DOI: https://doi.org/10.4414/smw.2015.14188
Many countries have achieved high standards of healthcare for their populations. However, maintaining these care levels is accompanied by a nearly uncontrolled increase of costs that has required many countries to reorganise their healthcare systems during recent years. Costs are thus the most visible surrogate parameter reflecting ongoing irresistible improvements in modern medicine, as well as epidemiological phenomena like increasing population age, and increase in cardiovascular diseases, diabetes mellitus and obesity [1]. One should also keep in mind patients’ strong expectations for a long, healthy and active life in return for paying their national healthcare system.
In this setting, cancer belongs to the greatest burden on healthcare in Western countries, as it is associated with a considerable consumption of resources [2]. The fulminant growing knowledge in various fields of basic research and clinical medicine is leading towards personalised medicine by using novel diagnostic and treatment options for individual patients. For some cancer types, even curative treatment options are available nowadays, while some other cancers can be at least transformed into long-lasting, chronic diseases with repeated treatments. Nonetheless, modern medicine struggles to develop effective treatments for aggressive cancers, such as pancreatic adenocarcinoma, where patients’ long-term survival is rare [3, 4].
Realistic estimations of future cancer incidences and mortality rates are important parameters impacting on planning and organisation of national healthcare [5]. Therefore, meticulous data on cancer incidence and mortality over the past years or, even better, decades, are required to establish solid future trends. Unfortunately, national tumour registries are not yet established everywhere. Furthermore, a lot of demographic items and epidemiological data (e.g., birth rates, risk factors, population aging, or migration rates) need to be known in order to be taken into account for creating reliable models of the future development of national populations.
This study primarily aimed to evaluate the future national burden of gastrointestinal cancers that Switzerland could face in 2020–24 and 2025–29. Future crude incidence and mortality rates of oesophageal, gastric, pancreatic, liver and colorectal cancers were estimated.
Swiss Statistics is the Federal Office of Statistics ( http://www.bfs.admin.ch ) that has provided incidences and mortality rates on various cancers since 1985 by summarising the data of 16 regional tumour registries covering almost the whole country [6]. Cancer incidences (new cases per 100 000 inhabitants, crude and standardised rates for European population) and mortality rates (deaths per 100 000 inhabitants, crude and standardised rates for European population) from 1985 to 2009 were analysed to estimate trends of future incidence and mortality rates. All Swiss data used for calculations were obtained from the online database (STAT-TAB) of Swiss Statistics [6]. European-standardised incidences are based on the European-standardised population of 2013.
Based on available national epidemiological data and estimates of external factors (i.e., migration phenomena, Swiss foreign policy [socioeconomic trends and free movement of persons in Europe], and demographic evolution [population aging, birth and mortality rates]), Swiss Statistics has constructed three different models of future developments of the Swiss population. The low hypothesis model takes into account the lowest estimations of all the above-mentioned parameters, whereas the high hypothesis model takes into account the highest estimations. The average model between the low and high hypothesis models is considered by Swiss Statistics as the most probable scenario. These population models can also be obtained online from Swiss Statistics [6]. The most probable scenario of the future development of the Swiss population, as proposed by Swiss Statistics, was used to calculate the new cancer cases (incident cases) and the cancer-related deaths for 2024 and 2029. Of note, crude rates were used since they represent the real national cancer burden, and therefore, they fit better for future specific planning of healthcare resources.
According to Swiss Statistics’ proposed most probable scenario, the Swiss population will be 8 524 627 inhabitants in 2024 and 8 687 312 in 2029 comprising 4 200 991 males and 4 323 636 females in 2024, and 4 283 347 males and 4 403 965 females in 2029. The male:female ratio will be 0.97 in 2024 and 2029 in comparison with 0.98 in 2012. Compared with 2012 (8 039 060 inhabitants), the population will increase by 6% in 2024 and by 8.1% in 2029. The median age range will be 55–59 years in 2024 and 60–64 years in 2029. Of the overall population, 22.4% will be older than 65 in 2024 and 24.7% in 2029; in 2012, only 17.4% were among this age group.
Only primary cancers of the respective organs were included in this current analysis; metastases from other organs were excluded. Oesophageal cancers included squamous cell carcinomas, adenocarcinomas and rare primaries such as sarcomas. Gastric cancers included adenocarcinomas and rare primaries such as sarcoma or malignant gastrointestinal stromal tumours (GIST). Tumours of the gastroesophageal junction were classified as oesophageal cancers. Pancreatic cancers encompassed ductal adenocarcinomas and all other types like cystadenocarcinomas or malignant intraductal papillary and mucinous neoplasms (IPMN). Liver cancers included hepatocellular carcinomas, cholangiocarcinomas and rare primaries such as sarcomas. Colorectal cancers mainly encompassed adenocarcinomas.
Linear regressions and Joinpoint analyses [7] were performed to estimate the future trends of incidences and mortality rates. Linear regressions were calculated using GraphPad Prism 5.0 for Mac OS X (GraphPad Software Inc.). Joinpoint analyses allowed only one joinpoint (breakpoint) and were performed by using Joinpoint Regression Program, version 4.0.1 (January 2013), from the Statistical Research and Applications Branch of the National Cancer Institute [7]. Joinpoint projections were extrapolated from the linear equation of the final segment. As Joinpoint is not suitable for long-term predictions, mid-term time points (2024 and 2029) were chosen.
Comparisons with other European and North American countries were made. Relevant articles on gastrointestinal cancer incidences and mortality rates were identified in MEDLINE (through PubMed) by use of the appropriate MeSH terms for the following search items: gastrointestinal cancer, epidemiology AND incidences AND mortality. The search was limited to studies published between January 1980 and June 2013. Only articles published in English were considered eligible [8].
Standardised rates for European populations were used for international comparisons as appropriate. Otherwise, crude incidence rates were preferred because they represent the real national cancer burden.
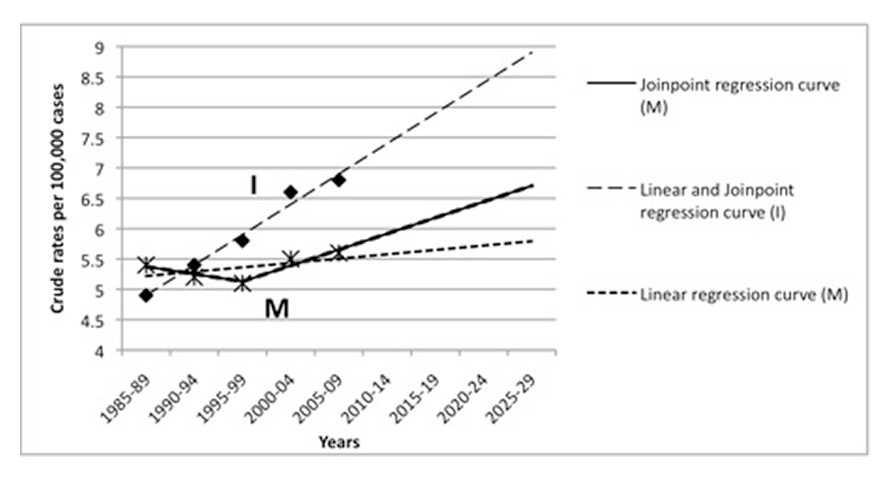
Crude incidence and mortality rates for Switzerland are summarised graphically in figure 1. Joinpoint projections of incidence and death rates for 2020–2024 and 2025–29 for all five cancers are reported in table 1.
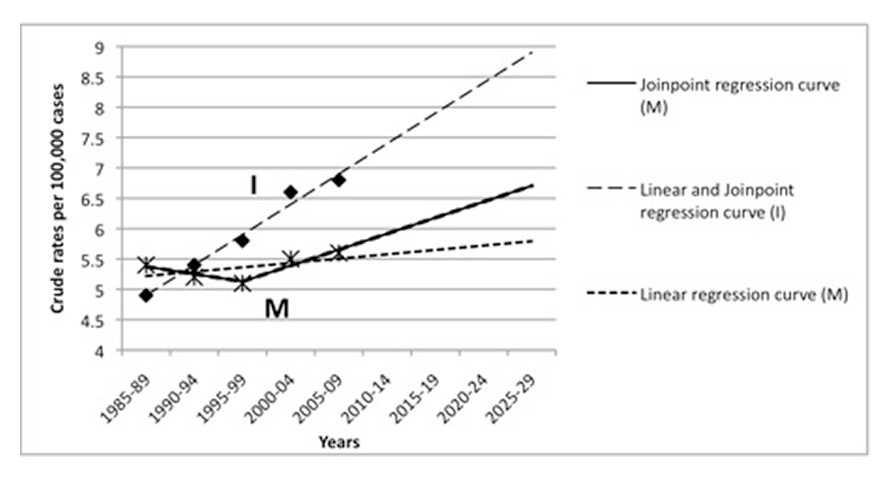
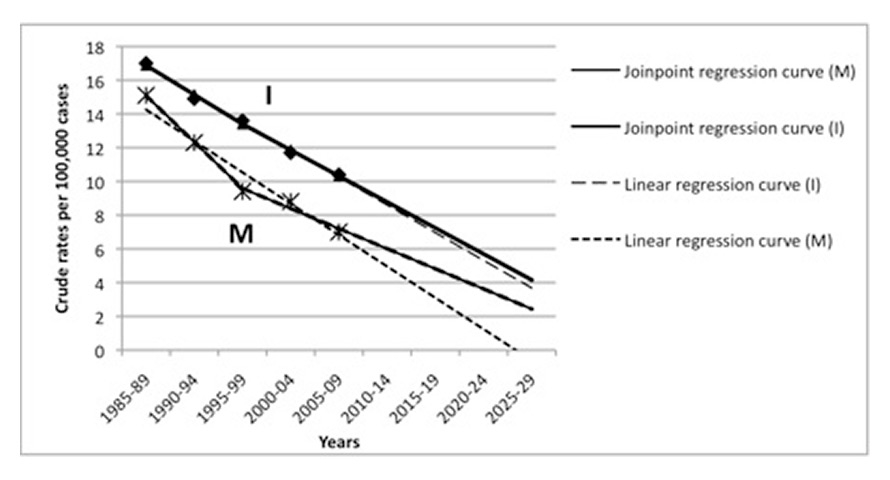

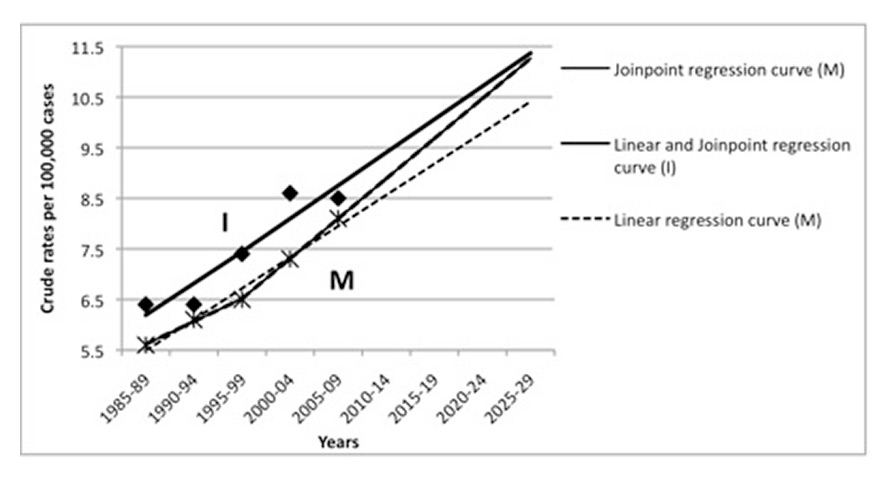
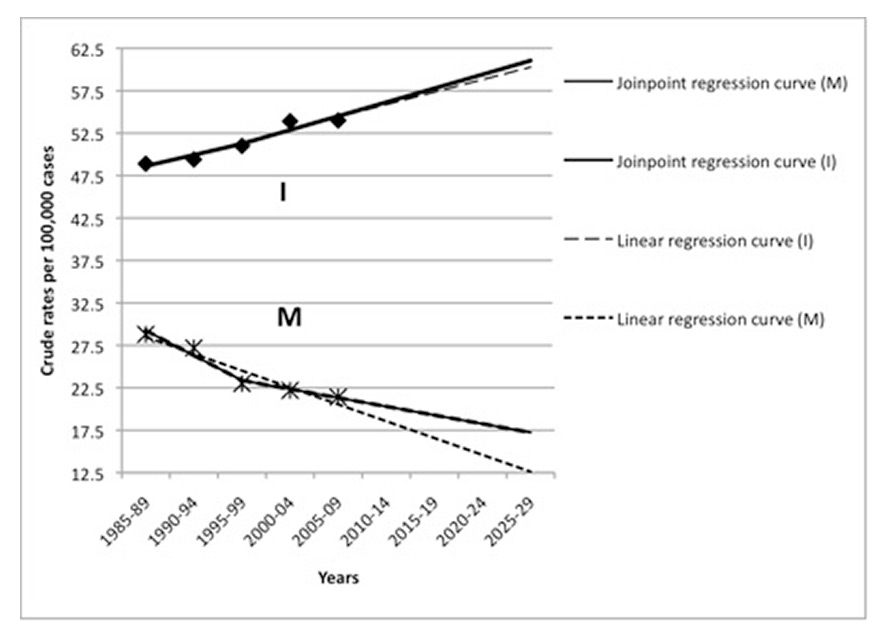
Figure 1
Crude incidence (I, diamonds represent the figures extracted from STAT-TAB) and mortality (M, asterisks represent the figures extracted from STAT-TAB) rates (median per year per 100 000 inhabitants) from 1985‒89 to 2025‒2029 in Switzerland with linear and Joinpoint regression models.
A Oesophageal cancer
B Gastric cancer
C Pancreatic cancer
D Liver cancer
E Colorectal cancer
Table 2 shows the Joinpoint projections of incidence rates stratified by gender for 2020–24 and 2025–29 for all five cancers (crude rates). It depicts that the incidence rates in men followed and are predicted to follow similar trends as the incidence rates in women for all the five cancers examined.
From 1985–89 to 2025–29, median annual crude rates of oesophageal cancer incidences increased, according to the two statistical methods used. According to the Joinpoint regression, crude incidence rates will reach 8.4/100 000 in 2020–24 and 8.9/100 000 in 2025–29, whereas European-standardised incidence rates will be 5.8/100 000 in 2020–24 and 5.9/100 000 in 2025–29. The crude mortality rates will rise slightly (linear method: from 5.4 in 1985–89 to 5.8/100 000 in 2025–29 and Joinpoint method: 6.7/100 000 in 2025–29). The numbers of new oesophageal cancer patients are predicted to be 716 and 773 in 2024 and 2029, respectively (317 in 1989), whereas the numbers of oesophageal cancer deaths is predicted to be 546 and 582, respectively (349 in 1989).
According to the two statistical methods, median annual crude and European-standardised gastric cancer incidences will strongly decrease until 2025–29. In 2020–24 the crude incidence rate will be 5.7/100 000 (European-standardised: 4.7) and 4.2/100 000 (European-standardised: 3) in 2025–29 (Joinpoint method). The crude mortality rates will also drastically diminish from 15.1 in 1985‒89 to 2.4/100 000 in 2025–29 (Joinpoint method). The number of new patients suffering from gastric cancer is estimated to be 486 in 2024 and 361 in 2029 (1 106 in 1989), despite the increased population. The numbers of deaths from gastric cancer in 2024 and 2029 are estimated to be 307 and 209, respectively (977 in 1989).
The linear and Joinpoint regressions predict that the crude incidence rates of pancreatic cancer will increase in the 2025–29 period. According to the Joinpoint method the median annual crude incidence rates will be 16.8/100 000 (standardised rate: 9.7) and 17.8/100 000 (standardised rate: 9.7) in 2020–24 and 2025–29, respectively. The crude mortality rate is predicted to increase (linear method: from 12.2 in 1985-89 to 13.9/100 000 in 2025–29 and Joinpoint regression: 16.1/100 000 in 2025–29). The numbers of new pancreatic cancer patients are predicted to be 1 434 in 2024 and 1 542 in 2029 (840 in 1989), while the number of deaths related to pancreatic cancer is predicted to be 1 313 in 2024 and 1 399 in 2029 (789 in 1989).
In 2025–29, the crude incidence rate of liver cancer patients is predicted to increase according to our two methods. The crude incidence is estimated to be 10.7/100 000 and 11.4/100 000 in 2020–24 and 2025–29, respectively (Joinpoint analysis). According to the Joinpoint analysis, the European-standardised incidence is estimated to be 7.5/100 000 and 7.7/100 000 in 2020–24 and 2025–29, respectively. Crude mortality rates are predicted to increase in 2020–24 (Joinpoint method: 10.5/100 000 and linear method: 9.8/100 000) and 2025–29 (Joinpoint method: 11.3/100 000 and linear method: 10.4/100 000) periods. The number of new liver cancer patients is estimated to be 913 in 2024 and 987 in 2029 (412 in 1989). Deaths due to liver cancer are projected to be 895 and 982 in 2024 and 2029, respectively (362 in 1989).
Our two methods predict an increased crude incidence rate of colorectal cancer in 2025–29. According to the Joinpoint method crude incidence rates will reach 59.4/100 000 (European-standardised: 38) in 2020–24 and 61.1/100 000 (European-standardised: 37.2) in 2025–29. On the contrary, crude mortality rates will significantly diminish in 2020–24 (from 28.8 in 1985‒89 to 18.3/100 000 according to the Joinpoint regression) and 2025‒29 (17.2/100 000 according to the Joinpoint regression). The number of new patients suffering from colorectal cancers is predicted to be 5 066 and 5 304 in 2024 and 2029, respectively (3 194 in 1989). The number of deaths due to colorectal cancer is estimated to be 1 560 in 2024 and 1 494 in 2029 (1 863 in 1989).
| Table 1: Joinpoint predicted incidence and death rates (median per year per 100’000 inhabitants) in Switzerland compared to 1985–89 and 2005–09 for all five tumour entities. | ||||
| Incidences (per 100 000) / Death rates (per 100 000) | ||||
| 1985–89 | 2005–09 | 2020–24 | 2025–29 | |
| Crude rates | ||||
| Oesophageal cancer | 4.9/5.4 | 6.8/5.6 | 8.4/6.4 | 8.9/6.7 |
| Gastric cancer | 17/15.2 | 10.4/7 | 5.7/3.6 | 4.2/2.4 |
| Pancreatic cancer | 12.9/12.2 | 14/13.4 | 16.8/15.4 | 17.8/16.2 |
| Liver cancer | 6.4/5.6 | 8.5/8.1 | 10.7/10.5 | 11.4/11.3 |
| Colorectal cancer | 48.9/28.8 | 54/21.4 | 59.4/18.3 | 61.1/17.2 |
| Rates standardised to European population | ||||
| Oesophageal cancer | 4.6/5.1 | 5.4/4.3 | 5.8/4.2 | 5.9/4.2 |
| Gastric cancer | 14.4/12.3 | 7.7/4.9 | 4.7/1.1 | 3/0 |
| Pancreatic cancer | 10.7/10.1 | 9.7/9.2 | 9.7/9.2 | 9.7/9.2 |
| Liver cancer | 5.8/4.9 | 6.8/6.1 | 7.5/6.9 | 7.7/7.2 |
| Colorectal cancer | 41.6/23.3 | 40/14.6 | 38/9.5 | 37.2/7.8 |
| Table 2: Incidence rates by gender from 1985 to 2009 and Joinpoint predicted incidence rates stratified by gender for 2020–24 and 2025–29 (median per year per 100 000 inhabitants) in Switzerland for all five tumour entities (crude rates). | ||||||||||
| Oesophageal | Gastric | Pancreatic | Liver | Colorectal | ||||||
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| 1985–89 | 7.5 | 2.3 | 20.5 | 13.4 | 12.8 | 12.9 | 9.8 | 3.0 | 52.5 | 45.2 |
| 1990–94 | 8.1 | 2.7 | 17.9 | 11.8 | 12.1 | 11.7 | 9.7 | 3.0 | 53.7 | 45.0 |
| 1995–99 | 8.6 | 2.9 | 17.0 | 10.2 | 12.5 | 12.2 | 11.2 | 3.6 | 55.5 | 46.4 |
| 2000–04 | 10.0 | 3.2 | 14.6 | 8.7 | 13.2 | 13.2 | 13.1 | 4.1 | 59.8 | 48.0 |
| 2005–09 | 10.1 | 3.4 | 12.8 | 7.9 | 13.6 | 14.3 | 12.9 | 4.0 | 61.1 | 46.9 |
| 2020–24 | 12.6 | 4.1 | 6.9 | 4.3 | 15.6 | 17.9 | 16.0 | 4.9 | 70.3 | 48.7 |
| 2025–29 | 13.4 | 4.3 | 4.9 | 3.1 | 16.3 | 19.1 | 17.1 | 5.2 | 73.2 | 49.1 |
This study estimated future developments of gastrointestinal cancer incidences and mortality rates in Switzerland up to 2030 and compared these findings with current international data. While oesophageal, pancreatic, liver and colorectal cancer incidences will significantly increase, gastric cancer incidence is decreasing to a very low level. Mortality rates of oesophageal, pancreatic and liver cancer will remain either stable or slightly increase. In contrast, gastric cancer and colorectal cancer mortality will significantly decrease. The most common gastrointestinal malignancy in Switzerland will be colorectal cancer, followed by pancreatic, liver and oesophageal cancer.
Among the different tumour entities analysed, oesophageal cancer will show an impressive increase in the number of new cases (rise of 40% from 2005–09 to 2020–24), in which males still predominate. As the Swiss population substantially increases and gets older, the absolute number of new cases per year will be 2.4 times higher in 2029 compared with 1985. Since most oesophageal cancer patients nowadays undergo multimodal treatment with radiochemotherapy and surgery, treatment costs will massively increase. Similar findings have been reported in the United Kingdom. Gatenby et al. estimated that the number of new cases (adenocarcinomas and squamous cell carcinomas) will rise by 40% for men from 2007 to 2020 [9].
In all European countries, gastric cancer mortalities have shown an undiminished decline since 1980. For France, the Netherlands, Sweden, Finland, Norway, Denmark and the United Kingdom, it has been estimated that death rates will further diminish by 66% from 2005 to 2030 [10]. Switzerland presented a similar diminution of gastric cancer mortality rates for the past three decades. The 2000–04 mortality rates are predicted to diminish by 73% up to 2025–29 (8.8 to 2.4 per 100 000). As a consequence, management of gastric cancer – regarding neither patient numbers nor healthcare consumption – will represent an important issue in the future. The only relevant question will be whether the treatment of gastric cancer patients should not be centralised in a few centres to get a reasonable caseload guaranteeing high quality treatment.
Patient age is the single most important epidemiological risk factor for pancreatic cancer. In order to get realistic patient numbers for the planning of future healthcare resources, only crude incidence rates should be used. It is an illustrative example of how a malignant disease can be potentially underestimated by reporting age-standardised incidence rates. In Switzerland, the global age-standardised incidence of pancreatic cancers has diminished from 10.7/100 000 in 1985–89 to 9.7/100 000 in 2005–09. Nevertheless, according to our prediction based on crude incidence rates, in 2025–29 the number of new patients suffering from pancreatic cancers will increase by 61% compared with 2000–2004 (i.e., up to 1 542 patients) with a slight preponderance of male patients. Very similar findings have been reported from Canada, where the incidence of pancreatic cancer has been stable for women from 1995 to 2002, and has slightly diminished for men. However, the number of pancreatic cancer cases is expected to more than double in 2031: it is likely to be 5 619 patients as a result of a substantial increase of the population over 65 years of age [11].
Eheman et al. [12] predicted that in 2020 pancreatic cancer will be the second cause of cancer death in the United States, just behind lung cancer, which means it would jump from the fourth to the second place. It is important to mention that pancreatic cancer is the only gastrointestinal cancer that has an increase of both death rate and incidence. The number of US people suffering from pancreatic cancer is predicted to double by 2030 increasing to 62 000 people [13]. Pancreatic cancer has become the fourth most frequent cause of cancer death in both sexes in the European Union (world-adjusted mortality rate 6.6/100 000 in 2013) [14]. Our prediction model for Switzerland estimates that in 2025‒29, pancreatic cancer could be the leading cause of gastrointestinal cancer-related deaths.
Whereas worldwide liver cancer incidences will probably remain stable in the forthcoming years, according to Bray et al. [5], incidences in Switzerland will slightly increase in the near future (from 6.8 per 100 000 inhabitants to 7.5 in 2020–24 and 7.7 in 2025–29 for the Joinpoint analysis). Of note, once a successful treatment of hepatitis C is available, liver cancer incidences will decrease with a latency of several years owing to the diminution of hepatocellular carcinomas [15]. In Switzerland, the peak of hepatitis C has been predicted to be in 2030, because presently around 50% of the cases are estimated to be undiagnosed. After reaching the incidence peak of the disease, a 20-year latency will be seen before a diminution of hepatocellular carcinomas will appear [16].
Regarding the liver cancer predictions (hepatocellular carcinomas, cholangiocarcinomas and other rare primaries), an important point should be mentioned. Once the hepatitis C incidence has decreased, the number of non-alcoholic fatty liver disease (NAFLD) diagnoses will probably rise. As NAFLD has been proven to be a risk factor for hepatocellular carcinoma, projections of future liver cancer incidence are therefore very difficult [17].
Currently, Ireland has one of the highest rates of colon cancer mortality in Europe (standardised rate: 16.2 per 100 000 for the 2003–07 period). However, the future trend is toward a decline of this mortality rate (14 per 100 000 for 2013–17) due to screening programmes and public health promotion [18, 19]. In Spain, colorectal cancer crude mortality is likely to increase to 30.5/100 000 in 2015–19. Mortality will slightly increase among men, and level off among women [20]. In the USA, the population over 50 years of age represented 26% of the entire population in 1992 and will represent 36% in 2050. The consequence will be a doubling of colorectal cancer admissions if the incidence rates remain the same as today [21]. The colorectal standardised mortality rate in Switzerland was 14.6 per 100 000 in 2005–09. The mortality will also diminish in the future (prediction of a mortality rate of 9.5/100 000 in 2020–24 according to the Joinpoint regression).
In the Aragon province of Spain, colorectal cancer incidence will rise gradually reaching 39/100 000 in 2022. The incidence will particularly increase in men and slightly decrease in women [22]. Predictions of Swiss colorectal cancer incidences show a slight decrease for future years. Indeed, the European population-adjusted incidence could drop to 38 per 100 000 in 2020–24 compared to 41.7 in 1995–99. Switzerland will face a substantial increase of the population aged over 50 years (from 32% of the population in 1992 to 47.7% in 2050). The total number of colorectal cancer cases will therefore increase in upcoming years.
Epidemiological data need to be interpreted cautiously. All projections hypothesise that the same rate of cancer detection will apply for the forthcoming years. However, increase of incidences among some gastrointestinal cancers can be a result of recent improvements of screening or diagnostic methods. Moreover, the projection method should be chosen according to the natural history of the cancer, based on epidemiology. In this study, we decided to choose two methods in order to have different variants. Regarding the Joinpoint method used for extrapolation, it was assumed that in the upcoming 10 to 15 years there will be no important events that would induce significant changes in the trajectory of the incidence rates. If this latter assertion was false, the precision of the Joinpoint extrapolations would decrease. Higher population age, increasing obesity and diabetes mellitus rates, as well as behavioural changes (e.g. smoking habits among women) are commonly observed in many Western countries. Changes in cancer risk factors will definitely influence future cancer epidemiology. In addition, migration phenomena impact importantly on national populations. As migration is often driven by economic reasons and the prospect of a better life, rich countries encounter an increase of their national population even though birth rates of the native population are low; while poorer countries are at risk of younger people leaving. The constant improvement of diagnostic tools and cancer treatments is also an element to take into account when analysing the future cancer burden. In addition to all these aspects, changes of gastrointestinal cancer incidences are also possibly related to genetic and epigenetic variations between different populations.
Switzerland is classified as a high-income country and several papers have shown that cancer epidemiology in Switzerland is similar to some other Western and Northern European countries [23–26]. Moreover, the majority of the international comparisons of future cancer burden predictions made between Switzerland and other European and North American countries showed similar results [9–11, 14]. Data presented in this study can therefore be generalisable, or at least extrapolated, to countries with similar cancer epidemiology and comparable population demographic evolution.
In conclusion, oesophageal, pancreatic, hepatic and colorectal malignancies will represent an increasing gastrointestinal cancer burden in Switzerland. Their national incidences are well in line with the findings in most European and North American countries. Only gastric cancer will become a rare disease by the mid-21st century. Since centralisation of complex surgery is an ongoing process, future multidisciplinary cancer centres will require substantial resources in order to maintain a high treatment quality.
1 United Nations, Department of Economic and Social Affairs, Population Division (2013). World Population Prospects: The 2012 Revision. http://esa.un.org/wpp/Excel-Data/population.htm. Accessed 2014.
2 Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013;14:1165–74.
3 Ferrone CR, Brennan MF, Gonen M, Coit DG, Fong Y, Chung S, et al. Pancreatic adenocarcinoma: the actual 5-year survivors. J Gastrointest Surg. 2008;12:701–6.
4 Hartwig W, Hackert T, Hinz U, Gluth A, Bergmann F, Strobel O, et al. Pancreatic cancer surgery in the new millennium: better prediction of outcome. Ann Surg. 2011;254:311–9.
5 Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008-2030): a population-based study. Lancet Oncol. 2012;13:790–801.
6 Swiss Federal Statistical Office. Online data search (STAT-TAB) http://www.bfs.admin.ch/bfs/portal/en/index.html. Accessed 2014.
7 Joinpoint Regression Program. 4.0.1. Jan 2013; Statistical Research and Applications Branch. National Cancer Institute NCI, USA.
8 Moher D, Pham B, Klassen TP, Schulz KF, Berlin JA, Jadad AR, et al. What contributions do languages other than English make on the results of meta-analyses? J Clin Epidemiol. 2000;53:964–72.
9 Gatenby PAC, Hainsworth A, Caygill C, Watson A, Winslet M. Projections for oesophageal cancer incidence in England to 2033. Eur J Cancer Prev. 2011;20:283–6.
10 Amiri M, Janssen F, Kunst AE. The decline in stomach cancer mortality: exploration of future trends in seven European countries. Eur J Epidemiol. 2011;26:23–8.
11 Flook R, van Zanten SV. Pancreatic cancer in Canada: incidence and mortality trends from 1992 to 2005. Can J Gastroenterol. 2009;23:546–50.
12 Eheman C, Henley SJ, Ballard-Barbash R, Jacobs EJ, Schymura MJ, Noone AM, et al. Annual Report to the Nation on the status of cancer, 1975-2008, featuring cancers associated with excess weight and lack of sufficient physical activity. Cancer. 2012;118:2338–66.
13 Smith BD, Smith GL, Hurria A, Hortobagyl GN, Buchholz TA. Future of cancer incidence in the United States: burdens upon an aging, changing nation. J Clin Oncol. 2009;27:2758–65.
14 Malvezzi M, Bertuccio P, Levi F, La Vecchia C, Negri E. European cancer mortality predictions for the year 2013. Ann Oncol. 2013;24:792–800.
15 Testino G, Borro P. Chemoprevention of hepatocellular carcinoma in patients with hepatitis C virus related cirrhosis. World J Hepatol. 2013;5:521–7.
16 Razavi H, Waked I, Sarrazin C, Myers RP, Idilman R, Calinas F, et al. The present and future disease burden of hepatitis C virus (HCV) infection with today's treatment paradigm. J Viral Hepat. 2014;21:34–59.
17 White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012;10:1342–59.
18 O’Lorcain P, Deady S, Comber H. Mortality predictions for colon and anorectal cancer for Ireland, 2003–17. Colorectal Dis. 2006;8:393–401.
19 Maddams J, Utley M, Møller H. Projections of cancer prevalence in the United Kingdom, 2010–2040. Br J Cancer. 2012;107:1195–1202.
20 Ribes J, Navarro M, Clèries R, Esteban L, Pareja L, Binefa G, et al. Colorectal cancer mortality in Spain: trends and projections for 1985-2019. Eur J Gastroenterol Hepatol. 2009;21:92–100.
21 Seifeldin R, Hantsch JJ. The economic burden associated with colon cancer in the United States. Clin Ther. 1999;21:1370–9.
22 Bezerra-de-Souza DL, Bernal MM, Gómez FJ, Gómez GJ. Predictions and estimations of colorectal cancer mortality, prevalence and incidence in Aragon, Spain, for the period 1998-2022. Rev Esp Enferm Dig 2012;104:518–23.
23 Bertuccio P, Chatenoud L, Levi F, Praud D, Ferlay J, Negri E. Recent patterns in gastric cancers: A global overview. Int J Cancer. 2009;125:666–73.
24 Malvezzi M, Bertuccio P, Levi F, La Vecchia. European cancer mortality predictions for the year 2014. Ann Oncol. 2014;25:1650–6.
25 Fernandez E, La Vecchia C, Gonzalez JR, Lucchini F, Negri E, Levi F. Converging patterns of colorectal cancer mortality in Europe. Eur J Cancer. 2005;41:430–7.
26 Bosetti C, Bertuccio P, Malvezzi M, Levi F, Chatenoud L, Negri E, et al. Cancer mortality in Europe, 2005-2009, and an overview of trends since 1980. Ann Oncol. 2013;24:2657–71.
Disclosure statement: No financial support and no other potential conflict of interest relevant to this article was reported.
This paper was presented in part at the 100th Annual Congress of the Swiss Surgical Society, June 12‒14, 2013, Bern, Switzerland.