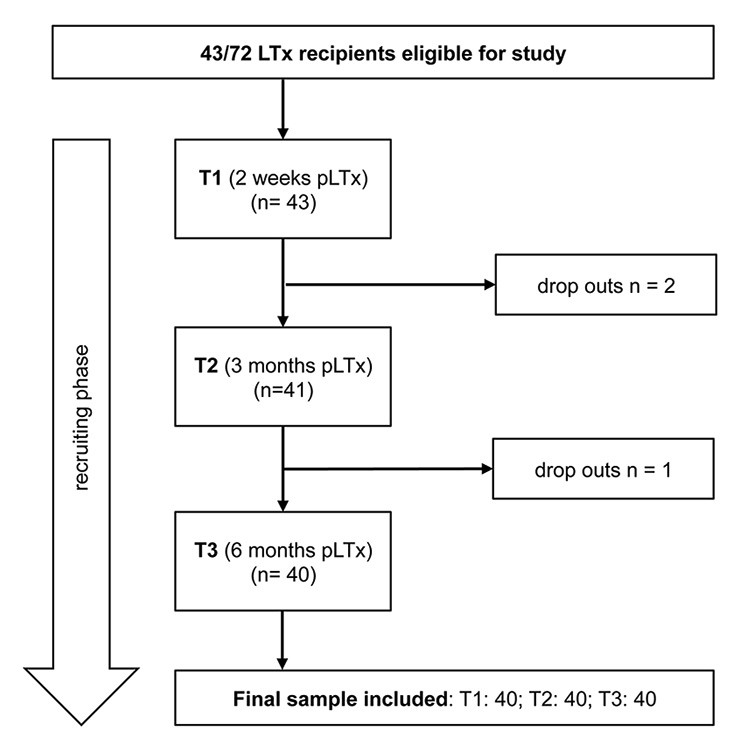
Figure 1
Patient recruitment.
LTx = lung transplantation; pLTx = post lung transplantation; T1–T3 = three measurement time-points.
DOI: https://doi.org/10.4414/smw.2015.14236
A 6-months observational study
Abbreviations
ANOVA analysis of variance
ECMO extracorporeal membrane oxygenation
EQ-5D EuroQOL five-dimension health-related quality of life questionnaire
FEV1 forced expiratory volume in one second
HRQoL health-related quality of life
ICU intensive care unit
IPF interstitial pulmonary fibrosis
ISHLT International Society for Heart and Lung Transplantation
LOS length of hospital stay
SCL-K-9 Symptom Checklist short version-9
SF-36 Short Form Health Survey
Lung transplantation is an established therapeutic option for end-stage lung disease, yielding successful outcomes in carefully selected patients characterised by reduced disability, extended survival and improved health-related quality of life (HRQoL) [1–3]. To date, more than 47 000 adult lung transplants have been reported worldwide to the Registry of the International Society for Heart and Lung Transplantation (ISHLT) [4], while in Switzerland more than 700 lung transplants have been performed since 1992 [5]. During the last 20 years, overall patient survival has progressively improved. From January 2000 to December 2011, a total of 240 lung transplants were performed at the Zurich University Hospital with one-, three-, and five-year survival rates of 87%, 75% and 69%, respectively, comparable to results of international high-volume programmes [6]. In Switzerland, there are two transplant centres performing lung transplantations (University Hospital of Zurich and University Hospital of Lausanne). The annual number of lung transplantations in 2014 was 24 at the transplant centre in Lausanne and 34 in Zurich [7].
To date, studies on psychosocial outcomes following transplantation have primarily compared the post-operative HRQoL trajectories of different types of solid organ transplantation [8–10]. In these studies, recipients of different solid organ transplants did not share the same HRQoL trajectories. In particular, the HRQoL outcomes of lung transplant recipients appeared to be inferior to those receiving other solid organs [9, 11]. Interestingly, most studies looked at the entire group, and did not distinguish between patients with improved postoperative HRQoL and patients with similar or worse quality of life compared with their pretransplant scores.
Understanding the predictive impact of psychosocial and medical variables on post-operative HRQoL could be useful when making choices regarding therapy. Although previous research has identified associations between psychosocial and medical characteristics and post-transplant HRQoL, the predictors of post-transplant HRQoL are still not well described for lung transplant patients. There is a paucity of consistent data regarding predictive factors for post-transplant HRQoL [12]. In general, studies on predictors of post-transplant HRQoL in lung recipients demonstrate that bronchiolitis obliterans syndrome, the most common form of chronic lung allograft dysfunction, the adverse effects of immunosuppressant medications, and pain significantly reduce HRQoL and increase depressive symptoms [13–15]. In contrast, results on other potential outcome predictors – including age, gender, psychiatric history, longer waiting times for transplantation and forced expiratory volume in one second (FEV1) – have been contradictory and supported only by single studies [1, 16-18].
In light of the above, it is of clinical relevance to assess the psychosocial health of lung transplant patients to identify those at risk for unfavourable postoperative outcomes and to make more informed therapeutic choices to enhance patients’ symptom experience. The main objectives of the current study were therefore: (1) to determine outcome clusters of post-transplant psychological distress and HRQoL of lung transplant recipients over the first 6 months after lung transplantation; (2) to identify those lung recipients with poor postoperative outcomes; and (3) to assess potential short-term predictors and their impact upon psychological distress and HRQoL. This subject has clinical relevance with respect to the treatment of patients who undergo lung transplantation but fail to experience any improved quality of life.
Between January 2012 and April 2014, 72 lung transplants were performed at the Transplant Centre at the University Hospital of Zurich, Switzerland. All patients who received transplants over this time period were considered to be eligible for inclusion, unless they were: (1) younger than 18 years of age, (2) unable or unwilling to provide informed consent, or (3) unable or unwilling to complete questionnaires in German. Forty-three consecutive adult lung transplant recipients qualified for the study. During data collection, three subjects in total unexpectedly withdrew from participation for medical or personal reasons (e.g., feeling overwhelmed by hospital routines and preparations for discharge, distressed, overly-tired, and/or short of time). One of these three patients had to be excluded owing to a critical health condition and repeated hospitalisations in the intensive care unit (ICU). The final sample included 40 patients (fig. 1).
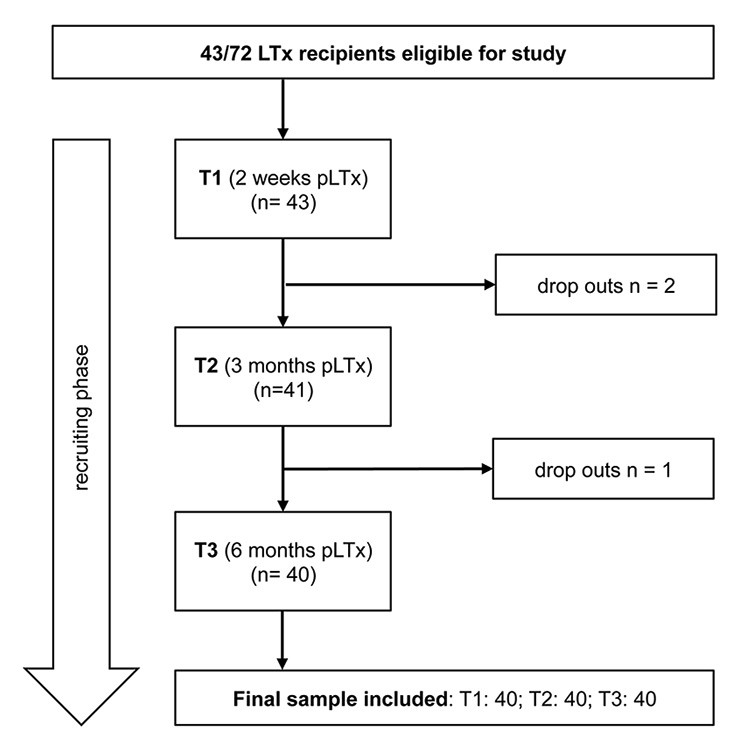
Figure 1
Patient recruitment.
LTx = lung transplantation; pLTx = post lung transplantation; T1–T3 = three measurement time-points.
In this prospective, longitudinal study, 40 lung transplant recipients were examined at three different measurement time-points (T1: 2 weeks; T2: 3 months; T3: 6 months after transplantation) to capture specific types of outcome clusters in terms of psychological distress and HRQoL over the first 6 postoperative months. Following approval by the Ethics Committee of the Canton of Zurich, Switzerland, all patients provided written informed consent prior to their participation. Eligible patients were asked to complete the same battery of questionnaires at every data collection point. The initial assessment at T1 was performed during hospitalisation, and the follow-up assessments at T2 and T3 typically were conducted during regular transplant clinic out-patient visits at the University Hospital Zurich. Few patients were still hospitalised or admitted to hospital because of complications at T2 or T3. Demographic and medical data were retrieved from patient medical records. Medical data included the underlying diagnosis/indication for transplantation, the presence of comorbid conditions, the time on the waiting list, the number of days spent in the ICU after transplantation, the length of hospital stay (LOS), treatment with antidepressants, and the mortality rate over the course of the data collection phase.
The German version of the Symptom Checklist-Short form (SCL-K-9) was used to assess overall psychological distress [19]. The SCL-K-9 [20] is comprised of nine items, each rated on a five-point Likert scale ranging from 0 (not at all) to 4 (very strong). According to the original global severity index, a mean score (0–4) for the nine items was computed, with higher values indicating greater distress (the community-based standard value = 0.41). The SCL-K-9 is highly correlated with the original SCL-90-R [21] and offers similarly good psychometric properties and sensitivity to change, with a Cronbach’s alpha of 0.87. In our clinical sample, internal consistency of the SCL-K-9 over the three measurement points was good, with Cronbach’s alpha ranging from 0.75 to 0.84.
All study subjects completed the EQ-5D, a five-item self-administered survey instrument that measures HRQoL [22, 23]. The questionnaire covers five dimensions of health: (1) mobility, (2) self-care, (3) usual activities, (4) pain/discomfort, and (5) anxiety/depression. For each dimension, patients selected one of three graded responses, indicating no problems, some problems, or severe problems with the activity. A single global EQ-5D score (range 0–100) was generated by use of the sum model as describe by Hinz et al. [23] (community-based standard value = 91.7). The EQ-5D is used in studies to assess psychotherapeutic treatment, where it has been shown to be valid, sensitive to change, and responsive to improvements in mental health. In the current study, the EQ-5D demonstrated acceptable to good internal consistency over the three data collection points, with Cronbach’s alpha ranging between 0.60 and 0.76. The lower level of internal consistency observed across the different outcome measures might be explained by the high level of homogeneity in our clinical sample.
Additionally, we used a pretransplant comorbidity index developed by Barrios et al. [24], consisting of ten extrapulmonary comorbidities that may have negatively impacted short- and long-term postoperative trajectories. This comorbidity index included the following factors: (1) body mass index >30 kg/m2, (2) osteoporosis, (3) insulin-dependent diabetes, (4) arterial hypertension, (5) cardiac disease, (6) chronic liver disease, (7) diverticulosis, (8) gastroesophageal reflux, (9) history of malignancy, and (10) psychiatric disorders. The comorbidity index was computed by summing up the number of comorbidities for each patient. Values between 0 and 10 were possible.
The Statistical Package for the Social Sciences (SPSS, version 22.0) was used to perform all statistical analyses, with a two-tailed probability value of 0.05 considered statistically significant [25]. Descriptive statistics were reported as means and standard deviations, or as counts and percentages. Hierarchical cluster analysis was performed to identify different post-transplant outcome clusters related to psychological distress and HRQoL over the first 6 postoperative months based on six variables (SCL-K-9 global severity index and EQ-5D score measured at T1, T2 and T3). All these variables were standardised prior to clustering. Squared Euclidean distance as a proximity measure and Ward’s minimum variance agglomerative method were used [26]. The clustering process starts with the same number of clusters as cases, and reduces the number of clusters step-wise using dissimilarities or distances between objects, that is, combining those clusters whose combination results in a minimum increase in the total within-group sum of squares. If a point is reached whereby clusters are combined that are dissimilar, the within-group sum of squares noticeably increases (as can be seen in the agglomeration schedule). The number of clusters prior to this rapid increase in the agglomeration coefficient is considered the natural grouping scheme [27]. However, it must be taken into account that this analysis was exploratory in nature, and that the choice of the number of a cluster to extract is somewhat arbitrary. Patients’ characteristics were compared between the cluster groups using one-way analysis of variance (ANOVA), with Bonferroni post hoc test to identify statistically significant differences between specific cluster groups. Moreover, to generate some appreciation regarding the clinical significance of our results, effect sizes (Eta2 for interval scalded variables and Cramer’s V for categorical variables) were computed according to Cohen [28]. Values for Eta2 are categorised as small (0.01), intermediate (0.06), or large (0.14) while for Cramer’s V, a value of 0.1 is considered a small effect, 0.3 a medium effect and 0.5 a large effect. Pearson correlation coefficients were calculated to identify relevant predictor variables of psychological distress (SCL-K-9) and HRQoL (EQ-5D) 6 months post-transplant.
| Table 1: Demographic and medical data of lung transplant recipients. | |
| Variables | 40 LTx-Recipients n (%) |
| Male gender | 22 (55) |
| Median age (range) | 50 (20–68) |
| Education level Elementary Secondary Tertiary | 7 (17) 21 (53) 12 (30) |
| Married | 17 (43) |
| Indication for LTx | |
| COPD | 15 (38) |
| Cystic fibrosis | 13 (33) |
| Idiopathic pulmonary fibrosis | 7 (17) |
| Other | 5 (12) |
| ECMO use | 13 (33) |
| Bilateral LTx | 40 (100) |
| Retransplant | 2 (5) |
| Average time on wait list (d) | 270.5 (10–992) |
| Days in ICU (mean; range) | 4 (2–29) |
| Weeks in hospital pLTx (mean; range) | 4.5 (3–14) |
| COPD = chronic obstructive pulmonary disease; ECMO = extracorporeal membrane oxygenation; ICU = intensive care unit; LTx = lung transplantation; pLTx = post-transplant. | |
Detailed patient demographics and clinical characteristics are summarised in table 1. The main indication for lung transplantation in our clinical sample was chronic obstructive pulmonary disease (38%), followed by cystic fibrosis (33%). With respect to employment status, 45% were not working prior to transplant for health reasons, while 20% were already retired. Six months after transplantation, all 40 patients were still alive.
The agglomeration coefficients generated by cluster analysis revealed a demarcation point between three- and four-cluster solutions, suggesting that a four-cluster solution best distinguished the groups with regard to post-transplant psychological distress and HRQoL. However, a four- cluster solution produced one cluster with only two patients. For statistical reasons, we therefore decided on a three-cluster solution. An inspection of the clustering tree (dendrogram) indicated a three-cluster solution to be appropriate.
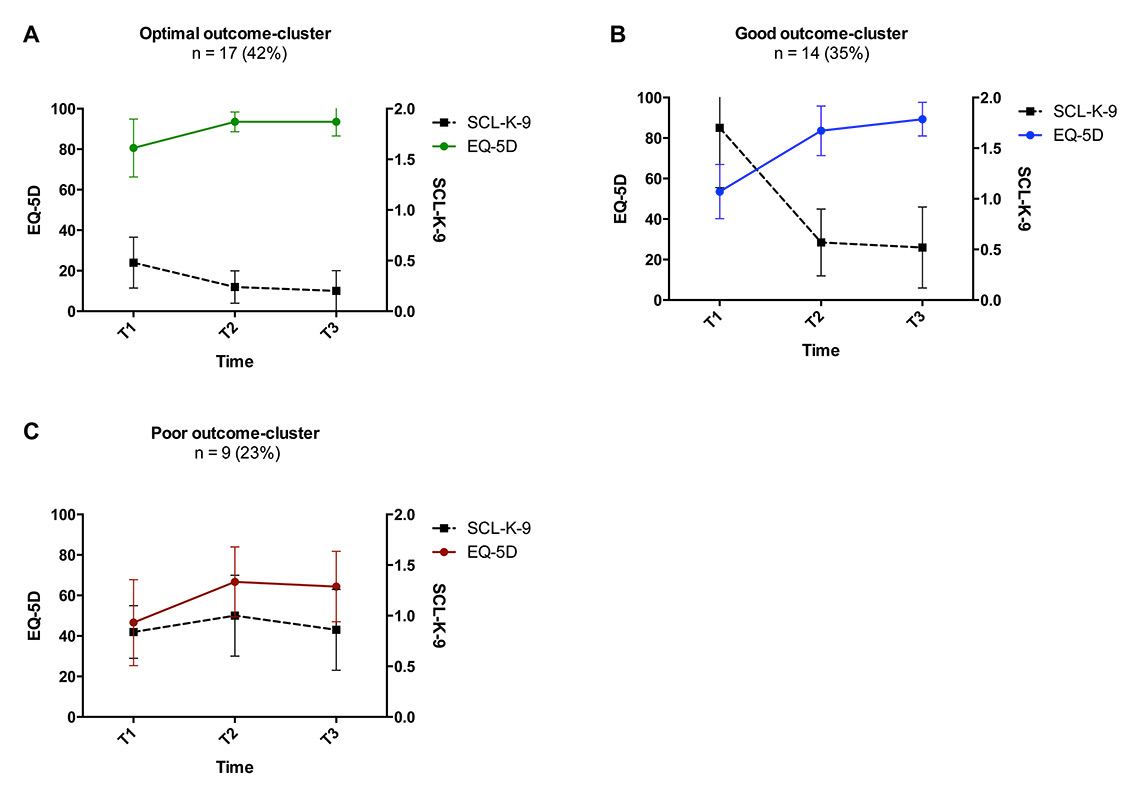
Figure 2
Post-transplant outcome clusters in lung transplant recipients.
Plots A–C illustrate postoperative outcome clusters after lung transplant determined by cluster analysis. The left y-axis represents mean values for EQ-5D, while the right y-axis represents mean values for global SLK-9 values. Higher values indicate higher EQ-5D or poorer SCL-K-9 values, respectively. T1–T3 stand for the three different measurement time points (T1: 2 weeks; T2: 3 months; T3: 6 months post-transplant).
EQ-5D = the EuroQOL five-dimension Health-Related Quality of Life questionnaire; SCL-K-9 =Symptom Checklist short version-9
The resultant three-cluster solution generated relatively well-sized groups related to psychological distress and HRQoL over T1 – T3, labelled according to their most distinguishing characteristics (fig. 2). Cluster characteristics are displayed in table 2. Cluster A included those patients with optimal postoperative outcomes over time (n = 17; 42%) in terms of a high EQ-5D and low SCL-K-9 scores within 2 weeks of surgery. EQ-5D further improved over the three data collection points and SCL-K-9 decreased progressively. At 6 months post-transplant, these patients reported HRQoL levels comparable to those of a community-based sample (EQ-5D value of 91.7) [23] and small but not significantly elevated SCL-K-9-values. Cluster B included transplant recipients with good post-operative outcomes over time (n = 14; 35%). In contrast to Cluster A, patients of Cluster B were characterised by considerably reduced EQ-5D and high SCL-K-9 scores 2 weeks after surgery, but significant improvements in EQ-5D and SCL-K-9 at 6 months. EQ-5D-values at 6 months of follow-up were slightly lower than those of the healthy normal population. Cluster C incorporated transplant recipients with poor post-operative outcomes over time (n = 9; 23%), with both a low EQ-5D and high SCL-K-9 score 2 weeks after transplantation, and only a small gain in EQ-5D while SCL-K-9 scores remained steadily elevated over the remainder of the first 6 months of follow-up.
For predictor analyses to distinguish the three groups of clusters, the following demographic, clinical and psychosocial characteristics were included: sex, age, underlying diagnosis, disease severity, time on the waiting list, extracorporeal membrane oxygenation (ECMO) use (pretransplant), comorbidities, number of days in the intensive care unit (ICU), length of stay (LOS), number of hospitalisations, number of infections, number of rejections and use of antidepressants within the first 6 months after lung transplant (table 3). The median comorbidity index value across the 40 patients was two and ranged between none and four comorbidities. Thirty-five percent of the transplant recipients suffered from three or more comorbidities. Significant intergroup differences were identified for LOS (Eta2 = 0.53), number of hospital admissions (Eta2 = 0.23) and use of antidepressants (Cramer’s V = 0.53) within the first 6 months after lung transplant, with large effect sizes. No significant cluster differences were evident for all other investigated variables. However, medium to large effect sizes were found for age (Eta2 = 0.07), disease severity (Eta2 = 0.13), comorbidities (Eta2 = 0.06), and number of days in ICU (Eta2 = 0.08), indicating that relative to patients of the optimal or good cluster groups, those with poor postoperative outcomes tended to be older, to suffer from considerably more severe disease, to have more comorbid conditions, and to have spent longer periods of time in the ICU and hospital. No meaningful intercluster differences were identified for patient gender, underlying diagnosis, time on waiting list, ECMO use prior to transplantation, or number of infections or rejections post-transplant.
Table 4 presents the results of correlation analyses used to identify associations between each potential outcome predictor and both the level of psychological distress (SCL-K-9) and HRQoL score (EQ-5D) 6 months post-transplant. Significant associations with the SCL-K-9 score at T3 were evident for disease severity (r = 0.39; p = 0.001); length of hospital stay (r = 0.44; p = 0.005), the EQ-5D score at T1 (r = –0.37; p = 0.02), number of hospitalisations (r = 0.66; p = 0.01) and use of antidepressants (r = 0.47; p = 0.01) within the first 6 months post-transplant. The following variables were significantly correlated with T3 EQ-5D: disease severity (r = –0.42; p = 0.006); T1 EQ-5D (r = 0.39; p = 0.01); number of days in the ICU (r = –0.36; p = 0.02); length of hospital stay (r = –0.72; p = 0.001), number of hospitalisations (r = –0.43; p = 0.01) and use of antidepressants (r = –0.63; p = 0.01) within the first 6 months after lung transplant.
| Table 2: Cluster characteristics. | ||||||
| Time-point instrument | Optimal cluster (A) n = 17 (42%) | Good cluster (B) n = 14 (35%) | Poor cluster (C) n = 9 (23%) | Between groups | ||
| Mean (SD) | Mean (SD) | Mean (SD) | p-value | Bonferroni post hoc test | p-value | |
| T1 SCL-K-9 | 0.5 (0.2) | 1.7 (0.6) | 0.8 (0.3) | <0.001 | A vs B A vs C B vs C | <0.001 0.105 <0.001 |
| T1 EQ-5D | 80.6 (14.3) | 53.6 (13.4) | 46.7 (21.1) | <0.001 | A vs B A vs C B vs C | <0.001 <0.001 0.937 |
| T2 SCL-K-9 | 0.2 (0.2) | 0.6 (0.3) | 1.0 (0.4) | <0.001 | A vs B A vs C B vs C | 0.008 <0.001 0.004 |
| T2 EQ-5D | 93.5 (4.9) | 83.6 (12.2) | 66.7 (17.3) | <0.001 | A vs B A vs C B vs C | 0.058 <0.001 0.004 |
| T3 SCL-K-9 | 0.2 (0.2) | 0.5 (0.4) | 0.9 (0.4) | <0.001 | A vs B A vs C B vs C | 0.027 <0.001 0.042 |
| T3 EQ-5D | 93.5 (7.0) | 89.3 (8.3) | 64.4 (17.4) | <0.001 | A vs B A vs C B vs C | 0.814 <0.001 <0.001 |
| EQ-5D = EuroQuol (range 0–100; community-based standard value = 91.7); p = level of significance; SCL-K-9 = the Symptom Checklist (community-based standard value = 0.41; higher values indicating greater distress); SD = standard deviation; T1–T3 = measurement time-points; | ||||||
| Table 3: Sociodemographic and medical characteristics of post-transplant outcome-clusters. | ||||||||
| Optimal cluster (A) n = 17 (42%) | Good cluster (B) n = 14 (35%) | Poor cluster (C) n = 9 (23%) | Effect size | p-value | ||||
| Sex | 0.17a | 0.551a | ||||||
| Male | 11 | 27.5% | 7 | 17.5% | 4 | 10 % | ||
| Female | 6 | 15% | 7 | 17.5% | 5 | 12.5% | ||
| Age (years; mean, SD) | 46.5 | 16.6 | 44.2 | 13.9 | 54.6 | 15.4 | 0.07b | 0.286b |
| Underlying diagnosis* (n, %) | 0.34a | 0.160a | ||||||
| COPD | 9 | 22.5% | 3 | 7.5% | 3 | 7.5% | ||
| Cystic fibrosis | 6 | 15% | 6 | 15% | 1 | 2.5% | ||
| Idiopathic pulmonary fibrosis | 2 | 5% | 2 | 5% | 3 | 7.5% | ||
| Other | 3 | 7.5% | 2 | 5% | ||||
| Disease severityc (mean, SD) | 1.8 | 0.6 | 1.9 | 0.3 | 2.3 | 0.5 | 0.13b | 0.075b |
| Time on waiting list (days, mean, SD) | 258.3 | 288.5 | 313.4 | 210.4 | 226.7 | 77.9 | 0.02b | 0.700b |
| ECMO use (n, %) | 6 | 15% | 4 | 10% | 3 | 7.5% | 0.08a | 0.883a |
| Comorbidities (mean, SD) | 1.7 | 1.2 | 1.8 | 1.3 | 2.3 | 1.1 | 0.06b | 0.386b |
| Number of days in ICU pLTx (mean, SD) | 5.8 | 5.5 | 5.9 | 4.6 | 10.4 | 11.0 | 0.08b | 0.210b |
| Length of stay (weeks; mean, SD) | 4.4 | 1.4 | 4.6 | 1.4 | 9.6 | 3.6 | 0.53b | 0.001b |
| Number of hospitalisations pLTx (M, SD) | 0.50 | 0.6 | 0.50 | 0.7 | 2.0 | 1.2 | 0.24b | 0.006b |
| Number of infections pLTx (mean, SD) | 0.5 | 0.7 | 0.7 | 1.1 | 0.7 | 0.9 | 0.01b | 0.836b |
| Number of rejections pLTx (m, SD) | 0.1 | 0.5 | 0.1 | 0.3 | 0.1 | 0.3 | 0.01b | 0.943b |
| Antidepressants pLTx (n, %) | 3 | 7.5% | 1 | 2.5% | 6 | 15% | 0.53a | 0.004a |
| COPD = chronic obstructive pulmonary disease; ECMO = extracorporal membrane oxygenation; ICU = intensive care unit; pLTx = post-transplant; SD = standard deviation. a Chi-square test for comparison of nominal or dichotomised variables and Cramer’s V for computing effect sizes. b F-test for multiple comparison analysis of variance with continuous variables and Eta2 for computing effect sizes. c Disease severity refers to the pretransplant health status while on waiting list and was judged by the treating pneumonologist (M.S.) into one of three categories (1–3). Higher values indicate higher disease severity. 1 = patients with progressive lung diseases, some required oxygen therapy but predominantly treated as out-patients; 2 = patients with progressive lung disease and oxygen therapy in bad health condition, partly treated as out-patients and partly transferred to inpatient hospital care; 3 = patients with progressive lung disease in extremely critical health conditions (ICU, ECMO use; intubation, decarboxylation device). Statistical significance: p <0.05. | ||||||||
| Table 4: Predictor analyses for psychological distress and health-related quality of life 6 months post-transplant. | ||
| Medical factors | T3 SCL-K-9 (n = 40) | T3 EQ-5D (n = 40) |
| Age | 0.25 | –0.20 |
| Sex† | –0.13 | –0.12 |
| Disease severity | 0.39* | –0.42** |
| Time on waiting list | –0.02 | 0.24 |
| ECMO use | –0.02 | 0.29 |
| Comorbidities | 0.16 | –0.05 |
| Number of days in ICU | 0.11 | –0.36* |
| Length of hospital stay | 0.44* | –0.72** |
| Number of hospitalisations pLTx | 0.66** | –0.43** |
| Number of infections pLTx | 0.30 | –0.13 |
| Number of rejections pLTx | 0.67 | –0.18 |
| Antidepressants pLTx† | 0.47** | –0.63** |
| T1 EQ-5D | –0.37* | 0.39* |
| ECMO = extracorporal membrane oxygenation; EQ-5D = EuroQuol (range 0–100; community-based standard value = 91.7); ICU = intensive care unit; pLTX = post-transplant; SCL-K-9 = the Symptom Checklist (community-based standard value = 0.41; higher values indicating greater distress); T1,T3 = measurement time-points * p ≤0 .05; ** p ≤0.01; *** p ≤0.001. † Statistical relationship computed with Spearman Correlation. Sex: 1 = male; 2 = female. | ||
In this study, a hierarchical cluster analysis was performed – so as to identify distinctive post-transplant sub-groups related to psychological distress and HRQoL over those first 6 postoperative months. Our data revealed a three-cluster solution, distinguishing transplant recipients manifesting optimal, good and poor postoperative clusters. Transplant recipients of the optimal postoperative cluster (42%) reported surprisingly high HRQoL levels and notably low levels of psychological distress shortly after transplantation, and by 6 months post-transplant, their reported HRQoL and stress levels were similar to healthy population values. Patients in the good cluster (35%) experienced impaired HRQoL and elevated stress levels 2 weeks after transplantation, but by 3 months follow-up reported significantly increased HRQoL and significantly reduced psychological distress. This group of patients benefitted most from lung transplant surgery by demonstrating substantial improvements in HRQoL dimensions and levels of psychological distress over the first 6 months after transplantation compared with the other two cluster groups. Importantly to note, almost a quarter of our clinical sample (23%) showed poor postoperative outcomes over time, suffering from elevated stress levels that continued to remain high over the first 6 months post-transplant, and experiencing only slightly increased HRQoL that remained low throughout the six-month observation period. Most investigations on psychosocial outcomes after lung transplantation have focused on the average value of HRQoL and did not distinguish between favourable and poor postoperative outcome. However, lung transplant recipients are a heterogeneous group of patients and do not necessarily experience the same improvements in health status. The use of cluster analyses instead of considering only outcomes at discrete measurement time points is beneficial for identifying patients who did not experience significant improvements of postoperative HRQoL. Our results indicate that lung transplant recipients respond in different ways to their surgery and that quality of life gain after transplantation varies greatly from patient to patient. The majority of patients appear to cope very well, while others seem to struggle postoperatively. For many patients, the transplantation itself, as well as the ICU stay, might be perceived as a traumatic stressor that can decrease HRQoL and trigger mental distress [29]. Additionally, the rehabilitation period can vary greatly from patient to patient. A lung recipient’s own history of lung disease plus enduring functional impairments and symptom distress post-transplant may negatively affect the patient’s HRQoL perception [30]. Furthermore, the concept of resilience might explain at least some of the different responses to transplantation. For instance, previous studies in transplant medicine illustrated that a high degree of resilience and self-efficacy [31] as well as social support [32, 33], are essential to coping successfully with the transplant experience.
As a second analytical step, we sought to identify differences between the cluster groups and thereby detect those with poor post-transplant trajectories. Our patients with poor postoperative HRQoL generally were older, were more likely to suffer from more severe disease, had more comorbid conditions, were more likely to have had prolonged ICU and hospital stays, had more hospital admissions after transplantation and were more frequently treated with antidepressants. Previous studies have suggested a negative impact of comorbidities on HRQoL after lung transplant [13, 16]. Our results are consistent with these findings, indicating that clinical complications (e.g., greater disease severity, a higher number of comorbidities, and longer hospital stays) are associated with progressive quality of life deterioration over the early post-transplant period. With regards to demographic variables, in the psychosocial transplant literature reduced HRQoL-gains have been commonly described in older lung transplant recipients, presumably because older patients have less energy and reserves to cope with the taxing post-operative period than those who are younger [14, 34]. On the other hand, researchers have reported significant gender differences in overall HRQoL, reflecting better outcomes in men [15, 35]; notwithstanding, we did not observe this in the current study.
Lastly, we explored potential predictors of psychological distress and poor HRQoL 6 months after transplantation. In particular, disease severity, the number of days spent in the ICU and hospital, self-reported HRQoL 2 weeks post-transplant, number of post-transplant hospital admissions as well as use of antidepressants predicted impaired HRQoL at 6 months of follow-up. Meanwhile, disease severity, length of hospital stay, self-reported HRQoL 2 weeks post-transplant, number of hospital admissions, and use of antidepressants significantly predicted levels of psychological distress at 6 months. Age, gender, time on the waiting list, preoperative ECMO use, the number of comorbid conditions, number of infections or rejections failed to predict 6-month levels of psychological distress or HRQoL. Our findings are similar to those of an earlier cross-sectional cohort study investigating HRQoL determinants among patients between 1 and 5 years since their lung transplant, suggesting that lung disease and events leading to hospitalisation negatively affect most of the SF-36 (Short Form Health Survey) domains, whereas other variables like age, gender and FEV1 exert little to no influence on HRQoL [34].
Taken together, almost a quarter of the investigated patients suffered from elevated distress and substantially impaired quality of life, with no considerable improvements over time. This result is of high clinical importance, given that elevated psychological distress and impaired HRQoL in the early postoperative phase can have a persistent negative impact upon long-term mental health and HRQoL [36]. Furthermore, a growing body of literature suggests that early post-transplant depression and psychological distress significantly increase the risk for long-term transplant-related morbidity and mortality [37–39]. Thus, the precocious identification of transplant recipients with clinically significant distress and impaired HRQoL is critical to initiate pharmacological and psychotherapeutic interventions for these patients in order to reduce their symptom experience.
Strengths of the current study include our investigation of a lung transplant population treated exclusively by the transplant centre using a prospective, longitudinal study design, as well the use of a rigorous statistical methodology to identify distinct cluster groups, and the utilisation of validated outcome measures with well-known psychometric properties. Potential limitations include the relatively small study sample. Because of the small sample, our results lack statistical power, meaning that the results of our cluster analyses were presented only descriptively. Moreover, we surveyed lung transplant recipients over a relatively short period of time (only 6 months). The follow-up of lung transplant recipients over several years would add further insights into the development of post-transplant psychosocial trajectories and outcome predictors. Although our findings should be interpreted with caution owing to these limitations, we believe that our study provides realistic and valid predictors for early post-operative psychosocial outcomes.
The assessment of post-transplant psychological distress and HRQoL in terms of cluster analyses instead of considering only outcomes at discrete time points is beneficial in identifying patients who experience no significant postoperative improvement in HRQoL. Psychosocial care of transplant recipients who suffer from emotional distress and impaired HRQoL is critical to maximizing recovery and outcomes. Additional longitudinal research with larger samples remains necessary to clarify the long-term post-transplant outcomes of these patients and to identify other potentially important outcome predictors.
1 Rodrigue JR, Baz MA, Kanasky WF Jr, MacNaughton KL. Does lung transplantation improve health-related quality of life? The University of Florida experience. J Heart Lung Transplant. 2005;24(6):755–63.
2 Kugler C, Fischer S, Gottlieb J, Tegtbur U, Welte T, Goerler H, et al. Symptom experience after lung transplantation: impact on quality of life and adherence. Clin Transplant. 2007;21(5):590–6.
3 Munro PE, Holland AE, Bailey M, Button BM, Snell GI. Pulmonary rehabilitation following lung transplantation. Transplant Proc. 2009;41(1):292–5.
4 Yusen RD, Edwards LB, Kucheryavaya AY, Benden C, Dipchand AI, Dobbels F, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-first Adult Lung and Heart-Lung Transplant Report-2014; Focus Theme: Retransplantation. J Heart Lung Transplant. 2014;33(10):1009–24.
5 Swisstransplant, Annual Report 2013, 2013, Swisstransplant, Schweizerische Nationale Stiftung für Organspende und Transplantation: Bern, Switzerland. p. 1–43.
6 Inci I, Schuurmans MM, Boehler A, Weder W. Zurich University Hospital lung transplantation programme: update 2012. Swiss Med Wkly. 2013;143:w13836.
7 Swisstransplant Swisstransplant Annual Report 2014. 2015.
8 Myaskovsky L, Dew MA, McNulty ML, Switzer GE, DiMartini AF, Kormos RL, et al. Trajectories of change in quality of life in 12-month survivors of lung or heart transplant. Am J Transplant. 2006;6(8):1939–47.
9 Pinson CW, Feurer ID, Payne JL, Wise PE, Shockley S, Speroff T. Health-related quality of life after different types of solid organ transplantation. Ann Surg. 2000;232(4):597–607.
10 Goetzmann L, Ruegg L, Stamm M, Ambühl P, Boehler A, Halter J, et al. Psychosocial profiles after transplantation: a 24-month follow-up of heart, lung, liver, kidney and allogeneic bone-marrow patients. Transplantation. 2008;86(5):662–8.
11 Kugler C, Tegtbur U, Gottlieb J, Bara C, Malehsa D, Dierich M, et al. Health-related quality of life in long-term survivors after heart and lung transplantation: a prospective cohort study. Transplantation. 2010;90(4):451–7.
12 Butler J, McCoin NS, Feurer ID, Speroff T, Davis SF, Chomsky DB, et al. Modeling the effects of functional performance and post-transplant comorbidities on health-related quality of life after heart transplantation. J Heart Lung Transplant. 2003;22(10):1149–56.
13 Vermeulen KM, Ouwens JP, van der Bij W, de Boer WJ, Koëter GH, TenVergert EM. Long-term quality of life in patients surviving at least 55 months after lung transplantation. Gen Hosp Psychiatry. 2003;25(2):95–102.
14 Vermuelen KM, van der Bij W, Erasmus ME, TenVergert EM. Long-term health-related quality of life after lung transplantation: different predictors for different dimensions. J Heart Lung Transplant. 2007;26(2):188–93.
15 Santana MJ, Feeny D, Ghosh S, Lien DC. Patient-reported outcome 2 years after lung transplantation: does the underlying diagnosis matter? Patient Relat Outcome Meas. 2012;3:79–84.
16 Kugler C, Fischer S, Gottlieb J, Welte T, Simon A, Haverich A, et al. Health-related quality of life in two hundred-eighty lung transplant recipients. J Heart Lung Transplant. 2005;24(12):2262–8.
17 Gerbase MW, Spiliopoulos A, Rochat T, Archinard M, Nicod LP.. Health-related quality of life following single or bilateral lung transplantation: a 7-year comparison to functional outcome. Chest. 2005;128(3):1371–8.
18 Dew MA, DiMartini AF, DeVito Dabbs AJ, Fox KR, Myaskovsky L, Posluszny DM, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychiatry. 2012;34(2):127–38.
19 Klaghofer R, Braehler E. Construction and validation of a shor form of the SCL-90-R. Z Klin Psychol Psychiatr Psychother. 2001;49(2):115–24.
20 Rosen CS, Drescher KD, Moos RH, Finney JW, Murphy RT, Gusman F. Six- and ten-item indexes of psychological distress based on the Symptom Checklist-90. Assessment. 2000;7(2):103–11.
21 Franke GH, SCL-90-R. Die Symptomcheckliste von Derogatis – Deutsche Version. Manual.1995, Göttingen: Beltz.
22 EuroQol Group, EuroQol – a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208.
23 Hinz A, Klaiberg A, Brähler E, König HH. [The Quality of Life Questionnaire EQ-5D: modelling and norm values for the general population.] Psychother Psychosom Med Psychol. 2006;56(2):42–8. German.
24 Vaquero Barrios JM, Redel Montero J, Santos Luna F. Comorbidities impacting on prognosis after lung transplant. Arch Bronconeumol. 2014;50(1):25–33.
25 IBM Corp, IBM SPSS Statistics for Windows, Version 22.02013, Armonk, NY: IBM Corp.
26 Ward JH. Hierarchical Grouping to Optimize an Objective Function. J Am Stat Assoc. 1963;58(301):236–44.
27 Hair JF, Black WC. Cluster analysis., in In Reading and Understanding More Multivariate Statistics. L.G. Grimm, P.R. Yarnold, eds.2000, American Psychological Association: Washington DC. p. 147–205.
28 Cohen L, Littlefield C, Kelly P, Maurer J, Abbey S. Predictors of quality of life and adjustment after lung transplantation. Chest. 1998;113(3):633–44.
29 Baranyi A, Krauseneck T, Rothenhausler HB. Overall mental distress and health-related quality of life after solid-organ transplantation: results from a retrospective follow-up study. Health Qual Life Outcomes. 2013;11:15.
30 Dew MA, DiMartini AF, DeVito Dabbs AJ, Fox KR, Myaskovsky L, Posluszny DM, et al. Onset and risk factors for anxiety and depression during the first 2 years after lung transplantation. Gen Hosp Psychiatry. 2012;34(2):127–38.
31 Schumacher A, Sauerland C, Silling G, Berdel WE, Stelljes M. . Resilience in patients after allogeneic stem cell transplantation. Support Care Cancer. 2014;22(2):487–93.
32 DeVito Dabbs A, Terhorst L, Song MK, Shellmer DA, Aubrecht J, Connolly M, et al. Quality of recipient-caregiver relationship and psychological distress are correlates of self-care agency after lung transplantation. Clin Transplant. 2013;27(1):113–20.
33 Archonti C, D'Amelio R, Klein T, Schäfers HJ, Sybrecht GW, Wilkens H. [Physical quality of life and social support in patients on the waiting list and after a lung transplantation.] Psychother Psychosom Med Psychol. 2004;54(1):17–22. German.
34 Vasiliadis HM, Collet JP, Poirier C. Health-related quality of life determinants in lung transplantation. J Heart Lung Transplant. 2006;25(2):226–33.
35 Rodrigue JR, Baz MA. Are there sex differences in health-related quality of life after lung transplantation for chronic obstructive pulmonary disease? J Heart Lung Transplant. 2006;25(1):120–5.
36 Goetzmann L, Irani S, Schwegler K, Stamm M, Bricman R, Buddeberg C, et al. Distress and alexithymia in lung recipients – psychosocial strains and associations with chronic allograft dysfunction. Swiss Med Wkly. 2010;140(25-26):382–7.
37 Havik OE, Sivertsen B, Relbo A, Hellesvik M, Grov I, Geiran O, et al. Depressive symptoms and all-cause mortality after heart transplantation. Transplantation. 2007;84(1):97–103.
38 Sirri L, Potena L, Masetti M, Tossani E, Magelli C, Grandi S. Psychological predictors of mortality in heart transplanted patients: a prospective, 6-year follow-up study. Transplantation. 2010;89(7):879–86.
39 Rosenberger EM, DiMartini AF, DeVito Dabbs AJ, Bermudez CA, Pilewski JM, Toyoda Y, et al. Psychiatric Predictors of Long-Term Transplant-Related Outcomes in Lung Transplant Recipients. Transplantation. 2015. [Epub ahead of print.]
Author contributions: AS was responsible for drafting the manuscript and takes responsibility for the integrity of the data and the accuracy of the data analysis. She is the guarantor. JJ and RK were consultants and provided advice during the conception and design of the project. All authors critically revised the paper for important intellectual content. JJ and AS obtained the funding.
Disclosure statement:This study was funded by grants from the Olga Mayenfisch Foundation, the Hartmann-Müller Foundation for Medical Research and the Lunge Zürich. No other potential conflict of interest relevant to this article was reported.