Sudden cardiac death in forensic medicine – Swiss recommendations for a multidisciplinary approach
DOI: https://doi.org/10.4414/smw.2015.14129
Matthias
Wilhelm, Stephan A
Bolliger, Christine
Bartsch, Siv
Fokstuen, Christoph
Gräni, Viktor
Martos, Argelia
Medeiros Domingo, Antonio
Osculati, Claudine
Rieubland, Sara
Sabatasso, Ardan M
Saguner, Christian
Schyma, Joelle
Tschui, Daniel
Wyler, Zahurul A.
Bhuiyan, Florence
Fellmann, Katarzyna
Michaud
Summary
Sudden cardiac death (SCD) is by definition unexpected and cardiac in nature. The investigation is almost invariably performed by a forensic pathologist. Under these circumstances the role of the forensic pathologist is twofold: (1.) to determine rapidly and efficiently the cause and manner of death and (2.) to initiate a multidisciplinary process in order to prevent further deaths in existing family members. If the death is determined to be due to “natural” causes the district attorney in charge often refuses further examinations. However, additional examinations, i.e. extensive histopathological investigations and/or molecular genetic analyses, are necessary in many cases to clarify the cause of death. The Swiss Society of Legal Medicine created a multidisciplinary working group together with clinical and molecular geneticists and cardiologists in the hope of harmonising the approach to investigate SCD. The aim of this paper is to close the gap between the Swiss recommendations for routine forensic post-mortem cardiac examination and clinical recommendations for genetic testing of inherited cardiac diseases; this is in order to optimise the diagnostic procedures and preventive measures for living family members.
The key points of the recommendations are (1.) the forensic autopsy procedure for all SCD victims under 40 years of age, (2.) the collection and storage of adequate samples for genetic testing, (3.) communication with the families, and (4.) a multidisciplinary approach including cardiogenetic counselling.
Introduction
Sudden cardiac death (SCD) is a major public health issue worldwide. The exact incidence of sudden death in the younger population remains unclear and the published incidences are generally thought to be underestimated [1–4]. No exact data exist for Switzerland concerning the incidence of SCD in the young or for the autopsy rate. The presumed values were recently published for the canton of Vaud by Hofer et al. [5]. According to this study, the presumed incidence of SCD in the young (aged 5–39 years) is 1.71/100,000 person-years (2.73 for men and 0.69 for women). However, it might be higher as not all possible cases of SCD (unexplained deaths, drowning, traffic accidents, etc.) are included. The autopsy rate of sudden deaths classified as “diseases of the circulatory system” was evaluated at 47.5% and is low compared with other countries [5].
In Switzerland, most autopsies of SCD victims are performed in forensic centres. Although the majority of cases are middle aged individuals who died from ischaemic heart disease, there are SCDs of children and young adults who died from genetically determined cardiac pathologies such as cardiomyopathies and channelopathies, from the literature data [6–9]. Therefore, the autopsy diagnosis is very important for living family members.
Despite clinical recommendations on genetic testing, the management of SCD victims and their families remains problematic [10–12]. The availability, or lack, of proband DNA was identified as the flow-limiting step in the UK [11, 13]. The current international recommendations on genetic testing for cardiomyopathies and channelopathies established by experts from Heart Rhythm Society, the European Heart Rhythm Association and European Society of Cardiology [14, 15] do not address practical aspects for our Swiss practice during forensic autopsy, nor the issues surrounding cardiogenetic counselling of the family members, which is very important for the prevention and potential treatment of disease.
In order to improve the diagnosis and management of genetically determined cardiac deaths, and the diagnostic procedures and preventive measures for living family members, the working group of forensic pathologists and associated cardiologists, clinical and molecular geneticists looked into the decision making process for the SCD autopsy guidelines. The multidisciplinary working group strove to provide recommendations on the interdisciplinary collaboration and workflow for forensic SCD cases in Switzerland, based on the existing guidelines for autopsy practice and genetic testing for the channelopathies and cardiomyopathies [14–18], considering the legal framework of forensic activity.
Aetiology of sudden cardiac death
The most commonly detected disease in SCD victims over 35 years of age is coronary artery disease (CAD) [6, 19]. In the younger population of less than 35 years of age, cardiomyopathies or a morphologically normal heart are the most frequent findings. According to epidemiological data from the general population, approximately 80% of SCD cases are attributed [15] to CAD, whereas 10–15% result from cardiomyopathies with a morphological substrate, such as hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), non-compaction cardiomyopathy (NCCM), or myocardial infiltrative diseases. For the remaining 5–10% the cause of SCD is related either to a structurally abnormal congenital cardiac condition (i.e. coronary artery abnormalities) or to arrhythmias without any structural changes, including many genetic arrhythmias such as channelopathies [6].
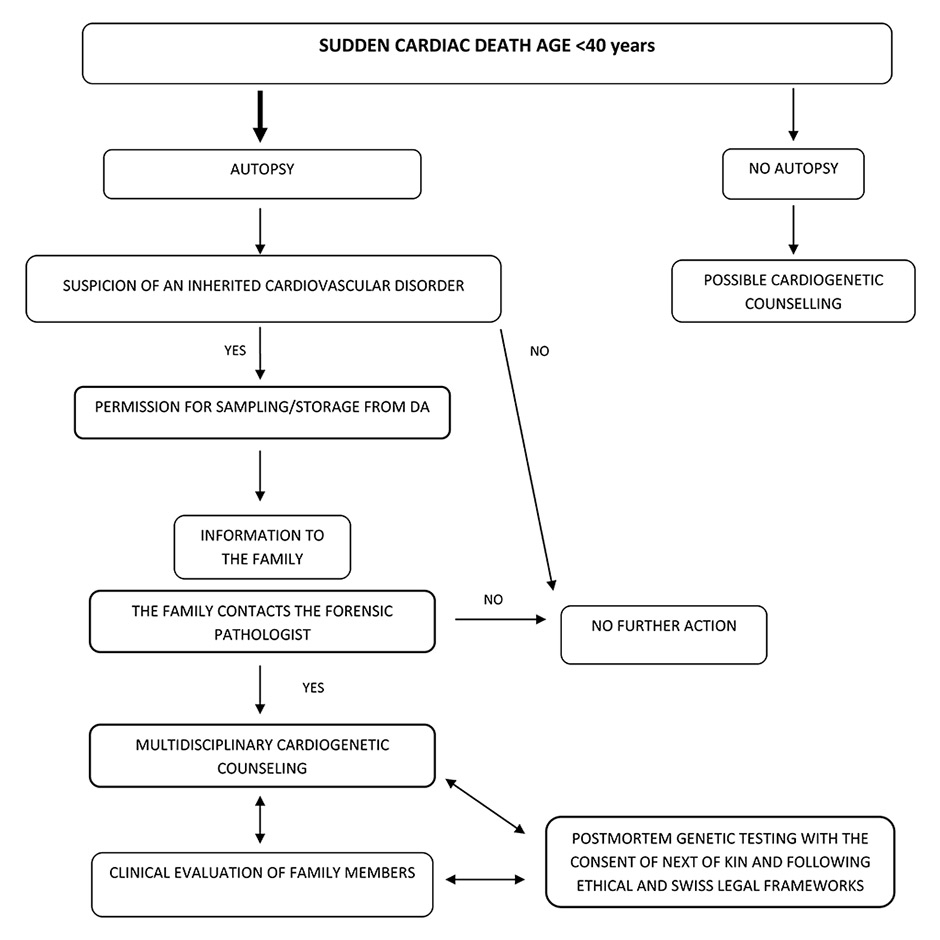
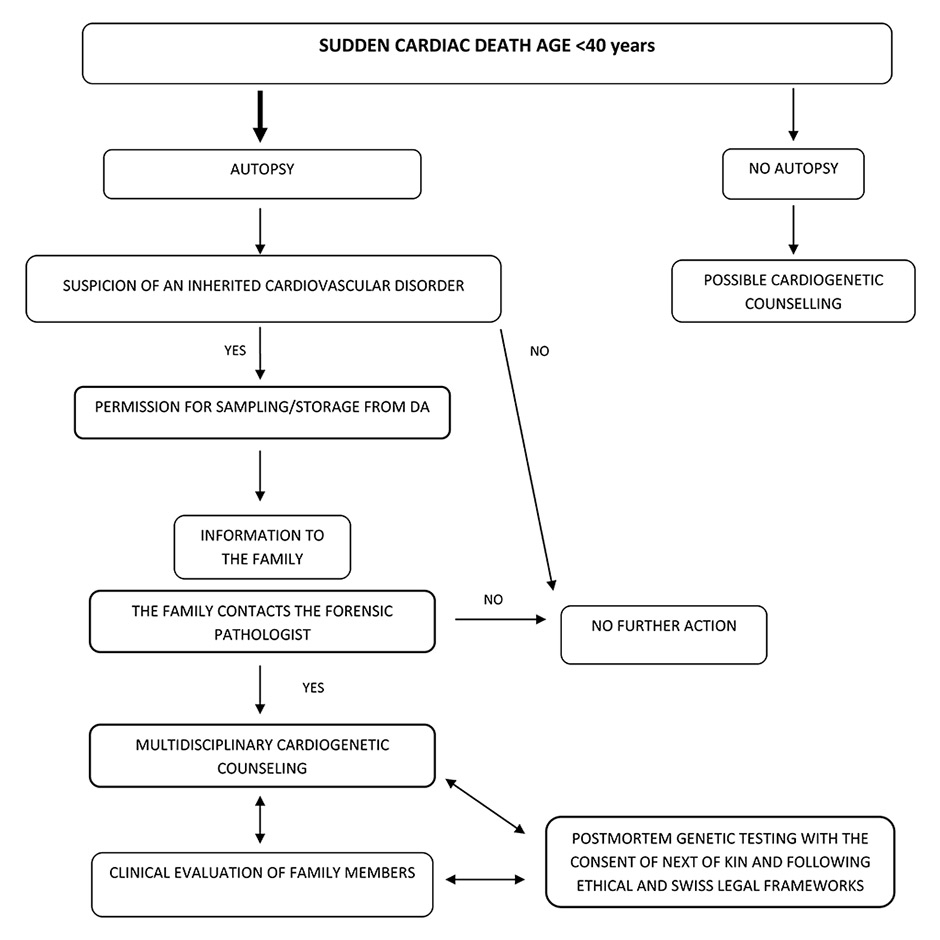
Figure 1
Flowchart of the recommended actions after a sudden cardiac death (SCD) and forensic autopsy. Even if an autopsy is not performed, cardiogenetic counselling is advised after a presumed SCD. More explanations in” Recommended course of action in Swiss practice for SCD”
DA = district attorney
A detailed autopsy and histopathological examination of the heart may identify CAD or structural cardiac disease and is best performed for all cases of SCD, especially in the young, by or in conjunction with an expert cardiac pathologist [16, 18, 20]. Not all causes of SCD can be determined at autopsy. “Autopsy-negative SCD” corresponds to cases where (1.) the autopsy failed to identify the cause of death and (2.) non-cardiac aetiologies were excluded (e.g., drug overdose by toxicological analyses). The percentage of hearts without morphological substrate found in SCD victims varies from 6% to 53% [7–9].
Some genetically determined cardiac diseases responsible for sudden cardiac death are characterized by morphological alterations that may be observed at autopsy and/or upon histopathological examination, for example, HCM, DCM, ARVC or NCCM [18, 21–23]. Those related to cardiac channelopathies, such as congenital long QT syndrome (LQTS), Brugada syndrome (BrS) or catecholaminergic polymorphic ventricular tachycardia (CPVT) can be diagnosed only after molecular genetic analyses [7, 12, 24–26]. Most of these genetic disorders are characterised by a wide genetic heterogeneity and follow an autosomal dominant mode of inheritance [14, 27–29] (table 1).
Current situation of sudden cardiac death management in Switzerland
In Switzerland, as in many other countries, SCDs and all other sudden unexpected deaths (SUDs) must be reported to the district attorney’s (DA’s) office, which in turn seizes the corpse and initiates an inquiry. The main focus of such an inquest is to determine the manner of death (natural, accidental, suicidal or homicidal). Since 1 January 2011, Swiss Criminal Procedure Code has been harmonised throughout Switzerland. The DA commissions forensic pathologists to conduct the examination of the body. In Switzerland, the preliminary forensic examination is a scene investigation, a thorough external examination of the corpse, ideally at the scene, performed by specially trained physicians who evaluate the findings at the scene and the medical history. If third-party involvement is excluded, the DA will often refrain from commissioning further examinations, such as an autopsy. For example, for elderly individuals with no signs of relevant trauma and/or a medical history which could explain the cause of death, the corpse would be liberated after an external examination and not be subjected to an autopsy. As younger individuals often do not have a medical history that could reasonably explain their death, the DA usually commissions a forensic autopsy. The main focus of the forensic autopsy, which does not require the consent of the next-of-kin, is to find out under what circumstances the person died and to reconstruct the course of events that led to the individual’s demise. The actual cause of death is legally of minor importance. Many forensic pathologists will refrain from performing histopathological or toxicological examinations if a natural death, such as an acute coronary artery occlusion with resulting myocardial infarction, is detected. In some cases, a genetic test is required in order to reach a final forensic autopsy diagnosis, and as such may be requested by the DA [30, 31]. However, genetic testing during the course of autopsy is rarely performed as (1.) medical diagnostics are not a priority for the DA, (2.) costs of genetic analysis would be supported by the DA and (3.) the feedback of results to the next-of-kin raises several ethical issues. In practice, the DA will mostly refrain from commissioning post-mortem molecular testing.
Although all SUDs must, by law, be reported to the DA, this is not always the case. Owing to lack of knowledge and/or fear of judicial issues, the death-certifying physician will occasionally deem a sudden death to be “natural” rather than “undetermined”. Such cases may, however, undergo a clinical autopsy if the next-of-kin wish it. The main focus of a clinical autopsy, performed by a clinical pathologist, is to determine the cause of death and identify any pathological disorders. Unfortunately, many cases will not undergo any further post mortem examinations and are subsequently buried or cremated. The percentage of non-autopsied cases of young victims of presumed SCD in Switzerland is unknown and could be high. Nevertheless, in cases of suspected inheritable cardiac disorder, cardiogenetic counselling should be suggested.
The Swiss protocols for forensic post-mortem cardiac examination have been rather inconsistent. In order to unify the different autopsy techniques and to improve the general standard of SCD case handling, the Swiss Society of Legal Medicine (SSLM) founded a working group to establish recommendations for minimum standards of autopsy practice for cardiac examination. These recommendations were published on the SSLM homepage: harmonisation of routine forensic autopsy practice for SCD cases in Switzerland [32]. There are currently several different definitions of sudden cardiac death. This paper is restricted to the terminology used in forensic pathology in Switzerland (table 2), which defines SCD as a sudden unexpected death (SUD) of cardiac causes occurring in a short time period (generally within 1 hour after symptom onset) in a person with known or unknown cardiac disease. Sudden infant death syndrome (SIDS) is a subgroup of unexplained sudden death among infants under one year of age. SIDS lies beyond the scope of these recommendations.
|
Table 1: Spectrum of the most frequent inherited cardiomyopathies and ion channel disorders (channelopathies) associated with sudden cardiac death. |
|
Disorder
|
Inheritance
|
Number of known genes
|
Yield of the genetic test
|
|
Cardiomyopathies
|
| Hypertrophic cardiomyopathy |
Usually AD |
~ 30 |
60% |
| Arrhythmogenic right ventricular cardiomyopathy |
Usually AD/AR |
12 |
50% |
| Dilated cardiomyopathy |
Usually AD |
~ 40 |
10–40% |
| Left ventricular non-compaction cardiomyopathy |
AD |
> 10 |
15–20% |
|
Channelopathies
|
| Long QT syndrome |
AD/AR |
15 |
70% |
| Brugada syndrome |
AD |
21 |
15–30% |
| Catecholaminergic polymorphic ventricular tachycardia |
AD/AR |
6 |
50–60% |
| Short QT syndrome |
AD/AR |
5 |
5–10% |
| AD = autosomal dominant; AR = autosomal recessive |
|
Table 2:Terms, abbreviations and definitions used in Swiss forensic pathology (in alphabetical order). |
|
Term
|
Abbreviation
|
Definition
|
| Cause of death |
COD |
Clinical condition that led to death |
| Clinical autopsy |
|
Autopsy performed upon the request of the treating physicians and/or family members, with the main focus on the cause of death. Permission from family compulsory. |
| District attorney |
DA |
Prosecutor |
| Forensic autopsy |
|
Autopsy commissioned by the DA with the main focus on legal issues. Permission from the relatives not necessary. |
| Genetic heterogeneity |
|
Mutations in genes that cause the same or different disorders |
| Manner of death |
MOD |
Circumstances that led to death |
| Sudden cardiac death |
SCD |
Unexpected death due to cardiac causes |
| Sudden infant death syndrome |
SIDS |
Unexpected, to date not fully understood, infant death |
| Sudden unexpected death |
SUD |
Sudden unexpected/unexplained death; all violent or unexpected deaths, regardless of their cause |
Recommended course of action in Swiss forensic practice for sudden death
In order to optimise the diagnostic procedures and the preventive measures for the family members, we recommend the following procedure (see also fig. 1).
Autopsy
The post-mortem heart examination should be performed in accordance with the guidelines given by the SSLM [31] for all cases of SCD under 40 years of age. If no morphological (macroscopic and microscopic) or toxicological cause of death can be established, and biochemical analyses do not show any significant disorder, a so-called “undetermined” or “functional death” can be postulated (also termed, in our opinion erroneously, “negative autopsy”). A “functional death” may be due to, for example, an arrhythmic disorder or an epileptic seizure. A “functional death” usually indicates that the forensic pathologist could not find any structural/morphological substrate as the cause of death.
In the autopsy report of SUD cases, and also in cases where a genetically determined cardiomyopathy is diagnosed by morphological examination (HCM, ARVC, DCM, NCCM), the possibility for genetic testing should be mentioned and the appropriate samples should be collected in anticipation of such testing. The DA should be asked for permission to store the collected samples for 5 years. The examiner should note, providing the DA permitted storage of the samples for 5 years, the following: “in addition to sample storage for toxicological analyses etc., samples were collected for possible genetic testing. These additional samples will be stored for 5 years.” These samples, namely EDTA blood or tissue, should be stored at least at –20 °C (ideally at –80 °C), initially in the laboratory of forensic medicine. The samples can then be sent to an accredited laboratory for genetic analysis with the agreement of the DA, who has the authority to do so. In the case of a suspected inherited cardiac disorder, the victim’s family should be informed that the results of the autopsy may be of clinical importance to them.
Multidisciplinary cardiogenetic counselling and information
If the relatives contact the forensic pathologist for more information or request the results of the autopsy, multidisciplinary counselling should be organised if an inherited cardiac disorder is suspected, and if wished for, initiated by the forensic pathologist. The way to contact the family is discussed with the local ethics committee (for example in Lausanne a succinct letter addressed to the family is sent through the DA; this solution allows the right not be informed to be respected). The forensic pathologist is encouraged to attend this multidisciplinary cardiogenetic counselling, which would involve at least a cardiologist and a clinical geneticist. This consultation should be performed in accordance to established international guidelines [14, 16]; ethical and Swiss legal frameworks must be respected [31]. The information concerning the autopsy results, the risk of a genetic disease and further examinations, such as a post-mortem genetic testing of the deceased should be discussed during this multidisciplinary counselling.
In our opinion, the proposed course of action should allow the gap to be closed between existing Swiss recommendations for routine forensic cardiac examination [32] and the clinical recommendations such as “HRS/EHRA Expert Consensus Statement on the State of Genetic Testing for the Channelopathies and Cardiomyopathies” [14] as well. Synchronisation of autopsy standards with multidisciplinary cardiogenetic counselling will improve the management of these rare but complex cases and the diagnostic and potential therapeutic procedures for the living family members.
Key points
1. The autopsy of sudden death victims under 40 years of age is strongly recommended.
2. Frozen (at least –20 °C, ideally –80 °C) post-mortem material for possible genetic testing (EDTA blood and/or tissue) should be collected and stored for at least 5 years upon permission from the DA.
3. The family should be informed about the autopsy results.
4. Multidisciplinary cardiogenetic counselling for the family of a SCD victim with a suspected inheritable cardiac disorder is recommended.
5. The recommended time to perform post-mortem genetic testing is after a cardiogenetic counselling of the family.
References
1 Papadakis M, Sharma S, Cox S, Sheppard MN, Panoulas VF, Behr ER. The magnitude of sudden cardiac death in the young: a death certificate-based review in England and Wales. Europace. 2009;11(10):1353–8.
2 Pilmer CM, Porter B, Kirsh JA, Hicks AL, Gledhill N, Jamnik V, et al. Scope and nature of sudden cardiac death before age 40 in Ontario: A report from the Cardiac Death Advisory Committee of the Office of the Chief Coroner. Heart Rhythm. 2013;10(4):517–23.
3 Vaartjes I, Hendrix A, Hertogh EM, Grobbee DE, Doevendans PA, Mosterd A, et al. Sudden death in persons younger than 40 years of age: incidence and causes. Eur J Cardiovasc Prev & Rehabil. 2009;16(5):592–6.
4 Winkel BG, Holst AG, Theilade J, Kristensen IB, Thomsen JL, Ottesen GL, et al. Nationwide study of sudden cardiac death in persons aged 1–35 years. Eur Heart J. 2011;32(8):983–90.
5 Hofer F, Fellmann F, Schlapfer J, Michaud K. Sudden cardiac death in the young (5–39 years) in the canton of Vaud, Switzerland. BMC Cardiovascular Disorders. 2014;14(1):140.
6 Chugh SS, Reinier K, Teodorescu C, Evanado A, Kehr E, Al Samara M, et al. Epidemiology of Sudden Cardiac Death: Clinical and Research Implications. Prog Cardiovasc Dis. 2008;51(3):213–28.
7 Boczek NJ, Tester DJ, Ackerman MJ. The molecular autopsy: an indispensable step following sudden cardiac death in the young? Herzschrittmacherther Elektrophysiol. 2012;23(3):167–73.
8 Semsarian C, Hamilton RM. Key role of the molecular autopsy in sudden unexpected death. Heart Rhythm. 2012;9(1):145–50.
9 Tester DJ, Ackerman MJ. The molecular autopsy: should the evaluation continue after the funeral? Pediatr Cardiol. 2012;33(3):461–70.
10 Michaud K, Mangin P, Elger B. Genetic analysis of sudden cardiac death victims: a survey of current forensic autopsy practices. Int J Legal Med. 2010:1–8.
11 Nunn LM, Lambiase PD. Genetics and cardiovascular disease – causes and prevention of unexpected sudden adult death: the role of the SADS clinic. Heart. 2011;97(14):1122–7.
12 Tester DJ, Medeiros-Domingo A, Will ML, Haglund CM, Ackerman MJ. Cardiac channel molecular autopsy: insights from 173 consecutive cases of autopsy-negative sudden unexplained death referred for postmortem genetic testing. Mayo Clin Proc. 2012;87(6):524–39.
13 Behr ER, Casey A, Sheppard M, Wright M, Bowker TJ, Davies MJ, et al. Sudden arrhythmic death syndrome: a national survey of sudden unexplained cardiac death. Heart. 2007;93(5):601–5.
14 Ackerman MJ, Priori SG, Willems S, Berul C, Brugada R, Calkins H, et al. HRS/EHRA Expert Consensus Statement on the State of Genetic Testing for the Channelopathies and Cardiomyopathies: This document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Europace. 2011;13(8):1077–109.
15 Authors/Task Force m, Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, et al. 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014;35(39):2733–79.
16 Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes: Document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10(12):1932–63.
17 Brinkmann B. Harmonisation of medico-legal autopsy rules. Int J Legal Med. 1999;113(1):1–14.
18 Basso C, Burke M, Fornes P, Gallagher P, de Gouveia R, Sheppard M, et al. Guidelines for autopsy investigation of sudden cardiac death. Virchows Archiv. 2008;452(1):11–8.
19 Eckart RE, Shry EA, Burke AP, McNear JA, Appel DA, Castillo-Rojas LM, et al. Sudden Death in Young Adults: An Autopsy-Based Series of a Population Undergoing Active Surveillance. J Am Coll Cardiol. 2011;58(12):1254–61.
20 Thiene G, Veinot JP, Angelini A, Baandrup UT, Basso C, Bruneval P, et al. AECVP and SCVP 2009 Recommendations for Training in Cardiovascular Pathology. Cardiovasc Pathol. 2010;19(3):129–35.
21 Basso C, Corrado D, Marcus FI, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. The Lancet. 2009;373(9671):1289–300.
22 Hughes SE. The pathology of hypertrophic cardiomyopathy. Histopathology. 2004;44(5):412–27.
23 Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, et al. Contemporary Definitions and Classification of the Cardiomyopathies: An American Heart Association Scientific Statement From the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113(14):1807–16.
24 Napolitano C, Bloise R, Monteforte N, Priori SG. Sudden Cardiac Death and Genetic Ion Channelopathies: Long QT, Brugada, Short QT, Catecholaminergic Polymorphic Ventricular Tachycardia, and Idiopathic Ventricular Fibrillation. Circulation. 2012;125(16):2027–34.
25 Wilde AA, Tan HL, Wilde AA, Tan HL. Inherited arrhythmia syndromes. Circulation Journal. 2007;71(Suppl A):A12–9.
26 Wilde AAM, Behr ER. Genetic testing for inherited cardiac disease. Nat Rev Cardiol. 2013;10(10):571–83.
27 Abriel H, Zaklyazminskaya EV. Cardiac channelopathies: genetic and molecular mechanisms. Gene. 2013;517(1):1–11.
28 Charron P, Arad M, Arbustini E, Basso C, Bilinska Z, Elliott P, et al. Genetic counselling and testing in cardiomyopathies: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2010;31(22):2715–26.
29 Koneru JN, Wood MA, Ellenbogen KA. Rare Forms of Preexcitation: A Case Study and Brief Overview of Familial Forms of Preexcitation. Circ Arrhythm Electrophysiol. 2012;5(4):e82–e7.
30 Elger BS, Michaud K, Fellmann F, Mangin P. Sudden death: ethical and legal problems of post-mortem forensic genetic testing for hereditary cardiac diseases. Clin Genet. 2010;77(3):287–92.
31 Michaud K, Fellmann F, Abriel H, Beckmann JS, Mangin P, Elger BS. Molecular autopsy in sudden cardiac death and its implication for families: discussion of the practical, legal and ethical aspects of the multidisciplinary collaboration. Swiss Med Wkly. 2009;139(49–50):712–8.
32 http://www.sgrm.ch/medizin/arbeitsgruppen/sudden-cardiac-death.html. (Accessed 11th February 2015.)