Clustering of cardiovascular disease risk factors among male youths in Southern Switzerland: preliminary study
DOI: https://doi.org/10.4414/smw.2016.14338
Maristella
Santi, Sebastiano A. G.
Lava, Giacomo D.
Simonetti, Andreas
Stettbacher, Mario G.
Bianchetti, Franco
Muggli
Summary
PRINCIPLES: The distribution of cardiovascular disease risk factors among youths in Southern Switzerland is poorly understood. The aim of this preliminary study was therefore to describe the prevalence of cardiovascular disease risk factors in 18- to 20-year-old males undergoing medical examination to assess fitness for recruitment into the army.
METHODS: Between 2009 and 2013, 1541 (21%) out of 7310 conscripts volunteered for answering a structured questionnaire addressing smoking behaviour, sedentariness and familial cardiovascular risk factors, as well as for measurement of blood pressure, lipidaemia and waist circumference.
RESULTS: Height, weight, body fatness and blood pressure were not statistically different between conscripts who had or had not volunteered to participate in the study. The following risk factors were detected: smoking (n = 656; 43% of the study participants), sedentariness (n = 594; 39%), positive cardiovascular family history (n = 235; 15%), blood pressure ≥140/90 mm Hg (n = 88; 5.7%), total cholesterol ≥5.2 mmol/l (n = 83; 5.4%), waist circumference ≥1.02 m (n = 55; 3.6%). No cardiovascular risk factor was detected in 434 (28%), one factor in 612 (40%) and two or more factors in 495 (32%) participants.
CONCLUSIONS: This preliminary cross-sectional survey generated the first analysis of cardiovascular risk factors among ostensibly healthy male youths living in Southern Switzerland. The main finding is that two or more cardiovascular disease risk factors are present in approximately one third of them. Since smoking and sedentary lifestyle, the most commonly detected cardiovascular risk factors, are preventable, youths represent an opportunity for the promotion of lifestyles that will affect the development and progression of atherosclerotic disease.
Introduction
Although atherosclerotic cardiovascular diseases, such as heart attack and stroke, do not usually present clinically until adulthood, the development of atherosclerosis may begin early in life [1]. Previous work has shown that in children and adolescents, the presence and extent of atherosclerotic lesions positively correlate with established risk factors such as familial cardiovascular history, sedentary lifestyle, smoking, high blood pressure and dyslipidaemia. Finally, an increasing body of research now documents the safety and success of interventions to reduce risk factors in this age group [2].
Studies from the United States and a limited number of European countries report the burden of cardiovascular disease risk factors in adolescents [1, 2]. The distribution of these factors among youths living in Southern Switzerland is only poorly understood. This knowledge, however, represents the basis for successful and sustainable preventive strategies to reduce future cardiovascular diseases. This preliminary report details the prevalence of cardiovascular disease risk factors in male Swiss Italian youngsters.
Methods
In Switzerland, ostensibly healthy male citizens undergo a compulsory medical examination to assess fitness for recruitment into the army in the year they turn 18 to 19. A medical history is obtained, height, weight, heart rate and blood pressure are measured, a physical examination is performed and a status of “medically fit for military service” or “unfit for military service” is finally assigned [3].
Among 7310 young men who underwent the examination between 2009 and 2013 in Southern Switzerland, 1541 (21%) volunteered (2009: 195; 2010: 254; 2011: 338; 2012: 421; 2013: 333) to answer a self-administered structured questionnaire addressing familial cardiovascular risk factors, smoking behaviour and sedentary lifestyle, and for measurement of waist circumference and total and high-density lipoprotein cholesterol levels.
Weight was measured to the nearest 0.1 kg with a platform scale, height to the nearest 0.1 cm with a stadiometer and waist circumference to the nearest 0.5 cm with a non-stretching tape placed around the abdomen at the iliac crest. Sitting blood pressure and heart rate were measured after the participant had been seated at least 5 minutes. A single high reading does not necessarily mean hypertension and the average of several readings provides a more reliable estimate of blood pressure [4]. Consequently, at least three more readings were made with the average mode technology [4] and averaged in volunteers with an initial reading ≥140/90 mm Hg. Three further readings were obtained 24 hours later in subjects with an average reading ≥140/90 mm Hg. Blood pressure was measured with an oscillometric automatic Microlife® monitor validated according to the protocol of the British Society of Hypertension. The average mode technology takes three or more measurements of blood pressure 15 seconds apart [4].
Blood was drawn for determination of total and high-density lipoprotein cholesterol (after precipitation of other lipoproteins) by means of a cholesterol oxidase assay.
The cardiovascular risk profile of the participants was classified as follows. Cardiovascular family history was categorised as positive in individuals with heart attack, diabetes mellitus, obesity or arterial hypertension in at least one first-degree relative before the age of 65 years. Smoking behaviour was categorised as smoker versus nonsmoker and physical lifestyle as sedentary versus active based on participation in physical activities (or sports) once a week or less. The following further cardiovascular disease risk factors were addressed, as recommend by the American Heart Association: body mass index ≥25.0 kg/m2; waist circumference ≥1.02 m; blood pressure ≥140/90 mm Hg; total cholesterol level ≥5.2 mmol/l; high-density lipoprotein cholesterol level ≤1.00 mmol/l; ratio of total to high-density lipoprotein cholesterol level ≥5.0.
Written informed consent was obtained from all participants. The study was approved by the Research Ethics Committee of Southern Switzerland (CE 2775). All data were made fully anonymous before analysis.
Since clustering of cardiovascular disease risk factors has proved a better measure of cardiovascular health than single risk factors [2], a clustering score was calculated for each participant by cumulating the following six risk factors: (1) positive cardiovascular family history; (2) smoker status; (3) sedentary lifestyle; (4) increased waist circumference; (5) arterial hypertension; (6) increased total cholesterol level.
The results are presented as mean and standard deviation. The two tailed Student’s t-test was used to compare the results obtained in conscripts who volunteered the study with those obtained in the remaining subjects. For each year, the proportion of study participants with the cardiovascular risk factors recorded was calculated and possible differences in the prevalence of each cardiovascular risk factor were tested across the five study years by using χ2-tests and the Bonferroni adjustment for multiple comparisons.
Results
Height, weight, body mass index, heart rate and first blood pressure reading were similar between conscripts who had (n = 1541) or had not (n = 5769) volunteered for the study, as shown in table 1.
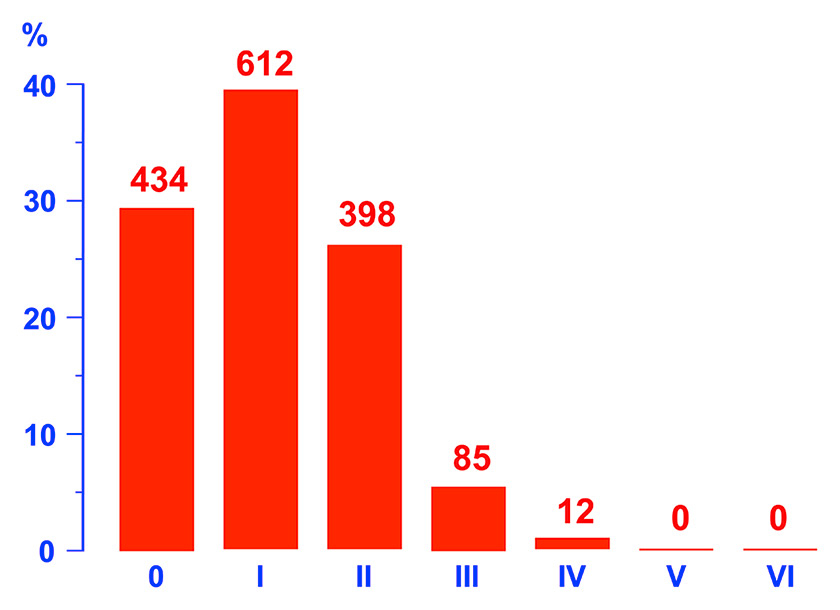
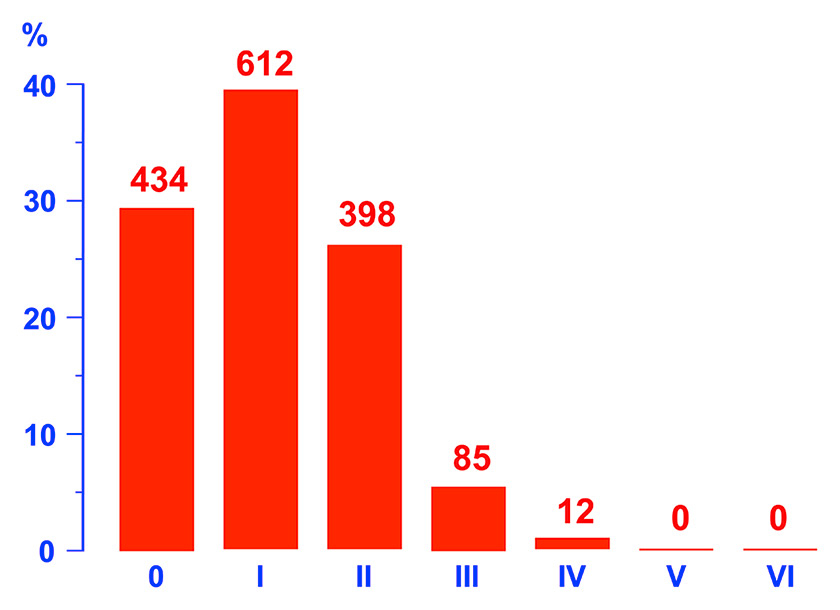
Figure 1
Clustering of cardiovascular risk factors (positive cardiovascular family history; smoker status; sedentary lifestyle; increased waist circumference; arterial hypertension; increased total cholesterol level) in 1541 ostensibly healthy male citizens undergoing a compulsory medical examination between 2009 and 2013 to assess fitness for recruitment into the Swiss army in the year they turn 18 to 19.
Among the 1541 study participants, the first blood pressure reading was ≥140/90 mm Hg in 552 (36%) and among 120–139 respectively 80–89 mm Hg in 432 (28%) subjects. Average mode blood pressure was still ≥140/90 mm Hg in 129 (23%) of the aforementioned 552 subjects. In 88 (68%) out of these 129 subjects, average mode blood pressure was still ≥140/90 mm Hg 24 hours later.
The cumulated results obtained across the five study years appear in table 2. The following cardiovascular disease risk factors were detected, in decreasing order of frequency: smoker (43% of the study participants), sedentary lifestyle (39%), increased body mass index (25%), decreased high-density lipoprotein cholesterol level (16%), positive cardiovascular family history (15%), arterial hypertension (5.7%), increased total cholesterol level (5.4%), increased waist circumference (3.6%) and increased total to high-density lipoprotein cholesterol ratio (3.1%).
The clustering of the cardiovascular disease risk factors of the participants is depicted in figure 1: no risk factor was detected in 434 (28%), one factor in 612 (40%) and two to four in 495 (32%) of the participants. None of participants had five or six risk factors. The following associations between cardiovascular risk factors were observed, in decreasing order of frequency: first, sedentary lifestyle and smoking (n = 328); second, hypertension and sedentary lifestyle (n = 47); third, hypertension and smoking (n = 46); fourth, increased waist circumference and smoking (n = 34); fifth, increased waist circumference and sedentary lifestyle (n = 19).
The prevalence of each of the risk factors was not statistically different in the five study years.
|
Table 1: Characteristics of Swiss-Italian conscripts who had respectively had not volunteered to participate in the study between 2009 and 2013. Results are given as mean and standard deviation. No statistically significant differences were noted between the two groups. |
| |
Volunteers
|
Non-volunteers
|
| n |
1541 |
5769 |
| Height, m |
1.78 ± 0.06 |
1.78 ± 0.07 |
| Body weight, kg |
74.0 ± 11.7 |
73.5 ± 13.8 |
| Body mass index, kg/m2
|
23.5 ± 3.4 |
23.4 ± 3.7 |
| Heart rate, bpm |
78 ± 16 |
77 ± 17 |
| Blood pressure (diastolic/systolic), mm Hg |
136 ± 15 / 80 ± 10 |
136 ± 14 / 80 ± 10 |
|
Table 2: Cardiovascular risk profile of the study population over the study period (2009–2013). Numerical data are presented as mean and standard deviation, categorical data as absolute value and percentage. |
| n |
1541 |
| Cardiovascular family history positive, n (%) |
235 (15) |
| Smoker, n (%) |
656 (43) |
| Sedentary lifestyle, n (%) |
594 (39) |
| Body mass index ≥25.0 kg/m2, n (%) |
384 (25) |
| Waist circumference, m |
|
| |
Absolute value |
0.82 ± 0.09 |
| |
>1.02, n (%) |
55 (3.6) |
| Arterial hypertension*, n (%) |
88 (5.7) |
| Circulating cholesterol level |
|
| |
Total level, mmol/L |
|
| |
|
Absolute value |
3.9 ± 0.7 |
| |
|
≥5.2, n (%) |
83 (5.4) |
| |
HDL level, mmol/L |
|
| |
|
Absolute value |
1.25 ± 0.26 |
| |
|
≤1.00, n (%) |
253 (16) |
| |
Total/HDL ratio |
|
| |
|
Absolute value |
3.3 ± 0.8 |
| |
|
≥5.0, n (%) |
47 (3.0) |
| HDL = high-density lipoprotein
* All three blood pressure studies ≥140/90 mm Hg |
Discussion
Cardiovascular disease risk factors predict the development of premature atherosclerosis. When two or more cardiovascular risk factors occur in one individual, they interact in a multiplicative way to promote cardiovascular disease [2]. This preliminary cross-sectional survey generates the first analysis of cardiovascular disease risk factors among ostensibly healthy male youths living in Southern Switzerland. The main finding is that two or more cardiovascular disease risk factors are present in approximately one third of them. While this percentage is notably high, it is similar to that described in earlier studies [5–8].
Smoking and sedentary lifestyle were common in our study population. These cardiovascular risk factors may be at least in part corrected by smoking cessation, healthy eating pattern and increased physical activity. Increased physical activity can also help raise high-density lipoprotein cholesterol, the most common lipid abnormality (approximately 15%) in our study population. The present data confirm that the cardiovascular family history is positive in many adolescents.
Two factors likely account for the rather rare recognition of arterial hypertension in our survey: first, a blood pressure device featuring the average mode technology [4] was used, which minimises the influence of the alerting reaction to the blood pressure reading [9]; second, arterial hypertension usually develops later in life.
The strengths of the study are twofold. First, the study population was drawn from all ostensibly healthy youths, who undergo a medical examination to assess fitness for recruitment into the army, which represents an excellent basis for investigations among unselected subjects [10]. Second, we did not identify differences between volunteers and non-volunteers for the study. This investigation also has some limitations. First, since Swiss females do not undergo any compulsory medical examination when they turn 18 to 19, they were not included in this study. Second, the rather low participation rate introduces some possible biases. Third, the study design did not address the possible occurrence of masked hypertension – normal blood pressure in the clinic, but “out-of-office” hypertension. Fourth, well-recognised cardiovascular risk factors such as diabetes, hyperuricaemia and hypovitaminosis D were not addressed. Finally, noninvasive surrogate endpoints for atherosclerotic disease such as carotid intima-medial thickness [11] or arterial stiffness [12] were not measured.
In conclusion, this preliminary survey indicates that fewer than one in three male Swiss Italian youths have optimal cardiovascular health. Since smoking and sedentary lifestyle, the most commonly detected cardiovascular risk factors, are preventable, youths represent an opportunity for the promotion of lifestyles that will affect the development and progression of atherosclerotic disease.
Acknowledgments: We would like to thank Dr Paolo Suter for giving advice on the project, and Manuela Christen, Angelica Fumi, Marlene Lorenzetti and Patrizia Venzin for collecting the data.
References
1 Gidding SS. Cardiovascular risk factors in adolescents. Curr Treat Options Cardiovasc Med. 2006;8(4):269–75.
2 Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al.; European Association for Cardiovascular Prevention & Rehabilitation (EACPR); ESC Committee for Practice Guidelines (CPG). European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33(13):1635–701.
3 Staub K, Wyss T, Lehmann S, Abel T, Frank Rühli F. Die Gesundheit junger Schweizer Männer: Monitoring-Ergebnisse der Armee-Rekrutierung. Praxis (Bern 1994). 2015;104(22):1203–10.
4 Wilton A, De Greef A, Shennan A. Rapid assessment of blood pressure in the obstetric day unit using Microlife MaM technology. Hypertens Pregnancy. 2007;26(1):31–7.
5 Cândido AP, Benedetto R, Castro AP, Carmo JS, Nicolato RL, Nascimento-Neto RM, et al. Cardiovascular risk factors in children and adolescents living in an urban area of Southeast of Brazil: Ouro Preto Study. Eur J Pediatr. 2009;168(11):1373–82.
6 Lambert M, Delvin EE, Levy E, O’Loughlin J, Paradis G, Barnett T, McGrath JJ. Prevalence of cardiometabolic risk factors by weight status in a population-based sample of Quebec children and adolescents. Can J Cardiol. 2008;24(7):575–83.
7 Müller-Riemenschneider F, Nocon M, Willich SN. Prevalence of modifiable cardiovascular risk factors in German adolescents. Eur J Cardiovasc Prev Rehabil. 2010;17(2):204–10.
8 Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM. Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005–2010. Circulation. 2013;127(13):1369–76.
9 ESH/ESC Task Force for the Management of Arterial Hypertension. 2013 practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC). J Hypertens. 2013;31(10):1925–38.
10 Vetterli DC, Lava SAG, Essig S, Milosevic G, Cajöri G, Uehlinger DE, Moor MB. Risk behavior and reciprocity of organ donation attitudes in young men. Transplant Proc. 2015;47(6):1560–6.
11 de Groot E, van Leuven SI, Duivenvoorden R, Meuwese MC, Akdim F, Bots ML, Kastelein JJ. Measurement of carotid intima-media thickness to assess progression and regression of atherosclerosis. Nat Clin Pract Cardiovasc Med. 2008;5(5):280–8.
12 Sander GE, Giles TD. Vascular stiffness is a biomarker of global cardiovascular risk. J Clin Hypertens (Greenwich). 2014;16(9):625–6.