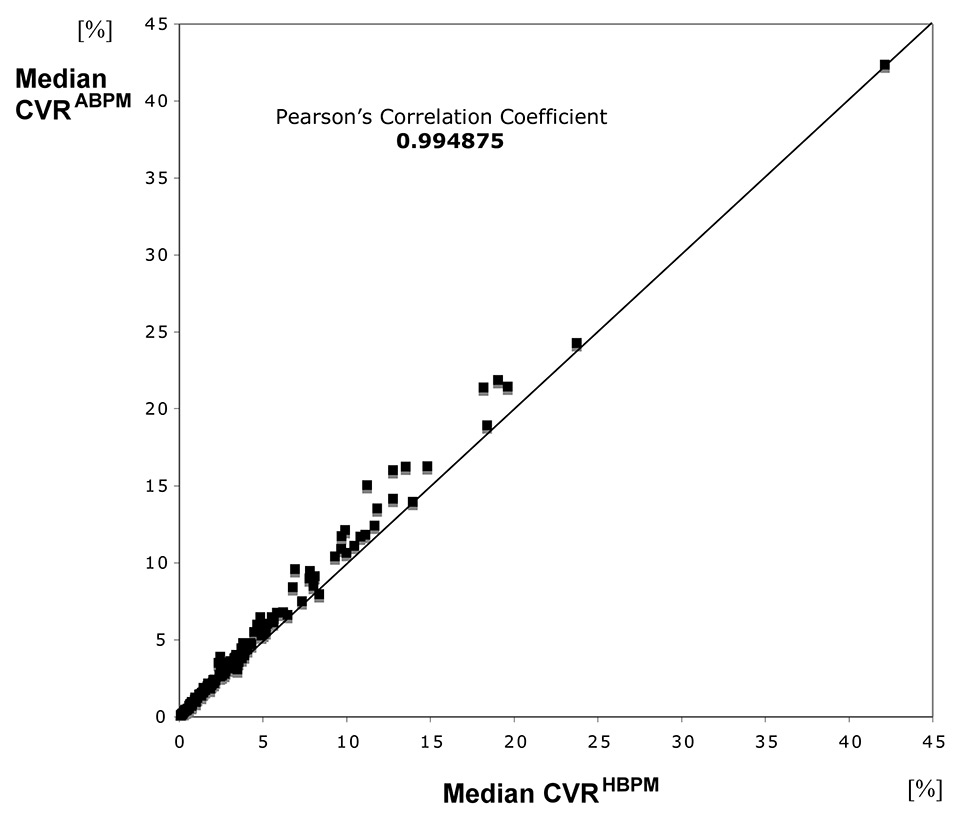
Figure 1
Correlation between CVRABPM and CVRHBPM, calculated by use of median blood pressure levels.
ABPM = ambulant blood pressure measurement; CVR = cardiovascular risk; HPBM = home blood pressure measurement
DOI: https://doi.org/10.4414/smw.2015.14180
Primary prevention of cardiovascular diseases is based on estimations of the patient’s individual cardiovascular risk derived from several risk factors and risk factor levels. Risk functions, derived from longitudinal studies, are used to identify persons at high, moderate and low risk. The significance of these risk functions is determined by the population and individuals that generated them. Several epidemiological studies and risk scores are established for calculation of cardiovascular risk: Framingham Score [1], PROCAM (PROspective CArdiovascular Münster) Score [2–5], Seven Countries Study [6], SCORE Project [7] and European Society of Cardiology (ESC) Heartscore [8]. All these studies use different diagnostic criteria for identification, classification and validation of events [9, 10]. In Germany, the assessment of overall cardiovascular risk is usually performed using the PROCAM algorithm, whereas in Switzerland the AGLA score (ArbeitsGruppe Lipide und Atherosklerose) [11], which is heavily associated with the PROCAM score, is in current use. Whereas the PROCAM score calculates the risk for myocardial infarction in the following decade, the ESC score indicates the 10-year risk for cardiovascular death.
Previously, we have shown that, in our setting, office blood pressure measurements (OBPM) taken by nurses were in the range of home-based self-measurements (HBPM) and that both OBPM and HBPM were lower than ambulatory blood pressure measurements (ABPM) [12]. We therefore used HBPMs and ABPMs to calculate the individual cardiovascular risk (CVR) as estimated with the PROCAM formula in unselected persons of the area of Luzern, Switzerland.
The protocol of this single-centre surveillance study was approved by the Committee for Human Ethics of the Kanton Luzern/Switzerland (No. 613). The study was locally advertised by flyers distributed in a hospital at Luzern (Kantonsspital), inviting interested male and female participants aged from 35 to 65 years to contact the hospital’s Department of Occupational Medicine. Exclusion criteria were defined as follows: a need for immediate antihypertensive treatment, angina pectoris, atrial fibrillation, organic heart disease with haemodynamic impairment, chronic renal or hepatic insufficiency, and current or contemplated pregnancy. After provision of written informed consent and assessment of baseline conditions with a standardised questionnaire, blood pressure was initially measured by our staff using a Boso-medicus PC oscillometric device (grading A/A, validated according to the Association of the Advancement of Medical Instrumentation [AAMI] and the British Hypertension Society protocol [BHS]). Participants were then trained how to measure their blood pressure correctly. They were instructed to undertake HBPMs in the morning, at lunch time and in the evening, for a whole surveillance period of 7–10 days. Each measurement was made three times, 2 minutes apart, after resting seated for at least 10 minutes, and at least 2 hours after any coffee or smoking. Thus, 9 (3x3) single measurements were made per day. Heart rate was recorded simultaneously. For all measurements carried out the size of cuff was adjusted to the individual arm circumference (standard size 12 or size 15 in patients whose arm circumference exceeded 33 cm). HBPM profiles were printed out at the end of the surveillance period.
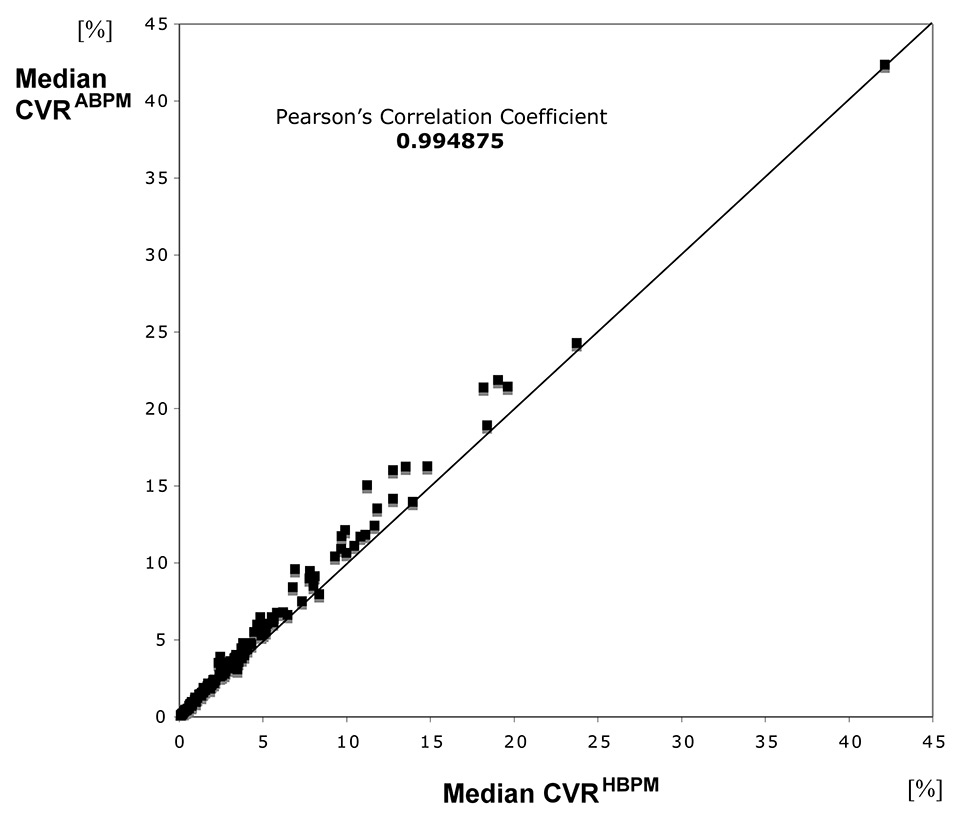
Figure 1
Correlation between CVRABPM and CVRHBPM, calculated by use of median blood pressure levels.
ABPM = ambulant blood pressure measurement; CVR = cardiovascular risk; HPBM = home blood pressure measurement
Those participants whose HBPM exceeded 125/80 mm Hg on average over the surveillance period (n = 153), were invited to participate in additional ABPM. The ABPMs were made on the same arm as used for the HBPMs, using Boso TM-2430 PC oscillometric devices (grading A/A, validated according to the AAMI and BHS). Automatic measurements were made every 15 min from 6 a.m. to 10 p.m.. Participants recorded their activities during the day and the quality of their night’s rest. All data were transferred to the software Boso-Profilmanager 2.
For each participant first quartile, median and third quartile of the distribution of blood pressure (ABPMs and HBPMs) were transferred into the PROCAM formula together with age, weight and laboratory variables, in order to estimate the individual CVR (risk of myocardial infarction) of each patient (CVRABPM, CVRHBPM). Moreover, corresponding risk levels according to the ESC score were mathematically derived (see http://www.uniklinik-freiburg.de/rechtsmedizin/forschung/phytomedizin.html ) using mean ABPM values. Statistical analysis was carried out using the UNIVARIATE, NPAR1WAY and CORR procedures in SAS 9.2, and the figures were plotted using Microsoft Excel.
A total of 153 volunteers (85 men, 68 women) with an average age of 55 years were included. About one third of them suffered from hypertension and consumed antihypertensive medications. Relevant quantitative risk factors are compiled in table 1 together with risk estimations resulting from the PROCAM score and conversions in ESC scores. More than 80% of the participants belong to the low-risk groups for myocardial infarction and cardiovascular events. Qualitative risk factors and the prevalence of sportive activity as an accepted “bonus factor” are summarised in table 2. The study population was characterised by a slightly elevated systolic blood pressure (ABPM) and a moderately increased body mass index (table 1). Mean blood lipid levels were not significantly increased and the mean high density lipoprotein (HDL) value was protective rather than harmful (1.69 mmol/l or 65 mg/dl). There were only a few smokers (12%) and persons consuming alcohol (18%). Only about 4% of all participants suffered from diabetes mellitus. Almost 60% of our study population practiced various kinds of sporting activities, half of them even for more than 20 minutes per day. Familial clustering of cardiovascular diseases was found in about one third of the participants. The majority of all participants (>80%) had a low CVR.
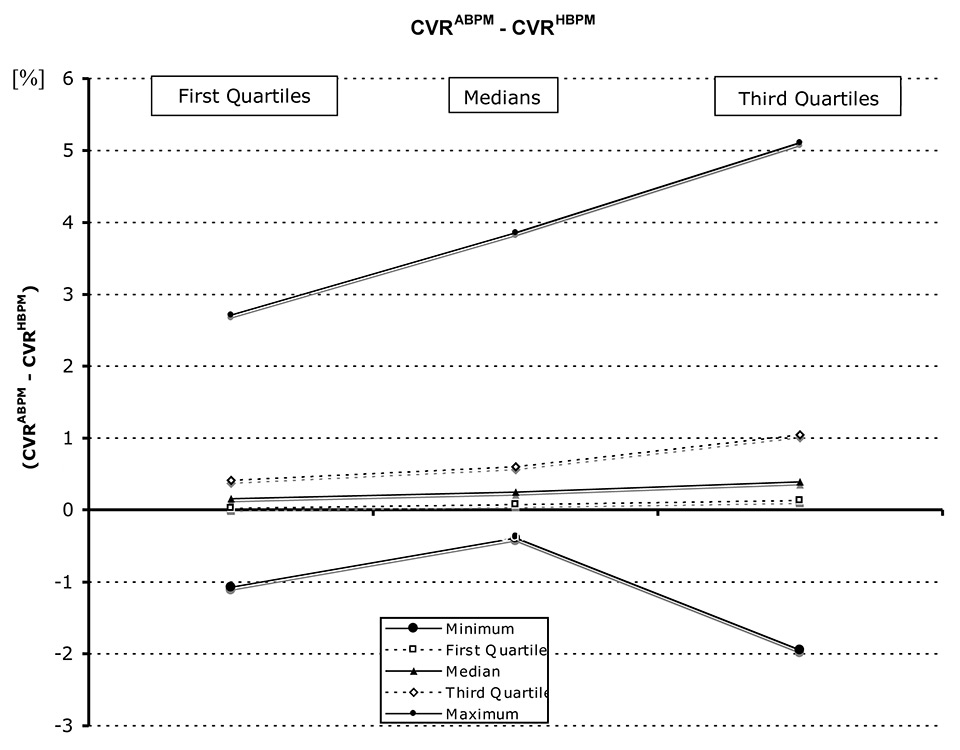
Figure 2
Average differences of measurements based on ABPM and HBPM (CVRABPM - CVRHBPM), calculated for the first quartile, median and third quartile of all patients.
ABPM = ambulant blood pressure measurement; CVR = cardiovascular risk; HPBM = home blood pressure measurement
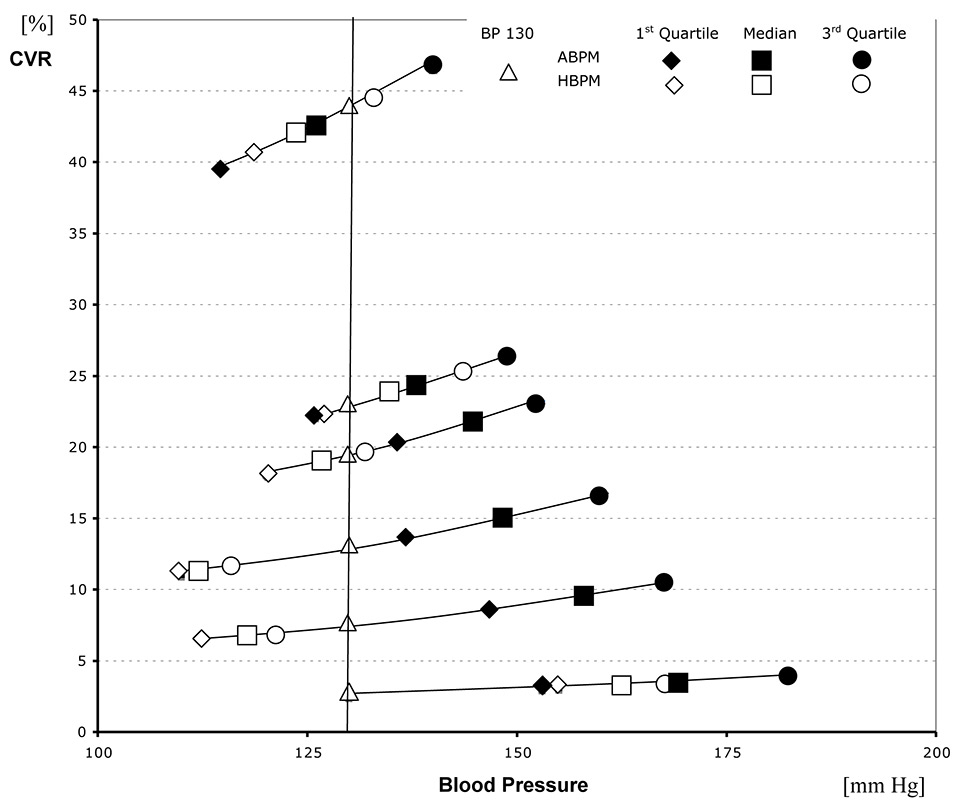
Figure 3
Examples from six participants (1 to 6) of the estimation of CVR by use of the PROCAM formulae, abscissa: blood pressure (mm Hg), ordinate: cardiovascular risk (%) according to the PROCAM algorithm, i.e. risk for myocardial infarction within a period of 10 years. PROCAM risk categories: low risk (<10%), medium risk (10–20%), high risk (>20%).
Moderate changes in systolic BP (mm Hg) lead to very low modifications of CVR. A “basic risk” was calculated as the CVR associated with 130 mm Hg blood pressure (standard value).
ABPM = ambulant blood pressure measurement; CVR = cardiovascular risk; HPBM = home blood pressure measurement
Figure 1 shows a plot of the median CVRABPM against the median CVRHBPM for the 153 participants. The corresponding Pearson correlation coefficient was 0.99. The data points are clustered quite closely around a line that tended to deviate slightly from the line of equality (the diagonal line) at higher values of CVR. Equivalent plots and correlation coefficients based on the first quartile and the third quartile showed no significant deviation from the findings and calculations derived from the median values. Thus, all coefficients and plots demonstrated a very strong correlation of measurements carried out as ABPM and HBPM regardless of whether they were derived from the first quartile, median or third quartile.
Because the difference between ABPM and HBPM was low, the corresponding cardiovascular risk levels estimated by use of the PROCAM score also showed very low numerical differences. For each participant, the CVRHBPM estimated from each index of distribution (first quartile, median and third quartile) was subtracted from the corresponding index of CVRABPM to calculate the average differences of numerical risk (CVRABPM – CVRHBPM). The results of these subtractions are shown in figure 2. CVRABPM tended to be a little bit larger than CVRHBPM in most cases.
Analyses of all data led to the finding that individual risk levels according to the PROCAM score were in the first line determined by the sum of other determinants (smoking, lipid levels, diabetes mellitus, body weight, age, gender) considered in the PROCAM algorithm. Differences in global risk did not result from differences of the average blood pressure. Some examples of this phenomenon are given in figure 3, which shows calculations from six participants (1 to 6) who belonged to different categories of risk. Measurements based on ABPM and HBPM resulted in small differences in risk estimation. For a hypothetical systolic blood pressure of 130 mm Hg, the total risk ranged from 2.5% to 44%. Participant 1 with blood pressure values of 155 to 185 mm Hg had a very low global risk (2.5%). In contrast, participant 6 had a very high global risk (approximately 40%–47%) although blood pressure values were normal (median: 125 mm Hg, range: 112.5–137.5 mm Hg) as a result of antihypertensive treatment.
Figure 4 shows a plot of PROCAM estimations of median CVRs versus the corresponding median blood pressure levels obtained by ABPM; the Pearson correlation coefficient was very low (0.12). Analogue calculations carried out for other quartiles and HBPM led to comparable results. These weak correlations also indicate that – at least in the participants examined – the risk of myocardial infarction (PROCAM score) and the risk of cardiovascular death (ESC score) (table 1) were primarily determined by other risk factors than blood pressure.
| Table 1: Some quantitative characteristics of the 153 volunteers, and their PROCAM and ESC score risk levels. | ||||
| Mean | Median | Standard deviation | Range | |
| Age (years) | 55.3 | 56 | 8.8 | 35–65 |
| Systolic blood pressure (mm Hg) | 146.7 | 145 | 12.9 | 101–190 |
| Diastolic blood pressure (mm Hg) | 87.3 | 87 | 7.7 | 69–109 |
| Heart rate (per min) | 76.5 | 76 | 8.9 | 54–102 |
| Cholesterol (mmol/l) | 5.64 | 5.54 | 1.21 | 3.07–11.88 |
| LDL (mmol/l) | 3.28 | 3.23 | 1.01 | 0.90–8.92 |
| HDL (mmol/l) | 1.69 | 1.61 | 0.45 | 0.80–3.88 |
| Triglycerides (mmol/l) | 1.40 | 1.28 | 0.69 | 0.47–3.95 |
| Body mass index (kg/m2) | 27.6 | 27.1 | 4.3 | 18.7–42.2 |
| Waist to hip ratio | 0.91 | 0.92 | 0.10 | 0.65–1.38 |
| WHR men | 0.96 | 0.97 | 0.09 | 0.65–1.38 |
| WHR women | 0.84 | 0.84 | 0.06 | 0.70–0.98 |
| Waist circumference (cm) | 98.8 | 97.3 | 11.4 | 75.5–126.0 |
| WC men (cm) | 100.7 | 99.8 | 10.6 | 80.0–126.0 |
| WC women (cm) | 96.5 | 95.0 | 12.1 | 75.5–125.5 |
| PROCAM score | ||||
| Global risk (n = 153) (%) | 4.5 | 2.6 | 5.7 | 0.1–42.6 |
| Low risk (n = 132) (%) | 2.7 | 2.1 | 2.4 | 0.1–9.6 |
| Medium risk (n = 16) (%) | 13.5 | 12.9 | 2.4 | 10.6–19.0 |
| High risk (n = 5) (%) | 26.9 | 21.8 | 10.5 | 21.4–42.6 |
| ESC Score | ||||
| Global risk (n = 153) (%) | 0.9 | 0.5 | 1.5 | 0.2–12.4 |
| Low risk (n = 125) (%) | 0.5 | 0.4 | 0.3 | 0.2–1.0 |
| Medium risk (n = 26) (%) | 2.7 | 2.4 | 0.8 | 2.0–4.4 |
| High risk (n = 2) (%) | 10.4 | 10.4 | 2.7 | 8.5–12.4 |
| ESC = European Society of Cardiology; HDL = high density lipoprotein; LDL = low density lipoprotein | ||||
| Table 2:Some qualitative characteristics of the 153 volunteers. | ||
| n | Percent | |
| Treatment with antihypertensive drugs | 49 | 31.8% |
| Nicotine | 18 | 11.7% |
| Diabetes mellitus | 6 | 3.9% |
| Familial clustering | 50 | 32.7% |
| Alcohol | 27 | 17.6% |
| Sports | 91 | 59.5% |
| Sports, >20 minutes per day | 48 | 31.4% |
According to other published findings, ABPM and HBPM are more valid measurement instruments than office measurements for risk assessments [13, 14]. When patients spent an adequate period resting and measurements were carried out by a nurse or other assistant instead of a doctor, office measurements were in the range of HBPMs [12]. In studies with a large numbers of HBPMs (up to 56 HBPMs), the average ABPMs were higher than the average HBPMs [16], similar to our findings [12, 15]. This justified inserting HBPM and ABPM as determinants in our statistical analyses to evaluate their impact on CVR.
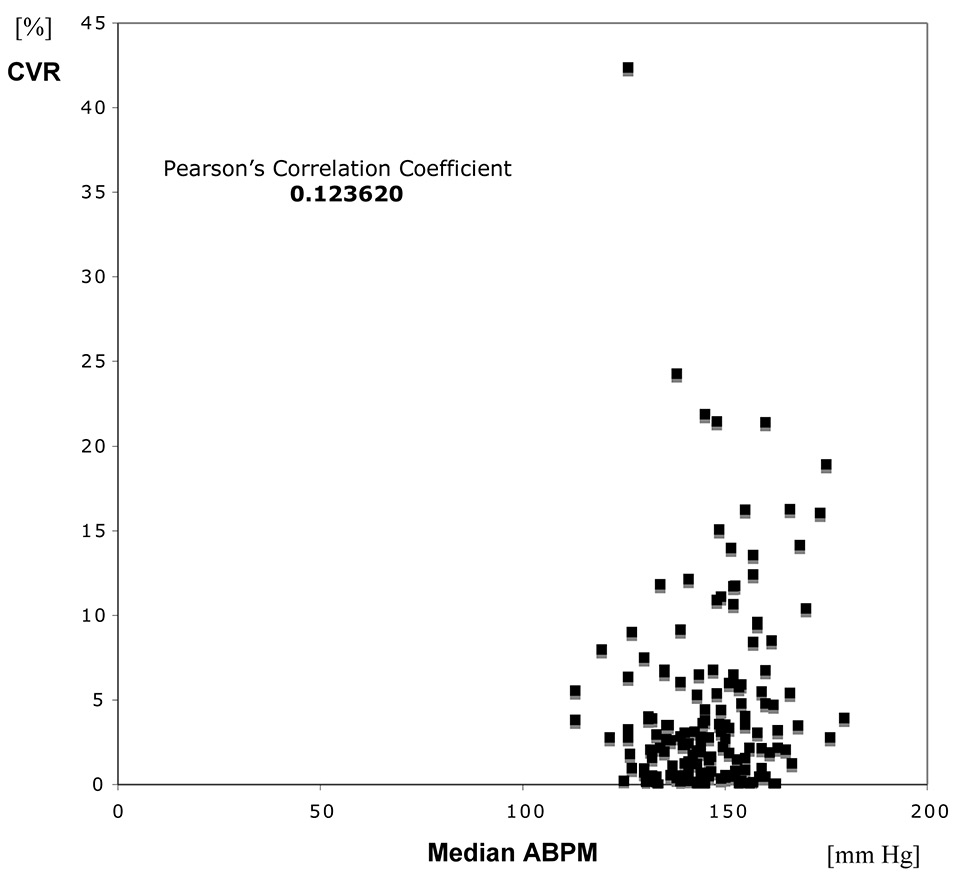
Figure 4
Correlation of CVRABPM with median ABPM.
ABPM = ambulant blood pressure measurement; CVR = cardiovascular risk
Blood pressure measurements are widely used to detect patients with pathological hypertension and to check antihypertensive therapy. Hypertension is the most important risk factor of stroke, but in third position (exceeded by smoking and hyperlipidaemia) with regard to myocardial infarction [17]. Although hypertension affects outcome or quality of life, it must be considered in conjunction with other variables and risk factors – such as age, gender, body weight (obesity), lifestyle habits (smoking), concurrent diseases (diabetes mellitus) and laboratory variables (lipid profiles) ‒ that have a major bearing on outcome. Moreover, familial clustering contributes to the individual cardiovascular risk. Besides the PROCAM Score (http://www.assmann-stiftung.de/procam-studie/procam-tests/), there are a number of models for incorporating these variables, such as the Framingham Score ( http://www.nhlbi.nih.gov/about/framingham/index.html ), the ESC Score (www.agla.ch/risikoberechnung/esc-score), the AGLA score [11], the Heartscore (www.escardio.org/initiatives/prevention/heartscore.htm).
As a “morbidity score”, the PROCAM score can be used to estimate risk of myocardial infarction for men aged from 25 (formerly 35) to 65 years. In women, the risk value calculated for men has to be multiplied by 0.25. This score is based on a total of seven risk factors: four quantitative determinants (LDL, HDL, triglycerides and systolic blood pressure) and three qualitative risk factors (diabetes mellitus, smoking and familial risk of cardiovascular death, “yes/no” criteria). The ESC score, however, is for calculation of risk for cardiovascular death so that it is a “mortality score”. This score can be used for male and female individuals aged from 40 to 65 years. In contrast to the PROCAM score, only three risk factors are considered in the ESC score: total cholesterol, systolic blood pressure and smoking (“yes/no”). However, only the latter discriminates high- from low-risk countries. Switzerland, Belgium, France, Greece, Italy, Luxembourg, Spain and Portugal are classified as low risk countries. Germany, Netherlands, Austria, United Kingdom, Ireland, Scandinavia and the United States of America and another 31 countries are classified as a high risk of cardiovascular mortality. Because the PROCAM and ESC scores are targeted to different events (myocardial infarction versus cardiovascular death), both scores can be regarded as complementary instruments for risk estimation. Because the risk of myocardial infarction is higher than the risk of cardiovascular death – even in the same individuals or populations – both scores differ in their quantitative definitions of risk categories, which are <10% (low risk), <20% (medium risk) and ≥20% (high risk) for the PROCAM score and <1% (low risk), 2–4% (medium risk) and ≥5% (high risk) for the ESC score. Since both scores are based on specific algorithms, mathematical models can be derived in order to convert risk levels from one score to the other [18, 19]. For low-risk countries, the proportionality factor between the PROCAM risk values and the ESC risks was evaluated to be 0.2 [www.uniklinik-freiburg.de/rechtsmedizin/forschung/phytomedizin.html].
Table 1 shows that 86% of the participants screened had a risk below 10% for myocardial infarction within the following decade, 16 participants (11%) had a medium risk and 5 participants only (3%) had a high risk (>20%). Calculated ESC scores (all participants included irrespective of age) classified 82% of the participants into the low-risk group (risk less than 1% for dying of a cardiovascular event), 26 individuals (17%) into the medium-risk group and 2 participants (1.3%) into the high risk group. The unselected population from the area of Luzern reflects, thus, the low-risk grading of Switzerland relative to countries with a high risk.
Because more risk factors and morbidity (not only mortality) are considered in the PROCAM score, compared with the ESC score, we chose to calculate the PROCAM instead of the ESC score, also to be able to include more participants (age 25–65 years [PROCAM] versus 40–65 years [ESC]). None of the currently used risk scores is ideal because some risk factors are considered quantitatively and others qualitatively, and recently identified risk factors are not considered at all [10]. In particular, the Interheart Study [20, 21] discovered that cardiovascular risk is determined by even more risk indicators than those considered in the established risk scores. Therefore, new mathematical models are needed for universal risk estimations that focus on all risk factors currently known (www.joerg-piper.de/Mathematische_Kalkulation_kard/mathematische_kalkulation_kard.html and http://www.joerg-piper.com/Mathematical_Calculation_of_Ca/mathematical_calculation_of_ca.html [18, 19]).
In a previous study we showed that the variability of ABPM was greater than that of HBPM [15]. Nevertheless, both methods seem to be equivalent as tools for long-term measurement of blood pressure and more effective than office measurements, especially with regard to their association with preclinical organ damage assessed by use of echocardiography [13]. This seems true also for other target organ damage [14]. Palatini suggested that both techniques, HBPM and ABPM, should have complementary roles (moderately raised values of the former being an indication to carry out the latter) [22].
Although the number of participants is limited in our pilot study (n = 153), it can be derived from our findings that – at least in our unselected population – given differences in blood pressure had only minor impact on the risk of myocardial infarction. Smoking and metabolic disorders are probably more important, which is in agreement with otherwise published epidemiological findings [17]. The risk of myocardial infarction is “only” increased 2.5-fold when the systolic blood pressure increases from 130 mm Hg to 220 mm Hg [18], but multiplied 9.3 times when the cholesterol/HDL quotient increases from 3.5 to 8.5, and quadrupled by intensive smoking [18]. Thus, even when the blood pressure is higher than normal, the risk for myocardial infarction will just moderately be enhanced, whereas pathologically increased lipid levels or excessive smoking will lead to severe accentuations of the resulting risk even when the blood pressure is normal.
(1) For cardiovascular risk calculation, blood pressure is only one of several risk factors that need to be considered – and it may not necessarily be the most important for lowering CVR. (2) The majority of unselected people recruited in the area of Luzern belong to a low-risk-group according to the PROCAM and ESC criteria. This conforms to the classification of Switzerland as a “low risk” country according to the ESC score.
Acknowledgements:The authors sincerely thank Michael Trippel / Arbeitsmedizinischer Dienst, Kantonsspital Luzern who has left the clinic without leaving an address and, A. Black / Bristol for his support during preparation of the manuscript.
1 National Heart Lung, and Blood Institute, National Institute of Health. Framingham Heart Study. 2002. www.nhlbi.nih.gov/about/framingham/index.html
2 Schulte H, Cullen P, Assmann G. Obesity, mortality and cardiovascular disease in the Münster Heart Study (PROCAM). Atherosclerosis. 1999;144:199–209.
3 Assmann G, Cullen P, Schulte H. Simple scoring scheme for calculating the risk of acute coronary events based on the 10-year follow-up of the Prospective Cardiovascular Münster (PROCAM) Study. Circulation. 2002;105:310–5.
4 Assmann G, Schulte H, Cullen P, Seedorf U. Assessing risk of myocardial infarction and stroke: new data from the Prospective Cardiovascular Münster (PROCAM) Study. Eur J Clin Invest. 2007;37:925–32.
5 International Task Force for Prevention of Coronary Heart Disease. Procam Risik Calculator. 2005. www.chd-taskforce.com/index.html
6 Kromhout D, Menotti A, Blackburn H (Eds). Prevention of coronary heart disease. Diet, lifestyle and risk factors in the Seven Countries Study. Kluwer Academic Publishers, Boston, 2002.
7 Conroy RM, Pyörälä K, Fitzgerald AP, et al., on behalf of the SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Result of a risk estimation study in Europe. Eur Heart J. 2003;24:987–1003.
8 European Society of Cardiology. Heartscore: the interactive tool for predicting and managing the risk of heart attack and stroke in Europe. 2005. www.escardio.org/initiatives/prevention/heartscore.htm http://www.escardio.org/knowledge/decision-tools/heartscore-old/Programme-Download.htm
9 Giampaoli S, Palmieri L, Mattiello A, Panico S. Definition of high risk individuals to optimise strategies for primary prevention of cardiovascular diseases. Nutr Metab Cardiovasc Dis. 2005;15:79–85.
10 Piper J. Kardiovaskuläre Risikostratifizierung in der Primärprävention Teil 1: Möglichkeiten und Grenzen etablierter Risiko-Scores. Präv.-Rehab. 2006;18:1–7. German.
11 Swiss Atherosclerosis Association, Arbeitsgruppe Lipide und Atherosklerose (AGLA): AGLA-Risikorechner. www.agla.ch/risikoberechnung/agla-risikorechner. German.
12 Warren RE, Marshall T, Padfield PE, Chrubasik S. Variability of office, 24-hour ambulatory, and self-monitored blood pressure measurements. Br J Gen Pract. 2010;60:675–80.
13 Bliziotis IA, Destounis A, Stergiou GS. Home versus ambulatory and office blood pressure in predicting target organ damage in hypertension: a systematic review and meta-analysis. J Hypertens. 2012;30:1289–99.
14 Gaborieau V, Delarche N, Gosse P. Ambulatory blood pressure monitoring versus self-measurement of blood pressure at home: correlation with target organ damage. J Hypertens. 2008;26:1919–27.
15 Chrubasik-Hausmann S, Chrubasik C, Walz S, Schulte Mönting J, Erne P. Comparison of home and daytime ambulatory blood pressure measurements. Cardiovascular Disorders. 2014;14:94.
16 Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, Deeks JJ, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BM. 2011;342:d3621.
17 Meurer, KA, Wambach G, Petri E, Deter H Ch. Arterielle Hypertonie (konsetrvative Behandlung). In: Bünte et al. (Edts.): Therapie-Handbuch. Urban & Scharzenberg, München, 1997.
18 Piper J. Kardiovaskuläre Risikostratifizierung in der Primärprävention Teil 2: Neue Aspekte einer erweiterten individuellen Risikoerfassung. Präv-Rehab. 2006;18:8–21.
19 Piper J. Kardiovaskuläre Risikostratifizierung in der Primärprävention Teil 3: Mathematische Modelle zur Relativität von Risikofaktoren und Risiko-Scores. Präv-Rehab. 2006;18:22–8.
20 Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al.; INTERHEART Study Investigators. Effect of protencially modificable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): chase control study. Lancet. 2004;364:937–52.
21 Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al.; INTERHEART Study Investigators. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study. Lancet. 2005;366:1640–9.
22 Palatini P. Ambulatory and home blood pressure measurement: complementary rather than competitive methods. Hypertension. 2012;59:2–4.
Authors’ contribution: All authors have made substantial contributions. Conception: SC-H, PE. Design: SC-H, PE. Acquisition of data: CC(†), JP. Statistical analysis: JS-M. Interpretation of data and discussion with regard to clinical context: SC-H, JP, PE and AB (acknowledged). Sigrun Chrubasik-Hausmann wrote the draft which was revised critically for important intellectual content by all authors except CC who died in a tragic accident. All authors except CC have given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Disclosure statement: Blood measurement devices were provided by boso GmbH, Juningen, Germany. No other potential conflict of interest relevant to this article was reported.