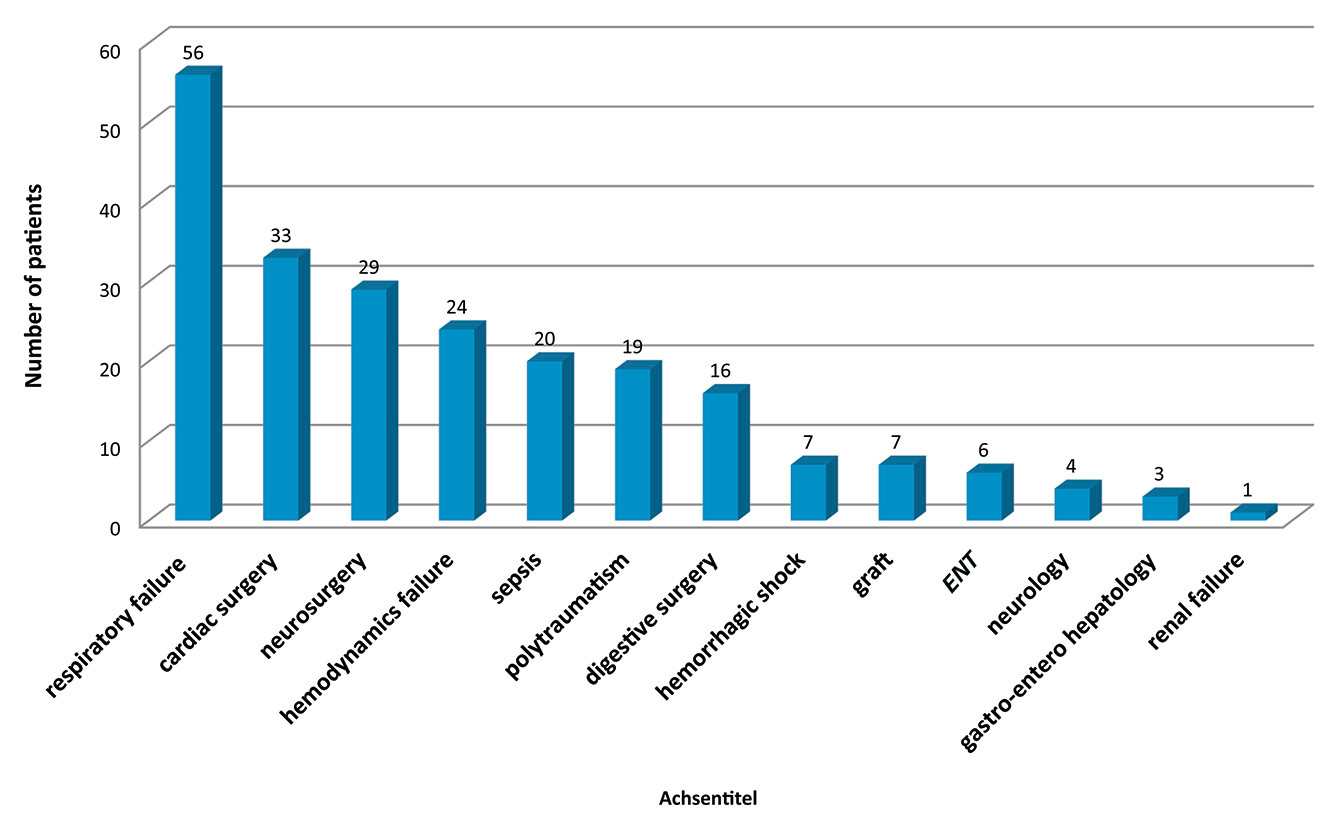
Figure 1
Diseases that commonly led to prolonged ICU stays in 2015.
ENT = ear nose throat
DOI: https://doi.org/10.4414/smw.2016.14336
Advances in intensive care medicine allow patients to survive serious health insults. However, their survival involves a cost for the patients who themselves suffer, their family members and society [1]. Indeed, many such patients require a prolonged stay in the intensive care unit (ICU) because of difficult weaning or repeated sepsis and represent an increasing new population of ICU patients called “the chronic critically ill” or “Patients Long Séjour (PLS)” in French meaning “Prolonged Length of Stay patient”. Chronic critical illness is a devastating condition in which mortality exceeds that of most malignancies, and for most survivors functional dependence persists [2–4], consisting of physical impairments, pain and significant psychosocial disorders [5, 6]. This article addresses the specific care aiming to improve the outcome of PLS.
A few ICU caregivers realised in 2006 that such patients needed to be managed differently from patients in the acute phase [7]. An interdisciplinary team composed of physicians, nurses, nurse assistants, physiotherapists and teachers, developed a new approach for PLS care. The group sought their particular requirements, innovated new specific monitoring tools and continues to develop therapeutic approaches adapted to their special needs. In parallel, it created a network in close cooperation with other specialists, i.e. orthopaedists, dieticians, neuropsychologists and a speech therapist, in order to extend their knowledge and adapt the therapies during the prolonged stay of PLSs in the ICU. This approach includes a palliative attitude, in accordance with the Swiss Academy of Medical Sciences [8], which needs to be adopted very early for each patient admitted into the ICU whatever his/her risk of dying. Indeed, the suffering of these patients should be duly cared for [9].
This article presents the multimodal approach developed up to the present in order to optimise the care of PLSs and aiming eventually to improve their future quality of life.
The definition of the “chronically critically ill patient” was coined by Girard and Raffin in 1985 in an article describing a set of patients who remained dependent on vital support treatments after an acute critical disease that required admission to the ICU [10]. In Geneva, patients who should benefit from specific PLS care were defined as those with a length of stay in the ICU of ≥7 days [11]. The second criterion for categorising a patient as a PLS was the necessity for support by sophisticated means available only in the ICU (the hallmark of chronic critical illness is respiratory failure requiring prolonged dependence on mechanical ventilation) (fig. 1). Patients in palliative care or nearing the end of life were excluded.
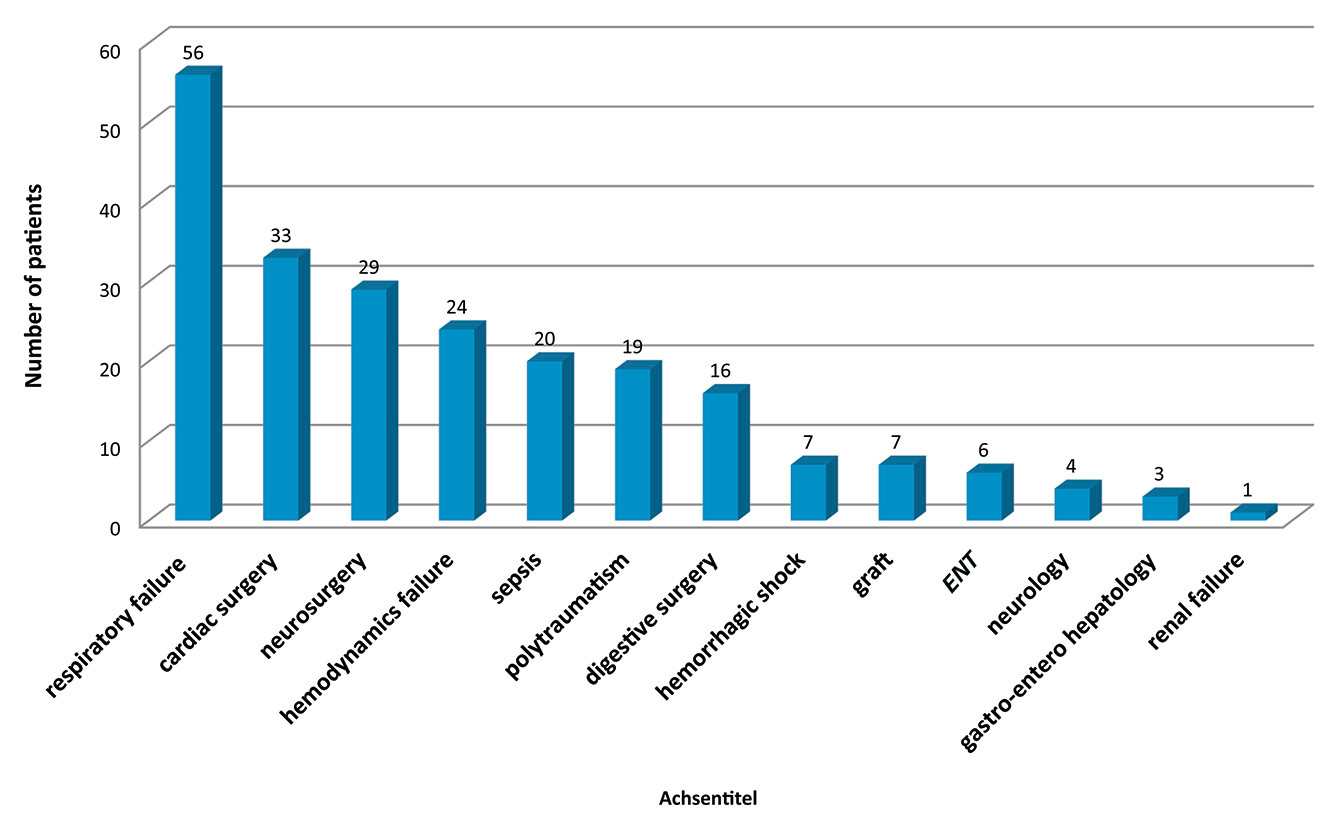
Figure 1
Diseases that commonly led to prolonged ICU stays in 2015.
ENT = ear nose throat
The former account for about 12 to 18% of the 2 500 patients admitted to the Geneva ICU each year, stay as long as 13.8 days (all patients: 3.8 days) and consume up to 52% of the ICU resources. They are not older than the ICU general population (60 ± 19 years). Their mortality in the ICU was assessed to be around 15% compared with 8–12% of the general ICU population. Nevertheless, since more than a third of PLSs eventually return home, the ICU caregivers should acknowledge the existence of this group and pay special attention to their care.
Their specific problems are summarised in table 1. Their symptoms differ from those of patients in the acute phase, will continue far beyond the ICU and may even impact their future life.
These patients require from caregivers not only expertise in the advanced technology of intensive medicine, but also extraordinary skill in human relationships. Their complex situations and the long stay in the special environment of intensive care can be a source of conflict amongst family members, amongst caregivers and between family members and caregivers, as was shown in the study from Studdert [12]. Nearly one-third of all ICU patients with prolonged stays experienced at least one conflict associated with life-sustaining treatment, disagreements about the plan of care, or poor communication. Also, conflicts are associated with burnout of caregivers, which in turn can be associated with conflicts with nurses, colleagues or patients’ families [13].
An attempt to pool these patients in a sector of the ICU in Geneva between 2006 and 2009 resulted in exhaustion of the team members, who expressed their unwillingness to take care of these patients [14]. In the beginning, the aim was to cohort the PLS to understand their specific needs and ensure their comfort including sleep, family visits and family needs in a confined area. The second goal was to acquire techniques and skills in this domain for future patients. The main reasons for the failure of the grouping of such patients included the burden of care, the difficult relationships with the family members as mentioned above, and the moral distress of caregivers regarding the meaning of care, as well as the uncertain prognoses and the slow evolution of PLS [15]. The PLS were then re-distributed throughout the entire service in 2009. However, this experience confirmed that the care of these patients could not be similar to that of acutely ill patients. In order to ensure the continuity of PLS care; a referent nurse should be designated on a long-term basis. Kept out of the day/night shifts, he/she is a resource person for the patient and family members, and ensures the training of the healthcare team in PLS-specific management.
The years of expertise taught us the specific needs for the care of PLSs: multidisciplinary management, recovery of physical and psychological independence, early rehabilitation, sleep, relationships with family members, planning for the future, and the spiritual dimension [16].
| Table 1:Specific problems of prolonged-stay patients in the intensive care unit (ICU), derived from Nelson et al. [3]. | |
| Problems | Causes and symptoms |
| Ventilator dependence | Ventilator-associated pneumonia Reduction of immune defences Multiresistant bacteria Neuromuscular weakness, ICU paresis Swallowing problems |
| Brain dysfunction Cognitive impairments | Neurological lesions Sepsis Sedation Day/night cycle dysregulation |
| Neuromuscular weakness | ICU paresis (myopathy, neuropathy) Immobilisation Muscle loss and increased adipose tissue |
| Endocrine disorders | Hormonal dysregulation - thyroid hormone - corticosteroid - antidiuretic hormone - catabolism / anabolism |
| Malnutrition | Nutritional deficiency Catabolism Disorders of the digestive system |
| Anasarca | Capillary leak Hormonal dysregulation Fluid intake/output imbalance |
| Skin breakdown | Bed rest, immobilisation Malnutrition Oedema Incontinence Medication (vasopressors) |
| Symptom distress | Pain Thirst Dyspnoea Anxiety, depression Difficulty with communication |
On the seventh day of hospitalisation of the patient, a predefined professional (the ICU receptionist in our context) sticks a PLS signalling system and algorithm of care on the bedside monitor. This procedure reminds the caregivers to start the specific provision of care as defined in a checklist that lists the potential problems to discuss during the medical rounds. Furthermore, a PLS guideline is available on the ICU website.
Muscle tone is assessed weekly by physiotherapists using the Medical Research Council scale [17]. Since skeletal muscle mass diminishes by 2 to 4% per day during critical illness and immobilisation, any measure to prevent its loss is important. Early activity is feasible even in ICU patients [18] and is a promising therapy to prevent or treat the neuromuscular complications of critical illness, although not enough data are available yet [19]. Since physical recovery is a major concern after an ICU stay, such an approach may improve the patient’s quality of life after discharge [20].
A weekly consultation with a specialist in rehabilitation helps the physiotherapists select the types of authorised treatments adapted to the patient.
Under- or overfeeding of critical patients is associated with an increase in complications, costs and mortality [21]. Insufficient caloric intake decreases the chances of returning home [22]. PLSs need systematic monitoring of nutrition by a dietician, who determines their energy expenditure and helps adjust their intake.
Swallowing difficulty is common, especially after prolonged endotracheal intubation, and is underdiagnosed. There is a major threat of inhalation pneumonia in these patients. Although there is no evidence, small calibre enteral feeding tubes are to be preferred as soon as possible. A speech therapist helps by introducing rehabilitation treatment whenever possible. Future research should investigate the best way to avoid such ICU complications.
After ICU and hospital discharge, many PLSs experience neurocognitive disorders and long-term impairment [23, 24]. Therefore, neurocognitive assessment should be an integral part of care: as soon as patients are conscious (Glasgow coma scale above 12), they are assessed weekly with a modified Mini Mental State Examination (MMSE). This tool has been developed by our team to be applicable to intubated patients, with the collaboration of a neuropsychiatrist, and has been validated [25]. The MMSE is used to anticipate, detect and monitor potential neurocognitive disorders. Early neurorehabilitative measures may be developed in the near future.
To decrease patient disorientation, a visual calendar and a visual daily activity schedule are placed on the bedside (fig. 2). This enables the patients to be informed and involved in the process of care.
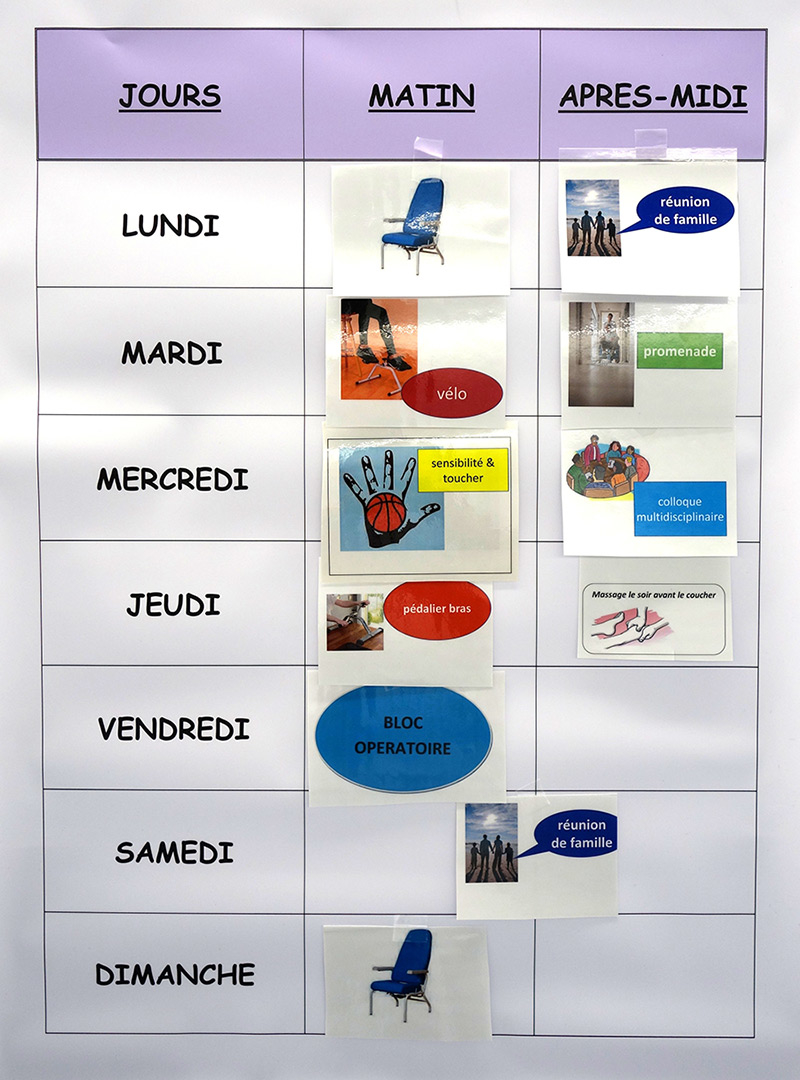
Figure 2
Poster showing the weekly schedule on the bedside of a PLS.
Jours = days; matin = morning; après-midi = afternoon; lundi = Monday; mardi = Tuesday; mecredi; Wednesday; jeudi = Thursday; vendredi = Friday; samedi = Saturday; dimanche = Sunday
Hospitalisation in the ICU can induce psychological distress in patients [26]. Memories of the stay may be absent or fragmented. Many patients report delusional memories of people who tried to hurt or kill them, as well as dreams, nightmares and hallucinations. Between 14 and 41% of patients will develop symptoms of post-traumatic stress disorder (PTSD).
A diary can help reconstruct the ICU experience and has been shown to prevent PTSD [27]. The patient’s relatives and caregivers write the ICU events in a notebook to allow the patient to recapture his/her history. It is given to the patient or their relatives upon ICU discharge.
After a prolonged stay in the ICU, the objectives of care sometimes become unclear or disparate for the team. It is mandatory to hold a multidisciplinary conference where the referent nurse, the physician, the nurse in charge of the patient, as well as the external caregivers (speech therapist, surgeons, consulting physicians, physiotherapists, etc.) meet to discuss the management of the PLS. The purpose of such a conference is to redefine the short-, medium- and long-term therapeutic objectives. It aims to ensure consistent care. The conference should then be summarised in the patient’s medical and nursing charts. The therapeutic project is also communicated to the relatives. Communication with family members is no different from other aspects of critical care and requires training, interdisciplinary teamwork, and implementation of effective and flexible protocols to achieve the best possible outcome [28].
PLSs become very dependent and require heavy nurse assistance. In the ICU, the nurse/patient ratio is 1/1–2. Moreover, a close relationship often binds the PLS to caregivers. The patients experience a real loss when discharged to the ward. Preparation is thus essential. The transfer of patients from the ICU to a medical unit can be a very challenging process [29].
Once the decision to transfer the patient is made, the ICU team organises an interview with the next caregiver team. Whenever possible, the patient is invited to visit the new department. This procedure provides the first human contact and serves to reduce patient apprehension. The focus is then applied to communication of the situation and ongoing problems (ventilator weaning, pain control, cognitive monitoring, motor rehabilitation, nutrition, social-family environment, sleep, etc.).
The PLS initiatives described are the result of 10 years of reflection, experience and research. The multidisciplinary group started a management framework, helped to develop the skills required for these patients and created new tools for their care. Because of the multimodal character of this experience, we have yet to demonstrate scientifically the benefit of such management. However, the project seems to make sense and future research may demonstrate the benefit of such an enterprise. Readmissions have already decreased and between 2014 and 2015 many former PLSs spontaneously gave updates to the team, and came back to meet their caregivers and to see the environment. Since these PLSs present problems that extend far beyond the duration of their stay in the ICU, the group wishes to offer a post-ICU consultation. This would allow us to gain knowledge about the patients’ outcome, and enhance the partnerships with the hospital caregivers post-ICU and possibly with general practitioners outside the hospital [30].
We are presently training the ICU team in massage techniques to decrease the anxiety and pain of patients, as well as to improve their sleep quality. The group aims to analyse the causes of poor sleep quality and propose strategies. This is the subject of our next research project in the Geneva ICU.
Acknowledgements: The PLS group is grateful to Maximilian Schindler, our orthopaedist who gave us valuable advice on the mobilisation programme for PLS; to Severine Graaf, our dietician who led nutrition management, and Françoise Esteve, our speech therapist whose teaching on swallowing difficulty were of great importance. The authors thank Mrs Radhika Sood for her thorough English editing.
1 Stricker K, Rothen HU, Takala J. Resource use in the ICU: short- vs. long-term patients. Acta Anaesthesiol Scand. 2003;47(5):508–15.
2 Zilberberg MD, Luippold RS, Sulsky S, Shorr AF. Prolonged acute mechanical ventilation, hospital resource utilization, and mortality in the United States. Crit Care Med. 2008;36(3):724–30.
3 Nelson JE, Cox CE, Hope AA, Carson SS. Chronic critical illness. Am J Respir Crit Care Med. 2010;182(4):446–54.
4 Friedrich JO, Wilson G, Chant C. Long-term outcomes and clinical predictors of hospital mortality in very long stay intensive care unit patients: a cohort study. Crit Care. 2006;10(2):R59.
5 Granja C, Lopes A, Moreira S, Dias C, Costa-Pereira A, Carneiro A. Patients’ recollections of experiences in the intensive care unit may affect their quality of life. Crit Care. 2005;9(2):R96–109.
6 Jackson JC, Mitchell N, Hopkins RO. Cognitive functioning, mental health, and quality of life in ICU survivors: an overview. Psychiatr Clin North Am. 2015;38(1):91–104.
7 Roulin MJ, Spirig R. Developing a care program to better know the chronically critically ill. Intensive Crit Care Nurs. 2006;22(6):355–61.
8 Swiss Academy of Medical Sciences. Medical-ethical guidelines and recommendations: Palliative Care (2006, updated 2012).
9 Puntillo K, Nelson JE, Weissman D, Curtis R, Weiss S, Frontera J, et al. Palliative care in the ICU: relief of pain, dyspnea, and thirst – a report from the IPAL-ICU Advisory Board. Intensive Care Med. 2014;40(2):235–48.
10 Girard K, Raffin TA. The chronically critically ill: to save or let die? Respir Care. 1985;30(5):339–47.
11 Weissman C. Analyzing the impact of long-term patients on ICU bed utilization. Intensive Care Med. 2000;26(9):1319–25.
12 Studdert DM, Mello MM, Burns JP, Puopolo AL, Galper BZ, Truog RD, et al. Conflict in the care of patients with prolonged stay in the ICU: types, sources, and predictors. Intensive Care Med. 2003;29(9):1489–97.
13 Embriaco N, Azoulay E, Barrau K, Kentish N, Pochard F, Loundou A, et al. High level of burnout in intensivists: prevalence and associated factors. Am J Respir Crit Care Med. 2007;175(7):686–92.
14 Roulin MJ, Boul’ch MF, Merlani P. Staff satisfaction between 2 models of care for the chronically critically ill. J Crit Care. 2012;27(4):426 e421–428.
15 Piers RD, Azoulay E, Ricou B, Dekeyser Ganz F, Decruyenaere J, Max A, et al. Perceptions of appropriateness of care among European and Israeli intensive care unit nurses and physicians. JAMA. 2011;306(24):2694–703.
16 Aitken LM, Marshall AP. Monitoring and optimising outcomes of survivors of critical illness. Intensive Crit Care Nurs. 2015;31(1):1–9.
17 De Jonghe B, Bastuji-Garin S, Sharshar T, Outin H, Brochard L. Does ICU-acquired paresis lengthen weaning from mechanical ventilation? Intensive Care Med. 2004;30(6):1117–21.
18 Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdjian L, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35(1):139–45.
19 Connolly B, Salisbury L, O’Neill B, Geneen L, Douiri A, Grocott MP, et al. Exercise rehabilitation following intensive care unit discharge for recovery from critical illness. Cochrane Database Syst Rev 2015, 6:CD008632.
20 Aitken LM, Burmeister E, McKinley S, Alison J, King M, Leslie G, et al. Physical recovery in intensive care unit survivors: a cohort analysis. Am J Crit Care. 2015;24(1):33–39; quiz 40.
21 Barr J, Hecht M, Flavin KE, Khorana A, Gould MK. Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest. 2004;125(4):1446–57.
22 Yeh DD, Fuentes E, Quraishi SA, Cropano C, Kaafarani H, Lee J, et al. Adequate Nutrition May Get You Home: Effect of Caloric/Protein Deficits on the Discharge Destination of Critically Ill Surgical Patients. JPEN J Parenter Enteral Nutr 2015.
23 Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16.
24 Hopkins RO, Brett S. Chronic neurocognitive effects of critical illness. Curr Opin Crit Care. 2005;11(4):369–75.
25 Miguelez M, Merlani P, Gigon F, Verdon M, Annoni JM, Ricou B. Feasibility of a multiple-choice mini mental state examination for chronically critically ill patients. Crit Care Med. 2014;42(8):1874–81.
26 Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369–379.
27 Jones C, Backman C, Griffiths RD. Intensive care diaries and relatives’ symptoms of posttraumatic stress disorder after critical illness: a pilot study. Am J Crit Care. 2012;21(3):172–6.
28 Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest. 2008;134(4):835–43.
29 St-Louis L, Brault D. A clinical nurse specialist intervention to facilitate safe transfer from ICU. Clin Nurse Spec. 2011;25(6):321–6.
30 Walsh TS, Salisbury LG, Merriweather JL, Boyd JA, Griffith DM, Huby G, et al. Increased Hospital-Based Physical Rehabilitation and Information Provision After Intensive Care Unit Discharge: The RECOVER Randomized Clinical Trial. JAMA Intern Med. 2015;175(6):901–10.
Disclosure statement: No financial support and no other potential conflict of interest relevant to this article was reported.