“An unspoken world of unspoken things”: a study identifying and exploring core beliefs underlying self-stigma among people living with HIV and AIDS in Ireland
DOI: https://doi.org/10.4414/smw.2015.14113
Nadine
Ferris France, Steve
McDonald, Ronan R
Conroy, Elaine
Byrne, Chris
Mallouris, Ian
Hodgson, Fiona
Larkan
Summary
PRINCIPLES: Human immunodeficiency virus (HIV) related self-stigma – negative self-judgements resulting in shame, worthlessness and self-blame – negatively influences access to care and treatment, and overall quality of life for people living with HIV (PLHIV). Despite evidence that high levels of self-stigma exist among PLHIV, and is experienced to a far greater extent than stigma received from the broader community, there is a paucity of research aimed at understanding causes and functions of self-stigma, and an absence of interventions to mitigate its harmful effects. Understanding the core beliefs underlying self-stigma is therefore essential.
METHODS: This pilot study used a qualitative approach to analyse interviews and written statements to uncover core beliefs underlying self-stigma, the functions thereof, and strategies used to overcome it, among a heterogeneous group of PLHIV in Ireland.
RESULTS: Core beliefs underlying HIV-related self-stigma were uncovered and grouped into four categories: disclosure; sexuality and sexual pleasure; self-perception; and body, illness and death. Reported functions of self-stigma included contributing to maintaining a “victim” status; providing protection against stigma received from others; and justifying non-disclosure of HIV status. To cope with self-stigma, participants highlighted: community involvement and professional development; personal development; and connection to others and sense of belonging. Findings were also used to create a conceptual framework.
CONCLUSIONS: This study helps fill identified gaps in knowledge about self-stigma as experienced by PLHIV. By understanding the core beliefs driving self-stigma, it will be possible to create targeted interventions to challenge and overcome such beliefs, supporting PLHIV to achieve improved wellbeing and lead productive lives free of self-limitation and self-judgement.
Introduction
Human immunodeficiency virus (HIV) infection is increasingly becoming perceived as a chronic disease. Those infected can expect to achieve a full life-span of 72–75 years [1], if appropriate treatment and support are available. As a consequence, the focus of health services, and of those living with HIV, is turning from preventing illness and death to optimising quality of life and enabling the fulfilment of life goals. Even where HIV prevention programmes are effective, ongoing fears around the outcomes of testing and disclosure (and broader social implications of a positive HIV diagnosis) mean the challenges of living with HIV are likely to persist.
HIV-related stigma acts as a significant barrier to prevention, testing and treatment [2–4]. Although Ireland has a relatively low incidence of HIV [5], stigma and discrimination for those infected still pose a significant challenge: 49% of people living with HIV (PLHIV) in Ireland reported experiencing discrimination by friends and 43% by the local community [6]. Stigma occurs at varying, interrelated, levels: enacted stigma (discrimination), referring to actions or omissions as a result of stigma; societal/perceived stigma, where an individual anticipates or perceives themselves as stigmatised; and finally self-stigma – negative self-judgements resulting in shame, worthlessness and self-blame [7].
Socially derived stigma has been widely studied in people living with illness and disabilities [8–11], but focussed rarely on self-stigma, also termed “internalised stigma”. In HIV, the Asia-Pacific Regional Analysis of the Stigma Index Study in nine countries, involving 4395 participants, found disturbingly high levels of internalised stigma manifesting as shame, guilt and self-loathing. For example, 75% of PLHIV in Pakistan reported they were ashamed of their HIV status, and even in Sri Lanka, which reported the least self-stigma, 54% of participants reported being ashamed [12]. Self-stigma also has broader repercussions, leading to failure to seek treatment and use care services, reduced wellbeing [13], depression [14], low self-esteem and reduced self-efficacy [15], poor long-term coping [7], and lower quality of life [16]. A recent study by Overstreet, cited in Cairns (2013) [17], also found that people with internalised stigma were less likely to disclose their HIV status to partners or families.
It would appear from the literature that self-stigma is experienced by HIV-infected people to a far greater extent than stigma received from the broader community [7, 12, 18–22]. Kalichman et al. [23] reported that, of 2,306 adults in the general public in Cape Town, 10% believed that PLHIV were dirty, contrasting with 27% of PLHIV who felt they were dirty; 13% of the general public believed that PLHIV had done something to deserve it, as opposed to the 41% of PLHIV who felt guilty about having been infected. The same pattern can be found in Ireland, where 84% of PLHIV feel they are viewed negatively by society whereas 54% of the general public shared that view [6]. Lastly, the fact that self-stigma was observed as greater than levels of stigma in the general population strongly suggests that self-stigma is not just an internalisation of the prevalent social stigma, but a distortion and amplification of it.
“Stigma” was defined by Goffman in 1963 as “an attribute that is significantly discrediting” which in the view of others serves to reduce the person who possesses it. Goffman also importantly identified stigma as a complex and multi-dimensional phenomenon [24]. For Link and Phelan (2001), there is variability not just in definition, but also its application by researchers [25]. Link et al. in 1997 defined “self-stigma” as “the extent to which people endorse negative beliefs and feelings associated with their stigmatized attribute and apply them to self” [26]. As they are central to the manifestation of self-stigma, core beliefs must be considered – i.e., the “fundamental, inflexible, absolute and generalised beliefs that people hold about themselves, others, the world and/or the future” [27]. In shaping an individual’s worldview, core beliefs that contribute to self-stigma can have a profound effect on a sense of self-efficacy and concept of self [28]. Understanding the core beliefs underpinning self-stigma can be a foundation for interventions and programmes designed to reduce its harm.
From the outset, the study reported on here was cognisant of gaps in interventions to support PLHIV in dealing with self-stigma. For example, Sengupta et al. [29] reported that, despite the negative impact of stigma on PLHIV, there have been surprisingly few intervention studies aimed at reducing HIV-stigma to date. This is particularly the case with self-stigma, which is under-represented in the research literature. Kalichman and Simbayi [30], who have widely published on HIV-related stigmas, acknowledge that approaches are needed that go beyond mass education and work within more ingrained belief systems.
The identification of unhelpful or negative core beliefs is the basis from which individuals can be supported in developing healthier belief systems through cognitive therapy strategies [28]. The use of stress-management interventions also shows evidence of efficacy: Brown and Vanable’s review [31] of literature reporting stress-management interventions for PLHIV, concluded that there is a growing body of evidence demonstrating that these interventions – including cognitive behavioural interventions, meditation, mindfulness and relaxation – in the context of HIV can reduce psychological distress and improve psychosocial functioning. Among such interventions, the inquiry-based stress reduction (IBSR) technique, developed by Byron Katie [32, 33] supports participants in reducing their perceived level of stress by self-inquiry on thoughts and beliefs connected to stressful circumstances or symptoms. IBSR has shown positive results in a trial among survivors of breast cancer [34], but has not yet been applied to the support of PLHIV. Another technique, cognitive behavioural therapy (CBT), is perhaps the most researched psychotherapeutic approach and has a growing reputation for being a highly effective treatment in dealing with stressful beliefs or thoughts [35].
To successfully address self-stigma, core beliefs underlying this phenomenon must first be identified and contextualised. This study was designed to: (a) identify and gain understanding of core beliefs underlying self-stigma in PLHIV in Ireland; (b) enhance understanding of the phenomenon; and (c) inform interventions aimed at mitigating its harmful effects. Three research questions were formulated:
1. What are the core beliefs underlying HIV-related self-stigma among the studied group of people living with HIV?
2. What are the functions of self-stigma among the studied group of people living with HIV?
3. What coping strategies are used by participants to manage self-stigma?
Methodology and data collection
A qualitative approach within the interpretivist paradigm was adopted for this research. This allowed for a deeper understanding of the lived experiences of individuals that could subsequently help inform the design of a therapeutic intervention. Semi-structured interviews and written statements were used to gather information from participants. Each interview lasted approximately one hour and was recorded, with prior written consent. During interviews, participants were asked to write the following open-ended statement: “I am HIV positive and that means that…” (participants with limited literacy dictated their statements to the researcher). This approach is commonly used to draw out core beliefs as part of inquiry-based stress reduction: the work of Bryon Katie [32]. A similar method is used in cognitive behavioural therapy [36].
Ethical approval for this study was granted by the Health Policy Management / Centre for Global Health Research and Ethics Committee at Trinity College Dublin.
Participants were purposively selected from Open Heart House, the largest Irish peer-support network of PLHIV at the time of the research. Owing to the highly varied nature of the epidemiology of HIV in Ireland [5], the studied group included a large degree of heterogeneity, incorporating male, female and transgender participants, as well as migrant individuals, drug users, men who have sex with men (MSM) and heterosexuals. Seventeen potential participants were approached, and all agreed to participate. Participants’ ages ranged between 31–51 years (average age 43 years); 6 were women, 10 were men, and 1 was transgender. Participants had been living with HIV for between 3 and 29 years (average 11 years). Participants’ nationality was predominantly Irish, but also included individuals from South, East and West Africa, and East and Central Europe. Further participant details are included in table 1. Although there was diversity within the sample, it was too small to analyse across differences in gender, race, ethnicity and nationality. The core beliefs outlined in this study are therefore drawn from across the group as a whole.
A review of current frameworks and models for measuring stigma and self-stigma informed the analysis and thematic clustering of this study. Early work by Berger et al. [37] highlighted four main categories to understand and measure stigma: personalised stigma, disclosure concerns, negative self-image and concern for public attitude. Poku et al. [38], in a qualitative study better to understand stigma, highlighted social rejection, financial insecurity, internalised shame, social interaction, self-worth, and body image as main dimensions. Providing more detail and broadening the categories on self-stigma, Holzemer et al. [39] presented a framework that also included self-exclusion, negative self-perception and overcompensation.
Most recently, building on extensive formative qualitative and quantitative research on HIV-stigma, Kalichman et al. [7] developed the Internalised AIDS-related Stigma Scale (IASS). The framework drew upon previously validated scales and beliefs guided by the theoretical framework offered by Goffman [24], and proposed six scale items covering self-defacing beliefs and negative perceptions.
Interviews were transcribed in full, then thematically coded and analysed using an iterative coding strategy guided by the frameworks outlined above. The themes were continually and systematically updated as the data was analysed, reanalysed and grouped into various themes. New themes were added as they emerged, and this process continued until no more new themes arose and data saturation was reached [40].
|
Table 1: Study demographics and participant information (n = 17), showing participants’ medication status, country of origin, exposure group, employment and relationship status. |
| Currently taking ARVs: |
|
| Yes |
16 |
| No |
1 |
| No. of years taking ARVs: |
|
| Mean |
9 |
| Range |
0.2–26 |
| Country of origin: |
|
| Ireland |
11 |
| Germany |
1 |
| Poland |
1 |
| Côte d’Ivoire |
1 |
| South Africa |
1 |
| Nigeria |
1 |
| Botswana |
1 |
| Exposure group: |
|
| Heterosexual |
9 |
| IDU |
4 |
| MSM |
3 |
| Unknown |
1 |
| Currently employed: |
|
| Yes |
11 |
| No |
6 |
| Ever been ill due to HIV: |
|
| Yes |
13 |
| No |
4 |
| Has children: |
|
| Yes |
10 |
| No |
7 |
| Currently with initimate partner: |
|
| Yes |
7 |
| No |
10 |
| ARVs = antiretroviral drugs; IDU = intravenous drug use; MSM = men who have sex with men |
Core beliefs
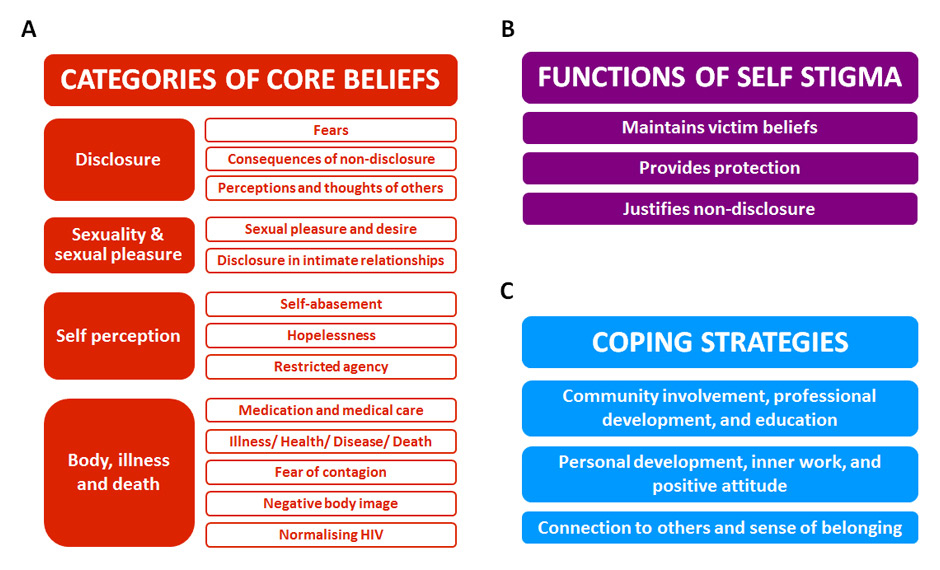
Owing to the complex nature of stigma and self-stigma [41], some overlap occurred between the emerging themes. However, it was possible to group participants’ core beliefs contributing to HIV-related self-stigma under four categories (fig. 1A).
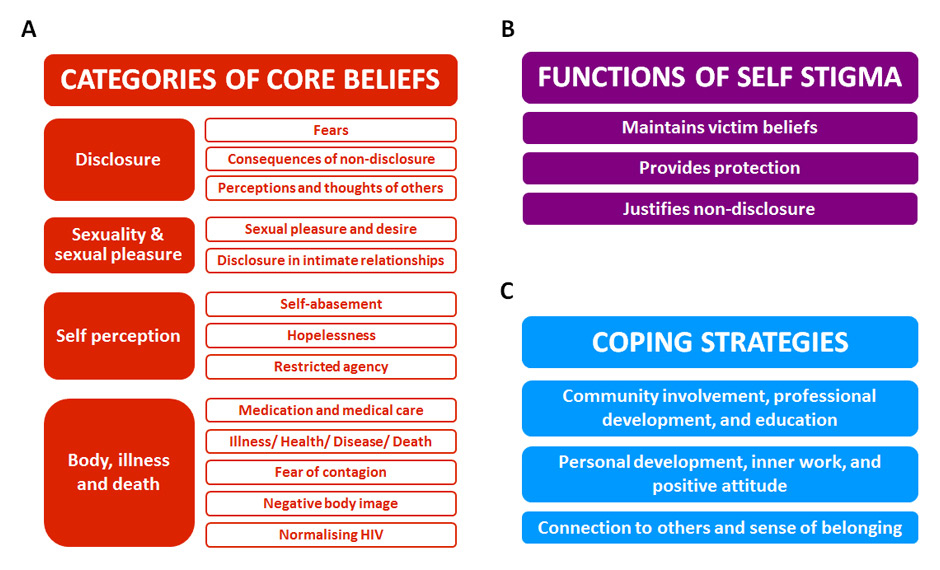
Figure 1
Framework for qualitative analysis of interview data.
Three main areas of analysis are shown: Categories of core beliefs (A, red), Functions of self-stigma (B, magenta) and Coping strategies (C, blue). Emergent themes were organised into categories (solid boxes), and subcategories where required (open boxes).
1. Disclosure: here, participants’ core beliefs surrounding disclosure of their HIV status were reported – for example, some held the belief that others would reject them if they were discovered to be HIV positive.
2. Sexuality and sexual pleasure: this category included participants’ core beliefs influencing sexual behaviour, such as the belief that they could no longer enjoy sex with an intimate partner.
3. Self-perception: the core beliefs held by participants about, for example, their sense of worth or agency fell into this category ‒ such as believing that they were worthless or that they could not have a child or find employment because of their status.
4. Body, illness and death: in this category, beliefs surrounding the physical effects of HIV were recorded – for example, some of the participants believed that they were likely to suffer prolonged illness, and a slow death, as they had witnessed in other HIV patients.
Disclosure
Fears and consequences of disclosing one’s HIV status are well documented elsewhere [37, 42–44]. Notably, people with higher levels of self-stigma are more likely to avoid disclosing their status [45]. We sought to understand more fully the beliefs contributing to fear and stress around disclosure, and within this category participants’ beliefs were broadly grouped into three subcategories.
Fears
A fear of being talked about and ridiculed was expressed by many participants, as well as of being labelled and stigmatised. Here, beliefs about being rejected predominated:
“I don’t want people to throw me away, like if yesterday I was talking very good with this person, today you tell him you are HIV positive, tomorrow you can feel like he don’t want to talk to you.” (Participant K)
Fears of betrayal had also engendered a lack of trust in many participants:
“You can’t trust nobody, so everyone is like an island…you stick to yourself, you sort your problems out yourself, you can’t call on anyone because the person you think you can talk to and trust will end up betraying you.”(Participant P)
A variety of beliefs regarding disclosure within families were reported. These included the belief that non-disclosure could protect family members from emotional hurt, or that disclosure would expose family members to secondary stigma. In certain cases where participants had already disclosed to their family a culture of silence emerged where HIV was never discussed.
Consequences of non-disclosure
Social exclusion and secrecy were commonly mentioned as outcomes of non-disclosure, in particular self-isolation and loneliness. Few participants reported actually losing friends, whereas most reported withdrawing themselves from social circles. Although social exclusion has been previously identified in the literature [39, 46, 47], it is possible that withdrawing from society is a bigger negative influence in the lives of PLHIV than actually being rejected – a finding supported by the Global Network of People living with HIV (GNP+) [12]. Some participants believed that they lived two lives – one open and honest amongst other people with HIV and another secretive, false and lonely in the outside world.
“It’s almost like trying to bring these two worlds together, where it can be the same in both, so that’s exactly the point I’m at right now…bringing it out into my real life, and with the hope I can be like, the way I am here [in Open Heart House], where I can have the same energy.” (Participant I)
Perceptions and thoughts of others
A common belief among participants was that they were viewed as bad and different:
“They think I’m a scumbag, the lowest of the low.” (Participant H)
This was particularly linked with perceived judgements from others as to how they contracted HIV:
“…if I had to tell somebody I had HIV, the first question they ask me is: 'how did you get it?'… if I was to answer that question, ‘I got it through drugs’…you see the change in people – you see the look they give you, it's like, ‘oh, she deserved that’…” (Participant B)
Several participants also reported believing their HIV status was viewed by others as less “worthy” of sympathy than other diseases:
“If you've done a survey and you asked people, ‘there's two people there…that one has cancer, that one has HIV – who do you feel more sorry for?’, nine times out of ten, people say ‘cancer’.” (Participant A)
One participant suggested human interaction begins to be framed within the context of HIV, and becomes the overriding perspective when dealing with others:
“There is this thing when you are HIV positive, you become very sensitive to what people say and how they treat you. You judge people…you become sensitive to what people do to you, because you feel they do it because you're HIV positive… So every single thing someone does to you, you read it as because you're HIV positive.” (Participant A)
Sexuality and sexual pleasure
Whereas some participants were currently involved in sexual relationships, many reported that sexual pleasure and intimacy were affected by their beliefs about self-image, fears of transmitting HIV, feelings of guilt, and lack of freedom. Here, core beliefs fell into two subcategories.
Sexual pleasure and desire
Here, participants described beliefs about never being able to have a partner, or that “normal” relationships could not be regained:
“[In] my sex life, like he doesn’t say it, but I feel it, the intimacy is gone. The, you know, experimentation and stuff, all that’s gone, it’s just basic with the condom. I tried to say to him, you know I’m undetectable, this is what the doctors say. But then I feel guilty for saying that, ‘cause I’m saying, sure he must be thinking this one just wants to have sex without a condom…does she want me to catch it and it’s not about that, it’s about trying to get back what we used to have.” (Participant A)
Some reported sex was no longer spontaneous and they no longer had sexual feelings. Additional negative influences, such as fear of contagion, feelings of guilt for having sexual needs, and lack of energy and interest, were also mentioned. The inability to enjoy sex or any sexual aspect of a relationship was also discussed, and many participants believed their own sexuality had been lost or taken from them:
“I feel like something has been stolen from me, because I can’t, as much as I’m sexually active, I cannot do that, I can’t just be free and do what I want to do.” (Participant Q)
Disclosure in intimate relationships
Outside of core beliefs affecting sexual behaviour itself, a common belief among participants was their inability to seek a new partner – the risk of rejection and discrimination was too great:
“…I don’t know what to do, where to go, how to proceed. I’m afraid of telling the person, getting a bad reaction, and that person having that information that [they] can just tell anybody else…” (Participant F)
Not all beliefs were negative, however, and some participants shared their positive experiences of being honest and not experiencing rejection:
“If anything I was more respected for being honest and being in the position to be able to give the information.” (Participant C)
Self-perception
Well documented in the literature on self-perception and self-stigma are issues of self-abasement and restricted agency [7]. In this study, core beliefs affecting self-perception were reported across three subcategories.
Self-abasement
For one participant:
“It’s great when I’m here in Open Heart House – I’m with [my own people]. But it’s different when I’m outside. It’s very hard…because I know I’m just the same as everybody else, and I don’t deserve, you know…but that dirty feeling still stands, no matter how much I wash, or how many clothes you buy, or how pretty you look. Inside [you still feel] that...worm picking away. Some days I feel toxic…as if there’s something eating away from the inside that no one else can see. But every day I feel a little bit less, like I’ve changed. You change when you’re diagnosed, and it’s not what people [say] to me. I really believe, it’s an unspoken world of unspoken things.” (Participant A)
Another participant explained just how powerful the inner world of self-stigmatising beliefs was:
“[My] inner dialogue was [that] God has punished and [put] the X on the red [door]. I felt like I couldn’t touch other people [and] couldn’t use utensils in the house that other people were using…I just felt really, really unclean all the time. I was one of the undesirables. I had really fallen…to an undesirable part of society and this was God’s choice and I was done.” (Participant F)
Many participants shared feelings and beliefs about being different from others. For one:
“I see everyone out there as the same but I’m different, and that I don’t have the same chances. You feel like this special case…a weakness.” (Participant I)
A powerful theme in the data included beliefs about being less human, undeserving, and attributing self-blame. Illustrating how some participants devalue themselves one participant said:
“If the world was ending me, and other people like me, would be left – we would not be saved.” (Participant A)
Though many participants became emotional as they shared beliefs and experiences during interviews, it was sharing how they viewed themselves that caused the most distress. This suggests strongly the damaging influence of self-stigma in the lives of participants.
Hopelessness
Hopelessness and self-pity frequently emerged among participants’ core beliefs. Several cited depression, suicidal thoughts, and feelings of hopelessness stemming from beliefs such as life being over, HIV being a killer disease, feeling a victim, being a burden to people, and not seeing any hope for the future. Though participants were answering questions specifically about HIV, responses encompassed their lived experience as a person, with HIV being just one of many difficult life challenges.
“I’ve been abandoned by my parents, living on the streets of Dublin, [and] get HIV – so why I am on this planet? For punishment, punishment, punishment. That’s all I seem to be getting. I can’t find happiness anymore. Some days I try to be up but more times I’m down and there’s only so much you can take as a human being. Sometimes I question myself: what am I living for? I don’t see any life out there. I see nothing there for me. All I see is a brick wall and every time I try to get over it something knocks me back.” (Participant J)
Restricted agency
In line with wider literature [12, 18], in relation to restricted agency, participants described a number of significant actions and opportunities they believed were not possible because they were HIV positive. For many, this included not being able to have a child, not being able to find work, or work in places of their choice, not being able to travel, having to choose friends carefully, and not being able to find a life partner:
“It stops so many things.” (Participant Q)
Body, illness and death
Among core beliefs shared by participants around medication and medical care, negative side-effects and an inability to take part in life activities were mentioned frequently. Here, core beliefs emerged across five subcategories.
Medication and medical care
In some cases, participants felt as though they were not treated properly as human in their dealings with medical services:
“Sometimes you feel like a guinea pig, they are taking blood tests and they don’t tell you what’s it for.”(Participant M)
Illness/health/disease/death
When discussing illness, most participants expressed fears about sickness and dying:
“I [will] end up dying the way I have actually seen others people dying, which is piece by piece and become mentally deficient, physically deficient, and the fact that it is a slow process.” (Participant O)
Beliefs that led to stress around health emerged frequently:
“Health has become much more of a focus – any health. I get a cold, I get worried. I get a headache, I get worried.”(Participant O)
Fear of contagion
In addition to fears for their own wellbeing, core beliefs extended to the impact of their condition on the lives of others. Many believed they would be a risk to family and friends. For one:
“I was paranoid because I didn’t know when I found out [my status]. I had my own cups, my own knives and forks, [and] I kept all of them. I wouldn’t kiss my grandchildren. Even now I won’t kiss them – my grandson asks why I turn my face away.” (Participant M)
Body image
Several participants shared beliefs about negative body image – including weight and body-shape changes – that contributed to their self-abasing thoughts. Notably, self-perception had changed – even if physical changes had not yet occurred:
“It's amazing what you see in the mirror that isn't there; I really, really hated myself.” (Participant F)
Demonstrating the complexities for some, one participant shared their experience:
“For me, all this stuff is intermingled with trans-identity. In order to go on hormones to get an ideal body shape to be a she, obviously I’ve had some breast development, not much. I’ve had to stop taking hormone replacement therapy because of contraindications [with HIV medication].” (Participant O)
Normalising HIV
Conversely, some participants stated that their self-image had improved, mentioning they now took more effort in self-care – for example giving up smoking and doing exercise.
Functions of self-stigma and coping strategies
In addition to core beliefs, the findings also provide insights into the functions of self-stigma (i.e. the “purpose” of self-stigma, as participants perceived it), and coping strategies to assist in its reduction (e.g. adaptations in behaviour and social interactions).
Functions of self-stigma
In the same way that social stigma may be seen to serve some function or benefit to society [48], it is also likely that self-stigma has a function or benefit to individuals. Participants’ responses highlighted three subcategories of functions of self-stigma (see fig. 1B).
Maintains victim beliefs
Self-stigma may subconsciously reinforce the individual as a victim, taking away the sense of personal agency and thereby contributing to a feeling of disempowerment:
“Before someone can do anything to stigmatise me or discriminate me I’ve already felt the discrimination, because you need to blame someone for what is happening to you. If you go downstairs here [at Open Heart House] and ask 50 people that are HIV positive, they will say it’s not their fault. Everyone will explain to you that it’s not their fault – everyone will be a victim. Yes it’s a strong word to call HIV positive people.” (Participant P)
Provides protection
By thinking negative thoughts about themselves, individuals may self-stigmatise in anticipation of being hurt by others:
“I say all these things to myself first that when I do have to go out into the world to survive, the stuff that people thinking about, I’ve already thought about myself, so nothing can get through, so its like a protection mode, you self-stigmatise yourself so that other people can’t hurt you.” (Participant A)
Justifies non-disclosure
Self-stigma may serve as a reasoning tool to limit one’s life choices, and rationalise actions such as avoiding disclosure:
“I come up with all the bad stuff that people can think about me. It’s to protect myself so that I don’t have to come out and say I’m HIV positive.” (Participant A)
Coping strategies
Many negative outcomes arising from being HIV positive and experiencing self-stigma had functional opposites in the coping strategies reported by participants. For example, several spoke of the importance of having a sense of belonging, acceptance, and a connection to others, thus directly addressing their feelings of social withdrawal and isolation. A sense of renewed agency was also reported, where participants found work or started volunteering after being diagnosed. Indeed, a sense of personal development strongly beneficial. Coping strategies were grouped into three broad subcategories (fig. 1C).
Community involvement, professional development and education
Some participants were motivated to return to education and, as a result, were now working – some for the first time. Participants sharing this view were engaged in community work and spoke of the sense of self-worth gained through providing support to others:
“I would have never ended up in a job if I had never become HIV positive. It just gives me great joy to sit with somebody who is in great despair and desperation and to say to them, ‘I genuinely know what you are going through’.” (Participant A)
Personal development, inner work and positive attitude
Participants also shared positive beliefs about themselves, their lives and abilities, having come to a positive place through personal development, inner work, and finding peace.
“I believe that I’m more accepting today – actually I fully accept who I am now. [Living with HIV is] a tiny part of who I am so it doesn’t stop me from doing absolutely anything.” (Participant C)
Connection to others and sense of belonging
The majority of participants shared the importance of the space created by Open Heart House in fostering a sense of belonging, providing support, and being community of people they would not have otherwise met.
Discussion and conclusions
Core beliefs of participants: Rather than simply showing levels of self-stigma, the results of this formative study build our understanding of beliefs reported by PLHIV. Although these are likely to vary across geographies and cultures, a number of core beliefs reported by this small and heterogeneous group could occur independently of gender, religion, or country – for example, the belief that one is “unclean”, undeserving of sympathy, or somehow unemployable because of being HIV-positive. Such generic core beliefs can significantly moderate behaviour, for example, decisions around disclosure or accessing treatment [49], and it is especially in the latter case that stigma represents a significant risk to the wellbeing of PLHIV. Recognising this clear danger, as well as the need to support PLHIV in achieving their life goals unhindered by self-imposed limitations, there is a now scope for targeted interventions to be created. The core beliefs reported from this study will also help inform future research and generation of meaningful measurement scales.

Figure 2
Conceptual framework of self-stigma.
Designed using concepts from Morrison (2006) [52], the framework comprises three interacting groups of factors (factors listed are non-exhaustive) which influence self-stigma: social factors, contextual factors and self factors. The complex interaction between these factors influences the development and perpetuation of self-stigma.
Functions of self-stigma: The results demonstrate key functions of self-stigma for participants. For example, it maintains victim beliefs, provides protection,and can justify non-disclosure. Unpicking the functions of stigma further could contribute substantially to our understanding of how to address it. For instance, although non-disclosure might protect against stigma received from others, to what lengths must someone go to hide their HIV status? Social withdrawal and even missing medication to maintain appearances have been reported among self-stigmatising PLHIV [50], again both representing a risk to overall wellbeing.
Coping strategies:Participants’ reported strategies for coping with HIV-related self-stigma included community involvement, personal development, and maintaining a connection with others. Like the previously reported functions of self-stigma, these had grounding in core beliefs, however in this case participants were able to challenge those beliefs. For example, in gaining employment, participants began to revise views of their lack of agency, and it was through interacting with others and undergoing personal development that they could overcome their feelings of isolation, or being worthless. Interventions to successfully address self-stigma could therefore incorporate techniques that include group, interpersonal or community interactions [51].
Conceptual framework of self-stigma:Results from this study were incorporated into a conceptual framework of self-stigma (fig. 2), designed using concepts from Morrison (2006) [52]. This framework may be of use in visualising and understanding self-stigma as a complex, multi-dimensional phenomenon. In doing so, it may inform future research into HIV-related self-stigma, as distinct from social, perceived, or enacted stigma.
Despite the negative impacts of self-stigma identified in the wider literature and from participants in this study, interventions to support PLHIV in dealing with self-stigma, particularly at the level of core beliefs, are lacking. Stigma applied by, and to, the self is unlikely to be overcome by interventions aimed at the general public, since the negative beliefs held by PLHIV are often not representative of the population as a whole [13, 17, 23]. In this study, coping strategies such as personal development and inner work were highlighted as supportive, and a targeted approach incorporating these elements could prove beneficial. It is here that interventions such as IBSR [32, 34] and CBT [35] are more likely to meet with success: both utilise a strategy of working directly with individuals to systematically identify, challenge, and ultimately overcome self-imposed negative behaviours and beliefs. Such interventions, tailored to the context of HIV self-stigma and using knowledge of underlying core beliefs, may better equip participants with the mental tools and strategies to mitigate self-stigma.
These findings help fill previously identified gaps in knowledge regarding social and psychological factors around core beliefs about HIV and personal experiences [30], moving towards understanding the origins of self-abasing and negative perceptions of PLHIV [7]. In doing so, a small but concrete step has been taken to enable others to design interventions and programmes to address this complex and important issue. This study contributes a deeper view of the issue of self-stigma among PLHIV, and it is hoped that by directing more attention towards research and support for self-stigma, treatment adherence, access to services, and general wellbeing can be improved.
The authors acknowledge that this study has limited representative potential for PLHIV in other settings, because of the relatively small number of participants. Additional research will therefore be useful in confirming that the experiences of self-stigma reported in this study also occur in other settings. Furthermore, there was considerable heterogeneity among participants in this study. However, it was also noted that the participants shared many common experiences and core beliefs underlying HIV self-stigma, and there were no instances where two participants reported contradictory experiences or beliefs.
Acknowledgements:First and foremost, we would like to thank the courageous and inspiring participants, members of Open Heart House, for their insight and their willingness to take part in this study so that we can all learn from their experience. We would also like to thank the Advisory Group members who agreed to guide and shape this study together with other friends and colleagues: Joanne Manchester, Dr. Christoforos Mallouris, Sandra King, Byron Katie, Dr. Shahar Lev-ari, Kate Considine, David O’Duffy and Joseph Jordan. We also want to thank Marife Tanate for continuing to provide inspiration to do more and do better on self-stigma. This study formed part of a Master's degree undertaken by the first author (NFF).
References
1 Nakagawa F, Lodwick RK, Smith CJ, Smith R, Cambiano V, Lundgren JD, et al. Projected life expectancy of people with HIV according to timing of diagnosis. AIDS Lond Engl. 2012;26(3):335–43.
2 Parker R, Aggleton P, Attawell K, Pulerwitz J, Brown L. HIV/AIDS-related Stigma and Discrimination: A Conceptual Framework and an Agenda for Action. New York: The Population Council; 2002.
3 Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. Am J Public Health. 2005;95(1):53–9.
4 Deacon H. Towards a Sustainable Theory of Health-related Stigma: Lessons From the HIV/AIDS Literature. J Community Appl Soc Psychol. 2006;16(6):418–25.
5 Health Services Executive Health Protection Surveillance Centre (HPSC). HIV in Ireland 2011 Report. Dublin: Government of Ireland Health Services Executive; 2012.
6 Stamp Out Stigma Campaign. HIV-Related stigma and discrimination in Ireland today. Dublin: Government of Ireland Department of Health; 2007.
7 Kalichman SC, Simbayi LC, Cloete A, Mthembu PP, Mkhonta RN, Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: the Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93.
8 Scambler G, Hopkins A. Being epileptic: coming to terms with stigma. Sociol Health Illn. 1986;8(1):26–43.
9 Robertson M, Katona C. Depression and physical illness: perspectives in psychiatry. Chichester: Wiley; 1997.
10 Ablon J. The nature of stigma and medical conditions. Epilepsy Behav EB. 2002;3(6S2):2–9.
11 Jamison KR. The many stigmas of mental illness. Lancet. 2006;367(9509):533–4.
12 Global Network of People Living with HIV (GNP+), International Community of Women Living with HIV/AIDS (ICW Global), International Planned Parenthood Federation (IPPF), Joint United Nations Programme on HIV/AIDS (UNAIDS). People living with HIV stigma index: Asia Pacific Regional Analysis 2011. Bangkok: UNAIDS; 2011.
13 Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 1982. 2007;64(9):1823–31.
14 Wight RG. Precursive depression among HIV infected AIDS caregivers over time. Soc Sci Med. 1982. 2000;51(5):759–70.
15 Health and Development Networks (HDN). Living on the outside: Key findings and recommendations on the nature and impact of HIV/AIDS-related stigma. Chiang Mai: Health and Development Networks; 2006.
16 Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17(2):157–68.
17 Cairns G. Issue 215: Spring 2013 – The diminished self – HIV and self-stigma [Internet]. NAM AIDSMap. 2013 [cited 2014 Jun 5]. Available from: http://www.aidsmap.com/The-diminished-self-HIV-and-self-stigma/page/2657859
18 Demchenko I, Sosidko T, Kostyuchok M, Belonosova N, Salabai N, Hvozdetska O, et al. People living with HIV stigma index Ukraine: Analytical report based on research findings. Kiev: All-Ukranian Network of People Living With HIV/AIDS; 2011.
19 Association des Veuves Vulnerables Affectees et Infectees par le HIV/AIDS (AVVAIS), Conseil Nationale de Lutte Contre le Sida (CNLS), Rwanda Network of People Living with HIV/AIDS (RRP+), Joint United Nations Programme on HIV/AIDS (UNAIDS). People living with HIV stigma index: Rwandan stigma and discrimination survey report. Kigali: AVVAIS; 2009.
20 Myanmar Positive Group (MPG), MMRD Research Group, Joint United Nations Programme on HIV/AIDS (UNAIDS). People living with HIV stigma index: Myanmar. Yangon: UNAIDS; 2010.
21 Network of Networks of HIV Positives in Ethiopia (NEP+), Joint United Nations Programme on HIV/AIDS (UNAIDS), Global Network of People Living with HIV (GNP+), International Planned Parenthood Federation (IPPF), Catholic Organisation for Relief and Development Aid (CORDAID), UKAID. People living with HIV stigma index: Ethiopia stigma and discrimination report. Addis Ababa: Network of Networks of HIV Positives in Ethiopia (NEP+); 2011.
22 Network of Zambian People Living with HIV/AIDS (ZNP+), Global Network of People Living with HIV (GNP+), UKAID. People Living with HIV stigma index: Zambia. Lusaka: Network of Zambian People Living with HIV/AIDS; 2012.
23 Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–43.
24 Goffman E. Stigma: notes on the management of spoiled identity. Englewood Cliffs, N.J.: Prentice-Hall; 1963.
25 Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Sociol. 2001;27(1):363–85.
26 Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38(2):177–90.
27 Beck JS. Cognitive Behavior therapy: Basics and beyond. 2nd ed. New York: Guildford Press; 2011.
28 Wenzel A. Modification of Core Beliefs in Cognitive Therapy. In: Reis de Oliviera I, editor. Standard and Innovative Strategies in Cognitive Behavior Therapy [Internet]. InTech; 2012 [cited 2014 Sep 30]. Available from: http://www.intechopen.com/books/standard-and-innovative-strategies-in-cognitive-behavior-therapy
29 Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87.
30 Kalichman SC, Simbayi L. Traditional beliefs about the cause of AIDS and AIDS-related stigma in South Africa. AIDS Care. 2004;16(5):572–80.
31 Brown JL, Vanable PA. Stress management interventions for HIV-infected individuals: review of recent intervention approaches and directions for future research. Neurobehav HIV Med. 2011;95.
32 Katie B, Mitchell S. Loving what is: Four questions that can change your life. New York: Harmony Books; 2002.
33 Katie B, Mitchell S. A Thousand Names for Joy: Living in Harmony with the Way Things Are. New York: Harmony Books; 2007.
34 Lev-ari S, Zilcha-Mano S, Rivo L, Geva R, Ron I. A prospective pilot clinical trial of “The work” meditation technique for survivors of breast cancer. Eur J Integr Med. 2013;5(6):487–94.
35 Hayes C. Clinical Pyschology: A psychoeducational cognitive behavioural approach to helping people cope. In: Devonport TJ, editor. Managing stress: From theory to application. Hauppage, NY: Nova Science Publishers; 2012. p. 229–60.
36 Williams C, Garland A. A cognitive–behavioural therapy assessment model for use in everyday clinical practice. Adv Psychiatr Treat. 2002;8(3):172–9.
37 Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29.
38 Poku KA, Linn JG, Fife BL, Azar S, Kendrick L. A comparative analysis of perceived stigma among HIV-positive Ghanaian and African American males. SAHARA J J Soc Asp HIVAIDS Res Alliance SAHARA Hum Sci Res Counc. 2005;2(3):344–51.
39 Holzemer WL, Uys L, Makoae L, Stewart A, Phetlhu R, Dlamini PS, et al. A conceptual model of HIV/AIDS stigma from five African countries. J Adv Nurs. 2007;58(6):541–51.
40 Silverman D. Doing qualitative research: A practical handbook. London: Sage; 2000.
41 Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychol Health Med. 2006;11(3):335–45.
42 Petrak JA, Doyle AM, Smith A, Skinner C, Hedge B. Factors associated with self-disclosure of HIV serostatus to significant others. Br J Health Psychol. 2001;6(Pt 1):69–79.
43 Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 1982. 2003;57(1):13–24.
44 Medley AM, Kennedy CE, Lunyolo S, Sweat MD. Disclosure outcomes, coping strategies, and life changes among women living with HIV in Uganda. Qual Health Res. 2009;19(12):1744–54.
45 Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 1982. 2008;67(8):1225–35.
46 Brouard P, Willis C. A closer look: The internalization of stigma related to HIV. Washington: POLICY Project; 2006.
47 Golden J, Conroy RM, O’Dwyer AM, Golden D, Hardouin J-B. Illness-related stigma, mood and adjustment to illness in persons with hepatitis C. Soc Sci Med. 1982. 2006;63(12):3188–98.
48 Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528–9.
49 Malta M, Petersen ML, Clair S, Freitas F, Bastos FI. Adherence to antiretroviral therapy: a qualitative study with physicians from Rio de Janeiro, Brazil. Cad Saúde Pública. 2005 Oct;21(5):1424–32.
50 Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. [Internet]. 2013[cited 2014 Sep 19];16(3(Suppl 2)). Available from: http://www.jiasociety.org/index.php/jias/article/view/18640
51 Mburu G, Ram M, Skovdal M, Bitira D, Hodgson I, Mwai GW, et al. Resisting and challenging stigma in Uganda: the role of support groups of people living with HIV. J Int AIDS Soc. 2013;16(Suppl. 2):18636.
52 Morrison K. Breaking the cycle: Stigma, discrimination, internal stigma, and HIV. Washington, DC: USAID; 2006.