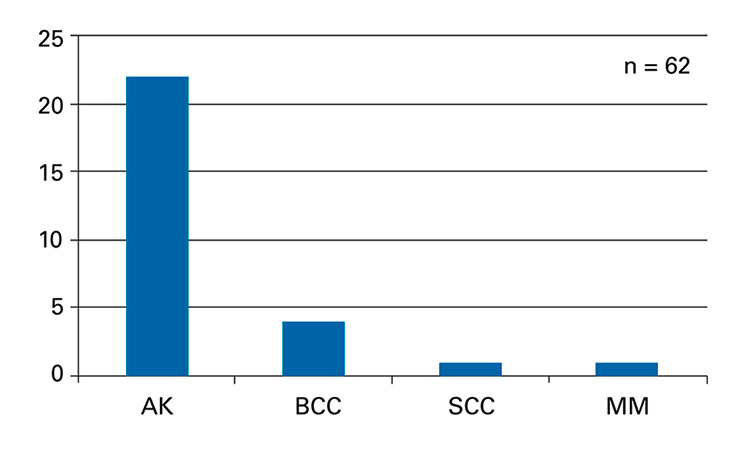
Figure 1
Individuals clinically diagnosed with actinic keratosis (AK), basal-cell carcinoma (BCC), squamous-cell carcinoma (SCC), and with high suspicion for melanoma (MM) during a full body check-up by a dermatologist using a dermatoscope.
DOI: https://doi.org/10.4414/smw.2016.14380
Nonmelanoma skin cancer (NMSC) is the most common cancer in Caucasians worldwide, and Switzerland has one of the highest rates in Europe [1, 2]. One of the premalignant stages of NMSC is actinic keratosis (AK), which progresses to NMSC in up to 8% of all cases [3, 4]. Although NMSC and AK have an enormous socioeconomic impact [5] and can be lethal, these malignant diseases are typically not recognised in conventional National Cancer Registries. Ultraviolet (UV) radiation, the main risk factor for NMSC [3, 4, 6], increases by approximately 10–12% with every 1000 m of increased altitude owing to the thinner atmosphere [7] and is not sufficiently shielded by clouds [7–9]. An additional factor that increases UV exposure at higher altitudes is snowfields, which reflect up to 80% of UV radiation [7]. As mountain and ski guides spend most of their professional time on mountains at altitude (e.g., up to 4800 m in Europe and up to 8800 m in the Himalayas), their median UV exposure is six times the threshold limit issued by the International Radiation Protection Association and other societies [10]. Reports suggest a significantly increased risk for NMSC in all active guides in mountainous areas due to these high UV doses [11, 12]. The role of individual precautions taken against the development of NMSC, however, remains unclear. Sunscreen products have improved noticeably within the past few years, and NMSC recently received significant attention after being officially recognised as an occupational disease in Germany in 2015 [13]. Nonetheless, studies focusing on NMSC related to specific outdoor activities are rare and data required to develop evidence-based prevention recommendations for specific outdoor professions are virtually unavailable. Thus the aim of this study was to examine the prevalence of NMSC and its precancerous lesions, and the associated risk behaviour of mountain and ski guides in order to develop future awareness and prevention programmes.
This cross-sectional study was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee of the Technical University of Munich. All participants were over the age of 18 and provided written informed consent prior to study inclusion. The inclusion criteria were official membership of the German Association of Mountain and Ski Guides and official certification as a mountain and ski guide by the government. All data were collected during the annual general assembly of the German Association of Mountain and Ski Guides 2016. All members of the association (approximately 700 people) were informed of the study prior to the meeting by e-mail and were reminded of the study details at the meeting via posters. Completion of the paper-based questionnaire was a prerequisite for the skin check-up that was performed by an experienced dermatologist using a dermatoscope. NMSC, AK and other skin-related findings were documented, and the participants were referred to a local dermatologist for further treatment. Apart from general data (age, sex and residence), the paper-based questionnaire included questions on risk behaviour and risk factors for NMSC (number of annual tours and sunburns within the last few years and in childhood), sun protection methods (wearing of long clothes and headgear [14, 15], general use of sunscreen and of what sun protection factor [SPF] [16]), regular skin self-examination and previous dermatological consultations for skin check-ups or any other reason. The study questionnaire was custom-designed with adaptions from a validated sun protection questionnaire. Questions with multiple answers were analysed according to the highest-ranked responses. For example, the highest marked SPF in the question about the mostly chosen SPF in sunscreen products was used for statistical analysis. Data management and analyses were performed with SAS onDemand version 3.2. Owing to the limited study population, only descriptive statistical analysis was performed for risk factors and medical findings. Means and standard deviations were calculated and frequencies analysed; ranges were provided where feasible.
Of the 81 association affiliates attending the annual meeting of the Certified Mountain and Ski Guides in 2016, 62 (55 men and 7 women) member guides agreed to participate in the study. Participant mean age was 52.9 ± 13.4 years (range 30–78 years), and mean duration of experience as a mountain and ski guide was 22.4 ± 15.5 years, with an average of 99.5 ± 63.9 mountain or ski tours every year (table 1).
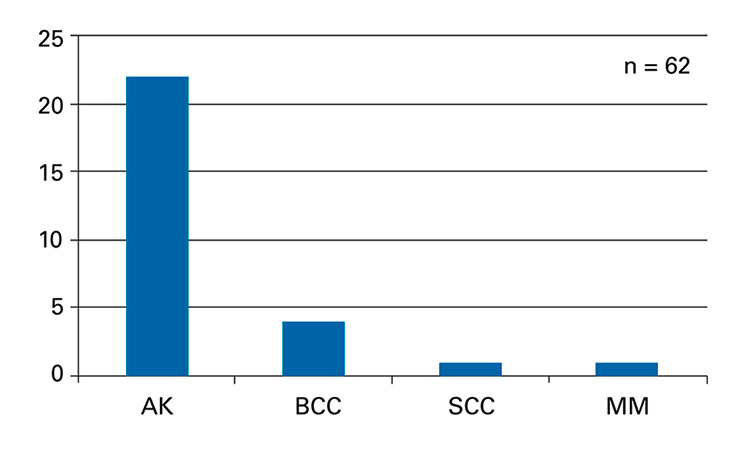
Figure 1
Individuals clinically diagnosed with actinic keratosis (AK), basal-cell carcinoma (BCC), squamous-cell carcinoma (SCC), and with high suspicion for melanoma (MM) during a full body check-up by a dermatologist using a dermatoscope.
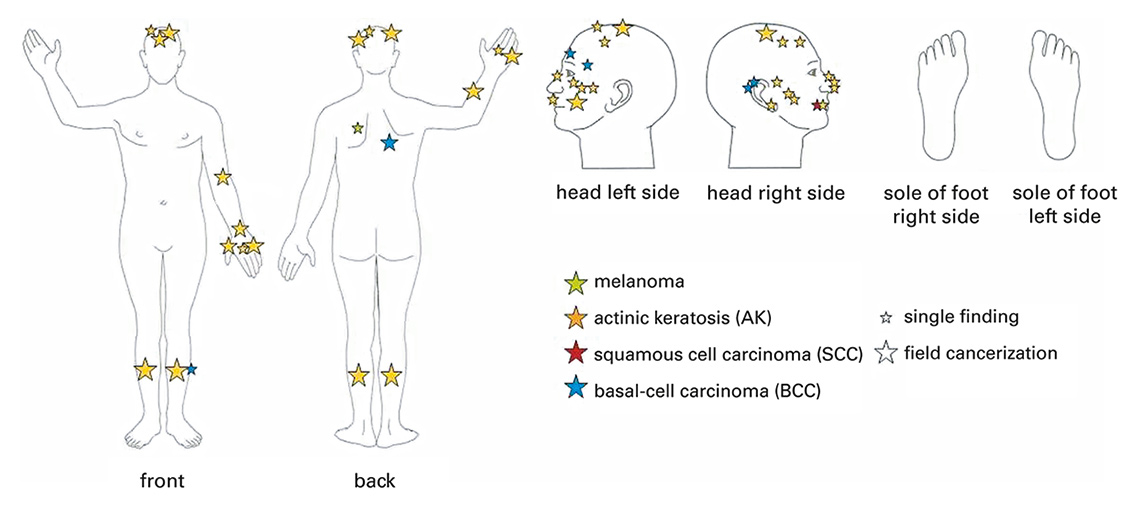
Figure 2
Graphical presentation of nonmelanoma skin cancer and its premalignant stages found during the full-body skin examination of all participants by a dermatologist. The size of the stars depicts the number of findings: a small star represents a single finding, a big star field cancerization.
A professional skin check-up by a dermatologist was performed exclusively after the participants had completed the paper-based questionnaire, which allowed for complete data on skin cancer and its precursors for all participants. As expected, not all questions of the self-completed questionnaire were answered by all participants; for example, three participants did not state the yearly number of mountain tours. Through the screening, 22 participants (35.4%) were clinically diagnosed with AK and 5 participants (8.1%) with NMSC (1 with squamous-cell carcinoma, and 4 with basal-cell carcinoma [BCC]; fig. 1). Of note, a skin lesion with a high probability of being a malignant melanoma was found in one participant. Most of the findings mentioned were located on the typically sun-exposed body parts (head, lower legs, and lower arms), except for two cases of BCC located on the upper back (fig. 2).
In the questionnaire (table 2), 59.7% (37 participants) stated that they would like to improve their sun protection and almost half (48.4%) had never consulted a dermatologist in their life before. Only 17.7% asserted that they have their skin examined for UV radiation-induced changes on a regular basis. In addition, 34.4% (21 participants) had experienced sunburn at least once in the last year and 63.9% (39 participants) had experienced sunburn in their childhood at least once a year. In total, 34.4% (21 participants) used sunscreen occasionally, rarely, or never. If sunscreen was used by participants during a typical mountain day tour, 31.9% used one with a SPF less than 30. Long-sleeved shirts were worn by 16.1% of the participants, long trousers by 43.5% and a hat by 79.0%. Interestingly, 95.2% participants said they were aware that UV radiation was the main risk factor for skin cancer. However, 83.6% lamented that there is not enough information available about skin cancer, especially for the specific needs of mountain and ski guides, who spend several hours daily outdoors during tours.
| Table 1: Baseline characteristics of 62 alpine guides (n = 62; 7 women, 55 men). | |||
| Variable | Mean | SD | Range |
| Age, years | 52.9 | 13.4 | 30–78 |
| Experience as an alpine guide, years | 22.4 | 15.5 | 1–52 |
| Alpine tours per year, n | 99.5 | 63.9 | 5–300 |
| Table 2: Answers given by alpine guides in the self-completed paper-based questionnaire (n = 62). | ||
| Question | Yes n (%) | No n (%) |
| Have you ever been to a dermatologist? | 32 (51.6%) | 30 (48.4%) |
| Do you regularly see a dermatologist for a skin check-up? | 11 (17.7%) | 51 (82.3%) |
| Do you think ultraviolet radiation is the main risk factor for skin cancer? | 59 (95.2%) | 3 (4.8%) |
| Do you regularly use sunscreen during alpine tours? | 41 (65.6%) | 21 (34.4%) |
| Do you think you should improve your sun protection measures during alpine tours? | 37 (59.7%) | 25 (40.3%) |
| Have you experienced sunburn at least once during alpine tours within the last year? | 21 (34.4%) | 41 (65.6%) |
| Do you remember experiencing sunburn in childhood? | 39 (63.9%) | 23 (36.1%) |
| There is enough information available about skin cancer and risk for me as mountain guide. | 10 (16.4%) | 51 (83.6%) |
Our findings confirm the results of an NMSC prevalence cross-sectional study in mountain guides conducted in 1999. During several local mountain guide meetings, 283 male guides from Austria, Germany, and Switzerland were assessed with a standardised interview and a medical examination [12]. The rate of NMSC prevalence in our study (8.1%) is comparable to that of the 1991 study (8.5%), whereas AK prevalence was higher in our study (35.5%) than in the previous one (25.4%). This could be due to the higher age range of our study population compared to the previous study, (median age 53 vs 41 years, respectively) and longer average experience as Alpine guides (mean 22 vs 17 years, respectively).
Despite the high prevalence of NMSC and AK found in our study, only a little over half the mountain and ski guides (51.6%) had consulted a dermatologist in their life prior to the study. This finding alone confirms not only the immediate need for information and awareness campaigns concerning NMSC, but also the need to address issues specific to mountain and ski guides, as well as those with other outdoor professions and alpine hobbies. It also questions the currently available data, which are solely based on information provided by insurance companies [7, 17]. Owing to the low rate of visits to dermatologists, insurance companies do not have any archived data on the skin health of mountain guides. This raises the question of whether NMSC is underestimated in non-referred individuals with outdoor professions; recent hospital-based studies have shown an increased NMSC risk for outdoor professions [18]. It is a great advance for outdoor-working groups that NMSC has been officially recognised as an occupational disease in some European countries. However, the next step towards developing evidence-based protective behaviour recommendations for the prevention of NMSC, in addition to educational programmes for doctors [19], seems overdue and should be addressed in further studies. Moreover, the majority of the study population (83.6%) called for more information about UV radiation, NMSC and possible prevention tools.
This study has some limitations. A recall bias owing to the lack of randomisation of participants has to be considered. It is likely that this study attracted guides especially concerned about their health or those who recently noticed abnormal skin findings, thus leading to an overestimation of NMSC prevalence and associated protective behaviour in mountain and ski guides. However, the fact that mountain and ski guides are at a high risk for NMSC should not only be considered by all dermatologists worldwide in their daily clinical routine, but also by alpine guide associations in order to promote adequate preventive and screening measures for their members. With the high interest shown by mountain and ski guides in learning more about NMSC and associated risk factors, as well as the high rate of participation in this limited study, further studies combining primary and secondary prevention campaigns targeted toward this outdoor profession are needed. The development and implementation of specialised NMSC prevention campaigns for Alpine guides, and continuous evaluation, adaptations and improvements to these campaigns could be used to establish a general prevention model. This knowledge could then be transferred to other potential high NMSC risk groups, especially other outdoor workers, in order to lower the worldwide burden of NMSC.
Acknowledgments: We are indebted to all the mountain guides who participated in the study and completed the questionnaire.
1 Reinau D, Meier C, Gerber N, Hofbauer GF, Surber C. Sun protective behaviour of primary and secondary school students in North-Western Switzerland. Swiss Med Wkly. 2012;142:w13520.
2 Lomas A, Leonardi-Bee J, Bath-Hextall F. A systematic review of worldwide incidence of nonmelanoma skin cancer. Br J Dermatol. 2012;166(5):1069–80. doi:http://dx.doi.org/10.1111/j.1365-2133.2012.10830.x.
3 Glogau RG. The risk of progression to invasive disease. J Am Acad Dermatol. 2000;42(1 Pt 2):S23–4. doi:http://dx.doi.org/10.1067/mjd.2000.103339.
4 Stockfleth E, Terhorst D, Hauschild A, Zouboulis CC, Schlaeger M, Oster-Schmidt C, et al. Aktinische Keratosen. [Actinic keratoses]. J Dtsch Dermatol Ges. 2012;10(Suppl 7):S1–23. doi:http://dx.doi.org/10.1111/j.1610-0379.2012.08019.x. German.
5 Gordon LG, Rowell D. Health system costs of skin cancer and cost-effectiveness of skin cancer prevention and screening: a systematic review. Eur J Cancer Prev. 2015;24(2):141–9. doi:http://dx.doi.org/10.1097/CEJ.0000000000000056.
6 Schaefer I, Augustin M, Spehr C, Reusch M, Kornek T. Prevalence and risk factors of actinic keratoses in Germany – analysis of multisource data. J Eur Acad Dermatol Venereol. 2014;28(3):309–13.
7 World Health Organization, World Meteorological Organization, United Nations Environment Programme and International Commission on Non-Ionizing Radiation Protection. Global solar UV index. A practical guide. 2002. Available at http://www.who.int/uv/publications/en/GlobalUVI.pdf?ua=1 (accessed 26 Jul 2016)
8 Mahé E, Corrêa MP, Godin-Beekmann S, Haeffelin M, Jégou F, Saiag P, et al. Evaluation of tourists’ UV exposure in Paris. J Eur Acad Dermatol Venereol. 2013;27(3):e294–304. doi:http://dx.doi.org/10.1111/j.1468-3083.2012.04637.x
9 Zink A, Ring J. Images in clinical medicine. Phototoxic dermatitis. N Engl J Med. 2014;371(6):559. doi:http://dx.doi.org/10.1056/NEJMicm1315566
10 Moehrle M, Dennenmoser B, Garbe C. Continuous long-term monitoring of UV radiation in professional mountain guides reveals extremely high exposure. Int J Cancer. 2003;103(6):775–8. doi:http://dx.doi.org/10.1002/ijc.10884
11 Schwartz RA, Bridges TM, Butani AK, Ehrlich A. Actinic keratosis: an occupational and environmental disorder. J Eur Acad Dermatol Venereol. 2008;22(5):606–15. doi:http://dx.doi.org/10.1111/j.1468-3083.2008.02579.x
12 Lichte V, Dennenmoser B, Dietz K, Häfner HM, Schlagenhauff B, Garbe C, et al. Professional risk for skin cancer development in male mountain guides – a cross-sectional study. J Eur Acad Dermatol Venereol. 2010;24(7):797–804. doi:http://dx.doi.org/10.1111/j.1468-3083.2009.03528.x
13 John SM, Trakatelli M, Gehring R, Finlay K, Fionda C, Wittlich M, et al. CONSENSUS REPORT: Recognizing non-melanoma skin cancer, including actinic keratosis, as an occupational disease – A Call to Action. J Eur Acad Dermatol Venereol. 2016;30(Suppl 3):38–45. doi:http://dx.doi.org/10.1111/jdv.13608
14 Christoph S, Cazzaniga S, Hunger RE, Naldi L, Borradori L, Oberholzer PA. Ultraviolet radiation protection and skin cancer awareness in recreational athletes: a survey among participants in a running event. Swiss Med Wkly. 2016;146:w14297
15 Bauer A, Beissert S, Knuschke P. Prävention von durch berufliche solare UV-Exposition bedingtem epithelialem Hautkrebs [Prevention of occupational solar UV radiation-induced epithelial skin cancer]. Hautarzt. 2015;66(3):173–8. doi:http://dx.doi.org/10.1007/s00105-015-3584-2. German
16 Tan S, Sinclair C, Foley P. Running behind a tourist: leisure-related skin cancer prophylaxis. Br J Dermatol. 2012;167(Suppl 2):70–5. doi:http://dx.doi.org/10.1111/j.1365-2133.2012.11089.x
17 Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015;151(10):1081–6. doi:http://dx.doi.org/10.1001/jamadermatol.2015.1187
18 Trakatelli M, Barkitzi K, Apap C, Majewski S, De Vries E; EPIDERM group. Skin cancer risk in outdoor workers: a European multicenter case-control study. J Eur Acad Dermatol Venereol. 2016;30(Suppl 3):5–11. doi:http://dx.doi.org/10.1111/jdv.13603
19 Badertscher N, Braun RP, Held U, Kofmehl R, Senn O, Hofbauer GF, et al. Diagnostic competence of Swiss general practitioners in skin cancer. Swiss Med Wkly. 2013;143:w13834
Disclosure statement: The study was supported by a research grant from Galderma Germany. Alexander Zink, Elisabeth Koch, Florian Seifert, Markus Rotter, Christoph Spinner, and Tilo Biedermann have no conflicts of interest to declare.