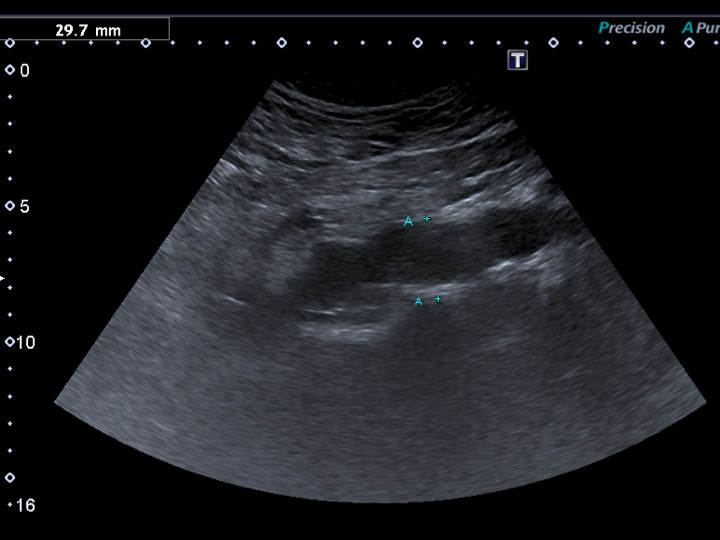
Figure 1
Previously undiagnosed small abdominal aortic aneurysm detected on vascular duplex ultrasound in a 62-year-old smoker with erectile dysfunction, otherwise asymptomatic regarding cardiovascular disease.
DOI: https://doi.org/10.4414/smw.2015.14268
The three most common sexual dysfunctions in males are decreased libido, erectile dysfunction (ED) and ejaculatory dysfunction. ED is a common problem in primary care and currently affects more than 150 million men worldwide, with a projected prevalence increase to 322 million men by the year 2025 [1]. ED has a significant impact on patients’ quality of life, self-confidence and interpersonal relations.
ED is defined as the recurrent or persistent inability to achieve or maintain an erection in order for satisfactory sexual intercourse to occur and may be caused by both nonorganic and organic factors.
Whereas the pathogenesis of organic ED may frequently be multifactorial, vascular, endocrine or drug treatment are among its leading causes [2]. Besides the functional impairment associated with the presence of ED for which patients present to their general practitioner, the latter may be an important sentinel symptom for an underlying undiagnosed cardiovascular disease [3]. There is a growing body of evidence indicating that ED shares aetiological and pathophysiological origins with cardiovascular disease and that it may be a sentinel symptom indicating a future threat of myocardial infarction, peripheral arterial disease or stroke [3]. Remarkably, up to 70% of patients with new onset angina pectoris and angiographically verified coronary artery disease report a history of ED [3]. Unsurprisingly, the risk factor profile is similar across these different vascular disorders and commonly includes diabetes mellitus, arterial hypertension, dyslipidaemia and cigarette smoking as well as increased age.
During the past two decades, treatment of ED has evolved considerably, and was revolutionised by the introduction of phosphodiesterase-5 (PDE5) inhibitors in the late 1990s. The latter are currently considered the first-line therapy for erection problems.
The purpose of the present article is to provide an overview on current diagnostic and treatment options for patients with ED.
Erectile dysfunction is a burden for both affected men and their partners. It remains problematic for many patients with ED to consult a healthcare professional. Therefore, the most important task for the general practitioner is to ask their patients whether they suffer from ED [4].
Specifically, patients at risk for ED, i.e. with underlying medical conditions promoting ED, need to be identified. Most important risk factors are traditional cardiovascular risk factors such as cigarette smoking, diabetes mellitus, obesity, dyslipidaemia and arterial hypertension.
Workup of patients with ED should include a detailed medical, sexual and psychosocial history, an identification of underlying cardiovascular risk factors (obesity, arterial hypertension, diabetes mellitus, smoking, family history) and physical examination with a basic neurological and vascular work-up. Current medication should be assessed, as various substances can have a negative impact on erectile function (table 1). Neurogenic disorders need to be evaluated carefully, i.e. spinal cord injuries, cerebrovascular insults or polyneuropathies. Previous surgery in the pelvis or radiotherapy can be an underlying cause for ED and needs to be evaluated (table 1). Further, psychological causes such as anxiety, depression or stress should be ruled out. For assessment of ED, a standardised questionnaire can be used: the International Index of Erectile Function or Sexual Health Inventory for men (IIEF; see appendix) [5, 6].
Blood tests should include lipid status (total cholesterol, low-density lipoprotein (LDL)-cholesterol, high-density lipoprotein (HDL)-cholesterol, triglycerides, glycated haemoglobin (HbA1c), basic blood measurements to exclude underlying renal or liver insufficiency, and urinary albumin excretion [7]. Hypogonadism must be excluded by measuring total testosterone (8:00 a.m.). Because of the considerable intraindividual day-to-day variation of total testosterone levels a second sample to confirm hypogonadism is suggested [8]. Age-related reference ranges of total testosterone should be considered [9]. In cases of confirmed low morning total testosterone levels, further workup by an endocrinologist is recommended.
ED not only shares risk factors with coronary artery disease, but is rather a marker of a significantly increased risk of cardiovascular disease, coronary artery disease, stroke and all-cause mortality [10]. Since ED occurs with a time window of 2–5 years before the onset of a cardiac event [11], the general practitioner or internist must seize the chance to use a first anamnestic sign to detect a serious underlying condition.
| Table 1: Important causes of erectile dyfunction. | |
| Vascular | Arteriosclerotic Diabetic microangiopathy Pelvic irradiation |
| Endocrine | Hypogonadism, diabetes mellitus |
| Neurogenic | Central (e.g., cerebral insult, spinal cord injury, multiple sclerosis) Peripheral neuropathy (diabetes mellitus, alcoholic neuropathy, other polyneuropathies) |
| Systemic diseases | e.g. respiratory, cardiac, renal, liver insufficiency |
| Local | Cavernous nerve injury after pelvic surgery Pelvic irradiation Cavernous fibrosis Peyronie’s disease Penile fracture |
| Drug induced | Antiandrogens – spironolactone, flutamide, ketoconazole – gonadotropin releasing hormone agonists (e.g., goserelin) – chemotherapy (cyclophosphamide, busulfan) Antihypertensives– thiazide diuretics – β-blockers – calcium channel blockers Antiarrhythmics – digoxin – amiodarone – disopyramide Statins – controversial evidence Psychotropic drugs – tricyclic antidepressants – selective serotonin reuptake inhibitors – phenothiazines – butyrophenones Recreational drugs (e.g., alcohol, tobacco, marijuana, cocaine, opiates) |
| Psychogenic | e.g. traumatic past experiences, relationship problems |
| Adapted from Ghanem and Shamloul [5] | |
Taking care of diabetic and hypogonadal patients, this specialist overlooks a selection of patients with a notably high risk of erectile dysfunction. Therefore, this condition must be kept in mind at any consultation with these patients. In patients with newly diagnosed hypogonadism, the endocrinologist/diabetologist further evaluates the reason the patient suffers from hypogonadism. The diagnostic steps in erectile dysfunction with suspicion of hypogonadism are described on page 18 in the pocket guide of the EndoDiabNet (Kantonsspital Aarau AG, University Hospital Basel, Kantonsspital Lucerne) [12]. To differentiate primary from secondary or tertiary hypogonadism, luteinising hormone (LH) and follicle stimulating hormone (FSH) levels have to be determined and a gonadotropin-releasing hormone (GnRH) test has to be performed. Elevated LH and FSH levels (>10 mU/l) and peak LH >30 mU/l after GnRH administration are typical for primary hypogonadism (e.g. Klinefelter’s syndrome, cryptorchidism, orchitis). The GnRH test helps to differentiate secondary hypogonadism (LH peak <15 mU/l, e.g. hyperprolactinaemia, hypopituitarism) from tertiary hypogonadism (LH peak >15 mU/l; e.g. obesity, partial androgen deficiency of the aging male, comorbidities).
In cases of anatomic anomalies of the penis, a urological consultation can be helpful. Penile anomalies can be assessed and treated if necessary (i.e. Peyronie’s disease, phimosis, frenulum breve, etc.).
Nocturnal penile rigidity (RIGISCAN) can be measured to assess erectile function during sleep. In this examination, the rigidity of the penis is recorded overnight. Furthermore, dynamic Doppler ultrasound can be performed with intracavernous injection of aprostadil to induce erection and measure arterial perfusion of the penis with corresponding velocity. The measurement allows impaired arterial perfusion of the penis to be documented or ruled out.
Cavernosometry and carvernosography can assist in differentiating between arterial and venous abnormalities. In these examinations intracavernous pressure is measured when inducing artificial erection and with radiographic contrast medium venous leakage of the penis can be assessed.
Besides venous leakage, an incompetence of the penile veins to store blood in the corpora cavernosa during sexual intercourse, for which currently no ideal therapy exists, arterial obstructions of aortoiliac and pelvic arteries may lead to restriction of blood flow to the penis thereby resulting in an inability to achieve and maintain an erection sufficient for satisfactory intercourse.
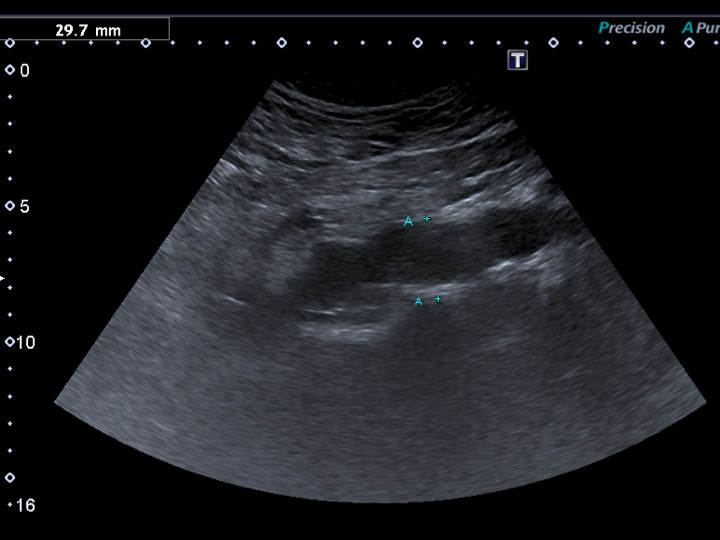
Figure 1
Previously undiagnosed small abdominal aortic aneurysm detected on vascular duplex ultrasound in a 62-year-old smoker with erectile dysfunction, otherwise asymptomatic regarding cardiovascular disease.
Cardiovascular workup in patients with ED and cardiovascular risk factors may both enable early detection of patients at increased risk for cardiovascular events and provide improvement of symptoms related to vascular ED [3, 13]. Therefore, patients with symptoms of ED and the presence of cardiovascular risk factors should be referred for arterial workup.
Arterial workup of ED patients with cardiovascular risk factors primarily consists of a noninvasive haemodynamic workup such as oscillometry and assessment of ankle-brachial index. In addition, duplex-sonographic workup of erection-related arteries (i.e. abdominal aorta, common and internal iliac arteries) is warranted. Given the association of vascular ED with the potential presence of peripheral arterial disease, duplex-sonographic evaluation of the femoropopliteal and carotid arteries may be considered.
Figure 1 shows a sonographic depiction of a previously undiagnosed abdominal aortic aneurysm in an otherwise healthy and asymptomatic smoker referred for vascular workup of erectile dysfunction.
To quantify arterial perfusion, penile duplex sonography is warranted during an erection pharmacologically induced via intracavernosal injection of alprostadil (10 to 40 μg) [14].
The first step in treatment of patients with ED is to eliminate modifiable risk factors. In obese patients loss of weight and increase of physical activity may result in a reduction of ED symptoms in 30% [15]. A balanced diet, cessation of smoking, and reduction of stress and alcohol consumption may assist in increasing erectile function.
After a thorough search for underlying chronic conditions, these should be treated according to international guidelines. Blood sugar has to be optimised on the basis of individual preconditions [16]. In the case of diabetic patients with ED, other late complications of diabetes mellitus must be looked for: testing for microalbuminuria, retinoscopy, foot examination including sensitivity. In patients with cardiovascular risk factors and ED, other manifestations of atherosclerosis must be excluded. Exercise tolerance should be established before the initiation of ED therapy regardless of cardiovascular risk [10].
In cases of anxiety, depression or stress, psychological or psychiatric treatment should be considered.
The safety and efficacy of phosphodiesterase 5 (PDE5) inhibitors has been well documented. First-line therapy for the treatment of ED is medication with a PDE5 inhibitor. At present, sildenafil, vardenafil and tadalafil are available in Switzerland, also avanafil will soon be available. A contraindication for the use of PDE5 inhibitors is the intake of nitrates, and patients with severe cardiovascular comorbidities should not use a PDE5 inhibitor (fig. 2, table 2). There are no clearly defined guidelines as to which patients should not get a PDE5 inhibitor. Studies with PDE5 inhibitors have often excluded patients after myocardial infarction within the last 90 days or New York Heart Association (NYHA) grade II cardiac insufficiency. It seems appropriate to wait at least 90 days after a cardiac event or, if in doubt to consult a cardiologist, before initiating PDE5 inhibitor.
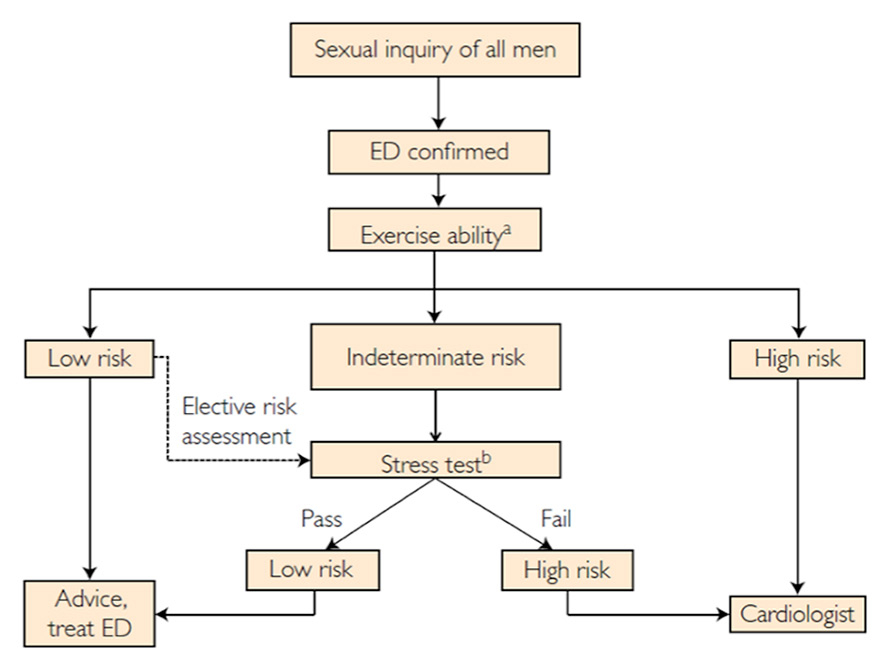
Figure 2
Management of erectile dysfunction (ED) in patients with cardiovascular disease.
a Sexual activity is equivalent to walking 1 mile on the flat in 20 min or briskly climbing two flights of stairs in 10 seconds.
bSexual activity is equivalent to 4 minutes of the Bruce treadmill protocol.
Adapted from Nehra A, Jackson G, Miner M, Billups KL, Burnett AL, Buvat J, et al. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clin Proc. 2012;87(8):766–78, reprinted with permission.
The practical differences between the various PDE5 inhibitors are most importantly their time of onset of action, their half-life and price. PDE5 inhibitors are normally not reimbursed by healthcare insurers. For sildenafil, generic alternatives are available and therefore treatment costs are slightly lower for this PDE5 inhibitor.
Success in 60–75% of treatment-naïve ED patients can expected upon initiation of a PDE5 inhibitor. It is well documented in the literature that at least two to eight attempts for sexual intercourse under PDE5 inhibition should be performed before changing the substance or increasing the dosage.
Substitution of testosterone should only be administered in patients with confirmed hypogonadism, since a benefit of testosterone substitution has been shown only in men with hypogonadal testosterone levels [8, 17–19]. Age-specific reference ranges have to be considered since serum testosterone levels are lower with increasing age [9]. Data on potential risks of testosterone replacement (prostate hypertrophy, acceleration of prostate cancer, cardiovascular events) are controversial. Large, carefully designed and long-term studies investigating these side-effects of testosterone replacement are lacking. Therefore, any patient treated with testosterone replacement should be carefully monitored for prostate hypertrophy, prostate cancer, haematocrit >50% and cardiovascular events at baseline, at 3 and 6 months and then annually [8, 20].
The endocrinologist/diabetologist has to initiate testosterone substitution once substitution is indicated, and has to evaluate whether the dosage and/or substitution interval of testosterone are adequate to achieve sufficient testosterone levels. Treatment of secondary or tertiary hypogonadism in men wishing to sustain fertility requires gonadotropin substitution and therefore necessitates profound endocrinological or andrological knowledge.
Especially diabetic patients with longstanding diabetes mellitus, patients requiring functional insulin therapy or whose blood sugar is not sufficiently controlled should be treated by an endocrinologist/diabetologist according to international guidelines [21].
For cases with an unsatisfactory effect of a PDE5 inhibitor, further local therapies do exist. Alprostadil can be applied in the urethra (MUSE), thus stimulating blood flow to the penis. Further, alprostadil can be administered as a direct intracavernosal injection, this being successful in about 85% of men who do not respond to PDE5 inhibitors. In the contrast to PDE5 inhibition, alprostadil induces an erection regardless of sexual stimulation.
Surgical intervention is usually only recommended if all other treatment methods have failed. It can also be used in the context of trauma or in cases of anatomical problems. Surgery most often includes penile implants. These are currently not reimbursed by healthcare insurance in Switzerland.
| Table 2: Exercise ability and sexual activity risk stratification for patients with erectile dysfunction. | ||
| Low risk | Intermediate risk | High risk |
| Moderate exercise without symptoms possible | Mild to moderate stable angina pectoris | Unstable/refractory angina pectoris |
| Coronary artery disease with successful revascularisation | Past myocardial infarction (2–8 weeks) without intervention | |
| Hypertension asymptomatic and controlled | Uncontrolled hypertension | |
| Mild valvular disease | Moderate to severe valvular disease (aortic stenosis), obstructive hypertrophic cardiomyopathies | |
| Left ventricular dysfunction with stress test passed | Congestive heart failure (NYHA grade III) | Congestive heart failure (NYHA grade IV) |
| Noncardiac sequelae of arteriosclerotic disease (peripheral arterial disease, stroke, transient ischaemic attack) | High-risk arrhythmias | |
| NYHA = New York Heart Association Adapted from Nehra et al. [10]. | ||
Endovascular revascularisation of small-calibre erection-related arteries has become technically feasible [14, 22, 23]. Restoration of arterial inflow in ED patients with atherosclerotic obstructions of erection-related arteries can result in improvement of erectile function [22].

Figure 3
Sub-total occlusion of both hypogastric arteries (*) in a patient with cardiovascular risk factors and erectile dysfunction.
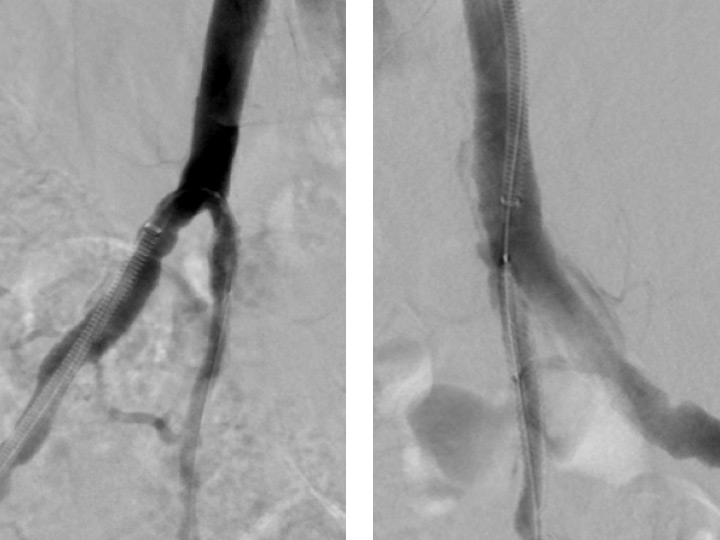
Figure 4
Angiographic result after bilateral placement of drug eluting stents.
The impact of impaired arterial inflow into the pelvic arteries on erectile function was observed almost a century ago by the French surgeon René Leriche [24]. He observed that aortoiliac occlusion may cause erectile impotence due to failure of perfusion of the corporal bodies, as well as buttock claudication and gluteal muscle atrophy. Subsequently, revascularisation of arterial obstructions for ED has traditionally been performed surgically in younger men without cardiovascular risk factors and with blunt perineal trauma or pelvic fracture.
Endovascular therapy for obstructions of the common iliac and hypogastric arteries has traditionally been performed for many years. Figures 3 and 4 show angiograms of the pelvic arteries of a 62-year-old architect with erectile dysfunction. He had undergone aorto-coronary bypass grafting 3 years previously and, based on duplex ultrasound, an arterial inflow obstruction had been diagnosed. On intra-arterial angiography, a high-grade obstruction of both hypogastric arteries was diagnosed (fig. 3), both of which have been stented using drug-eluting stents (fig. 4). Erectile dysfunction in this patient was significantly improved during follow-up.
During recent years, downsizing of catheter material has facilitated endovascular revascularisation of small-calibre erection-related arteries [14, 22, 23]. In the ZEN study, Rogers and colleagues analysed outcomes of 30 patients undergoing drug-eluting stent placement in the internal pudendal artery [14]. Procedural success was 100% with no major adverse events during follow-up. About 60% of patients undergoing stent placement showed functional improvement subsequent to endovascular revascularisation. However, the restenosis rate was reported to be as high as 34% in these small-calibre arteries after 6 months of follow-up.
Wang and colleagues demonstrated in a recently published single-centre experience in 20 patients that angioplasty down to the level of the penile arteries is technically feasible, clinically safe and may be associated with clinical improvement in 60% of patients [23].
Erectile dysfunction (ED) is a common problem. Men visiting the general practitioner should be asked whether they suffer from ED, as patients often feel embarrassed to discuss this problem.
ED is recognised as an early marker of cardiovascular disease, atherosclerosis and diabetes mellitus. The risk factors associated with ED are very similar to those for cardiovascular disease.
First-line therapy for men with ED is a phosphodiesterase-5 (PDE5) inhibitor. Patients with cardiovascular risk factors or not responding to PDE5 inhibition can profit from vascular workup and potentially from interventional treatment, thus increasing erectile function by treating the underlying cause.
1.Wie würden Sie ihre Zuversicht einschätzen, eine Erektion zu bekommen und zu behalten?
‒ fast nicht vorhanden (1 Punkt)
‒ niedrig (2 Punkte)
‒ mittelmässig (3 Punkte)
‒ gross (4 Punkte)
‒ sehr gross (5 Punkte)
2.Wenn Sie bei sexueller Stimulation eine Erektion hatten, wie oft war sie hart genug für eine Penetration?
‒ fast nie (1 Punkt)
‒ selten (2 Punkte)
‒ ungefähr 50 % (3 Punkte)
‒ meistens (4 Punkte)
‒ fast immer (5 Punkte)
3.Wie oft waren Sie bei dem Geschlechtsverkehr in der Lage, nach der Penetration die Erektion aufrecht zu erhalten?
‒ fast nie (1 Punkt)
‒ selten (2 Punkte)
‒ ungefähr 50 % (3 Punkte)
‒ meistens (4 Punkte)
‒ fast immer (5 Punkte)
4.Wie oft waren Sie bei dem Geschlechtsverkehr in der Lage, die Erektion bis zum Ende aufrecht zu erhalten?
‒ fast nie (1 Punkt)
‒ selten (2 Punkte)
‒ ungefähr 50 % (3 Punkte)
‒ meistens (4 Punkte)
‒ fast immer (5 Punkte)
5.Wenn Sie versuchten, Geschlechtsverkehr zu haben, wie oft war er befriedigend für Sie?
‒ fast nie (1 Punkt)
‒ selten (2 Punkte)
‒ ungefähr 50% (3 Punkte)
‒ meistens (4 Punkte)
‒ fast immer (5 Punkte)
Ergebnis:
22–25 Punkte: Keine erektile Dysfunktion
17–21 Punkte: Milde erektile Dysfunktion
12–16 Punkte: Milde bis moderate erektile Dysfunktion
8–11 Punkte: Moderate erektile Dysfunktion
Unter 8 Punkte: schwere erektile Dysfunktion
http://www.smw.ch/fileadmin/smw/pdf/smw-14268-Appendix.pdf
1 Aytac IA, Araujo AB, Johannes CB, Kleinman KP, McKinlay JB. Socioeconomic factors and incidence of erectile dysfunction: findings of the longitudinal Massachussetts Male Aging Study. Soc Sci Med. 2000;51(5):771–8.
2 Goldstein I. Male sexual circuitry. Working Group for the Study of Central Mechanisms in Erectile Dysfunction. Sci Am. 2000;283(2):70–5.
3 Dong JY, Zhang YH, Qin LQ. Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J Am Coll Cardiol. 2011;58(13):1378–85.
4 Jackson G. Prevention of cardiovascular disease by the early identification of erectile dysfunction. Int J Impot Res. 2008;20(Suppl 2):S9–14.
5 Ghanem H, Shamloul R. An evidence-based perspective to commonly performed erectile dysfunction investigations. J Sex Med. 2008;5(7):1582–9.
6 Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49(6):822–30.
7 Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, et al. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56(25):e50–103.
8 Christ-Crain M, Meier C, Huber P, Zimmerli L, Trummler M, Muller B. Comparison of different methods for the measurement of serum testosterone in the aging male. Swiss Med Wkly. 2004;134(13-14):193–7.
9 Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR, Baltimore Longitudinal Study of A. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore Longitudinal Study of Aging. J Clin Endocrinol Metab. 2001;86(2):724–31.
10 Nehra A, Jackson G, Miner M, Billups KL, Burnett AL, Buvat J, et al. The Princeton III Consensus recommendations for the management of erectile dysfunction and cardiovascular disease. Mayo Clin Proc. 2012;87(8):766–78.
11 Hodges LD, Kirby M, Solanki J, O'Donnell J, Brodie DA. The temporal relationship between erectile dysfunction and cardiovascular disease. Int J Clin Pract. 2007;61(12):2019–25.
12 Available from: Pocket Guide EndoDiabNet (Aarau – Basel – Lucerne): http://www.ksa.ch/public/pocketguide/pocket-guide.pdf.
13 Jackson G. Problem solved: erectile dysfunction (ED) = early death (ED). Int J Clin Pract. 2010;64(7):831–2.
14 Rogers JH, Goldstein I, Kandzari DE, Kohler TS, Stinis CT, Wagner PJ, et al. Zotarolimus-eluting peripheral stents for the treatment of erectile dysfunction in subjects with suboptimal response to phosphodiesterase-5 inhibitors. J Am Coll Cardiol. 2012;60(25):2618–27.
15 Evans MF. Lose weight to lose erectile dysfunction. Can Fam Physician. 2005;51:47–9.
16 Borm A, Luescher S, Mueller B. Erste Behandlungsschritte bei neuentdecktem Diabetes mellitus. Swiss Med Forum. 2012;12:929–35.
17 Wu FC, Tajar A, Beynon JM, Pye SR, Silman AJ, Finn JD, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363(2):123–35.
18 Isidori AM, Giannetta E, Greco EA, Gianfrilli D, Bonifacio V, Isidori A, et al. Effects of testosterone on body composition, bone metabolism and serum lipid profile in middle-aged men: a meta-analysis. Clin Endocrinol (Oxf). 2005;63(3):280–93.
19 Bolona ER, Uraga MV, Haddad RM, Tracz MJ, Sideras K, Kennedy CC, et al. Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc. 2007;82(1):20–8.
20 Nigro N, Christ-Crain M. Testosterone treatment in the aging male: myth or reality? Swiss Med Wkly. 2012;142:w13539.
21 Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, et al. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2012;55(6):1577–96.
22 Rogers JH, Rocha-Singh KJ. Endovascular therapy for vasculogenic erectile dysfunction. Curr Treat Options Cardiovasc Med. 2012;14(2):193–202.
23 Wang TD, Lee WJ, Yang SC, Lin PC, Tai HC, Hsieh JT, et al. Safety and six-month durability of angioplasty for isolated penile artery stenoses in patients with erectile dysfunction: a first-in-man study. EuroIntervention. 2014;10(1):147–56.
24 Leriche R. Des obliterations arterielle hautes (obliteration de la termination de l’aorte) comme cause de insufficances circulatoire des membres inferieurs. Bull Mem Soc Chir. 1923;49:1404.
Disclosure statement: No financial support and no other potential conflict of interest relevant to this article was reported.