Referral rates in Swiss primary care with a special emphasis on reasons for encounter
DOI: https://doi.org/10.4414/smw.2015.14244
Ryan
Tandjung, Andreas
Hanhart, Fredi
Bärtschi, Rebecca
Keller, Andy
Steinhauer, Thomas
Rosemann, Oliver
Senn
Summary
QUESTIONS UNDER STUDY: Referrals from primary to secondary care reflect a crucial role of primary care physicians (PCPs). Most referral rates are based on the number of consultations, rather than on the number of problems addressed during consultations (reasons for encounter = RFE). The aim of the study was to update data on consultations, RFE and referrals in Swiss primary care and calculate a referral rate based on RFE rather than on the number of consultations.
METHOD: Cross-sectional study in Swiss primary care. PCPs collected data on consultations on 15 different days in three nonconsecutive months in 2012/2013. Demographic data of patients and up to six RFE per consultation were collected. For each RFE the PCP had to indicate whether a referral was initiated. Data were analysed using descriptive statistics.
RESULTS: Ninety PCPs (18.9% females) participated and 24 774 consultations with 42 890 RFE (corresponding to 1.73 [standard deviation 1.07] RFE per consultation) were recorded. A total of 2 427 RFE (of 2 341 consultations) led to a referral, corresponding to a referral rate of 9.44% (95% confidence interval [CI] 9.08–9.81%) based on consultations and 5.65% (95% CI 5.43–5.87%) based on the number of RFE.
CONCLUSIONS: An average of 1.7 RFE per consultation and a broad clinical spectrum of problems were presented in primary care; nevertheless, 94.3% of all problems were solved in primary care, reflecting the crucial role of PCPs as a coordinator of healthcare.
Introduction
There is growing evidence that strong primary care contributes to efficiency and quality in healthcare [1, 2]. Referrals from primary to secondary care reflect this important role of primary care physicians (PCPs). In Switzerland, systematic data on referrals was last collected in 1989 as part of a European referral study [3]. Many conditions have changed since then; the study was taking place at a time where 3 833 PCPs were working in private practices. Today Switzerland has a higher density of population (6.75 million in 1990 to 8.04 million in 2012) [4], of PCPs (2013: 5 929) [5], and also of specialists in secondary care. The population growth of 19.1% is opposed by a growth of numbers of physicians in primary care of 54.7%. The Swiss healthcare system is mainly financed through private health insurance. Health insurance is mandatory for every Swiss citizen since a new law established in January 1996. A gatekeeping system is not mandatory for health insurance and the role of PCPs as gatekeepers is often challenged. It remains unclear how these changes affected referral rates.
Earlier studies reporting referral rates were calculated on the basis of consultations. This does not completely reflect the work of PCPs. Some studies have shown that during a consultation usually more than one problem is discussed between patient and PCP [6–8].
The aim of our study was to investigate consultations and to update recordkeeping and the database on referrals of Swiss primary care. Unlike, for example, in the United Kingdom, electronic health record coverage in Switzerland is still low and currently available databases in primary care, such as the FIRE database (Family Medicine ICPC-Research using Electronic Medical Records), were not able to answer our question [9, 10]. Therefore, we decided to collect prospectively data on consultations; furthermore, we specifically aimed to calculate a referral rate based not only on consultations, but also based on all problems raised during these consultations.
Methods
Participants
PCPs were recruited through primary care organisations and networks situated in rural as well as in urban regions of Switzerland; we aimed to include at least 60 PCPs of different regions in Switzerland. As remuneration PCPs were paid 500 Swiss francs for participation. Patients were not remunerated.
Timeframe
The study was conducted in 2012 and 2013. PCPs collected data during three study months. During each study month (March 2013, May 2013 and November 2012 or 2013) five weekdays (each month Monday to Friday to achieve representative data [11]) were fixed as study days. PCPs were asked to participate according to their normal workload; full time corresponds to 15 study days during the whole study period. If PCPs were not able to collect data on the study day, they were asked to collect data within 4 weeks on the same weekday. Data for analysis were excluded when a PCP did not collect data on at least two days per study month.
Measurements
During each study day the PCP documented every consultation on a paper form, collecting following information: patient’s year of birth, sex, membership in a managed care model and up to six reasons for encounter (RFE). The study form was piloted with four PCPs, where an average of three RFE were documented; we therefore included up to six RFE on the final study form. PCPs were asked to write down reasons for encounter and not their diagnosis and to fill in the consultation form after each consultation rather than at the end of the working day. For each RFE the PCP indicated whether a referral was initiated or not. If a referral was initiated, PCPs completed a second form to further assess referral details (e.g. type of specialist, aim, initiator, shared decision and timeframe). During a study day all face-to-face physician-patient consultations were documented. Telephone encounters and administrative work (such as reviewing a discharge letter in the absence of a patient) were not documented. Referral was considered to cover investigations by another doctor, including radiological investigations such as computed tomography (CT) scans or magnetic resonance imaging (MRI). Conventional x-rays are commonly available in Swiss private practices and were, therefore, not considered as a referral. Emergency referrals to hospitals were also not documented.
Data management and coding
Data were consecutively sent to the Institute of Primary Care in Zurich and entered into a database. The RFE were written in full text by PCPs and then coded by two researchers according to the ICPC-2 classification (12). ICPC-2 is a coding system acknowledged by the World Health Organization and particularly suitable for primary care, since it includes not only diagnoses, but also symptoms (e.g. headache). The coding system is based on chapters usually representing organ systems (e.g. chapter K = circulatory or L = musculoskeletal). To achieve a high coding reliability a random sample of 1 000 RFEs was double coded and inter-rater agreement was assessed by using kappa statistics. Agreement was substantial on single code levels (letter indicating organ system and number indicating diagnosis or procedure; 80.6%) and reached an almost perfect congruence of 94.4% on organ chapter levels, consistent with the literature [13]; thus all further RFE were coded only once by the one of the two independent researchers.
Statistics
We used descriptive statistics for patient and PCP characteristics. Figures are reported in absolute numbers and percentage of total in brackets and/or means and standard deviation (SD) in brackets. Referral rates and 95% confidence intervals (95% CI) were calculated as a proportion of the number of consultations and of the number of all RFE. Patient and PCP characteristics were compared using parametric and nonparametric tests as appropriate. We considered a p-value <0.05 as statistically significant.
Ethical issues
In 2012, under Swiss ethics guidelines a study based on anonymous data does not require a formal ethics approval. For the present study we consulted the Ethics Committee of the Canton of Zurich, which confirmed that an ethical approval was not necessary (correspondence letter from June 28th 2012).
|
Table 1: Data for the participating primary care physicians and patients. |
|
|
All
|
Male
|
Female
|
| Primary care physicians |
|
|
|
| Number of participants(n, %) |
90 |
73 (81.1%) |
17 (18.9%) |
| Years of practice experiences (SD) |
17.3 (9.3) |
18.6 (9.3) |
11.4 (6.7) |
| Workload (days per week, mean (SD)) |
3.7 (0.8) |
3.9 (0.7) |
2.7 (0.9) |
| Average number of consultations per full working day (SD) |
24.7 (8.2) |
|
|
| Average number of RFE per consultation (SD) |
1.73 (1.07) |
1.72 (1.07) |
1.83 (1.22) |
| Patients |
|
|
|
| Number of patients (n, %)* |
24 774 |
11 268 (45.5%) |
13 363 (53.9%) |
| Age (mean, SD) |
53.9 (21.8) |
52.8 (21.5) |
54.8 (22.0) |
| Average number of RFE per consultation (SD) |
1.73 (1.07) |
1.69 (1.03) |
1.77 (1.10) |
| PCP = primary care physician; RFE = reasons for encounter; SD = standard deviation
Figures indicate mean and standard deviation in brackets Figures of participants describe numbers and percentages of male and female PCPs or patients.
* 143 values concerning sex in patients are missing. |
Results
Participating PCPs
Ninety-two PCPs participated in our study; data of two PCPs were excluded because they did not collect data throughout the whole study period. Overall 24 774 consultations of patients were included. Overall, 9 278 (37.5%) patients were insured in a managed-care model. A summary of data on PCPs and patients is provided in table 1.
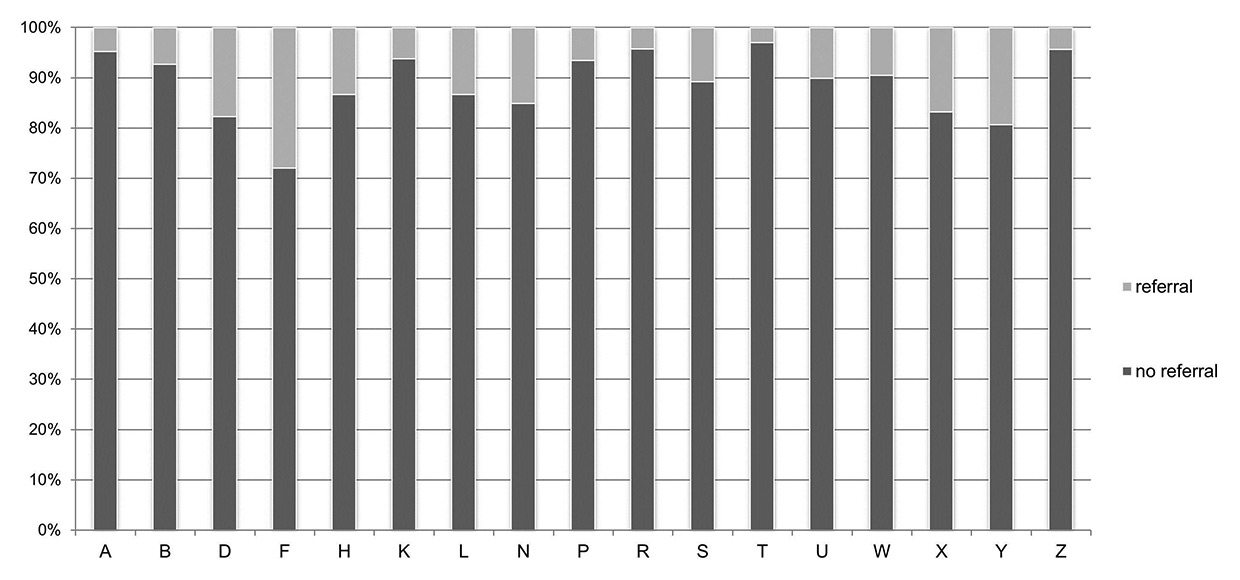
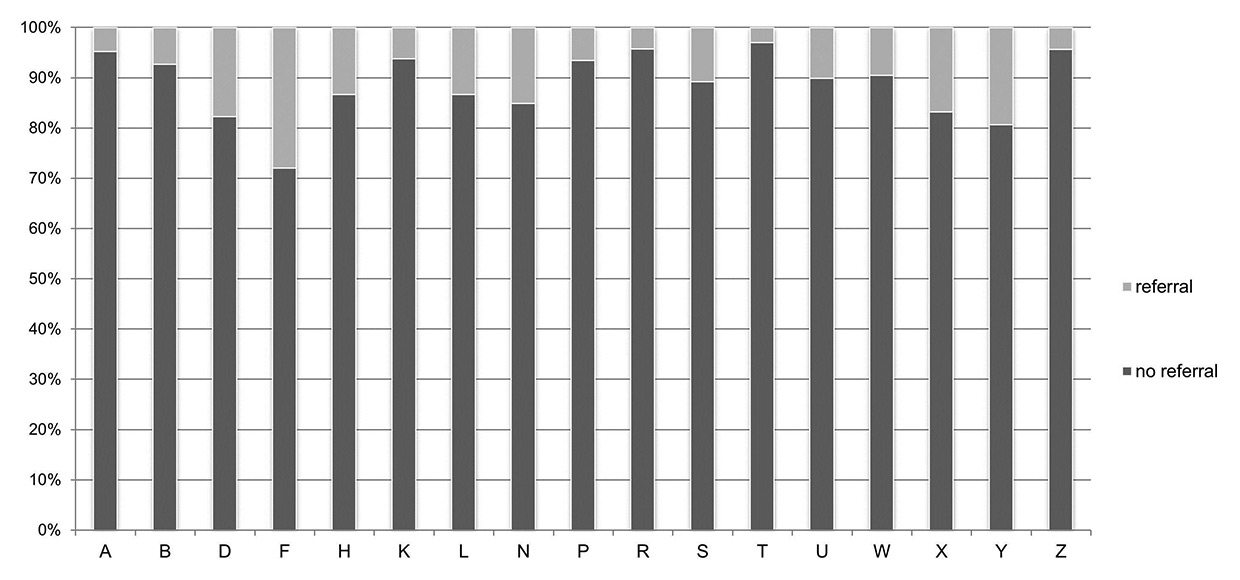
Figure 1
Referral rates according to ICPC-2 chapters.
Percentage of reasons for encounter (RFE) according to ICPC-2 chapters which led to a referral (light) or were handled in primary care (dark). (A General and unspecified; B Blood, blood forming organs, lymphatic, spleen; D Digestive; F Eye; H Ear; K Circulatory; L Musculoskeletal; N Neurological; P Psychological; R Respiratory; S Skin; T Endocrine, metabolic and nutritional; U Urology; W Pregnancy, childbirth, family planning; X Female genital system and breast; Y Male genital system; Z Social problems)
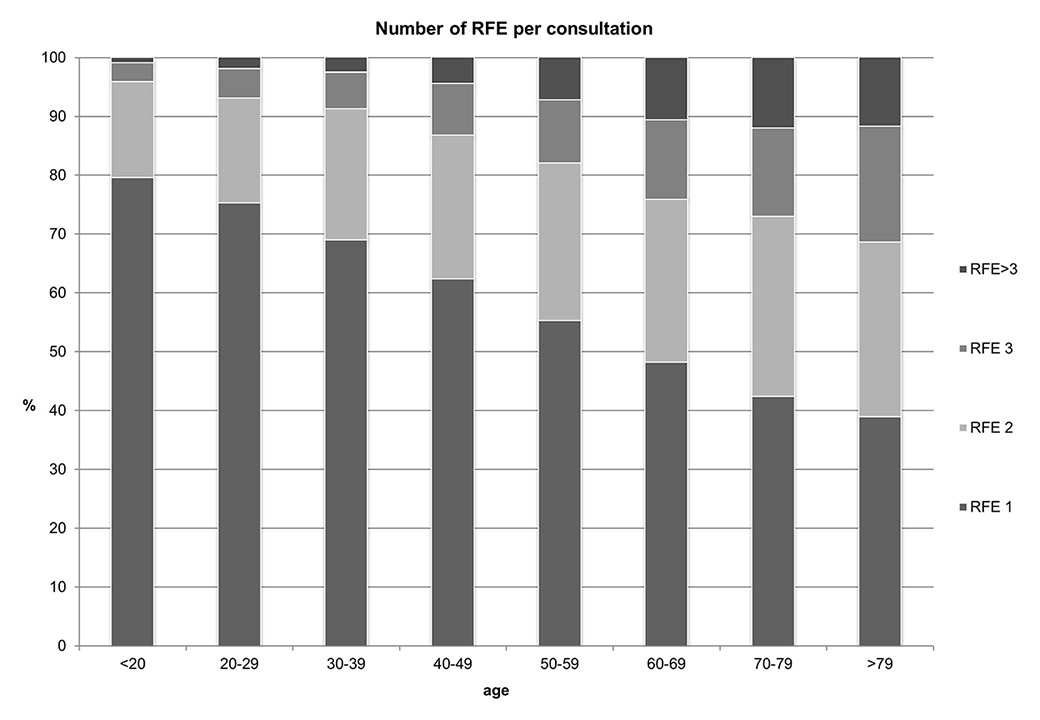
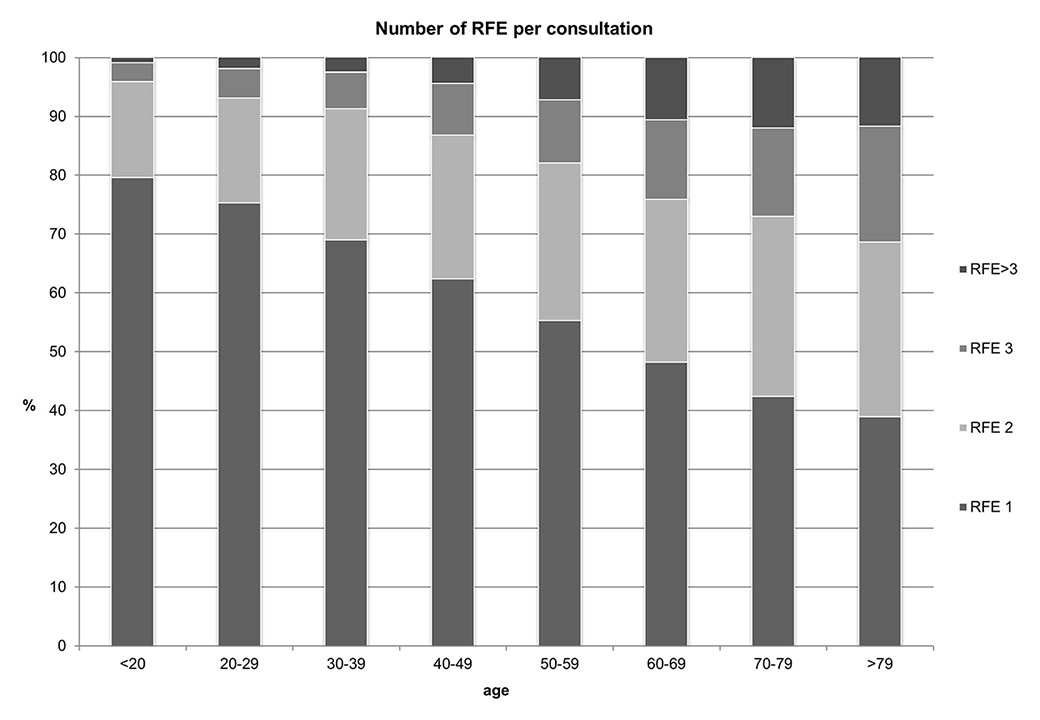
Figure 2
Number of RFE per consultation.
Number of reasons for encounter (RFE), x-axis describes age of patients, y-axis describes percentages of each group.
Referrals
During the study, 2 427 RFE (brought up during 2 341 consultations) led to a referral; which corresponds to a referral rate of 5.65% (95% CI 5.43–5.87%) based on all RFE and 9.44% (95% CI 9.08–9.81%) based on consultations. The PCP was initiator of the referral in 68.4%, in 19.4% the patient was initiator of the referrals, and in 12.2% the situation is not clear. The decision concerning a referral was shared by patient and PCP in 97.2%. The most frequent referral recipients were radiologists (495, 21.14%), gastroenterologists (219, 9.35%), and orthopaedic surgeons (218, 9.31%). The most frequent aim of referrals was advice concerning diagnosis or therapy (n = 1 084, 46.3%), radiological investigation (computed tomography, MRI, ultrasound) (492, 21.01%), nonsurgical intervention (280, 11.96%), and surgical intervention (251, 10.72%). Referral rates differed between the RFE chapters in a range from 1.4% for chapter T (endocrine, metabolic and nutritional) up to 18.7% for chapter F (eye). Figure 1 shows the referral rate according to the RFE chapters.
Consultations and reasons for encounter
Overall data on 1 179 study days were collected, corresponding to 992.5 full working days. On average a PCP had 24.7 consultations per day (SD 9.8). The total of 24 774 consultations corresponds to 42 890 RFE. This corresponds to a mean of 1.73 RFE (SD 1.07) per consultation. In 13 893 (56.1%) of the consultations one RFE was documented, in 6 312 (25.5%) two reasons, in 2 760 (11.1%) three reasons and in 1 806 (7.3%) more than three reasons per consultation were documented. In the group younger than 20 a mean of 1.25 RFE (SD 0.55) and in the group older than 80 a mean of 2.11 (SD 1.19) RFE per consultation were found. Figure 2 shows the numbers of RFE per consultation according to age groups of the patients.
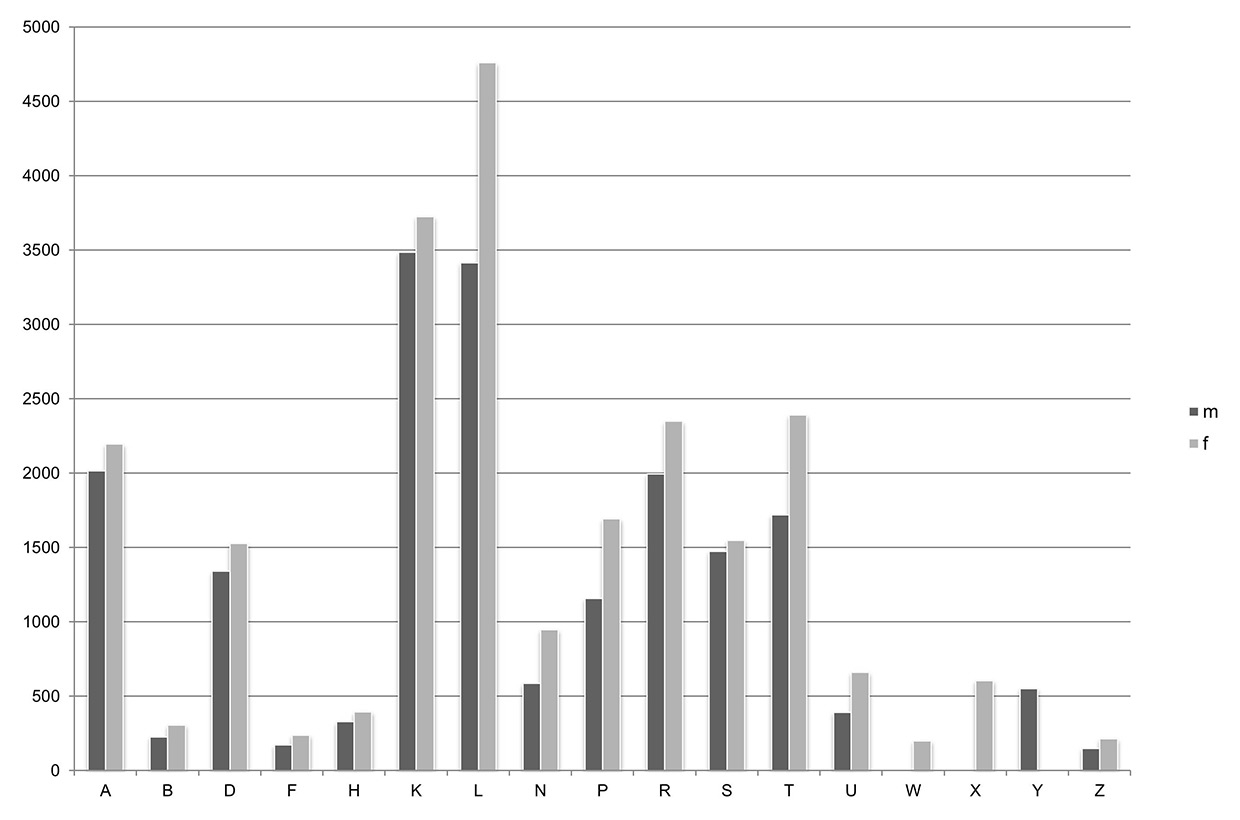
We analysed the RFE according to the chapters of ICPC corresponding to an organ region. The most common categories of RFE were musculoskeletal (chapter L, n = 5 309, 21.4%), cardiovascular (K, n = 3 427, 13.8%) and respiratory (R, n = 2 827, 11.4%). The frequency of ICPC chapters were different between male and female patients- In female patients the most common reasons were musculoskeletal (21.7%), cardiovascular (13.0%) and respiratory (11.4%); in male patients the most common reasons were musculoskeletal (21.3%), cardiovascular (15.0%) and general (11.6%). Overall a total of 830 RFE were coded. The most frequent codes were K86 (uncomplicated hypertension, n = 2 636, 6.15%), K34 (cardiovascular blood test, n = 1 264, 2.95%), T90 (Diabetes, noninsulin dependent, n = 1 182, 2.76%), P76 (depressive disorder, n = 769, 1.79%) and L29 (other musculoskeletal symptoms, n = 677, 1.58%). The three most common RFE were identical in male and female patients. Figure 3 shows the frequency of RFE by chapter chapters in male and female patients.
Discussion
In 24 774 consultations a total of 42 890 reasons for encounters were raised, which results in an average of 1.73 RFE per consultation. A broad spectrum of RFE was brought up during the consultations, and overall 830 different RFE were recorded. Nevertheless, 90.6% of the consultations or 94.3% of problems raised in primary care consultations were managed by PCPs and did not need a referral.
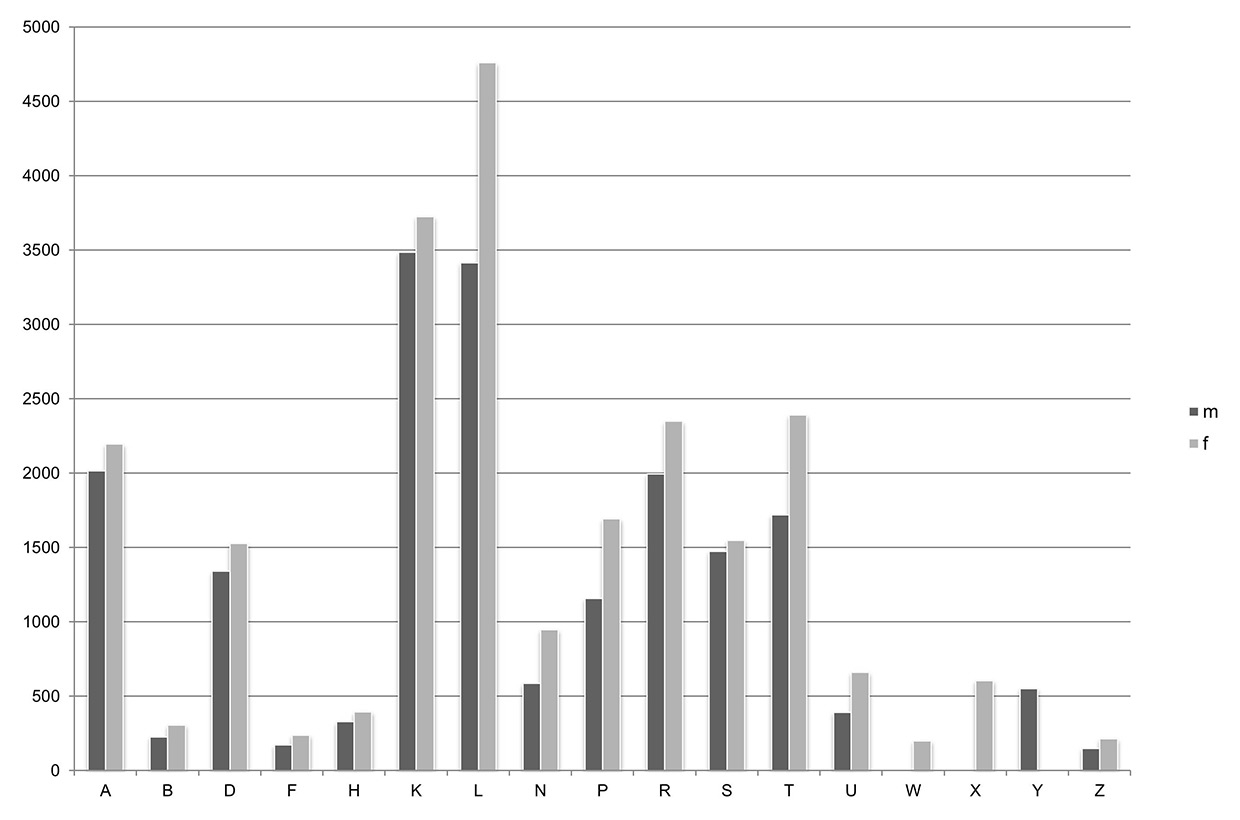
Figure 3
Frequency of RFE in male and female patients.
Frequency of reasons for encounter (RFE) according to ICPC-2 chapters in male (dark) and female (light) patients. (A General and unspecified; B Blood, blood forming organs, lymphatics, spleen; D Digestive; F Eye; H Ear; K Circulatory; L Musculoskeletal; N Neurological; P Psychological; R Respiratory; S Skin; T Endocrine, metabolic and nutritional; U Urology; W Pregnancy, childbirth, family planning; X Female genital system and breast; Y Male genital system; Z Social problems)
The corresponding referral rate of 9.4% has almost tripled compared with the European Referral study from 1989, which found a 3.7% referral rate in Switzerland [3]. Increased diagnostic and therapeutic options may account for the increase in the referral rate. We used similar definitions of referral as in 1989, but in one specific point our definition differed from the European referral study: we included radiological investigations with involvement of a radiologist (such as CT and MRI scans); these entities were not included in the European referral study, but also were not very common in 1989. Furthermore, radiological interventions that accounted for a fifth of the referrals have to be differentiated from other referrals, especially considering that there is rarely direct contact between radiologist and patient for diagnostic procedures and the results are often communicated by the PCP in a further consultation.
Contemporary referral rates in Switzerland are comparable to recent referral rates in the United States of 9.3% in 2009 [14], but lower than Danish, Norwegian or UK data at 12.7%, 13.7% and 13.9%, respectively [15–17]. Because of the different healthcare systems, the comparison might be limited, especially considering the strong gatekeeper role of PCPs in Denmark, Norway and UK, while in the US direct contact to a specialist is possible. In Switzerland gatekeeping with first contact with a PCP is not mandatory, but insurance companies have introduced managed-care health plans, where patients pay lower monthly fees. Furthermore, specialisation to become a PCP differs: in Switzerland PCPs have comparable training to specialists [18]. In addition, investigative instruments, such as a point-of-care laboratory tests, conventional x-rays and ECG are commonly available in Swiss primary care practices.
This infrastructure (including its reimbursement) might contribute to the number of problems that can be solved in primary care.
However, a referral rate as a proportion of the number of consultations does not completely reflect work in primary care. Often more than one subject is handled within a consultation [6–8]. In our study we confirmed an increasing number of RFE with increasing age; most likely explained by the higher prevalence of chronic conditions and multimorbidity in older patients [19, 20]. To our knowledge, this is the first study using the number of RFE as basis of the referral rate. In our analysis, the most common clinical chapters of RFE resulted in lower referral rates than the average. The highest referral rate was observed for ophthalmological diseases, overall a very rare RFE in primary care, and for which diagnostic and treatment options are very limited in primary care. These data are not very surprising, but just confirm that the most common reasons could be handled best. Additionally, a wide range of RFE was reported in these consultations. A total of 830 different RFE were recorded in this dataset, and only 18 were more frequent than 1%. These figures demonstrate the broad clinical spectrum that can be handled in primary care. Despite different problems within one consultation and the broad variety of clinical problems during consultations, PCPs were able to handle 94.3% of the problems in primary care, which clearly reflects the crucial role of primary care in coordination of care.
Strengths and limitations
We present representative data of 90 PCPs from different regions in Switzerland, collected over a study period of three nonconsecutive months and all weekdays. Data were collected prospectively and not analysed based e.g. on administrative data. Our study is limited by following circumstances. Data were collected on random days throughout the whole year and therefore a long-term observation of a single patient (e.g. with several consultations with the same RFE) was not possible. Our PCPs are from the German-speaking part of Switzerland only and female PCPs are slightly underrepresented; nevertheless, data on consultation content are similar to earlier studies in Swiss primary care. Furthermore, our data collection included data on RFE that were recorded directly by the PCPs. This might underestimate the number of RFE per consultation. With ICPC-2 we used an accepted coding system and achieved a high interrater agreement. Finally our study does not allow any conclusions on adequacy of referrals, quality of care or satisfaction with the referral.
Acknowledgements: This study was based on an idea of the “Qualitätszirkel Brugg” (Dres. Andreas Haefeli, Barbara Röpke and Fredi Bärtschi). Thank you to all 92 PCPs that participated in our study.
References
1 Kringos DS, Boerma W, van der Zee J, Groenewegen P. Europe’s strong primary care systems are linked to better population health but also to higher health spending. Health affairs. 2013;32(4):686–94.
2 Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. The Milbank quarterly. 2005;83(3):457–502.
3 The European study of referrals from primary to secondary care. Concerned Action Committee of Health Services Research for the European Community. Occas Pap R Coll Gen Pract. 1992(56):1–75.
4 Switzerland FOoS. Population of Switzerland 1950–2012 2013 [August 4th 2014]. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/themen/01/02/blank/key/bevoelkerungsstand.html.
5 FMH SMA. Statistics on physicians in Switzerland [interactive webpage]. Swiss Medical Association; 2013 [updated 2013February 16th 2015]. Available from: http://aerztestatistik.myfmh2.fmh.ch/.
6 Litschgi L, Fehr F, Zeller A. Die Konsultation beim Hausarzt: Aufbau, Themen und Redeverteilung. Praxis. 2011;100(18):1085–95.
7 Salisbury C, Procter S, Stewart K, Bowen L, Purdy S, Ridd M, et al. The content of general practice consultations: cross-sectional study based on video recordings. The British journal of general practice: the journal of the Royal College of General Practitioners. 2013;63(616):e751–9.
8 Beasley JW, Hankey TH, Erickson R, Stange KC, Mundt M, Elliott M, et al. How many problems do family physicians manage at each encounter? A WReN study. Ann Fam Med. 2004;2(5):405–10.
9 Rosemann T, Marty F, Bhend H, Wagner J, Brunner L, Zoller M. Utilisation of information technologies in ambulatory care in Switzerland. Swiss Medical Wkly. 2010;140:w13088.
10 Chmiel C, Bhend H, Senn O, Zoller M, Rosemann T. The FIRE project A milestone for research in primary care in Switzerland. Swiss Med Wkly. 2011;141.
11 Vehvilainen AT, Kumpusalo EA, Takala JK. They call it stormy Monday – reasons for referral from primary to secondary care according to the days of the week. Brit J Gen Pract. 1999;49(448):909–11.
12 ICPC-2-R. International Classification of Primary Care. Revised Second Edition. Oxford: Oxford University Press; 2005. 2005.
13 Frese T, Herrmann K, Bungert-Kahl P, Sandholzer H. Inter-rater reliability of the ICPC-2 in a German general practice setting. Swiss Med Wkly. 2012;142:w13621.
14 Barnett ML, Song Z, Landon BE. Trends in physician referrals in the United States, 1999–2009. Arch Intern Med. 2012;172(2):163–70.
15 Moth G, Olesen F, Vedsted P. Reasons for encounter and disease patterns in Danish primary care: changes over 16 years. Scand J Prim Health Care. 2012;30(2):70–5.
16 Ringberg U, Fleten N, Deraas TS, Hasvold T, Forde O. High referral rates to secondary care by general practitioners in Norway are associated with GPs’ gender and specialist qualifications in family medicine, a study of 4350 consultations. BMC Health Serv Res. 2013;13:147.
17 Forrest CB, Majeed A, Weiner JP, Carroll K, Bindman AB. Comparison of specialty referral rates in the United Kingdom and the United States: retrospective cohort analysis. BMJ. 2002;325(7360):370–1.
18 Djalali S, Frei A, Rosemann T, Tandjung R. Vocational training for general practitioners-comparing Switzerland with other European countries. Praxis (Bern 1994). 2013;102(6):327–33.
19 Rizza A, Kaplan V, Senn O, Rosemann T, Bhend H, Tandjung R. Age- and gender-related prevalence of multimorbidity in primary care: the Swiss FIRE project. BMC Fam Pract. 2012;13:113.
20 Busato A, Bhend H, Chmiel C, Tandjung R, Senn O, Zoller M, et al. Improving the quality of morbidity indicators in electronic health records in Swiss primary care. Swiss Med Wkly. 2012;142:w13611.