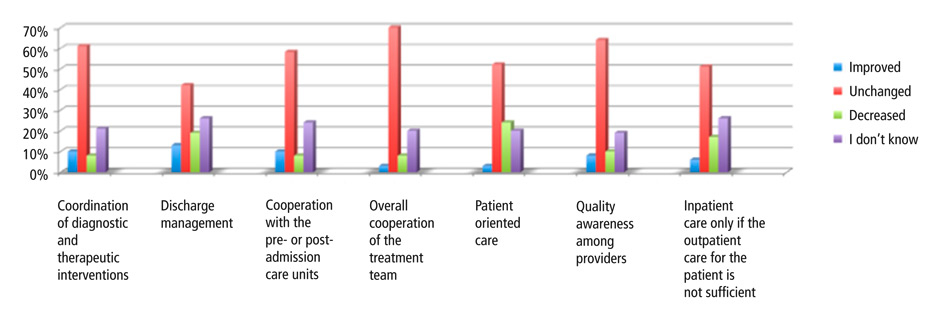
Figure 1
An increased focus on efficiency: change of items.
DOI: https://doi.org/10.4414/smw.2015.14080
In 2012 Switzerland introduced several changes in its hospital financing system, of which the transition from different cantonal reimbursement systems (e.g., daily rates, fee-for-service elements or the All Patients Diagnosis-Related Groups (APDRG)) to a country-wide use of a single newly developed DRG System, the SwissDRG, was the most discussed. SwissDRG was developed on the basis of the German DRG system; however, in the Swiss system future investments are to be financed through the earnings from patient care, which is a paradigm shift from the German and also from the former Swiss financing practice [1–3]. Further changes included a new cost split for hospital care between the cantons and the insurers (new 55:45 vs formerly 50:50) that will be fully implemented in 2017 with a transition period of 5 years, and the obligation for cantons to plan hospital capacity in their area by listing hospitals that meet their infrastructure, economic, and quality of care requirements. Furthermore, the new legislation forbids subsidies and deficit guarantee for hospitals from the cantons. All these changes can be expected to result in higher economic pressure on each hospital and increased competition for patients.
DRG-based prospective payments, which provide a fixed amount per patient based on diagnoses, procedures, and additional factors (such as age, severity of the condition and co-morbidities or complications), set incentives for hospitals and providers to treat patients in a cost-efficient way, by focusing on a patient’s leading symptoms (that form the main diagnosis as defined at discharge) and by assuring a timely work-up and discharge while keeping down expenses. This means that for physicians, specific conflicts of interest may arise, mainly in terms of the commitment to the patient’s interests and well-being on one side and the consideration of the economic interests of the hospital and the “requirement of cost-effective medicine” on the other [4]. (Although conflicts of interest do arise in other reimbursement systems as well, the situation has changed in Switzerland with regard to (1.) an increased emphasis on economic considerations, at least in public, non profit-oriented hospitals and (2.) the concrete pattern of incentives for over- or under-provision, which differs from fee-for-service or daily rate-based systems.) The persistence of such conflicts of interest can not only decrease job satisfaction and perceived autonomy of the physicians but can also lead to an impairment of quality and equity of health care [5–7].
A range of problematic potential consequences of DRG-based reimbursement have been projected early on, including “bloody exits”, case splitting, up-coding, and cherry picking of uncomplicated patients or those with diagnoses that come with a lucrative DRG code [8]. Monitoring of some relevant parameters, such as re-admission rates, seems not to have yielded an indication that quality of care has deteriorated in Switzerland with the introduction of DRGs [9]. However, there are two challenges to the assumption that everything is fine under DRGs: First, quality could be compromised in ways that are not picked up by standard measurement. Second, quality might not be affected because physicians hold up against the economic nudges and put their patients’ wellbeing first [6, 7].
Given that maintaining or improving quality and equity is a genuine concern to all health care systems, it would seem that thorough analyses of the effects of the DRG-based reimbursement system are considered urgently needed and highly desirable. Yet, so far there do not seem to be any monitoring tools in place that would address ethically relevant aspects in a comprehensive and sufficiently fine-grained way.
To fill this gap we studied the impact of DRGs on patient care and professional practice as perceived by physicians. In our study we focused on perceived or expected ethical concerns such as conflicts of interest undermining patient care, limitations of professional autonomy, discrepancies between physicians’ ethical standards and their real life practise, and implications on work motivation and job satisfaction. For this study we have been drawing on results of an analysis of ethical issues raised in the context of DRGs [5, 6, 10] and the results of an earlier quantitative study in 2011/12 (manuscript in preparation).
The study is embedded in a larger interdisciplinary research project “Assessing the Impact of DRGs on Patient Care and Professional Practice” (IDoC), supported by the Swiss National Science Foundation (SNSF). The purpose of the project was to develop and apply a set of tools to monitor ethical concerns physicians encounter in their daily clinical work, to identify problematic areas in delivery of health care to hospital patients and to explore perceived changes – both positive and negative – following the introduction of DRGs.
| Table 1:Demographic data (n = 382). | |
| Age mean ± SD | 37.5 ± 8.8 years |
| Years of clinical activity as a physician mean ± SD | 10.0 ± 7.7 years |
| Years worked in hospitals in which services were (at least in part*) billed according to DRGs mean ± SD | 4.1 ± 3.8 years |
| Gender | |
| Male | 55% |
| Female | 45% |
| Most prevalent specialties | |
| Internal medicine specialties | 30% |
| Surgical specialties | 23% |
| Anaesthesiology | 12% |
| Other | 35% |
| Position | |
| Assistant physician / resident | 46% |
| Senior physician / fellow | 33% |
| Chief physician or head of department | 20% |
| Other | 1% |
| Hospital | |
| Public | 85% |
| Privately owned | 11% |
| Not specified | 4% |
| Hospital size / level of care | |
| University hospital | 37% |
| Regional hospital with more than 9,000 patients per year | 44% |
| Other hospital with ≤9,000 patients per year | 16% |
| Not specified | 3% |
| * Before SwissDRG were introduced there was a great variety of reimbursement systems among Swiss hospitals including systems whose compensation was partially or fully based on DRGs. | |
We present data of a cross-sectional survey of physicians working in Swiss hospitals in 2013.
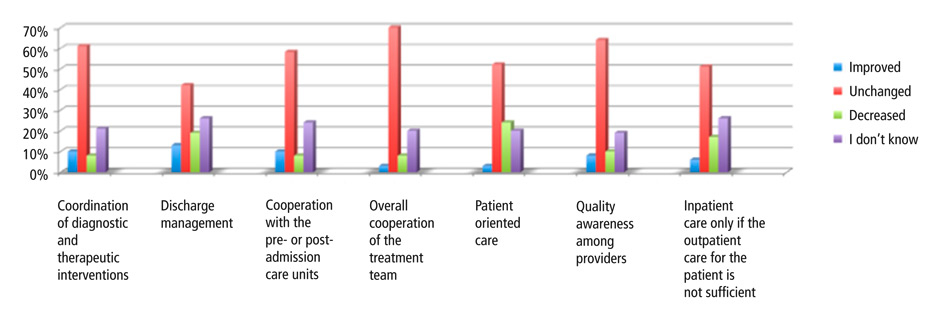
Figure 1
An increased focus on efficiency: change of items.
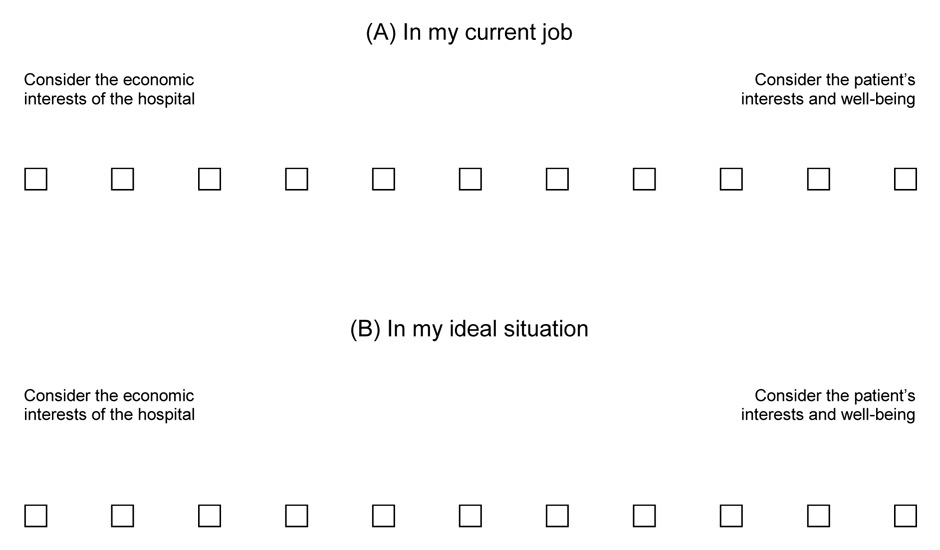
Figure 2
Patient interest vs economic considerations.
Various considerations play a role in the decisions you make during your everyday clinical work. On one hand you strive to achieve the best possible medical outcome for your patients and, on the other, you try to consider the economic interests of your department. Please estimate the relative weight of your considerations.
In total 1048 postal addresses were pulled from the register of the Swiss Medical Association (FMH), which comprised a random sample of all physicians working with inpatients in Swiss hospitals. From this sample we excluded psychiatrists and physicians working in outpatient clinics, as they work with a different reimbursement system, as well as pathologists and physicians working in laboratories, who are usually not directly involved with patients. We also excluded affiliated physicians (“Belegärzte”) not employed by the hospitals who have specific contracts bearing different potential conflicts of interest than the employed physicians.
Prior to the study we obtained ethical approval from the research ethics committees in those three cantons that required a review of the study.
The four page questionnaire consisted of 16 simple or multi-unit questions; it can be downloaded from www.ethik.uzh.ch/ibme/forschung/drg/publications.html in its original German version as well as in a French and English translation. The French version was used in the French- and Italian-speaking cantons. The questionnaire was divided into five parts: (A) personal data, (B) working environment and future perspectives, (C) economic pressures in everyday clinical work (ten scenarios that capture situations in which patient care might be compromised for economic reasons, table 3), (D) increased focus on efficiency (seven items on different dimensions of efficiency [table 4, fig. 1]), (E) ethical position of physicians (eight items on moral principles, plus an additional item covering the tension between clinical and economic considerations [table 5, fig. 2]). As an example figure 2 presents a question belonging to part (C).
This study was based on questions from an earlier survey of physicians in 2011/12 (data in preparation for publication). The current questionnaire includes items that have proven to work well during the first survey as well as refined questions and some new questions. By means of an analysis of relevant literature including similar surveys from Germany, own experiences of a team member in working with the German DRG system, and some preceding interviews of physicians, we developed a number of initial questions. These questions were scrutinised and selected with respect to its importance. It was piloted with 22 physicians. The questionnaire was developed in German and translated by a native French speaker. A member of our team translated the questionnaire back to German to disclose and resolve discrepancies.
The questionnaires were sent out by mail with a cover letter explaining the goals of the survey and the anonymous data processing (i.e. questionnaires did not contain any code for identification of the respondents and the presentation of the results did not allow conclusions about individuals or institutions). The envelope also contained a return envelope and a postcard in case the recipients wished to state that they did not work with inpatients, belonged to a group that was excluded from the survey, or did not want to participate in the study.
The questionnaire was first sent out in July 2013, with reminders following in August and September. To set an incentive for participation we used a total of 300 book vouchers worth 20 CHF each when sending out reminders.
Data is expressed as the mean and standard deviation (SD) for continuous variables and as the frequency for nominal variables. The overall direction towards increased or decreased time allocation for six activities was tested using the binomial test. With the same test statistical significance of the direction towards higher or lower efficiency of work processes under the new reimbursement system was examined. To compare the assessment of the ideal with the current work situation (see fig. 2) the sign test was used. A p-value ≤0.05 was considered statistically significant. SPSS Statistics 20 (IBM, Armonk, USA) was used for statistical analysis.
| Table 2:Changes in working time allocation for certain activities since the introduction of SwissDRG in 2012 (n = 382). | |||||||
| Activities | Significantly less | Less | Equal | More | Significantly more | Don't know | p-value* |
| Time for administrative tasks | 1% | 2% | 36% | 32% | 20% | 9% | p <0.0001 |
| Time for communication within the care team | 2% | 15% | 67% | 5% | 1% | 9% | p <0.0001 |
| Time for communication with patients and relatives | 4% | 21% | 64% | 2% | 0% | 9% | p <0.0001 |
| Time for own training / education | 5% | 22% | 63% | 1% | 1% | 9% | p <0.0001 |
| Time for training of young colleagues | 5% | 23% | 60% | 0% | 1% | 11% | p <0.0001 |
| Overtime | 1% | 1% | 53% | 28% | 8% | 10% | p <0.0001 |
| * Binomial test of the overall direction of changes in time allocation. | |||||||
| Table 3:Economic pressure in everyday clinical work (n = 382). | |||||||
| How often have you experienced this situation in the last 6 months in your hospital? | |||||||
| Situations in everyday clinical work | Currently I sense pressure in this respect | At least once a day | At least once a week | At least once a month | Less than once a month | Never | Question does not apply to me |
| (1) A measure useful to the patient was not executed because of cost-related reasons, or substituted by a less expensive and also less effective medical procedure. | 18% | 3% | 17% | 17% | 27% | 36% | – |
| (2) For a patient with various diagnostic and therapeutic options, a riskier option was chosen for cost reasons. | 5% | 1% | 4% | 5% | 14% | 65% | 11% |
| (3) A medical procedure was applied for economic reasons although it was not medically necessary. | 8% | 5% | 10% | 15% | 19% | 52% | – |
| (4) I decide for or against a medical intervention because management urged me to for economic reasons. If I could have decided in the interest of the patient, I would have chosen a different medical procedure. | 14% | 3% | 11% | 17% | 18% | 44% | 7% |
| (5) I attend to more patients than I am able to with due care. | 14% | 11% | 19% | 18% | 19% | 34% | – |
| (6) Certain patients are not admitted to the hospital because they represent a financial risk (e.g. multi-morbid patients; patients with a less lucrative DRG). | 7% | 1% | 3% | 4% | 12% | 65% | 13% |
| (7) Patients are discharged too early due to DRG-limited length of stay. | 12% | 4% | 13% | 14% | 19% | 36% | 13% |
| (8) Patients are not discharged although it would be medically justifiable, as the minimum length of stay has not yet been reached. | 11% | 6% | 15% | 13% | 16% | 35% | 15% |
| (9) To increase reimbursement, patients are admitted to hospital although a treatment as outpatients would be appropriate. | 12% | 4% | 14% | 14% | 16% | 36% | 14% |
| (10) For economic reasons, patients are admitted more than once, for a treatment that could have been completed in the first stay. | 8% | 2% | 7% | 15% | 17% | 40% | 17% |
| Table 4:An increased focus on efficiency (n = 382). | ||||||||||
| Current situation | Since the beginning of the year 2012 | |||||||||
| Very good | Rather good | Rather poor | Very poor | I don't know | Improved | Unchanged | Decreased | I don't know | p-value* | |
| > The coordination and/or sequence of diagnostic and therapeutic measures | 9% | 67% | 16% | 3% | 6% | 10% | 61% | 8% | 21% | p = 0.33 |
| > Discharge management | 8% | 59% | 19% | 4% | 11% | 13% | 42% | 19% | 26% | p = 0.037 |
| > Cooperation with the pre- or post-admission care units | 8% | 61% | 19% | 2% | 10% | 10% | 58% | 8% | 24% | p = 0.33 |
| > Overall cooperation of the treatment team | 14% | 71% | 8% | 1% | 6% | 3% | 69% | 8% | 20% | p = 0.003 |
| > Patient oriented care | 15% | 63% | 13% | 3% | 6% | 3% | 52% | 24% | 20% | p <0.0001 |
| > Quality awareness among suppliers | 13% | 68% | 12% | 3% | 5% | 8% | 64% | 10% | 19% | p = 0.33 |
| > Admission only if outpatient care for the patient is not sufficient | 16% | 54% | 15% | 3% | 12% | 6% | 51% | 17% | 26% | p <0.0001 |
| * Binomial test of the direction of change (improvement or decrease). | ||||||||||
We received 1048 addresses from the FMH database to form a representative sample. A total of 230 physicians were excluded for following reasons: 27 invalid mail addresses; 176 physicians claimed not to be working with inpatients anymore; 18 physicians, mainly psychiatrists, were not working with DRGs; and 9 were affiliated physicians. Thus the final study population consisted of 818 Swiss physicians working with inpatients. A total of 382 physicians filled in the questionnaire (response rate 47%). A total of 80% of the returned questionnaires were in German, and the remaining questionnaires were in French. This corresponds to the geographic distribution of addresses in German and French/Italian speaking cantons in the sample (81% vs 19%) we had received from the FMH. The socio-demographic characteristics of the sample are shown in table 1.
Of the 202 non-respondents, 34 physicians had indicated on the postcard that they did not want to participate in the study. In this subgroup, 47% were male and 50% female, their mean age was 38.7 ± 8.0 years. There were no significant differences between age and gender distribution between these non-respondents and study participants.
Overall, 32% of study participants assessed the quality of patient care in their department as very good and 60% as good. Only 6% of the respondents thought that the quality was poor, 2% thought it was very poor, and 1% did not know.
Asked about their job satisfaction in the last six months, 24% of the physicians were “very satisfied”, 59% “satisfied”, 15% “dissatisfied”, and 2% “very dissatisfied”. Additionally, 82% of those who were dissatisfied or very dissatisfied with their present working conditions were currently considering changing their job or reducing their working hours at the hospital because of their dissatisfaction, 12% were not considering that, and 6% did not know.
No one stated that their job satisfaction had improved since January 2012 because of the DRG-based hospital financing. The majority judged their job satisfaction had remained unchanged (56%), a considerable percentage reported a decrease (29%) and 15% did not feel qualified to make a statement.
We also asked physicians if there was enough time for communication between care team and physicians in their department. Half of the respondents agreed (53%), 19% strongly agreed, 19% disagreed 8% did not know and nobody strongly disagreed.
Table 2 shows the subjective assessment of study participants regarding changes in how they allocated their working hours for defined activities since the introduction of SwissDRG in 2012. Half of the physicians thought they spent more time on administrative tasks since the new hospital financing system had been introduced. In addition, 25% of the physicians said they had less time for communication with patients and relatives and for their own continuous education, as well as for the training of young colleagues. A third of the physicians stated they were working more overtime than before the introduction of DRG. All reported changes were statistically significant.
In this section we present ten different scenarios that refer to often discussed apprehensions or consequences of DRGs (table 3). Study participants were asked, had they experienced these scenarios in their hospital and/or had they sensed economic pressure in this respect over the past six months.
Almost two-thirds of physicians (64%) stated that at least once over the past six months a useful medical intervention was not carried out because of cost, or was substituted by a cheaper but less effective measure (situation 1). 18% indicated they currently felt pressure to act in this way. Situations 2 to 7 capture other aspects of compromised patient care: Exposing patients to unnecessary risks was seen by almost a quarter (23%) at least once in the past six months (situation 2), overtreatment and decisions against the patient’s interest for economic reasons (situation 3 and 4) by almost half (49%), work overload with inadequate level of diligence by 66% (situation 5), refusal of patients by 20% (situation 6), and too early hospital discharge by 49% (situation 7).
Beyond overtreatment the study revealed further forms of waste (delayed discharge; hospital admission for care that could have been delivered in outpatient setting; case splitting with repeated admissions; cf. situations 8 to 10 in table 3). Half of the study participants had experienced that patients were kept longer in the hospital only to reach the DRG-specific minimum length of stay at least once over the past six months. Additionally, 49% of respondents had seen patients being admitted to hospital although outpatient setting would have been appropriate (situation 9), and 42% of the respondents had experienced case splitting (situation 10).
Some physicians indicated that the questions did not apply to them. These physicians were likely not involved in admitting or discharging patients, such as anaesthetists, or were physicians working relatively autonomously regarding their clinical decisions (situation 4). The choice “does not apply to me” was not given for items which we considered as being encountered by all physicians treating inpatients (situations 1, 3 and 5).
In order to capture the projected positive consequences of DRGs, we dedicated a section of the questionnaire to effects on efficiency of work processes and on perceived relation of any changes following the introduction of DRGs (table 4, fig. 1).
Overall, efficiency was considered to be rather good by the majority of respondents. At the same time, respondents noted little improvement with DRGs; most considered the status quo unchanged. For some items – discharge management, cooperation of the treatment team, patient-oriented care, and hospital admission only for patients who could not be treated adequately in an outpatient clinic – the majority considered the situation unchanged or didn’t know and those who considered the situation worse under DRGs exceeded the number of those who saw an improvement.
Study participants were asked to assess the relevance of eight moral principles (A–H) that related to their work as physicians, and the extent to which they were able to comply with them in their daily work (see table 5). Primacy of the wellbeing of the patient (A), treatment according to best available standards (B), respect for patient autonomy (F) and treating all patients with equal care (G) stand out as being considered “very relevant” by most physicians (>80%). By contrast, only a third of the respondents rated the principle “As a physician I strive for cost-effective treatment so that everyone can receive medical care” as very important; half of the respondents rated this principle as “important”.
More than half of the study participants thought moral principles might at best be realised with limitations. This means that physicians cannot fully adhere to the moral principles they deem important in their own clinical work. Taking sufficient time to develop a good physician-patient-relationship, maintaining professional autonomy, good cooperation within the treatment team and heeding cost-efficiency in the interest of a sustainable public health system were considered to be challenging or impossible to implement by more than 75% of respondents.
To investigate the tension between two professional principles we asked the physicians to quantify the following two considerations in their everyday clinical decision-making (fig. 2): Striving to achieve the best possible medical outcome for their patients versus considering the economic interests of their department. We asked study participants to assign a value to both principles on an 11–point Likert scale (A) for their current job and (B) for their personal ideal situation. Mean value of the answers related to the current job was 5.5 (SD 2.4); slightly over the balance point of 5, meaning they gave economic considerations and their patients’ interests equal weight, with a small bias towards their patients’ interests. Mean value of the answers related to the ideal situation was 7.7 (SD 1.8) and therefore tended more towards patient interests.
| Table 5: Moral principles for physicians – relevance and realisability [percentages], n = 382. | ||||||||
| Principals | Relevance | Feasibility | ||||||
| Very important | Important | Less important | Unimportant | Easily realisable | Realisable with limitations | Difficult to realise | Completely unrealisable | |
| A) The health status of the patient is top priority for a physician’s action. | 87% | 12% | 1% | 0% | 38% | 56% | 5% | 2% |
| B) As a physician I treat my patients according to the highest current medical standards. | 82% | 16% | 2% | 0% | 41% | 53% | 5% | 1% |
| C) As a physician I take sufficient time to build a good relationship with my patients and take their psychosocial condition into account. | 64% | 31% | 4% | 1% | 14% | 51% | 31% | 4% |
| D) As a physician I am able to make independent decisions regarding the type and extent of services I offer to the patient based on medical criteria. | 51% | 45% | 5% | 0% | 23% | 61% | 14% | 3% |
| E) As a physician I strive for cost-effective treatment so that everyone can receive medical care. | 33% | 53% | 14% | 0% | 15% | 65% | 18% | 2% |
| F) As a physician I inquire about and respect the will of the patients. | 85% | 14% | 1% | 0% | 51% | 44% | 5% | 1% |
| G) As a physician I treat all my patients with equal diligence. | 81% | 17% | 2% | 0% | 44% | 47% | 7% | 2% |
| H) As a physician I am committed to good cooperation between all medical professions in patient care. | 58% | 37% | 5% | 0% | 20%* | 64%* | 15%* | 2%* |
| The total percentage may not equal 100 due to rounding. | ||||||||
This cross-sectional survey of physicians in Swiss hospitals showed that under SwissDRG conditions the general quality of patient care is perceived to be good or rather good and despite financial pressure, work satisfaction is (still) high; two findings that are consistent with other studies [11, 12]. However, our study identified a number of issues that might undermine the best possible quality, equity and efficiency of patient care in future.
A significant number of physicians have experienced situations in the recent past that indicate important impairments to patient care, such as looking after more patients than they are able to with due care, withholding an intervention that would have been useful or replacing it by a cheaper but less effective one, or discharging patients too early. However, there are not only certain forms of underprovision, but also elements of overprovision or waste, such as keeping patients in hospital for longer than medically required or treating them in hospital – rather than in an ambulatory setting.
These findings challenge the declared goals of SwissDRG to discourage unnecessary care and to promote an overall increase in efficiency of health care services [13]. We investigated seven aspects of efficiency – among them coordination of diagnostic and therapeutic procedures, discharge management, and cooperation of teams – and did not find any improvement. However, every third physician said that the level of patient oriented care has decreased, which is particularly deplorable given that patient-orientation is a marker of good quality health care and that it helps to avoid unnecessary cost. Half of the physicians spent more time in administrative tasks, one third reported more overtime, and one quarter dedicated less time to medical training of young colleagues and to their own continuous education. These factors may contribute to the finding that one out of three physicians who felt qualified to compare the situation pre and post introduction of DRGs, thought that their job satisfaction has decreased with DRGs, while not a single physician noticed an improvement.
In our study the random sample of physicians and the response rate of 47% enable a transfer of the results, the latter however limits the representativeness of the data. The gender distribution among study participants was comparable to the data of the Swiss Federal Statistics Office from 2011 (54% male and 46% female physicians working in hospitals) [14]. The mean age of the physicians working with inpatients was slightly younger as compared to the statistics 2012 of the Swiss Medical Association – FMH (43.1 years compared to 37.5 years in our sample) [15]. These are the only indications that we obtained a quite representative sample but one should consider that our target population excluded some physicians not working with DRGs or without making clinical decisions for patients, so the comparison of the demographic data with official statistics has limitations.
Another limitation is the subjective assessments of physicians that may depart from real effects. Some data, like the increase in overtime, may be verified from objective sources. Other findings are inherently subjective, such as the perceived gap between an ideal situation and the clinical reality. To explore such issues further, qualitative approaches would be a valuable addition. Our study is limited to a retrospective and subjective comparison of pre-post situations. Although another survey was performed just before the introduction of DRGs (manuscript in preparation), it differs in sampling, and due to its timing may not provide a genuine baseline that would allow for a proper pre-post comparison. Therefore no independent pre-data were available to compare directly to the data of 2013.
In 2011, 2012, and 2013, the Swiss Medical Association commissioned three surveys of physicians. Some of their data was comparable to ours [9, 12]. The answers to work satisfaction were similar (FMH versus our data in 2013): 22% vs 24% “very satisfied” and 60% vs 59% “satisfied”. This is important, as work satisfaction may in turn affect the ability to deliver high quality patient care. Similar to ours, the FMH study found an increase in overtime in 2013 compared to 2012 but no difference to 2011. Furthermore, the FMH study found an increase in administrative work – the mean time spent on medical documentation and reports rose from 86 to 104 minutes per day within two years. Compared to previous years the 2013 FMH survey yielded a lower number of physicians who stated that all diagnostic procedures needed to make a treatment decision were in fact performed; every third physician thought that patient care was compromised by high workload or time pressure and perceived attempts to transfer multi-morbid or chronically ill patients to other hospitals [9].
In hospitals fighting for economic survival, management could urge physicians to change their practice of medicine to cut cost, thus placing them in a strong conflict of interest [16, 17]. In the absence of a close and comprehensive monitoring system, such increased focus on economic parameters could come at the expense of the quality and equity of care provided. Even now some of our study participants reported pressure in varying respects and noted that they give economic considerations more weight compared to patients’ interests than they would like.
In Germany, the perspective of physicians on the introduction of the DRG system has been investigated by several studies [18, 19], among them a longitudinal study with physicians working in hospitals in Hesse within the WAMP project (Wandel in Medizin und Pflege im DRG-System, surveys carried out between 2004 and 2007) [20]. Similar to our study, some indications for a compromised quality of patient care were found, for example increased occurrences of lack of time, of burdensome decisions made by physicians, and of failure to complete the assigned workload as well as a decreased use of the best available interventions.
Many German physicians and experts are dissatisfied with the current state attributed to DRGs and to insufficient funding of the health care system, and some of them wish to abandon this reimbursement system [16, 21]. They claim that under the current DRG system hospitals do not have enough resources to pay for operating expenses, adapt innovations or invest in new infrastructure. A recent study supports this notion: The “Hospital Barometer” is an annual representative survey of German hospitals on behalf of the hospital operators of the German Hospital Institute (Deutsches Krankenhaus Institut). It showed that by 2013 more than half of the hospitals were making losses; compared to earlier years this number increased considerably (2011: 21%, 2012: 31%) [22–24]. Although there is still sufficient funding available for health care delivery in Switzerland and the issues seen in Germany may not materialise, it is important to be aware of issues that may arise if the level of funding is decreased.
If patients became more aware of the potential tension between economic considerations and the quality of care delivered to them, a loss of trust in the system and in physicians may result. Patients may question their physicians’ advice because they are uncertain whether their physician acts in their best interest or in the economic interest of the hospital. This point was made at a recent symposium “The doctor-patient relationship in the shadow of the market” in Berlin, where health experts stated that a system that over-stresses efficiency puts the physician-patient relationship at risk and eventually results in de-professionalisation of the medical profession [25].
There are very few physician surveys from other countries investigating the impact of the DRG system on patient care that our study could be compared to [26–28]. Only cross-sectional studies, but no longitudinal studies that would allow for pre-post comparisons, were found in the literature. A Norwegian study with 1298 physicians was conducted four years after the introduction of the DRG system in 2002. It found some indications that physicians assessed quality of medical work worse than before the reform and half of the physicians felt that the hospital reform had mainly had a negative impact on hospitals [26]. A study from the USA included 33 physicians working in hospital one year after introduction of the DRG system in the 1980s. Their responses and comments were dominated by complaints and criticisms aimed at efforts at cost-containment seen as potential threat to appropriate patient care and their own professional autonomy [28], a theme that has come up in our own study as well.
Each change of a hospital financing system needs to be monitored to assess if quality of health care was compromised and if core ethical values such as fair access to health care were guaranteed. A survey of health professionals should be a central component of such monitoring as well as linking such data to other administrative hospital data, patient data, and other studies with validated and established instruments allowing international comparisons. Despite the huge majority of Swiss physicians attesting the health care system as good quality there are some indications that quality could be seriously compromised if more economic pressure is put on physicians in future. The reported forms of under- and overtreatment need to be further investigated, and the conflicts of interest minimised through suitable governance and management strategies in hospitals. The physician questionnaire developed for our survey can help identify possible problem areas in clinical practise, thus contributing to further development of SwissDRG and to the ongoing evaluation of the most recent health care reform.
Acknowledgement:We are indebted to the participating physicians who provided the data. We would like to thank all the pilot study participants who provided comments to earlier versions of the questionnaire, the FMH for the provision of addresses, and Corine Mouton Dorey for the French translation of the questionnaire.
1 Busse R, Geissler A, Quentin W, Wiley M. European Observatory on Health Systems and Policies Series: Diagnosis-Related Groups in Europe. Available from: http://www.euro.who.int/en/about-us/partners/observatory/studies/diagnosis-related-groups-in-europe.
2 Brügger U. Impact of DRGs: Introducing a DRG reimbursement system: A literature review; Gesundheitspolitik SGf, editor. Bern, Switzerland: 2010.
3 Bundesgesetz über die Krankenversicherung (KVG) (Spitalfinanzierung). Available from: http://www.admin.ch/opc/de/official-compilation/2008/2049.pdf.
4 Swiss Medical Association. Standesordnung FMH. Available from: https://www.fmh.ch/ueber_fmh/rechtliche_grundlagen/standesordnung.html.
5 Fourie C, Biller-Andorno N, Wild V. Systematically Evaluating the Impact of Diagnosis-Related Groups (DRGs) on Health Care Delivery: A Matrix of Ethical Implications. Health Policy. 2014;115:157–64.
6 Wild V, Pfister E, Biller-Andorno N. Kriterien für die DRG-Begleitforschung aus ethischer Perspektive. Schweiz Arzteztg. 2009;90(40):1553–6.
7 Wild V, Pfister E, Biller-Andorno N. DRG: Ethik vs. Ökonomie? Bulletin SAMW. 2009;11–5.
8 Faller H, Grefe C. Geld oder Leben. Die Zeit. 2012;3930–3.
9 gfs.bern. Gute Patientenversorgung trotz administrativem Aufwand – punktuelle Probleme. Schlussbericht 2013. Available from: http://www.fmh.ch/files/pdf14/2013_12_20_FMH-Begleitstudie_Spitalfinanzierung_Schlussbericht_2013_D.pdf.
10 Wild V, Pfister E, Biller-Andorno N. Ethical research on the implementation of DRGs in Switzerland – a challenging project. Swiss Med Wkly. 2012;142w13610.
11 OECD. OECD Reviews of Health Systems: Switzerland 2011. Available from: http://www.oecd-ilibrary.org/content/book/9789264120914-en.
12 gfs.bern. DRG: Befürchtungen einer zunehmenden Bürokratisierung der Medizin. Schlussbericht. Available from: http://www.fmh.ch/files/pdf9/2012_01_04_Begleitstudie_SwissDRG_Langversion_D.pdf.
13 Swiss DRG AG. Aims. Available from: http://www.swissdrg.org/de/02_informationen_swissDRG/ziele.asp?navid=11.
14 Statistik Bfr. Eidgenössisches Departement des Innern EDI. BFS Aktuell. Krankenhausstatistik 2011 – Standardtabellen. Available from: http://www.bfs.admin.ch/bfs/portal/de/index/news/publikationen.html?publicationID=5104.
15 Kraft E, Hostettler S. 31 858 Ärztinnen und Ärzte garantieren die ärztliche Versorgung. Schweiz Arzteztg. 2013;94(12):453–7.
16 Simon M. Das deutsche DRG-System: Grundsätzliche Konstruktionsfehler. Dtsch Arztebl International. 2013;110(39):1782–6.
17 Gesundheit. Grunddaten der Krankenhäuser. Fachserie 12 Reihe 6.1.1. Available from: https://www.destatis.de/DE/Publikationen/Thematisch/Gesundheit/Krankenhaeuser/GrunddatenKrankenhaeuser.html.
18 Dreimal «Auswirkungen der DRGs»: Ähnliche und völlig unterschiedliche Ergebnisse und Bewertungen dreier Politikfolgen-Studien. Available from: http://www.forum-gesundheitspolitik.de/artikel/artikel.pl?artikel=1775.
19 Braun B, Buhr P, Klinke S, Müller R, Rosenbrock R. Pauschalpatienten, Kurzlieger und Draufzahler – Auswirkungen der DRGs auf Versorgungsqualität und Arbeitsbedingungen im Krankenhaus. Bern, Switzerland: Huber: 2010.
20 Braun B. Entwicklung der objektiven und subjektiven Arbeitsbedingungen von Krankenhausärztinnen und -ärzten im DRG-System. Available from: http://www.zes.uni-bremen.de/GAZESse/201001/20091211_BB_Laekh.pdf.
21 124. Hauptversammlung Marburger Bund: Fallpauschalensystem sofort korrigieren. Available from: http://www.marburger-bund.de/artikel/allgemein/pressemitteilungen/2013/marburger-bund-fallpauschalensystem-sofort-korrigieren.
22 Krankenhaus Barometer. Umfrage 2013. Available from: https://www.dki.de/service/publikationen.
23 Krankenhausbarometer. Umfrage 2012. Available from: https://www.dki.de/sites/default/files/publikationen/krankenhaus-barometer-2012.pdf.
24 Krankenhausbarometer. Umfrage 2011. Available from: https://www.dki.de/sites/default/files/publikationen/krankenhaus_barometer_2011.pdf.
25 Ankowitsch E. Arzt-Patient-Beziehung: Vertrauen über Jahrzehnte weggespart. Dtsch Ärztebl International. 2013;110(42):1940.
26 Aasland OG, Hagen TP, Martinussen PE. The 2002 hospital reform – physicians’ views. Tidsskr Nor Laegeforen. 2007;127(17):2218–21.
27 Patel K. Physicians and DRGs. Hospital management alternatives. Eval Health Prof. 1988;11(4):487–505.
28 Notman M, Howe KR, Rittenberg W, Bridgham R, Holmes MM, Rovner DR. Social policy and professional self-interest: physician responses to DRGs. Soc Sci Med. 1987;25(12):1259–67.
Funding / potential competing interests: The project was supported by a Sinergia grant (CRSII3_132786) from the Swiss National Science Foundation (SNSF), Bern, Switzerland. All authors declare that they have no competing interests.