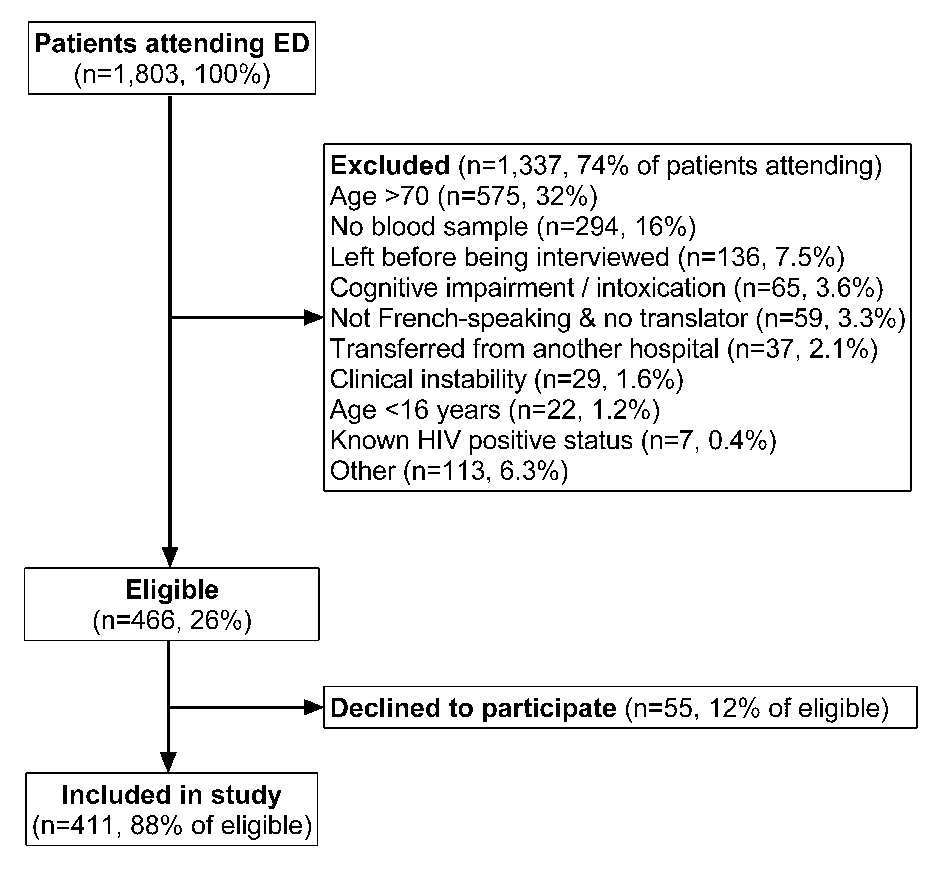
Figure 1
Flowchart of patients included in the study out of those attending the emergency department (ED) during 56 shifts of recruitment.
DOI: https://doi.org/10.4414/smw.2015.14206
The term “blood test” is used ubiquitously by healthcare professionals and patients and is usually understood to mean a screening or diagnostic procedure. In the case of screening, the aim is to detect early disease in individuals who are asymptomatic; diagnostic testing is performed to establish the presence (or absence) of disease in patients with symptoms or a positive screening test. For some screening tests, specific communication is required between clinician and patient. Formal screening for diabetes mellitus and high cholesterol, for example, requires fasting blood so the patient must be suitably prepared; screening for human immunodeficiency virus (HIV) in a patient with decision-making capacity requires that patient’s informed consent [1, 2]. When screening tests do not require specific patient preparation, the clinician might omit the details of tests being performed to limit consultation time and avoid unnecessary patient anxiety. If clinician-patient communication is insufficient, however, there is potential for patient misunderstanding as to what specifically has been screened for [3].
In the field of HIV, screening has been characterised as (1) non-targetedscreening, where a patient is tested regardless of the probability of HIV infection, (2) targetedscreening, where a patient has risk factors for HIV infection and (3) diagnostictesting, where a patient exhibits features of HIV infection and where testing will make the diagnosis, [4]. In all cases, the patient must be informed if an HIV test is to take place. Whilst these screening approaches may be described in the medical press, it is likely that they are not part of general patient knowledge [5]. At our centre, Albrecht et al. (2012) described patient misunderstanding of blood tests among individuals undergoing elective orthopaedic surgery. Of 991 patients, 38% believed erroneously they had been tested for HIV preoperatively and, of patients with this belief, 96% interpreted the lack of result communication as indicating a negative test result [6]. Similar misunderstanding has been described among emergency department (ED) patients in the US, where 5.8% of 276 patients questioned reported erroneously that they had been tested for HIV [7].
In Switzerland, the ED has an exceptional position in healthcare provision: many patients use this service as a source of primary care rather than visit a general practitioner [8]; for otherwise fit individuals, those presenting with trauma-related injuries, for example, the ED may be the only point of contact with a doctor in many years [6]. Whether it is the role of the ED to participate in screening programmes in addition to delivering life-saving care is a cause of debate [9]. However, what patients believe they have been screened for during an ED visit is relatively underexplored.
The Swiss Federal Office of Public Health (FOPH) HIV testing recommendations propose ‘Physician-Initiated Counselling and Testing’ (PICT), in which HIV screening is targeted and patients must be informed that they are being tested before a test can take place [2]. To date, we have reported HIV testing rates of ≤1% in EDs in French-speaking Switzerland [10, 11]. To examine patient attitudes to “routine” (non-targeted) HIV screening in the ED, we studied the proportion of patients who believed they had been screened for HIV infection during their ED visit and the proportion who agreed in principle with routine HIV screening. To put HIV results in perspective, we asked the same questions regarding screening for diabetes and high cholesterol.
This study was approved by the ethics committee on human scientific research of the canton of Vaud, Switzerland. Written informed consent was obtained from all participants (see below). In accordance with Public Health Legislation of the Canton of Vaud, no ethical approval was required for the step of cross-referencing the patient database with other hospital databases as the latter were retrospective and anonymised [12, 13].
The study was conducted in the ED at Lausanne University Hospital (LUH) between 1st October 2012 and 28th February 2013. LUH is a 1 200-bed teaching hospital which functions as a primary-level community hospital for the 300 000 inhabitants of the Lausanne area, and as a secondary- and tertiary-level referral hospital for Western Switzerland (approximate population 1 to 1.5 million) [14]. HIV seroprevalence in the local population is 0.4% [15].
Patients aged 16 to 70 years old presenting acutely to LUH ED and undergoing blood testing were eligible. Exclusion criteria were clinical instability, leaving the ED before being seen or admitted for >12 hours, transfer from another hospital or from prison, suffering from cognitive difficulties, dementia, psychosis, intoxication or other factors precluding informed consent, and known positive HIV status. Inability to speak French was not an exclusion criterion if it was possible to conduct the questionnaire in another language or via an interpreter. None of the patients enrolled had been formally tested for the conditions in the questionnaire (diabetes, high cholesterol and HIV) and so we did not document which patients had received the results of their blood tests prior to interview, nor how results had been delivered (for example, “everything is fine” or with specific details of each test performed).
The study was cross-sectional with a convenience sample and consisted of questionnaire-based face-to-face interviews. To limit interviewer bias, the number of interviewers was restricted to two medical students in their final year of training (TFB and DB). The interviews took place after blood sampling and before discharge from the ED. As the questionnaire involved the offer of an HIV test, and as this could not be performed out of hours in our hospital at the time of this study, all interviews were conducted between 07:00 and 22:00. However, patients being interviewed at 07:00 could have presented to the ED up to 11 hours previously (see exclusion criteria, above). The interviews were performed throughout a total of 56 shifts, organised around the students’ medical studies. To determine how representative the patients included in the study were compared to the total patient population attending the ED, we examined the time of presentation, and age and sex of all patients presenting to the ED during the study period by extracting anonymised data from the central ED database.
The interviews followed a questionnaire previously validated in another department at our centre [6]. Patient date of birth, nationality and sex were recorded on the front page and the questionnaire was then divided into three sections. In section 1, patients were asked if they thought they had been screened for diabetes, high cholesterol and HIV as part of their routine ED work up (response options: “yes” and “no”, or “I don’t know” if the patient did not know or was unfamiliar with the medical condition). We chose diabetes and high cholesterol as these are well-known cardiovascular risk factors for which screening has been recommended over many years in national campaigns [16, 17].
On completion of section 1, the patients were informed that none of the three conditions were formally screened for routinely in the ED. In section 2, patients were asked if they would agree in principle to being screened for the three conditions as part of the routine ED work-up. Response options were “yes”, “no” or “I don’t know”.
In section 3, patients were asked if they would agree to being tested for HIV during the current ED visit (response options: “yes” and “no”). As rapid point-of-care testing is not available in our ED, and as ethical approval was not obtained to allow the medical students to perform HIV testing as part of this study, patient requests and oral consent to be HIV tested were transmitted to the clinician in charge. Patients not subsequently admitted for hospitalisation were provided with information detailing where HIV testing could be sought as an outpatient, namely, the hospital anonymous testing service or the patient’s primary care physician.
Demographic data and questionnaire responses were entered at interview into a separate database by each of the two medical students. A single final dataset was created after data comparison and resolution of discrepancies [18]. The database was then cross-referenced against the database of the service of immunology and allergy, where all HIV tests performed at our hospital non anonymously are documented. Of note, rapid testing is not performed in our ED. To identify testing performed at or related to the index ED visit, we examined records by hospital episode number and by date. Random measurements of glucose or cholesterol relating to the ED visit, as opposed to formal (fasting-state) screening samples for diabetes and high cholesterol, were not quantified.
The final study database was anonymised prior to analysis. Data were expressed as means ± standard deviation (SD) or as percentages. We used the chi-squared test or Fisher’s exact test to compare categorical variables and Student’s t-test to analyse continuous data. To examine the effect of patient demographics on questionnaire responses, patient age was divided into six categories and patient nationality was grouped as being from Switzerland, Europe, Africa, South America, North America or Asia. Patients of nationality other than Swiss or European were grouped by continent as numbers were small. Missing data was not imputed. All statistical analyses were performed using Stata software, version 12.1 (Stata Corporation, College Station, TX, USA). A bilateral p-value <0.05 was considered statistically significant.
| Table 1: Demographic parameters of the 411 participating patients, those believing they had been screened for HIV as part of their emergency department work-up, those not believing they had been screened for HIV and those unsure. | |||||
| Participating patients (n = 411) | Believing HIV screening had taken place (n = 113) | Not believing HIV screening had taken place (n = 288) | Unsure (n = 10) | p-value ¶ | |
| Gender, n (%) | |||||
| Male | 219 (53) | 61 (54) | 150 (52) | 8 (80) | 0.2 |
| Female | 192 (47) | 52 (46) | 138 (48) | 2 (20) | |
| Age categories (years) | |||||
| 16–25 | 63 (15) | 11 (9.7) | 52 (18) | 0 (0) | 0.01 |
| 26–35 | 67 (16) | 16 (14) | 50 (17) | 1 (10) | |
| 36–45 | 55 (13) | 8 (7.1) | 45 (16) | 2 (20) | |
| 46–55 | 85 (21) | 23 (20) | 58 (20) | 4 (40) | |
| 56–65 | 82 (20) | 31 (27) | 49 (17) | 2 (20) | |
| 66–70 | 59 (14) | 24 (21) | 34 (12) | 1 (10) | |
| Nationality | |||||
| Switzerland | 262 (64) | 73 (65) | 185 (64) | 4 (40) | 0.16 |
| Europe | 104 (25) | 27 (24) | 71 (25) | 6 (60) | |
| Africa | 17 (4.1) | 8 (7.1) | 9 (3.1) | 0 (0) | |
| South America | 16 (3.9) | 3 (2.7) | 13 (4.5) | 0 (0) | |
| Other * | 9 (2.9) | 2 (1.8) | 10 (3.5) | 0 (0) | |
| Missing | 3 (0.7) | 1 (0.9) | 2 (0.7) | 0 (0.0) | |
| Destination | |||||
| Discharged | 208 (51) | 58 (51) | 144 (50) | 6 (60) | 0.6 |
| Admitted | 199 (48) | 53 (47) | 142 (49) | 4 (40) | |
| Transferred | 3 (0.7) | 2 (1.8) | 1 (0.4) | 0 (0) | |
| Missing | 1 (0.2) | 0 (0) | 1 (0.4) | 0 (0) | |
| HIV = human immunodeficiency virus; NA = not available * Patients from North America (6 patients), Asia (3 patients) and those of unknown origin (3 patients). ¶ p- values are derived from the chi squared test or Fisher’s exact test, as appropriate. | |||||
During the study period, 1st October 2012 to 28th February 2013, 1 803 patients were screened for study eligibility during their ED visit, of whom 1 337 (74%) were excluded, mostly because they were older than 70 years (32%) (fig. 1). Of the 466 eligible patients, 411 (88%) agreed to participate, of whom 192 (47%) were women. Mean age was 46 ± 16 years and most patients were Swiss (262/411, 64%) or of EU origin (104/411, 25%) (table 1). Against these figures, 21 922 patients attended the ED during the study period, of whom 17 304 (79%) presented between 07:00 and 22:00, when the questionnaire was performed. Of the total number, 15 052 patients (69%) were aged ≥16 years and ≤70 years, of whom 8 635 (57%) were male and 6 417 (43%) were female. The breakdown of these 15 052 patients and the study patients by age category is shown in table 2.
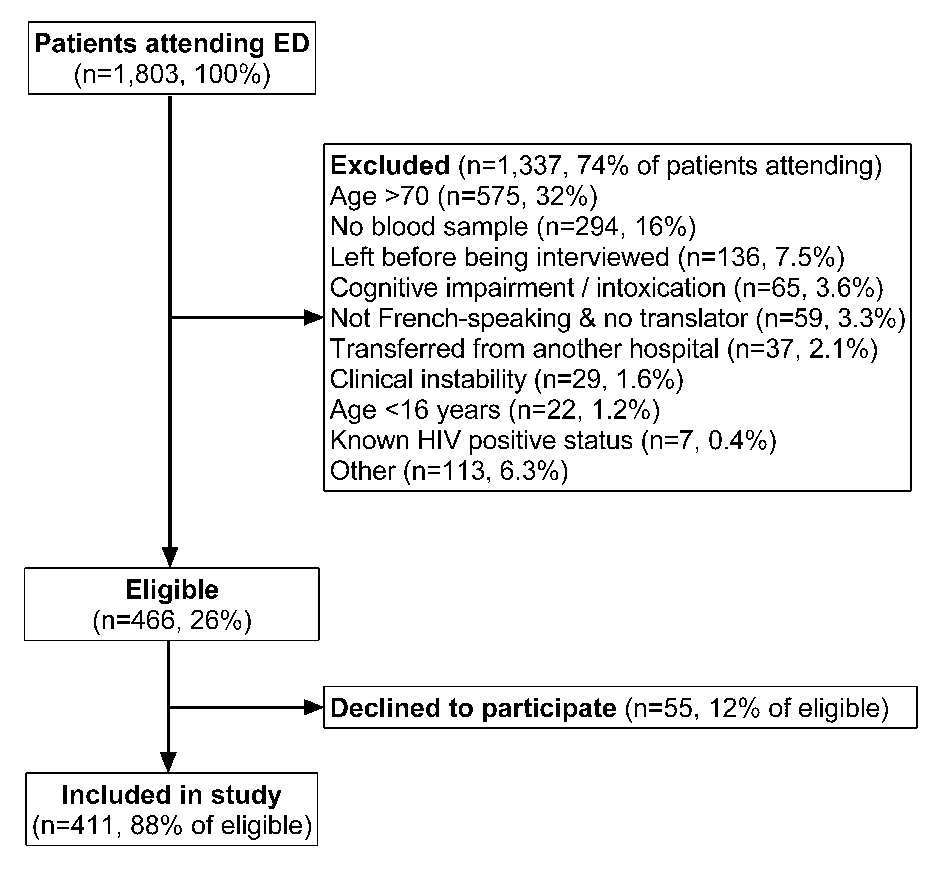
Figure 1
Flowchart of patients included in the study out of those attending the emergency department (ED) during 56 shifts of recruitment.
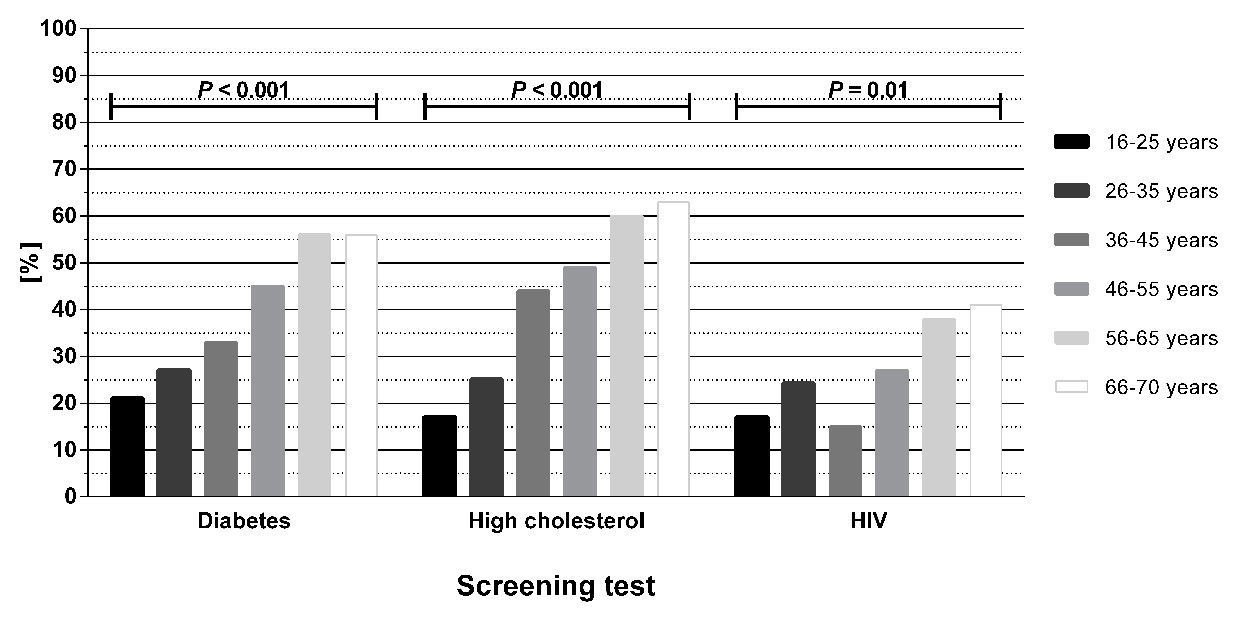
Figure 2
Profile of participating patients, by age, who believed they had been screened for diabetes, high cholesterol and human immunodeficiency virus (HIV) as part of their ED work-up. The p-values are derived from the chi squared test.
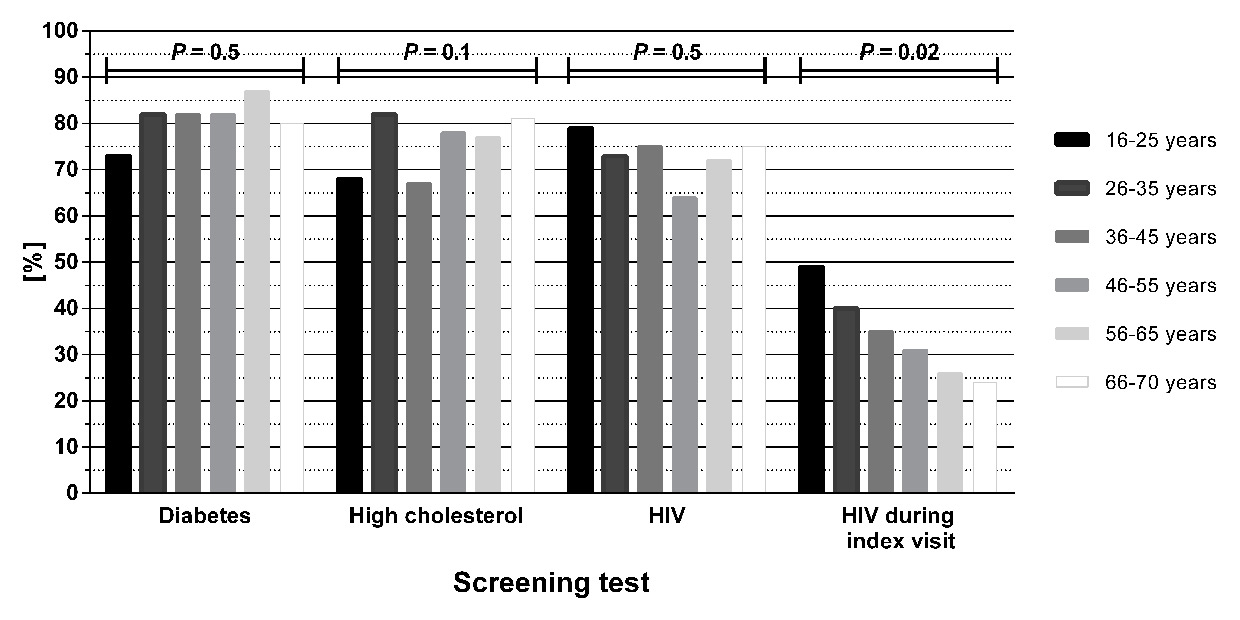
Figure 3
Profile of participating patients, by age, who agreed in principle to non-targeted screening in the emergency department (ED) for diabetes, high cholesterol and human immunodeficiency virus (HIV) and who agreed to be HIV tested during their current ED visit. The p-values are derived from the chi squared test.
In section 1 of the questionnaire, 113 patients (of 411, 27%) believed incorrectly that they had been tested for HIV. Older patients were more likely to hold this belief (p = 0.01, fig. 2). Mean age was 51 ± 16 years for those who believed an HIV test had been performed, and 43 ± 16 years for those without this belief (p <0.001). There was no association between believing a test had been performed and gender or nationality. Regarding non-HIV blood tests, 40% and 44% believed they had been tested for diabetes and high cholesterol, respectively (table 3). Again, percentage of belief increased with age (p < 0.001, fig. 2).
In section 2, the majority of patients agreed in principle with routine screening in the ED for the conditions listed in the questionnaire, with 72% agreeing with screening for HIV and 76–81% agreeing with screening for the non-HIV conditions (table 3). There was no significant difference in patient age (fig. 3), gender or nationality between those who agreed with HIV screening and those who did not.
In section 3, 138 patients (34%) agreed to be HIV tested immediately (that is, during their current ED visit). These patients comprised 129 of the 297 patients (43%) who agreed with routine HIV screening in questionnaire section 2, plus 9 patients who stated they did not agree with routine screening. Older patients were less accepting of immediate testing than younger patients (p= 0.02, fig. 3). Mean age was 42 ± 17 years for patients accepting immediate testing and 48 ± 16 years for those declining (p<0.001). Again, there was no association with gender or nationality. Twenty-two patients agreed to the request for HIV testing being transmitted to the ED clinician. Cross-referencing the study database against the database of the service of immunology and allergy demonstrated that ten of these 22 patients were tested during their ED visit or subsequent hospital admission and that fourteen patients who had initially declined HIV testing were subsequently tested. Of 411 patients, therefore, a total of 24 (5.8%) underwent HIV testing, of whom one had a reactive test.
| Table 2:Breakdown by age category of all the patients aged 16 to 70 years old who attended the ED during the study period and those who were included in the study. | ||||
| Age category (years) | All patients presenting to ED (n = 15 052) | Percentage of all patients by age category * | Study patients (n = 411) | Percentage of study patients by age category * |
| 16–25 | 2622 | 17% | 73 | 18% |
| 26–35 | 2692 | 18% | 59 | 14% |
| 36–45 | 2629 | 18% | 59 | 14% |
| 46–55 | 2838 | 19% | 83 | 20% |
| 56–65 | 2759 | 18% | 87 | 21% |
| 66–70 | 1512 | 10% | 50 | 12% |
| ED = emergency department * As a result of rounding, the sum of the percentages in each column might not equal 100% in all cases. | ||||
| Table 3:Questionnaire responses among the 411 participating patients. | |||
| Questionnaire response, n (%) * | |||
| Yes | No | Don't know | |
| Conditions believed to have been screened for: | |||
| Diabetes | 166 (40%) | 214 (52%) | 31 (7.6%) |
| High cholesterol | 180 (44%) | 201 (49%) | 30 (7.3%) |
| HIV | 113 (27%) | 288 (70%) | 10 (2.4%) |
| Agree in principle to non-targeted screening: | |||
| Diabetes | 334 (81%) | 77 (19%) | 0 (0.0%) |
| High cholesterol | 312 (76%) | 97 (24%) | 2 (0.5%) |
| HIV | 297 (72%) | 113 (27%) | 1 (0.2%) |
| Agree to HIV testing during current ED visit | 138 (34%) | 273 (66%) | 0 (0.0%) |
| ED = emergency department; HIV = human immunodeficiency virus * As a result of rounding, the sum of the percentages in each column might not equal 100% in all cases. | |||
In this study of patients’ understanding of blood tests in the ED, we observed that 27% of patients questioned believed incorrectly they had been tested for HIV as part of their routine work-up, despite the fact that, in Switzerland, individuals must be informed that an HIV test is indicated before it is performed. The figure of 27% is slightly lower than that reported by Albrecht et al, (2012) among patients undergoing orthopaedic surgery (38%) [6]. Although neither group of patients was asked to give reasons for believing they had been HIV tested, it is possible that a higher proportion of surgical patients believed they had been HIV tested as a measure to protect the operating staff [6, 19]. Unlike Albrecht et al., we did not ask patients about their interpretation of having no test result communicated as, in the setting of our study, some patients would not yet have received their blood results. However, if the ED patients who believed they had been HIV tested did assume that no result provision indicated a negative test, as observed among surgical patients [6], they might be falsely reassured about their HIV status and unintentionally misinform healthcare providers about previous HIV tests. For undiagnosed HIV positive patients, this could contribute to delaying the HIV diagnosis, continued risky behaviour and onward transmission of infection [20], especially during acute infection [21].
Our 27% figure is higher than that of Khakoo et al, (2014), who reported that 5.8% of patients erroneously believed they had been HIV tested during their ED visit [7]. This difference might be explained by the fact that in our questionnaire, we grouped HIV testing with other tests (diabetes and high cholesterol), potentially destigmatising HIV testing and providing an anchoring bias. If this effect was real, it is possible that offering HIV testing together with that for other chronic diseases would have several implications: the HIV test would be destigmatised and dedramatised for both ED medical staff and patients; the patient would be informed that HIV is now a chronic disease; and the HIV testing rate in the ED could increase.
We observed that 72% of patients agreed in principle with routine HIV testing in the ED, a figure similar to that reported elsewhere [6, 22–24]. Reasons given by patients for not agreeing with routine screening related to population civil rights and perceived excessive healthcare costs (TFB, DB, personal observations). The proportion of patients agreeing with routine HIV screening was not significantly different to that for the non-HIV conditions (76–81%), suggesting that patient attitudes might be less of a barrier to HIV testing in the Swiss ED setting than reticence among ED clinicians [11].
Against the 72% of patients agreeing with HIV testing in principle, 34% agreed to be tested during the current ED visit. We did not ask patients for reasons behind their answers to questionnaire sections 2 and 3, and so we can only speculate as to why patients agreeing with routine testing in principle did not accept testing straight away and vice versa. Many patients declining immediate testing stated they had been tested recently, or that they did not consider themselves at risk (TFB, DB, personal observations). These reasons for test refusal have been observed elsewhere [24–26]. The discrepancy between the number of patients agreeing to be tested and the number of tests subsequently performed was observed by cross-referencing two databases and we have no means of determining what factors were responsible. Such discrepancies have been described in the ED setting [27, 28] and a study is currently underway to examine the barriers to testing specific to the LUH ED.
Older individuals in this study were more likely to believe they had been HIV tested but less likely to agree with routine testing in principle and to testing during the current ED visit. Freeman et al. (2009) reported similar observations on the influence of age on HIV testing [29]. Although some patients volunteered that they did not consider themselves likely to be positive (TFB, DB, personal observations), we did not formally explore patient attitudes to HIV risk. That older patients were less likely to agree with routine HIV screening is noteworthy in the light of observed changes in HIV epidemiology, in which a 3.5-fold increase in the number of adults aged over 50 accessing HIV care has been described in some countries [30].
There are many arguments for proposing the ED as an appropriate setting for routine HIV screening in Switzerland. A recently published national profile of emergency medicine reported that over 1.5 million people visited a hospital-based ED during 2006 [31], and this figure has been steadily increasing since then [32]. Our own centre sees over 50 000 patients per annum [11], a figure which is also increasing [10, 33]. Many of these patients use the ED as their primary care provider [8], and the ED may represent their only contact with medical professionals [8, 33]. However, most ED clinicians in French-speaking Switzerland are unaware of the FOPH testing recommendations and perform few HIV tests [11]. A non-targeted screening approach would bypass the need for clinicians to be aware of national HIV testing recommendations and indeed the majority of patients in our study agreed in principle with “routine” screening. It must be emphasised, however, that our questionnaire referred to “routine” screening in which the non-targeted approach was implied but not explicitly mentioned. Whilst our results shed light on patient attitudes to testing, they should not be interpreted as proof of superiority of non-targeted screening over targeted screening / diagnostic testing as currently recommended by the Swiss FOPH [2].
Relatively little has been published on patients’ understanding of “routine” (non-targeted) blood testing in the ED setting. To our knowledge, this is the first study examining patients’ understanding of HIV screening in the ED setting in Europe. In the US, Cowan et al. (2013) published a qualitative assessment of ED patients’ beliefs and acceptance related to HIV testing strategies through 34 individual interviews, reporting that many ED patients were unaware of HIV testing recommendations and the different screening approaches [5].
Our study has limitations. The fact that some patients might have received their blood test results prior to interview might have altered their responses to questionnaire section 1 and, therefore, the percentage of patients who believed they had been tested for each condition. As this was a face-to-face questionnaire, social desirability bias might have contributed to the discrepancy between the numbers of patients agreeable to testing in principle and those subsequently tested. Because the interviewers were not granted permission by our ethics committee to perform rapid HIV testing in the ED, we cannot explain why patients who agreed to be HIV tested were not ultimately tested, according to our laboratory database. It is possible that patients were tested anonymously following ED discharge, but we have no way of determining this. We did not examine patient socioeconomic factors like income, housing, medical status or education level and we could not verify whether patients were familiar with the conditions they were questioned about. However, 89% of patients were Swiss or from European countries of high literacy. Our study was conducted in a country which has universal health insurance and access to health care without gate-keeping. Our ED population may therefore differ from countries with different health care systems and where ED access is restricted. Finally, as noted above, the fact that HIV was grouped with diabetes and cholesterol may have influenced attitudes favourably towards HIV testing, potentially increasing the proportion of patients who believed they had been tested or agreeing to testing in principle.
In conclusion, 27–44% of patients studied would have left the ED assuming they had been tested for conditions they had not formally been tested for. In the ED setting, we observed that the majority of patients (72%), once informed that HIV screening is not performed routinely, would agree with routine screening as part of standard care. If ED patients agree with being HIV tested, and if indeed they currently incorrectly believe that they are being tested, the ED is exactly the setting where non-targeted testing should be introduced. Finally, we highlight an urgent need for better public education regarding national HIV screening policies, particularly among older individuals, and for improved doctor-patient communication as to what a “blood test” does and does not involve.
Acknowledgements: We thank Dr Lionel Trueb, ED physician at Lausanne University Hospital, for providing data from the central ED database concerning the patient population who attended the ED during the study period but who were not included in the study.
1 Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17; quiz CE1-4.
2 Office fédéral de la santé publique: Dépistage du VIH effectué sur l’initiative des médecins en présence de certaines pathologies (maladies évocatrices d’une infection à VIH). Bull OFSP. 2013;47/13:1–5 http://www.bag.admin.ch/hiv_aids/05464/12752/index.html?lang=fr. Bulletin de l’OFSP. 2013;47/13:1–5 .
3 Musso MW, Perret JN, Sanders T, Daray R, Anderson K, Lancaster M, et al. Patients’ comprehension of their emergency department encounter: a pilot study using physician observers. Ann Emerg Med. 2015;65:151–5 e4.
4 Lyons MS, Lindsell CJ, Haukoos JS, Almond G, Brown J, Calderon Y, et al. Nomenclature and definitions for emergency department human immunodeficiency virus (HIV) testing: report from the 2007 conference of the National Emergency Department HIV Testing Consortium. Acad Emerg Med. 2009;16:168–77.
5 Cowan E, Leider J, Velastegui L, Wexler J, Velloza J, Calderon Y. A qualitative assessment of emergency department patients’ knowledge, beliefs, attitudes, and acceptance toward revised HIV testing strategies. Acad Emerg Med. 2013;20:287–94.
6 Albrecht E, Frascarolo P, Meystre-Agustoni G, Farron A, Gilliard N, Darling K, et al. An analysis of patients’ understanding of “routine” preoperative blood tests and HIV screening. Is no news really good news? HIV Med. 2012;13:439–43.
7 Khakoo NM, Lindsell CJ, Hart KW, Ruffner AH, Wayne DB, Lyons MS. Patient Perception of Whether an HIV Test Was Provided during the Emergency Department Encounter. J Int Assoc Provid AIDS Care. 2014;13:506–10.
8 Darling KE, Gloor E, Ansermet-Pagot A, Vaucher P, Durieux-Paillard S, Bodenmann P, et al. Suboptimal access to primary healthcare among street-based sex workers in southwest Switzerland. Postgrad Med J. 2013;89:371–5.
9 Irvin CB, Flagel BT, Fox JM. The emergency department is not the ideal place for routine HIV testing. Ann Emerg Med. 2007;49:722.
10 Darling KE, Hugli O, Mamin R, Cellerai C, Martenet S, Berney A, et al. HIV testing practices by clinical service before and after revised testing guidelines in a Swiss university hospital. PLoS One. 2012;7:e39299.
11 Darling KE, de Allegri N, Fishman D, Kehtari R, Rutschmann OT, Cavassini M, et al. Awareness of HIV testing guidelines is low among Swiss emergency doctors: a survey of five teaching hospitals in French-speaking Switzerland. PLoS One. 2013;8:e72812.
12 Cantonal Act on Public Health, article 25ss (Public Health Law of the Canton of Vaud, RSV 800.01).
13 Cantonal Regulations of Biomedical Research, article 3 and 14 paragraph 2 (RRB, RSV 800.21.1).
14 Vilpert S, Ruedin HJ, Trueb L, Monod-Zorzi S, Yersin B, Bula C. Emergency department use by oldest-old patients from 2005 to 2010 in a Swiss university hospital. BMC Health Serv Res. 2013;13:344.
15 Joint United Nations Programme on HIV/AIDS. UNAIDS report on the global AIDS epidemic 2012. http://www.unaids.org/sites/default/files/media_asset/20121120_UNAIDS_Global_Report_2012_with_annexes_en_1.pdf [cited 2015 20 August].
16 Bogousslavsky J RW, Mattle H. Hirnschlag-Kampagne der Schweizerischen Herzstiftung (SHS) und Zerebrovaskularen Arbeitsgruppe der Schweiz (ZAS) (German). Schweiz Arzteztg. 2000;81:677–9.
17 Mancini M. Self Care Diabète: Campagne nationale de dépistage (French). Primary Care. 2002;2:205–9
18 Ohmann C, Kuchinke W, Canham S, Lauritsen J, Salas N, Schade-Brittinger C, et al. Standard requirements for GCP-compliant data management in multinational clinical trials. Trials. 2011;12:85.
19 LaPorte DM, Mont MA, Jones LC, Padden DA, Hungerford DS. Human immunodeficiency virus testing for elective orthopedic procedures: results in a community-based hospital. Orthopedics. 2001;24:52–5.
20 Marks G, Crepaz N, Janssen R. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–50.
21 Brenner BG, Roger M, Routy JP, Moisi D, Ntemgwa M, Matte C, et al. High rates of forward transmission events after acute/early HIV-1 infection. J Infect Dis. 2007;195:951–9.
22 Haukoos JS, Hopkins E, Byyny RL, Denver Emergency Department HIVTSG. Patient acceptance of rapid HIV testing practices in an urban emergency department: assessment of the 2006 CDC recommendations for HIV screening in health care settings. Ann Emerg Med. 2008;51:303–9, 9 e1.
23 White DA, Sadoun T, Tran T, Alter HJ. Increased acceptance rates of HIV screening using opt-out consent methods in an urban emergency department. J Acquir Immune Defic Syndr. 2011;58:277–82.
24 Brown J, Kuo I, Bellows J, Barry R, Bui P, Wohlgemuth J, et al. Patient perceptions and acceptance of routine emergency department HIV testing. Public Health Rep. 2008;123(Suppl 3):21–6.
25 Ubhayakar ND, Lindsell CJ, Raab DL, Ruffner AH, Trott AT, Fichtenbaum CJ, et al. Risk, reasons for refusal, and impact of counseling on consent among ED patients declining HIV screening. Am J Emerg Med. 2011;29:367–72.
26 Christopoulos KA, Weiser SD, Koester KA, Myers JJ, White DA, Kaplan B, et al. Understanding patient acceptance and refusal of HIV testing in the emergency department. BMC Public Health. 2012;12:3.
27 d’Almeida KW, Pateron D, Kierzek G, Renaud B, Semaille C, de Truchis P, et al. Understanding providers’ offering and patients’ acceptance of HIV screening in emergency departments: a multilevel analysis. ANRS 95008, Paris, France. PLoS One. 2013;8:e62686.
28 Rayment M, Rae C, Ghooloo F, Doku E, Hardie J, Finlay S, et al. Routine HIV testing in the emergency department: tough lessons in sustainability. HIV Med. 2013;14(Suppl 3):6–9.
29 Freeman AE, Sattin RW, Miller KM, Dias JK, Wilde JA. Acceptance of rapid HIV screening in a southeastern emergency department. Acad Emerg Med. 2009;16:1156–64.
30 Smith RD, Delpech VC, Brown AE, Rice BD. HIV transmission and high rates of late diagnoses among adults aged 50 years and over. AIDS. 2010;24:2109–15.
31 Sanchez B, Hirzel AH, Bingisser R, Ciurea A, Exadaktylos A, Lehmann B, et al. State of Emergency Medicine in Switzerland: a national profile of emergency departments in 2006. Int J Emerg Med. 2013;6:23.
32 Vilpert S. Consultations dans un service d’urgence en Suisse (French/German). Neuchâtel: Observatoire suisse de la santé, 2013 Report No. 3/2013.
33 Diserens L, Egli L, Fustinoni S, Santos-Eggimann B, Staeger P, Hugli O. Emergency department visits for non-life-threatening conditions: evolution over 13 years in a Swiss urban teaching hospital. Swiss Med Wkly. 2015;145:w14123.
Disclosure statement: No financial support and no other potential conflict of interest relevant to this article was reported.
Authors’ contributions: TFB and DB participated in the design of the study, carried out the questionnaire and data collection and helped to draft the manuscript. KD participated in data analysis and in the drafting of the manuscript. RM cross-referenced study patients with the immunology laboratory database and contributed to the drafting of the manuscript. SP participated in the drafting of the manuscript. OH participated in the design of the study, the drafting of the manuscript and performed the statistical analyses. MC conceived the study, participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.