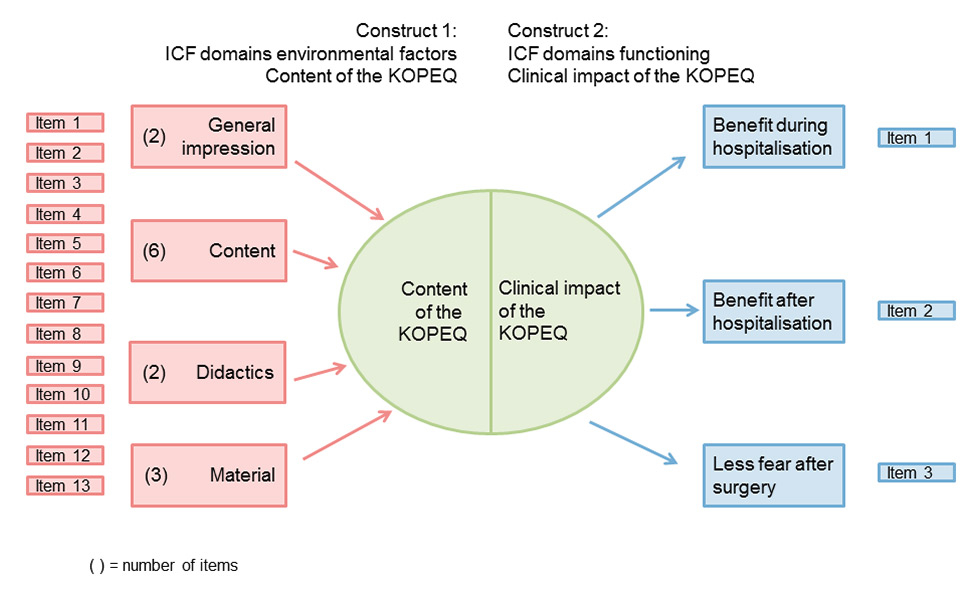
Figure 1
Conceptual framework of the Knee Osteoarthritis Patient Education Questionnaire (KOPEQ).
ICF = International Classification of Functioning, Disability and Health
DOI: https://doi.org/10.4414/smw.2015.14210
Patients scheduled for total knee replacement (TKR) have a long history of osteoarthritis which, over the years, has made them into experts on their own disease and its management. The impending TKR is a new event and it is important to understand patients’ perceptions and concerns. This knowledge will be of assistance in preoperative preparation, postsurgical recovery, rehabilitation and discharge planning [1]. Several studies have confirmed that patients have questions about immediate perioperative issues and the recuperation process [2–5]. For TKR, semistructured interviews of German patients found that they were mainly interested in information on the operation and recovery [6]. Trousdale et al. found that pain immediately after surgery, length of recovery, ability to walk, and ability to return to recreational activities were the four most important concerns of patients undergoing TKR [7]. Moran et al. demonstrated that cancellation of surgery, no decrease in pain, risk of losing the leg, risk of joint infection and risk of dying were the top five concerns [8].
The benefit of preoperative education on postoperative outcomes was recently evaluated in a review by the Cochrane collaboration [9]. Postoperative outcomes were anxiety, pain, function, health-related quality of life and side effects (such as infection or deep vein thrombosis). All types of surgical intervention and its postoperative rehabilitation delivered by a health professional within 6 weeks of surgery were accepted. The format of education ranged from one-to-one verbal communication, patient group sessions, to video or booklet with no verbal communication. The authors were uncertain as to whether it offers benefits over usual care in terms of reducing anxiety, or to surgical outcomes, such as pain, function and adverse events.
In all studies the content of the educational intervention itself was not evaluated and patients were not asked whether the content of the education programme actually suited their needs. It is necessary not only to evaluate the impact of the knee school on functioning domains, but also to evaluate the validity of the intervention itself [10]. Sjöling et al. pointed out in their study, that issues of validity were raised, because it seemed that some patients had problems in understanding and answering questions [11].
The aim of this study was to develop a generic instrument for the use of patients, named the Knee Osteoarthrtis Patient Education Questionnaire (KOPEQ), to assess the validity of a preoperative educational intervention and to make a preliminary test of its psychometric properties. An expert team developed a questionnaire (Knee Osteoarthritis Patient Education Intervention [KOPEI]), corresponding to the predefined conceptual framework. Furthermore we hypothesised that this questionnaire would be reliable and that an exploratory factor analysis would generate at maximum a four-factor model.
| Table 1:Conception of the Knee Osteoarthritis Patient Education Intervention (KOPEI). | |
| Overall aim | The overall aim of the KOPEI is to enable the individual patient to take control of this situation and to take a more active part in the postoperative recuperation process. |
| Underlying goal | The underlying goal is to impart practical knowledge, including information and illustrative material on the anatomy of the knee joint and adjacent functional structures, recommended activities with a prosthesis and postoperative pain management, as well as details on the postoperative rehabilitation phase. |
| Didactical elements and materials | Didactical elements and materials to be used include: models of the knee joint and the lower extremity, working sheets, photos and videos, activities pyramid, hand-outs, PowerPoint presentations, discussion and exchange of experience. |
| Organisation | The content is apportioned over three self-contained sessions with no hierarchy. |
| Content Session 1 | Functional anatomy: (a) What does the knee joint do?Anatomy: bones; muscles; other soft tissues Function: flexion extension; function of the patella (b) Vicious circlePain => Dysfunction => Protection => Pain ↑ (c) LegacyAfter a knee replacement the joint is “new“ while the muscles and other soft tissues remain “old”. (d) ConsequenceAs a result, training following a knee replacement is very important. |
| Content Session 2 | Recommended activities and postoperative pain reduction: (a) How does the musculature function?Function: isometric/concentrically/eccentrically what activities need how much mobility?Examples: sitting, standing-up, standing, walking, climbing steps, bicycle riding (b) Muscle effort and impact on the jointswith gravity / without gravity / against gravity soft surface / hard surface small range of motion / large range of motion, impacts/jumps (c) Postoperative pain reductionLeg elevation bandaging Quark compress / possibly ice (according to the clinic) Pain medication (prescribed by a doctor) |
| Content Session 3 | Postoperative rehabilitation (a) Time scheduleDiscussion of the treatment regimen in the respective clinic of the acute care hospital and the procedure after discharge from hospital. Focus will be laid on physiotherapeutic care and the active participation of the patient in relation to reaching the objectives. (b) Wound healingInflammation phase, proliferation phase, remodulation phase |
| ICF | In terms of the ICF the domain of contextual factors was addressed such as services, systems and policies (e5). In terms of the ICF the functioning domains addressed were: mental functions (b1), sensory functions and pain (b2), neuromusculoskeletal and movement-related functions (b7), mobility (d4), self-care (d5), domestic life (d6) and interpersonal interactions and relationships (d7). |
| ICF = International Classification of Functioning, Disability and Health | |
The development of the first version of the KOPEQ consisted of two phases, the development of the questionnaire itself, and the psychometric testing of internal consistency and factor analysis.
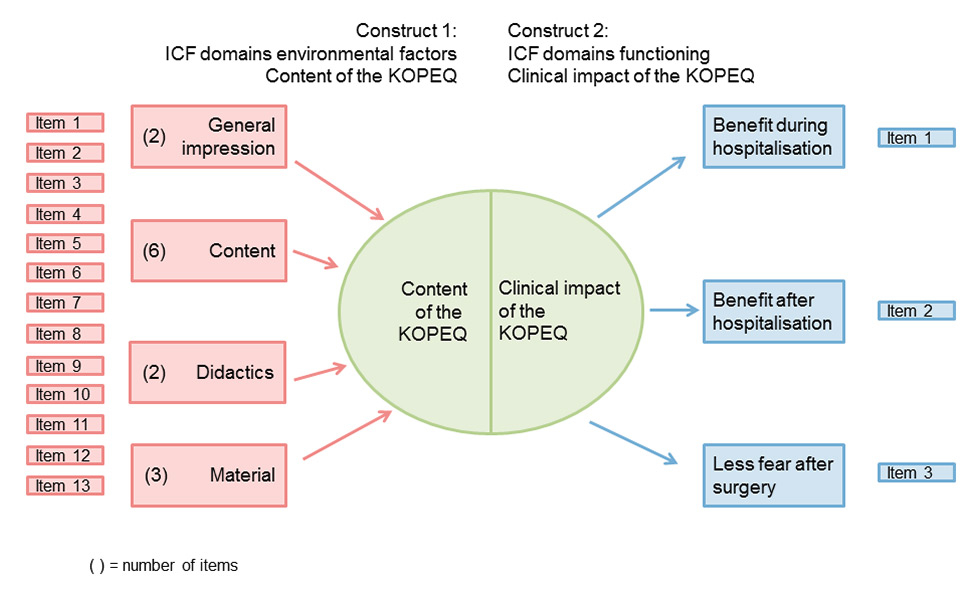
Figure 1
Conceptual framework of the Knee Osteoarthritis Patient Education Questionnaire (KOPEQ).
ICF = International Classification of Functioning, Disability and Health
A patient-reported outcome instrument to measure validity and outcome of the knee school intervention was designed. Items were developed by the same four persons (expert team) who had developed the content of the KOPEI. The concept of the KOPEI is shown in table 1.
During the development of the items, we used the conceptual framework of Wilson and Cleary as a methodological guide [12, 13]. It shows the relationship between construct and items and has implications for the scores and its examinations. In the reflective model the construct is reflected by the items, meaning that they will correlate with each other and also may replace each other. In the formative model, the items “cause” or “form” the construct, meaning that each item contributes to a part of the construct. In this case, Items do not necessarily correlate with each other and one item cannot be replaced by another. The conceptual framework of the first topic is a formative model and of the second topic a reflective model (fig. 1).
In a first step, an initial list of 25 questions was assembled and discussed via a brainstorming conference by the expert team. Based on the concept of the knee school, four dimensions were identified as being important for the formative model: general impression, content, didactics and material. Two to six items were developed for each dimension. Based on reported questions to patients who were undergoing lower extremity joint replacement [7, 14], three dimensions were identified as being important for the reflective model: less fear after surgery, benefit during and after hospitalisation until 6 weeks after surgery. The physical therapists decided to formulate only one item per dimension, in order to leave as much openness for patients to answer the questions.
The second step was to reduce items by looking at their similarity, so that the survey took no longer than 5 minutes to complete. The third step involved formulation of the items, taking care to use simple language, avoid words with multiple meanings, choose specific terms, ask only one question per item and avoid negative wordings.
A Likert five class scale with a range from one to five was chosen for the scoring. The KOPEQ has two subscales (content and clinical impact) and item scores within the subscales were just summed together.
Feasibility and interpretability of administering the KOPEQ was conducted. Targeted patients answered questions on the comprehensibility of questions, the response options and the length of the KOPEQ. Using a think-aloud methodology (cognitive interview) [15], patients were also asked to formulate in words which benefits they expected to receive from the KOPEI during and after hospitalisation.
For clinical practice or for research purposes, information on the specific content at item level is required [16]. The ICF provides an instrument to evaluate the content of a measure (item) in a systematic way [17]. Therefore, the items were linked to the ICF, respecting the patients’ words from the think-aloud methodology. The linking process was done by an experienced ICF-linking expert (F.ME) [18].
The study used a cross-sectional design, which was embedded within a randomised controlled trial [19]. Participants were patients with severe knee osteoarthritis on a waiting list for primary TKR. The intervention consisted of the KOPEI. Patients had to be proficient in German and have a Mini-Mental State Examination score of greater than 24/30 [20]. All of the participants gave their informed written consent. The study was approved as an amendment of the main study by the Ethics Committee of the Cantons Aargau and Solothurn, Switzerland, approval number 2009/12 and the trial is registered with ClinicalTrials.gov, identifier: NCT00913575.
Descriptive statistics were performed to describe the demographic variables of the target population.
The internal consistency was investigated, using Cronbach’s alpha [21]. A score above 0.70 was set as an indication of sufficient reliability [22].
An exploratory factor analysis of the 16 items of the KOPEQ was performed to model their underlying covariance structure. Exploratory factor analysis is usually applied in the development phase of an instrument. It is based on a formal model predicting observed variables from theoretical latent factors. Factor analysis identifies factors containing items that correlate highly with each other and explain as much as possible of the covariance with a minimal number of factors. A modern approach to estimate the parameters of the factor-analysis model is via maximum likelihood [23]. Therefore, we fitted the model by optimising the log likelihood assuming multivariate normality over the errors. Within the maximum likelihood approach, we could test whether k = 1, 2,... factors were sufficient by constructing a likelihood-ratio-test comparing the null hypothesis: “k factors are sufficient” versus the alternative: “k factors are not sufficient”. In addition, a parallel analysis was performed by extracting factors until the eigenvalues of the reduced correlation matrix were less than the corresponding eigenvalues of a random data set of the same size [24]. In the factor-analysis model, the factor loadings are identified only up to orthogonal rotations. The varimax rotation was applied to the extracted factors [25]. This solution maximises the sum of the variances of the squared loadings, leading to a rotation that aims to clarify the structure of the loadings matrix. The statistician was blinded to the meaning of the items.
All analyses were conducted with R version 2.14.1 software [26].
| Table 2:List of the items of the KOPEQ linked to the ICF. | ||
| Items | Concept | For analysis |
| Topic “education and training services” | ||
| 1. Overall impression of the knee school | Content: Health services, systems and policies, Education and training services | e580, e585 |
| 2. Division into three sessions | ||
| 3. Comprehensibility of the text in the handouts | ||
| 4. Completeness of the handouts | ||
| 5. Relation between theory and active participation | ||
| 6. Session “anatomy and function” | ||
| 7. Session “recommended activities” | ||
| 8. Session “rehabilitation phases after surgery” | ||
| 9. Answers to patients’ questions | ||
| 10. Comprehensibility of the imparted knowledge | ||
| 11. Arrangement of the handouts | ||
| 12. PowerPoint presentations | ||
| 13. Material to look at | ||
| Topic “functioning domains” | ||
| 14 Benefit during hospitalisation | Clinical impact: pain, walking, washing oneself, caring for body parts, toileting, dressing, formal relationships | b280, d450 d510, d520 d530 d540, d740 |
| 15 Benefit after hospitalisation | Clinical impact: pain, walking, washing oneself, caring for body parts, toileting, dressing, acquisition of goods and services, preparing meals, doing housework | b280, d450 d510, d520 d530 d540, d620, d630, d640 |
| 16 Fear of the time after surgery | Clinical impact: emotional functions | b152 |
| The linking of the items of the KOPEQ to the ICF was approved by Monika E. Finger on 24th July 2014. ICF = International Classification of Functioning, Disability and Health; KOPEI = Knee Osteoarthritis Patient Education Intervention | ||
Based on the conceptual framework, a total of 25 items were developed. After discussion within the group of experts, nine items were excluded, on the basis of similarity or relevance. Finally, the wording was carefully reconsidered and the list edited to a total of 16 items.
Targeted patients confirmed in interviews that all 16 questions were highly understandable and that the length of the questionnaire was feasible and acceptable. Patients were satisfied with the two different response options for the two subscales. Only one patient was rather expecting a four-point scale, without the option of a middle position answer. Overall, it seemed that the items of the KOPEQ covered most of the issues that were of importance to the patients.
Patients also formulated in words the benefits they expected from the KOPEI both during and after hospitalisation. During hospitalisation they generally expected less fear, empowerment to cope better with pain, and facilitated walking with canes and stair climbing. One patient pointed out that there is information overload on entrance day. Presurgery information is, therefore, very much appreciated and allows the focus in hospital to be on what is really important at that moment. Another patient was happy about being empowered to understand health professionals better. Another patient remarked that she was not a person who felt comfortable in group sessions.
After hospitalisation, they expected motivational support for exercising at home and empowerment to walk and undertake the activities of daily living in general. One patient pointed out how important it is to get advice on how far (in distance) to walk. Another patient underlined the importance of being patient, which is easier when knowing more about the healing and recovery process.
The list of items of the KOPEQ and their linking to the ICF is presented in table 2.
From May 2009 to June 2012 a total of 35 patients from a waiting list for TKR were recruited and assessed for this study. The mean age was 69.5 ± 7.9 years, Body Mass Index was 30.5 ± 5.5 and 18 of 35 patients were male. The characteristics of the 16 items of the KOPEQ are presented in table 3.
There was good internal consistency for the 16-item KOPEQ with a Cronbach’s alpha of 0.83 (95% confidence interval [CI] 0.71–0.94).
Parallel analysis suggested four factors. Equivalently, the likelihood-ratio-tests for the four-factor model suggested that four factors were sufficient. Sixty-one percent of the variance was explained by a four-factor model and the factors were named “didactics”, “addressability”, “empowerment” and “theory”. The loading of the separate items was between 0.469 and 0.958 (table 4).
| Table 3:Characteristics of the items of the KOPEQ. | ||||
| Items | Mean (SD) | Median | Minimum | Maximum |
| 1 | 4.5 (0.56) | 4.0 | 3 | 5 |
| 2 | 4.3 (0.47) | 4.0 | 4 | 5 |
| 3 | 4.5 (0.51) | 5.0 | 4 | 5 |
| 4 | 4.4 (0.56) | 4.0 | 3 | 5 |
| 5 | 4.4 (0.60) | 4.0 | 3 | 5 |
| 6 | 4.6 (0.50) | 5.0 | 4 | 5 |
| 7 | 4.6 (0.55) | 5.0 | 3 | 5 |
| 8 | 4.4 (0.74) | 5.0 | 2 | 5 |
| 9 | 4.7 (0.44) | 5.0 | 4 | 5 |
| 10 | 4.7 (0.52) | 5.0 | 3 | 5 |
| 11 | 4.4 (0.55) | 4.0 | 3 | 5 |
| 12 | 4.5 (0.61) | 5.0 | 3 | 5 |
| 13 | 4.5 (0.70) | 5.0 | 2 | 5 |
| 14 | 4.4. (0.70) | 4.0 | 2 | 5 |
| 15 | 4.3 (0.85) | 4.5 | 1 | 5 |
| 16 | 4.2 (1.26) | 5.0 | 1 | 5 |
| KOPEQ = Knee Osteoarthritis Patient Education Intervention; SD = standard deviation | ||||
| Table 4:Factor analysis with loadings of the 16 items of the KOPEQ on the 4 extracted factors*. | |||||
| Items | Description | Factor 1 Didactics | Factor 2 Addressability | Factor 3 Empowerment | Factor 4 Theory |
| Item 14 | Benefit of the imparted knowledge during hospitalisation | 0.800 | |||
| Item 10 | How comprehensible was the imparted knowledge? | 0.702 | |||
| Item 12 | How were the PowerPoint presentations? | 0.625 | |||
| Item 11 | How was the arrangement of the handouts? | 0.625 | |||
| Item 13 | How was the material to look at? | 0.616 | |||
| Item 9 | How were my questions answered? | 0.601 | |||
| Item 15 | Benefit of the imparted knowledge after hospitalisation | 0.569 | |||
| Item 2 | Division into three sessions | 0.840 | |||
| Item 1 | Overall impression of the knee school | 0.752 | |||
| Item 3 | How was the comprehensibility of the text in the handouts? | 0.658 | |||
| Item 4 | How was the completeness of the handouts? | 0.546 | |||
| Item 8 | How was the session “Rehabilitation phases after surgery”? | 0.930 | |||
| Item 7 | How was the session “recommended activities” | 0.632 | |||
| Item 16 | Less fear of the time after surgery by the imparted knowledge | 0.469 | |||
| Item 5 | How was the relation between theory and active participation? | 0.958 | |||
| Item 6 | How was the session “Anatomy and function”? | 0.487 | |||
| Sum of squares loadings | 3.38 | 2.73 | 2.00 | 1.61 | |
| Proportion variance | 0.21 | 0.17 | 0.12 | 0.10 | |
| Cumulative variance | 0.21 | 0.38 | 0.51 | 0.61 | |
| 61% of the variance was explained by a four-factor model. * Factors extracted by maximum likelihood estimation, extracted factors rotated with varimax. | |||||
This article reports on the development and preliminary psychometric testing of the Knee Osteoarthritis Patient Education Questionnaire (KOPEQ), a new instrument to evaluate the validity of preoperative patient education interventions such as the Knee Osteoarthritis Patient Education Intervention (KOPEI). The development process was based on a conceptual framework and was guided by a group of experts. The KOPEQ had strong internal consistency and a four-factor model was able to explain 61% of the variance.
The characteristics of the items of the KOPEQ demonstrated that for each item at least one person had chosen the ultimate score [5]. When evaluating a personalised intervention there is always a certain risk that patients aim to please. Therefore, it is not unexpected that the ultimate score appears in each item. The difference between the minimal and maximal score is ≥2 in 12 out of 16 items, which is sufficient. The residual four items (2, 3, 6 and 9) show a difference of 1. Item 2 asks for the division of the intervention into three sessions and had a load of 0.840 in the factor analysis. The division of the intervention into three sessions is important. Item 6 is the same type of question as items 7 and 8. Interestingly, the range in item 6 is 1, whereas in item 7 it is 2 and in item 8 it is 3. Therefore, we do not believe that we need to reconsider the formulation of item 6. However, the formulation of items 3 and 9 (“How was the comprehensibility of the text in the hand-outs?”) and (“How were my questions asked?”, respectively) should be reconsidered. Maybe the wording used was too suggestive.
The factor analysis revealed important insights on how “education and training services” and “functioning domains” might be linked together by patients. Factor 1 “didactics” shows the importance of the manner, or how information and knowledge are imparted. Arrangement, layout and comprehensibility of handouts seem to be related to the quality of the answers from the perspective of patients. All aspects are important and all different approaches, and especially their combination, are necessary. These results are supported by Feicke et al., who identified a need to include didactical knowledge to patient education interventions [27].
Factor 2 “addressability” illustrates the overall appearance of the intervention, which is strongly related to the division of the intervention into three sessions. It seems that patients need more than one session, to consolidate the imparted knowledge, which makes sense from the didactical point of view. We have all experienced in different situations the way in which questions arise only after a delay. The second and third sessions, therefore, are also used to clarify questions from the previous session.
Factor 3 “empowerment” demonstrates that practical knowledge on “How will the rehabilitation phase be?” and “What can I do to help myself?” are important issues. Practical knowledge empowers patients to take responsibility and to take control over their situation in some way. This empowerment can also lead to a reduction in fear, which has previously been described by several authors [28–30].
Factor 4 “theory” leads us to believe that patients need information on theory, such as anatomy and function. This knowledge allows them to connect theory and practice, and increases the chance that they are able and willing to transfer theoretical knowledge into their daily activities.
The interviews with patients generated important information. Firstly, patients are focused on walking with canes and climbing stairs, which is understandable since these are often functional discharge criteria [31]. Secondly, patients expect practical advice, as an example on the distance they are recommended to walk after discharge, and they expect motivational support for home exercise. Neither expectation is covered by outcome measures typically used in knee osteoarthritis. Thirdly, none of the patients expressed higher expectations in consequence, as some authors have reported [3, 32, 33]. One patient mentioned explicitly that the imparted knowledge helped her to modify her expectations regarding recovery and to be more patient. Mancuso et al. showed that patients’ expectation can be modified by preoperative education [34].
There is increasing interest in the validation of aspects of patient education interventions. Shoemaker et al. recently presented the Patient Education Materials Assessment Tool (PEMAT), a new measure of understandability and actionability for print and audiovisual patient information [35]. The PEMAT can help lay persons and health professionals select patient education materials that reduce health literacy demands. It can be used to identify understandable and actionable patient education materials. Comprehensibility of print material (or “addressability”) is also an important aspect of our study. In contrast to PEMAT, the KOPEQ includes other aspects to evaluate the validity of a patient education intervention, e.g. didactics, empowerment and theory. Eschalier et al. reported on the validation of an educational booklet targeted at patient-candidates for total knee arthroplasty [36]. The dissemination of an education booklet can ensure uniformity of information delivered by all the professionals involved. It was shown to be effective in improving knowledge in preoperative patients, but not in postoperative patients. It had no influence on beliefs. In contrast to this study, the KOPEQ was designed to evaluate patient education interventions, measuring impacts from 1 week before to up to 6 weeks after TKR surgery. In summary, both groups used the term patient education but focused only on patient information, such as print or audiovisual material. The definition of patient education encompasses much more than patient information. Newman et al. defined patient education as “any combination of planned and organized learning experiences designed to facilitate voluntary adoption of behavior and / or beliefs conducive to health” [37]. In our opinion, in order to increase understanding and motivation, it is important to embed discussion and exchange of experience in patient education interventions.
Our study has several strengths. Firstly, the KOPEQ has undergone psychometric testing and its internal consistency is strong. Secondly, it has been tested qualitatively in patients, in order to understand how they link the content of an educational intervention with its clinical benefit. Thirdly, the FA revealed new insights into how patients link aspects of the intervention with clinical outcomes.
Although specially designed for evaluation of the KOPEI, the principles in this patient education intervention could be applied to other patient education interventions, since all the important aspects of patient education are included.
As with all newly-developed instruments, the KOPEQ can be improved through further development and use in the field. This includes further validation with a larger sample of patients, followed by translation into other languages from the original German and a corresponding cross-cultural adaption.
Our study has some limitations. The relatively small convenience sample of patients (n = 35) may have driven results and, therefore, limited the generalisability of the results.
The KOPEQ can help to provide health professionals with valid feedback on how patients assessed the applied patient education intervention. It is important to evaluate not only the outcome of a patient education intervention, but also its validity. Interviews with patients and a factor analysis revealed new and important insights.
1 Hall M, Migay AM, Persad T, Smith J, Yoshida K, Kennedy D, Pagura S. Individuals’ experience of living with osteoarthritis of the knee and perceptions of total knee arthroplasty. Physiother Theory Pract. 2008;24(3):167–81.
2 Chang HJ, Mehta PS, Rosenberg A, Scrimshaw SC. Concerns of patients actively contemplating total knee replacement: differences by race and gender. Arthritis Rheum. 2004;51(1):117–23.
3 Marcinkowski K, Wong VG, Dignam D. Getting back to the future: a grounded theory study of the patient perspective of total knee joint arthroplasty. Orthop Nurs. 2005;24(3):202–9.
4 McGregor AH, Rylands H, Owen A, Dore CJ, Hughes SP. Does preoperative hip rehabilitation advice improve recovery and patient satisfaction? J Arthroplasty. 2004;19(4):464–8.
5 Lithner M, Zilling T. Pre- and postoperative information needs. Patient Educ Couns. 2000;40(1):29–37.
6 Hoermann S, Doering S, Richter R, Walter MH, Schussler G. Patients’ need for information before surgery. Psychother Psychosom Med Psychol. 2001;51(2):56–61.
7 Trousdale RT, McGrory BJ, Berry DJ, Becker MW, Harmsen WS. Patients’ concerns prior to undergoing total hip and total knee arthroplasty. Mayo Clin Proc. 1999;74(10):978–82.
8 Moran M, Khan A, Sochart DH, Andrew G. Evaluation of patient concerns before total knee and hip arthroplasty. J Arthroplasty. 2003;18(4):442–5.
9 McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A. Preoperative education for hip or knee replacement. Cochrane Database Syst Rev. 2014, 5:CD003526.
10 Hoogeboom TJ, Oosting E, Vriezekolk JE, Veenhof C, Siemonsma PC, de Bie RA, et al. Therapeutic validity and effectiveness of preoperative exercise on functional recovery after joint replacement: a systematic review and meta-analysis. PloS one. 2012;7(5):e38031.
11 Sjoling M, Nordahl G, Olofsson N, Asplund K. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ Couns. 2003;51(2):169–76.
12 Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65.
13 Wilson IB, Kaplan S. Clinical practice and patients’ health status: how are the two related? Med Care. 1995;33(4 Suppl):AS209–214.
14 Macario A, Schilling P, Rubio R, Bhalla A, Goodman S. What questions do patients undergoing lower extremity joint replacement surgery have? BMC Health Serv Res. 2003;3(1):11.
15 Using the think aloud method (cognitive labs) to evaluate test design for students with disabilities and English language learners (Technical Report 44). Available from: [http://education.umn.edu/NCEO/OnlinePubs/Tech44/. 26 July 2014]
16 Schepers VP, Ketelaar M, van de Port IG, Visser-Meily JM, Lindeman E. Comparing contents of functional outcome measures in stroke rehabilitation using the International Classification of Functioning, Disability and Health. Disabil Rehabil. 2007;29(3):221–30.
17 World Health Organization. International Classification of Functioning, Disability and Health. Geneva, Switzerland
18 Alviar MJ, Olver J, Brand C, Hale T, Khan F. Do patient-reported outcome measures used in assessing outcomes in rehabilitation after hip and knee arthroplasty capture issues relevant to patients? Results of a systematic review and ICF linking process. J Rehabil Med. 2011;43(5):374–81.
19 Huber EO, Roos EM, Meichtry A, de Bie RA, Bischoff-Ferrari HA. Effect of preoperative neuromuscular training (NEMEX-TJR) on functional outcome after total knee replacement: an assessor-blinded randomized controlled trial. BMC Musculoskelet Disord. 2015;16:101.
20 Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
21 Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334.
22 Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
23 Lawley DN, Maxwell AE. Factor analysis as a statistical method: American Elsevier Pub. Co.; 1971.
24 Ledesma RDaPV-M. Determining the Number of Factors Retain in EFA: An easy-to-use computer program for carrying out Parallel Analysis. Practical Assessment Research & Evaluation 2007;12(2):1–11.
25 Kaiser H. The varimax criterion for analytic rotation in factor analysis. Psychometrika. 1958;23(3):187–200.
26 R Core Team. R: A language and environment for statistical computing [http://www.R-project.org/.]
27 Feicke J, Sporhase U. Improvements in patient education from the didactical point of view. Rehabilitation. 2012;51(5):300–7.
28 Loft M, McWilliam C, Ward-Griffin C. Patient empowerment after total hip and knee replacement. Orthop Nurs. 2003;22(1):42–7.
29 MacDonald V, Arthur B, Parent S. The Vancouver General Hospital joint replacement rapid recovery program: Optimizing outcomes through focused pathways. Orthop Nurs. 2005;9(2):95–102.
30 Lucas B. Preparing patients for hip and knee replacement surgery. Nursing standard (Royal College of Nursing (Great Britain): 1987) 2007;22(2):50–6; quiz 58.
31 Jones S, Alnaib M, Kokkinakis M, Wilkinson M, St Clair Gibson A, Kader D. Pre-operative patient education reduces length of stay after knee joint arthroplasty. Ann R Coll Surg Engl. 2011;93(1):71–5.
32 Hawker GA. Who, when, and why total joint replacement surgery? The patient’s perspective. Curr Opin Rheumatol. 2006;18(5):526–30.
33 Mahomed NN, Liang MH, Cook EF, Daltroy LH, Fortin PR, Fossel AH, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29(6):1273–9.
34 Mancuso CA, Graziano S, Briskie LM, Peterson MG, Pellicci PM, Salvati EA, Sculco TP. Randomized trials to modify patients’ preoperative expectations of hip and knee arthroplasties. Clin Orthop Relat Res. 2008;466(2):424–31.
35 Shoemaker SJ, Wolf MS, Brach C. Development of the Patient Education Materials Assessment Tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information. Patient Educ Couns. 2014;96(3):395–403.
36 Eschalier B, Descamps S, Boisgard S, Pereira B, Lefevre-Colau MM, Claus D, Coudeyre E. Validation of an educational booklet targeted to patients candidate for total knee arthroplasty. Orthopaedics & traumatology, surgery & research: OTSR 2013;99(3):313–9.
37 Newman S, Mulligan K, Steed L. What is meant by self-management and how can its efficacy be established? Rheumatology. (Oxford, England) 2001;40(1):1–4.
Disclosure statement: No financial support and no other potential conflict of interest relevant to this article was reported.