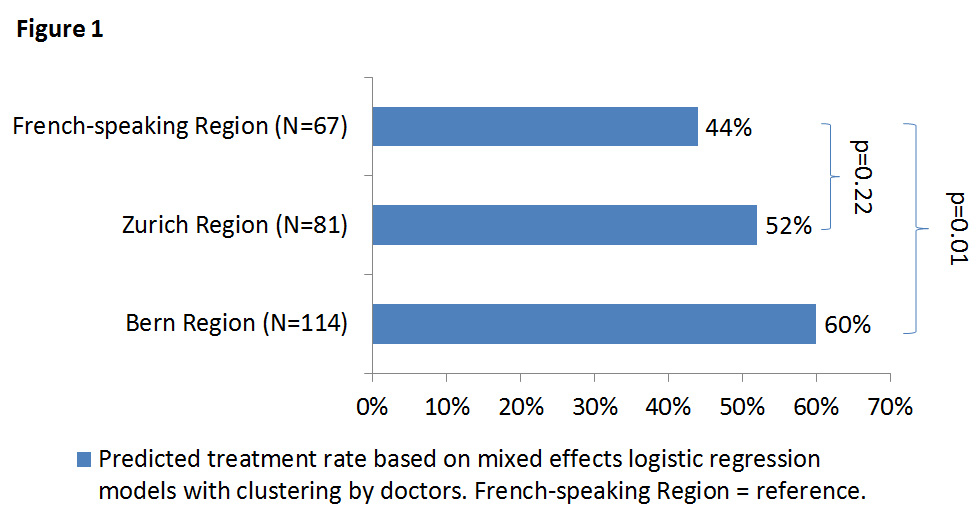
Figure 1
Variation in general practitioners’ decision to start treatment stratified by region. p-values for the difference between the French-speaking region (reference) and the Zurich or Bern Region, respectively.
DOI: https://doi.org/10.4414/smw.2015.14156
The prevalence of subclinical hypothyroidism, which is defined as high thyroid stimulating hormone (TSH) levels with free thyroxin (fT4) concentrations within the reference range [1], increases with age and ranges from 3% to 18% in the adult population, with a higher prevalence in women than men [2, 3]. Subclinical hypothyroidism has been associated with an increased risk of coronary heart disease events, heart failure and cardiovascular death [4, 5]. Despite being a common disorder, evidence on the risks and benefits of screening and treatment is still controversial [6]. A Cochrane review including 350 subclinically hypothyroid patients from 12 trials with a follow-up time between 6 and 14 months has concluded that levothyroxine replacement might improve lipid profiles and left ventricular function, but that evidence from adequately powered randomised controlled trials with longer follow-up durations was needed in order to assess the impact of treatment on cardiovascular events [7]. Risks of levothyroxine overtreatment and consecutive subclinical hyperthyroidism include an increased risk of atrial fibrillation, heart failure events and bone loss [5, 8, 9].
A recent international survey that we performed with a similar research group has shown large national variations in strategies for treatment of elderly patients with subclinical hypothyroidism among general practitioners (GPs) from different countries [10], reflecting the current lack of an international consensus concerning the management of these patients and the wide variations in guideline recommendations from different medical societies and across countries [11–14]. In Switzerland, the Swiss Society of Endocrinology and Diabetes has published guidelines on the treatment of subclinical hypothyroidism [13], but no specific national guidelines for primary care exist. Given this international variation in the management of elderly patients with subclinical hypothyroidism, we aimed to assess whether there were also regional variations in treatment strategies within one country among Swiss GPs in relation to different Swiss regions and patient characteristics.
We sent an online survey to Swiss GPs, presenting eight fictional clinical cases involving elderly female patients with subclinical hypothyroidism (appendix). The survey was developed using NetQuestionnaire [15] as part of an international survey to assess variations in treatment strategies of elderly patients with subclinical hypothyroidism among GPs from different countries [10]. For Switzerland, we further aimed to assess the variation in treatment strategies among Swiss GPs depending on different Swiss regions. The fictional patients all reported nonspecific fatigue and had a normal body mass index, but varied in age (70 years vs 85 years), vitality status (vital vs vulnerable) and TSH levels (6 mIU/l vs 15 mIU/l). In all cases fT4 concentrations were within the reference range. The cases are described in appendix table 1. After each case description, the GPs were asked the following questions concerning treatment strategy: (1) would you treat this patient with thyroxine? (2) if yes, what would you recommended as initiation dose? Furthermore, the GPs were asked to state whether their treatment strategy would change if the patient were a man instead of a woman. We also collected the GP’s gender, the duration of professional experience as a GP and the percentage of registered elderly persons aged 65 years or older in their practice. Finally, the GPs were asked to indicate the time since their last diagnosis of subclinical hypothyroidism in a patient aged ≥65 years, and the last time they had started thyroxine replacement in an elderly patient with subclinical hypothyroidism.
The survey, which was first developed in English, was translated and validated by several authors including German and French native speakers. German and French versions of the survey were sent to regional GP institutes in Geneva, Lausanne, Bern and Zurich, and the institute coordinators circulated an Internet link containing the questionnaire to all GPs participating in teaching or other activities related to the institutes within their region between April and September 2012, with a reminder sent out 2 weeks later. GPs affiliated with the institutes in Geneva and Lausanne were pooled to represent the French-speaking region of Switzerland; their anonymised answers had the same site code. Approval from the ethics committees was exempted since the survey, which treated only fictional patients, qualified as a peer-audit.
Questionnaires with at least one answer to Case 1 provided by the GP were considered for analysis. Differences in baseline GP characteristics by region were compared using chi-square tests. The tendency of GPs to initiate treatment and levothyroxine starting doses were compared between GPs from different Swiss regions. GPs were divided into three different regions based on their affiliation with the regional GP institutes: Bern region, Zurich region and the French-speaking region (including the affiliations to the GP institutes of Lausanne and Geneva). The probability of the GPs starting treatment was analysed using mixed effects logistic regression models with GP as a random effect. The models’ predicted marginal probabilities of initiating treatment in each region were presented. For comparison between the different regions, first an unadjusted model was used, using the region as a fixed covariate. In a second step, we adjusted for GP characteristics by adding the GP’s gender and experience as additional fixed variables. To test for a trend of increasing experience we included this variable as a continuous fixed effect, where a one unit increase represented 5 years of experience. We further analysed the probability of the GPs initiating treatment in the subgroup of patients with a TSH of 6 mIU/l, including only cases 1, 2, 5, and 6. For those who indicated that they would start treatment, the suggested initial levothyroxine dose was compared between regions using a mixed effects linear regression and restricted maximum likelihood (REML) estimation. Nine GPs were excluded from this analysis because of unrealistic starting doses, such as 1 µg or 2 µg.
Differences in treatment strategies depending on patient characteristics (age, vitality status and TSH concentrations) were calculated with separate odds ratios (ORs) for each combination of cases that only differed with respect to that specific characteristic within each Swiss region. Random-effects models based on the variance model by DerSimonian and Laird [16] were used to calculate a pooled estimate of the ORs of the different comparisons for each Swiss region.
Analysis was done using Stata version 13.1 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
| Table 1:Characteristics of the general practitioners who participated in the survey. | |||||
| Characteristic | Total | Bern region | Zurich region | French-speaking region | p-value |
| n = 262 | n = 114 | n = 81 | n = 67 | ||
| Men | 213 (81%) | 100 (88%) | 64 (79%) | 49 (73%) | 0.04 |
| More than 15 years of clinical experience | 168 (64%) | 73 (64%) | 47 (58%) | 48 (72%) | 0.23 |
| >30% patients in the practice aged ≥65 years | 114 (44%) | 56 (49%) | 29 (36%) | 29 (43%) | 0.18 |
| Diagnosis of subclinical hypothyroidism in a patient <1 year ago | 246 (94%) | 110 (96%) | 75 (93%) | 61 (91%) | 0.28 |
| Started thyroxine treatment in a patient <1 year ago | 196 (75%) | 88 (77%) | 61 (75%) | 47 (70%) | 0.57 |
| Note: Data are presented as n (%); p- values were obtained by chi-squared tests. Adapted from [10]. | |||||
| Table 2:Mixed effects logistic regression for the probability of providing treatment. | ||||
| Variable | GPs (n) | Treatment rate | OR (95% CI) | p-value |
| Unadjusted model | ||||
| French-speaking region | 67 | 44% | Reference | |
| Zurich region | 81 | 52% | 1.40 (0.82–2.39) | 0.22 |
| Bern region | 114 | 60% | 1.92 (1.16–3.16) | 0.01 |
| Adjusted model* | ||||
| French-speaking region | 45% | Reference | ||
| Zurich region | 51% | 1.30 (0.76–2.22) | 0.34 | |
| Bern region | 59% | 1.80 (1.08–2.98) | 0.02 | |
| GP gender (female) | 49 | 0.84 (0.48–1.44) | 0.519 | |
| Years of clinical practice <5 years | 13 | Reference | 0.216 | |
| 5–10 years | 35 | 0.82 (0.29–2.30) | ||
| 11–15 years | 46 | 1.31 (0.48–3.56) | ||
| 16–20 years | 47 | 0.90 (0.33–2.47) | ||
| 21–25 years | 42 | 1.37 (0.49–3.82) | ||
| >25 years | 79 | 0.69 (0.26–1.82) | ||
| Trend per 5 years’ experience | 0.94 (0.82–1.07) | 0.354 | ||
| Including only patients with a TSH of 6 mU/l | ||||
| Unadjusted model | ||||
| French-speaking region | 67 | 7% | Reference | |
| Zurich region | 81 | 7% | 1.01 (0.33–3.13) | 0.98 |
| Bern region | 114 | 16% | 2.36 (0.83–6.74) | 0.11 |
| Adjusted model* | ||||
| French-speaking region | 8% | Reference | ||
| Zurich region | 8% | 1.03 (0.32–3.24) | 0.97 | |
| Bern region | 17% | 2.49 (0.85–7.31) | 0.10 | |
| GPs’ decisions to treat or not to treat were the binary outcomes. GP ID was included as a random effect to control for within GP correlation. CI = confidence interval; GP = general practitioner; OR = odds ratio; *Adjusted for GP’s gender and year’s of experience | ||||
Among 1,068 GPs who were contacted, a total of 262 GPs responded to the survey (Bern region n = 114, Zurich region n = 81, French-speaking region n = 67), with an overall response rate of 25% (appendix table 2). Overall, 235 of all respondents (89.7%) answered to all eight cases, whereas 27 participants responded to at least one, but not all cases. The characteristics of the GPs who returned the questionnaire are presented in table 1, with slightly more male GPs participating in Bern. In total, 44% of the respondents indicated that more than 30% of the patients registered in their practice were aged 65 years or older. Within the past year, the vast majority of the GPs (94%) had diagnosed subclinical hypothyroidism in a patient, and 75% of the GPs indicated that they had initiated thyroxine treatment in an elderly patient with subclinical hypothyroidism.
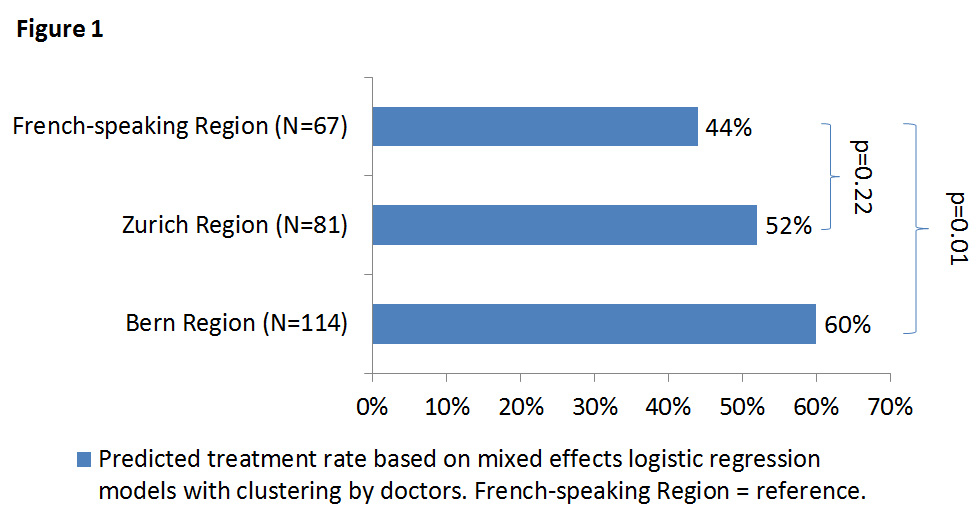
Figure 1
Variation in general practitioners’ decision to start treatment stratified by region. p-values for the difference between the French-speaking region (reference) and the Zurich or Bern Region, respectively.
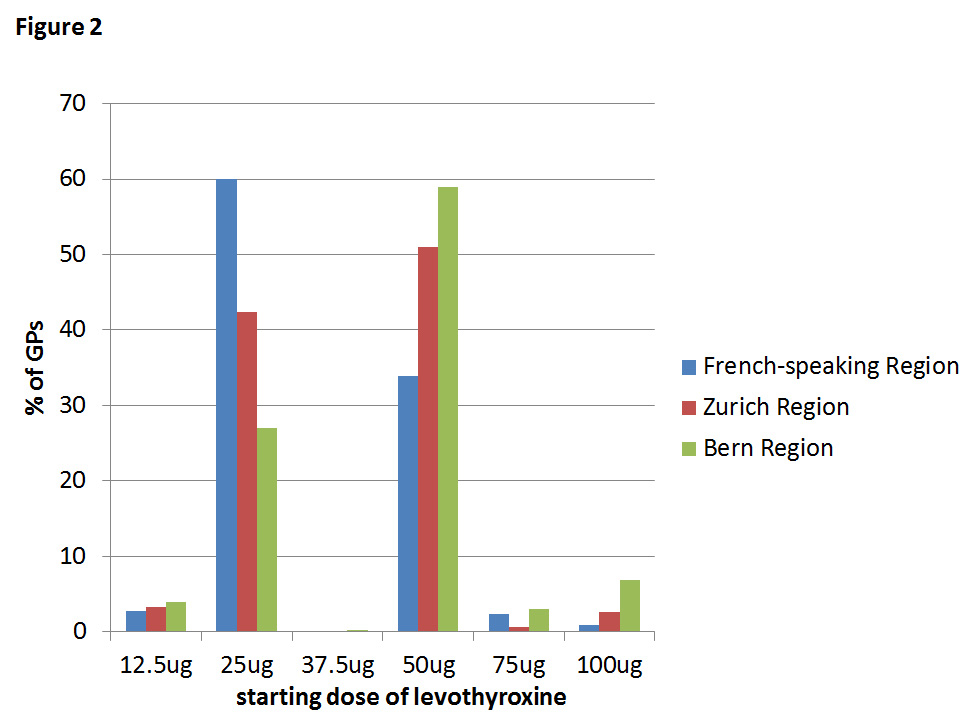
Figure 2
Starting dose of levothyroxine chosen by general practitioners according to region.
The GPs’ inclination to initiate treatment differed significantly between regions (p = 0.036), with GPs from the Bern region being more inclined to initiate thyroxine treatment with a predicted treatment rate of 60% compared with GPs from the Zurich region (52%) or the French-speaking region (44%, fig. 1). This resulted in a significantly higher odds of thyroxine use in the Bern region (p = 0.01) compared with the French-speaking region, also after adjustment for GP’s gender and years of clinical experience (table 2). The probability of a female GP initiating thyroxine treatment did not differ from that of male doctors. The number of years of clinical experience was not significantly associated with treatment rate. In the subgroup of patients with a TSH of 6 mIU/l, the probability of starting treatment was increased in GPs from the Bern region with a treatment rate of 16% compared with those from the Zurich and French-speaking regions (treatment rates 7%), although the difference was not statistically significant (p = 0.10–0.11).
Thyroxine starting doses varied from 25 µg to 100 µg and differed significantly across regions (p <0.01, table 3). GPs in the Bern region implemented the highest starting dose (predicted mean starting dose 45 µg, p <0.01) compared with the French-speaking region (36 µg), whereas the mean starting dose implemented by GPs in the Zurich region was 39 µg. The starting doses chosen by the GPs according to the different regions pooled for all cases are shown in figure 2, and the distribution of the starting doses for each case is illustrated in appendix figure 2.
Swiss GPs were more reluctant to initiate treatment in 85-year-old than in 70-year-old women (pooled OR 0.77, 95% confidence interval [CI] 0.63–0.94, Appendix fig. 2), and women with a TSH of 15 mU/l were treated more often than those with a TSH of 6 mU/l (pooled OR 8.71, 95% CI 6.21–12.20). Vitality status of the patient did not influence the treatment strategy. These results did not significantly differ across regions.
The majority of the GPs in all regions stated that they would not change their treatment strategy if the patient were male rather than female (percentage ‘no change’: Zurich region 98.6%, Bern region 95.3%, French-speaking region 94.7%, p = 0.46; appendix table 3).
| Table 3: Initial thyroxine dose suggested by doctors who would initiate treatment. | ||||
| Variable | GPs (n) | Predicted starting dose in µg (95% CI) | Coef. (95% CI) | p-value |
| Unadjusted model | ||||
| French-speaking region | 64 | 36.1 (32.2‒40.0) | Reference | |
| Zurich region | 77 | 39.4 (36.1‒42.8) | 3.3 (–1.8 ‒ 8.5) | 0.20 |
| Bern region | 112 | 44.6 (41.2‒48.1) | 8.5 (3.3‒13.8) | <0.01 |
| Adjusted for gender and years of experience | ||||
| French-speaking region | 36.0 (31.6‒40.5) | Reference | ||
| Zurich region | 39.3 (35.4‒43.2) | 3.3 (–2.6 ‒ 9.2) | 0.28 | |
| Bern region | 44.7 (41.5‒47.8) | 8.7 (3.2‒14.1) | <0.01 | |
| Analysis by mixed effects linear regression including GP ID as a random effect. Predicted dose are the predicted marginal means, adjusted or unadjusted, for each site. The p-value for a general difference between the three regions was <0.01 for the unadjusted and <0.01 for the adjusted model. Coefficients represent the difference from the reference level. CI = confidence interval; Coef. = coefficient; GP = general practitioner | ||||
Treatment strategies of elderly patients with subclinical hypothyroidism vary considerably throughout the different Swiss regions in terms of initiation of thyroxine treatment and starting dose, with GPs in the Bern region treating more often and with higher doses, whereas GPs in the Zurich and French-speaking regions were less inclined to treat and implemented lower starting doses. Starting doses varied from 25 to 100 µg, whereas the Swiss Society for Endocrinology and Diabetes recommends a thyroxine starting dose of 25 µg in patients older than 50 years [13], like those in our survey. GPs were more inclined to start treatment in patients with higher TSH levels and younger age.
Few previous studies have assessed treatment strategies for subclinical hypothyroidism, and none has highlighted regional differences within a single country. Our previous international survey on the treatment of subclinical hypothyroidism in elderly patients found large variations in GP treatment strategies across different countries, with treatment rates varying between 34% in the Netherlands and 73% in Germany [10]. In line with our results, the international survey showed that younger age and higher TSH levels were positively associated with the decision of the GPs to start treatment [10]. In a case-based survey in the United States, the management of patients with overt and subclinical hypothyroidism differed significantly between primary care physicians and members of the American Thyroid Association [17]. Treatment decisions in individuals with subclinical hypothyroidism varied according to different clinical factors among international members of different American endocrine societies as shown in a recent survey [18]. Sixty-two percent of the 802 respondents indicated that they would initiate treatment in the presence of positive thyroid peroxidase antibodies, 47% would start treatment in a patient with goitre and 26% in those with known cardiovascular disease. These results probably reflect the inconsistent recommendations from different national guidelines and the lack of an international consensus as to whether or not subclinical hypothyroidism should be treated [1, 7, 11]. The Swiss Society for Endocrinology and Diabetes guidelines [13] recommend basing the decision to initiate treatment on a risk assessment, taking into consideration a TSH value >10 mIU/l, prevalent goitre, thyroid-peroxidase antibodies, cardiovascular risk factors or coronary heart disease, clinical symptoms, ovulary dysfunction, and pregnancy. In the presence of any of these risk factors, the initiation of thyroxine replacement is recommended with a starting dose of 25 µg in patients older than 50 years or those with known coronary heart disease; in all other patients, thyroxine treatment can be started at a dose of 50 to 75 µg [13]. In our study, the GPs implemented higher starting doses than recommended for elderly patients in the Swiss guidelines. The European Thyroid Association published similar recommendations with thyroxine starting doses of 25–50 µg in elderly persons with subclinical hypothyroidism [19], and the guidelines of the American Association of Clinical Endocrinologists and the American Thyroid Association recommend a thyroxine starting dose of 50 µg in individuals older than 50–60 years, which should be reduced to 12.5–25 µg in those with concomitant coronary heart disease [20].
Our study has some limitations. First, the overall response rate was 25%, limiting the generalisability of our results. However, the response rate in our survey was similar to the response rate seen in a previous survey on subclinical hypothyroidism among American primary care physicians [17], and the problem of achieving high response rates in GP surveys has been recognised [21]. Participation rates differed across regions, possibly introducing nonresponse bias, although this risk seems to be lower in physician surveys than in surveys performed among the general population [22]. We did not have a clear explanation for the different participation rates across regions, but potential explanations might be the number of ongoing studies taking place at a similar time or differences in the degree of involvement of GPs with their regional institutes. As the survey presented only hypothetical cases with a short case description, comparability to real-life cases might be limited. Another limitation is the restricted choice of possible answers, not allowing the option of watchful waiting with monitoring of TSH levels to be chosen [6, 23]. Furthermore, we were not able to adjust for other possible confounding factors such as the willingness of the patient to receive treatment or the GP’s affiliation to primary care networks.
Our results likely reflect the current uncertainties regarding the benefits of thyroxine treatment in elderly patients with subclinical hypothyroidism, not only across countries but also across different regions of the same country, where GPs work with the same national guidelines [13]. Possible explanations are recommendations by local experts within training rounds or different teaching about managing subclinical hypothyroidism. Because of the lack of specific primary care guidelines in Switzerland, local GP networks and associations have created their own “unofficial” guidelines [24], which are often discussed in quality circles, with a known effect on prescribing patterns [25]. In contrast to the national guidelines, these standards are created by physicians associated with these specific networks. It has been shown that treatment strategies from Swiss GPs working in networks differed from those of GPs in usual primary care [26]. Therefore, the proportion of GPs associated with specific networks could explain some regional differences, but these data were not collected in the present survey. Furthermore, GPs might follow different guidelines, such as those from the American Thyroid Association [20] and the European Thyroid Association [19], that recommend higher starting doses in nonelderly patients than the Swiss Society for Endocrinology and Diabetes guidelines and may have higher levels of dissemination among GPs in some regions. Another possible explanation for the regional differences despite uniform national guidelines might be a limited adherence to evidence-based treatment guidelines in primary care [27]. Data from clinical trials assessing the benefits and risks of treatment of subclinical hypothyroidism are needed in order to obtain evidence-based recommendations for guideline development and inform clinical decisions. The TRUST trial (Thyroid hormone Replacement for Untreated older adults with Subclinical hypothyroidism: a randomized placebo-controlled Trial) is a large multinational multicentre placebo-controlled randomised clinical trial currently ongoing in four European countries including Switzerland. This trial aims to investigate the benefits and risks of thyroxine replacement among elderly persons with subclinical hypothyroidism [28]. An additional substudy in the oldest old is currently underway in the Netherlands as the IEMO 80-Plus Thyroid Trial [23, 29] with recruitment of individuals aged 80 years and older.
In conclusion, our findings show that there are important variations in treatment strategies of elderly patients with subclinical hypothyroidism throughout the different Swiss regions, including application of higher starting doses than recommended in the Swiss guidelines. These variations reflect the current uncertainty regarding the benefits of treatment and emphasise the importance of ongoing clinical trials for obtaining strong evidence-based treatment recommendations.
This survey was previously published in [10].
Survey
1. What is your gender?
O Male
O Female
2. How many years have you been practicing as a GP?
O <5
O 5-10
O 11-15
O 16-20
O 21–25
O >25
3. What percentage of patients in your practice is 65 years or above?
O <10
O 10–20
O 20–30
O >30
4. When did you last diagnose a patient over 65 with subclinical hypothyroidism in your practice?
O Less than 1 week ago
O Less than 1 month ago
O Less than 1 year ago
O Less than 3 years ago
O More than 3 years ago
5. When did you last start thyroxin treatment in a patient over 65 with subclinical hypothyroidism?
O Less than 1 week ago
O Less than 1 month ago
O Less than 1 year ago
O Less than 3 years ago
O More than 3 years ago
O Never
In each case we discuss an older woman of average height and weight, presenting with aspecifc complaints of fatigue. You found sufficient reason in her complaints to perform a blood test. The test showed subclinical hypothyroidism.
6. Case 1.
Female, 70 years old, vital
Elevated TSH: 6 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 6c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
7. Case 2.
Female, 70 years old, vulnerable.
Elevated TSH: 6 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 7c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
8. Case 3.
Female, 70 years old, vital.
Elevated TSH: 15 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 8c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
9. Case 4.
Female, 70 years old, vulnerable.
Elevated TSH: 15 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 9c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
10. Case 5.
Female, 85 years old, vital
Elevated TSH: 6 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 10c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
11. Case 6.
Female, 85 years old, vulnerable
Elevated TSH: 6 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 11c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
12. Case 7.
Female, 85 years old, vital.
Elevated TSH: 15 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 12c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
13. Case 8.
Female, 85 years old, vulnerable.
Elevated TSH: 15 mU/L (reference range 0.5–4.4 mU/L).
Free T4 is within the reference range (13–25 pMol/L).
a) Would you start thyroxin treatment?
O Yes
O No → go to question 13c
b) To start treatment, how much thyroxin (mcg) would you prescribe?
c) Explanation (optional)
14a) Would you act any differently if the patient was an older male of average weight and normal BMI instead of a woman?
O Yes, go to 14b
O No, go to 15
b) Explanation
15. Would you like to be informed about the results of this study?
O Yes, à email address
O No
Comments:
Starting dose of levothyroxine chosen by general practitioners for each case according to region.
| Appendix table 1: The eight clinical cases. | ||||
| Case | Gender | Age (years) | TSH (mIU/l) | Vitality status |
| 1 | Woman | 70 | 6 | Vital |
| 2 | Woman | 70 | 6 | Vulnerable |
| 3 | Woman | 70 | 15 | Vital |
| 4 | Woman | 70 | 15 | Vulnerable |
| 5 | Woman | 85 | 6 | Vital |
| 6 | Woman | 85 | 6 | Vulnerable |
| 7 | Woman | 85 | 15 | Vital |
| 8 | Woman | 85 | 15 | Vulnerable |
| All cases presented in the survey involved an older female patient with a normal free thyroxine level, a normal body mass index and nonspecific symptoms resulting in fatigue. TSH = thyroid-stimulating hormone. Adapted from [10] | ||||
| Appendix table 2: Participating Swiss regional general practitioner (GP) institutes. | ||||
| Region | Regional GP institute | Number of GPs invited to participate | Number of GPs who participated | Response Rate |
| Zurich region | Institute of General Practice and Health Services Research, University of Zurich | 478 | 81 | 17% |
| Bern region | Bern Institute of General Practice, University of Bern | 260 | 114 | 44% |
| French-speaking region | Institute of General Medicine, University of Lausanne* | 330 | 67 | 20% |
| Department of Community Medicine and Primary Care, Geneva University Hospitals* | ||||
| Total | 1,068 | 262 | 25% | |
| * 18 GPs could not be allocated to Geneva or Lausanne owing to insufficient data (data collected together), and were excluded from this subgroup analysis. | ||||
| Appendix table 3: Would treatment strategy change for a male patient? | ||||
| Site | Total | Yes | No | p-p-value |
| Zurich region | 72 | 1 (1.4%) | 71 (98.6%) | 0.46 |
| Bern region | 106 | 5 (4.7%) | 101 (95.3%) | |
| French-speaking region | 57 | 3 (5.3%) | 54 (94.7%) | |
| Data are presented as n (%).The p-value was derived using Fisher's exact test. Data are missing for 27 general practitioners (9 from Bern region, 8 from Zurich region, 10 from French-speaking region). | ||||
Disclosures: This study was supported by a grant from the Swiss National Science Foundation (SNSF 320030-150025) and partially supported by a grant from the Swiss Heart Foundation (all to Prof. N. Rodondi), and the TRUST study (by HEALTH-FP7-2011 grant agreement 278148-2) and IEMO Thyroid Trial (Dutch Ministry of Health and Welfare, ZonMw627001001).
1 Helfand M. Screening for subclinical thyroid dysfunction in nonpregnant adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Internal Med. 2004;140(2):128–41.
2 Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000;160(4):526–34.
3 Hollowell JG, Staehling NW, Flanders WD, Hannon WH, Gunter EW, Spencer CA, et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). J Clin Endocrinol Metab. 2002;87(2):489–99.
4 Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010;304(12):1365-74. Epub 2010/09/23. doi: 10.1001/jama.2010.1361.
5 Gencer B, Collet TH, Virgini V, Bauer DC, Gussekloo J, Cappola AR, et al. Subclinical thyroid dysfunction and the risk of heart failure events: an individual participant data analysis from 6 prospective cohorts. Circulation. 2012;126(9):1040–9.
6 Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, Cobin RH, et al. Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA.2004;291(2):228–38.
7 Villar HC, Saconato H, Valente O, Atallah AN. Thyroid hormone replacement for subclinical hypothyroidism. The Cochrane database of systematic reviews. 2007(3):CD003419.
8 Collet TH, Gussekloo J, Bauer DC, den Elzen WP, Cappola AR, Balmer P, et al. Subclinical hyperthyroidism and the risk of coronary heart disease and mortality. Arch Intern Med. 2012;172(10):799–809.
9 Wirth CD, Blum MR, da Costa BR, Baumgartner C, Collet TH, Medici M, et al. Subclinical thyroid dysfunction and the risk for fractures: a systematic review and meta-analysis. Ann Intern Med. 2014;161(3):189–99.
10 den Elzen WP, Lefebre-van de Fliert AA, Virgini V, Mooijaart SP, Frey P, Kearney PM, et al. International variation in GP treatment strategies for subclinical hypothyroidism in older adults: a case-based survey. Br J Gen Pract. 2015;65(631):e121–32.
11 Gharib H, Tuttle RM, Baskin HJ, Fish LH, Singer PA, McDermott MT. Subclinical thyroid dysfunction: a joint statement on management from the American Association of Clinical Endocrinologists, the American Thyroid Association, and the Endocrine Society. J Clin Endocrinol Metab. 2005;90(1):581–5; discussion 6–7.
12 Vanderpump MP, Ahlquist JA, Franklyn JA, Clayton RN. Consensus statement for good practice and audit measures in the management of hypothyroidism and hyperthyroidism. The Research Unit of the Royal College of Physicians of London, the Endocrinology and Diabetes Committee of the Royal College of Physicians of London, and the Society for Endocrinology. BMJ. 1996;313(7056):539–44.
13 Müller B. «Subklinische» Hypo- und Hyperthyreose. Schweizerische Gesellschaft für Endokrinologie und Diabetologie. http://www.sgedssed.ch/fileadmin/files/dokumente/EDM_Key_Slides_2010-2011/SGED_Subklinische_Hypo_Hyperthyresose.pdf2010-2011. German.
14 American Academy of Family Physicians. Periodic health examination: Summary of AAFP policy recommendations and age charts, revision 4.0. American Academy of Family Physicians, 2000.
15 NETQ. http://wwwnetq-enquetenl/nl.
16 DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
17 McDermott MT, Haugen BR, Lezotte DC, Seggelke S, Ridgway EC. Management practices among primary care physicians and thyroid specialists in the care of hypothyroid patients. Thyroid. 2001;11(8):757–64.
18 Burch HB, Burman KD, Cooper DS, Hennessey JV. A 2013 survey of clinical practice patterns in the management of primary hypothyroidism. J Clin Endocrinol Metab. 2014;99(6):2077–85.
19 Pearce SH, Brabant G, Duntas LH, Monzani F, Peeters RP, Razvi S, et al. 2013 ETA Guideline: Management of Subclinical Hypothyroidism. Eur Thyroid J. 2013;2(4):215–28.
20 Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012;22(12):1200–35.
21 McAvoy BR, Kaner EF. General practice postal surveys: a questionnaire too far? BMJ. 1996;313(7059):732–3; discussion 3–4.
22 Kellerman SE, Herold J. Physician Response to Surveys. A Review of the Literature. Am J Prev Med. 2001;20(1):61–7.
23 Baumgartner C, Blum MR, Rodondi N. Subclinical hypothyroidism: summary of evidence in 2014. Swiss Med Wkly. 2014;144:w14058.
24 mediX. Guideline Schilddrüsenerkrankungen. http://www.medix.ch/wissen/guidelines/stoffwechselkrankheiten/schilddruesenerkrankungen.html. 2011. German.
25 Wensing M, Broge B, Riens B, Kaufmann-Kolle P, Akkermans R, Grol R, et al. Quality circles to improve prescribing of primary care physicians. Three comparative studies. Pharmacoepidemiol Drug Saf. 2009;18(9):763–9.
26 Frei A, Senn O, Huber F, Vecellio M, Steurer J, Woitzek K, et al. Congruency of diabetes care with the Chronic Care Model in different Swiss health care organisations from the patients’ perspective: a cross sectional study. Swiss Med Wkly. 2014;10(144).
27 Cranney M, Warren E, Barton S, Gardner K, Walley T. Why do GPs not implement evidence-based guidelines? A descriptive study. Fam Pract. 2001;18(4):359–63.
28 Rodondi N, Bauer DC. Subclinical hypothyroidism and cardiovascular risk: how to end the controversy. J Clin Endocrinol Metab. 2013;98(6):2267–9.
29 Mooijaart SP. Letter regarding the Paper by Pearce et al. Entitled “2013 ETA Guideline: Management of Subclinical Hypothyroidism”. Eur Thyroid J. 2014;3(2):141–2.