The proportion of correct diagnoses is low in emergency patients with nonspecific complaints presenting to the emergency department
DOI: https://doi.org/10.4414/smw.2015.14121
Arno
Peng, Martin
Rohacek, Selina
Ackermann, Julia
Ilsemann-Kakaroumis, Leyla
Ghanim, Anna
Messmer, Franziska
Misch, Christian
Nickel, Roland
Bingisser
Summary
OBJECTIVE: To determine the proportion of correct emergency department (ED) diagnoses and of hospital discharge diagnoses, in comparison with final diagnoses at the end of a 30-day follow-up, in patients presenting with nonspecific complaints (NSCs) to the ED; to determine differences between male and female patients in the proportion of missed diagnoses.
METHODS: Prospective observational study. Diagnoses made at the ED, hospital discharge diagnoses, and final diagnoses were compared.
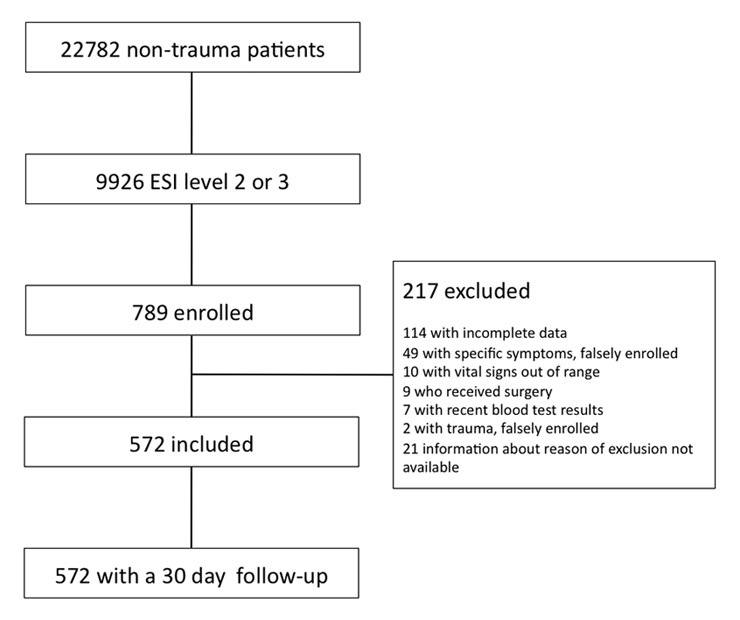
RESULTS: Of 22,782 nontrauma patients presenting to the ED from May 2007 until May 2009, 9,926 were triaged as emergency severity index level 2 or 3, of whom 789 presented with NSCs. After exclusion of 217 patients, 572 were included for final analysis.
The final diagnosis at the end of follow-up was taken to be the correct “gold standard” diagnosis. In 263 (46.0%) patients, this corresponded to the primary ED diagnosis, and in 292 (51%) patients to the hospital discharge diagnosis. The most frequent final diagnoses were urinary tract infections (n = 49), electrolyte disorders (n = 40) and pneumonia (n = 37), and were correctly diagnosed at the ED in 23, 21 and 27 patients, respectively. Of the twelve most common diagnoses (corresponding to 354 patients), functional impairment was most frequently missed. Among these 354 patients, diagnoses were significantly more often missed in women than in men (142 of 231 [62%] women vs 57 of 123 [46%] men, p = 0.004).
CONCLUSION: Patients presenting to the ED with NSCs present a diagnostic challenge. New diagnostic tools are needed to help in the diagnosis of these patients.
ClinicalTrials.gov registration number: NCT00920491
Introduction
Nonspecific complaints (NSCs) are prevalent in about 20% of elderly patients presenting to the emergency department (ED) [1, 2]. These patients are characterised by multiple comorbidities, polypharmacy and atypical disease presentation [3–6]. Altered mental status or inadequate ability to communicate may further increase diagnostic difficulties, especially when taking the history. Moreover, illness severity tends to be underestimated, leading to delayed or incorrect diagnosis and treatment, and increasing the risk of disability or death [7–12]. Although elderly patients account for an increasing number of ED visits [3, 13], little is known about the proportion of correct ED diagnoses in these patients. We therefore performed a prospective observational study including patients presenting with NSCs to the ED. The aim was to determine the proportion of correct ED diagnoses and of hospital discharge diagnoses, in comparison with final diagnoses at the end of a 30 day follow-up, and to determine differences between male and female patients in the proportion of missed diagnoses.
Methods
Study design
This prospective observational study with a 30-day follow-up was conducted from May 24th 2007 through to May 14th 2009. The study was performed at the ED of Basel University Hospital, a 700-bed tertiary care facility. The study protocol was approved by the local ethics committee, and all patients signed an informed consent form.
Figure 1
Overview of the enrolment of patients. ESI denotes emergency severity index (level 1: requires immediate life-saving intervention; level 2: high risk situation, confused, lethargic, disoriented, or severe pain/distress; level 3: two or more resources are needed; level 4: one resource is needed; level 5: no resource is needed)
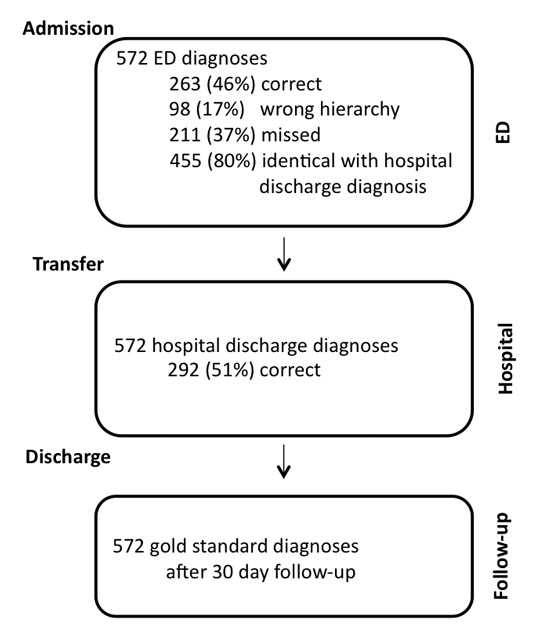
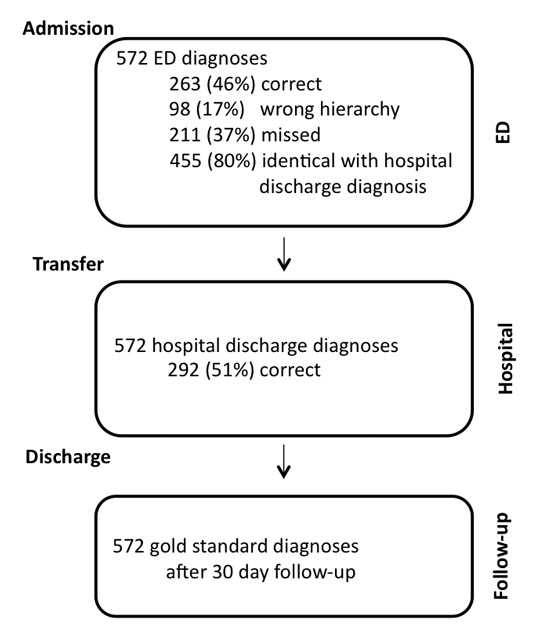
Figure 2
Overview of the proportions of correct diagnoses.
Gold standard diagnosis:Final diagnosis, according to rules of the 10th International Classification of Diseases and Related Health Problems (ICD-10), made independently by two physicians as described above.
ED diagnoses (primary, i.e. first listed):The ED diagnoses that were made by the emergency physicians at the end of the stay in the ED.
Hospital (i.e. Basel University Hospital) discharge diagnoses (primary, i.e. first listed):Diagnoses from the hospital discharge letters. If the patient was not hospitalised, the hospital discharge diagnosis was identical with the ED diagnosis.
Correct diagnosis: Primary ED diagnosis or hospital discharge diagnosis is identical with gold standard diagnosis.
Wrong hierarchy: The gold standard diagnosis was listed as a secondary ED diagnosis, but not as the primary ED diagnosis.
Missed diagnosis: The gold standard diagnosis was not made at the ED.
A validated German version of the emergency severity index (ESI) was used to triage patients [14, 15]. All adult (i.e. ≥18 years) nontrauma patients with an ESI of 2 or 3 whose vital parameters were not markedly out of range, and who presented to the ED with nonspecific complaints were eligible. Patients referred from other hospitals, patients who brought results of recent blood tests to the ED, falsely enrolled patients with specific complaints or patients with vital parameters markedly out of range (systolic blood pressure <80 mm Hg, heart rate >120 beats/minute, temperature >38.4 °C or <35.6 °C, respiratory rate >30 breaths/minute), patients who needed surgery, patients who did not sign the informed consent form, and patients with incomplete data were excluded. All patients were enrolled consecutively, 24 hours a day, by a study team.
Measurements and outcomes
Three previously trained study physicians recorded the following data on the patients’ case report forms shortly after admission: demographic baseline data, vital signs (pulse, blood pressure, respiratory rate, and oxygen saturation), all complaints (using a structured interview form), ESI, Glasgow Coma Scale score, medical history, physical examination, and electrocardiography. Venous blood samples were taken from all patients; chest X-rays and urinalysis were performed at the discretion of the treating physician. The outcome measures were (i.) the proportion of correct diagnoses made at the ED; (ii.) the proportion of correct hospital discharge diagnoses, both in comparison to the final gold standard diagnoses made at the end of a 30-day follow-up; and (iii.) the difference between male and female patients in the proportion of missed diagnoses.
Definitions
Non-specific complaints: complaints (i.) for which there were no evidence-based management protocols for emergency physicians; (ii.) on the basis of which no initial diagnosis could be made after the first assessment; (iii.) with various possible or potential interpretations; or (iv.) with little discriminative power in establishing a diagnosis; (v.) absence of trauma, bleeding, fever, headache, chest pain, abdominal pain, dyspnoea, cough, vertigo, nausea, vomiting, diarrhoea, dysuria, swollen extremity, stroke-like symptoms, syncope, palpitations, skin lesion, allergic reaction, anxiety, psychotic symptoms, suicidal tendency, confusion, intoxication or seizure. Examples of an NSC are weakness, not feeling well, fatigue, inability to walk, or inability to cope with usual daily activities.
Gold standard diagnosis:Final diagnosis, according to rules of the 10th International Classification of Diseases and Related Health Problems (ICD-10), made at the end of a 30-day follow-up. Information to establish the gold standard diagnosis was collected from the patients’ general practitioners or from hospital discharge reports. The gold standard diagnosis was established by two independent physicians with longstanding experience, certified in internal medicine. These two physicians did not make the ED or hospital discharge diagnosis. In the case of disagreement, patient records were reviewed and consensus was reached by an expert panel, consisting of two physicians certified in internal medicine and in emergency medicine, with at least 10 years of experience. If the patient was hospitalised more than 30 days, the hospital discharge diagnosis was the same as the gold standard diagnosis.
ED diagnoses (primary, i.e. first listed):The ED diagnoses that were made by the emergency physicians (EPs) at the end of the stay in the ED.
Hospital (i.e. Basel University Hospital) discharge diagnoses (primary, i.e. first listed): Diagnoses taken from the hospital discharge letters. If the patient was not hospitalised, the hospital discharge diagnosis was identical with the ED diagnosis.
Correct Diagnosis: Primary ED diagnosis or hospital discharge diagnosis was identical with the gold standard diagnosis.
Hierarchy problem: The gold standard diagnosis was listed as a secondary ED diagnosis, but not as the primary ED diagnosis.
Missed diagnosis: The gold standard diagnosis was not made at the ED.
If the primary ED diagnosis was a narrow differential diagnosis compatible with the gold standard diagnosis it was classified as a correct diagnosis. If, however, the gold standard diagnosis was one of numerous and highly variable differential ED diagnoses, it was classified as a missed diagnosis.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics 22. For the twelve most common ED diagnoses, sensitivity (true positives / (true positives + false negatives), specificity (true negatives / (true negatives + false positives), and accuracy (true positives + true negatives) / (true positives + true negatives + false positives + false negatives) were calculated, relative to the gold standard diagnoses [16].
To detect an association between the rate of missed diagnoses and gender, the two proportion z test was used, cross-tables were calculated and χ2 tests were performed. Age and gender were compared with the unpaired t-test. A p-value <0.05 was considered significant.
|
Table 1:Patients’ baseline characteristics. |
| Total, n |
572 |
| Sex, n (%) |
|
| Male |
220 (38) |
| Female |
352 (62) |
| Age, years, median (range) |
|
| All |
81 (25–101) |
| Male |
79 (31–96) |
| Female |
83 (25–101) |
| Admission to acute ward, n (%) |
|
| All |
228 (40) |
| Male |
97 (43) |
| Female |
131 (57) |
| Admission to ICU, n (%) |
|
| All |
30 (5) |
| Male |
6 (53) |
| Female |
14 (47) |
| Admission to geriatric ward or geriatric hospital, n (%) |
|
| All |
191 (33) |
| Male |
53 (24) |
| Female |
138 (39) |
| Length of hospital stay, days, mean (SD) |
|
| All |
6 (12.7) |
| Male |
9 (10.9) |
| Female |
3 (13.7) |
| ICU = Intensive Care Unit; SD = standard deviation |
Results
A total of 22,782 nontrauma patients presented to the ED during the study period from May 24th 2007 until May 14th 2009. A total of 9,926 patients were triaged as ESI level 2 or 3, of whom 789 presented with NSCs. After exclusion of 217 patients fulfilling the exclusion criteria, 572 patients were included (fig. 1). Table 1 shows the baseline characteristics of the patients. Median age was 81 years (range 25–101), and 352 (61.5%) were female. Women were significantly older (p <0.001). A total of 449 patients were hospitalised, 123 were outpatients.
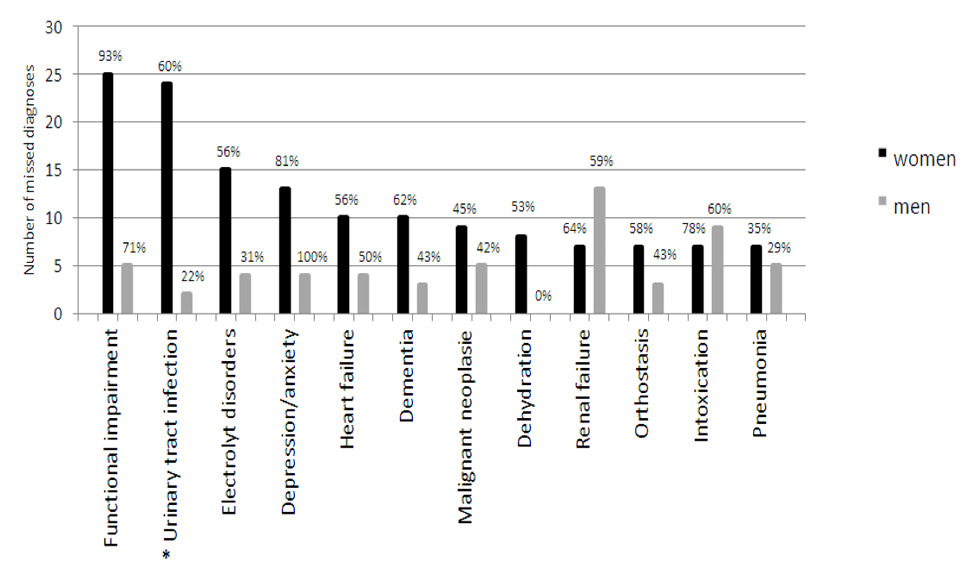
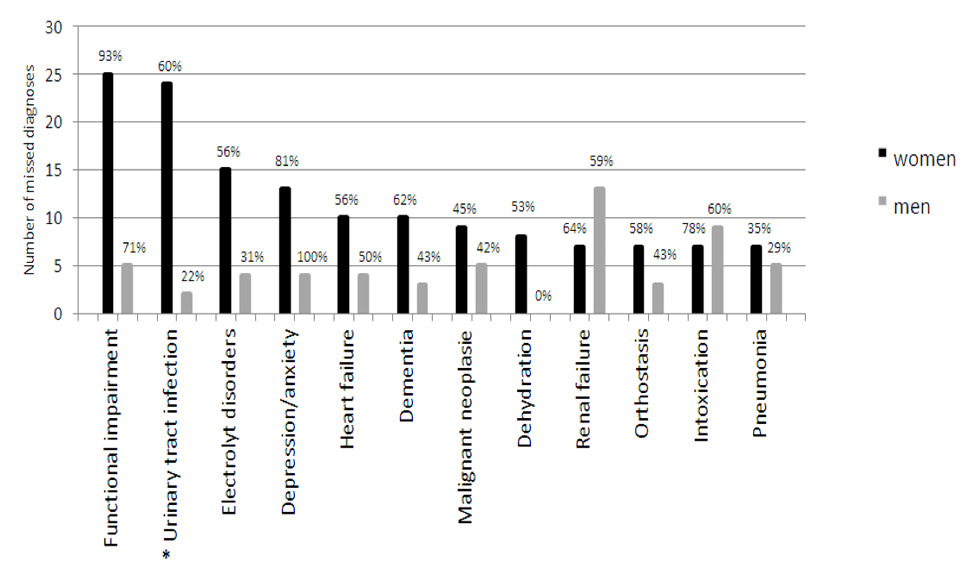
Figure 3
Missed diagnoses by gender. Missed diagnoses are shown on the y-axis in absolute numbers and in percentages (above each bar). Diagnoses are shown on the x-axis.
* The difference between men and women was significant (urinary tract infection, p = 0.04).
The primary ED diagnosis was correct in 263 (46%) patients, and a hierarchy problem occurred in 98 (17%) patients. The primary ED diagnosis and the primary hospital discharge diagnosis were identical in 455 (80%) patients; the primary hospital discharge diagnosis was correct in 292 (51%) patients (fig. 2). In 53 (9%) patients, the incorrect primary ED diagnosis was changed during the hospital stay to a correct diagnosis. On the other hand, in 24 (4%) patients, the primary ED diagnosis was correct, but was changed during hospitalisation to an incorrect diagnosis.
Table 2 shows the 12 most common diagnoses at the ED, representing a total of 354 patients. In this group of patients, a total of 155 (44%) diagnoses were correct. The most often missed conditions were functional impairment, depression or anxiety, and intoxication.
The three most common diagnoses identified were urinary tract infection (UTI, 8.6%), electrolyte disorders (7.0%), and pneumonia (6.5%). The sensitivity and specificity (ED diagnosis compared with gold standard diagnosis) were 46.9% and 96.0% in UTI, 52.5% and 98.5% in electrolyte disorders, and 67.6% and 98.9% in pneumonia, respectively. Diagnostic accuracy was 91.8% in UTI, 95.3% in electrolyte disorders and 96.9% in pneumonia.
Of these 354 patients, diagnoses were significantly more often missed in women than in men (142 of 231 [61%] women vs 57 of 123 men [46%], p = 0.004). Figure 3 shows the proportion of missed diagnoses for the 12 most common diagnoses according to gender. The occurrence of UTI was significantly higher in women (7.0%) than in men (1.6%). UTI was missed in 24 (60%) female patients, and in 2 (22%) male patients (p = 0.04). There was no significant difference in gender in the other 11 most common diagnoses.
Women diagnosed with UTI, electrolyte disorders or intoxication were significantly older than men (p = 0.024, p = 0.037 and p = 0.032, respectively). However, age had no significant effect on the proportion of correct diagnoses in these conditions. Patients with the correct diagnosis of heart failure were older than patients for whom this diagnosis was missed (p = 0.01).
|
Table 2:Twelve most frequent emergency department (ED) diagnoses. |
|
ED diagnosis
|
All
|
Correct
|
Sensitivity
|
Specificity
|
Accuracy
|
|
n (%)
|
n (%)
|
%
|
%
|
%
|
| Urinary tract infection |
49 (8.6) |
23 (47) |
46.9 |
96.0 |
91.8 |
| Electrolyte disorders |
40 (7.0) |
21 (53) |
52.2 |
98.5 |
95.3 |
| Pneumonia |
37 (6.5) |
25 (68) |
67.6 |
98.9 |
96.9 |
| Functional impairment |
34 (6.0) |
4 (12) |
11.8 |
84.4 |
80.1 |
| Renal failure |
33 (5.8) |
13 (39) |
39.4 |
99.3 |
95.8 |
| Malignant neoplasm |
32 (5.6) |
18 (56) |
56.3 |
98.9 |
96.5 |
| Heart failure |
26 (4.6) |
12 (46) |
46.2 |
99.1 |
96.7 |
| Intoxications |
24 (4.2) |
8 (33) |
33.3 |
98.9 |
96.2 |
| Dementia |
23 (4.0) |
10 (43) |
43.5 |
98.5 |
96.3 |
| Depression/anxiety |
20 (3.5) |
3 (15) |
15.0 |
98.8 |
96.9 |
| Orthostasis |
19 (3.3) |
9 (47) |
47.4 |
99.8 |
98.1 |
| Dehydration |
17 (3.0) |
9 (53) |
52.9 |
99.1 |
97.7 |
| Correct: primary ED diagnosis was identical with the gold standard diagnosis. Sensitivity, specificity, and accuracy were calculated relative to the gold standard diagnosis. Sensitivity: true positives/(true positives + false negatives). Specificity: true negatives/(true negatives + false positives). Accuracy: (true positives + true negatives) / (true positives + true negatives + false positives + false negatives). |
Discussion
In this study we found that less than half of patients presenting to the ED with NSCs were discharged from the ED with a correct diagnosis. Diagnoses were more often missed in women than in men. Moreover, the proportion of correct diagnoses increased from 46% to only 51% during hospitalisation. However, the twelve most frequent ED diagnoses showed high accuracy, probably owing to the large number of true negatives. For the same reason, the specificity was high. In contrast, sensitivity was low in all conditions. Even pneumonia, with the highest rate of correct diagnosis, was correctly identified in only 27 of 39 patients (69%).
The low rate of correct diagnoses in patients with NSC might be the result of various factors. As reported previously, atypical presentation of disease, the broad spectrum of underlying diagnoses and difficulties in history taking in an overcrowded ED present challenges for EPs, and may therefore explain the low rate of correct diagnoses [1, 3–5, 8, 12, 17, 18].
On the other hand, missed primary ED diagnoses were only rarely corrected at discharge. There were even patients whose correct initial diagnosis was subsequently changed to a faulty diagnosis. This is surprising, given the fact that workup is continued on the wards. Even though the average length of stay was 6 days, most patients were not given a more accurate diagnosis during this period. It is conceivable that the ward physicians were influenced by wrong diagnoses given by the EPs [19]. Another possible explanation is that in patients with NSCs, ward physicians are encouraged to initiate a number of supplemental tests and investigations owing to the broad spectrum of possible diagnoses, which might mislead them even more.
Diagnoses were significantly more often missed in women than in men. This is well known for other clinical situations, such as acute coronary syndrome and psychiatric diseases [6, 20–22]. Women are at a greater risk of suffering from frailty [6, 20, 22, 23], which is consistent with the greater prevalence of frailty in women in the present study. Because frailty was often missed in our patients, this might provide a possible explanation for the relatively large number of missed diagnoses in women. Moreover, UTIs were more frequently missed in women than in men. This may be due to the more nonspecific and generalised presentation of UTI in elderly women, and the low sensitivity and specificity of urinalysis in detecting UTI [24, 25].
Another possible explanation for the frequency with which UTI was missed in women was proposed by Webster [26], who demonstrated that UTIs are often mislabelled with the psychiatric diagnosis of somatisation disorder. The bias towards psychogenic explanations – particularly in conditions of obscure aetiology and nonspecific presentation – certainly affects both women and men; however, this seems to occur more frequently with female patients, and may lead to inappropriate treatment [21].
In our study, women were older than men, but there was no evident effect of age on the rate of correct diagnoses. Except in patients suffering from heart failure, it was observed that patients in whom the diagnosis was missed tended to be younger (around 80 years old). Thus, it may be speculated that diagnosing heart failure may be easier in very old people (around 90 years old), and that in very old patients, the presentation is more recognisable for EPs.
To our knowledge, this is the first prospective study that analyses the proportion of correct diagnoses in patients with NSC. The proportion of correct diagnoses in patients with specific complaints was assessed in a previous study at our ED, which showed that correct diagnoses were reached in 87% of patients [27]. This is in line with results from other studies in different settings in Europe [19, 28, 29]. In contrast to patients with NSCs, checklists and diagnostic algorithms are available for patients with specific complaints, and these have been shown to be useful in preventing diagnostic errors [30].
Our study had several limitations. Firstly, the characteristics of ED physicians and physicians working on wards were not assessed. Thus, the influence of factors such as the physician’s age and experience was not included in the analysis. Secondly, we assessed the outcome correct diagnosis, but not mortality. Thus, we are not able to determine the influence on mortality of making wrong diagnoses or of missing diagnoses. However, current quality standards in our healthcare system require a diagnosis for every patient seen in the ED. Moreover, Diagnosis Related Groups (DRGs) require a diagnosis to invoice hospitalised patients. Thus, correct diagnosis might be an interesting outcome, even though mortality was not assessed. Thirdly, a total of 114 patients were excluded because ER diagnoses were not available. This was due to the fact that ER diagnoses were written on paper and got lost. However, because these data were lost randomly, we do not expect a selection bias. Finally, this was a single centre study and our study population mainly consisted of elderly patients. Thus, our results cannot be generalised.
In conclusion, we have shown that establishing diagnoses in patients with NSC presenting to the ED is challenging. Further research is needed to find diagnostic tools for these patients.
Acknowledgement: We thank Dr. Rodney Yeates for language editing.
References
1 Nemec M, Koller MT, Nickel CH, Maile S, Winterhalder C, Karrer C, et al. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med. 2010;17:284–92.
2 Vanpee D, Swine C, Vandenbossche P, Gillet JB. Epidemiological profile of geriatric patients admitted to the emergency department of a university hospital localized in a rural area. European journal of emergency medicine: official journal of the European Society for Emergency Medicine 2001;8:301–4.
3 Chew WM, Birnbaumer DM. Evaluation of the elderly patient with weakness: an evidence based approach. Emerg Med Clin North Am. 1999;17:265–78, x.
4 Eliastam M. Elderly patients in the emergency department. Ann Emerg Med. 1989;18:1222–9.
5 Sanders AB, Morley JE. The older person and the emergency department. J Am Geriatr Soc. 1993;41:880–2.
6 Jarrett PG, Rockwood K, Carver D, Stolee P, Cosway S. Illness presentation in elderly patients. Arch Intern Med. 1995;155:1060–4.
7 Rutschmann OT, Chevalley T, Zumwald C, Luthy C, Vermeulen B, Sarasin FP. Pitfalls in the emergency department triage of frail elderly patients without specific complaints. Swiss Med Wkly. 2005;135:145–50.
8 Kulstad EB, Sikka R, Sweis RT, Kelley KM, Rzechula KH. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010;28:304–9.
9 Schiff GD, Hasan O, Kim S, Abrams R, Cosby K, Lambert BL, et al. Diagnostic error in medicine: analysis of 583 physician-reported errors. Arch Intern Med. 2009;169:1881–7.
10 Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005;165:1493–9.
11 Grossmann FF, Zumbrunn T, Frauchiger A, Delport K, Bingisser R, Nickel CH. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann Emerg Med. 2012;60:317–25 e313.
12 Nickel CH, Ruedinger J, Misch F, Blume K, Maile S, Schulte J, et al. Copeptin and peroxiredoxin-4 independently predict mortality in patients with nonspecific complaints presenting to the emergency department. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine 2011;18:851–9.
13 Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39:238–47.
14 Gilboy N TP, Travers DA, ed. Emergency Severity Index, Version 4: Implementation Handbook. Rockville: Agency for Healthcare Research and Quality; 2005.
15 Grossmann FF, Nickel CH, Christ M, Schneider K, Spirig R, Bingisser R. Transporting Clinical Tools to New Settings: Cultural Adaptation and Validation of the Emergency Severity Index in German. Ann Emerg Med. 2011;57:257–64.
16 Zhu W, (2010) Sensitivity, specificity, accuracy, associated confidence interval and ROC analysis with practical SAS implementations. [Accessed 14th November, 2010] http://www.nesug.org/Proceedings/nesug10/hl/hl07.pdf.
17 Nickel CH, Nemec M, Bingisser R. Weakness as presenting symptom in the emergency department. Swiss Med Wkly. 2009;139:271–2.
18 Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184:208–12.
19 Heuer JF, Gruschka D, Crozier TA, Bleckmann A, Plock E, Moerer O, et al. Accuracy of prehospital diagnoses by emergency physicians: comparison with discharge diagnosis. Eur J Emerg Med. 2012;19:292–6.
20 Lewis R, Lamdan RM, Wald D, Curtis M. Gender bias in the diagnosis of a geriatric standardized patient: a potential confounding variable. Acad Psychiatry. 2006;30:392–6.
21 Munch S. Gender-biased diagnosing of women’s medical complaints:contributions of feminist thought, 1970–1995. Women Health. 2004;40:101–21.
22 Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Cardiovascular Health Study Collaborative Research G. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sc. 2001;56:M146–56.
23 Safran DG, Rogers WH, Tarlov AR, McHorney CA, Ware JE. Gender differences in medical treatment: The case of physician-prescribed activity restrictions. Soc Sci Med. 1997;45:711–22.
24 Mody L, Juthani-Mehta M. Urinary tract infections in older women: a clinical review. JAMA. 2014;311:844–54.
25 Khasriya R, Khan S, Lunawat R, Bishara S, Bignall J, Malone-Lee M, et al. The inadequacy of urinary dipstick and microscopy as surrogate markers of urinary tract infection in urological outpatients with lower urinary tract symptoms without acute frequency and dysuria. J Urol. 2010;183:1843–7.
26 Webster DC. Interstitial cystitis: women at risk for psychiatric misdiagnosis. AWHONNS Clin Issues Perinat Womens Health Nurs. 1993;4:236–43.
27 Benedict M. Wert der klinischen Erstbeurteilung. Habil.-Schr. Med. Fak. Basel, 2000, Basel. German.
28 Arntz HR, Klatt S, Stern R, Willich SN, Beneker J. Are emergency physicians’ diagnoses accurate? Der Anaesthesist. 1996;45:163–70. German.
29 Berner ES, Graber ML. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121:S2–23.
30 Ely JW, Graber ML, Croskerry P; Checklists to reduce diagnostic errors. Acad Med. 2011;86:307–13.