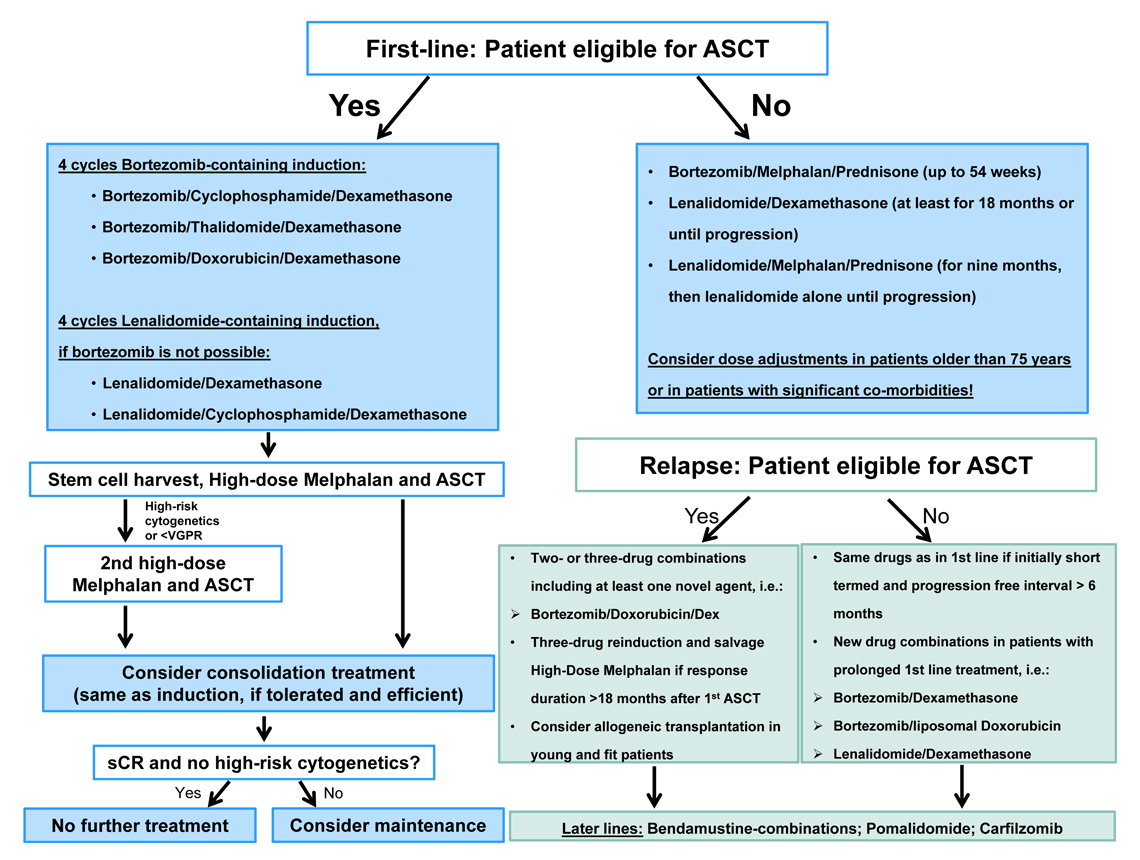
Figure 1
Treatment algorithm.
DOI: https://doi.org/10.4414/smw.2015.14100
Plasma cell myeloma is the second most common haematological malignancy and accounts for over 500 new cases per year in Switzerland [1]. In most patients, it develops from a precursor state called monoclonal gammopathy of undetermined significance (MGUS) which has a mean risk of progression to myeloma of 1% per year [2]. Plasma cell myeloma is a disease of the elderly population: most patients are diagnosed in their seventh life decade [3]. The clinical presentation may vary from asymptomatic disease detected by laboratory work-up (asymptomatic myeloma) to features dependent on the grade of the infiltration of bone, bone marrow or other organs by myeloma cells, and the amount of monoclonal protein produced by these cells. Patients may develop one or more of the four leading symptoms hyperCalcaemia, Renal failure, Anaemia and Bone disease, summarised as the acronym CRAB criteria. Bone involvement may cause progressive bone pain, which often leads to the diagnosis of the disease. Other common symptoms are fatigue, weight loss and recurrent infections due to an underlying immune dysfunction. Some patients with high levels of monoclonal protein may develop hyperviscosity symptoms, with vision impairment, neurological symptoms, or heart failure. The prognosis of the patients depends on numerous factors, including age, the stage at diagnosis and genetic features of the myeloma cells. Today, myeloma is considered an incurable disease, but long-term remissions have been documented after more intense treatment with high-dose chemotherapy and autologous stem cell transplantations (ASCT) in about 10%–20% of the patients [4, 5]. Some promising results have been achieved with allogeneic stem cell transplantation after reduced intensity conditioning (RIC-allo) in selected patient populations and prompted some experts to consider this a curative treatment approach in plasma cell myeloma [6, 7]. The current status regarding diagnosis, staging, response assessment and treatment of patients will be addressed in this article. In addition, new and emerging drugs and their expected impact on the treatment of myeloma patients will be discussed briefly.
For initial staging of patients with newly diagnosed myeloma the quantification of the monoclonal protein in serum and light chains in 24-hour urine is still recommended. In addition, quantification of immunoglobulins IgG, IgA and IgM, immunofixation and measurement of serum free light chains (FLC) with the corresponding ratio should be performed. The panel agrees that the clinical relevance of 24-hour urine analysis has decreased owing to the high sensitivity of available FLC assays (Freelite®, The Binding Site Group, Birmingham, United Kingdom). Serum levels of β2-microglobulin and albumin should be measured to define the stage according to the International Staging System (ISS). The degree of bone marrow infiltration should be assessed upfront, with a bone marrow biopsy and aspiration, including cytogenetic analysis and, if possible, multiparameter flow cytometry (MFC). MFC may help to detect minimal bone marrow involvement and could be useful for differential diagnosis between normal plasma cells, plasma cell myeloma, and other plasma cell disorders, as well as for risk stratification of patients with asymptomatic myeloma and MGUS [8, 9]. MFC may also be considered for the choice of consolidation or maintenance therapy, but it is, as yet, not standard outside of a clinical trial.
Plain radiographs are used for skeletal surveys to assess the nature of bone disease in plasma cell myeloma. Conventional radiographs are still considered the standard imaging technique for myeloma despite the low sensitivity compared with computed tomography (CT) and magnetic resonance imaging (MRI). Low-dose CT and whole-body MRI are more sensitive methods and may detect early active disease necessitating the initiation of myeloma treatment. Therefore, low-dose CT and MRI are the preferred and, thus, recommended imaging techniques for staging plasma cell myeloma. In addition, positron emission tomography-computed tomography (PET/CT) may provide additional useful information to guide therapy, but it is not standard in the diagnostic work-up of patients with plasma cell myeloma. Patients in whom it is unclear whether active disease is present or the extent of the disease is unclear (plasma cell myeloma or solitary plasmocytoma) may particularly benefit from this imaging modality. MRI has the advantage of detecting focal bone marrow infiltration even before bone lesions develop. New data are available which suggest that whole-body MRI may be used for risk stratification of patients with MGUS and asymptomatic/smouldering plasma cell myeloma. Moreover, the presence of more than one focal bone lesion as assessed by MRI studies may help to distinguish symptomatic plasma cell myeloma, considered suitable for treatment, from solitary plasmocytoma or asymptomatic/smouldering plasma cell myeloma[10–12].
Cytogenetic testing is especially recommended at diagnosis and in younger patients, as it allows for risk stratification and may thus facilitate individualised treatment decisions. Fluorescence in situ hybridisation (FISH) is the method of cytogenetic testing preferred over conventional cytogenetic analysis, since it enables a comprehensive analysis of proliferative as well as nonproliferative tumour cells. The myeloma panel should include testing for ploidy status, translocations t(4;14), t(14;16), t(11;14), t(14;20), chromosomal gains (1q gains), and deletions 13q and 17p [13]. For risk stratification in transplant candidates, at least t(4;14), t(14;16) and del17p should be determined. Recently, the combination of FISH data with other prognostic factors such as the ISS stage has been reported to allow precise risk stratification in daily practice [14]. In a recent meeting of the International Myeloma Working Group (IMWG), this combination has been proposed as the current standard for risk stratification and is therefore recommended [15].
The response assessment to treatment is being made based on the IMWG uniform response criteria (table 1) [16]. The panel agrees that the indispensable backbone of myeloma patient follow-up is the measurement of serum M-protein levels every 3 to 6 months. Immunofixation is indicated if the M-protein is no longer (reliably) detectable by serum electrophoresis to differentiate complete response (CR).
Accordingly, repeated serum FLC measurement is indicated if the initial M-protein is <10 g/l or not reliably measurable (provided that initially involved FLC levels are >100 mg/l and the FLC ratio is abnormal). Otherwise, the measurement of serum FLC levels is only useful to confirm a stringent complete response (sCR) in a patient fulfilling all other criteria for CR. The repeated measurement of Bence Jones protein in the 24-hour urine may be omitted in patients with available serum parameters and if renal function remains stable. Lytic bone lesions should be evaluated if clinically indicated with low-dose CT or MRI.
It has been shown in immunohistochemistry studies that negative immunofixation in serum combined with a normal serum FLC ratio are sensitive surrogate markers for a myeloma-free bone marrow [17, 18]. Despite the reported independent prognostic value of bone marrow examination, regular punctures may be therefore omitted and only be reserved for patients with nonsecretory or dedifferentiated myeloma, and for patients treated within clinical study protocols demanding regular bone marrow assessment. It has to be noted, however, that bone marrow assessment is required for documentation of sCR or CR after treatment according to the IMWG definition. Lacking the bone marrow data, at most only very good partial response (VGPR) can be ascertained. A practical approach would be to validate the achievement of sCR or CR with a bone marrow puncture after ASCT and subsequently to follow up the patient with serum parameters if he or she remains stable.
In addition, monitoring of the remission status in the bone marrow with more sensitive techniques such as polymerase chain reaction or MFC to detect minimal residual disease (MRD) after conventional treatment or after high-dose chemotherapy with autologous or allogeneic stem cell transplantation may identify a patient subset with a lower risk of relapse and a very favourable clinical outcome [19–21]. However, these examinations are not standard and await further validation in clinical trials.
| Table 1: International response criteria according to the International Myeloma Working Group [16]. | |
| Response | Criteria |
| sCR | CR plus normal FLC ratio AND no MRD in the bone marrow as evaluated by immunohistochemistry or MFC. |
| CR | Negative immunofixation in serum and urine AND disappearance of any soft tissue plasmocytoma AND ≤5% plasma cells in the bone marrow. |
| VGPR | Serum and urine M protein detectable by immunofixation but not electrophoresis OR ≥90% reduction of serum M protein plus urine M protein <100 mg per 24 hours. |
| PR | ≥50% reduction of serum M protein and reduction in 24-hour urinary M protein by ≥90% or to <200 mg per 24 hours. If the serum and urine M protein are not assessable, a ≥50% reduction in the difference between involved and uninvolved FLC levels is required in place of the M-protein criteria. If serum and urine M protein and serum FLC are not assessable, ≥50% reduction in plasma cells is required, provided that baseline bone marrow plasma cell percentage was ≥30%. ≥50% reduction in the size of soft tissue plasmocytoma is required if present at baseline. |
| SD | Not meeting criteria for CR, VGPR, PR or PD |
| PD | Requires one or more of the following: Increase of ≥25% from baseline in Serum M protein (absolute increase ≥0.5 g/dL) AND/OR Urine M protein (absolute increase ≥200 mg/24 hours) AND/OR In patients without assessable serum or urine M protein: difference between involved and uninvolved FLC (absolute increase >10 mg/dl Bone marrow involvement (absolute percentage ≥10%) New bone lesions or soft tissue plasmocytoma OR increase in size of known lesions/plasmocytomas Development of hypercalcaemia attributed to the myeloma |
| Clinical relapse | Requires one or more of the following: New soft tissue plasmocytomas or bone lesions Increase in size of existing plasmocytomas or bone lesions, defined as 50% (and at least 1 cm) increase Hypercalcaemia of >11.5 mg/dl [2.65 mmol/l] Decrease in haemoglobin of ≥2 g/dl [1.25 mmol/l] Increase in serum creatinine of 2 mg/dl or more [177 µmol/l] |
| Relapse from CR | Requires one or more of the following: Reappearance of serum or urine M protein by immunofixation or electrophoresis Development of ≥5% plasma cells in the bone marrow Appearance of any other sign of progression |
| CR = complete response; FLC = free light chains; PD = progressive disease; MFC = multiparameter flow cytometry; MRD = minimal residual disease; PR = partial response; SD = stable disease; sCR = stringent complete response; VGPR = very good partial response | |
MGUS has a risk of progression to plasma cell myeloma of 1% per year, and patients may thus benefit from adequate follow-up, depending on age and comorbidities. With the laboratory parameters serum M-protein (<15 g/l vs ≥15 g/l), type of immunoglobulin (IgG vs non-IgG) and serum FLC ratio (normal vs pathological), low-risk MGUS can be distinguished from high-risk MGUS, which has a substantially higher cumulative risk of progression. By using this initial stratification, patient monitoring can be optimised individually [22]. More recently, it has been shown that MFC and whole-body MRI may also be of value for risk stratification of newly diagnosed MGUS, but these techniques are not yet standard outside of clinical trials [10, 23, 24]. No data are currently available supporting pre-emptive treatment of patients with MGUS.
Patients with asymptomatic/smouldering plasma cell myeloma have a risk of progression to symptomatic plasma cell myeloma of up to 40% per year, depending on the presence of various risk factors, and are subject to closer follow-up [25]. Similarly to MGUS, various clinical parameters may be used for risk stratification. The amount of the serum M protein (<30 g/l vs ≥30 g/l), the number of bone marrow plasma cells (<10% vs ≥10%) and serum FLC ratio (normal vs pathological) should be used to establish a risk score for progression and allow optimised monitoring of the patients [22, 25]. In the recent update of the criteria for diagnosis of plasma cell myeloma, additional biomarkers have been defined in order to discriminate symptomatic plasma cell myeloma without evidence of typical end-organ damage from asymptomatic/smouldering plasma cell myeloma: a percentage of clonal bone marrow plasma cells of 60% or above, a serum FLC ratio above 100, or more than one focal lesion on MRI studies [12]. In addition, MFC may help to stratify patients better, but this needs to be further validated in clinical trials and is not yet standard [24]. Early treatment of high-risk asymptomatic/smouldering plasma cell myeloma with lenalidomide and dexamethasone with subsequent lenalidomide maintenance for 2 years has recently been shown to improve progression free and overall survival [26]. The panel agrees that no general recommendation for early treatment interventions can be yet formulated. However, on the basis of this new data on therapy and risk stratification, individualised treatment strategies for asymptomatic myeloma patients may emerge in the near future.
The goal of treatment is to achieve the best possible response (i.e. complete response) for a long period of time. This is usually achieved with an intensive treatment algorithm including induction, high-dose chemotherapy and autologous stem cell transplantation, consolidation and, in selected cases, maintenance therapy. The presence of risk factors and treatment toxicity need to be considered on an individual basis.
Three to four cycles of a three drug regimen are used in most cases. Based on the general correlation of depth of response and long-term outcome, the panel agrees that a bortezomib-based triple combination (bortezomib, cyclophosphamide, dexamethasone [VCD]; bortezomib, thalidomide, dexamethasone [VTD]; or bortezomib, doxorubicin, dexamethasone [PAD]) achieves better pre- and post-transplant responses than double therapy and should be preferred for induction therapy if possible [27–31]. Recently, a meta-analysis of all available phase III studies using bortezomib-based induction demonstrated significantly higher post-transplant CR/nCR rates (38% vs 24%, p <0.001), improved median progression free survival (PFS; 36 months vs 29 months, p <0.001), and 3-year overall survival (OS; 80% vs 75%, p = 0.04) as compared with non-bortezomib-based induction regimens. The benefit was noted across all patient subgroups including patients with high-risk cytogenetic features [32]. The VCD regimen, one of the most frequently used induction regimens in Switzerland, is currently being evaluated in the ongoing international phase III study EMN-02 by the European Myeloma Network (clinicaltrials.gov identifier: NCT01208766).
Equal efficacy has been demonstrated for subcutaneously and intravenously applied bortezomib in the relapsed setting [33]. Although no randomised trial proved equivalent activity in the first-line setting, many centres implemented the subcutaneous administration of bortezomib on a routine basis regardless of the treatment line, and this application route is also being increasingly incorporated into prospective clinical studies.
In case of contraindications (i.e. neuropathy) for bortezomib treatment, lenalidomide-based combinations should be used [34, 35]. A possible triple combination is lenalidomide, cyclophosphamide and dexamethasone (RCD) [36]. The treating physician should be aware of the potential adverse impact on the ability to collect stem cells after prolonged lenalidomide treatment. Therefore, early contact with a transplantation centre and stem cell mobilisation within the first four treatment cycles is recommended [37, 38]. Bortezomib has recently been approved for induction therapy in Switzerland, in contrast to lenalidomide. Nevertheless, the treating physician has to apply to the respective health insurance provider for cost coverage of either drug before start of treatment.
High-dose chemotherapy (HDT) with melphalan followed by autologous stem cell transplantation (ASCT) is still considered the consolidation treatment of choice for patients who are eligible (age <65–75 years). The goal is to improve the quality of response and achieve a sustained CR, as this has been reported to correlate with improved survival [39, 40]. The introduction of highly active antimyeloma agents has markedly improved the results in the transplant and nontransplant settings, and ongoing studies are currently challenging the classical strategy of upfront HDT plus ASCT by using continued sequential treatment with new drug combinations. Two very similar phase III studies use four cycles of lenalidomide and low-dose dexamethasone (Rd) for induction and compare lenalidomide-containing regimens with tandem high-dose melphalan (MEL200) as consolidation. In one study, patients received six cycles of lenalidomide, melphalan and prednisone (MPR) and in the other study six cycles of lenalidomide, cyclophosphamide and dexamethasone (RCD) for consolidation. The PFS was markedly better in patients after tandem auto-transplant compared with patients who received MPR consolidation (median PFS 43 months vs 22.4 months, p <0.001) or RCD consolidation (2-year PFS 72% vs 61%, p = 0.02). In addition, OS was also improved in the former trial (4-year OS 82% vs 65%, p = 0.02). These two studies suggest that HDT with subsequent ASCT still has an independent impact on patient outcome, despite the availability of new compounds, and remains the standard of care in the first-line setting [41, 42]. A recent report suggests that tandem transplantation may improve outcome in patients with advanced stage (ISS III), unfavourable cytogenetic features (t(4;14), del17p) or suboptimal response to bortezomib induction therapy (i.e. not achieving a CR) when compared with a single transplant [43]. In particular, the presence of at least two adverse risk factors strongly favoured the use of tandem transplantation. However, these data have to be interpreted with caution owing to the retrospective nature of the analysis. Therefore, single transplant with melphalan 200 mg/m2 (MEL200) remains the standard of care in Switzerland, but a second transplantation within 3–6 months should be considered in high-risk patients or patients not achieving at least a VGPR after the first transplant [44–46]. In patients older than 65 years or with impaired kidney function the dose of melphalan may be reduced to 100–140 mg/m2 (MEL100/140).
Eligibility for transplantation is assessed individually based on organ function and patient age. Patients up to 65 years are considered eligible for high-dose treatment, but older patients up to 75 years with good performance status are also increasingly offered transplantation. Excellent outcomes with regard to response and survival have been reported recently in patients over 65 years of age with a bortezomib containing triple-combination as induction, followed by tandem high-dose therapy with a reduced melphalan dose (100 mg/m2, MEL100) and subsequent ASCT, followed by lenalidomide-containing consolidation and maintenance until progression [31].
Convincing data have emerged supporting the introduction of short-term chemotherapy consolidation after ASCT to improve depth and duration of response.
In two phase III studies, VTD was compared with TD as consolidation, and single-agent bortezomib consolidation was compared with no consolidation. All patients benefited from consolidation with bortezomib, and the improvement of response was particularly evident in patients who did not reach at least VGPR after ASCT [28, 47, 48].
In the placebo-controlled phase III study IFM-2005–02 which primarily evaluated maintenance therapy with low-dose lenalidomide (10–15 mg daily) until progression, all patients received additional consolidation after ASCT with two cycles of lenalidomide at a dose of 25 mg at days 1–21 of a 28-day cycle. The rate of CR or VGPR was improved from 58% before to 69% after consolidation (p <0.001). In addition, response rates were further improved by the maintenance treatment (p = 0.009) as compared with placebo [49]. Based on these results, patients with contraindications for treatment with bortezomib may be considered for two cycles of lenalidomide for consolidation therapy.
The outcome of two ongoing phase III studies – the European EMN-02 and the American Blood and Marrow Transplant Clinical Trials Network (BMT CTN) 0702, both using bortezomib, lenalidomide and dexamethasone for consolidation – have to be awaited before consolidation therapy can be considered the standard of care. Based on all available data thus far, the use of bortezomib- or lenalidomide-containing consolidation, ideally the same regimen successfully used for induction, initiated within the first three months after ASCT, should be considered in patients with less than CR after ASCT.
(a) Bortezomib-based maintenance
Two phase III studies evaluated bortezomib as maintenance treatment after ASCT and three phase III studies are available for lenalidomide maintenance therapy.
The Dutch-Belgian Haemato-Oncology Cooperative Group (HOVON) and the German Multicentre Myeloma Group (GMMG) reported results of a study that used bortezomib-containing triple therapy (PAD) for induction and bortezomib alone as maintenance treatment for two years after single or tandem transplantation, compared with VAD induction and thalidomide maintenance for two years after ASCT. This design was developed to assess sustained bortezomib treatment during first-line therapy, as no second randomisation was planned after ASCT. Higher response rates and improved progression free and overall survival were achieved with bortezomib treatment. Patients with myeloma-related renal failure and/or del(17p) mutations seemed to benefit most from the prolonged bortezomib treatment. Although not a preplanned analysis owing to the lack of statistical power, patients receiving tandem ASCT in German centres had longer OS as compared with single transplanted patients in Dutch and Belgian centres (p = 0.03), but additional comparative subgroup analyses have not been performed in this context. The main adverse event was neurotoxicity, but discontinuation of bortezomib due to adverse events was necessary in only 11% of the patients as compared with 30% of patients receiving thalidomide [28, 50].
(b) Lenalidomide-based maintenance
A study conducted by the Cancer and Leukaemia Group B (CALGB) randomised patients after completion of induction chemotherapy and single ASCT to lenalidomide maintenance at a dose of 10–15 mg daily until progression or to no maintenance. Patients without progression treated in the placebo arm could cross over to lenalidomide during the follow-up period. Assessment of cytogenetic features was not mandatory and no data regarding cytogenetics have been reported. The median time to progression was improved from 27 months to 46 months (p <0.001) with lenalidomide maintenance. Patients without CR after ASCT seemed to benefit most from lenalidomide maintenance with regard to time to progression. OS was also improved in lenalidomide-treated patients (3-year OS 88% vs 80%, p = 0.03). Interestingly, in a subgroup analysis there was a greater difference in time to progression (p = 0.06) and OS (p = 0.03) in patients with lenalidomide maintenance who had already received lenalidomide as induction treatment, suggesting a positive impact on survival with a strategy of sustaining the exposure to the same agent during first line-treatment. A higher rate of second primary malignancies (SPM) was seen for lenalidomide-treated patients (7.8% vs 2.6%). More hematological and nonhematological adverse events were observed with lenalidomide, and treatment discontinuation was necessary in 10% of the patients [51].
One study conducted by the Intergroupe Francophone du Myélome (IFM) – the outcome of two cycles of lenalidomide consolidation therapy was discussed above – showed a marked improvement of PFS from median 23 months to 41 months (p <0.001) with lenalidomide maintenance until progression. This benefit in PFS was seen across all patient subgroups, including myeloma stage and type, cytogenetic profile, induction regimen chosen, number of ASCTs received, and response at randomisation. After documenting an increased SPM risk in the lenalidomide group during the follow-up period with an incidence of 3.1 versus 1.2 per 100 patient years (p = 0.002), lenalidomide was stopped in all patients in accordance with the recommendation of the Independent Data Monitoring Committee. Although a marked difference in PFS was noted, OS was not different between the two treatment arms [49]. One possible explanation for this finding may be the high survival probability of all patients as a result of the intensive treatment strategy pursued, including the use of bortezomib induction in half of the patients, induction reinforcement with polychemotherapy, tandem autotransplant in patients with less than VGPR after the first ASCT, and two cycles of consolidation with lenalidomide before randomisation. An updated analysis suggests a shorter survival after progression under maintenance with lenalidomid, eventually caused by adverse impacts on the myeloma clone [52].
One phase III study comparing MPR consolidation with tandem autotransplantation (as discussed above), also tested the value of lenalidomide maintenance with a bifactorial 2x2 design. After completion of MPR consolidation or tandem autotransplantation, respectively, patients were randomised to receive lenalidomide maintenance or no maintenance at all. The patients receiving lenalidomide until progression had a significantly improved progression free survival (median PFS 42 months vs 22 months, p <0.001) [42, 53].
Based on trials performed on maintenance, the panel agrees that maintenance therapy with lenalidomide or bortezomib cannot be considered standard of care yet, but may be considered for patients on an individual basis based on the underlying risk profile and response to treatment. High-risk patients may benefit most from prolonged therapy with bortezomib for 2 years. It has to be taken into account that the optimal duration of maintenance therapy with lenalidomide has not yet been defined, in particular considering the possible SPM risk. Therefore, maintenance therapy with low doses of lenalidomide (10–15 mg daily) should not be administered for more than 2 years. Maintenance treatment should be initiated within 3 months after ASCT.
The concept of high-dose chemotherapy with autologous stem cell transplantation followed by reduced intensity conditioning with allogeneic stem cell transplantation (auto/allo) has been evaluated in a few studies, with ambiguous results. Two recently published meta-analyses of all available data report that an auto/allo approach may achieve higher response rates with the cost of higher treatment related mortality rates than double autotransplantation, but without improving survival [54, 55]. This result holds true also for patients with high-risk features such as adverse cytogenetic abnormalities [55]. One recent update of a large prospective study comparing tandem auto/RIC-allo with tandem auto showed an improved long-term outcome regarding PFS and OS after auto/RIC-allo [6]. The panel agrees that allogeneic transplantation should not be included within the routine standard first-line treatment for myeloma patients and should be offered only to highly selected patients as first-line treatment, ideally within clinical study protocols.
The goal of treatment is to achieve the best response possible for a long period of time, balancing treatment-related toxicity against quality of life. This is usually achieved by a prolonged treatment (up to 74 weeks) and dose adjustments if necessary.
Patients not considered eligible for high-dose melphalan are usually treated with regimens incorporating novel agents. One large phase III trial added bortezomib to MP (VMP), and demonstrated a marked improvement of response, PFS and OS with the triplet combination (VISTA trial). Patients received nine 6-week cycles of VMP or MP. After a median follow-up time of 5 years, median OS was improved from 43.1 to 56.4 months by the addition of bortezomib (p <0.001). The survival benefit was seen across all prespecified subgroups, including patient age over 75 years, renal impairment and stage III disease. Importantly, the survival benefit was maintained after VMP was stopped, and despite the various salvage treatments subsequently administered to relapsing patients. The OS benefit could not be balanced by salvage treatment with bortezomib in MP-treated patients, highlighting the importance of upfront administration of bortezomib [56].
One study evaluated bortezomib-based induction combined with bortezomib-based maintenance therapy. In a study using a bifactorial 2x2 design, the PETHEMA group compared six 6-week cycles VMP with six 6-week cycles VTP (bortezomib, thalidomide, prednisone) induction (first randomisation) and bortezomib/thalidomide maintenance with bortezomib/prednisone maintenance for up to three years (second randomisation). In both arms, patients received twice weekly doses of bortezomib in the first cycle only, to achieve rapid tumour reduction. In the following cycles bortezomib was administered only once weekly to reduce toxicity and avoid early treatment discontinuation. No differences were seen between the treatment arms regarding response rate, PFS and OS for both the induction and the maintenance therapy period. Patients treated with VTP experienced significantly more toxicities (p = 0.01) and discontinued treatment more frequently (p = 0.03) compared with VMP. Importantly, the rate of neurological and gastrointestinal toxicities with the weekly bortezomib schedule was markedly lower compared with the data reported in the VISTA trial, despite similar efficacy. Moreover, maintenance therapy improved the CR rate of the overall patient population from 24% after induction to 42%, which is higher than the 30% CR rate reported in the VISTA trial. In addition, 22% of the patients achieved also an immunophenotypic remission (MRD negativity) with a 3-year PFS rate of 90% [21].
Several randomised studies have demonstrated the advantage of thalidomide combined with melphalan and prednisone (MPT) over the classical MP with regard to response and PFS, but with conflicting results regarding OS. A meta-analysis based on the individual data of all 1,685 patients included demonstrated a highly significant increase of median OS from 32.7 months to 39.3 months (p = 0.004) by the addition of thalidomide to MP. No benefit for MPT was seen in frail patients and in patients with cast nephropathy [57].
A recent retrospective case-match analysis compared VMP with MPT in newly diagnosed elderly myeloma patients and observed an advantage for VMP in terms of CR rates (21% vs 13%, p = 0.007), median PFS (33 vs 23 months, p <0.001), and median OS (80 vs 45 months, p <0.001). The benefit was seen across all subgroups except in patients older than 75 years [58].
One randomised study assessed the impact of adding lenalidomide to MP as first-line treatment (MPR). Induction treatment was administered over 9 months in all patients (nine 4-week cycles). Importantly, lenalidomide was given in a low dose of 10 mg daily from start of induction. In a third treatment arm, patients received additional lenalidomide maintenance therapy after MPR induction until progression (MPR-R). Both MPR-R and MPR resulted in higher response rates compared with MP (77% and 68% vs 50% for MP, p <0.001 and p = 0.002, respectively), only treatment with MPR-R significantly improved median PFS compared with either MPR alone or MP alone (31 months vs 14 months vs 13 months, p <0.001). The survival advantage was observed only in patients up to 75 years of age, whereas older patients did not benefit from lenalidomide. Interestingly, the use of lenalidomide during induction alone did not result in a statistically significant improvement of PFS compared with MP [59]. These data highlight that mainly the prolonged treatment with lenalidomide is able to further improve patient outcome after completion of the induction period.
One study has been reported that evaluated lenalidomide in combination with high-dose dexamethasone (RD) or low-dose dexamethasone (Rd). Lenalidomide was administered at a dose of 25 mg daily for 3 weeks of each 4-week cycle; high-dose dexamethasone consisted of 480 mg and low-dose dexamethasone of 160 mg per cycle. Treatment could be continued until disease progression. The high-dose dexamethasone arm achieved higher OR rates (79% vs 68%, p = 0.008), but OS rate at 1 year was significantly higher with the low-dose dexamethasone combination (96% vs 87%, p = 0.0002), because of higher toxicities and treatment-related mortality with RD [34]. Thus, lenalidomide combined with low doses of weekly dexamethasone is the better tolerated and preferred regimen.
The FIRST trial compared lenalidomide plus low-dose dexamethasone until progression (Rd) with lenalidomide plus low-dose dexamethasone for 18 months (Rd18) or MPT for 18 months. Continuous lenalidomide plus low-dose dexamethasone until progression showed improved PFS compared with MPT and Rd18 (25.5 vs 21.2 versus 20.7 months; Rd vs MPT, p = 0.00006) and improved 4-year OS compared with MPT (59.4% vs 51.4%, p = 0.0168). All subgroups benefited from continuous lenalidomide plus low-dose dexamethasone. Haematological and nonhaematological toxicities were as expected. No increased risk of secondary primary malignancies was observed with continuous lenalidomide plus low-dose dexamethasone. Rd until progression is another treatment option for elderly patients, especially in the case of pre-existing peripheral neuropathy or strong preference of an oral therapy [60]. Selected regimens for either first or later lines of therapy are shown in table 2.
In patients older than 75 years or younger patients with significant comorbidities, upfront treatment dosage should be carefully and individually adapted, since excessive toxicity may result in therapy-related deaths and treatment interruption, and may consequently negatively affect survival [61]. The panel agrees that the dose of the most relevant antimyeloma agents may be modified in accordane with existing recommendations (table 3).
| Table 2: Selected regimens. | |||
| Regimen | Doses | Schedule | Setting |
| VCD (clinicaltrials.gov: 01208766) | Bortezomib 1.3 mg/m2 i.v./s.c. d1,4,8,11 Cyclophosphamide 500 mg/m2 i.v. d1, 8 Dexamethasone 40 mg p.o. d1,2,4,5,8,9,11,12 | Repeated every 21 days | First line pretransplant |
| VTD (27) | Bortezomib 1.3 mg/m2 i.v./s.c. d1,4,8,11 Thalidomide 200 mg p.o. daily Dexamethasone 40 mg p.o. d1–4 and 9–12 | Repeated every 28 days | First line pretransplant |
| Rd (34) | Lenalidomide 25 mg p.o. d1–21 Dexamethasone 40 mg p.o. d1,8,15,22 | Repeated every 28 days | First line pre- or non-transplant; Relapsed/refractory |
| RCD (35) | Lenalidomide 25 mg p.o. d1–21 Cyclophosphamide 300 mg/m2 d1,8,15 Dexamethasone 40 mg p.o. d1,8,15,22 | Repeated every 28 days | First line pretransplant |
| PAD (28) | Bortezomib 1.3 mg/m2 i.v./s.c. d1,4,8,11 Doxorubicin 9 mg/m2 i.v. d1–4 Dexamethasone 40 mg p.o. d1–4, 9–12, 17–20 | Repeated every 28 days | First line Pretransplant; reinduction before salvage ASCT |
| VD (106) | Bortezomib 1.3 mg/m2 i.v./s.c. d1,4,8,11 Dexamethasone 40 mg p.o. d1–4 (all cycles) and 9–12 (cycles 1 and 2) | Repeated every 21 days | First line pretransplant |
| MPT (107) | Melphalan 0.25 mg/kg p.o. days 1–4 Prednisone 2 mg/kg p.o. days 1–4 Thalidomide 100–400 p.o. daily | Repeated every 6 weeks | First line nontransplant |
| VMP (21) | Bortezomib 1.3 mg/m2 i.v./s.c. d1,4,8,11,22,25,29,32 (cycle 1); or d1,8,15,22 (cycle 2+) Melphalan 9 mg/m2 p.o. days 1–4 Prednisone 60 mg/m2 p.o. days 1–4 | Cycle 1: 6 weeks From cycle 2 on: repeated every 5 weeks | First line nontransplant |
| Pom Dex (77) | Pomalidomide 4 mg/day p.o. d1–21 Dexamethasone 40 mg p.o. d1,8,15,22 | Repeated every 28 days | Relapsed/refractory |
| i.v. = intravenously; p.o. = per os; s.c. = subcutaneously. | |||
| Table 3: Recommended dose modifications for elderly patients according to Palumbo and Anderson [61]. | |||
| Drug | Age <65 year | Age 65–75 years | Age >75 years |
| Dexamethasone | 40 mg/day p.o. days 1–4, 15–18 every 4 weeks; or 40 mg/day p.o. given on days 1, 8, 15, 22 every 4 weeks | 40 mg/day p.o. on days 1, 8, 15, 22 every 4 weeks | 20 mg/day p.o. on days 1, 8, 15, 22 every 4 weeks |
| Melphalan | 0.25 mg/kg p.o. on days 1–4 every 6 weeks | 0.25 mg/kg p.o. on days 1–4 every 6 weeks; or 0.18 mg/kg given p.o. on days 1–4 every 4 weeks | 0.18 mg/kg p.o. on days 1–4 every 6 weeks; or 0.13 mg/kg given p.o. on days 1–4 every 4 weeks |
| Cyclophosphamide | 300 mg/m2 p.o. on days 1, 8, 15, 22 every 4 weeks | 300 mg/m2 p.o. on days 1, 8, 15, every 4 weeks; or 50 mg/day p.o. on days 1–21 every 4 weeks | 50 mg/day given p.o. on days 1–21 every 4 weeks; or 50 mg every other day p.o. on days 1–21 every 4 weeks |
| Thalidomide | 200 mg/day p.o. continuously | 100–200 mg/day p.o. continuously | 50–100 mg/day p.o. continuously |
| Lenalidomide | 25 mg/day p.o. on days 1–21 every 4 weeks | 15–25 mg/day p.o. on days 1–21 every 4 weeks | 10–25 mg/day p.o. on days 1–21 every 4 weeks |
| Bortezomib | 1.3 mg/m2 i.v. or s.c. on days 1, 4, 8, 11 every 3 weeks | 1.3 mg/m2 i.v. or s.v. On days 1, 4, 8, 11 every 3 weeks; or 1.3 mg/m2 i.v. or s.c. on days 1, 8, 15, 22 every 5 weeks | 1.0–1.3 mg/m2 i.v. or s.c. on days 1, 8, 15, 22 every 5 weeks |
| p.o., per os; i.v., intravenously; s.c., subcutaneously. | |||
Treatment of relapsed and/or refractory myeloma aims at reinducing a response and at maintaining it for as long as possible. As in first-line treatment, various treatment strategies may be considered according to the individual patient situation, such as the use of new drugs or a rechallenge with already administered regimens, or even salvage autologous or allogeneic transplantation.
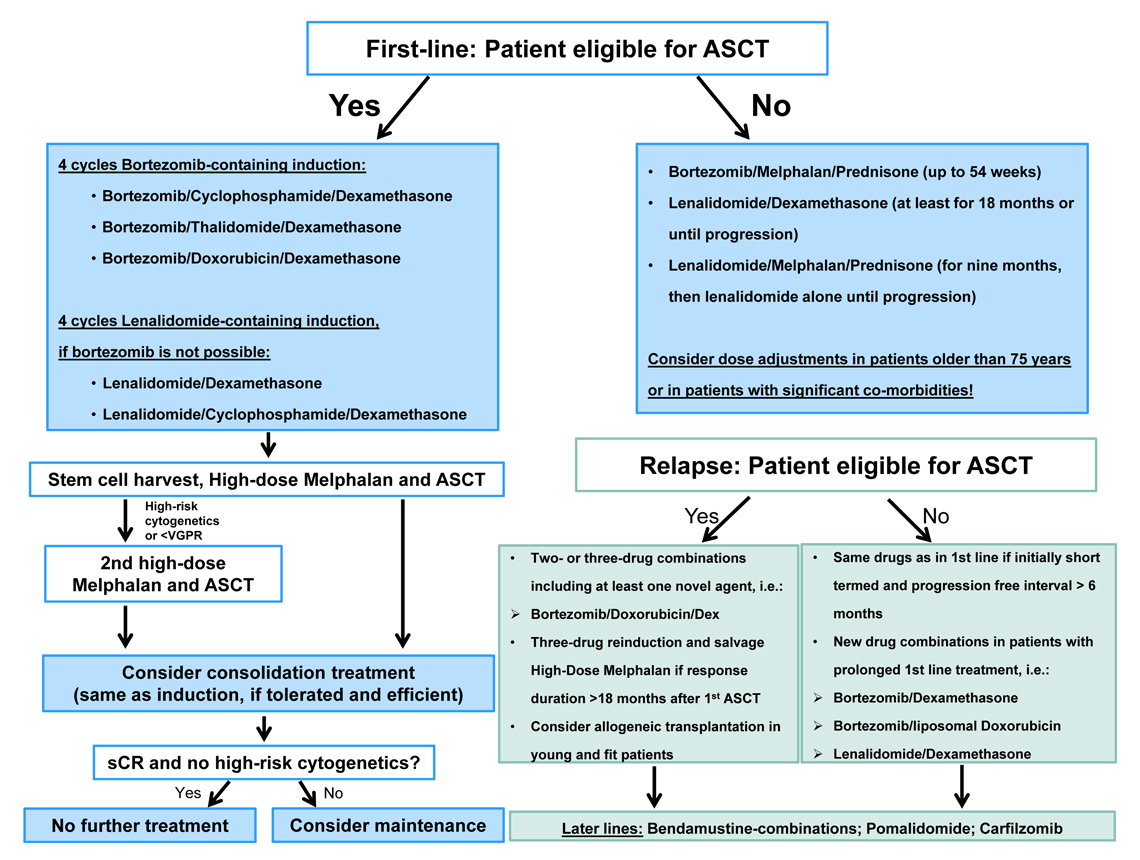
Figure 1
Treatment algorithm.
Unfortunately, the vast majority of successfully treated cases of plasma cell myeloma will relapse. The treatment approach is based on duration of the first-line therapy, the level and duration of the first remission, age and comorbidities of the patient and the clinical presentation at the onset of relapse [62]. Criteria for relapse and disease progression are shown in table 1 [16].
Transplant-ineligible patients who experienced remission lasting at least 6 months may be retreated with the drugs used in first-line therapy, especially when the initial treatment was of short duration and stopped after achieving the best response. In patients with prolonged first-line treatment new drug combinations should be preferred.
Transplant-eligible patients not transplanted during first-line therapy can benefit from high-dose melphalan plus ASCT in second line after reinduction treatment. For patients who experienced a remission of at least 18-24 months after the first autologous transplant a second, consolidating autologous transplant after induction therapy is generally proposed [63–66].
Two or three drug combinations including at least one novel agent are preferred for reinduction. Approved drug combinations in this setting are bortezomib/dexamethasone and lenalidomide/dexamethasone. The addition of an immunomodulatory drug (IMi)D or pegylated liposomal doxorubicin to bortezomib/dexamethasone is another option [67–69]. Response rates with four-drug combinations are not superior compared with triple therapy [70]. It has been shown that sequential therapy may be associated with less toxicity [62, 69, 71–73].
Third-line treatment and beyond: bendamustine in combination with novel agents has been tested in several phase II trials. With the combination of bendamustine, bortezomib, dexamethasone ORRs ranging from 60%–70% are achieved, which translate into PFS of 9.7–16 months [74, 75]. The combination of bendamustine with lenalidomide/dexamethasone showed a lower ORR of 52% and a PFS of 6.5 months – most probably because of the need to tailor lenalidomide dose to 10 mg [76]. Recently, the second generation irreversible proteasome inhibitor carfilzomib and the third generation IMiD pomalidomide have been added to the armamentarium for patients with multiple myeloma. A prospective phase III study comparing pomalidomide, a next generation IMiD, combined with low-dose dexamethasone to high dose dexamethasone alone in patients with refractory or relapsed and refractory plasma cell myeloma pretreated with bortezomib and lenalidomide has been reported. Both progression free and overall survival were significantly increased with the combination therapy as compared with dexamethasone alone. The documented overall response rate was 31%. The most frequent toxicities of grade ≥3 were infections, cytopenias and pneumonia [77]. Pomalidomide has recently been approved by Swissmedic for patients with refractory or relapsed plasma cell myeloma after at least two previous treatment lines, including bortezomib and lenalidomide. Carfilzomib is a next generation proteasome inhibitor that has been recently approved in the United States for treatment of patients with refractory or relapsed and refractory plasma cell myeloma who had received at least two previous therapies including bortezomib and an IMiD. Three single-arm phase II studies reported overall response rates of 17%–24% and a median duration of response of about 7–8 months in bortezomib-refractory patients [78–81]. The toxicity profile raised some concerns since cardiac failure of grade ≥3 after onset of treatment was seen in 7% of the patients, with some cases of cardiac death occurring shortly after treatment start [82]. Other relevant toxicities were fatigue, cytopenias, diarrhoea, pyrexia and dyspnoea. It has to be noted that carfilzomib is still not approved in Switzerland but may be available within an early access programme for selected patients. Ideally, heavily pretreated patients in need and ability of receiving treatment should be offered a clinical trial, whenever possible. An overview on labelling and reimbursement of new drugs in Switzerland is shown in table 4.
Allogeneic transplantation is an additional option in the relapsed/refractory setting. Graft versus myeloma reaction leads to significantly lower relapse rates and long lasting remissions compared to other salvage treatments. However, this beneficial effect is put off by early transplant related mortality resulting in overall survival rates similar to patients not transplanted from an allogeneic donor [83]. Follow up in most trials however is too short to draw definitive conclusions. Since the results remain controversial allogeneic HSCT is being performed preferentially within a clinical trial.
An algorithm for first and later line treatment options is being depicted in the figure.
| Table 4: Labelling and reimbursement of myeloma drugs in Switzerland (as of September 2014). | |||
| Drug | Swissmedic-Approval | Reimbursement | Availability |
| Thalidomide | TPL 1st line: no Non-TPL 1st line: no Later lines: no | No; individual application for cost coverage needed No; individual application for cost coverage needed No; individual application for cost coverage needed | Yes; customised importing for named patient use |
| Bortezomib | TPL 1st line: yes, with standard chemotherapy Non-TPL 1st line: yes, with melphalan/prednisone Later lines: yes | Yes, with formal application Yes, with formal application Yes, with formal application | Yes |
| Lenalidomide | TPL 1st line: no Non-TPL 1st line: no Later lines: yes, in combination with dexamethasone | No; individual application for cost coverage needed No; individual application for cost coverage needed Yes, with formal application | Yes |
| Bendamustine | TPL 1st line: no Non-TPL 1st line: no Later lines: no | No; individual application for cost coverage needed No; individual application for cost coverage needed No; individual application for cost coverage needed | Yes |
| Pomalidomide | TPL 1st line: no Non-TPL 1st line: no Later lines: yes, after at least two previous lines, including lenalidomide and bortezomib | No; individual application for cost coverage needed No; individual application for cost coverage needed Yes, with formal application | Yes |
| Carfilzomib | Not yet approved in Switzerland | No; individual application for cost coverage needed | Via EAP |
| Pegylated Liposomal Doxorubicin | TPL 1st line: no Non-TPL 1st line: no Later lines: yes, after at least one previous line | No; individual application for cost coverage needed No; individual application for cost coverage needed Yes, with formal application | Yes |
| EAP = early access programme; TPL = transplantation. | |||
Various new promising drugs are currently being tested in clinical trials and will be available for myeloma patients in the near future. Small molecules include new,, orally available, proteasome inhibitors (MLN9708), histone deacetylase (HDAC) inhibitors (panobinostat), and the kinesin spindle inhibitor filanesib. New antibodies currently undergoing clinical evaluation are daratumumab, targeting CD38, and elotuzumab, targeting the molecule CS1 [84–88].
Another promising approach, ‒ resensitising refractory myeloma cells to bortezomib ‒ has been reported with nelfinavir, a protease inhibitor approved for the treatment of human immunodeficiency virus. In a phase I study nelfinavir has been shown to exhibit pan-proteasome inhibiting activity and to re-establish sensitivity to bortezomib in bortezomib-refractory patients [89].
In 60% of patients, skeletal lytic lesions are present at time of diagnosis. Pain, pathological fractures of the vertebrae, and spinal cord compression are often associated with these lesions, motivating specific therapies. Furthermore, vertebral compression fractures occur frequently and may result in decreased lung function associated with dyspnoea.
Vertebroplasty (percutaneous injection of bone cement in the lytic lesion) or kyphoplasty (introduction of inflatable bone tamps into the vertebral bone, which after inflation restore the height of the vertebra) are both techniques which have been shown to induce pain relief [90–93]. In three prospective phase II–III trials with kyphoplasty and/or vertebroplasty, marked or complete pain relief was achieved in 80–84% of patients with plasma cell myeloma. Despite the fact that these procedures have never been examined in randomised, placebo controlled, blinded trials in myeloma, they are used today with success in daily practice. The choice between vertebroplasty and kyphoplasty depends on the expertise of the orthopaedic surgeon or interventional radiologist.
In up to 40% of patients, lytic lesions will require radiotherapy for pain control. Myeloma cells are highly sensitive to irradiation, thus irradiation is indicated for spinal cord compression from plasmocytoma. Limited involved fields should be preferred in order to limit the impact of irradiation on future stem-cell harvest or on potential future myelotoxic treatments. Post-surgical radiation after stabilisation of impending fractures is rarely needed [94].
Myeloma patients with or without documented bone lesions should be treated with bisphosphonates (zoledronate, pamidronate, or ibandronate) when receiving antimyeloma therapy [95, 96]. The most frequent side effects are fever occurring several hours after administration, acute renal failure, osteonecrosis of the jaw (particularly in patients with poor dental hygiene) and albuminuria (in particular after pamidronate administration). This therapy significantly reduces the number of skeletal events (pathological fractures, need of irradiation, or surgery on bone and spinal cord compression). Bisphosphonates should be given monthly, continued in patients with active disease and resumed in the case of myeloma relapse if discontinued in patients achieving complete or very good partial response with regularly monitoring of the renal function. In these patients, the optimal treatment duration with bisphosphonates is not clear, and experts and international guidelines propose that therapy should be administered for at least 12 months and up to 24 months.
Denosumab (a RANK-ligand inhibiting the osteoclast function) has been compared with zolendronic acid in patients suffering from bone lesions due to various tumours: denosumab was more active in solid tumour bone metastases, but not in plasma cell myeloma lesions. In fact, in the post-hocanalysis in 180 myeloma patients, denosumab led to a significantly increased mortality as compared with zoledronic acid [97, 98].
Infections are frequent in myeloma patients. Several prophylactic therapies are indicated, in particular when dexamethasone and/or bortezomib are administered: Intravenous immunoglobulin therapy should be considered for recurrent, life-threatening infections, particularly in patients with very low immunoglobulin levels. The vaccination schedule of the Swiss Health Department proposes pneumococcal, influenza and varicella vaccine in patients who are in clinical remission [99]. Pneumocystis jirovecii (carinii) pneumonia (PCP), herpes, and antifungal prophylaxis is recommended if a high-dose regimen is used. Herpes zoster prophylaxis is recommended in patients receiving bortezomib therapy [73, 100, 101].
Patients with plasma cell myeloma have an increased risk of developing venous thromboembolism [102]. This results from a combination of several factors including high immmunoglobulin levels, inflammation secondary to cytokines, hyperviscosity, and procoagulant activity of gammopathies. The indication for primary thrombosis prophylaxis in patients with plasma cell myeloma has to be evaluated according to the presence of individual risk factors [103]. Myeloma patients are not routinely preventively anticoagulated. Importantly, combination treatments with IMiDs can induce high rate of VTE and justify per se primary prophylaxis. The type of prophylaxis is still debated; nevertheless low risk patients should receive ASA, whereas high-risk patients or those receiving high-dose dexamethasone, anthracyclines, or polychemotherapy should be treated with prophylactic doses of low molecular weight heparin (LMWH) or oral anticoagulant therapy with vitamin K antagonists [104].
In more than 90% of myeloma patients, anaemia (haemoglobin <120 g/l) will be responsible for discomfort (fatigue, loss of appetite, dyspnoea and other typical symptoms). The initial evaluation should exclude other causes such as iron (chronic bleeding) or vitamin deficiency.
The indication for anaemia therapy depends essentially on the severity of the symptoms and on the level of haemoglobin. In these cases, red blood cell (RBC) transfusions (leucocyte-reduced, cross-matched red cells) are administered in order to increase the haemoglobin level to render patients asymptomatic. However, RBC transfusions should be administered carefully in patients with high levels of monoclonal protein as they may aggravate an underlying hyperviscosity syndrome.
Erythropoiesis-stimulating agents (ESAs) are usually reserved for patients with symptomatic anaemia during the plateau phase of the paraproteinaemia after chemotherapy. In a double-blind phase of a randomised study comparing erythropoietin to placebo, erythropoietin resulted in a significantly lower incidence of transfusions (47% vs 28%), and an increase of the haemoglobin concentration by 18 g/l [105]. Seven preparations of ESA are available in Switzerland, with three approved in the context of chemotherapy.
1 Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer. 2013;49(6):1374–403. PubMed PMID: 23485231.
2 Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF, et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002;346(8):564–9. PubMed PMID: 11856795.
3 Rodriguez-Abreu D, Bordoni A, Zucca E. Epidemiology of hematological malignancies. Annals of oncology: official journal of the European Society for Medical Oncology / ESMO. 2007;18(Suppl 1):i3–i8. PubMed PMID: 17311819.
4 Martino M, Postorino M, Gallo GA, Messina G, Neri S, Piro E, et al. Long-term results in multiple myeloma after high-dose melphalan and autologous transplantation according to response categories in the era of old drugs. Clin Lymphoma Myeloma Leuk. 2014;14(2):148–54. PubMed PMID: 24417912.
5 Martinez-Lopez J, Blade J, Mateos MV, Grande C, Alegre A, Garcia-Larana J, et al. Long-term prognostic significance of response in multiple myeloma after stem cell transplantation. Blood. 2011;118(3):529–34. PubMed PMID: 21482708.
6 Gahrton G, Iacobelli S, Bjorkstrand B, Hegenbart U, Gruber A, Greinix H, et al. Autologous/reduced-intensity allogeneic stem cell transplantation vs autologous transplantation in multiple myeloma: long-term results of the EBMT-NMAM2000 study. Blood. 2013;121(25):5055–63. PubMed PMID: 23482933.
7 Bruno B, Rotta M, Patriarca F, Mordini N, Allione B, Carnevale-Schianca F, et al. A comparison of allografting with autografting for newly diagnosed myeloma. N Engl J Med. 2007;356(11):1110–20. PubMed PMID: 17360989.
8 Paiva B, Almeida J, Perez-Andres M, Mateo G, Lopez A, Rasillo A, et al. Utility of flow cytometry immunophenotyping in multiple myeloma and other clonal plasma cell-related disorders. Cytometry Part B, Clinical cytometry. 2010;78(4):239–52. PubMed PMID: 20155853.
9 Robillard N, Bene MC, Moreau P, Wuilleme S. A single-tube multiparameter seven-colour flow cytometry strategy for the detection of malignant plasma cells in multiple myeloma. Blood cancer journal. 2013;3:e134. PubMed PMID: 23955589. Pubmed Central PMCID: 3763387.
10 Hillengass J, Weber MA, Kilk K, Listl K, Wagner-Gund B, Hillengass M, et al. Prognostic significance of whole-body MRI in patients with monoclonal gammopathy of undetermined significance. Leukemia. 2014;28(1):174–8. PubMed PMID: 23958921.
11 Hillengass J, Fechtner K, Weber MA, Bauerle T, Ayyaz S, Heiss C, et al. Prognostic significance of focal lesions in whole-body magnetic resonance imaging in patients with asymptomatic multiple myeloma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28(9):1606–10. PubMed PMID: 20177023.
12 Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos M, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. The Lancet Oncology. 2014;15:e538–e47.
13 Ross FM, Avet-Loiseau H, Ameye G, Gutierrez NC, Liebisch P, O’Connor S, et al. Report from the European Myeloma Network on interphase FISH in multiple myeloma and related disorders. Haematologica. 2012 Aug;97(8):1272–7. PubMed PMID: 22371180. Pubmed Central PMCID: 3409827.
14 Avet-Loiseau H, Durie BG, Cavo M, Attal M, Gutierrez N, Haessler J, et al. Combining fluorescent in situ hybridization data with ISS staging improves risk assessment in myeloma: an International Myeloma Working Group collaborative project. Leukemia. 2013;27(3):711–7. PubMed PMID: 23032723. Pubmed Central PMCID: 3972006.
15 Chng WJ, Dispenzieri A, Chim CS, Fonseca R, Goldschmidt H, Lentzsch S, et al. IMWG consensus on risk stratification in multiple myeloma. Leukemia. 2014;28(2):269–77. PubMed PMID: 23974982.
16 Durie BG, Harousseau JL, Miguel JS, Blade J, Barlogie B, Anderson K, et al. International uniform response criteria for multiple myeloma. Leukemia. 2006;20(9):1467–73. PubMed PMID: 16855634.
17 Tatsas AD, Jagasia MH, Chen H, McCurley TL. Monitoring residual myeloma: high-resolution serum/urine electrophoresis or marrow biopsy with immunohistochemical analysis? Am J Clin Pathol. 2010;134(1):139–44. PubMed PMID: 20551278.
18 Chee CE, Kumar S, Larson DR, Kyle RA, Dispenzieri A, Gertz MA, et al. The importance of bone marrow examination in determining complete response to therapy in patients with multiple myeloma. Blood. 2009;114(13):2617–8. PubMed PMID: 19641191. Pubmed Central PMCID: 2756122.
19 Martinelli G, Terragna C, Zamagni E, Ronconi S, Tosi P, Lemoli RM, et al. Molecular remission after allogeneic or autologous transplantation of hematopoietic stem cells for multiple myeloma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2000;18(11):2273–81. PubMed PMID: 10829048.
20 Paiva B, Vidriales MB, Cervero J, Mateo G, Perez JJ, Montalban MA, et al. Multiparameter flow cytometric remission is the most relevant prognostic factor for multiple myeloma patients who undergo autologous stem cell transplantation. Blood. 2008;112(10):4017–23. PubMed PMID: 18669875. Pubmed Central PMCID: 2581991.
21 Mateos MV, Oriol A, Martinez-Lopez J, Gutierrez N, Teruel AI, de Paz R, et al. Bortezomib, melphalan, and prednisone versus bortezomib, thalidomide, and prednisone as induction therapy followed by maintenance treatment with bortezomib and thalidomide versus bortezomib and prednisone in elderly patients with untreated multiple myeloma: a randomised trial. The Lancet Oncology. 2010;11(10):934–41. PubMed PMID: 20739218.
22 Kyle RA, Durie BG, Rajkumar SV, Landgren O, Blade J, Merlini G, et al. Monoclonal gammopathy of undetermined significance (MGUS) and smoldering (asymptomatic) multiple myeloma: IMWG consensus perspectives risk factors for progression and guidelines for monitoring and management. Leukemia. 2010;24(6):1121–7. PubMed PMID: 20410922.
23 Perez-Persona E, Mateo G, Garcia-Sanz R, Mateos MV, de Las Heras N, de Coca AG, et al. Risk of progression in smouldering myeloma and monoclonal gammopathies of unknown significance: comparative analysis of the evolution of monoclonal component and multiparameter flow cytometry of bone marrow plasma cells. Br J Haematol. 2010;148(1):110–4. PubMed PMID: 19821821.
24 Perez-Persona E, Vidriales MB, Mateo G, Garcia-Sanz R, Mateos MV, de Coca AG, et al. New criteria to identify risk of progression in monoclonal gammopathy of uncertain significance and smoldering multiple myeloma based on multiparameter flow cytometry analysis of bone marrow plasma cells. Blood. 2007;110(7):2586–92. PubMed PMID: 17576818.
25 Dispenzieri A, Stewart AK, Chanan-Khan A, Rajkumar SV, Kyle RA, Fonseca R, et al. Smoldering multiple myeloma requiring treatment: time for a new definition? Blood. 2013;122(26):4172–81. PubMed PMID: 24144641. Pubmed Central PMCID: 3952477.
26 Mateos MV, Hernandez MT, Giraldo P, de la Rubia J, de Arriba F, Lopez Corral L, et al. Lenalidomide plus dexamethasone for high-risk smoldering multiple myeloma. N Engl J Med. 2013;369(5):438–47. PubMed PMID: 23902483.
27 Rosinol L, Oriol A, Teruel AI, Hernandez D, Lopez-Jimenez J, de la Rubia J, et al. Superiority of bortezomib, thalidomide, and dexamethasone (VTD) as induction pretransplantation therapy in multiple myeloma: a randomized phase 3 PETHEMA/GEM study. Blood. 2012;120(8):1589–96. PubMed PMID: 22791289.
28 Sonneveld P, Schmidt-Wolf IG, van der Holt B, El Jarari L, Bertsch U, Salwender H, et al. Bortezomib induction and maintenance treatment in patients with newly diagnosed multiple myeloma: results of the randomized phase III HOVON-65/ GMMG-HD4 trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2012;30(24):2946–55. PubMed PMID: 22802322.
29 Reeder CB, Reece DE, Kukreti V, Chen C, Trudel S, Hentz J, et al. Cyclophosphamide, bortezomib and dexamethasone induction for newly diagnosed multiple myeloma: high response rates in a phase II clinical trial. Leukemia. 2009;23(7):1337–41. PubMed PMID: 19225538. Pubmed Central PMCID: 2711213.
30 Cavo M, Tacchetti P, Patriarca F, Petrucci MT, Pantani L, Galli M, et al. Bortezomib with thalidomide plus dexamethasone compared with thalidomide plus dexamethasone as induction therapy before, and consolidation therapy after, double autologous stem-cell transplantation in newly diagnosed multiple myeloma: a randomised phase 3 study. Lancet. 2010;376(9758):2075–85. PubMed PMID: 21146205.
31 Gay F, Magarotto V, Crippa C, Pescosta N, Guglielmelli T, Cavallo F, et al. Bortezomib induction, reduced-intensity transplantation, and lenalidomide consolidation-maintenance for myeloma: updated results. Blood. 2013;122(8):1376–83. PubMed PMID: 23775712.
32 Sonneveld P, Goldschmidt H, Rosinol L, Blade J, Lahuerta JJ, Cavo M, et al. Bortezomib-based versus nonbortezomib-based induction treatment before autologous stem-cell transplantation in patients with previously untreated multiple myeloma: a meta-analysis of phase III randomized, controlled trials. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2013;31(26):3279–87. PubMed PMID: 23897961.
33 Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M, et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. The Lancet Oncology. 2011;12(5):431–40. PubMed PMID: 21507715.
34 Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME, et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. The Lancet Oncology. 2010;11(1):29–37. PubMed PMID: 19853510. Pubmed Central PMCID: 3042271.
35 Khan ML, Reeder CB, Kumar SK, Lacy MQ, Reece DE, Dispenzieri A, et al. A comparison of lenalidomide/dexamethasone versus cyclophosphamide/lenalidomide/dexamethasone versus cyclophosphamide/bortezomib/dexamethasone in newly diagnosed multiple myeloma. Br J Haematol. 2012;156(3):326–33. PubMed PMID: 22107129.
36 Kumar SK, Lacy MQ, Hayman SR, Stewart K, Buadi FK, Allred J, et al. Lenalidomide, cyclophosphamide and dexamethasone (CRd) for newly diagnosed multiple myeloma: results from a phase 2 trial. Am J Hematol. 2011;86(8):640–5. PubMed PMID: 21630308. Pubmed Central PMCID: 3901994.
37 Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, Gastineau DA, et al. Impact of lenalidomide therapy on stem cell mobilization and engraftment post-peripheral blood stem cell transplantation in patients with newly diagnosed myeloma. Leukemia. 2007;21(9):2035–42. PubMed PMID: 17581613.
38 Kumar S, Giralt S, Stadtmauer EA, Harousseau JL, Palumbo A, Bensinger W, et al. Mobilization in myeloma revisited: IMWG consensus perspectives on stem cell collection following initial therapy with thalidomide-, lenalidomide-, or bortezomib-containing regimens. Blood. 2009;114(9):1729–35. PubMed PMID: 19561323.
39 Harousseau JL, Avet-Loiseau H, Attal M, Charbonnel C, Garban F, Hulin C, et al. Achievement of at least very good partial response is a simple and robust prognostic factor in patients with multiple myeloma treated with high-dose therapy: long-term analysis of the IFM 99–02 and 99–04 Trials. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2009;27(34):5720–6. PubMed PMID: 19826130.
40 Barlogie B, Anaissie E, Haessler J, van Rhee F, Pineda-Roman M, Hollmig K, et al. Complete remission sustained 3 years from treatment initiation is a powerful surrogate for extended survival in multiple myeloma. Cancer. 2008;113(2):355–9. PubMed PMID: 18470907.
41 Gay F, Hajek, R., Diramondo, F., et al. Cyclophosphamide-lenalidomide-dexamethasone vs autologous transplant in newly diagnosed myeloma: a phase 3 trial. Clin Lymphoma Myeloma Leuk. 2013;13(suppl 1):S40.
42 Palumbo A, Cavallo F, Gay F, Di Raimondo F, Ben Yehuda D, Petrucci MT, et al. Autologous transplantation and maintenance therapy in multiple myeloma. N Engl J Med. 2014;371(10):895–905. PubMed PMID: 25184862.
43 Cavo M, Salwender H, Rosiñol L, Moreau P, Petrucci MT, Blau IW, et al. Double Vs Single Autologous Stem Cell Transplantation After Bortezomib-Based Induction Regimens For Multiple Myeloma: An Integrated Analysis Of Patient-Level Data From Phase European III Studies. ASH 2013 Annual Meeting. 2013:Abstract 767.
44 Attal M, Harousseau JL, Facon T, Guilhot F, Doyen C, Fuzibet JG, et al. Single versus double autologous stem-cell transplantation for multiple myeloma. N Engl J Med. 2003;349(26):2495–502. PubMed PMID: 14695409.
45 Cavo M, Tosi P, Zamagni E, Cellini C, Tacchetti P, Patriarca F, et al. Prospective, randomized study of single compared with double autologous stem-cell transplantation for multiple myeloma: Bologna 96 clinical study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2007;25(17):2434–41. PubMed PMID: 17485707.
46 Kumar A, Kharfan-Dabaja MA, Glasmacher A, Djulbegovic B. Tandem versus single autologous hematopoietic cell transplantation for the treatment of multiple myeloma: a systematic review and meta-analysis. J Natl Cancer Inst. 2009;101(2):100–6. PubMed PMID: 19141779.
47 Cavo M, Pantani L, Petrucci MT, Patriarca F, Zamagni E, Donnarumma D, et al. Bortezomib-thalidomide-dexamethasone is superior to thalidomide-dexamethasone as consolidation therapy after autologous hematopoietic stem cell transplantation in patients with newly diagnosed multiple myeloma. Blood. 2012;120(1):9–19. PubMed PMID: 22498745.
48 Mellqvist UH, Gimsing P, Hjertner O, Lenhoff S, Laane E, Remes K, et al. Bortezomib consolidation after autologous stem cell transplantation in multiple myeloma: a Nordic Myeloma Study Group randomized phase 3 trial. Blood. 2013;121(23):4647–54. PubMed PMID: 23616624. Pubmed Central PMCID: 3674665.
49 Attal M, Lauwers-Cances V, Marit G, Caillot D, Moreau P, Facon T, et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma. N Engl J Med. 2012;366(19):1782–91. PubMed PMID: 22571202.
50 Neben K, Lokhorst HM, Jauch A, Bertsch U, Hielscher T, van der Holt B, et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood. 2012;119(4):940–8. PubMed PMID: 22160383.
51 McCarthy PL, Owzar K, Hofmeister CC, Hurd DD, Hassoun H, Richardson PG, et al. Lenalidomide after stem-cell transplantation for multiple myeloma. N Engl J Med. 2012;366(19):1770–81. PubMed PMID: 22571201. Pubmed Central PMCID: 3744390.
52 Attal M L-CV, Marit G, et al. Lenalidomide maintenance after stem-cell transplantation for multiple myeloma: Follow-up analysis of the IFM 2005–02 trial. 2013 ASH Annual Meeting. 2013:Abstract 406.
53 Boccadoro M, Cavallo F, Gay FM, Di Raimondo F, Nagler A, Montefusco V, et al. Melphalan/prednisone/lenalidomide (MPR) versus high-dose melphalan and autologous transplantation (MEL200) plus lenalidomide maintenance or no maintenance in newly diagnosed multiple myeloma (MM) patients. ASCO Annual Meeting 2013. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2013;31(suppl; abstr 8509).
54 Kharfan-Dabaja MA, Hamadani M, Reljic T, Nishihori T, Bensinger W, Djulbegovic B, et al. Comparative efficacy of tandem autologous versus autologous followed by allogeneic hematopoietic cell transplantation in patients with newly diagnosed multiple myeloma: a systematic review and meta-analysis of randomized controlled trials. Journal of hematology & oncology. 2013;6:2. PubMed PMID: 23289975. Pubmed Central PMCID: 3548722.
55 Armeson KE, Hill EG, Costa LJ. Tandem autologous vs autologous plus reduced intensity allogeneic transplantation in the upfront management of multiple myeloma: meta-analysis of trials with biological assignment. Bone marrow transplantation. 2013;48(4):562–7. PubMed PMID: 22964593.
56 San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M, et al. Persistent overall survival benefit and no increased risk of second malignancies with bortezomib-melphalan-prednisone versus melphalan-prednisone in patients with previously untreated multiple myeloma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2013;31(4):448–55. PubMed PMID: 23233713.
57 Fayers PM, Palumbo A, Hulin C, Waage A, Wijermans P, Beksac M, et al. Thalidomide for previously untreated elderly patients with multiple myeloma: meta-analysis of 1685 individual patient data from 6 randomized clinical trials. Blood. 2011;118(5):1239–47. PubMed PMID: 21670471.
58 Morabito F, Bringhen S, Larocca A, Wijermans P, Victoria Mateos M, Gimsing P, et al. Bortezomib, melphalan, prednisone (VMP) versus melphalan, prednisone, thalidomide (MPT) in elderly newly diagnosed multiple myeloma patients: A retrospective case-matched study. Am J Hematol. 2014;89(4):355–62. PubMed PMID: 24273190.
59 Palumbo A, Hajek R, Delforge M, Kropff M, Petrucci MT, Catalano J, et al. Continuous lenalidomide treatment for newly diagnosed multiple myeloma. N Engl J Med. 2012;366(19):1759–69. PubMed PMID: 22571200.
60 Facon T, Dimopoulos MA, Dispenzieri A, Catalano JV, Belch AR, Hulin C, et al. Initial Phase 3 Results Of The First (Frontline Investigation Of Lenalidomide + Dexamethasone Versus Standard Thalidomide) Trial (MM-020/IFM 07 01) In Newly Diagnosed Multiple Myeloma (NDMM) Patients (Pts) Ineligible For Stem Cell Transplantation (SCT). Blood. 2013;122:abstract 2.
61 Palumbo A, Anderson K. Multiple myeloma. N Engl J Med. 2011;364(11):1046–60. PubMed PMID: 21410373.
62 Lonial S, Mitsiades CS, Richardson PG. Treatment options for relapsed and refractory multiple myeloma. Clinical cancer research: an official journal of the American Association for Cancer Research. 2011;17(6):1264–77. PubMed PMID: 21411442.
63 Alvares CL, Davies FE, Horton C, Patel G, Powles R, Morgan GJ. The role of second autografts in the management of myeloma at first relapse. Haematologica. 2006;91(1):141–2. PubMed PMID: 16434386.
64 Lemieux E, Hulin C, Caillot D, Tardy S, Dorvaux V, Michel J, et al. Autologous stem cell transplantation: an effective salvage therapy in multiple myeloma. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2013;19(3):445–9. PubMed PMID: 23186983.
65 Olin RL, Vogl DT, Porter DL, Luger SM, Schuster SJ, Tsai DE, et al. Second auto-SCT is safe and effective salvage therapy for relapsed multiple myeloma. Bone marrow transplantation. 2009;43(5):417–22. PubMed PMID: 18850013. Pubmed Central PMCID: 2757257.
66 Cook G, Williams C, Brown JM, Cairns DA, Cavenagh J, Snowden JA, et al. High-dose chemotherapy plus autologous stem-cell transplantation as consolidation therapy in patients with relapsed multiple myeloma after previous autologous stem-cell transplantation (NCRI Myeloma X Relapse [Intensive trial]): a randomised, open-label, phase 3 trial. The Lancet Oncology. 2014;15(8):874–85. PubMed PMID: 24948586.
67 Jimenez-Zepeda VH, Reece DE, Trudel S, Chen C, Tiedemann R, Kukreti V. Lenalidomide (Revlimid), bortezomib (Velcade) and dexamethasone for heavily pretreated relapsed or refractory multiple myeloma. Leukemia & lymphoma. 2013;54(3):555–60. PubMed PMID: 22881043.
68 Richardson PG, Xie W, Jagannath S, Jakubowiak A, Lonial S, Raje NS, et al. A phase 2 trial of lenalidomide, bortezomib, and dexamethasone in patients with relapsed and relapsed/refractory myeloma. Blood. 2014;123(10):1461–9. PubMed PMID: 24429336.
69 Orlowski RZ, Nagler A, Sonneveld P, Blade J, Hajek R, Spencer A, et al. Randomized phase III study of pegylated liposomal doxorubicin plus bortezomib compared with bortezomib alone in relapsed or refractory multiple myeloma: combination therapy improves time to progression. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2007;25(25):3892–901. PubMed PMID: 17679727.
70 Kumar S, Flinn I, Richardson PG, Hari P, Callander N, Noga SJ, et al. Randomized, multicenter, phase 2 study (EVOLUTION) of combinations of bortezomib, dexamethasone, cyclophosphamide, and lenalidomide in previously untreated multiple myeloma. Blood. 2012;119(19):4375–82. PubMed PMID: 22422823.
71 Weber DM, Chen C, Niesvizky R, Wang M, Belch A, Stadtmauer EA, et al. Lenalidomide plus dexamethasone for relapsed multiple myeloma in North America. N Engl J Med. 2007;357(21):2133–42. PubMed PMID: 18032763.
72 Dimopoulos MA, Chen C, Spencer A, Niesvizky R, Attal M, Stadtmauer EA, et al. Long-term follow-up on overall survival from the MM-009 and MM-010 phase III trials of lenalidomide plus dexamethasone in patients with relapsed or refractory multiple myeloma. Leukemia. 2009;23(11):2147–52. PubMed PMID: 19626046.
73 Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352(24):2487–98. PubMed PMID: 15958804.
74 Ludwig H, Kasparu H, Leitgeb C, Rauch E, Linkesch W, Zojer N, et al. Bendamustine-bortezomib-dexamethasone is an active and well-tolerated regimen in patients with relapsed or refractory multiple myeloma. Blood. 2014;123(7):985–91. PubMed PMID: 24227817. Pubmed Central PMCID: 3924931.
75 Offidani M, Corvatta L, Maracci L, Liberati AM, Ballanti S, Attolico I, et al. Efficacy and tolerability of bendamustine, bortezomib and dexamethasone in patients with relapsed-refractory multiple myeloma: a phase II study. Blood cancer journal. 2013;3:e162. PubMed PMID: 24270324. Pubmed Central PMCID: 3880441.
76 Lentzsch S, O’Sullivan A, Kennedy RC, Abbas M, Dai L, Pregja SL, et al. Combination of bendamustine, lenalidomide, and dexamethasone (BLD) in patients with relapsed or refractory multiple myeloma is feasible and highly effective: results of phase 1/2 open-label, dose escalation study. Blood. 2012;119(20):4608–13. PubMed PMID: 22451423. Pubmed Central PMCID: 3392072.
77 San Miguel J, Weisel K, Moreau P, Lacy M, Song K, Delforge M, et al. Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory multiple myeloma (MM-003): a randomised, open-label, phase 3 trial. The lancet oncology. 2013;14(11):1055–66. PubMed PMID: 24007748.
78 Vij R, Siegel DS, Jagannath S, Jakubowiak AJ, Stewart AK, McDonagh K, et al. An open-label, single-arm, phase 2 study of single-agent carfilzomib in patients with relapsed and/or refractory multiple myeloma who have been previously treated with bortezomib. Br J Haematol. 2012;158(6):739–48. PubMed PMID: 22845873.
79 Jagannath S, Vij R, Stewart AK, Trudel S, Jakubowiak AJ, Reiman T, et al. An open-label single-arm pilot phase II study (PX-171–003–A0) of low-dose, single-agent carfilzomib in patients with relapsed and refractory multiple myeloma. Clinical lymphoma, myeloma & leukemia. 2012;12(5):310–8. PubMed PMID: 23040437.
80 Siegel DS, Martin T, Wang M, Vij R, Jakubowiak AJ, Lonial S, et al. A phase 2 study of single-agent carfilzomib (PX-171–003–A1) in patients with relapsed and refractory multiple myeloma. Blood. 2012;120(14):2817–25. PubMed PMID: 22833546.
81 Vij R, Wang M, Kaufman JL, Lonial S, Jakubowiak AJ, Stewart AK, et al. An open-label, single-arm, phase 2 (PX-171–004) study of single-agent carfilzomib in bortezomib-naive patients with relapsed and/or refractory multiple myeloma. Blood. 2012;119(24):5661–70. PubMed PMID: 22555973.
82 Herndon TM, Deisseroth A, Kaminskas E, Kane RC, Koti KM, Rothmann MD, et al. U.s. Food and Drug Administration approval: carfilzomib for the treatment of multiple myeloma. Clinical cancer research: an official journal of the American Association for Cancer Research. 2013;19(17):4559–63. PubMed PMID: 23775332.
83 Patriarca F, Einsele H, Spina F, Bruno B, Isola M, Nozzoli C, et al. Allogeneic stem cell transplantation in multiple myeloma relapsed after autograft: a multicenter retrospective study based on donor availability. Biology of blood and marrow transplantation: journal of the American Society for Blood and Marrow Transplantation. 2012;18(4):617–26. PubMed PMID: 21820394.
84 Kumar SK BJ, Niesvizky R, Lonial S, Hamadani M, Stewart AK, et al. A Phase 1/2 Study of Weekly MLN9708, an Investigational Oral Proteasome Inhibitor, in Combination with Lenalidomide and Dexamethasone in Patients with Previously Untreated Multiple Myeloma (MM). ASH 2012 Annual Meeting. 2012 (Abstract 332).
85 Richardson PG, Schlossman RL, Alsina M, Weber DM, Coutre SE, Gasparetto C, et al. PANORAMA 2: panobinostat in combination with bortezomib and dexamethasone in patients with relapsed and bortezomib-refractory myeloma. Blood. 2013;122(14):2331–7. PubMed PMID: 23950178.
86 Lonial S SJ, Zonder J, Bensinger WI, Cohen AD, Kaufman JL, et al. Prolonged Survival and Improved Response Rates With ARRY-520 (Filanesib) In Relapsed/Refractory Multiple Myeloma (RRMM) Patients With Low α-1 Acid Glycoprotein (AAG) Levels: Results From a Phase 2 Study. ASH 2013 Annual Meeting. 2013 (Abstract 285).
87 Plesner T AT, Lokhorst H, Gimsing P, Krejcik J, Lemech C, et al. Preliminary Safety and Efficacy Data Of Daratumumab In Combination With Lenalidomide and Dexamethasone In Relapsed Or Refractory Multiple Myeloma. ASH 2013 Annual Meeting. 2013 (Abstract 1986).
88 Richardson PG JS, Moreau P, Jakubowiak A, Raab MS, Facon T, et al. . A Phase 2 Study of Elotuzumab (Elo) in Combination with Lenalidomide and Low-Dose Dexamethasone (Ld) in Patients (pts) with Relapsed/Refractory Multiple Myeloma (R/R MM): Updated Results. ASH 2012 Annual Meeting. 2012 (Abstract 202).
89 Driessen C H, D, Pabst, T, Haile SR, Joerger M, von Moos R, et al. SAKK 65/08: A Phase I Trial of the HIV Protease Inhibitor Nelfinavir in Combination with Bortezomib Identifies Nelfinavir As FDA Approved, Oral Drug that Inhibits the Proteasome and Induces Proteotoxic Stress in Vivo and has Potential Antimyeloma Activity. ASH 2012 Annual Meeting. 2012 (abstract 2956).
90 Dudeney S, Lieberman IH, Reinhardt MK, Hussein M. Kyphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2002;20(9):2382–7. PubMed PMID: 11981012.
91 Fourney DR, Schomer DF, Nader R, Chlan-Fourney J, Suki D, Ahrar K, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. Journal of neurosurgery. 2003;98(1 Suppl):21–30. PubMed PMID: 12546384.
92 Lane JM, Hong R, Koob J, Kiechle T, Niesvizky R, Pearse R, et al. Kyphoplasty enhances function and structural alignment in multiple myeloma. Clin Orthop Relat Res. 2004(426):49–53. PubMed PMID: 15346051.
93 Hentschel SJ, Burton AW, Fourney DR, Rhines LD, Mendel E. Percutaneous vertebroplasty and kyphoplasty performed at a cancer center: refuting proposed contraindications. J Neurosurg Spine. 2005;2(4):436–40. PubMed PMID: 15871483.
94 Lecouvet F, Richard F, Vande Berg B, Malghem J, Maldague B, Jamart J, et al. Long-term effects of localized spinal radiation therapy on vertebral fractures and focal lesions appearance in patients with multiple myeloma. Br J Haematol. 1997;96(4):743–5. PubMed PMID: 9074416.
95 Terpos E, Morgan G, Dimopoulos MA, Drake MT, Lentzsch S, Raje N, et al. International Myeloma Working Group recommendations for the treatment of multiple myeloma-related bone disease. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2013;31(18):2347–57. PubMed PMID: 23690408.
96 Morgan GJ, Davies FE, Gregory WM, Cocks K, Bell SE, Szubert AJ, et al. First-line treatment with zoledronic acid as compared with clodronic acid in multiple myeloma (MRC Myeloma IX): a randomised controlled trial. Lancet. 2010 Dec 11;376(9757):1989–99. PubMed PMID: 21131037. Pubmed Central PMCID: 3639680.
97 Henry DH, Costa L, Goldwasser F, Hirsh V, Hungria V, Prausova J, et al. Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2011;29(9):1125–32. PubMed PMID: 21343556.
98 Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH, et al. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28(35):5132–9. PubMed PMID: 21060033.
99 Bundesamt für Gesundheit, Schweizerischer Impfplan 2013, page 20.
100 Chanan-Khan A, Sonneveld P, Schuster MW, Stadtmauer EA, Facon T, Harousseau JL, et al. Analysis of herpes zoster events among bortezomib-treated patients in the phase III APEX study. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2008;26(29):4784–90. PubMed PMID: 18711175.
101 Mateos MV, Hernandez JM, Hernandez MT, Gutierrez NC, Palomera L, Fuertes M, et al. Bortezomib plus melphalan and prednisone in elderly untreated patients with multiple myeloma: results of a multicenter phase 1/2 study. Blood. 2006;108(7):2165–72. PubMed PMID: 16772605.
102 Zamagni E, Brioli A, Tacchetti P, Zannetti B, Pantani L, Cavo M. Multiple myeloma, venous thromboembolism, and treatment-related risk of thrombosis. Sem Thromb Hemost. 2011;37(3):209–19. PubMed PMID: 21455855.
103 http://myeloma.org/, IMWG guidelines for the prevention of thalidomide- and Lenalidomide-associated thrombosis in myeloma.
104 Palumbo A, Cavo M, Bringhen S, Zamagni E, Romano A, Patriarca F, et al. Aspirin, warfarin, or enoxaparin thromboprophylaxis in patients with multiple myeloma treated with thalidomide: a phase III, open-label, randomized trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2011;29(8):986–93. PubMed PMID: 21282540.
105 Osterborg A, Boogaerts MA, Cimino R, Essers U, Holowiecki J, Juliusson G, et al. Recombinant human erythropoietin in transfusion-dependent anemic patients with multiple myeloma and non-Hodgkin's lymphoma – a randomized multicenter study. The European Study Group of Erythropoietin (Epoetin Beta) Treatment in Multiple Myeloma and Non-Hodgkin’s Lymphoma. Blood. 1996;87(7):2675–82. PubMed PMID: 8639883.
106 Harousseau JL, Attal M, Avet-Loiseau H, Marit G, Caillot D, Mohty M, et al. Bortezomib plus dexamethasone is superior to vincristine plus doxorubicin plus dexamethasone as induction treatment prior to autologous stem-cell transplantation in newly diagnosed multiple myeloma: results of the IFM 2005–01 phase III trial. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28(30):4621–9. PubMed PMID: 20823406.
107 Facon T, Mary JY, Hulin C, Benboubker L, Attal M, Pegourie B, et al. Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99–06): a randomised trial. Lancet. 2007;370(9594):1209–18. PubMed PMID: 17920916.
Funding / potential competing interests: The process of compiling this review was supported by an unrestricted grant from beupdated. Beupdated has provided financial support for a face-to-face meeting and a limited honorarium to authors. There was no direct link between pharmaceutical industry and authors.