Reimbursement of care for severe trauma under SwissDRG
DOI: https://doi.org/10.4414/smw.2016.14334
Rudolf M
Moos, Kai
Sprengel, Kai Oliver
Jensen, Thorsten
Jentzsch, Hans-Peter
Simmen, Burkhardt
Seifert, Bernhard
Ciritsis, Valentin
Neuhaus, Jörk
Volbracht, Tarun
Mehra
Summary
QUESTIONS: Treatment of patients with severe injuries is costly, with best results achieved in specialised care centres. However, diagnosis-related group (DRG)-based prospective payment systems have difficulties in depicting treatment costs for specialised care. We analysed reimbursement of care for severe trauma in the first 3 years after the introduction of the Swiss DRG reimbursement system (2012–2014).
MATERIAL/METHODS: The study included all patients with solely basic insurance, hospital admission after 01.01.2011 and discharge in 2011 or 2012, who were admitted to the resuscitation room of the University Hospital of Zurich, aged ≥16 years and with an injury severity score (ISS) ≥16 (n = 364). Clinical, financial and administrative data were extracted from the electronic medical records. All cases were grouped into DRGs according to different SwissDRG versions. We considered results to be significant if p ≤0.002.
RESULTS: The mean deficit decreased from 12 065 CHF under SwissDRG 1.0 (2012) to 2 902 CHF under SwissDRG 3.0 (2014). The main reason for the reduction of average deficits was a refinement of the DRG algorithm with a regrouping of 23 cases with an ISS ≥16 from MDC 01 to DRGs within MDC21A. Predictors of an increased total loss per case could be identified: for example, high total number of surgical interventions, surgeries on multiple anatomical regions or operations on the pelvis (p ≤0.002). Psychiatric diagnoses in general were also significant predictors of deficit per case (p<0.001).
CONCLUSION: The reimbursement for care of severely injured patients needs further improvement. Cost neutral treatment was not possible under the first three versions of SwissDRG.
Abbreviations
CHOP Swiss classification of operations (surgical interventions)
DRG diagnosis-related group
ICD international classification of diseases
ICU intensive care unit
ISS injury severity score
LOS length of stay
MDC major diagnostic category
NEMS nine equivalents of nursing manpower use score
SD standard deviation
Introduction
Background
Increasing international evidence points towards improved outcomes for treatment of severe injuries in specialised trauma centres, justifying efforts for regionalisation of care [1–6]. However, treatment in specialised centres is costly [7]. In 2012, Switzerland switched reimbursement for inpatient care from mostly day rates to a prospective payment system based on German diagnosis-related groups (DRGs) [8]. Nonetheless, with a population of approximately 8 million and an estimated incidence of severe trauma ranging from 25 to 52 per 100 000 [9, 10], the statistical population with which the DRGs are calculated in Switzerland is small. The accurate calculation of reimbursement rates for cases less frequently encountered poses a challenge, such as in the case of trauma or burn patients [11–13]. Especially patients with multiple injuries are often discussed as being underfinanced [7, 14–18]. Some previous investigations even suggest that cost-neutral treatment of severely injured patients might not be realistic under a DRG-based prospective payment system [14, 19]. Since costs are positively correlated with length of stay it has been suggested that various problems regarding cost coverage are caused by high outliers [20]. In most of the studies, earnings were analysed without knowledge of individual treatment costs per case and if they were known, the treatment costs were often estimates based on general assumptions instead of calculated individual costs [14, 21–25]. For our study we were able to provide the individual full-absorption costs for every single case from our hospital unit accounts. Therefore, we were able to calculate the financial result for every single case, providing the possibility to analyse the revenue structure and the DRG-selection within our study group under the first three catalogue versions of SwissDRG, which were valid for the three consecutive years 2012, 2013 and 2014, by calculating the simulated DRG-revenues for all cases under the corresponding SwissDRG versions 1.0, 2.0 and 3.0. Thus, we were able to focus on the refinement of the reimbursement system within the first 3 years after its introduction, assuming that severity of injuries, treatments and costs stayed the same throughout the years.
DRG and Switzerland
DRG systems categorise hospital cases into clusters which, in terms of resource utilisation and treatment costs, are expected to be similar [13]. Originally developed to allow hospital output measurements [26], DRGs are currently used to determine the revenues for inpatient treatments in many countries around the globe [27, 28]. Technically, the revenue for a certain case is determined by the DRG and its related case mix points multiplied by the base rate of the hospital, as long as the length of stay (LOS) is within the low and high margins of the ascertained DRG (inlier definition). Therefore, for most DRGs a low and a high trim point is defined. If the actual LOS is below the low trim point the case is defined as a low outlier and the case mix points for inliers are reduced by a constant rate for every day below the low trim point. If LOS exceeds the high trim point, the case is accordingly defined as a high outlier and the hospital receives additional money for every day the LOS exceeds the defined high trim point of the DRG. Therefore the revenues within a DRG system are fixed only for inliers within these limits. The revenue for a typical DRG according to LOS can be obtained from the appendix (supplementary figure S1). Since the margins for low and high outliers are variable throughout the catalogue versions this can affect the average revenues significantly. Therefore, the quality of DRG depiction and the impact of LOS on revenues were investigated separately when analysing the catalogue effects within this study. In addition, certain procedures or medications make cases eligible for supplementary payments on top of the revenues described so far, so supplementary payments were investigated too.
Material and methods
Ethics
Institutional review board approval was obtained from the Ethics Committee of the Canton Zurich prior to the start of the study (KEK-ZH-Nr. 2014-0231). All patient-based data from our centre were anonymised before the analysis.
Inclusion criteria
All patients with solely basic insurance, hospital admission after 1 January 2011 and discharge in 2011 or 2012, who were admitted to the resuscitation room of the University Hospital of Zurich, aged 16 years and older with an injury severity score (ISS) greater or equal to 16 were included in this study. With an ISS greater or equal to 16 we followed the definition of severely injured patients of the German Society for Trauma Surgery [29]. Three cases with hospital admission before 1 January 2011 and discharge in 2012 or later had to be excluded because cost data could not be obtained completely owing to the structure of our database.
Analysed data
The discharges in 2011 and 2012 were classified with different SwissDRG groupers. The following grouper versions have been used: batch grouper v1.0 planning version, v2.0 planning version 1 and v3.0 catalogue version for cases discharged in 2011; batch grouper v1.0 billing version, v2.0 planning version 2 and v3.0 planning version 1 for cases discharged in 2012. A base rate of 11 300 CHF per case-mix point was assumed. The supplementary payments (“Zusatzentgelte”) under SwissDRG versions 1.0 and 2.0, as well as the supplementary payments for blood products under SwissDRG version 3.0, were taken into account.
Data recorded for the trauma register for the “Deutsche Gesellschaft für Unfallchirurgie” (DGU: Germany Society for Emergency Surgery), administrative data as well as the coded diagnoses and procedures were analysed. The diagnoses were encoded according to the international classification of diseases (ICD) version ICD-10 GM 2010, the procedures according to the Swiss classification of operations (CHOP) catalogues 2011 and 2012.
The cost data were obtained from the internal REKOLE®-based full-absorption cost-unit accounts [30]. The data are based on the PRISMA formatted data set, as specified by the Canton of Zurich [31].
Statistics
Diagnostic data were organised into clusters (see appendix, supplementary tables S1a and S1b) and binomially coded for further statistical analysis (1 = yes, 0 = no). Association of net profit per case (total DRG revenue per case calculated as the sum of case mix points times base rate plus supplementary payments minus total case costs) with nominal variables was determined with the Mann-Whitney-test. For continuous variables, Spearman’s rank correlation with net per case profit was determined.
Statistical analysis was performed using IBM SPSS Statistics, version 22 (IBM Corp., Armonk, NY, USA). Assuming a general significance level of α = 0.05, we considered results to be significant for p ≤0.002 after Bonferroni correction, to maintain the probability of false significances due to multiple testing of 24 variables (supplementary table S2).
Results
Descriptive statistics of the study population
Data of 364 patients were evaluated in this study. Population characteristics such as age, length of stay (LOS), LOS in intensive care units (ICUs) and others can be obtained from table 1. The overall in-house mortality was 25.8% (3.8% unsuccessful reanimation in resuscitation room, 8.5% after restricted comfort therapy owing to declared intention, 13.5% albeit standard care). The mean ISS was 34.2 points with a median of 27 points, and a range from 16 to 75 points. The mean abbreviated injury score per body region can be obtained from table 2.
Revenue structure
The mean revenue of all cases under SwissDRG 1.0 (case mix points x base rate / number of cases) amounted to 57 058 CHF including supplementary payments, the average case cost amounted to 69 123 CHF (standard deviation [SD] 86 537 CHF), leading to a theoretical average loss of 12 065 CHF (SD 43 019 CHF) per case under SwissDRG 1.0, which amounted to a total loss of approximately 4.4 million CHF (table 3). So if all cases included in our study were discharged in 2012 (SwissDRG Version 1.0), this would have been the real financial loss for our institution caused by the treatment of the severely injured patients included in this study. In order to assess the financial results for the following SwissDRG versions 2.0 and 3.0 (valid for discharges in 2013 and 2014, respectively) we calculated the corresponding catalogue effects.
Catalogue effects
Catalogue effects affect revenues through changes to DRG definitions, grouper algorithms and modifications in the case-mix points of the SwissDRG catalogue versions from one year to the next. They are normally expressed as percentage change of case-mix index from one year to the next. To analyse this effect, we grouped all cases included in our study with the corresponding SwissDRG batch grouper. The ascertained case-mix points were multiplied by the same base rate of 11 300 CHF to determine the theoretical revenue under the current SwissDRG catalogue versions between 2012 and 2014.
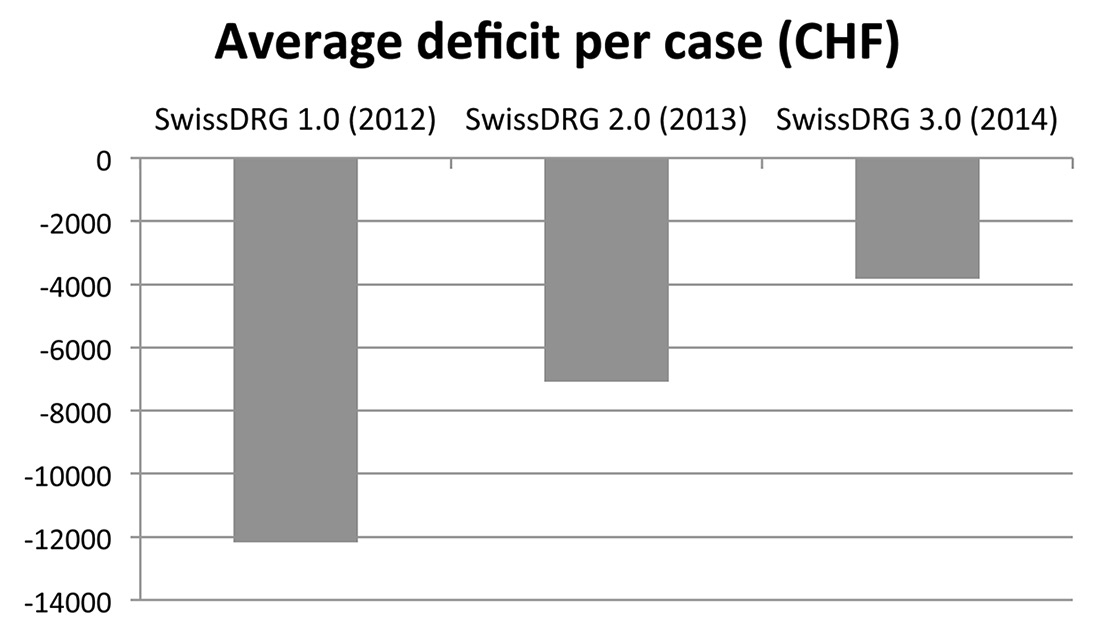
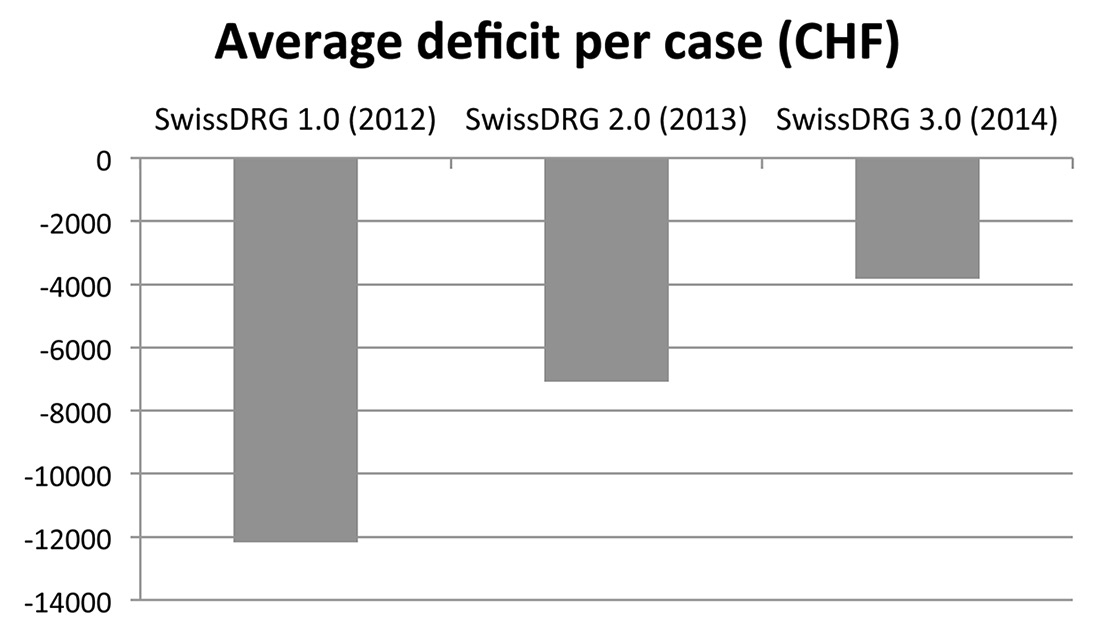
Figure 1
Average deficit under different SwissDRG catalogue versions. Average deficits were calculated as the mean of diagnosis-related group (DRG) revenue minus total costs per case. DRG revenue was determined by multiplying the effective case-mix points of the case’s DRGs as defined by the different catalogue versions (V1.0, 2014; V2.0, 2013; V3.0, 2014) by a base rate of 11 300 CHF. Supplementary payments (“Zusatzentgelte”) were taken into account.
As depicted in figure 1, the evolution of the reimbursement of severely injured patients showed a positive trend, the simulated loss per case reduced. However, even under SwissDRG version 3.0 (2014), a cost-neutral treatment of severely injured patients was not achievable (table 4). Interestingly, the positive catalogue effects were solely due to regrouping of cases to other DRGs (increase of 188.290 case-mix points from SwissDRG version 1.0 to 2.0), whereas the case-mix points of those cases that were not grouped into a different DRG declined by 24.372 case-mix points. Similar observations were made between version 2.0 and 3.0, although the amount of DRG regroupings was strikingly less between 2.0 and 3.0 in comparison with 1.0 and 2.0 (68 to 105 regroupings).
The average per-case deficit substantially dropped from 12 065 CHF under SwissDRG catalogue 1.0 to 2902 CHF under catalogue version 3.0 (table 3).
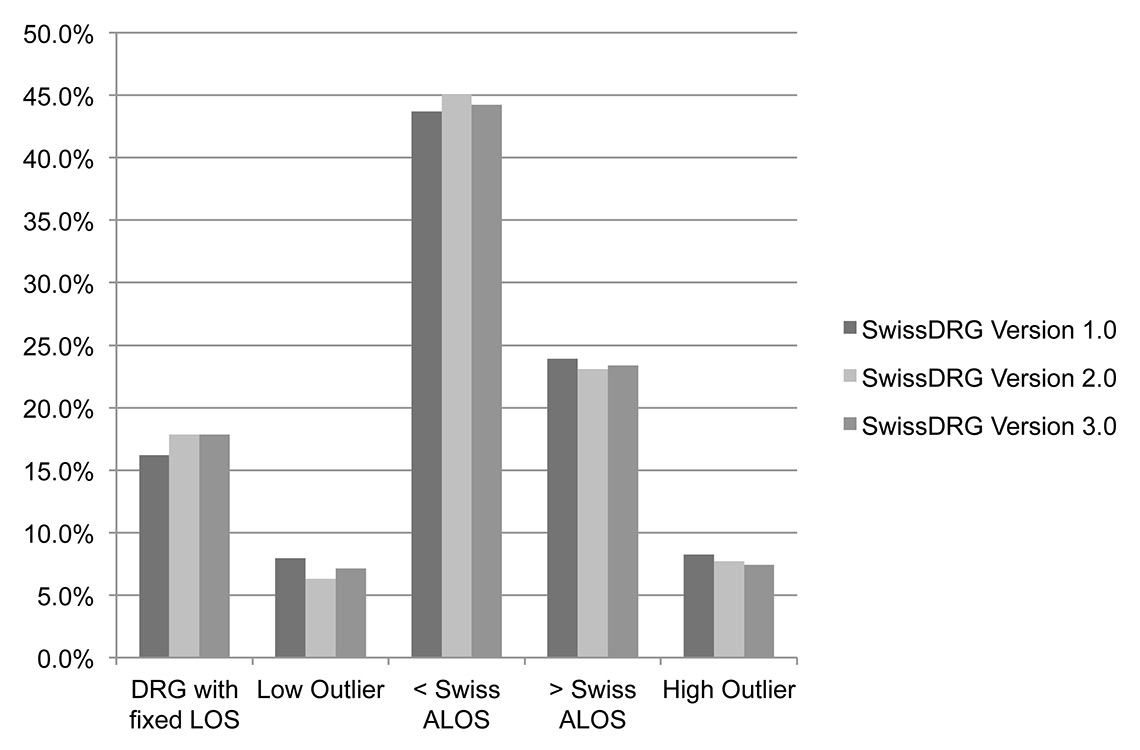
Since for DRG outliers LOS is driving the revenue side of the DRG system also, we analysed the percentage of low and high outliers in our study group under the three consecutive DRG versions, as well as the evolution of total case-mix point reductions and supplements due to changing thresholds for outliers. As figure 2 clearly demonstrates, the proportion of low and high outliers was comparably stable for all investigated SwissDRG versions. The vast majority of the cases are inliers (including DRGs with fixed length of stay) for all investigated SwissDRG versions. Nevertheless, the total sum of reductions for low outliers decreased, especially from SwissDRG 1.0 to 2.0, while the total sum of supplements for high outliers decreased slightly too (table 5). Overall, the proportion of case-mix points compared with the total sum of case-mix points that could be charged under the different SwissDRG versions first increased slightly from 3.8% to 4.0% between SwissDRG 1.0 and 2.0 and then decreased again to 3.5% under SwissDRG version 3.0 (table 5).
Supplementary payments
Supplementary payments were very cautiously introduced under SwissDRG in 2012, with very few procedures receiving supplementary reimbursement. Originally, they were developed especially for high-cost services required by heterogeneous patients. The English healthcare resource group (HRG) system has developed the concept of “unbundling”, which separates a set of certain services, such as chemotherapy, radiotherapy, diagnostic imaging, renal dialysis and high-cost drugs, from the core HRGs [32], which is a similar concept. By separating these services, the economic homogeneity of core DRGs/HRGs should be improved and, at the same time, adequate reimbursement through supplementary payments should be guaranteed [33]. In total, only three patients discharged in 2012 of the study group were eligible for supplementary payments under catalogue 1.0 (total of 41 987 CHF). For patients discharged in 2011, the corresponding data were not available. As the amount is marginal in comparison with the total revenue (less than 0.2%), this imprecision was judged tolerable. However, the supplementary payments for blood products introduced with the catalogue version 3.0 in 2014 have a strong influence on revenue for severely injured patients: in total, 69 cases of the study group were eligible (approximately 19%), totalling 290 466 CHF.
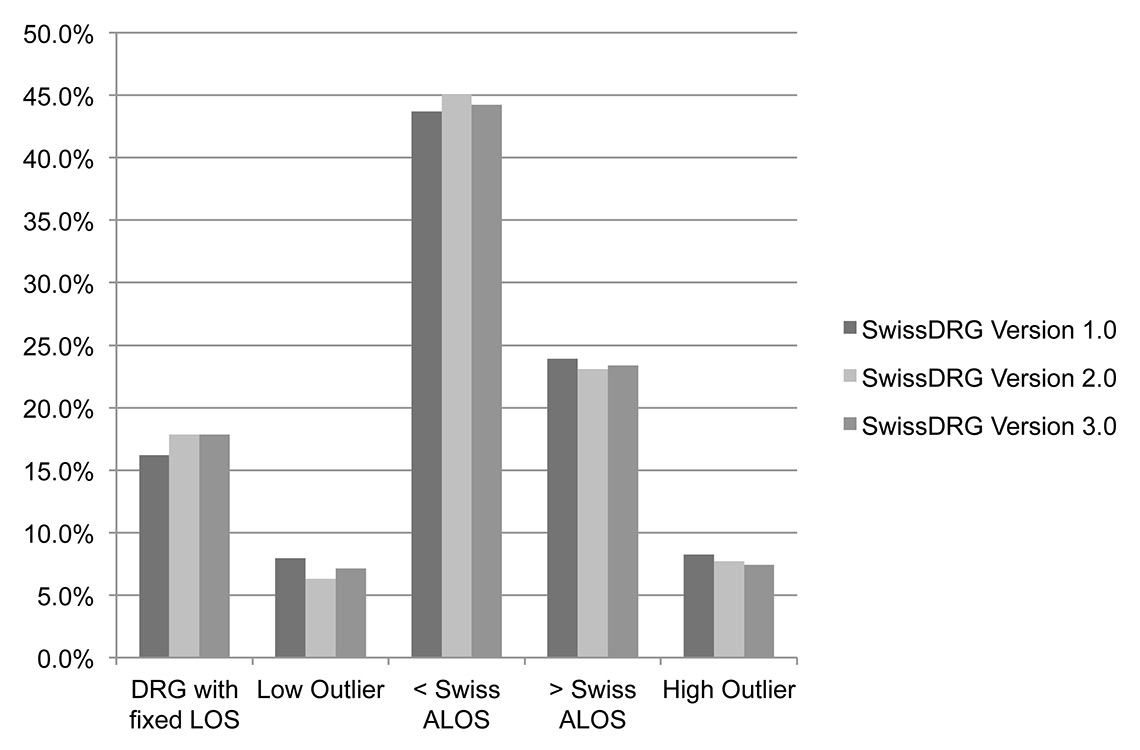
Figure 2
Proportions of DRG inliers (< Swiss ALOS and > Swiss ALOS), DRGs with fixed LOS and outliers (low and high outlier) according to length of stay and definition of low and high trim points for outlier under SwissDRG Versions 1.0, 2.0 and 3.0 respectively.
ALOS = average length of stay; LOS = length of stay
Discriminatory power of SwissDRG
From all cases included in our study, the numbers grouped into a polytrauma DRG especially designed for severely injured cases (major diagnostic category [MDC] 21A = DRG category 1) were 135 (37.1%) according to the grouper algorithm of SwissDRG version 1.0, 171 (47.0%) cases according to version 2.0 and 166 (45.6%) according to version 3.0 (table 4). Fifty-eight (15.9%) cases were classified into pre-MDC or ICU-related DRGs (DRG category 2) according to SwissDRG 1.0, 52 cases (14.3%) according to SwissDRG 2.0 and 57 (15.7%) cases according to SwissDRG 3.0. The remaining 171 (47%) cases according to version 1.0 and 141 cases according to versions 2.0 and 3.0 (38.7%) were grouped into other DRGs (DRG category 3). Therefore, only 53 % of the patients meeting the clinical criteria for a severely injured patient (ISS score ≥16) were classified appropriately under SwissDRG 1.0 (MDC 21A [polytrauma] or pre-MDC [intensive care DRGs]). Under SwissDRG 2.0 and 3.0 this number increased to 61.2%.
DRG categories and grouper algorithm
The average deficit of the 135 polytrauma DRGs (DRG category 1) amounted to 645 CHF (SD 37 409 CHF) under SwissDRG Version 1.0 as shown in table 3. Cases within DRG category 2 incurred an average loss of 36 075 CHF (SD 70 387 CHF) and the remaining cases (DRG category 3) for an average loss of 13 871 CHF (SD 30 163 CHF). Therefore, only severely injured patients who were grouped into a specific polytrauma DRG could be treated with cost coverage. The main improvement from SwissDRG 1.0 to 3.0 was due to a regrouping of cases from MDC 01 DRGs (neurological DRGs) to MDC 21A DRGs (n = 23). Under version 3.0, the pre-MDC cases still had the highest average loss per case. However, severely injured cases grouped into MDC 01 DRGs accounted for most of the total loss with 1 055 684 CHF in total and an average loss per case of 9 959 CHF (SD 22 142 CHF). Here, the grouper algorithm classified cases with injuries of the cranium or spine in combination with severe abdominal injuries such as lacerations of visceral organs or with other serious injuries into DRGs such as B02D or B61Z, although these DRGs are meant to represent neurosurgical cases without concomitant injuries.
Predictors for high deficit cases
We identified a number of variables that were significantly correlated with the per-case deficit. Cases with a high number of surgical interventions, surgery on multiple anatomical regions, the existence of certain injuries, such as fractures of the tibia, fibula or pelvis, or certain procedures such as open reductions and internal fixations of the tibia showed an increased loss per case (p ≤0.002) as demonstrated in tables 6 and 7. The total number of surgical operations is a stronger predictor of loss than the number of anatomical regions injured (p = 0.002 vs p = 0.72). In addition, in DRG category 3 hours of ICU treatment is also a better predictor of deficit than the hours of mechanical ventilation (p >0.001 vs p = 0.003). For cases with DRGs in category 3, a stay in the ICU correlated more strongly with the deficit than the number of surgical procedures or the number of anatomical regions with surgical interventions. In these cases, the nine equivalents of nursing manpower use score (NEMS) and the simplified acute physiology score for severity of illness (SAPS) were insufficient to classify them into pre-MDC DRGs or into B36B.
The presence of psychiatric illnesses in general also showed an increased loss per case (p <0.001). Depressive disorders showed a tendency to be underfunded as well, although the correlation was not significant (p = 0.006). For the full detail of all results, please refer to supplements 3 and 4.
|
Table 1: Population characteristics of patients with severe trauma, discharged in 2011 and 2012 (n = 364). |
|
|
Study population ISS ≥16
(n = 364)
|
|
Mean
|
(Standard deviation)
|
Median
|
(Range)
|
| Age (years) |
50.7 |
(21.6) |
49 |
(16–95) |
| GCS (n = 253) |
9.9 |
(4.9) |
12 |
(3–15) |
| ISS |
34.2 |
(18.6) |
27 |
(16–75) |
| NISS |
40.4 |
(18.1) |
34 |
(16–75) |
| RISC |
26.8 |
(31.0) |
12.6 |
(1.1–99.9.) |
| Length of intensive care treatment (days) |
7.1 |
(10.4) |
3.0 |
(0–95) |
| Duration of mechanical ventilation (h) |
93.8 |
(182.6) |
12 |
(0–1577) |
| Length of stay (days) |
14.2 |
(15.4) |
11 |
(1–118) |
| PCCL |
2.5 |
(1.7) |
3 |
(0–4) |
| Injured body regions |
2.5 |
(1.4) |
2 |
(0–7) |
| Number of surgical operations |
2.2 |
(3.1) |
1 |
(0–26) |
| Number of operated body regions |
1.5 |
(1.2) |
1 |
(0–6) |
| GCS = Glasgow coma score; ISS = injury severity score; NISS = new injury severity score; PCCL = patient clinical complexity level; RISC = revised Injury severity classification score |
|
Table 2: Abbreviated injury score distribution of cases with severe trauma discharged in 2011 and 2012 by injured body region (n = 364). |
|
|
Study population ISS ≥16
(n = 364)
|
|
Mean
|
(Standard deviation)
|
Median
|
(Range)
|
| AIS Head |
3.2 |
(2.0) |
4 |
(0–6) |
| AIS Face |
0.7 |
(1.2) |
|
(0–4) |
| AIS Thorax |
1.9 |
(1.8) |
3 |
(0–6) |
| AIS Abdomen |
1.0 |
(1.5) |
|
(0–5) |
| AIS Extremities |
1.5 |
(1.5) |
2 |
(0–5) |
| AIS Soft tissue injuries |
0.8 |
(0.9) |
1 |
(0–5) |
| AIS = abbreviated injury score; ISS = injury severity score |
|
Table 3: Average results per case according to SwissDRG versions 1.0, 2.0 and 3.0, including supplementary payments, for study group and different DRG categories. A base rate of 11 300 CHF was assumed (n = 364). Results per case are given as mean (standard deviation). |
|
DRG catalogue version
|
Mean revenues/costs/results (CHF)
(SD)
|
Mean results per DRG category in CHF (SD)
|
|
Revenue
|
Costs
|
Profit/deficit
|
DRG category 1
|
DRG category 2
|
DRG category 3
|
| SwissDRG 1.0 (2012) |
57 058 (66 495) |
69 123 (86 537) |
–12 065 (65 974) |
–645 (37 409) |
–34 517 (70 387) |
–13 466 (30 163) |
| SwissDRG 2.0 (2013) |
62 146 (72 007) |
69 123 (86 537) |
–6977 (38 197) |
–1019 (36 604) |
–14 930 (65 442) |
–11 268 (22 596) |
| SwissDRG 3.0 (2014) |
66 221 (80 018) |
69 123 (86 537) |
–2902 (35 713) |
2497 (33 752) |
–4800 (59 911) |
–10 551 (20 864) |
| DRG = diagnosis-related group; ICU = intensive care unit; SD = standard deviation
DRG category 1: polytrauma DRGs, DRG category 2: ICU DRGs, DRG category 3: other DRGs |
|
Table 4: Cumulative revenue, costs and financial results according to SwissDRG versions 1.0, 2.0 and 3.0, including supplementary payments, as well as catalogue effects for the whole study group and DRG categories. A base rate of 11 300 CHF was assumed (n = 364). Results per case are given as mean (standard deviation). The CMI is given in case mix points. |
|
DRG Catalogue Version
|
Cumulative revenues/costs/results (CHF)
Whole study population (n = 364)
|
Cumulative results per DRG category
(number of cases)
|
Catalogue effect
(CE)
|
|
Revenue
|
Costs
|
Cumulative results
|
DRG-category 1
|
DRG-category 2
|
DRG-category
3
|
CMI
|
CE
|
| SwissDRG 1.0 (2012) |
20 768 948 |
25 160 666 |
–4 391 718 |
–87 068 (n = 135) |
–2 001 978 (n = 58) |
–2 302 672 (n = 171) |
5.039 |
– |
| SwissDRG 2.0 (2013) |
22 621 220 |
25 160 666 |
–2 539 446 |
–174 232 (n = 171) |
–776 370 (n = 52) |
–1 588 844 (n = 141) |
5.489 |
8.93% |
| SwissDRG 3.0 (2014) |
24 104 417 |
25 160 666 |
–1 056 249 |
414 510 (n = 166) |
–273 604 (n = 57) |
–1 487 622 (n = 141) |
5.779 |
5.28% |
| DRG = diagnosis-related group; ICU = intensive care unit
CMI: case mix index (average cost weight per case)
CE: catalogue effect (change in average cost weight in % from one year to the next soley due to change of DRG catalogue)
DRG category 1: polytrauma DRGs, DRG category 2: ICU DRGs, DRG category 3: Other DRGs |
|
Table 5: Development of low outlier reductions and high outlier supplements in case mix points and in CHF (base rate 11 300) under SwissDRG versions 1.0, 2.0 and 3.0. |
|
DRG catalogue version
|
Reductions and supplements (in CM)
|
Reductions and supplements (in CHF)
|
Percentage of total CM
|
|
Low outlier reductions
|
High outlier supplements
|
Sum of reductions and supplements
|
Low outlier reductions
|
High outlier supplements
|
Sum of reductions and supplements
|
Total CM (n = 364)
|
Proportion of total CM in %
|
| SwissDRG 1.0 (2012) |
–25.928 |
95.158 |
69.230 |
–292 986 |
1 075 285 |
782 299.000 |
1 834.244 |
3.8% |
| SwissDRG 2.0 (2013) |
–14.676 |
93.879 |
79.203 |
–165 839 |
1 060 833 |
894 993.900 |
1 998.162 |
4.0% |
| SwissDRG 3.0 (2014) |
–14.415 |
88.596 |
74.181 |
–162 890 |
1 001 135 |
838 245.300 |
2 103.714 |
3.5% |
| CM = case-mix points; DRG = diagnosis-related group
CE: catalogue effect (change in average cost weight in % from one year to the next due to sole change of DRG catalogue) |
Discussion
We completed an analysis of the reimbursement for severely injured patients, from a healthcare provider perspective. Like previous investigations from other countries, we also can conclude that treatment at cost coverage for trauma patients under SwissDRG was not possible for our cohort when reimbursement tariffs from 2012 to 2014 were applied [14, 19]. However, we were able to establish predictors of underfunding in our cohort, based on clusters of diagnoses or surgical procedures. Further, since only one previous Swiss investigation estimating the actual average treatment costs for severely injured patients in Switzerland has been published, we also wanted to determine the actual costs of care at a Swiss level 1 trauma centre [34].
A benchmarking of our costs to those of other Swiss university hospitals did not show higher treatment costs for trauma patients at our centre compared with the reference group, as the average costs per case, including all patients with solely basic insurance coverage, were 0.6% below the benchmark [35]. Therefore, the deficit is most likely not due to the cost structure of our centre, but due to a structural underfinancing of care of the severely injured under SwissDRG.
We demonstrated improvements in the refinancing of severe injury care from SwissDRG 1.0 (catalogue of 2012) to 3.0 (catalogue of 2014), due to algorithm rearrangements, more case-mix points assigned and new supplementary payments for blood products. The results also indicated, that changes in thresholds for DRG outlier definitions (changes in high trim points and low trim points) cannot explain the improvements that have been achieved. However, even under SwissDRG 3.0, care for 364 patients with an ISS ≥16 still caused a total loss of approximately 1.1 million CHF at a base rate of 11 300 CHF per case-mix point. We would like to underline the fact that the base rate employed for our calculations is high at 11 300 CHF, in comparison with base rates of the majority of other Swiss hospitals or cantons. At a base rate of 9 600 CHF per case-mix point, the loss would increase to 5.0 million CHF per year.
The analysis of the DRG subgroups showed that the main deficit sources were the cases grouped into DRG categories 2 (ICU DRGs) and 3 (other, not strictly polytrauma or ICU DRGs) (table 4). The polytrauma DRGs as such (category 1) allowed cost-coverage for medical care under SwissDRG 3.0.
The 141 cases grouped into a DRG in category 3, a rather inhomogeneous group of cases that were not assigned a special DRG for multiply injured patients or ICU-related cases, accounted for the majority of the remaining deficit under SwissDRG 3.0. The average deficit per case did not decrease markedly between the catalogue versions 1.0 and 3.0. The main improvement came from a regrouping of 30 cases into a polytrauma DRG. It should, therefore, be possible to further improve the cost coverage of underfinanced severe-injury care by further fine-tuning the grouper algorithm. We identified possible split criteria, which should be analysed by SwissDRG AG and which could possibly be of use in the further development of the reimbursement system. Such variables include the number of surgical interventions and the number of operated body regions. We advocate the addition of fractures of the lower extremities, especially of the tibia, as well as surgical procedures such as the stabilisation of pelvic bones in order to separate polytrauma DRGs in combination with other injuries to allow for a more accurate grouping of severely injured patients into adequate DRGs. We also strongly recommend the prioritisation of MDC 21A over MDC 01 in the grouper algorithm, to improve the classification of severely injured patients with spinal cord injuries.
We would welcome discussion about the necessity to increase the number of available polytrauma DRGs. Perhaps the introduction of further MDC-21A DRGs for cases with long intensive care treatment, albeit not sufficient for qualifying for a pre-MDC DRG, could be part of the solution.
A limitation to this study lies in the fact that it can only hint at the possibility of improvements of SwissDRG and the definite improvements need to be made based on the data of all Swiss hospitals delivering cost data to the SwissDRG AG for calculation purposes.
SwissDRG 3.0 uses a complicated DRG algorithm but does not take into account the number of surgical sites or the number of surgical interventions, even though they correlate with total treatment costs.
Furthermore, cases grouped into B02D, which include spinal cord injuries, were also eligible for classification into a polytrauma DRG. However, the grouper algorithm gave preference to the MDC 01 category, so that severely injured cases with injuries of the spinal cord were classified into MDC 01 leading to high losses per case. We are confident that the predictors identified could be of use as split criteria in the future refinement of the accuracy of the DRG reimbursement system for severe trauma care. We are aware of the fact that the DRG system is not meant to be cost-covering at an individual case level, but since only trauma centres should treat patients with severe injuries, cost coverage for the selected cohort should be targeted. However, there will be no easy solution to the problem as long as the clinical criteria for classifying a patient as a severe trauma case (ISS) are not reflected in the criteria for DRG selection. Currently, the ISS cannot be coded with ICD-10 or CHOP codes. Other alternatives will most likely always suffer from some drawbacks of variable impact.
Conclusion
A further refinement of the DRG grouping algorithms is suggested above. In addition, the introduction of further supplementary payments for costly implants, medication and coagulation factors may further improve the reimbursement system and solve the continuing problems.
Figure S1
SwissDRG and revenues according to length of stay (LOS).
References
1 Westhoff J, Hildebrand F, Grotz M, Richter M, Pape HC, Krettek C. Trauma care in Germany. Injury 2003;34:674–83.
2 MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–78.
3 Celso B, Tepas J, Langland-Orban B, Pracht E, Papa L, Lottenberg L, Flint L. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–8; discussion 8.
4 Papa L, Langland-Orban B, Kallenborn C, Tepas JJ, 3rd, Lottenberg L, Celso B, Durham R, Flint L. Assessing effectiveness of a mature trauma system: Association of trauma center presence with lower injury mortality rate. J Trauma. 2006;61:261–6; discussion 6–7.
5 Twijnstra MJ, Moons KG, Simmermacher RK, Leenen LP. Regional trauma system reduces mortality and changes admission rates: a before and after study. Ann Surg. 2010;251:339–43.
6 Morshed S, Knops S, Jurkovich GJ, Wang J, MacKenzie E, Rivara FP. The impact of trauma-center care on mortality and function following pelvic ring and acetabular injuries. J Bone Joint Surg Am. 2015;97:265–72.
7 Mahlke L, Lefering R, Siebert H, Windolf J, Roeder N, Franz D. Description of the severely injured in the DRG system. Is treatment of the severely injured still affordable? Chirurg. 2013;84:978–86.
8 Fallpauschalen in Schweizer Spitälern – Basisinformationen für Gesundheitsfachleute [monograph on the internet]. SwissDRG AG, Bern; 2011. Available from: http://www.swissdrg.org/assets/pdf/Broschuere/Broschuere_SwissDRG_d_A4.pdf
9 Liener UC, Rapp U, Lampl L, Helm M, Richter G, Gaus M, et al. Incidence of severe injuries. Results of a population-based analysis. Unfallchirurg. 2004;107:483–90. German.
10 Di Bartolomeo S, Sanson G, Michelutto V, Nardi G, Burba I, Francescutti C, et al. Epidemiology of major injury in the population of Friuli Venezia Giulia-Italy. Injury. 2004;35:391–400.
11 W F, H B, N R. Ist eine Kalkulation von seltenen und sehr aufwendigen Krankenhausfällen im G-DRG-System sachgerecht? Krankenhaus. 2011;7:680–6.
12 Mehra T, Muller CT, Volbracht J, Seifert B, Moos R. Predictors of High Profit and High Deficit Outliers under SwissDRG of a Tertiary Care Center. PLoS One 2015;10: e0140874.
13 Mehra T, Koljonen V, Seifert B, Volbracht J, Giovanoli P, Plock J, Moos RM. Total inpatient treatment costs in patients with severe burns: towards a more accurate reimbursement model. Swiss Med Wkly. 2015;145:w14217.
14 Juhra C, Franz D, Roeder N, Vordemvenne T, Raschke MJ. Classification of severely injured patients in the G-DRG System 2008. Unfallchirurg. 2009;112:525–32. German.
15 Flohe S, Buschmann C, Nabring J, Merguet P, Luetkes P, Lefering R, Nast-Kolb D, Ruchholtz S. Definition of polytrauma in the German DRG system 2006. Up to 30% “incorrect classifications”. Unfallchirurg. 2007;110:651–8. German.
16 Franz D, Schemmann F, Selter DD, Auhuber T, Wirtz DC, Roeder N, et al. Remuneration for Orthopedic and Trauma Surgery in the German an Diagnosis-Related Groups (DRG) System Current Developments and Future Action. Unfallchirurg. 2013;116:760–6.
17 Franz D, Schemmann F, Roeder N, Mahlke L. Financing of inpatient orthopedics and trauma surgery in the G-DRG system 2010. Unfallchirurg. 2010;113:682–9.
18 Probst C, Schaefer O, Hildebrand F, Krettek C, Mahlke L. The economic challenges of polytrauma care. Unfallchirurg. 2009;112:975–80.
19 Franz D, Schemmann F, Roeder N, Mahlke L. Financing of inpatient orthopedics and trauma surgery in the G-DRG system 2010. Unfallchirurg. 2010;113:682–9.
20 Freitas A, Silva-Costa T, Lopes F, Garcia-Lema I, Teixeira-Pinto A, Brazdil P, Costa-Pereira A. Factors influencing hospital high length of stay outliers. BMC Health Serv Res. 2012;12:265.
21 Obertacke U, Neudeck F, Wihs HJ, Schmit-Neuerburg KP. Emergency care and treatment costs of polytrauma patients. Langenbecks Arch Chir Suppl Kongressbd 1996;113:641–5.
22 Obertacke U, Neudeck F, Wihs HJ, Schmit-Neuerburg KP. Cost analysis of primary care and intensive care treatment of multiple trauma patients. Unfallchirurg. 1997;100:44–9.
23 Wilke MH, Hocherl E, Scherer J, Janke L. Introduction of the new DRG-based reimbursement system in German hospitals – a difficult operation? Experiences and possible solutions from the viewpoint of trauma surgery. Unfallchirurg. 2001;104:372–9.
24 Schwermann T, Grotz M, Blanke M, Ruchholtz S, Lefering R, JM VdS, et al. Evaluation of costs incurred for patients with multiple trauma particularly from the perspective of the hospital. Unfallchirurg. 2004;107:563–74.
25 Grotz M, Schwermann T, Lefering R, Ruchholtz S, Graf v d Schulenburg JM, Krettek C, Pape HC. DRG reimbursement for multiple trauma patients – a comparison with the comprehensive hospital costs using the German trauma registry. Unfallchirurg. 2004;107:68–75.
26 Fetter RB, Shin Y, Freeman JL, Averill RF, Thompson JD. Case mix definition by diagnosis-related groups. Med Care. 1980;18: iii, 1–53.
27 Geissler A, Quentin W, Busse R. Heterogeneity of European DRG systems and potentials for a common EuroDRG system Comment on “Cholecystectomy and Diagnosis-Related Groups (DRGs): patient classification and hospital reimbursement in 11 European countries”. Int J Health Policy Manag. 2015;4:319–20.
28 Mathauer I, Wittenbecher F. Hospital payment systems based on diagnosis-related groups: experiences in low- and middle-income countries. Bull World Health Organ 2013;91:746–56A.
29 Whitebook – Medical Care of the Severely Injured. 2 ed: German Society for Trauma Surgery (reg. assoc.), Berlin, 2012.
30 REKOLE® Handbuch – Betriebliches Rechnungswesen im Spital [monograph on the internet]. Bern, Switzerland; 2014. Available from: http://www.hplus.ch/de/dienstleistungen/betriebswirtschaft/rechnungswesen_spital/rekoler_handbuch/
31 Zürich GdK. Handbuch PRISMA Wegleitung zur Erhebung des Patientenrecord in der Somatik [monograph on the internet]. 2014. Available from: http://www.gd.zh.ch/dam/gesundheitsdirektion/direktion/themen/gesundheitsinstitutionen/spitaeler_kliniken/handbuecher_vorgaben_erhebungsunterlagen/handbuecher_und_vorgaben/prisma/handbuch_prisma_2.1.pdf.spooler.download.1421054735957.pdf/handbuch_prisma_2.1.pdf
32 The Casemix Service HRG4, Guide to Unbundling. Leeds: NHS Information Centre for Health and Social Care 2009.
33 Diagnosis-Related Groups in Europe. In: Reinhard Busse AG, Wilm Quentin, Miriam Wiley, ed. Moving towards transparency, efficiency and quality in hospitals, 2011.
34 Ganzoni D, Zellweger R, Trentz O. Cost analysis of acute therapy of polytrauma patients. Swiss Surg. 2003;9:268–74.
35 Webfeedback 2013 Fallkostendaten 2012 Grouperversion 1.0, 2.0 und 3.0 [monograph on the internet]. Bern, Switzerland: SwissDRG AG; 2014. Available from: https://apps.swissdrg.org/webfeedback2013_10/users/sign_in