Focused use of drug screening in overdose patients increases impact on management
DOI: https://doi.org/10.4414/smw.2015.14242
Andreas
Erdmann, Dominique
Werner, Olivier
Hugli, Bertrand
Yersin
Summary
Drug poisoning is a common cause for attendance in the emergency department. Several toxicology centres suggest performing urinary drug screens, even though they rarely influence patient management.
STUDY OBJECTIVES: Measuring the impact on patient management, in a University Emergency Department with approximately 40 000 admissions annually, of a rapid urinary drug screening test using specifically focused indications. Drug screening was restricted to patients having a first psychotic episode or cases demonstrating respiratory failure, coma, seizures, a sympathomimetic toxidrome, severe opiate overdose necessitating naloxone, hypotension, ventricular arrhythmia, acquired long QT or QRS >100 ms, and high-degree heart block.
METHODS: Retrospective analysis of Triage® TOX drug screen tests performed between September 2009 and November 2011, and between January 2013 and March 2014.
RESULTS: A total of 262 patients were included, mean age 35 ± 14.6 (standard deviation) years, 63% men; 29% poisoning with alcohol, and 2.3% deaths. Indications for testing were as follows: 34% were first psychotic episodes; 20% had acute respiratory failure; 16% coma; 8% seizures; 8% sympathomimetic toxidromes; 7% severe opioid toxidromes; 4% hypotension; 3% ventricular arrhythmias or acquired long QT intervals on electrocardiogram. A total of 78% of the tests were positive (median two substances, maximum five). The test resulted in drug-specific therapy in 6.1%, drug specific diagnostic tests in 13.3 %, prolonged monitoring in 10.7% of methadone-positive tests, and psychiatric admission in 4.2%. Overall, 34.3% tests influenced patient management.
CONCLUSIONS: In contrast to previous studies showing modest effects of toxicological testing, restricted use of rapid urinary drug testing increases the impact on management of suspected overdose patients in the ED.
Introduction
Drug poisoning due to psychotropic medication or illegal drug use is frequent in emergency departments (EDs). In most cases, supportive treatment alone is sufficient without the need for specific drug identification. However, severe intoxication with unknown substances is considered an indication for urinary drug screening by several toxicology centres, despite very limited influence on therapeutic decisions [1].
A thorough history and exploration of the environment by relatives, friends, witnesses and paramedics is mandatory, but the reliability of information provided and the personal history in intoxicated and/or psychiatric ED patients are often limited [2, 3]. In these situations, there is an unmet need for precise information concerning potential drug poisoning. Consequently, laboratory screening of susceptible patients is widely utilised, including qualitative urinary drug screening tests providing rapid results. Other more expensive methods such as liquid or gas chromatography and mass spectrometry are rarely used. Guidelines from several toxicology centres recommend testing in severe drug poisoning where the responsible agents are unknown [4]; however, in adult psychiatric patients with stable vital signs, routine testing is discouraged by the American College of Emergency Physicians (ACEP) guidelines [5]. Data on the impact of toxicology tests on patient management are, however, scarce and have shown relatively little impact, if any [1, 6–11]. To date, no study done amongst nontrauma emergency patients using focused indications for drug screening has been published and no such clinical trial is currently under way ( http://www.clinicaltrials.gov ; 16.08.2015).
The purpose of this study was to investigate whether focused use of rapid drug screening tests has an impact on treatment decisions.
Patients and methods
This monocentric study was performed at the ED of our university hospital, which serves as a primary care centre for our city, as well as a tertiary care centre for our and neighbouring cantons. The ED admits around 40 000 patients every year.
We performed a retrospective analysis of the patients’ medical records for all 262 rapid urinary drug screening tests performed between September 2009 and November 2011, and between January 2013 and March 2014 for ED patients over 18 years of age. Data for the intervening 113 tests performed between December 2011 and December 2012 were unavailable, owing to the loss of the laboratory database during this period. However, our rules for requesting drug screening tests and outlining drug poisoning treatment remained unchanged during this period. In our institution, we had developed certain clinical criteria for screening patients, aimed at improving patient selection and so enhancing the positive yield of toxicology testing. We used the prediction criteria for severe overdoses requiring intensive care defined by Brett et al. [12], in addition to other criteria (table 1).
Once hypoglycaemia was excluded, attending physicians were obliged to complete a specific form to order the test, noting the presence of at least one of the mandatory criteria and also noting the expected impact of the test result on patient management from the following list: (1) treatment decision, (2) diagnostic decision, (3) duration of monitoring (i.e. methadone), (4) patient admission (i.e., transfer to a psychiatric ward). Physicians were informed that the test detected therapeutic as well as toxic levels of paracetamol and that treatment decisions related to paracetamol should thus be based on quantitative tests [13].
We used the Triage® TOX drug screen (Biosite Inc., San Diego, CA, USA), a fluorescence immunoassay using 11 distinct monoclonal antibodies for the simultaneous qualitative determination of paracetamol, amphetamines, methamphetamines, barbiturates, benzodiazepines, cocaine, methadone, opioids, phencyclidine, cannabinoids or tetrahydrocannabinoids and tricyclic antidepressants. Test results were interpreted by the Triage MeterPro from Biosite Inc., an automatic scanner minimising the possibility of ambiguous results. Threshold concentrations, and sensitivity and specificity data for each molecule are displayed in the appendix.
Based on a retrospective analysis of medical records, we considered the following decisions as triggered by test results: (1) administration of a specific antidote (N-acetylcysteine, flumazenil or naloxone), (2) administration of any other considered drug-specific treatment, (3) completion of further drug-specific diagnostic tests, (4) change in a patient’s admission orientation if the indication was a first psychotic episode (i.e. admission to a general ward if the test was positive vs psychiatric ward if negative), or (5) continuous electrocardiogram monitoring in the ED for methadone-positive cases. Drug-specific treatments were, for example, administration of N-acetylcysteine if testing for paracetamol was positive and then confirmed by quantitative analysis, bicarbonate in tricyclic antidepressant positive patients, naloxone in opioid, or flumazenil in benzodiazepine positive patients, and any decision prior to test results was interpreted as not test-triggered. (An overview of the drug-related criteria which were used is shown in table 2.)
Medical decisions taken only after test results were available were interpreted as being based on the test results. The study protocol was approved by our local ethics committee.
|
Table 1: Restrictive indications for toxicological screening in the emergency department for suspected overdose. |
| Acute respiratory failure (pCO2 45–80 mm Hg or emergency intubation) |
| Seizures |
| Coma / Glasgow coma scale score ≤8 |
| Systolic hypotension (<80 mm Hg) |
| Acquired QRS enlargement (QRS >100 ms) |
| QT interval prolongation (QT >480 ms) |
| Severe ventricular arrhythmia (ventricular tachycardia or flutter, or torsades de pointes) |
| New ≥2nd degree heart block |
| Opioid toxidrome treated with naloxone |
| Sympathomimetic toxidrome |
| First psychotic episode |
|
Table 2:Drug specific tests, disposition or therapeutic decisions based on a positive result of the urine drug screening. |
|
Screened substance
|
Other tests / disposition
|
Therapeutic decision
|
| Paracetamol |
Serum paracetamol concentration
Liver enzymes |
Administration of N-acetylcysteine |
| (Met)amphetamines |
Creatine kinase
Liver enzymes |
Administration of nitrates, NaCl 3% (in the case of hyponatraemia), aggressive hydration, bicarbonate |
| Benzodiazepines |
|
Administration of flumazenil |
| Cocaine |
Creatine kinase, troponin, computed tomography if aortic dissection or subarachnoid haemorrhage suspected |
Administration of nitrates, acetylsalicylic acid, nitroprusside, and/or phentolamine.
No beta-blockers. |
| Methadone/opiates |
Prolonged monitoring if methadone positive |
Administration of naloxone |
| Tricyclic antidepressants |
Electrocardiogram |
Administration of bicarbonate |
| All |
Somatic hospitalisation if first psychotic episode and test positive / transfer to psychiatry if negative |
|
Results
Between September 2009 and November 2011, and between January 2013 and March 2014, 262 urine toxicology screening tests were performed. The mean patient age was 35 years ± 14.6 (standard deviation [SD]) (range 16–88 years); 63% were men; 76 patients (29%) had concomitant poisoning with alcohol (blood alcohol level >11 mmol/l). Six patients (2.3%) died, one of a fatal overdose (rapid test positive for benzodiazepines, opiates, methadone, cannabinoids), one of an intracranial haemorrhage attributed to cocaine abuse despite a negative urine screening test, one of a diphenhydramine overdose with a positive benzodiazepine test, one of a fatal subarachnoid haemorrhage with a negative drug screen, one of multiple stab wounds with a negative drug screen, one a recipient of a liver transplant with positive tests for paracetamol and tricyclic antidepressants.

Figure 1
Indications for urinary drug screening (n = 369) in 262 patients.
Arrhythmia or long QT = QT prolongation >480 ms, or ventricular tachycardia or flutter, or torsade de pointes tachycardia; Hypotension = systolic hypotension (<80 mm Hg); Opiate toxidrome = if requiring antagonist administration; Psychosis = first psychotic episode; Resp failure = acute respiratory failure (pCO2 45‑80 mm Hg or emergency intubation); Sympathomimetic = clinical signs of sympathomimetic toxicity

Figure 2
Spectrum of substances detected with the Triage® TOX screen (204 positive urine samples with 348 substances detected).
AMP = amphetamines; BAR = barbiturates; BZO = benzodiazepines; COC = cocaine; MAMP = metamphetamines; MTD = methadone; OPI = opiates; PAR = paracetamol; TCA = tricyclic antidepressants; THC = tetrahydrocannabinoids
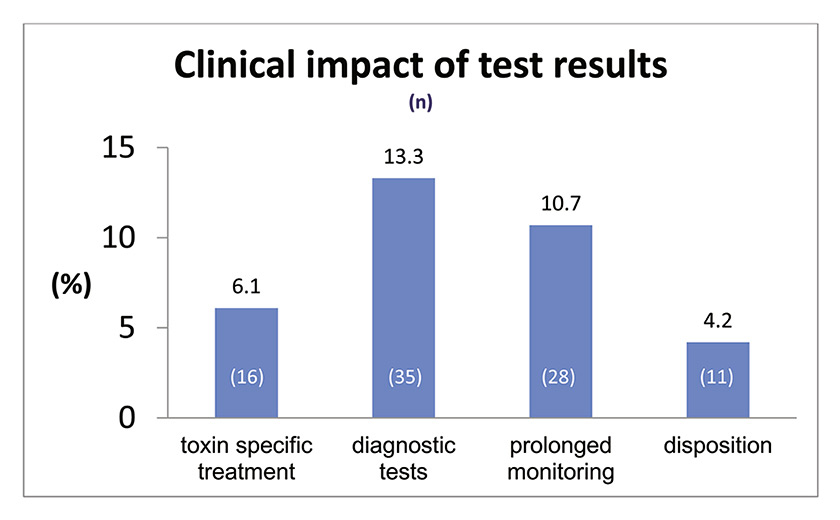
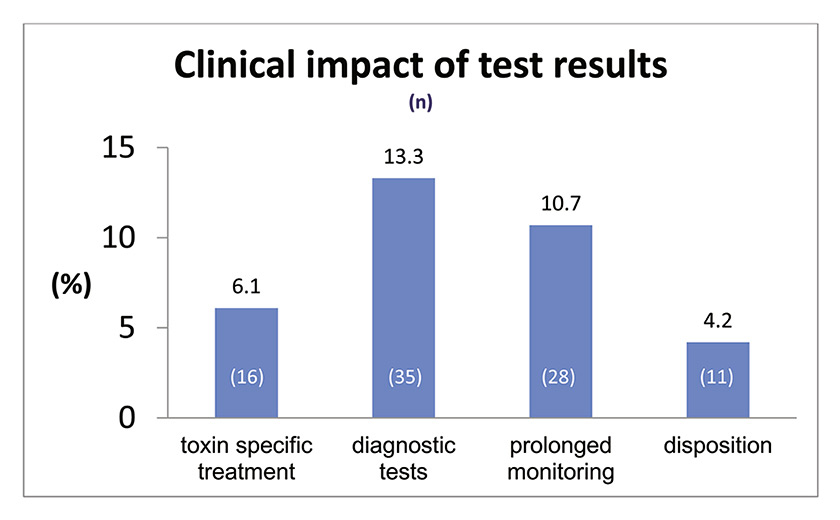
Figure 3
Impact of test results on clinical decisions (in %, n = 90) consecutive to the detection of substances with the Triage® TOX drug screen (n = 262 tests). Toxin-specific administration of naloxone, flumazenil or N-acetycysteine or other drug-specific treatments after test results.
Diagnostic tests = drug-related diagnostic tests ordered after test result; disposition = psychiatry transfer influenced by negative screening / somatic transfer if positive; prolonged monitoring = longer monitoring when methadone positive
Test indications (fig. 1) were a first psychotic episode in 126 (34%), acute respiratory failure in 75 (20%), coma in 59 (16%), seizures in 29 (8%), severe opioid toxidrome in 26 (7%), sympathomimetic toxidrome in 28 (8%), hypotension in 15 (4%), and severe ventricular arrhythmia or acquired long QT syndrome in 11 (3%). Many patients had more than one test indication leading to a total number of 369 reported indications in 262 patients.
204 urine tests (78%) were positive, including 92 (35%) for more than one drug. Altogether, 348 substances were detected, with a median of two per patient and a maximum of five (fig. 2). None of the 262 patients was tested positive for phencyclidine.
The tests resulted in prescription of a drug-specific therapy in 16 (6.1%) cases, in drug-specific additional diagnostic tests in 35 (13.3%), in prolongation of monitoring in 28 patients (10.7%) with tests positive for methadone, and in the patient’s psychiatry admission in 11 (4.2%). Altogether 90 patients (34.3%) had their management influenced by the rapid urine drug screen.
Discussion
Our study shows that focused indications for urine drug testing in ED patients with suspected drug poisoning does change patient management in more than one in three patients. Our results confirm results of Fabbri et al., who reported that focused toxicological testing increases interobserver agreement on patient placement and management and leads to reduced admission rates [14]. On the other hand, unrestricted use of urinary drug testing influenced patient management in only 4.4% [6] or not at all [1]. Equally, in an urban psychiatric emergency service, routine drug screening tests had no effect on patient management [7]. Similarly, in paediatric overdose patients, one study showed only 3% treatment changes [8], while others did not report any impact on treatment and/or placement [9, 10].
Consequently, better patient selection appears to be the key determinant in terms of the usefulness of urinary drug screening tests. A Swiss study on 74 patients concluded that testing was justified in only 28%, but the authors did not detail the exact impact on treatment decisions [11]. In trauma patients, a clinical decision rule selecting patients for screening based on age, hour of the day, day of the week and type of trauma was suggested. This rule reduced screening by 48%, missing only 5% of true overdoses [15]. However this rule has not yet been prospectively validated.
In other studies, the yield of screening using a comprehensive test detecting 900 substances, ranged from 18% in unselected emergency patients [16] to 64% [17], much lower than the 78% in our highly selected patients. This higher proportion of positive tests underlines the usefulness of insisting on focused indications for testing, especially given the costs generated by these tests (CHF 155.60 each).
Rapid urinary drug screening tests, however, have their specific limitations; they are mostly immunoassays, recognising parts of the molecular structure of a substance or its metabolites, and were developed originally to screen employees for substance abuse. Their cut-off limits are not adapted to identify overdoses and do not provide quantitative information [18]. Moreover, there are many reports of false positive and false negative tests, thus limiting the accuracy of these tests [19]. On the other hand, rapid tests alone have the potential to influence specific management of patients presenting with drug-poisoning in the ED. However, most urinary toxicology screening tests only detect a limited number of substances. Designer drugs are detected with highly variable sensitivity. In our study, two patients died of drug overdose, one because of the antihistamine diphenhydramine, which is not detected by the test. A negative drug screen can thus lead inexperienced physicians erroneously to exclude an overdose. Positive drug screens indicate the presence of a substance, and do not confirm overdose, and must be interpreted cautiously in the clinical context of the patient. Therefore, education about the specific characteristics of each screening test is essential prior to their implementation. In our institution, there is clear notification on the test order form for doctors concerning the limitations of the test. As the test does not detect cholinergic and anticholinergic drugs, which, furthermore, require supportive treatment, the related toxidromes are not listed in the indications.
There are some limitations in our study: it was a monocentric and retrospective analysis of a highly selected patient population, which corresponds to a small percentage of 40 000 annual ED patients in our institution.
In-patient placement was sometimes incompletely documented. Other diagnostic tests may also have been conducted in parallel with the rapid toxicology screening test, especially timing of blood tests for parameters considered routine like creatine kinase or liver enzymes, and interference with the results of these other tests cannot be excluded, making our assumptions on clinical decision-making possibly flawed. Our study addressed the potential overuse of a rapid screening test, but its retrospective design prevented the documentation of underuse. We observed longer monitoring periods for methadone-positive patients and concluded the prolongation of monitoring to be a decision triggered by the test.
In conclusion, our study shows that the restrictive use of a rapid drug screening test increases its efficiency in relation to a change in the management of severe drug poisoning. Our focused policy has the potential both of improving patient management, and reducing costs generated by unnecessary laboratory tests or inappropriate admission. However, our policy needs to be validated prospectively in other settings. With the proviso that supportive care must continue to be based on the suspected cause of poisoning based on patient and witness histories, toxidromes, and clinical findings, qualitative tests have a place in specific selected cases.
Appendix
| Threshold concentrations for a presumptive positive result with the Triage® TOX drug screen. |
|
Drug class screened
|
Calibrated compound
|
Threshold concentration of calibrated compound
|
| Paracetamol |
Paracetamol |
5 μg/ml |
| Amphetamines |
d-Amphetamine |
1000 ng/ml |
| Metamphetamines |
d-Methamphetamine |
1000 ng/ml |
| Barbiturates |
Pentobarbital |
300 ng/ml |
| Benzodiazepines |
Estazolam |
300 ng/ml |
| Cocaine |
Benzoylecgonine |
300 ng/ml |
| Methadone |
d/l-Methadone |
300 ng/ml |
| Opiates |
Morphine |
300 ng/ml |
| Phencyclidine |
Phencyclidine |
25 ng/ml |
| Cannabinoids/tetrahydrocannabinoids |
11-nor-9 carboxy-Δ9-THC |
50 ng/ml |
| Tricyclic antidepressants |
Desipramine |
1000 ng/ml |
| Sensitivity / Specificity for cut-off concentrations of Triage® TOX drug screen for each detected compound as compared with gas chromatography-mass spectrometry (GC/MS), except high-performance liquid chromatography (HPLC) for tricyclic antidepressants (data provided from manufacturer’s brochure). |
|
Drug class screened
|
Sensitivity (%)
|
Specificity (%)
|
| Paracetamol |
100 |
95 |
| Amphetamines |
95 |
98.4 |
| Metamphetamines |
97.5 |
96.8 |
| Barbiturates |
100 |
81.4 |
| Benzodiazepines |
97.9 |
97.3 |
| Cocaine |
91.9 |
100 |
| Methadone |
100 |
84.2 |
| Opiates |
100 |
90.7 |
| Phencyclidine |
100 |
97.6 |
| Cannabinoids/tetrahydrocannabinoids |
100 |
84.4 |
| Tricyclic antidepressants |
92.1 |
90.2 |
| Sensitivity / Specificity for cut-off concentrations of Triage® TOX drug screen for each detected compound as compared with Microgenics cloned enzyme donor immunoassay (CEDIA) or DRI (tricyclic antidepressants) methods on a Roche Hitachi 917 (data calculated from unpublished data, Scholer A. University Hospital Basel 2007, 50 urine samples). All discrepant results were confirmed by LCMS mass spectrometry (LCMSMS) (benzodiazepines, THC-carbonic acid), liquid chromatography-mass spectrometry (LCMS) (opiates, cocaine plus metabolites, amphetamine class) and other immunoassays; acetaminophen on DADE Dimension or, if enough sample material, HPLC (acetaminophen). |
|
Drug class screened
|
Sensitivity (%)
|
Specificity (%)
|
| Paracetamol |
88.9 |
100 |
| Amphetamines + metamphetamines |
100 |
100 |
| Barbiturates |
100 |
100 |
| Benzodiazepines |
95.6 (100)* |
100 |
| Cocaine |
100 |
100 |
| Methadone |
100 |
100 |
| Opiates |
100 |
100 |
| Cannabinoids/tetrahydrocannabinoids |
100 |
100 |
| Tricyclic antidepressants |
25 |
97.6 |
| * Urine sample was negative as confirmed by chromatography resulting in sensitivity of Triage® TOX drug screen of 100%. Phenylcyclidine negative samples were not further tested. |
References
1 Montague RE, Grace RF, Lewis JH, Shenfield GM. Urine drug screens in overdose patients do not contribute to immediate clinical management. Ther Drug Monit. 2001;23(1):47–50.
2 Perrone J, De Roos F, Jayaraman S, Hollander JE. Drug screening versus history in detection of substance use in ED psychiatric patients. Am J Emerg Med. 2001;19(1):49–51.
3 Tijdink JK, van den Heuvel J, Vasbinder EC, van de Ven PM, Honig A. Does on-site urine toxicology screening have an added diagnostic value in psychiatric referrals in an emergency setting? Gen Hosp Psychiatry. 2011;33(6):626–30.
4 Wu AH, McKay C, Broussard LA, Hoffman RS, Kwong TC, Moyer TP, et al.; National Academy of Clinical Biochemistry Laboratory Medicine. National academy of clinical biochemistry laboratory medicine practice guidelines: recommendations for the use of laboratory tests to support poisoned patients who present to the emergency department. Clin Chem. 2003;49(3):357–79 (revised & updated 2005)
5 Lukens TW, Wolf SJ, Edlow JA, Shahabuddin S, Allen MH, Currier GW, et al. Clinical Policy: critical issues in the diagnosis and management of the adult Psychiatric patient in the Emergency Department. Ann Emerg Med. 2006;47:79–99.
6 Kellermann AL, Fihn SD, LoGerfo JP, Copass MK. Impact of drug screening in suspected overdose. Ann Emerg Med. 1987;16(11):1206–16.
7 Schiller MJ, Shumway M, Batki SL. Utility of routine drug screening in a psychiatric emergency setting. Psychiatr Serv. 2000;51(4):474–8.
8 Belson MG, Simon HK, Sullivan K, Geller RJ. The utility of toxicologic analysis in children with suspected ingestions. Pediatr Emerg Care. 1999;15(6):383–7.
9 Fortu JM, Kim IK, Cooper A, Condra C, Lorenz DJ, Pierce MC. Psychiatric patients in the pediatric emergency department undergoing routine urine toxicology screens for medical clearance: results and use. Pediatr Emerg Care. 2009;25(6):387–92.
10 Belson MG, Simon HK. Utility of comprehensive toxicologic screens in children. Am J Emerg Med. 1999;17(3):221–4.
11 Jolivet P, Vuille G, Kehtari R. “Extensive” toxicologic research in emergencies: a luxury or a necessity? Rev Med Suisse Romande. 2003;123(4):235–7.
12 Brett AS, Rothschild N, Gray R, Perry M. Predicting the clinical course in intentional drug overdose. Implications for use of the intensive care unit. Arch Intern Med. 1987;147(1):133–7.
13 Ingram DN, Bosse GN, Womack EP, Jortani S. Evaluation of a urine screen for acetaminophen. J Med Toxicol. 2008;4(2):96–100.
14 Fabbri A, Marchesini G, Morselli-Labate AM, Ruggeri S, Fallani M, Melandri R, et al. Comprehensive drug screening in decision making of patients attending the emergency department for suspected drug overdose. Emerg Med J. 2003;20(1):25–8.
15 Langdorf MI, Rudkin SE, Dellota K, Fox JC, Munden S. Decision rule and utility of routine urine toxicology screening of trauma patients. Eur J Emerg Med. 2002;9(2):115–21.
16 Inuzuka S, Hayashida M, Nihira M. An investigation of drug abuse and the utility of toxicology screening for use in emergency centers. Nippon Ika Daigaku Zasshi. 1997;64(4):344–52.
17 Fabbri A, Ruggeri S, Marchesini G, Vandelli A. A combined HPLC-immunoenzymatic comprehensive screening for suspected drug poisoning in the emergency department. Emerg Med J. 2004;21(3):317–22.
18 Tenenbein M. Do you really need that emergency drug screen? Clin Toxicol 2009;47(4):286–91.
19 Moeller KE, Lee KC, Kissack JC. Urine drug screening: practical guide for clinicians. Mayo Clin Proc. 2008;83(1):66–76.