High blood pressure: prevalence and adherence to guidelines in a population-based cohort
DOI: https://doi.org/10.4414/smw.2016.14323
Diana
Walther, Ivan
Curjuric, Julia
Dratva, Emmanuel
Schaffner, Carlos
Quinto, Thierry
Rochat, Jean-Michel
Gaspoz, Luc
Burdet, Pierre-Olivier
Bridevaux, Marco
Pons, Margaret W.
Gerbase, Christian
Schindler, Nicole
Probst-Hensch
Summary
QUESTIONS UNDER STUDY: High blood pressure, the single leading health risk factor worldwide, contributes greatly to morbidity and mortality. This study aimed to add to the understanding of diagnosed and undiagnosed high blood pressure in Switzerland and to evaluate adherence to hypertension guidelines.
METHODS: Included were 3962 participants from the first (2001–2003) and second (2010–2011) follow-ups of the population-based Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults. High blood pressure was defined as blood pressure ≥140/90 mm Hg and the prevalence of doctor-diagnosed hypertension was based on questionnaire information.
RESULTS: High blood pressure was found in 34.9% of subjects, 49.1% of whom were unaware of this condition; 30.0% had doctor-diagnosed hypertension and, although 82.1% of these received drug treatments, in only 40.8% was blood pressure controlled (<140/90 mm Hg). Substantial first-line beta-blocker use and nonadherence to comorbidity-specific prescription guidelines were observed and remained mostly unexplained. Age-adjusted rates of unawareness and uncontrolled hypertension were more than 20% higher than in the USA.
CONCLUSIONS: There is room for improvement in managing hypertension in Switzerland. Population-based observational studies are essential for identifying and evaluating unmet needs in healthcare; however, to pinpoint the underlying causes it is imperative to facilitate linkage of cohort data to medical records.
ACEI angiotensin converting-enzyme inhibitor
ARB angiotensin II receptor blocker
BB beta-blocker
BP blood pressure
CI confidence interval
DALY disability adjusted life year
ddHT doctor-diagnosed hypertension
HBP high blood pressure
OR odds ratio
SAPALDIA Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults
SSH Swiss Society of Hypertension
Introduction
High blood pressure (HBP) accounts for 17.8% of deaths and 7.0% of disability-adjusted life years (DALYs) globally, making it the number one single risk factor worldwide [1]. In Switzerland, a country with universal healthcare coverage and which ranks fourth in per capita total health expenditure [2], an estimated 27% of adults have hypertension [3] and 18.7% of deaths and 7.9% of DALYs [4] are attributed to this risk factor. The burden of disease related to hypertension is mainly mediated by ischaemic heart disease and stroke [5].
In Switzerland, concordant national data on hypertension prevalence from surveys, primary care or hospital discharge statistics are available [6]. However, when hypertension prevalence is based on diagnosed hypertension, the true prevalence of hypertension may be underestimated owing to the often asymptomatic nature of HBP. Regional estimates of undiagnosed hypertension in Switzerland vary from 6 to 13% of the adult population, this range may in part be explained by differences in age distributions and the age-standardisation of the reported rates in the respective studies [7, 8]. However, current nationwide population-based data covering varied geographical and cultural regions is lacking. Once diagnosed, one may expect uniformity in managing hypertension in a small and economically well-to-do country like Switzerland with its own guidelines for the management of hypertension [9]; however, national information on guideline adherence is scarce.
Managing hypertension according to guidelines remains a practical challenge, especially in a poly-morbid, poly-medicated population where more than one conflicting guideline may apply and drugs with antihypertensive properties are used for the treatment of other diseases. Moreover guidelines worldwide differ [9–12], and more than one document may influence clinical practice in a given country.
This study aimed to describe the prevalence, awareness, treatment and control of hypertension in Switzerland, and to evaluate adherence to the Swiss Society of Hypertension (SSH) guidelines in regards to drug choice.
Methods
Study population
This analysis was based on the Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults (SAPALDIA), with participants originally recruited from the general adult population in eight communities covering the range of geographical (urban, rural, alpine) and cultural (German-, French-, and Italian-speaking) conditions in Switzerland [13]. Beginning with a baseline assessment in 1991, the first and second follow-ups were in 2001–2003 (SAPALDIA 2) and 2010–2011 (SAPALDIA 3), respectively. Blood pressure (BP) measurement was added from SAPALDIA 2 onwards. Ethical approval was obtained from the Swiss Academy of Medical Sciences’ Central Ethical Committee and the appropriate cantonal ethics committees. Participants gave written informed consent. This analysis focused on data from SAPALDIA 3 using elements from SAPALDIA 2 for added depth. Included were SAPALDIA 2 and 3 participants for whom all relevant data were available: that is, questionnaire information on morbidities, medications, lifestyle and clinical information on blood pressure, weight and height (n = 3962) (see appendix, supplementary fig. S1).
Questionnaire information
Morbidity data were collected during an in-person interview with the use of questionnaires. Questions included: “Has a doctor ever told you that you have one of the following diseases?” followed by a list of diseases including hypertension, arrhythmia, asthma, etc. Only participants with asthma who had also had at least one attack in the last year or were taking asthma medication were considered as asthmatics in this analysis. Participants with atrial fibrillation were defined as those with arrhythmia taking either vitamin K antagonists or platelet aggregation inhibitors (excluding heparin). All medications taken were listed in a questionnaire. Drugs considered asantihypertensive were angiotensin converting-enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs), beta-blockers (BBs), calcium antagonists, diuretics, renin inhibitors and other hypertensives with anatomical therapeutic chemical (ATC) code C02. Questionnaire information on smoking (never, former, current), alcohol consumption (number of standard glasses/day), fruit and vegetable intake (number of servings/day) and physical activity (minutes of moderate and/or vigorous activity/week) was also collected. Neighbourhood-level socioeconomic index, a 0- to 100-point scale based on education, head of household occupation, rent and crowding derived from 2000 census data [14], was allocated on the basis of SAPALDIA 2 home address. Degree of urbanisation (high, medium, low) was allocated on the basis of home address according to the European-wide degree of urbanisation (DEGURBA) classification for local administrative units – usually communes.
Clinical measurements
Blood pressure was measured twice by trained field workers using an automatic device (705CP, OMRON, Tokyo, Japan) with a cuff of appropriate size (after having measured arm circumference) and using the Riva-Rocci method, in the sitting position after minimum 10 minutes rest, on the left arm, with 3 minutes between measurements. Blood pressure values are expressed as mean systolic and mean diastolic pressures in mm Hg. Height and weight were measured when the participants were without shoes and wearing light clothing.
High blood pressure and doctor-diagnosed hypertension
HBP was defined as systolic blood pressure ≥140 and/or diastolic blood pressure ≥90 mm Hg, simply described as HBP or “blood pressure ≥140/90” from now onwards. Doctor-diagnosed hypertension (ddHT) was based on the following question “Has a doctor ever told you that you have hypertension?” HBP unawareness refers to those with HBP but not ddHT and is expressed as a percentage of those with HBP. Uncontrolled ddHT refers to those with ddHT and HBP and is expressed as a percentage of those with ddHT.
Guideline adherence
Guideline adherence was evaluated in those with ddHT and was based on the Swiss Society of Hypertension 2009 guidelines [15] in effect at SAPALDIA 3 data collection. Specific recommendations are described in table 1. Current Swiss Society of Hypertension guidelines are available on their website [9].
Recommended lifestyle goals were combined in a lifestyle score, one point attributed for each recommendation successfully met; not smoking, low risk alcohol consumption (≤1 glass/day by women and ≤2 glasses/day by men) [16], fruit/vegetable consumption ≥5/day, body mass index <25 kg/m2and regular physical activity (150 minutes of moderate or 60 minutes of vigorous activity per week alone or in an equivalent combination with moderate activity).
|
Table 1: Selected 2009 Swiss Society of Hypertension guidelines [15]. |
|
Lifestyle improvements for all
|
| Smoking cessation, limited alcohol consumption, a diet rich in fruits and vegetables and poor in salt, physical activity, weight control |
|
Drug treatment
|
| First-line drugs: ACEI, ARB, CA, diuretics
Alternative drug: beta-blockers (not recommend as a first-line drug as some studies show them to be ineffective in reducing stroke and coronary heart disease and to have negative effects on lipid and glucose metabolism. However, beta-blockers are permitted to initiate therapy when certain comorbidities are present) [26] |
|
Comorbidity specific treatement, recommended drugs
|
| Coronary heart disease
Heart failure
Diabetes
Dyslipidaemia
Migraines
Asthma |
ACEI, ARB, BB, CA
ACEI, ARB, BB, diuretic
ACEI, ARB, BB*, CA
ACEI, ARB, CA
BB
avoid BB* |
|
Target blood pressure <140/90 in general
<130/80 in those with diabetes or kidney disease†
|
| ACEI = angiotensin converting enzyme inhibitor; ARB = angiotensin II receptor blocker; BB = beta-blocker; CA = calcium antagonist
* Beta-blockers are not recommended in people with abnormal glucose tolerance, but permitted in overt diabetes, blood pressure reduction being the main goal. The careful use of highly cardioselective beta-blockers is permitted in individuals with stable asthma if a good indication to beta-blocker use is present and with adequate monitoring [26].
† Note, the 2015 Swiss guidelines differ, placing target blood pressure at <140/85 in those with diabetes or kidney disease [9]. |
Statistical analysis
Unless noted otherwise, data presented are from SAPALDIA 3. Descriptive results are presented as number and percent for categorical variables and as median and interquartile range for quantitative variables. Chi-squared tests, t-tests and Wilcoxon rank-sum tests were used for bivariate analysis as appropriate. Several multivariable logistic regression models were constructed using the backwards stepwise method to assess determinants of the following outcomes; ddHT, HBP, HBP unawareness, uncontrolled ddHT and new onset of cardiovascular events (angina pectoris, myocardial infarction, heart failure and stroke). Covariates systematically considered in all models were: sex, age, language, degree of urbanisation, education, neighbourhood-level socioeconomic index and lifestyle score. Covariates additionally considered in some models were: systolic blood pressure, HBP, HBP unawareness, uncontrolled ddHT and a binomial variable for concomitant cardiovascular or metabolic disease (dyslipidaemia, diabetes, angina pectoris, myocardial infarction, heart failure or stroke). As neighbourhood-level socioeconomic index was available only for SAPALDIA 2 addresses, in sensitivity analyses the participants who had moved during the SAPALDIA 2–3 interval were excluded to determine if observed associations persisted. Since association patterns did not differ, results are not presented. All p-values <0.05 were considered statistically significant. Statistical analysis was performed using STATA 13 (StataCorp. 2013. Stata: Release 13. Statistical Software. College Station, TX: StataCorp LP.)
Results
Available characteristics of included and excluded participants at baseline and the first and second follow-ups are presented in supplementary table S1. In comparison with the excluded participants, our study sample was better educated, included fewer smokers and more physically active individuals having less HBP and/or ddHT, but having similar prevalences of other comorbidities. The analytical sample consisted of 3962 participants, 50% men and 50% women, with a median age of 60.4 years, ranging from 37 to 81 years old.
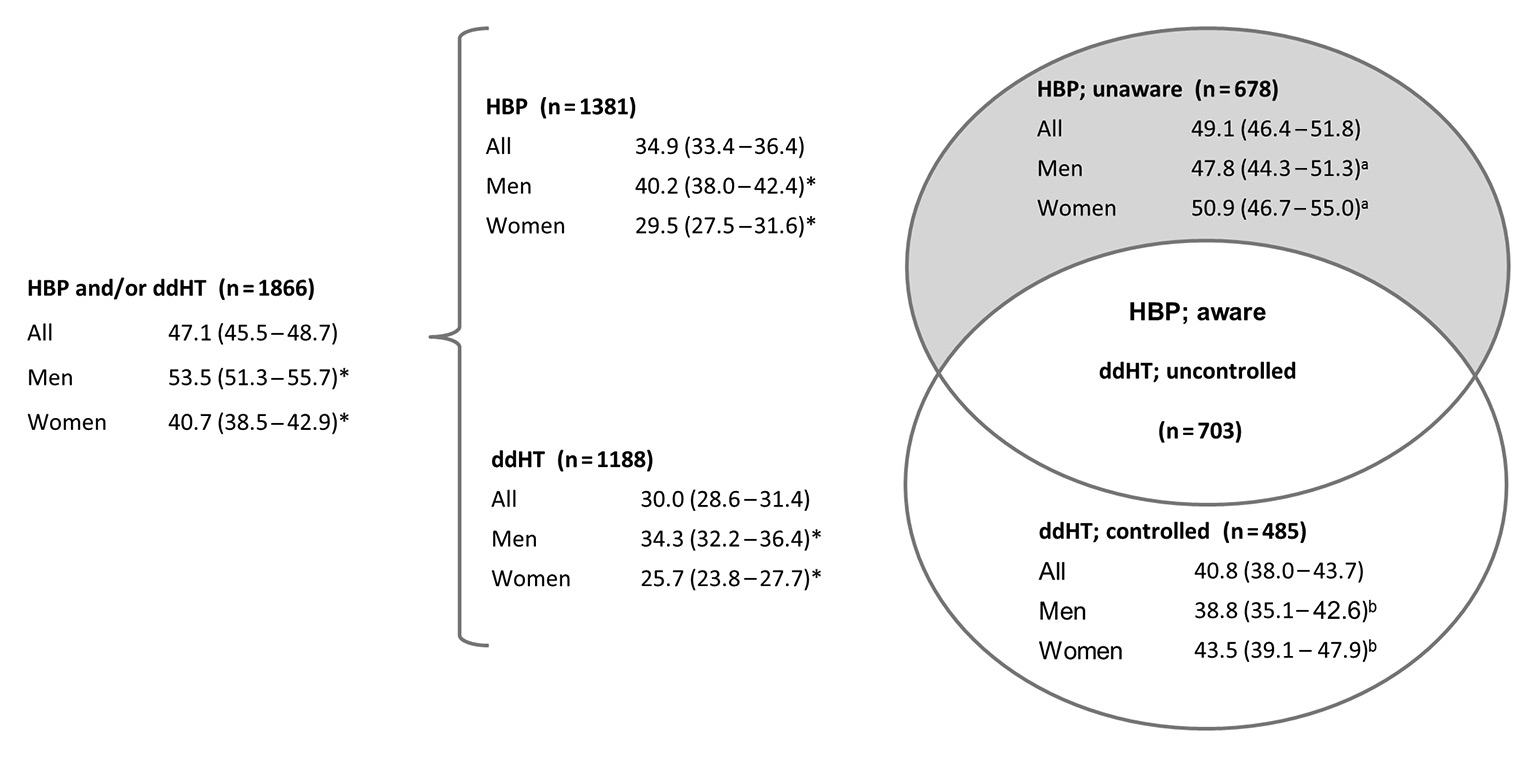
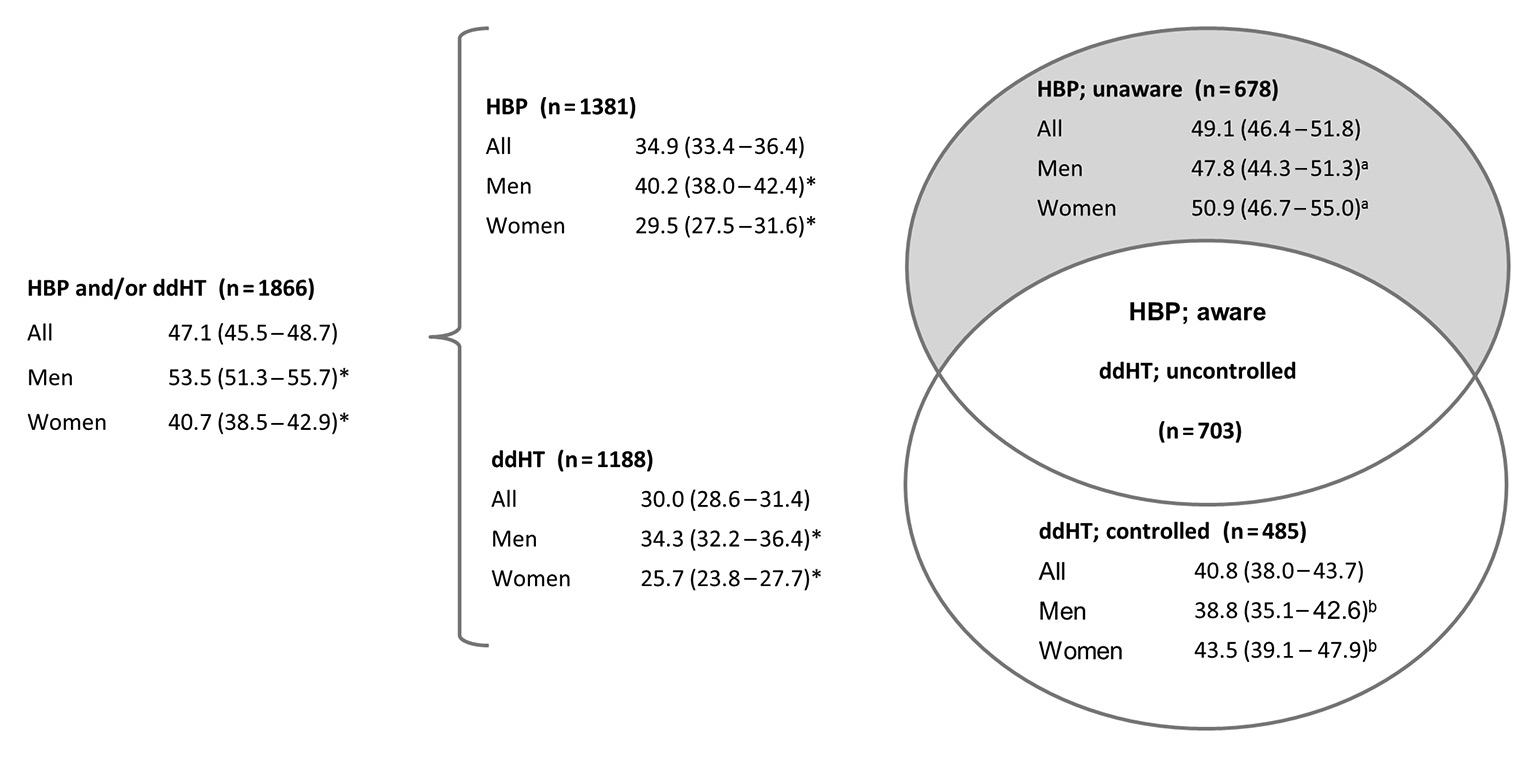
Figure 1
Prevalence of high blood pressure and doctor-diagnosed hypertension, stratified by gender (% [95%CI])
p-values for sex differences determined with chi-squared tests, * p <0.001, a p = 0.262, bp = 0.104
CI = confidence interval; ddHT = doctor diagnosed hypertension; HBP = high blood pressure
High blood pressure and hypertension; prevalence, awareness, and control
Of the 3986 participants, 34.9% had HBP (blood pressure ≥140/90) and 30.0% had ddHT. These two groups overlapped to some degree resulting in 47.1% having HBP and/or ddHT. Of those with HBP, 49.1% did not report a diagnosis of hypertension, and were therefore considered unaware, representing 17.1% of the analytical sample as a whole. Of those with ddHT, 59.2% had HBP and were therefore considered to have uncontrolled ddHT. Prevalence of HBP, ddHT, and HBP and/or ddHT was statistically significantly higher in men than in women (p <0.001). Prevalence data including sex differences are described in figure 1. Even after controlling for age, lifestyle score, presence of concomitant cardiovascular or metabolic disease, language, education level, degree of urbanisation and neighbourhood level socioeconomic level, men were more likely to have HBP (odds ratio [OR] 1.59, 95% confidence interval [CI] 1.38–1.85, p <0.001) and ddHT (OR 1.38, 95% CI 1.18–1.62, p <0.001).
Systolic blood pressure ≥160 and/or diastolic blood pressure ≥100 mm Hg was found in 19.5%, 33.0%, 27.0% and 20.8% of those with ddHT, uncontrolled ddHT, HBP and HBP unawareness, respectively. These blood pressure values correspond to grade 2 or 3 hypertension. Detailed distribution of blood pressure severity in these groups is described in table 2.
|
Table 2:Distribution of blood pressure measurements, by hypertension- or high blood pressure-group (data are proportion of group with 95% confidence interval). |
|
Blood pressure
(mm Hg)
|
In those with ddHT
(n = 1188)
|
In those with uncontrolled ddHT
(n = 703)
|
In those with HBP
(n = 1381)
|
In those unaware of their HBP
(n = 678)
|
| Normal
<140/90 |
40.8
(38.1–43.7) |
– |
– |
– |
| Grade 1*
140–159 / 90–99 |
39.6
(36.9–42.5) |
67.0
(63.4–70.4) |
73.0
(70.6–75.3) |
79.2
(76.0–82.1) |
| Grade 2*
160–179 / 100–109 |
15.5
(13.5–17.7) |
26.2
(23.0–29.6) |
21.8
(19.7–24.1) |
17.3
(14.6–20.3) |
| Grade 3*
≥180/110 |
4.0
(3.1–5.3) |
6.8
(5.2–9.0) |
5.2
(4.2–6.5) |
3.5
(2.4–5.2) |
| ddHT = doctor diagnosed hypertension; HBP = high blood pressure
*Grades 1–3 represent systolic blood pressure and/or diastolic blood pressure within the respective ranges. Participants were allocated to a group based on highest level of blood pressure, be it systolic or diastolic. |
Determinants of high blood pressure unawareness
A multivariable logistic regression with HBP unawareness as outcome was adjusted for age, sex, SAPALDIA 2 systolic blood pressure, presence of concomitant cardiovascular or metabolic disease, language, education level, degree of urbanisation, neighbourhood socioeconomic status and lifestyle score. Those more likely to be unaware of HBP were men (OR 1.42, 95% CI 1.09–1.86, p = 0.010), younger participants (OR 0.88 per 10-year increase, 95% CI 0.78–1.00, p = 0.047), those with lower systolic blood pressure (OR 0.90 per 2-mm Hg increase, 95% CI 0.88–0.92, p <0.001 ), those without concomitant cardiovascular disease (OR 2.35, 95% CI 1.82–3.02, p <0.001 ), those with lower neighbourhood-level socioeconomic status (OR 0.86 per 10-point increase, 95% CI 0.75–0.99, p = 0.031) and those with higher lifestyle score (OR 1.36 per point increase, 95% CI 1.19–1.55, p <0.001).
Target blood pressure and determinants of uncontrolled hypertension
Based on our blood pressure measurements, the general target blood pressure of <140/90 mm Hg was reached by 40.8% of the 1188 participants with ddHT. Of the 232 participants with ddHT and diabetes or kidney disease, only 23.7% (18.6–29.7%) reached the treatment goal of <130/80 mm Hg.
A multivariable logistic regression with uncontrolled ddHT as outcome was adjusted for age, sex, SAPALDIA 2 systolic blood pressure, presence of concomitant cardiovascular or metabolic disease, lifestyle score, language, education level, degree of urbanisation and neighbourhood-level socioeconomic status. More likely to have uncontrolled ddHT were those with higher SAPALDIA 2 systolic blood pressure (OR 1.08 per 2-mm Hg increase, 95% CI 1.06–1.10, p <0.001), and those with lower lifestyle score, though only with borderline statistical significance (OR 0.88 per point increase, 95% CI 0.77–1.00, p = 0.057).
Outcomes of high blood pressure, unawareness and uncontrolled hypertension
To determine the outcomes of HBP, HBP unawareness and uncontrolled ddHT and to evaluate possible overestimation of HBP due to the white coat effect (blood pressure measurements only being available from the study centre visits), we assessed the 10-year morbidity in the respective groups from SAPALDIA 2. Controlling for age and sex, the OR for developing angina pectoris during the SAPALDIA 2–3 interval in those with HBP compared with those with normal blood pressure in SAPALDIA 2 was 2.2 (1.2–4.1, p = 0.013). Similarly, ORs for developing myocardial infarction, heart failure, stroke and any of these four cardiovascular diseases were 3.3 (1.8–6.0, p <0.001), 2.5 (1.3–4.7, p = 0.004), 1.7 (0.9–3.2, p = 0.088) and 2.2 (1.6–3.1, p <0.001), respectively. Adjusted for age and sex, the ORs of developing cardiovascular outcomes during the SAPALDIA 2–3 interval in those unaware compared with those aware of their HBP at SAPALDIA 2 were for some outcomes higher than one and for some lower than one but never reached statistical significance. In contrast, after adjusting for age and sex, the ORs of developing angina pectoris, myocardial infarction, heart failure or stroke during the SAPALDIA 2–3 interval were higher than one in those with uncontrolled compared to those with controlled ddHT at SAPALDIA 2, although not reaching statistical significance.
Hypertension pharmacotherapy
Overall, 82.1% of the 1188 participants with ddHT took blood pressure-lowering agents, 42.3% of these took one drug, 36.3% took two and 21.4% took three or more. Of those taking at least two, 65.0% used a combined fixed dose preparation. When compared with subjects with drug-treated ddHT, those with non-drug-treated ddHT had higher lifestyle scores (Wilcoxon rank-sum p = 0.030), and higher mean systolic blood pressure (147.9 mm Hg [145.5–150.3] compared with 142.6 mm Hg [141.5–143.8]) and diastolic blood pressure (87.7 mm Hg [86.4–89.0] compared with 81.3 mm Hg [80.6–82.0], p ≤0.001).
Beta-blockers as a first-line drug
Though the Swiss Society of Hypertension did not recommend beta-blockers as a first-line drug, except in the presence of some comorbidities, 100 (24.2%, 20.4–28.7%) of the 412 hypertensive participants on monotherapy took beta-blockers. Providing possible explanations, 8.0% had coronary heart disease, 1.0% had heart failure, 9.0% had atrial fibrillation, 7.0% had diabetes, 16.0% had migraines and 34.0% had at least one of the above listed comorbidities. First-line beta-blocker prescription did not vary by age (p = 0.385).
Comorbidity specific treatment
Antihypertensive drug classes recommended on the basis of comorbidity as well as the distribution of guideline adherence are described in table 3. Of those with drug treated ddHT and dyslipidaemia (n = 406), 18.2% were taking neither ACEIs, ARBs nor calcium antagonists, despite recommendations. Only 33.8% of this seeming guideline nonadherence could be explained by the presence of other comorbidities where beta-blockers or diuretics were permitted or are commonly prescribed (coronary heart disease, heart failure, atrial fibrillation, diabetes, migraines or kidney disease). Beta-blockers were prescribed in 8 (19.5%) individuals with both asthma and hypertension. All eight had asthma medication and in six the prescribed beta-blockers were cardioselective. Of the possible explanations for beta-blocker prescription (coronary heart disease, heart failure, migraines or atrial fibrillation), only one of these asthmatic participants had migraines and one had atrial fibrillation.
|
Table 3:Comorbidity-specific guideline adherence and nonadherence in those with drug treated, doctor-diagnosed hypertension (n = 975). |
|
Comorbidity (number of participants) and recommended drug classes
|
Only recommended drugs prescribed
n (%)
|
Mix of recommended and nonrecommended drugs prescribed
n (%)
|
Only nonrecommended drugs prescribed
n (%)
|
| Coronary heart disease (n = 86)
ACEI, ARB, BB, CA |
49 (57.0%) |
36 (41.9%) |
1 (1.2%) |
| Heart failure (n = 35)
ACEI, ARB, BB, diuretic |
25 (71.4%) |
8 (22.9%) |
2 (5.7%) |
| Diabetes (n = 156)
ACEI, ARB, BB, CA |
68 (43.6%) |
82 (52.6%) |
6 (3.8%) |
| Dyslipidaemia (n = 406)
ACEI, ARB, CA |
118 (29.1%) |
214 (52.7%) |
74 (18.2%) |
| Migraines (n = 73)
BB |
16 (21.9%) |
17 (23.3%) |
40 (54.8%) |
| Asthma (n = 41)
avoid BB |
33 (80.5%) |
5 (12.2%) |
3 (7.3%) |
| ACEI = angiotensin converting enzyme inhibitor; ARB = angiotensin II receptor blocker; BB = betablocker; CA = calcium antagonist; ddHT = doctor-diagnosed hypertension |
Discussion
High blood pressure and hypertension: prevalence, awareness and control
In this analysis from the population-based SAPALDIA cohort 50% had either ddHT or blood pressure ≥140/90. Thirty percent had ddHT, among whom 60% had uncontrolled ddHT. Some uncontrolled ddHT may reflect a white coat effect or may have been intentional, accounting for orthostatic hypotension. Still, rates of uncontrolled HBP were high and the distribution of blood pressure severity was equally surprising, as 21% of those unaware of their HBP had measurements ≥160/100 mm Hg. Furthermore, recent research indicates that the 140 mm Hg target is not low enough; a 120 mm Hg target results in significantly lower cardiovascular mortality and morbidity in nondiabetic patients without previous stroke but at high risk of cardiovascular events [17]. The association of both HBP and uncontrolled ddHT with long-term cardiovascular outcomes reinforces the validity of our measurements and underlines the importance of early diagnosis and proper treatment. Similar odds of cardiovascular outcomes between those aware and unaware of their HBP were expected as HBP is harmful regardless of having a diagnosis or not.
After definitions were harmonised, our results were comparable to other Swiss data on hypertension prevalence, awareness and control [3, 7, 18] (see supplementary table S2). When comparing age-specific harmonised definitions from our study and 2009–2010 US data [19], we found that the prevalence of HBP and/or antihypertensive drug intake were similar, whereas awareness and control were respectively 20.0–37.4% and 23.8–34.4% lower in our data (see supplementary table S3). This is consistent with the literature which shows lower awareness and control in Europe compared to the USA [20–22].
In the current study, we assessed the prevalence, determinants and outcomes of HBP (defined as blood pressure ≥140/90 mm Hg) and hypertension as diagnosed by a doctor. The white coat effect, which should be excluded by performing 24-hour or home blood pressure measurement, and masked hypertension may have led to respectively over- or underestimation of HBP. Because of their long-term participation in SAPALDIA, our sample may be healthier and more compliant than the general population. Our results might thus underestimate the true population prevalence of diagnosed or undiagnosed hypertension. On the other hand, our blood pressure values are the mean of two measurements from a single visit and may overestimate an individual’s usual blood pressure [23]. Still, 140/90 remains an arbitrary cut-off across a spectrum of above-normal blood pressure within which cardiovascular risk increases [24]. Approximately 50% of DALYs attributed to above-normal blood pressure occur below this 140/90 cut-off [5].
Groups at higher risk
Identifying groups at higher risk for HBP unawareness and uncontrolled ddHT is challenging; accordingly, the results from the literature differ. In our study, younger age, male sex, healthier lifestyle, lower neighbourhood-level socioeconomic status and lower SAPALDIA 2 systolic blood pressure were associated with HBP unawareness. Uncontrolled hypertension was associated with higher SAPALDIA 2 systolic blood pressure. These findings are, in part, echoed in studies from Switzerland and elsewhere [7, 8, 19]. Differences in healthcare utilisation, drug prescription or adherence trends may explain these results, although we were unable to asses this in the current study.
Pharmacotherapy
High rates of uncontrolled hypertension despite high treatment rates might be explained by the complexity of clinical situations, or by physicians’ inertia in changing drugs or increasing dose even when blood pressure targets remain unmet as previously described in Switzerland [25]. Also, drug compliance is challenging because hypertension is chronic and often asymptomatic. In some cases fixed-combination antihypertensive preparations may be preferred to remedy this issue [10].
Several practical challenges arise in aligning pharmacotherapy to guidelines. Guidelines differ worldwide, and several documents potentially influence practitioners in a given country. Even within one document, conflicting recommendations may apply to the same individual. Also, drug choice is influenced by efficacy, tolerance, security and price. Lastly, antihypertensive drugs are used in the treatment of other conditions independently of hypertension. These elements may explain some of the seeming guideline nonadherence.
In our analysis, nonadherence was particularly high regarding beta-blockers. The Swiss Society of Hypertension did not recommend beta-blockers as first-line drugs since studies report them to be ineffective in reducing stroke and coronary heart disease and to have negative effects on lipid and glucose metabolism [26]. Similarly, US and UK guidelines [11, 12] did not generally encourage beta-blockers as first-line drugs. However, the European Society of Hypertension guidelines considered beta-blockers as appropriate for initial treatment [10, 27]. Since 24.2% of first-line drugs in our data were beta-blockers and their prescription remained largely unexplained by comorbidities, Swiss doctors were possibly unaware of the Swiss Society of Hypertension recommendation or were following European guidelines.
In the recommendation to avoid beta-blockers when asthma is present, the Swiss Society of Hypertension does nuance the statement [26]. However, a recent review recommends prudence, even when using cardioselective beta-blockers in hypertensive asthmatics [28]. Twenty percent of asthmatics with hypertension were receiving beta-blockers (mainly cardioselective), but clear indications for beta-blocker treatment were not evident in our data.
Needed action in hypertension management
While there is room for improvement in overall guideline adherence, one main concern is the high prevalence of uncontrolled hypertension. A European-wide survey, including Switzerland, showed that physicians underestimate their role in unmet blood pressure targets [29]. What should be done about guideline nonadherence, particularly in regard to unmet blood pressure goals? Redon et al. propose some practical solutions: increasing both awareness of the harmful nature of hypertension and patient accountability and simplifying treatment with combined preparations [30].
Strengths and limitations
Participants in the SAPALDIA cohort are characterised in great detail and reflect the geographical and cultural diversity of Switzerland. Yet the Swiss health care system is highly fragmented and its organisation does not allow for efficient access to objective information on medical diagnoses and treatment. In this study, diagnoses and medication intake were self-reported. The study was not designed to address particularly the issue of uncontrolled hypertension, so information on regularity of blood pressure measurements, drug compliance, or reasons for nonadherence to medical recommendations is lacking. Therefore we cannot fully explain the observed unawareness and noncontrol of hypertension; however, their high prevalence is unlikely to be due to bias or participant behaviour alone.
Conclusions
Prevalence of HBP, ddHT, HBP unawareness and uncontrolled ddHT were high. Nonadherence to comorbidity-specific drug prescription guidelines remained high and largely unexplained, particularly concerning the use of beta-blockers as first-line drugs. For HBP, a major cardiovascular risk factor, there is still room for substantial improvement from prevention to diagnosis, treatment and control, even in Switzerland, a high-income country. Our results underline the value of population-based cohorts for the identification and characterisation of potential unmet needs in healthcare practice. To further improve the value of these cohorts, it would be essential to facilitate efficient linkage of cohort data to medical records.
Figure S1
Selection of study population.
BP = blood pressure; SAPALDIA = Swiss Cohort Study on Air Pollution and Lung and Heart Disease in Adults.
|
Table S1:Characteristics of included and excluded participants at baseline, and first and second follow up. |
|
|
SAPALDIA 1
included
|
SAPALDIA 1
excluded
|
p-value
|
SAPALDIA 2
included
|
SAPALDIA 2
excluded
|
p-value
|
SAPALDIA 3
included
|
SAPALDIA 3
excluded
|
p-value
|
|
Participants
|
3962 |
5689 |
|
3962 |
4085 |
|
3962 |
2126 |
|
| Men |
1984 (50.1%) |
2761 (48.5%) |
0.136 |
1984 (50.1%) |
1883 (46.1%) |
<0.001 |
1984 (50.1%) |
913 (42.9%) |
<0.001 |
| Age years (IQR) |
41.2 (31.6, 48.9) |
42.2 (32.1, 51.6) |
0.003 |
52 (42.5, 59.8) |
53.5 (43.7, 62.8) |
<0.001 |
60.4 (50.9, 68.0) |
60.1 (50.5, 69.5) |
0.447 |
| German-speaking
French-speaking
Italian-speaking |
2148 (54.2%)
1267 (32.0%)
546 (13.8%) |
2758 (48.5%)
2004 (35.2%)
925 (16.3%) |
<0.001 |
2148 (54.2%)
1267 (32.0%)
546 (13.8%) |
2106 (51.6%)
1317 (32.2%)
662 (16.2%) |
0.005 |
2150 (54.3%)
1278 (32.3%)
534 (13.5%) |
663 (55.9%)
351 (29.6%)
171 (14.4%) |
0.214 |
| Highest education
Primary
Secondary#
Tertiary |
424 (10.7%)
2753 (69.6%)
781 (19.7%) |
1199 (21.2%)
3644 (64.3%)
826 (14.6%) |
<0.001 |
168 (4.2%)
2559 (64.6%)
1235 (31.2%) |
534 (13.1%)
2698 (66.1%)
847 (20.8%) |
<0.001 |
168 (4.2%)
2559 (64.6%)
1235 (31.2%) |
246 (11.6%)
1421 (66.9%)
457 (21.5%) |
<0.001 |
| Neighbourhood-level socio-economic index (0- to 100-point scale) |
|
|
|
64.2 (57.5, 71.0) |
63.4 (55.6, 70.3) |
0.001 |
64.2 (57.5, 71.0) |
64 (56.4, 71.1) |
0.557 |
| Degree of urbanisation
High
Medium
Low |
|
|
|
1187 (30.0%)
2244 (56.8%)
523 (13.2%) |
1485 (37.1%)
2146 (53.6%)
370 (9.2%) |
<0.001 |
1121 (28.3%)
2277 (57.5%)
564 (14.2%) |
605 (30.0%)
1165 (57.8%)
246 (12.2%) |
0.065 |
|
Blood pressure
|
| Systolic BP, mm Hg (IQR) |
|
|
|
124.5 (112.5, 138.0) |
127 (114.0, 139.5) |
<0.001 |
131.5 (120, 144.5) |
131 (120.0, 143.5) |
0.748 |
| Diastolic BP, mm Hg (IQR) |
|
|
|
79.0 (72.0, 86.5) |
79.0 (72.0, 87.0) |
0.481 |
78.5 (72.0, 85.0) |
79.0 (72.0, 85.5) |
0.303 |
| HBP and/or ddHT |
|
|
|
1265 (31.9%) |
1090 (41.2%) |
<0.001 |
1866 (47.1%) |
724 (58.3%) |
<0.001 |
| HBP (BP ≥140/90)
Unaware |
|
|
|
1032 (26.0%)
677 (65.6%) |
728 (29.2%)
445 (61.1%) |
0.006
0.055 |
1381 (34.9%)
678 (49.1%) |
331 (34.8%)
173 (55.4%) |
0.977
0.043 |
| ddHT
Uncontrolled |
|
|
|
588 (14.8%)
355 (60.4%) |
645 (18.7%)
283 (58.4%) |
<0.001
0.502 |
1188 (30.0%)
703 (59.2%) |
532 (28.4%)
139 (58.6%) |
0.225
0.881 |
|
Lifestyle characteristics
|
| Never smokers
Former smokers
Current smokers |
1960 (49.5%)
945 (23.9%)
1052 (26.6%) |
2269 (39.9%)
1236 (21.7%)
2180 (38.3%) |
<0.001 |
1825 (46.1%)
1269 (32.0%)
868 (21.9%) |
1569 (38.5%)
1255 (30.8%)
1248 (30.6%) |
<0.001 |
1787 (45.1%)
1542 (38.9%)
633 (16.0%) |
859 (40.8%)
764 (36.3%)
480 (22.8%) |
<0.001 |
| Low risk alcohol consumption
≤1 glass/day in women
≤2 glasses/day in men |
|
|
|
1916 (96.9%)
1701 (85.7%) |
690 (94.0%)
460 (87.5%) |
0.118 |
1910 (96.6%)
1759 (88.2%) |
560 (96.2%)
456 (89.8%) |
0.340 |
| Fruit and vegetable intake ≥5/day |
|
|
|
867 (21.9%) |
530 (20.3%) |
0.132 |
916 (23.1%) |
243 (22.1%) |
0.464 |
| Sufficient physical activity |
|
|
|
2913 (73.5%) |
1745 (67.5%) |
<0.001 |
2967 (74.9%) |
707 (67.6%) |
<0.001 |
| BMI <25 kg/m2
≥25 to <30 kg/m2
≥30 kg/m2
|
2773 (70.1%)
1002 (25.3%)
178 (4.5%) |
3528 (63%)
1581 (28.2%)
490 (8.8%) |
<0.001 |
1934 (48.8%)
1472 (37.2%)
556 (14.0%) |
1132 (42.9%)
1001 (38.0%)
503 (19.1%) |
<0.001 |
1669 (42.1%)
1568 (39.6%)
725 (18.3%) |
395 (40.1%) 395 (40.1%) 194 (19.7%) |
0.437 |
|
Comorbidities (self-reported doctor-diagnosed)
|
| Angina pectoris |
|
|
|
66 (1.7%) |
62 (1.8%) |
0.721 |
82 (2.1%) |
39 (2.8%) |
0.103 |
| Myocardial infarct |
|
|
|
47 (1.2%) |
54 (1.5%) |
0.181 |
92 (2.3%) |
75 (4%) |
<0.001 |
| Heart failure |
|
|
|
47 (1.2%) |
40 (1.5%) |
0.233 |
61 (1.5%) |
64 (3.4%) |
<0.001 |
| Atrial fibrillation |
|
|
|
|
|
|
119 (3.0%) |
27 (2%) |
0.040 |
| Stroke |
|
|
|
41 (1.0%) |
48 (1.4%) |
0.164 |
68 (1.7%) |
24 (1.7%) |
0.953 |
| Dyslipidaemia |
|
|
|
339 (38.7%) |
94 (46.3%) |
0.045 |
994 (25.1%) |
375 (20.3%) |
<0.001 |
| Diabetes |
|
|
|
90 (2.3%) |
151 (4.4%) |
<0.001 |
282 (7.1%) |
162 (8.6%) |
0.044 |
| Asthma |
|
|
|
137 (3.5%) |
155 (3.8%) |
0.384 |
172 (4.3%) |
76 (3.7%) |
0.208 |
| Migraines |
|
|
|
289 (7.3%) |
276 (8.0%) |
0.267 |
289 (7.3%) |
138 (8.3%) |
0.182 |
| BMI = body mass index; BP = blood pressure; ddHT = doctor-diagnosed hypertension; HBP = high blood pressure; IQR = interquartile range (25th, 75th percentile)
# including apprenticeships
Data are presented as number and percent or median and interquartile range; p-values were obtained with median tests or chi-squared tests. The number for comparison was minimum 1073, due to missing information. |
|
Table S2:Comparison of hypertension prevalence between SAPALDIA 3 and other Swiss data. |
|
|
SAPALDIA 3 2010–2011
Percent (95% CI)
|
Other Swiss data
Percent (95% CI)
|
|
Prevalence ddHT
|
30.0 (28.6–31.4) |
27#
|
|
Prevalence of HT:HBP and/or taking antihypertensive drugs |
48.5 (46.9–50.0) |
36 (35–38)* |
|
Awareness: those with ddHT among those with HBP and/or taking antihypertensive drugs |
58.7 (56.4–60.8) |
63 (61–65)* |
|
Control: those with BP<140/90 among those with HBP and/or taking antihypertensive drugs |
28.0 (26.1–30.1) |
23 (21–25)* |
| Here definitions of “hypertension”, “awareness” and “control” were adopted from the CoLaus study.
# Swiss Health Survey 2012, aged 15–75+ years [1]
* CoLaus 2003–2006, aged 35–75 years [2] SAPALDIA 3 participants were aged 37–81 years
BP = blood pressure; CI = confidence interval; ddHT = doctor-diagnosed hypertension; HT = hypertension; HBP = high blood pressure (blood pressure ≥140/90 mm Hg) |
|
Table S3: Prevalence comparison between SAPALDIA 3 and United States data. |
| |
Age strata (years)
|
SAPALDIA 3
2010–2011
Percent (95% CI)
|
United States
NHANES [3] 2009–2010
Percent (95% CI)
|
|
Prevalence:HBP and/or taking antihypertensive drugs |
40–59
60+ |
32.2 (30.1–34.5)
65.3 (63.2–67.3) |
30.3 (26.3–34.3)
66.7 (63.1–70.2) |
|
Awareness: those with ddHT among those with HBP and/or taking antihypertensive drugs |
40–59
60+ |
46.7 (42.6–50.8)
64.0 (61. –66.6) |
84.1 (80.4–87.7)
84.0 (80.8–87.1) |
|
Control: those with BP<140/90 among those with HBP and/or taking antihypertensive drugs |
40–59
60+ |
21.3 (18.1–24.8)
31.1 (28.6–33.6) |
55.7 (51.0–60.5)
54.9 (50.9–58.9) |
| Here definitions of “awareness” and “control” were adpoted from the NHANES.
BP = blood pressure; CI = confidence interval; ddHT = doctor-diagnosed HT; HBP = high blood pressure (blood pressure ≥140/90 mm Hg); NHANES = National Health and Nutrition Examination Survey. |
References
1 Storni M, Kaeser M, Lieberherr R. Swiss Health Survey 2012 Overview. Federal Statistical Office; 2013:1-31. http://www.bfs.admin.ch/bfs/portal/en/index/news/publikationen.html?publicationID=5355. Accessed July 17, 2015.
2 Danon-Hersch N, Marques-Vidal P, Bovet P, Chiolero A, Paccaud F, Pécoud A, Hayoz D, Mooser V, Waeber G, Vollenweider P. Prevalence, awareness, treatment and control of high blood pressure in a Swiss city general population: the CoLaus study. Eur J Cardiovasc Prev Rehabil. 2009;16:66–72.
3 Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606.
Acknowledgments:Many thanks to the study participants, technical, administrative and medical teams, field workers and the SAPALDIA team, without whom this study would not have been possible.
References
1 Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–60.
2 Table of key indicators for all the Member States; WHO Global Health Expenditure Database. [Internet] WHO. 2014 – [cited 2015 Sep 16]. Available from: http://apps.who.int/nha/database/Key_Indicators/Index/en.
3 Storni, Marco, Kaeser, Martine, Lieberherr, Renaud. Swiss Health Survey 2012 Overview. Neuchâtel: Federal Statistical Office (CH); 2013 Feb. 31p.
4 GBD Compare, IHME. (n.d.). http://viz.healthmetricsandevaluation.org/gbd-compare/ (accessed 2015 July 16,).
5 Lawes CMM, Vander Hoorn S, Law MR, Elliott P, MacMahon S, Rodgers A. Blood pressure and the global burden of disease 2000. Part II: estimates of attributable burden. J Hypertens. 2006;24(3):423–30.
6 Zellweger U, Bopp M, Holzer BM, Djalali S, Kaplan V. Prevalence of chronic medical conditions in Switzerland: exploring estimates validity by comparing complementary data sources. BMC Public Health. 2014;14:1157.
7 Danon-Hersch N, Marques-Vidal P, Bovet P, Chiolero A, Paccaud F, Pécoud A, et al. Prevalence, awareness, treatment and control of high blood pressure in a Swiss city general population: the CoLaus study. Eur J Cardiovasc Prev Rehabil. 2009;16(1):66–72.
8 Guessous I, Bochud M, Theler J-M, Gaspoz J-M, Pechère-Bertschi A. 1999–2009 Trends in prevalence, unawareness, treatment and control of hypertension in Geneva, Switzerland. PloS One. 2012;7(6):e39877.
9 Swiss Society of Hypertension Guidelines [Internet]. Swiss Society of Hypertension. [cited 2015 May 20]. Available from: http://www.swisshypertension.ch/guidelines.htm.
10 Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013;31(7):1281–357.
11 National Clinical Guideline Centre (UK). Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34 [Internet]. London: Royal College of Physicians (UK); 2011 [cited 2015 Oct 8]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK83274/.
12 James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
13 Martin BW, Ackermann-Liebrich U, Leuenberger P, Künzli N, Stutz EZ, Keller R, et al. SAPALDIA: methods and participation in the cross-sectional part of the Swiss Study on Air Pollution and Lung Diseases in Adults. Soz- Präventivmedizin. 1997;42(2):67–84.
14 Panczak R, Galobardes B, Voorpostel M, Spoerri A, Zwahlen M, Egger M, et al. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health. 2012;66(12):1129–36.
15 Swiss Society of Hypertension. Arterial hypertension, recommendations for doctors. Swiss Society of Hypertension (CH); 2009.
16 Marthaler M. Risques de maladies et de mortalité liés à l’alcool Bases pour des repères de consommation d’alcool à faible risque [Internet]. Addiction Suisse; 2013 [cited 2015 Jul 6]. Available from: http://www.bag.admin.ch/themen/drogen/00039/00594/11232/index.html?lang=fr
17 SPRINT Research Group. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015;373(22):2103–16.
18 Brenner R, Waeber B, Allemann Y. Medical treatment of hypertension in Switzerland. The 2009 Swiss Hypertension Survey (SWISSHYPE), Swiss Med. Wkly. 141 (2011) w13169.
19 Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60(7):599–606.
20 Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22(1):11–9.
21 Wang YR, Alexander GC, Stafford RS. Outpatient hypertension treatment, treatment intensification, and control in Western Europe and the United States. Arch Intern Med. 2007;167(2):141–7.
22 Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10–7.
23 Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–23.
24 Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–13.
25 Ferrari P, Hess L, Pechere-Bertschi A, Muggli F, Burnier M. Reasons for not intensifying antihypertensive treatment (RIAT): a primary care antihypertensive intervention study. J Hypertens. 2004;22(6):1221–9.
26 Erne, P, Allemann, Y. Comments to the 2007 recommendations for the treatment of essential hypertension by the Swiss Society of Hypertension. Cardiovasc Med. 2008;11(1):26–8.
27 Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009;27(11):2121–58.
28 Self TH, Wallace JL, Soberman JE. Cardioselective beta-blocker treatment of hypertension in patients with asthma: when do benefits outweigh risks? J Asthma. 2012;49(9):947–51.
29 Erdine S, Redon J, Böhm M, Ferri C, Kolloch R, Kreutz R, et al. Are physicians underestimating the challenges of hypertension management? Results from the Supporting Hypertension Awareness and Research Europe-wide (SHARE) survey. Eur J Prev Cardiol. 2013;20(5):786–92.
30 Redon J, Brunner HR, Ferri C, Hilgers KF, Kolloch R, van Montfrans G. Practical solutions to the challenges of uncontrolled hypertension: a white paper. J Hypertens Suppl. 2008;26(4):S1–14.