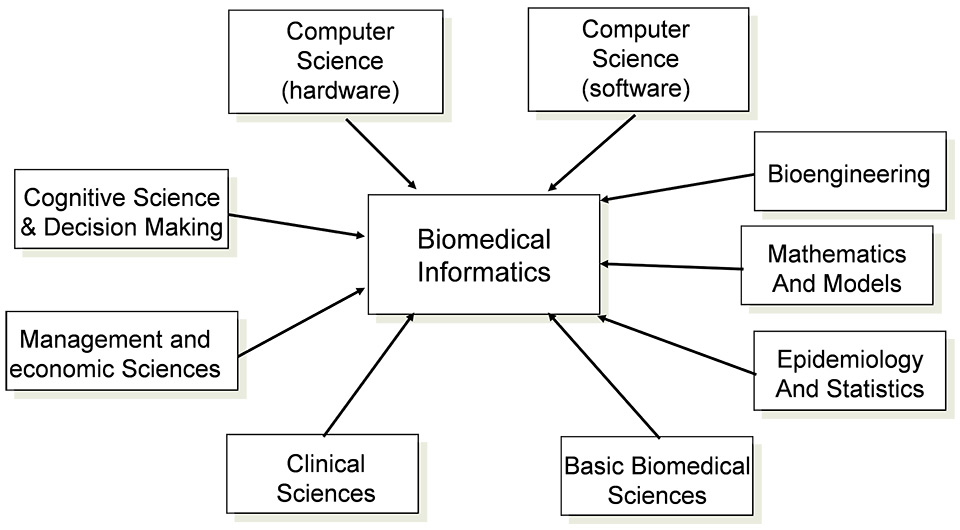
Figure 1
Biomedical informatics is a field of science at the intersection of other domains and is interdisciplinary by essence [1].
DOI: https://doi.org/10.4414/smw.2015.14173
As of 2011, the American Medical Informatics Association has defined the field “Biomedical Informatics” as the interdisciplinary field that studies and pursues the effective uses of biomedical data, information, and knowledge for scientific inquiry, problem solving, and decision making, motivated by efforts to improve human health [1, 2].
Biomedical informatics covers a broad spectrum of disciplines, from bioinformatics to clinical and public health informatics, and spans the spectrum from the molecular to the population level in health and biomedicine (fig. 1). Recognition of biomedical informatics as a core science in Switzerland, as is the case in numerous countries such as the USA, is of highest importance, to foster education, research and translational research. It is becoming even more important as eHealth develops into a major stream in the care system. Thus, building capacity and increasing numbers of knowledgeable professionals is of importance. A clear definition is a tool of choice in promoting the discipline as a career focus, and providing guidance to students and faculty designing graduate-level academic biomedical informatics programmes.
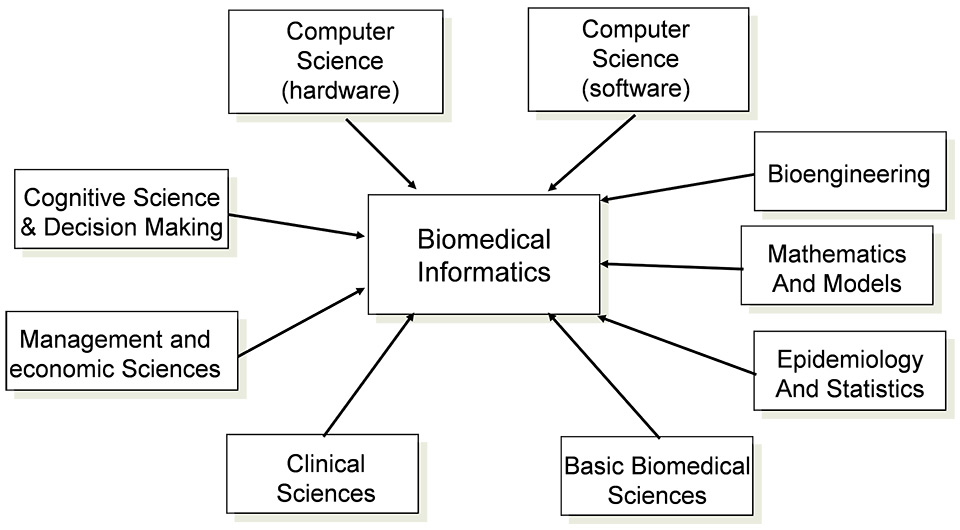
Figure 1
Biomedical informatics is a field of science at the intersection of other domains and is interdisciplinary by essence [1].
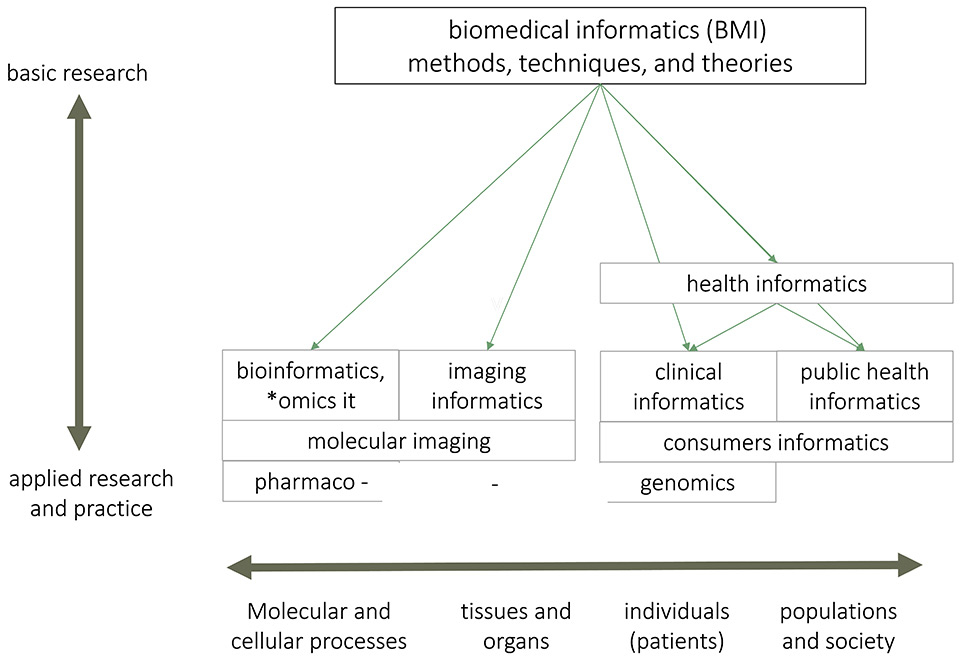
Figure 2
Biomedical informatics and its areas of application and practice.
This figure, adapted from the International Medical Informatics Association publication on the definition of biomedical informatics [3], illustrates the umbrella relation between biomedical informatics and other related fields applying information sciences and technologies to health.
Figure 3
Evolution of publications about “biomedical informatics” compared with “genetic therapy” according to Pubmed.
This figure illustrates the evolution of publications indexed in Pubmed with the MeSH term “medical informatics [MeSH]” (left axis, full line red) and “genetic therapy [MeSH]” (right axis, dotted line grey) between 1963 and 2013 as of 3 March 2015. The years 2014 and 2015 are left out to avoid bias of publication and indexing delays.
Biomedical informatics is pervasive, covering research, development and evaluation activities around reasoning, building models, simulations, experiments, and translation of data, information, knowledge and algorithm-driven approaches (fig. 2). It ranges from molecules to individuals to populations, from biological to social systems, bridging basic and clinical research and practice, and the healthcare enterprise.
Biomedical informatics develops, studies and applies theories, methods and processes for the generation, storage, retrieval, use, management and sharing of data, information and knowledge in the field of health. It covers genomics, phenotypes, and environmental, behavioural and lifestyle data.
Biomedical informatics builds on and contributes to computer, telecommunication and information sciences and technologies, emphasising their application in biomedicine, evaluating impacts, and assessing risks, challenges, and benefits.
Biomedical informatics builds upon social and behavioural sciences to design and evaluate technical solutions, policies and the evolution of economic, ethical, social, educational, and organisational systems.
Biomedical informatics is the major science dealing with electronic patient records, including clinical services, decision support, therapy and management. It is also the discipline dealing with secondary usage of data for medical and translational research amongst others, using multimodal sources of data, for example in pharmaceutical research, bioinformatics, biobanking and biomolecular imaging [4–7].
Biomedical informatics is developing rapidly, as illustrated by the fast increasing number of publications over time (see fig. 3). As of 23 February 2015, a search with the MeSH term “medical informatics” retrieved a total of 330,919 papers [8], compared with much lower cumulative numbers for other MeSH terms, e.g. 39,178 for “genetic therapy“ (fig. 3).
One important aspect of biomedical informatics is the very fast translational transfer into practice, strongly supported by public authorities in order to improve the safety, efficiency and transparency of the healthcare system. This results in increasing importance of clinical informatics in most countries, for personal health records, eHealth, computerised patient records, clinical decision support, etc.
Clinical informatics has formally been recognised as a medical subspecialty by the American Board of Medical Specialty since 2011.
A new federal law about the shared electronic patient record is currently being discussed at the political level. This law is promoting the use of electronic health services, eHealth and, in particular, the roll out of electronic patient records as an essential element in the strategy of the Federal Council entitled “Health2020”. In this context, the Swiss Society for Medical Informatics has been recently commissioned by the eHealth-Suisse coordination organisation to draw up a “Vision eHealth 2025” [9].
With the electronic patient record, there are great expectations of improvement in patient safety and increase in the efficiency of the healthcare system [10–13], while empowering patients. In order to achieve these objectives on a wide scale, capacity building, leadership awareness and serious incentives are necessary to overcome numerous resistances [14]. Within the US American Recovery and Reinvestment Act of 2009, approximately $160 billion was distributed to fund programmes to improve and preserve healthcare, health information technology, child and community services, scientific research and facilities, and community health and prevention initiatives [15]. There is a very strong Medicare/Medicaid Electronic Health Record (EHR) Incentive and Penalty Program that provides a two-step approach to improving EHR adoption: since 2009, $17 billion support incentives for physicians for adoption of the EHR with incentive payments totalling up to $44,000 per physician over 5 years for Medicare and up to $63,750 per physician over 6 years. On the penalty side, starting 1 January 2015, Medicare reimbursement rates will be reduced by 1% for physicians who do not meet this requirement. Only users of certified software, properly used and that meets the “meaningful use” requirements, will be entitled to the positive incentive [16–18]. There is a publicly available list of certified EHRs [19]. However, the programme presents many challenges ‒ economic, outcome-related, ethical, technical and scientific ‒ as described in a white paper from the American Medical Informatics Association, and requiring true expertise in the field [20]. There is no such incentive in Switzerland now, but the situation will start to change with a new federal law on the electronic patient record that should be enacted in 2017 [21]. This law will introduce mandatory use of the EHR for inpatients and some limited financial incentives.
Switzerland is facing an acute lack of both information technology scientists and physicians, cumulating in a severe lack of professionals in all the disciplines of biomedical informatics. This situation should be taken seriously and a fast and strong answer must be given to limit the war for talent. The societal challenges of the healthcare system, as well as consumerist movements such as quantified-self, or citizen empowerment, the demographic challenges and the need for healthy aging, pervasive and supportive environments, not to speak of managed care, clinical research, etc. require great expertise in biomedical informatics.
Swiss academic positions in biomedical informatics exist only in Geneva, with two faculty positions, one for eHealth and Telemedicine, and the other for medical information sciences; and in Zürich in clinical informatics. A few new positions are being created or discussed, but this is still far below the demand and the need.
Although the situation is evolving positively in Switzerland, the pace of this evolution is too slow to accommodate the speed of growth in needs in biomedical informatics in almost all fields of clinical care and life sciences. Thus, we call for action according to the following pillars, based on promotion, incentives and recognition-
a) Education
Education for healthcare professionals should be fostered, by including some new objectives in their curricula, notably covering the topics of clinical documentation and semantic standards, decision support systems, process-driven care, secondary usage of data, including big data, and ethical aspects.
There should be specific educational paths in general biomedical informatics, and also in specific tracks such as medical decision support or massive data reuse, with classical training from bachelor to doctorate.
Continuing education and certificates of advanced education must be more widely available, as they are still marginal in Switzerland.
For all these tracks, a consensus should allow proposal of a common list of objectives and standard contents, in order to become aligned with international standards and be compatible with the Bologna Process. Several examples of such curricula are available from other countries and may serve as basis for Switzerland.
b) Research and development
In Switzerland a great deal of research related to biomedical informatics is going on, but with little synergy and cooperation. An umbrella organisation in the field would foster collaborative work. Recent activities, such as the Swiss-Japanese workshop in Tokyo about technology and healthy ageing, proved the excellence of Swiss research, but there was little cooperation between the groups. Some research funding schemes that promote collaboration, such as the Sinergia SNF framework, would improve mutual cooperation. In addition, incentive programmes for early adopters, such as the “meaningful use” initiative in the United States [17], could induce a significant difference in implementation of up-to-date solutions in clinical informatics in Swiss hospitals, including reuse of clinical data for research.
c) Faculty positions
In order to fulfil the bioinformatics needs, faculty positions have to be greatly increased in Switzerland, at both the fundamental and applied levels. For example, all university hospitals should have at least one faculty position in the field of clinical informatics.
The use of novel technologies in healthcare offers many opportunities. However, strengthening biomedical informatics does come with a price tag. Programmes for promoting research and development in this field should be established in Switzerland, focussing on electronic patient records and decision support, clinical big data, semantics and data interoperability, infrastructure to support clinical trials and translational medicine. In addition, promotion of education and training, including academic curricula for both physicians and computer scientists, is needed.
Disclosures: The authors have no competing interests, except that they are biased by trying to promote Biomedical Informatics by any means in Switzerland.
1 Definition of Biomedical Informatics [Internet]. American Medical Informatics Association. [accessed 2015 Feb 26]. Available from: http://www.amia.org/presentation/definition-biomedical-informatics
2 Kulikowski CA, Shortliffe EH, Currie LM, Elkin PL, Hunter LE, Johnson TR, et al. AMIA Board white paper: definition of biomedical informatics and specification of core competencies for graduate education in the discipline. J Am Med Inform Assoc. 2012;19(6):931–8.
3 Presentation about Biomedical Informatics [Internet]. American Medical Informatics Association. [accessed 2015 Feb 19]. Available from: http://www.amia.org/sites/amia.org/files/AMIA-definition-of-Biomedical-Informatics-update.ppt
4 Schneeweiss S. Learning from big health care data. N Engl J Med. 2014;370(23):2161–3.
5 Martin-Sanchez F, Verspoor K. Big data in medicine is driving big changes. Yearb Med Inform. 2014;9(1):14–20.
6 Koutkias V, Thiessard F. Big data – smart health strategies. Findings from the yearbook 2014 special theme. Yearb Med Inform. 2014;9(1):48–51.
7 Miriovsky BJ, Shulman LN, Abernethy AP. Importance of health information technology, electronic health records, and continuously aggregating data to comparative effectiveness research and learning health care. J Clin Oncol. 2012;30(34):4243–8.
8 MeSH Browser [Internet]. Bethesda (MD): National Library of Medicine (US). [accessed 2015 Feb 23]. Available from: http://www.ncbi.nlm.nih.gov/mesh/68008490 MeSH Unique ID: D008490
9 Vision paper “eHealth 2025” from the Swiss Society for Medical Informatics [Internet]. E-Health Suisse. Coordination Office Confederation-Cantons for ehealth in Switzerland. [accessed 2015 Mar 23]. Available from: http://www.e-health-suisse.ch/grundlagen/00086/index.html?lang=de
10 Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348(25):2526–34.
11 Jones SS, Rudin RS, Perry T, Shekelle PG. Health information technology: an updated systematic review with a focus on meaningful use. Ann Intern Med. 2014;160(1):48–54.
12 Vermeulen KM, van Doormaal JE, Zaal RJ, Mol PGM, Lenderink AW, Haaijer-Ruskamp FM, Kosterink JGW, van den Bemt PMLA. Cost-effectiveness of an electronic medication ordering system (CPOE/CDSS) in hospitalized patients. Int J Med Inf. 2014;83(8):572–80.
13 Radley DC, Wasserman MR, Olsho LE, Shoemaker SJ, Spranca MD, Bradshaw B. Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems. J Am Med Inform Assoc. 2013;20(3):470–6.
14 Shah NR, Seger AC, Seger DL, Fiskio JM, Kuperman GJ, Blumenfeld B, Recklet EG, Bates DW, Gandhi TK. Improving acceptance of computerized prescribing alerts in ambulatory care. J Am Med Inform Assoc JAMIA. 2006;13(1):5–11.
15 US Recovery Accountability and Transparency Board [Internet]. American Recovery and Reinvestment Act. [accessed 2015 Feb 3]. Available from: http://www.recovery.gov/Pages/default.aspx
16 Classen DC, Bates DW. Finding the meaning in meaningful use. N Engl J Med. 2011;365(9):855–8.
17 Medicare and Medicaid Electronic Health Records (EHR) Incentive Programs [Internet]. Centers for Medicare and Medicaid Services. [accessed 2015 Feb 3]. Available from: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms
18 Medicare/Medicaid EHR Incentive and Penalty Programs [Internet]. American Medical Association (AMA). [accessed 2015 Feb 3]. Available from: http://www.ama-assn.org/ama/pub/advocacy/topics/digital-health/medicare-medicaid-incentive-programs.page
19 Certified health IT product list [Internet]. The Office of the National Coordinator for health Information technology. [accessed 2015 Feb 3]. Available from: http://oncchpl.force.com
20 Re-examining the strategies needed to successfully adopt health IT [Internet]. American Medical Informatics Association (AMIA). [accessed 2015 Mar 3]. Available from: https://www.amia.org/sites/amia.org/files/EHR-White-Paper.pdf
21 Entwurf des Bundesgesetzes über das elektronische Patientendossier [Internet]. Federal Office of Public Health (FOPH). [accessed 2014 Nov 26]. Available from: http://www.bag.admin.ch/themen/gesundheitspolitik/10357/10360/index.html?lang=en
Authors’ contribution: CL & JB contributed equally to the text.