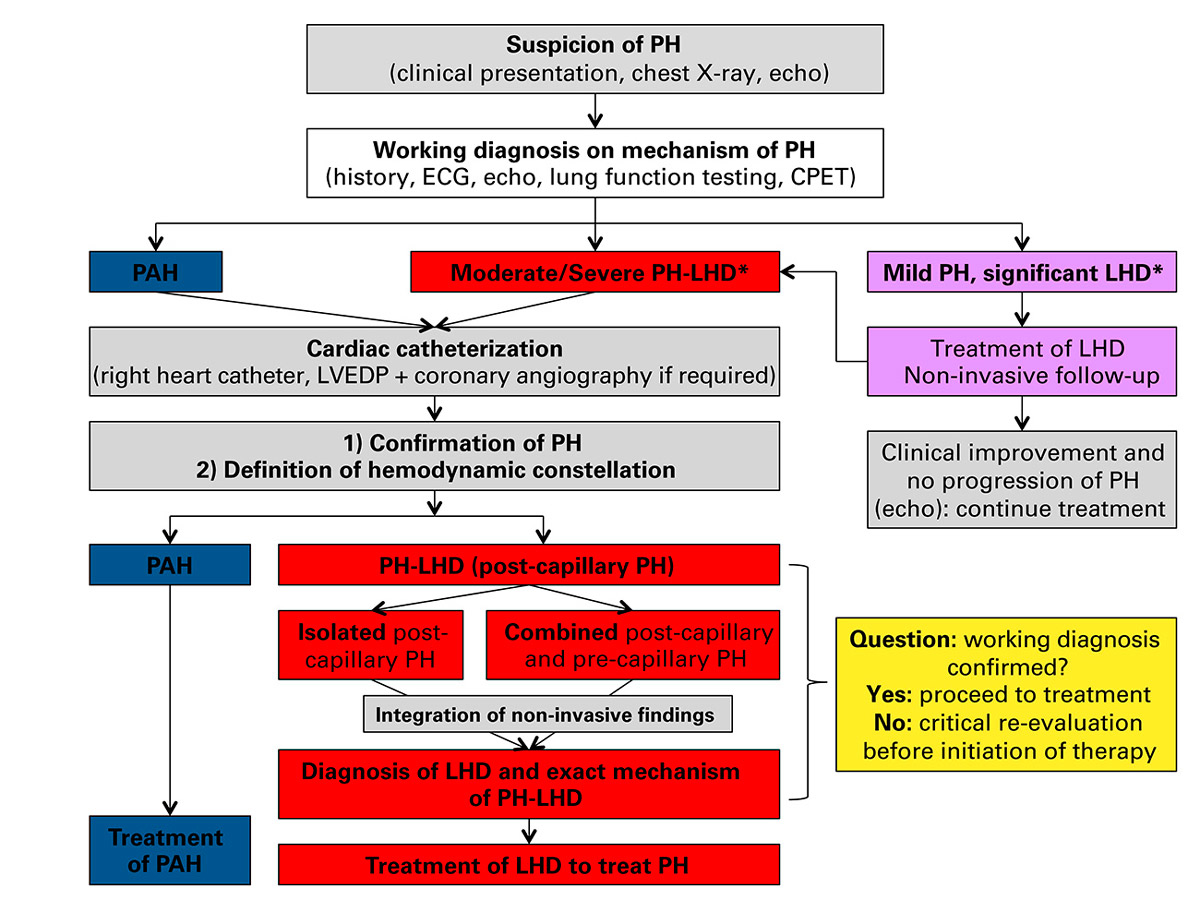
Figure 2 Approach to the patient with suspected pulmonary hypertension (modified and simplified according to [3]).
*There is no accepted definition of the severity of pulmonary hypertension. As an arbitrary definition it is suggested that “moderate/severe pulmonary hypertension” is a peak tricuspid regurgitation velocity (TRV) 2.9–3.4 m/s + indirect signs of pulmonary hypertension OR peak TRV >3.4 m/s with/without indirect signs of pulmonary hypertension. Accordingly, “mild pulmonary hypertension” is peak TRV ≤2.8 m/s but indirect signs OR peak TRV 2.9–3.4 m/s without indirect signs.
For further details, please see text.
CPET = cardiopulmonary exercise test; LHD = left-sided heart disease; LVEDP = left ventricular end-diastolic pressure; PAH = pulmonary arterial hypertension; PH = pulmonary hypertension
Differential diagnosis of pulmonary hypertension associated with left-sided heart disease
After the haemodynamic constellation of PH-LHD has been established, the underlying mechanism has to be determined based on noninvasive and invasive haemodynamic assessments and additional imaging findings: the point of the haemodynamic obstruction or problem in the circulation between pulmonary artery and aorta has to be identified (fig. 3). As shown in figure 3 and table 4, assessment of mean PAP, mean PAWP and LVEDP, and combination of these data with imaging findings (left atrial size, mitral valve disease, left ventricular diastolic and systolic function, aortic valve disease) will usually allow the mechanism underlying PH-LHD to be defined, which is absolutely crucial as a basis for management. Whereas the current guidelines describe three principle subgroups of PH-LHD (class 2.1 left ventricular systolic dysfunction; class 2.2 left ventricular diastolic dysfunction; class 2.3 valve disease), we herein discuss the different entities leading to PH-LHD in an “anatomico-haemodynamic” fashion. In figure 3 and table 4, seven levels of obstruction are shown (A–G), two of which belong to the pulmonary arterial hypertension spectrum, and five of which belong to the PH-LHD spectrum. An obstruction at each of these levels has a characteristic haemodynamic constellation, which in combination with history and imaging findings at least in theory allows an unequivocal diagnosis.

Figure 3 Schematic representation of the differential diagnosis of pulmonary hypertension according to the level of obstruction in the circulation. For explanation, please see table 4 and text.
AV = aortic valve; LA = left atrium; LV = left ventricle; MA = mitral valve; RA = right atrium; RV = right ventricle
Table 4 Haemodynamic differential diagnosis of pulmonary hypertension (complementary information to figure 3).
|
A
|
B
|
C
|
D
|
E
|
F
|
G
|
|
PAH
PH-lung |
PVOD |
PV stenosis |
Stiff LA |
MS |
MR |
HFpEF |
HFrEF |
AS |
| Mean PAP |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
| Mean PAWP |
↓/N |
N |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
| LVEDP |
↓/N |
↓/N |
↓/N |
↓/N |
↓/n |
↑ |
↑ |
↑ |
↑ |
| LA size |
N |
N |
N |
↑ |
↑ |
↑ |
↑ |
↑ |
↑ |
| MV |
N |
N |
N |
N |
Stenosis ± regurg. |
Regurg. |
N/regurg.†
|
N/regurg.†
|
N/regurg.†
|
| eʹ |
N |
N |
N |
N |
↓*
|
↓ |
↓ |
↓ |
N/↓ |
| LVEF |
N |
N |
N |
N |
N |
N/↓ |
N |
↓ |
N/↓ |
| AV |
N |
N |
N |
N |
N |
N |
N |
N |
Stenosis |
Pulmonary arterial hypertension (groups 1, 3, 4, and at least in part group 5 in table 1; level A in figure 3) is characterised by an obstruction at the level of the pulmonary arteries and arterioles (table 4). Pulmonary arterial hypertension is mentioned here only for didactic purposes. Diagnostic pathways and management strategies are described in detail in current guidelines [1].
Pulmonary veno-occlusive disease (PVOD; level B in Figure 3) is actually not an left-sided heart disease but is still due to a postcapillary problem in that the obstruction is at the level of the pulmonary venules. The constellation of high mean PAP and high mean PAWP (but not LVEDP, table 4) mimics left-sided heart disease. Nonetheless, PVOD has been categorised as group 1 (group 1ʹ, table 1). PVOD is a very rare disease, which is diagnosed on the basis of haemodynamic and typical high-resolution computed tomography findings. A correct diagnosis is important, since pulmonary vasodilator therapy may precipitate pulmonary oedema [1]. Pulmonary tumour thrombotic microangiopathy is another very rare disease characterised by obstruction of the terminal pulmonary vascular bed (currently categorised as group 5: “pulmonary hypertension with unclear and/or multifactorial mechanism”). Haemodynamic measurements reveal a high PAP and a low LVEDP. The PAWP is typically intermediate, since obstruction of the small pulmonary vessels prevents backward transmission of left atrial pressure, and PAWP represents a backward reflection of PAP. The disease is most often fatal, and diagnosis is obtained post-mortem [41].
Pulmonary vein stenosis (level C in fig. 3) is typically an acquired disease occurring after catheter ablation of atrial fibrillation and resulting from previously used techniques of pulmonary vein isolation. The diagnosis is based on echocardiography, computed tomography and invasive haemodynamic measurements.
Left atrial disease (level D in fig. 3): The left atrium makes an important contribution to optimal left ventricular filling and thus stroke volume. Chronic left atrial overload in the context of left ventricle and mitral valve disease results in decreased left atrial compliance and contractility. The severity of left atrial dysfunction determines how increased left ventricular pressures are transmitted to the pulmonary circulation. An extreme form of left atrial disease not directly resulting from left ventricular disease and also occurring in presence of low LVEDP is the “stiff left atrium” after extensive catheter ablation in the left atrium leads to fibrosis of large parts of the left atrium [42]. This disease is characterised by a discrepancy between PAWP / left atrial pressure and LVEDP. The diagnosis is based on history, echocardiography with exclusion of significant mitral regurgitation, invasive haemodynamic measurements and exclusion of pulmonary valve stenosis by computed tomography.
Mitral valve disease (level E in fig. 3): Mitral stenosis is the classical disease leading to postcapillary pulmonary hypertension, which if longstanding is often accompanied by a precapillary component. The haemodynamic hallmark of the disease and prerequisite for the diagnosis, made by use of echocardiography and/or simultaneous right and left heart catheterisation, is a significant diastolic pressure gradient from the left atrium to the left ventricle (table 4). In the Western world, mitral regurgitation is now much more common than mitral stenosis and can also lead to pulmonary hypertension as a result of left ventricular dysfunction following volume overload and systolic backflow into the left atrium, which, depending on left atrial compliance, will lead to increased left atrial pressure and pulmonary hypertension. The haemodynamic characteristics of pulmonary hypertension in the context of mitral regurgitation include elevated PAP, elevated PAWP with high v waves (= left ventricular contraction in the presence of a leaking mitral valve) and high LVEDP. Mitral regurgitation can be due to organic mitral valve disease (typically mitral valve prolapse; primary mitral regurgitation) or secondary due to distorted left ventricular geometry in the context of left ventricular dysfunction. The diagnostic work-up in patients with mitral regurgitation includes transthoracic and transoesophageal echocardiography to define the mitral valve anatomy and the mechanism of regurgitation, as well as examinations to investigate the cause of left ventricular dysfunction in cases of secondary mitral valve regurgitation (coronary angiography, cardiac magnetic resonance imaging).
Left ventricular disease (level F in fig. 3): Any form of significant left ventricular systolic and/or diastolic dysfunction associated with increased LVEDP and left atrial pressure can lead to PH-LHD. There are two major form of heart failure that differ fundamentally in terms of epidemiology, left ventricular structure and function, and response to treatment: HFrEF and HFpEF, the LVEF cut-off separating the two entities traditionally being set at 50% [43]. A detailed discussion of the pathophysiology and diagnosis of HFrEF and HFpEF is beyond the scope of this review. In brief, the left ventricle in HFrEF patients is dilated with eccentric remodelling and impaired systolic and diastolic function. Common aetiologies include coronary artery disease and dilated cardiomyopathy. In contrast, the left ventricle in HFpEF is not dilated, with concentric remodelling and preserved LVEF and left ventricular diastolic dysfunction. The haemodynamic hallmark of HFpEF is the steep end-diastolic pressure volume curve of the small left ventricle, i.e., high sensitivity of the left ventricular pressure to changes in preload [43]. Preserved LVEF is not synonymous with normal systolic left ventricular function. Subtle left ventricular systolic dysfunction (reduced longitudinal strain) is common, which in conjunction with the diastolic properties of the left ventricle leads to reduced stroke volume and stroke volume reserve. Patients with HFpEF are typically older and more likely to be female than HFrEF patients, and the most common aetiology underlying HFpEF is probably long-standing systemic hypertension. Whereas the diagnosis of HFrEF is relatively straightforward, the diagnosis of HFpEF can be challenging, although a diagnostic algorithm has been proposed [44]. The most recent guidelines suggest a third form of heart failure: heart failure with mid-range ejection fraction (HFmrEF) [45]. The underlying rationale is related to the fact that, on the one hand, therapeutic studies in HFrEF have typically included patients with significantly impaired LVEF (LVEF <40% or even 35%) and, on the other hand, there is evidence that “true” HFpEF is characterised by an LVEF of at least 50%. Thus, there is a group of patients with HF and an LVEF of 40–49%, which is now labelled as HFmrEF (HFrEF: LVEF <40%, HFpEF: LVEF ≥50%). Most likely these patients should be looked at and treated as HFrEF.
Left ventricular outflow tract (level G in fig. 3): Aortic stenosis is the most common valve disease in the ageing population. Severe aortic stenosis can lead to left ventricular hypertrophy, diastolic left ventricular dysfunction, and finally left ventricular systolic dysfunction, which can result in increased LVEDP, increased left atrial pressure, and pulmonary hypertension. The diagnosis of aortic stenosis can usually be made with transthoracic echocardiography. Additional imaging modalities (transoesophageal echocardiography, computed tomography, left heart catheterisation with direct simultaneous measurement of left ventricular and aortic pressures) may be required in selected cases and to plan catheter-based valve implantation. Relatively rare diseases with a similar pathophysiology in terms of the level of obstruction in the circulation include hypertrophic obstructive cardiomyopathy (dynamic left ventricular outflow tract obstruction), subaortic stenosis (subaortic membrane) and aortic coarctation. Aortic regurgitation is associated with left ventricular volume overload, which can lead to left ventricular dysfunction, a rise in filling pressures and, eventually, pulmonary hypertension.
Management of pulmonary hypertension associated with left-sided heart disease
General approach
The principle of therapy in patients with PH-LHD is to treat the underlying left-sided heart disease in an optimal manner. Importantly, there is no established role for specific pulmonary arterial hypertension therapeutics. Table 5 provides an overview of the treatment options for patients with different forms of PH-LHD. Some aspects are commented on in the following section. In particular, data on specific pulmonary arterial hypertension therapies are discussed (table 6).
Table 5 Treatment of different entities of pulmonary hypertension associated with left-sided heart disease.
|
Entity
|
Treatment
|
| Pulmonary vein stenosis |
Stenting |
| Stiff left atrium |
Diuretics
Rate/rhythm control of atrial fibrillaton |
| Mitral stenosis |
Valvuloplasty
Valve replacement |
Mitral regurgitation, primary
Mitral regurgitation, secondary |
Surgical mitral valve repair
Mitral valve replacement
Catheter-based mitral valve repair
Medical and device HFrEF therapy (cf. below)
Surgical mitral valve repair
Surgical mitral valve replacement
Catheter-based mitral valve repair |
| Heart failure with reduced ejection fraction |
Diuretics
ACE inhibitors / angiotensin receptor blockers
Angiotensin receptor neprilysin inhibitors
Beta-blockers
Mineralocorticoid receptor antagonists
Ivabradine
Cardiac resynchronisation
Exercise training
Cardiac transplantation
Assist device
Myocardial revascularisation |
| Heart failure with preserved ejection fraction |
Diuretics
Blood pressure control
Rate/rhythm control in atrial fibrillation
Spironolactone |
| Aortic stenosis |
Surgical aortic valve replacement
Catheter-based aortic valve implantation |
| Hypertrophic obstructive cardiomyopathy |
Beta-blockers
Calcium channel blockers
Alcohol septal ablation
Surgical myectomy |
| Aortic regurgitation |
Valve replacement |
Table 6 Studies on pulmonary vasodilators in pulmonary hypertension associated with left heart disease and left heart diseases.
|
Population
|
Intervention
|
Primary finding
|
|
Heart failure with reduced ejection fraction
|
| FIRST [46] |
LVEF <35%, NYHA III/IV
(n = 370) |
Epoprostenol (median dose 4.0 ng/kg/min) |
Cardiac index↑
mean PAWP↓
Early termination; trend towards increased mortality in verum group |
| REACH-1 [47] |
LVEF <35%, NYHA III/IV
(n = 370) |
Bosentan 2×500 mg vs placebo for 26 weeks |
Early termination due to safety concerns (early worsening heart failure) |
| ENABLE (unpublished, summarised in [48]) |
LVEF <35%, NYHA III/IV
(n = 1613) |
Bosentan 2×125 mg vs placebo |
No effect on mortality or heart failure hospitalisation |
| HEAT [49] |
LVEF ≤35%, NYHA III, mean PAWP >12 mm Hg, cardiac index <2.6 l/min/m2
(n = 157) |
Darusentan vs placebo for 3 weeks |
Cardiac index↑
No effect on mean PAWP |
| EARTH [50] |
LVEF <35%, NYHA II–IV
(n = 642) |
Darusentan vs placebo for 24 weeks |
No effect on change in left ventricular end-systolic volume
No effect on symptoms |
| Guazzi et al. [51] |
LVEF <40%, NYHA II/III
(n = 46) |
Sildenafil 3×50 mg versus placebo for 6 months |
Systolic PAP↓
Peak VO2↑ |
| Lewis et al. [52] |
LVEF <40%, NYHA II–IV, mean PAP >25 mm Hg
(n = 34) |
Sildenafil 3×5–75 mg vs placebo for 12 weeks |
Peak VO2↑
Cardiac output ↑and PVR↓ during exercise |
| LEPHT [53] |
LVEF ≤40% and mean PAP ≥25 mm Hg (n = 201)
Mean PAP ≈ 38 mm Hg, mean PAWP ≈ 24 mm Hg |
Riociguat 3×0.5, 1.0 or 2.0 mg vs placebo
over 16 weeks |
No effect on mean PAP
Cardiac index and stroke volume↑
PVR and SVR↓ |
| PITCH-HF |
LVEF <40% and mean PAP ≥25 mm Hg |
Tadalafil 1×20 mg for 1 week, then 1×40 mg vs placebo |
Clinical endpoints, but study terminated early |
| SIL-HF [54] |
LVEF ≤40% and systolic PAP ≥40 mm Hg (echo) |
Sildenafil 3×40 mg vs placebo |
Symptoms and 6-min walking distance, study ongoing |
|
Heart failure with preserved ejection fraction
|
| Guazzi et al. [55] |
LVEF ≥50%, systolic PAP >40 mm Hg
(n = 44)
Mean PAP ≈ 37 mm Hg, mean PAWP ≈ 22 mm Hg |
Sildenafil 3×50 mg vs placebo for 6 months |
Mean PAP↓, mean PAWP↓
Cardiac index↑
Right ventricular function↑ |
| RELAX [56] |
LVEF ≥50% + elevated NT-proBNP or noninvasive evidence of elevated filling pressures
(n = 216) |
Sildenafil 3×20 mg for 12 weeks, then 3×60 mg for 12 weeks vs placebo |
No effect on peak VO2
No effect on 6-min walking distance |
| Hoendermis et al. [57] |
LVEF ≥45%, mean PAP >25 mm Hg, mean PAWP >15 mm Hg |
Sildenafil 3×60 mg vs placebo for 12 weeks |
No effect on mean PAP
No effect on mean PAWP, cardiac output and peak VO2
|
| DILATE [58] |
LVEF>50%, mean PAP ≥25 mm Hg, mean PAWP >15 mm Hg
(n = 39)
Mean PAP ≈ 35 mm Hg, mean PAWP ≈ 20 mm Hg |
Single dose of riociguat 0.5, 1.0, or 2.0 mg vs placebo |
No effect on mean PAP after 6 hours
Stroke volume↑
Systolic blood pressure↓
Right ventricular end-diastolic area |
|
Heart failure with reduced or preserved ejection fraction
|
| MELODY-1 |
Combined precapillary and postcapillary PH due to LV dysfunction despite optimised diuretic therapy |
Macitentan 10 mg for 12 weeks |
Study completed but no results available yet
Primary endpoint: fluid retention or worsening NYHA class
Secondary endpoint: change in PVR |
Mitral valve disease
A detailed discussion of indications for and methods of valve surgery or catheter-based modalities for the treatment of valve disease is beyond the scope of this review and can be found elsewhere [59]. Some aspects are important with regards to pulmonary hypertension, however. In general, the presence of pulmonary hypertension in a patient with mitral stenosis or regurgitation represents an indication for an intervention. In patients with isolated postcapillary pulmonary hypertension, PAP typically normalises after correction of the mitral valve lesion. In patients with combined postcapillary and precapillary pulmonary hypertension, different haemodynamic responses to the elimination of the mechanical mitral valve problem can occur: ideally, the reduction in left atrial pressure is followed by normalisation of the precapillary component of pulmonary hypertension. However, in patients with a long-standing, significant precapillary component pulmonary hypertension can persist after left atrial pressure reduction, as is typically seen in patients with rheumatic mitral stenosis. This phenomenon can even result in the haemodynamic constellation of pulmonary arterial hypertension (i.e., a relatively normal PAWP but a significantly elevated DPG and PVR after correction of the mitral valve problem) and patients may remain symptomatic.
Heart failure with reduced ejection fraction
The most important treatment in patients with PH-LHD due to HFrEF is the standard medical treatment for HFrEF, which has been described in detail elsewhere [45]. The cornerstones of long-term therapy in these patients are summarised in table 5. The presence of pulmonary hypertension in HFrEF patients typically indicates venous congestion and this implies the need for intensified treatment, initially with diuretics, followed by optimisation of the measures with established prognostic benefit (table 5). Options in HFrEF patients with a significant precapillary pulmonary hypertension component include aggressive decongestion by diuretics and afterload reduction and/or the implantation of a left ventricular assist device. The latter has been shown to reduce both the postcapillary and the precapillary component of pulmonary hypertension in transplant candidates [12, 13]. There is currently no established role of specific pulmonary arterial hypertension therapies in patients with HFrEF. A number of studies using endothelin receptor antagonists and phosphodiesterase-5 inhibitors (PDE-5 inhibitors) have been performed in HFrEF patients [46–54] (table 6). Although the presence of pulmonary hypertension was not an inclusion criterion in these studies, these were typically patients with advanced HFrEF and presumably with elevated filling pressures, and thus the findings are potentially relevant to the management of PH-LHD in the context of HFrEF. Studies using endothelin receptor antagonists have, overall, revealed neutral results (table 6). One study reported an increase in cardiac index following short-term therapy (3 weeks) with darusentan [49]. A larger study using darusentan and a longer treatment period (24 weeks) showed no effect on left ventricular remodelling, and a study comparing bosentan and placebo found not effect on hard clinical endpoints [50]. Small, single-centre studies showed interesting effects of the PDE-5 inhibitor sildenafil on haemodynamics and exercise capacity in patients with PH-LHD in the context of HFrEF [51, 52]. Data on the effect of PDE-5 inhibitors on clinical endpoints in HFrEF and in PH-LHD in the context of HFrEF are not available, however. In a multicentre study, riociguat (a soluble guanylate cyclase stimulator) had no effect on mean PAP in HFrEF patients with significant PH-LHD (mean PAP approximately 38 mm Hg). There was, however, a decrease in PVR and an increase in stroke volume and cardiac output [53]. Additional trials on pulmonary vasodilators are underway, although at least one trial was stopped early (table 6).
Heart failure with preserved ejection fraction
There is still no treatment for patients with HFpEF with an established benefit in terms of survival [60]. In particular, large clinical trials have yielded neutral results with respect to mortality for inhibitors of the renin-angiotensin system and the mineralocorticoid receptor antagonist spironolactone. At least spironolactone has been shown to reduce the risk of rehospitalisation for heart failure. The management of PH-LHD in the context of HFpEF is not well defined either (table 5). The primary approach includes a combination of diuretic therapy and afterload reduction. It should be kept in mind, however, that a steep end-diastolic pressure–volume relationship is a pathophysiological hallmark in HFpEF patients, and that this makes them susceptible to significant changes in stroke volume and blood pressure following too aggressive preload reduction. Data on specific pulmonary arterial hypertension-specific therapies in HFpEF in general and HFpEF+PH-LHD are conflicting [55–58] (table 6). A placebo-controlled combined noninvasive and invasive study in patients with PH-LHD in the context of HFpEF revealed a significant reduction in mean PAP and an improvement in right ventricular function with sildenafil treatment [55]. On the other hand, a trial evaluating the use of sildenafil in patients with HFpEF (not necessarily with pulmonary hypertension) failed to show an improvement in exercise capacity compared with placebo [56]. In a carefully performed haemodynamic study specifically in patients with HFpEF und PH-LHD (mean PAP >25 mm Hg, mean PAWP >15 mm Hg) sildenafil had no effect on mean PAP compared with placebo [57]. Thus, the data currently do not support a role of sildenafil in the treatment of HFpEF patients with or without pulmonary hypertension. In a study investigating the acute haemodynamic effects of riociguat in HFpEF, no change in mean PAP was observed although there was an increase in stroke volume [58]. An interesting novel approach is the catheter-based creation of an intracardiac shunt (“neo-atrial septal defect”) to allow controlled decompression of the left atrium. An uncontrolled study in HFpEF patients with elevated PAWP at rest or during exercise (haemodynamics at baseline at rest: mean PAP 25 mm Hg, mean PAWP 17 mm Hg) has revealed promising results with regards to haemodynamics and exercise capacity [61], but data from a randomised study are not available yet.
Left ventricular outflow tract
Aortic valve replacement or catheter-based aortic valve implantation is the method of choice for the treatment of symptomatic aortic stenosis. Mild postcapillary pulmonary hypertension is common in patients with symptomatic aortic stenosis and usually resolves after valve replacement. In those with significant reactive postcapillary pulmonary hypertension the same considerations apply as for mitral valve disease.
Conclusions
PH-LHD is the most common type of pulmonary hypertension, which in a patient with left-sided heart disease is typically a marker of more advanced disease, worse exercise tolerance and worse prognosis. In contrast to pulmonary arterial hypertension, PH-LHD is characterised by an elevated PAWP (postcapillary pulmonary hypertension), without or with an additional precapillary component (isolated postcapillary or combined postcapillary and precapillary pulmonary hypertension). The work-up should reveal the pulmonary hypertension severity, the haemodynamic constellation, and the exact mechanisms of left-sided heart disease that led to PH-LHD. The general principle for the management of PH-LHD is to treat the underlying left-sided heart disease in an optimal manner using drugs and/or interventional or surgical therapy. The use of pulmonary arterial hypertension-specific therapies is contraindicated in patients with PH-LHD according to current guidelines [1].
References
1
Galiè
N
,
Humbert
M
,
Vachiery
JL
,
Gibbs
S
,
Lang
I
,
Torbicki
A
, et al.
2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J. 2016;37(1):67–119. doi:.https://doi.org/10.1093/eurheartj/ehv317
2
Maeder
MT
,
Kleiner
R
,
Weilenmann
D
,
Schoch
OD
. Pulmonary hypertension associated with left heart and lung diseases. Cardiovasc Med.
2014;17:320–7.
3
Rosenkranz
S
,
Gibbs
JS
,
Wachter
R
,
De Marco
T
,
Vonk-Noordegraaf
A
,
Vachiéry
JL
. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37(12):942–54. doi:.https://doi.org/10.1093/eurheartj/ehv512
4
Vachiéry
JL
,
Adir
Y
,
Barberà
JA
,
Champion
H
,
Coghlan
JG
,
Cottin
V
, et al.
Pulmonary hypertension due to left heart diseases. J Am Coll Cardiol. 2013;62(25, Suppl):D100–8. doi:.https://doi.org/10.1016/j.jacc.2013.10.033
5
Maeder
MT
,
Kleiner
R
,
Weilenmann
D
. Severely worsening dyspnea after initiation of macitentan therapy for pulmonary arterial hypertension. Int J Cardiol. 2016;202:244–5. doi:.https://doi.org/10.1016/j.ijcard.2015.08.132
6
Boilson
BA
,
Schirger
JA
,
Borlaug
BA
. Caveat medicus! Pulmonary hypertension in the elderly: a word of caution. Eur J Heart Fail. 2010;12(1):89–93. doi:.https://doi.org/10.1093/eurjhf/hfp171
7
Gerges
M
,
Gerges
C
,
Pistritto
AM
,
Lang
MB
,
Trip
P
,
Jakowitsch
J
, et al.
Pulmonary Hypertension in Heart Failure. Epidemiology, Right Ventricular Function, and Survival. Am J Respir Crit Care Med. 2015;192(10):1234–46. doi:.https://doi.org/10.1164/rccm.201503-0529OC
8
Lam
CS
,
Roger
VL
,
Rodeheffer
RJ
,
Borlaug
BA
,
Enders
FT
,
Redfield
MM
. Pulmonary hypertension in heart failure with preserved ejection fraction: a community-based study. J Am Coll Cardiol. 2009;53(13):1119–26. doi:.https://doi.org/10.1016/j.jacc.2008.11.051
9
Abramson
SV
,
Burke
JF
,
Kelly
JJ, Jr
,
Kitchen
JG, 3rd
,
Dougherty
MJ
,
Yih
DF
, et al.
Pulmonary hypertension predicts mortality and morbidity in patients with dilated cardiomyopathy. Ann Intern Med. 1992;116(11):888–95. doi:.https://doi.org/10.7326/0003-4819-116-11-888
10
Ghio
S
,
Gavazzi
A
,
Campana
C
,
Inserra
C
,
Klersy
C
,
Sebastiani
R
, et al.
Independent and additive prognostic value of right ventricular systolic function and pulmonary artery pressure in patients with chronic heart failure. J Am Coll Cardiol. 2001;37(1):183–8. doi:.https://doi.org/10.1016/S0735-1097(00)01102-5
11
Mentias
A
,
Patel
K
,
Patel
H
,
Gillinov
AM
,
Sabik
JF
,
Mihaljevic
T
, et al.
Effect of Pulmonary Vascular Pressures on Long-Term Outcome in Patients With Primary Mitral Regurgitation. J Am Coll Cardiol. 2016;67(25):2952–61. doi:.https://doi.org/10.1016/j.jacc.2016.03.589
12
Zimpfer
D
,
Zrunek
P
,
Roethy
W
,
Czerny
M
,
Schima
H
,
Huber
L
, et al.
Left ventricular assist devices decrease fixed pulmonary hypertension in cardiac transplant candidates. J Thorac Cardiovasc Surg. 2007;133(3):689–95. doi:.https://doi.org/10.1016/j.jtcvs.2006.08.104
13
Etz
CD
,
Welp
HA
,
Tjan
TD
,
Hoffmeier
A
,
Weigang
E
,
Scheld
HH
, et al.
Medically refractory pulmonary hypertension: treatment with nonpulsatile left ventricular assist devices. Ann Thorac Surg. 2007;83(5):1697–705. doi:.https://doi.org/10.1016/j.athoracsur.2007.01.019
14
Melenovsky
V
,
Hwang
SJ
,
Lin
G
,
Redfield
MM
,
Borlaug
BA
. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014;35(48):3452–62. doi:.https://doi.org/10.1093/eurheartj/ehu193
15
Borlaug
BA
,
Kane
GC
,
Melenovsky
V
,
Olson
TP
. Abnormal right ventricular-pulmonary artery coupling with exercise in heart failure with preserved ejection fraction. Eur Heart J. 2016;ehw241; epub ahead of print. doi:.https://doi.org/10.1093/eurheartj/ehw241
16
Kammerlander
AA
,
Marzluf
BA
,
Graf
A
,
Bachmann
A
,
Kocher
A
,
Bonderman
D
, et al.
Right ventricular dysfunction, but not tricuspid regurgitation, is associated with outcome late after left heart valve procedure. J Am Coll Cardiol. 2014;64(24):2633–42. doi:.https://doi.org/10.1016/j.jacc.2014.09.062
17
Galiè
N
,
Hoeper
MM
,
Humbert
M
,
Torbicki
A
,
Vachiery
JL
,
Barbera
JA
, et al.; ESC Committee for Practice Guidelines (CPG). Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J. 2009;30(20):2493–537. doi:.https://doi.org/10.1093/eurheartj/ehp297
18
Gerges
C
,
Gerges
M
,
Lang
MB
,
Zhang
Y
,
Jakowitsch
J
,
Probst
P
, et al.
Diastolic pulmonary vascular pressure gradient: a predictor of prognosis in “out-of-proportion” pulmonary hypertension. Chest. 2013;143(3):758–66. doi:.https://doi.org/10.1378/chest.12-1653
19
Tedford
RJ
,
Beaty
CA
,
Mathai
SC
,
Kolb
TM
,
Damico
R
,
Hassoun
PM
, et al.
Prognostic value of the pre-transplant diastolic pulmonary artery pressure-to-pulmonary capillary wedge pressure gradient in cardiac transplant recipients with pulmonary hypertension. J Heart Lung Transplant. 2014;33(3):289–97. doi:.https://doi.org/10.1016/j.healun.2013.11.008
20
Tampakakis
E
,
Leary
PJ
,
Selby
VN
,
De Marco
T
,
Cappola
TP
,
Felker
GM
, et al.
The diastolic pulmonary gradient does not predict survival in patients with pulmonary hypertension due to left heart disease. JACC Heart Fail. 2015;3(1):9–16. doi:.https://doi.org/10.1016/j.jchf.2014.07.010
21
Guazzi
M
,
Borlaug
BA
. Pulmonary hypertension due to left heart disease. Circulation. 2012;126(8):975–90. doi:.https://doi.org/10.1161/CIRCULATIONAHA.111.085761
22
Gerges
M
,
Gerges
C
,
Lang
IM
. How to define pulmonary hypertension due to left heart disease. Eur Respir J. 2016;48(2):553–5. doi:.https://doi.org/10.1183/13993003.00432-2016
23
McGoon
M
,
Gutterman
D
,
Steen
V
,
Barst
R
,
McCrory
DC
,
Fortin
TA
, et al.; American College of Chest Physicians. Screening, early detection, and diagnosis of pulmonary arterial hypertension: ACCP evidence-based clinical practice guidelines. Chest. 2004;126(1, Suppl):14S–34S. doi:.https://doi.org/10.1378/chest.126.1_suppl.14S
24
Rich
JD
,
Shah
SJ
,
Swamy
RS
,
Kamp
A
,
Rich
S
. Inaccuracy of Doppler echocardiographic estimates of pulmonary artery pressures in patients with pulmonary hypertension: implications for clinical practice. Chest. 2011;139(5):988–93. doi:.https://doi.org/10.1378/chest.10-1269
25
Testani
JM
,
St John Sutton
MG
,
Wiegers
SE
,
Khera
AV
,
Shannon
RP
,
Kirkpatrick
JN
. Accuracy of noninvasively determined pulmonary artery systolic pressure. Am J Cardiol. 2010;105(8):1192–7. doi:.https://doi.org/10.1016/j.amjcard.2009.11.048
26
Chemla
D
,
Castelain
V
,
Humbert
M
,
Hébert
JL
,
Simonneau
G
,
Lecarpentier
Y
, et al.
New formula for predicting mean pulmonary artery pressure using systolic pulmonary artery pressure. Chest. 2004;126(4):1313–7. doi:.https://doi.org/10.1378/chest.126.4.1313
27
Simon
MA
,
Rajagopalan
N
,
Mathier
MA
,
Shroff
SG
,
Pinsky
MR
,
López-Candales
A
. Tissue Doppler imaging of right ventricular decompensation in pulmonary hypertension. Congest Heart Fail. 2009;15(6):271–6. doi:.https://doi.org/10.1111/j.1751-7133.2009.00113.x
28
Mullens
W
,
Borowski
AG
,
Curtin
RJ
,
Thomas
JD
,
Tang
WH
. Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation. 2009;119(1):62–70. doi:.https://doi.org/10.1161/CIRCULATIONAHA.108.779223
29
Thenappan
T
,
Shah
SJ
,
Gomberg-Maitland
M
,
Collander
B
,
Vallakati
A
,
Shroff
P
, et al.
Clinical characteristics of pulmonary hypertension in patients with heart failure and preserved ejection fraction. Circ Heart Fail. 2011;4(3):257–65. doi:.https://doi.org/10.1161/CIRCHEARTFAILURE.110.958801
30
Opotowsky
AR
,
Ojeda
J
,
Rogers
F
,
Prasanna
V
,
Clair
M
,
Moko
L
, et al.
A simple echocardiographic prediction rule for hemodynamics in pulmonary hypertension. Circ Cardiovasc Imaging. 2012;5(6):765–75. doi:.https://doi.org/10.1161/CIRCIMAGING.112.976654
31
D’Alto
M
,
Romeo
E
,
Argiento
P
,
Pavelescu
A
,
Mélot
C
,
D’Andrea
A
, et al.
Echocardiographic prediction of pre- versus postcapillary pulmonary hypertension. J Am Soc Echocardiogr. 2015;28(1):108–15. doi:.https://doi.org/10.1016/j.echo.2014.09.004
32
Bonderman
D
,
Wexberg
P
,
Heinzl
H
,
Lang
IM
. Non-invasive algorithms for the diagnosis of pulmonary hypertension. Thromb Haemost. 2012;108(6):1037–41. doi:.https://doi.org/10.1160/TH12-04-0239
33
Abbas
AE
,
Fortuin
FD
,
Schiller
NB
,
Appleton
CP
,
Moreno
CA
,
Lester
SJ
. A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol. 2003;41(6):1021–7. doi:.https://doi.org/10.1016/S0735-1097(02)02973-X
34
Maeder
MT
,
Karapanagiotidis
S
,
Dewar
EM
,
Gamboni
SE
,
Htun
N
,
Kaye
DM
. Accuracy of Doppler echocardiography to estimate key hemodynamic variables in subjects with normal left ventricular ejection fraction. J Card Fail. 2011;17(5):405–12. doi:.https://doi.org/10.1016/j.cardfail.2010.12.003
35
Hoeper
MM
,
Bogaard
HJ
,
Condliffe
R
,
Frantz
R
,
Khanna
D
,
Kurzyna
M
, et al.
Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25, Suppl):D42–50. doi:.https://doi.org/10.1016/j.jacc.2013.10.032
36
Maeder
MT
,
Thompson
BR
,
Brunner-La Rocca
HP
,
Kaye
DM
. Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. J Am Coll Cardiol. 2010;56(11):855–63. doi:.https://doi.org/10.1016/j.jacc.2010.04.040
37
Robbins
IM
,
Hemnes
AR
,
Pugh
ME
,
Brittain
EL
,
Zhao
DX
,
Piana
RN
, et al.
High prevalence of occult pulmonary venous hypertension revealed by fluid challenge in pulmonary hypertension. Circ Heart Fail. 2014;7(1):116–22. doi:.https://doi.org/10.1161/CIRCHEARTFAILURE.113.000468
38
Borlaug
BA
,
Nishimura
RA
,
Sorajja
P
,
Lam
CS
,
Redfield
MM
. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3(5):588–95. doi:.https://doi.org/10.1161/CIRCHEARTFAILURE.109.930701
39
Herve
P
,
Lau
EM
,
Sitbon
O
,
Savale
L
,
Montani
D
,
Godinas
L
, et al.
Criteria for diagnosis of exercise pulmonary hypertension. Eur Respir J. 2015;46(3):728–37. doi:.https://doi.org/10.1183/09031936.00021915
40
Pulido
T
,
Adzerikho
I
,
Channick
RN
,
Delcroix
M
,
Galiè
N
,
Ghofrani
HA
, et al.; SERAPHIN Investigators. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369(9):809–18. doi:.https://doi.org/10.1056/NEJMoa1213917
41
Buser
M
,
Felizeter-Kessler
M
,
Lenggenhager
D
,
Maeder
MT
. Rapidly progressive pulmonary hypertension in a patient with pulmonary tumor thrombotic microangiopathy. Am J Respir Crit Care Med. 2015;191(6):711–2. doi:.https://doi.org/10.1164/rccm.201501-0004IM
42
Gibson
DN
,
Di Biase
L
,
Mohanty
P
,
Patel
JD
,
Bai
R
,
Sanchez
J
, et al.
Stiff left atrial syndrome after catheter ablation for atrial fibrillation: clinical characterization, prevalence, and predictors. Heart Rhythm. 2011;8(9):1364–71. doi:.https://doi.org/10.1016/j.hrthm.2011.02.026
43
Maeder
MT
,
Kaye
DM
. Heart failure with normal left ventricular ejection fraction. J Am Coll Cardiol. 2009;53(11):905–18. doi:.https://doi.org/10.1016/j.jacc.2008.12.007
44
Paulus
WJ
,
Tschöpe
C
,
Sanderson
JE
,
Rusconi
C
,
Flachskampf
FA
,
Rademakers
FE
, et al.
How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur Heart J. 2007;28(20):2539–50. doi:.https://doi.org/10.1093/eurheartj/ehm037
45
Ponikowski
P
,
Voors
AA
,
Anker
SD
,
Bueno
H
,
Cleland
JG
,
Coats
AJ
, et al.; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200. doi:.https://doi.org/10.1093/eurheartj/ehw128
46
Califf
RM
,
Adams
KF
,
McKenna
WJ
,
Gheorghiade
M
,
Uretsky
BF
,
McNulty
SE
, et al.
A randomized controlled trial of epoprostenol therapy for severe congestive heart failure: The Flolan International Randomized Survival Trial (FIRST). Am Heart J. 1997;134(1):44–54. doi:.https://doi.org/10.1016/S0002-8703(97)70105-4
47
Packer
M
,
McMurray
J
,
Massie
BM
,
Caspi
A
,
Charlon
V
,
Cohen-Solal
A
, et al.
Clinical effects of endothelin receptor antagonism with bosentan in patients with severe chronic heart failure: results of a pilot study. J Card Fail. 2005;11(1):12–20. doi:.https://doi.org/10.1016/j.cardfail.2004.05.006
48
Kalra
PR
,
Moon
JC
,
Coats
AJ
. Do results of the ENABLE (Endothelin Antagonist Bosentan for Lowering Cardiac Events in Heart Failure) study spell the end for non-selective endothelin antagonism in heart failure?
Int J Cardiol. 2002;85(2-3):195–7. doi:.https://doi.org/10.1016/S0167-5273(02)00182-1
49
Lüscher
TF
,
Enseleit
F
,
Pacher
R
,
Mitrovic
V
,
Schulze
MR
,
Willenbrock
R
, et al.; Heart Failure ET(A) Receptor Blockade Trial. Hemodynamic and neurohumoral effects of selective endothelin A (ET(A)) receptor blockade in chronic heart failure: the Heart Failure ET(A) Receptor Blockade Trial (HEAT). Circulation. 2002;106(21):2666–72. doi:.https://doi.org/10.1161/01.CIR.0000038497.80095.E1
50
Anand
I
,
McMurray
J
,
Cohn
JN
,
Konstam
MA
,
Notter
T
,
Quitzau
K
, et al.; EARTH investigators. Long-term effects of darusentan on left-ventricular remodelling and clinical outcomes in the EndothelinA Receptor Antagonist Trial in Heart Failure (EARTH): randomised, double-blind, placebo-controlled trial. Lancet. 2004;364(9431):347–54. doi:.https://doi.org/10.1016/S0140-6736(04)16723-8
51
Guazzi
M
,
Tumminello
G
,
Di Marco
F
,
Fiorentini
C
,
Guazzi
MD
. The effects of phosphodiesterase-5 inhibition with sildenafil on pulmonary hemodynamics and diffusion capacity, exercise ventilatory efficiency, and oxygen uptake kinetics in chronic heart failure. J Am Coll Cardiol. 2004;44(12):2339–48. doi:.https://doi.org/10.1016/j.jacc.2004.09.041
52
Lewis
GD
,
Shah
R
,
Shahzad
K
,
Camuso
JM
,
Pappagianopoulos
PP
,
Hung
J
, et al.
Sildenafil improves exercise capacity and quality of life in patients with systolic heart failure and secondary pulmonary hypertension. Circulation. 2007;116(14):1555–62. doi:.https://doi.org/10.1161/CIRCULATIONAHA.107.716373
53
Bonderman
D
,
Ghio
S
,
Felix
SB
,
Ghofrani
HA
,
Michelakis
E
,
Mitrovic
V
, et al.; Left Ventricular Systolic Dysfunction Associated With Pulmonary Hypertension Riociguat Trial (LEPHT) Study Group. Riociguat for patients with pulmonary hypertension caused by systolic left ventricular dysfunction: a phase IIb double-blind, randomized, placebo-controlled, dose-ranging hemodynamic study. Circulation. 2013;128(5):502–11. doi:.https://doi.org/10.1161/CIRCULATIONAHA.113.001458
54
Cooper
TJ
,
Guazzi
M
,
Al-Mohammad
A
,
Amir
O
,
Bengal
T
,
Cleland
JG
, et al.
Sildenafil in Heart failure (SilHF). An investigator-initiated multinational randomized controlled clinical trial: rationale and design. Eur J Heart Fail. 2013;15(1):119–22. doi:.https://doi.org/10.1093/eurjhf/hfs152
55
Guazzi
M
,
Vicenzi
M
,
Arena
R
,
Guazzi
MD
. Pulmonary hypertension in heart failure with preserved ejection fraction: a target of phosphodiesterase-5 inhibition in a 1-year study. Circulation. 2011;124(2):164–74. doi:.https://doi.org/10.1161/CIRCULATIONAHA.110.983866
56
Redfield
MM
,
Chen
HH
,
Borlaug
BA
,
Semigran
MJ
,
Lee
KL
,
Lewis
G
, et al.; RELAX Trial. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: a randomized clinical trial. JAMA. 2013;309(12):1268–77. doi:.https://doi.org/10.1001/jama.2013.2024
57
Hoendermis
ES
,
Liu
LC
,
Hummel
YM
,
van der Meer
P
,
de Boer
RA
,
Berger
RM
, et al.
Effects of sildenafil on invasive haemodynamics and exercise capacity in heart failure patients with preserved ejection fraction and pulmonary hypertension: a randomized controlled trial. Eur Heart J. 2015;36(38):2565–73. doi:.https://doi.org/10.1093/eurheartj/ehv336
58
Bonderman
D
,
Pretsch
I
,
Steringer-Mascherbauer
R
,
Jansa
P
,
Rosenkranz
S
,
Tufaro
C
, et al.
Acute hemodynamic effects of riociguat in patients with pulmonary hypertension associated with diastolic heart failure (DILATE-1): a randomized, double-blind, placebo-controlled, single-dose study. Chest. 2014;146(5):1274–85. doi:.https://doi.org/10.1378/chest.14-0106
59
Vahanian
A
,
Alfieri
O
,
Andreotti
F
,
Antunes
MJ
,
Barón-Esquivias
G
,
Baumgartner
H
, et al.; Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC); European Association for Cardio-Thoracic Surgery (EACTS). Guidelines on the management of valvular heart disease (version 2012). Eur Heart J. 2012;33(19):2451–96. doi:.https://doi.org/10.1093/eurheartj/ehs109
60
Maeder
MT
,
Rickli
H
. Herzinsuffizienz mit erhaltener linksventrikulärer Auswurffraktion. [Heart failure with preserved left ventricular ejection fraction] Praxis (Bern). 2013;102(21):1299–307. Article in German. doi:.https://doi.org/10.1024/1661-8157/a001439
61
Hasenfuß
G
,
Hayward
C
,
Burkhoff
D
,
Silvestry
FE
,
McKenzie
S
,
Gustafsson
F
, et al.; REDUCE LAP-HF study investigators. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, open-label, single-arm, phase 1 trial. Lancet. 2016;387(10025):1298–304. doi:.https://doi.org/10.1016/S0140-6736(16)00704-2