Saccadic eye movement performance as an indicator of driving ability in elderly drivers
DOI: https://doi.org/10.4414/smw.2015.14098
Kai-Uwe
Schmitt, Rolf
Seeger, Hartmut
Fischer, Christian
Lanz, Markus
Muser, Felix
Walz, Urs
Schwarz
Summary
OBJECTIVE: Regular checking of the fitness to drive of elderly car-license holders is required in some countries, and this will become increasingly important as more countries face aging populations. The present study investigated whether the analysis of saccadic eye movements could be used as a screening method for the assessment of driving ability.
METHODS: Three different paradigms (prosaccades, antisaccades, and visuovisual interactive (VVI) saccades) were used to test saccadic eye movements in 144 participants split into four groups: elderly drivers who came to the attention of road authorities for suspected lack of fitness to drive, a group of elderly drivers who served as a comparison group, a group of neurology patients with established brain lesion diagnoses, and a young comparison group. The group of elderly drivers with suspected deficits in driving skills also underwent a medical examination and a practical on-road driving test. The results of the saccadic eye tests of the different groups were compared.
RESULTS: Antisaccade results indicated a strong link to driving behaviour: elderly drivers who were not fit to drive exhibited a poor performance on the antisaccade task and the performance in the VVI task was also clearly poorer in this group.
CONCLUSIONS: Testing saccadic eye movements appears to be a promising and efficient method for screening large numbers of people such as elderly drivers. This study indicated a link between antisaccade performance and the ability to drive. Hence, measuring saccadic eye movements should be considered as a tool for screening the fitness to drive.
Introduction
Elderly drivers are progressively a focus of discussion in the context of traffic safety (see e.g. [1]) as the number of elderly driving license holders increases along with increasingly complex traffic and consequently an increasing risk of failure due to declining fitness to drive. Various factors such as eyesight or reduced cognitive functions can result in fitness to drive declining with age. Consequently, attempts are being undertaken to assess elderly drivers in order to make certain they are capable of safely driving a motor vehicle, and several countries have already introduced assessment procedures for evaluating older drivers [1]. Switzerland, for example, requires that all license holders aged 70+ years have a medical examination biennially to ensure fitness to drive. As this entails a large number of people being examined every year, a cost- and time-efficient and sensitive screening method would be very beneficial. Reviewing different procedures, Wheatley and di Stefano [2] concluded that a detailed clinical and on-road assessment is best suited for drivers with complex health, disability or age-related issues. However, such complex procedures are difficult and expensive for screening a large population. This study therefore investigated whether saccadic eye movement performance, which is more easily measured, can be used as a predictor of driving ability.
Saccadic eye movements are characterised by rapid movements of the eyes. Mostly saccades are executed as reflex-like behaviour, so-called prosaccades that are directed towards a target, but also can be induced voluntarily [3–5]. Quickly moving the point of gaze towards a suddenly appearing object is a task that is frequently required when driving a vehicle. To perform an antisaccade, a subject must first suppress the automatic response to look at the target (prosaccade) and then transform the location of the stimulus into a voluntary motor command to look away from the target (antisaccade) [6]. Besides the general relevance of antisaccades as a biomarker for neurological deficits, there are also specific situations in traffic where performance of antisaccades is required. Elderly drivers, for example, are sensitive to glare from oncoming cars with high light beams at night. The important task is not to look into the beam lights but to orientate on the own lane border.
Depending on the task, different brain regions are involved in saccade execution [5, 7–11]. Increasingly, the precise recording and detailed analysis of eye movements has become an important diagnostic tool in neurology for the assessment of regional brain function. To date, research has identified saccadic eye movements as a physiological marker of overall cognitive status. Changes in saccade characteristics due to, for instance, brain lesions or dementia have been demonstrated [9]. Thus, frontal cortical areas, which are involved in inducing voluntary saccades, are of interest as first indicators of dementia, as well as other diseases such as Parkinson’s disease or certain psychiatric disorders [9, 12, 13]. Abnormal eye movements can indicate the presence of neurodegeneration and thus the analysis of saccadic eye movements is common in neurology as it provides an invaluable adjunct to neurological and cognitive assessments. However, the application to traffic medicine has – to the knowledge of the authors – not yet been investigated. Given the experience that was already gained with such analyses in neurology and the (cost) efficiency of the method, it seems straightforward to explore the possibility to apply this method in related fields.
Neuropsychological tests such as the Clock Drawing Test and the Mini-mental State Examination [14] are often used to check for signs of dementia in the elderly and are also recommended as part of a medical examination to assess the ability to drive [15]. Saccade tests, however, have the advantage, owing to the difficulty of diagnosing the earliest stages of dementia, of being more sensitive to underlying brain function.
Dementia hinders the performance of complex cognitive tasks such as safely driving a vehicle. With significant growth in the number of older drivers and, concomitantly, the number of individuals living with Alzheimer’s disease or other forms of dementia, early detection of diminished driving capabilities is a critical public safety issue.
In this study, three different saccade paradigms were used to test a group of elderly drivers whose fitness to drive was questioned by the road authorities. The paradigms included prosaccades, antisaccades and volitional, visually induced (VVI) saccades, and thus covered saccadic tasks of different cognitive complexity. The results were compared with a comparison group of similar age, a younger comparison group and a group of patients with an established diagnosis of a brain lesion, in order to determine if the analysis of saccadic eye movements would enable identification of the impaired elderly drivers.
Methods
The experiments conducted in this study were approved by the responsible ethics committee of the Canton of Zurich, Switzerland (Permission no. 723/08).
Participants
Four different groups of volunteers were recruited into this study (table 1). The group of primary interest (Group LM) consisted of 21 elderly drivers who came to the attention of road authorities because of their involvement in a car accident or referral by a general physician. Based on Swiss law, these individuals were required to be checked at the Institute of Legal Medicine in order to keep their driving license. All individuals of this group were recruited at this institute.
For comparison, a group of elderly individuals, who were enrolled at the University of Zurich’s Senior Citizens’ University, participated in this study (Group EC). All senior-citizen controls possessed a driver’s license and stated that they regularly drove. Furthermore, 42 neurology patients, previously diagnosed with a brain lesion, were recruited at the Department of Neurology, University of Zurich (Group NP): 12 patients had frontal lobe lesions, 14 had lesions also partly involving the frontal lobe, and the remaining 16 had lesions in other brain areas. Finally, there was a comparison group of 34 younger, healthy volunteers (Group YC). Volunteers were recruited during a period of one year, resulting in different numbers of participants per group.
Procedures
All groups performed the same saccadic eye tests as described below. In addition, Group LM was examined at the Institute for Legal Medicine and took a practical road test, whereas Group NP underwent a medical examination at the Department of Neurology. Individuals in comparison groups EC and YC were questioned by a physician to exclude persons with obvious impairments, but were not examined in more detail.
Medical examination
Group LM was examined according to the legal requirements for driving, which include neuropsychological tests such as the Clock Drawing Test and the Mini-Mental State Examination. All examinations were conducted by the same experienced examiner at the Institute of Legal Medicine. As part of this study, Group NP had to undergo a neuropsychological test battery – including the above-mentioned tests – in the Neuropsychological Unit of the Department of Neurology.
Driving test
At the Institute of Legal Medicine, an integral part of the fitness to drive check for elderly drivers was a practical road test in the city of Zurich. A driving instructor and the physician who was responsible for the medical examination accompanied the elderly driver. The driving test can only be passed or failed; an overall assessment of the driving trial is made. The results of the road test, together with the outcome of the medical examination, formed the basis for the final recommendation of whether or not the individual was able to continue driving a motor vehicle. It should be noted that the results of the saccadic eye tests were not available to the physician; thus the decision on whether a person was regarded as fit to drive or not was based solely on the medical examination and the on-road driving test.
Saccade measurements
Saccadic eye movements were recorded using state-of-the-art methodology. A table-mounted, video-based infrared (IR) eye tracker device (OCULOMETRICS, Zurich, Switzerland), with a sampling rate of 250 Hz and a spatial resolution of 0.1°, was used. This spatial resolution is comparable to that of the commonly used (but invasive) magnetic search coil technique [16, 17]. Subjects were seated comfortably at a table with a soft chin rest. A LCD monitor (Asus MW221U, 1680 x 1050 pixel, refresh rate: 60 Hz, response time: 2 ms) for presenting stimuli was positioned in front of them. Three sessions with different saccade paradigms, but using the same stimulus (0.8 x 0.8°, maximum luminance of the monitor, background: black [i.e. luminance ≤1 cd/m2]), were conducted. Standardised instructions explaining each task were given to all participants . After each recording session, eye movements were evaluated by tracking both the pupil and the limbus, and stored for offline analysis (see [18] for details).
The paradigm sessions were run in the following order:
a) A simple, visually guided prosaccade paradigm was used to assess the state of reflexive eye movements. The target was presented on a black background at 5, 10, 15 and 20 degrees eccentricity to the right and left, with the same randomised sequence of trials for all sessions and subjects.
b) An antisaccade task, which used the same number of targets at the same degrees eccentricity as in the prosaccade paradigm, required the participant to voluntary decouple stimulus encoding and response preparation.
c) Using the prosaccade setup, but with 300 additional, randomly distributed vertical elements (0.2 x 0.8°) in the background to create disturbance, the performance of volitional, visually induced saccades (VVI) was tested. The elements in the background were moving (top to bottom of the screen), but did not cover the targets at any time.
Each session consisted of 126 saccadic trials.
Statistical analysis
All saccade data were analysed with MATLAB software (MATLAB R2011b, The Math Works Inc. Natick, MA). Abnormal eye movements and blinks were excluded from further evaluation. For each session, the so-called main sequence (see e.g. [5]), which includes the eye velocity, was established. Furthermore, latency parameters were evaluated and the number of correctly performed saccades for all targets and separately for near (5 and 10 degrees eccentricity to the right and left) and far targets (15 and 20 degrees eccentricity) were counted. The data were z-transformed to analyse differences between groups in terms of mean values and standard deviations.
The performance of the groups was compared by one-sided analysis of variance (ANOVA) including a Scheffe’s post hoc test (α = 0.05). The focus was on the performance of the group of elderly drivers (Group LM) in comparison to the other groups.
|
Table 1: Participants. |
|
Group
|
Number
|
Age (years, mean ± SD)
|
Age (years, median)
|
Driving experience (years, mean ± SD)
|
| YC: Young comparison group |
34 |
30 ± 7.1 |
28 |
12 ± 6.9 |
| EC: Elderly comparison group |
47 |
75 ± 4.0 |
74 |
42 ± 9.6 |
| LM: Patients at Dept. of Legal Medicine |
21 |
79 ± 3.9 |
79 |
30* ± n/a |
| NP: Patients at Dept. of Neurology |
42 |
53 ± 14.2 |
50 |
31 ± 11.3 |
| * Several participants were not able to precisely specify their driving experience; all reported to have much more than 30 years of experience. |
|
Table 2: Results of the examination and driving test of Group LM (patients at the Department of Legal Medicine).. |
|
Participant no.
|
Age (years)
|
Positive driving trial
|
Diagnosis based on medical / neuropsychological examination
|
| 109_00126 |
77 |
|
Light cortical and subcortical dementia |
| 110_00174* |
79 |
|
Early stage dementia, possibly Alzheimer’s disease |
| 111_00287* |
79 |
|
Possible dementia, sleeping disorder |
| 112_00454 |
74 |
|
Frontal dementia |
| 113_00266* |
84 |
|
Dementia |
| 114_00512 |
76 |
X |
Mild cognitive impairment, dementia |
| 115_01036 |
80 |
|
Obliviousness |
| 116_00651 |
76 |
X |
Light dementia |
| 117_00349* |
81 |
|
Frontal dementia |
| 118_01142 |
78 |
|
Frontal dementia |
| 119_01025 |
83 |
|
Light dementia |
| 120_01147* |
83 |
X |
Mild cognitive impairment |
| 121_00036 |
81 |
|
Light, frontal dementia |
| 122_01384* |
79 |
X |
Possibly cognitive disorder, logorrhoea |
| 123_02572 |
82 |
X |
Complicated, conspicuous behaviour |
| 124_01487 |
90 |
|
Light dementia |
| 125_01613 |
83 |
X |
Light vascular dementia |
| 126_00105 |
76 |
|
Light dementia |
| 127_00161 |
78 |
X |
Cardiopathy, subdural haematoma |
| 128_00437 |
75 |
|
Frontal dementia |
| 129_00434 |
75 |
X |
Light frontal dementia |
| * Indicates female participants. |
Results
The recruitment process for this study resulted in a total of 144 participants (table 1). Group LM, the elderly drivers who came to the attention of the road authorities, were the smallest and oldest group (21 persons including 6 females, mean age ± standard deviation 79 ± 3.9 years). Their driving experience was much longer than 30 years although some participants were unable to give precise dates. The age-matched comparison group (Group EC) consisted of 47 persons of a mean age of 75 ± 4.0 years and with a mean length of driving experience of 42 years. The group of patients at the Department of Neurology included 42 persons who had a younger average age (53 ± 14.2 years), but also a long driving experience, of 31 years on average. Overall, 26 of those 42 persons were diagnosed with a (partial) frontal brain lesion. The young comparison group was composed of 34 persons of 30 ± 7.1 years of age with a driving experience of 12 years (mean).
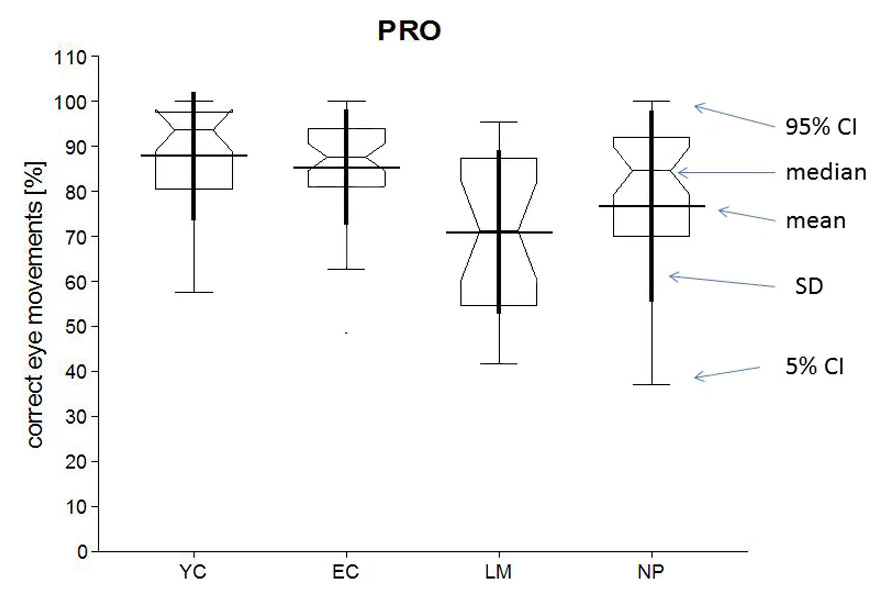
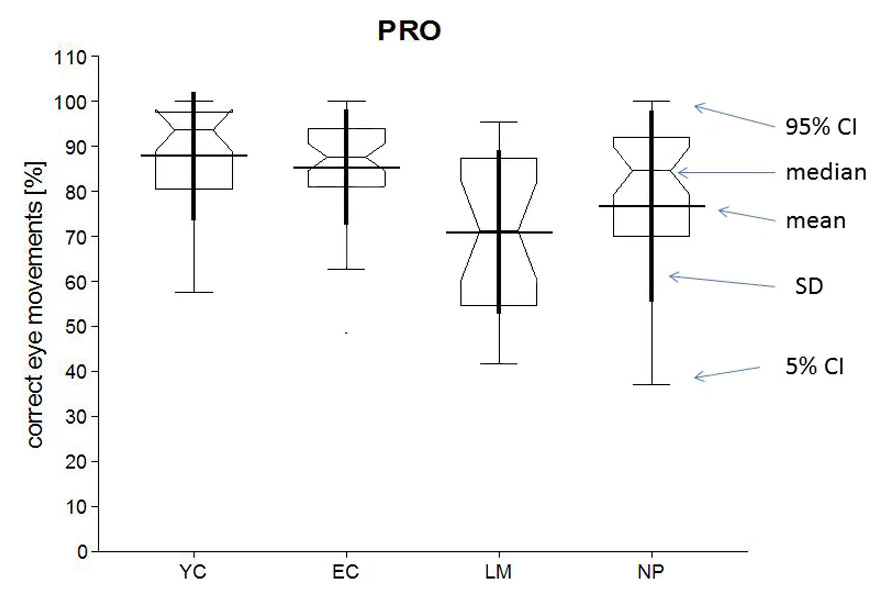
Figure 1
Evaluation of all prosaccades for all groups. The percentage of correctly performed eye movements is presented; boxes indicate the distribution of the data include mean and SD (thick line), median, confidence intervals (5%, 95%) and outliers (single dots).
EC = elderly comparison group; LM = patients at the Department of Legal Medicine; NP = patients at the Department of Neurology; YC = young comparison group
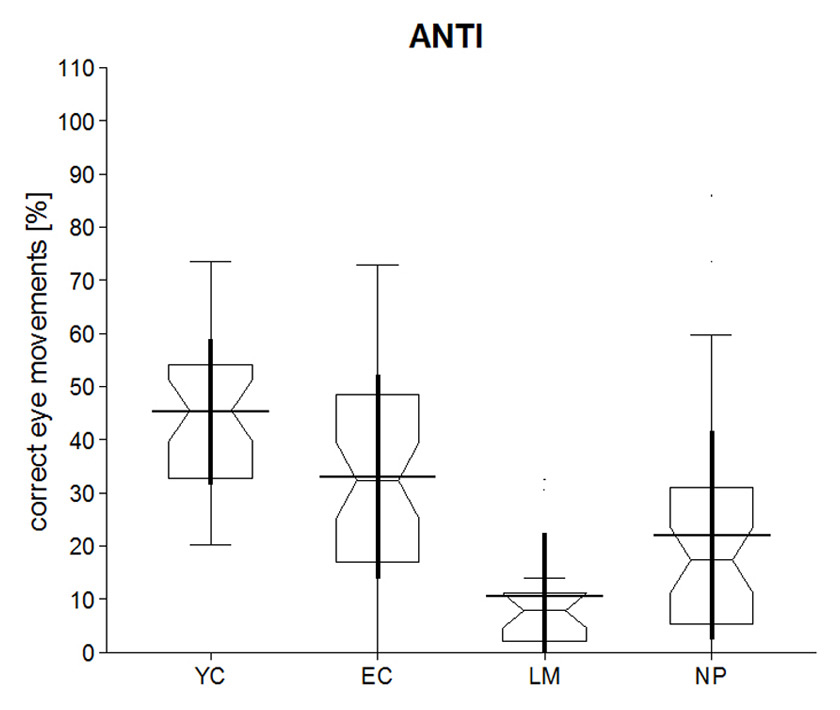
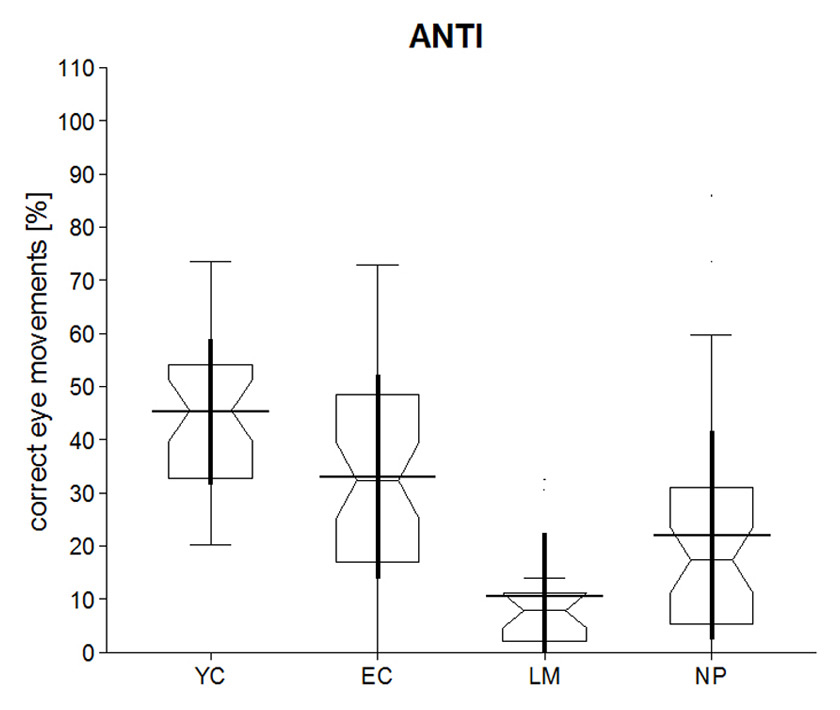
Figure 2
Evaluation of all antisaccades for all groups.
EC = elderly comparison group; LM = patients at the Department of Legal Medicine; NP = patients at the Department of Neurology; YC = young comparison group

Figure 3
Evaluation of all visuovisual interactive (VVI) saccades for all groups.
EC = elderly comparison group; LM = patients at the Department of Legal Medicine; NP = patients at the Department of Neurology; YC = young comparison group
The medical examination (including neuropsychological tests) of 21 elderly drivers (Group LM) revealed that 16 persons showed signs of dementia. Only eight individuals in Group LM performed adequately in the road test (table 2).
The results of the saccade tests are presented in figures 1–3. The figures summarise the percentage of correctly performed saccades, such that the eye-movement data of the different groups can be compared for all three paradigms. Overall 54,432 saccades were presented to the volunteers; excluding abnormal eye movements and blinks a total of 35,292 saccades for all volunteers were analysed (64.8% of all saccades presented). The percentage of saccades that could be analysed differed between the different groups. For the young comparisons (Group YC) 77.1% of all saccades could be included in the statistical analysis, for the elderly comparisons (Group EC) 69.0%, for the neurology patients (Group NP) 58.7%, and for the group of elderly drivers (Group LM) 48.0%. Table 3 summarises the results of the different parameters that were measured and table 4 presents the results of the analysis of variance (ANOVA) with regard to our target group (Group LM).
When comparing correctly executed prosaccades, it was observed that Groups LM and NP showed a slightly decreased performance and more variability than Groups YC and EC, whereas both comparison groups exhibited a similar saccadic performance. However, these results were not statistically significant (table 4).
In the antisaccade task, Group LM had a significantly lower number of correctly performed antisaccades than both comparison groups. A mean value of 10.6% (±12.0% SD) correctly performed eye movements was recorded for Group LM. Patients with brain lesions (Group NP, 22.1% ± 19.7%) performed better than Group LM, but the difference was not statistically significant. Older controls (Group EC) achieved a mean of 33.1% (±19.1%) correct, and the younger comparison group (Group YC) a mean of 45.3% (±13.7%) correct. Group YC performed significantly better than all groups, including the older controls. Both comparison groups made significantly more correct antisaccades than Groups LM and NP.
Concerning the VVI paradigm, it was found that Group YC achieved a significantly higher percentage of correct trials compared with Group LM (and all other groups). In addition, Group LM had fewer correct trials than the older comparison group.
The results show that most statistically significant differences were found with respect to the number of correct saccades. Latency was prolonged for Group NP in the prosaccade tasks, but elderly participants (Groups LM and EC) did not show any significant latency effects. The velocity of the eye movement was significantly slower for elderly drivers in Group LM only in the prosaccade condition.
Furthermore, Group NP was analysed separately such that patients with frontal lesions, partial frontal lesions and lesions in other brain areas were compared. No statistical significant difference was found in any parameter. Consequently the presentation of detailed results of this additional analysis was omitted and Group NP was regarded as one group when performing the ANOVA to check for differences with respect to the target group of this study (i.e., Group LM).
|
Table 3: Summary of the results. For all paradigms and all groups (LM, AC, EC, NP) mean and standard deviation (SD) are presented. Units are % for the number of correct saccades, ms for latency, °/s for velocity. |
|
|
Group LM
|
Group YC
|
Group EC
|
Group NP
|
|
Paradigm/parameter
|
Mean
|
SD
|
Mean
|
SD
|
Mean
|
SD
|
Mean
|
SD
|
|
Prosaccade task
|
|
|
|
|
|
|
|
|
| Number of correct saccades (all) |
71.0 |
18.1 |
87.9 |
14.3 |
85.4 |
12.8 |
76.7 |
21.6 |
| Number of correct saccades (near target 5°, 10°) |
73.5 |
17.9 |
89.4 |
13.4 |
86.0 |
13.9 |
79.6 |
21.0 |
| Number of correct saccades (far targets, 15°, 20°) |
68.5 |
21.3 |
86.3 |
15.6 |
84.7 |
13.6 |
73.8 |
22.8 |
| Latency (mean) |
233.0 |
39.9 |
228.6 |
20.3 |
204.9 |
36.4 |
281.6 |
46.7 |
| Velocity V0 (mean) |
399.8 |
89.2 |
509.9 |
97.4 |
462.5 |
82.2 |
460.7 |
86.3 |
|
Antisaccade task
|
|
|
|
|
|
|
|
|
| Number of correct saccades (all) |
10.6 |
12.0 |
45.3 |
13.7 |
33.1 |
19.1 |
22.1 |
19.7 |
| Number of correct saccades (near target 5°, 10°) |
11.9 |
13.5 |
49.4 |
16.6 |
37.4 |
21.1 |
24.7 |
20.2 |
| Number of correct saccades (far targets, 15°, 20°) |
9.2 |
12.8 |
41.2 |
15.3 |
28.8 |
19.9 |
19.5 |
21.3 |
| Latency (mean) |
332.7 |
62.8 |
354.3 |
34.6 |
313.5 |
44.0 |
362.4 |
74.6 |
| Velocity V0 (mean) |
398.9 |
67.0 |
421.3 |
86.1 |
399.6 |
82.9 |
410.4 |
130.6 |
|
VVI task
|
|
|
|
|
|
|
|
|
| Number of correct saccades (all) |
41.2 |
21.7 |
89.6 |
10.2 |
68.8 |
17.5 |
58.4 |
26.2 |
| Number of correct saccades (near target 5°, 10°) |
57.3 |
26.0 |
93.4 |
10.8 |
82.6 |
12.3 |
70.8 |
25.7 |
| Number of correct saccades (far targets, 15°, 20°) |
25.1 |
20.9 |
85.7 |
12.3 |
55.0 |
34.1 |
46.1 |
29.8 |
| Latency (mean) |
293.6 |
45.1 |
261.5 |
24.5 |
256.2 |
40.5 |
331.1 |
46.4 |
| Velocity V0 (mean) |
439.3 |
103.0 |
515.6 |
95.7 |
467.3 |
78.5 |
448.1 |
79.6 |
| EC = elderly comparison group; LM = patients at the Department of Legal Medicine; NP = patients at the Department of Neurology; VVI = visuovisual interactive; YC = young comparison group |
|
Table 4: Summary of analysis of variance (Scheffe’s post hoc test, α = 0.05) for all tasks and all parameters. The table provides p-values for comparison of Group LM with other groups. |
|
Paradigm/parameter
|
Comparing Group LM with…
|
|
|
Group YC
|
Group EC
|
Group NP
|
|
Prosaccade task
|
|
|
|
| Number of correct saccades (all) |
0.19003 |
0.32259 |
0.99428 |
| Number of correct saccades (near target 5°, 10°) |
0.21621 |
0.47845 |
0.98864 |
| Number of correct saccades (far targets, 15°, 20°) |
0.26834 |
0.31324 |
0.99843 |
| Latency (mean) |
1.00000 |
0.68860 |
0.04028*
|
| Velocity V0 (mean) |
0.02627*
|
0.58477 |
0.80921 |
|
Antisaccade task
|
|
|
|
| Number of correct saccades (all) |
0.00001*
|
0.02410*
|
0.80921 |
| Number of correct saccades (near target 5°, 10°) |
0.00001*
|
0.01387*
|
0.78994 |
| Number of correct saccades (far targets, 15°, 20°) |
0.00031*
|
0.14366 |
0.91601 |
| Latency (mean) |
0.99298 |
0.99604 |
0.94228 |
| Velocity V0 (mean) |
0.99991 |
1.00000 |
1.00000 |
|
VVI task
|
|
|
|
| Number of correct saccades (all) |
0.00000*
|
0.01170*
|
0.50550 |
| Number of correct saccades (near target 5°, 10°) |
0.00003*
|
0.01404*
|
0.73568 |
| Number of correct saccades (far targets, 15°, 20°) |
0.00000*
|
0.04159*
|
0.48578 |
| Latency (mean) |
0.68132 |
0.38074 |
0.42812 |
| Velocity V0 (mean) |
0.40825 |
0.99618 |
1.00000 |
| EC = elderly comparison group; LM = patients at the Department of Legal Medicine; NP = patients at the Department of Neurology; VVI = visuovisual interactive; YC = young comparison group
* Denotes significant p-values |
Discussion
The saccadic eye movements of elderly drivers who had come to the attention of road authorities were compared with patients with brain lesions, a younger- and an older-aged comparison group, using state-of-the-art methodology for measuring saccades in various experimental paradigms. The results indicate that elderly drivers with poor driving performance also exhibit a high error rate in the antisaccade and VVI task.
Different group sizes and a limited sample size, particularly of the group of elderly drivers who were believed unfit to drive by the road authorities, represent limitations of this study. Statistical measures (z-transformation) were therefore used to allow comparisons. However, it should be noted that the evaluation of saccadic eye movements is a well-validated technique; distinction of healthy and pathological performance is thus possible for small sample sizes owing to the large amount of available reference data. Additionally it should be pointed out that some of the data (figs 1–3) are obviously not normally distributed, but skewed. Nonetheless an analysis of variance (ANOVA) was performed to compare the four groups. Although ANOVA is robust with respect to a violation of the assumption of normality [19], this should be kept in mind even if the poor performance of the group of elderly drivers in some task (e.g. the antisaccade task) can easily be observed in the corresponding box plots (fig. 2).
Since the older comparison group was recruited at the University of Zurich’s Senior Citizens’ University, it was assumed that the incidence of dementia was low; however, no detailed medical or neuropsychological tests were conducted, which is a further limitation of the present study. The older controls comprised the largest in number and performed significantly better on experimental tasks than both the compromised elderly drivers and the neurology patients, so we believe that dementia was not a relevant contributing factor in their saccadic performance.
The medical and neuropsychological examinations indicated that most of the elderly drivers in Group LM suffered from dementia, primarily at an early stage. Most of these drivers failed the practical road test, although it should be noted that no quantitative evaluation of their driving behaviour/skills is available. As is common practice in Switzerland today, an overall assessment of fitness to drive was derived; thus, a failure cannot be clearly attributed to any specific aspects of the driving task that might be affected by dementia.
As expected, the younger comparison group demonstrated the best possible performance with results comparable to published data for prosaccades [20] and VVI saccades [21].
The younger subjects made more correct eye movements in all experimental conditions, although the difference was not significant in the prosaccade condition. The older comparison group performed similarly to the younger ones in the prosaccade condition, but a significant difference existed on the antisaccade and VVI tasks. This finding can possibly be interpreted in view of a presenile condition as reported in the literature [22]. Despite this poor VVI performance, individuals in the older comparison group reported that they regularly drive their cars. Thus, while VVI seems very sensitive to early changes in cognitive ability, the strength of its link to driving ability is more difficult to assess here. An even worse performance on the VVI task by Group LM indicates that VVI performance can be correlated with the ability to drive. However this test may be less sensitive towards early changes in driving ability because individuals with a significant reduction in VVI performance would presumably notice the deterioration themselves and abstain from driving on a regular basis. This, however, assumes that drivers would become aware of weaker VVI performance. A gradual development of impairment over time, on the other hand, might make it difficult for older persons to detect the level of impairment when driving should be stopped. Additionally, the convenience of driving may outweigh a perceived impairment in individual cases.
The number of correctly performed saccades was the parameter that varied the most between the groups participating in this study. Generally, it was observed that error rates in some tasks were higher than expected. This can, for example, be seen in the young and elderly comparison groups which performed the anti-saccadic task rather poorly. Given that the experimental set-up, the instructions and the data analysis were the same for all groups, this finding does not influence the comparison between the groups. Possibly the recruitment process was different compared to some other studies such that here only inexperienced subjects participated. Additionally it can be suspected that participants showed a somewhat timid behaviour as they were aware that their performance was analysed in the context of the ability to driving. For the elderly comparison group that represented an average age of 75 years (close to our target group of elderly drivers) some age-related factors could be involved (see also above). Nonetheless the poor performance cannot be fully explained.
Other parameters such as latency or the velocity of eye movements were hardly influenced in this study.
The elderly drivers of Group LM always performed worse than the comparison group of similar age (EC). The prevalence of dementia in Group LM most likely explains this difference. The difference was not significant in the prosaccade test, but it was highly significant in the antisaccade and VVI tasks.
The patients with established brain lesions and the compromised elderly drivers showed similar eye-movement results. Since the patients mainly suffered from frontal brain lesions, we speculate that the results of elderly drivers was also caused by limitations in frontal lobe functioning [23, 24].
In summary, antisaccadic eye movements were found to be sensitive in distinguishing the group of impaired elderly drivers from the other groups in this study. This paradigm was identified as the best differentiator with respect to the focus group of this study. Since performance of antisaccades involves mainly frontal brain regions, a reduced capacity in this region could explain the poor performance of Group LM. This finding is striking because the same group of elderly drivers showed inadequate driving skills during a road test. The results indicate that elderly drivers who fail on driving tests show similar deficits in saccadic eye movements as a group of patients with mainly frontal brain lesions. Testing saccadic eye movements might thus have the potential to work as early identification of at-risk drivers. Therefore future studies should further investigate the relationship between a bad performance in antisaccadic eye tests and specific driving skills as required to safely conduct a vehicle in different traffic situations. This holds particularly true as the measurement of saccades allows screening of large numbers of people and thus fulfils an important practical requirement for examining the fitness to drive in the elderly. The screening of saccadic eye movements therefore does not only elucidate the mental status of a driver (or/and possible adverse effects of medication), but it provides advice to the driver and his/her family to consider critically driving in public.
Acknowledgement:We thank the administrative and technical staff at the institutions involved for support.
References
1 Fildes BN, Charlton J, Pronk N, Langford J, Oxley J, Koppel S. An Australasian model license reassessment procedure for identifying potentially unsafe drivers. Traffic Injury Prevention. 2008;9(4):350–9.
2 Wheatley CJ, Di Stefano M. Individualized assessment of driving fitness for older individuals with health, disability, and age-related concerns. Traffic Injury Prevention. 2008;9(4):320–7.
3 Hallett PE. Primary and secondary saccades to goals defined by instructions. Vision Res. 1978;18:1279–96.
4 Everling S, Fischer B. The antisaccade: a review of basic research and clinical studies. Neuropsychologia. 1998;36:885–99.
5 Schwarz U. Neuroophthalmology: a brief Vademecum. Eur J Radiol. 2004;49(1):31–63.
6 Munoz DP, Everling S. Look away: the anti-saccade task and the voluntary control of eye movement. Nat Rev Neurosci. 2004;5(3):218–28.
7 Pierrot-Deseilligny C, Rivaud S, Gaymard B, Agid Y. Cortical control of reflexive visually-guided saccades. Brain. 1991;114(Pt 3):1473–85.
8 Gaymard B, Ploner CJ, Rivaud S, Vermersch AI, Pierrot D. Cortical control of saccades. Exp Brain Res. 1998;123:159–63.
9 Leigh RJ, Kennard C. Using saccades as a research tool in the clinical neurosciences. Brain. 2004;127(3):460–77.
10 Pierrot-Deseilligny C, Milea D, Muri RM. Eye movement control by the cerebral cortex. Curr Opin Neurol. 2004;17:17–25.
11 Hutton SB. Cognitive control of saccadic eye movements. Brain Cogn. 2008;68(3):327–40.
12 Garbutt S, Matlin A, Hellmuth J, Schenk A, Johnson J, Rosen H, et al. Oculomotor function in frontotemporal lobar degeneration, related disorders and Alzheimer's disease. Brain. 2008;131(5):1268–81.
13 Anderson T, MacAskill M. Eye movements in patients with neurodegenerative disorders. Nat Rev Neurol. 2013;9:74–85.
14 Folstein MF, Folstein SE, McHugh DR. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J Psychiatry Res. 1975;12:189–98.
15 Mosimann UP, Bächli-Biétry J, Boll J, Bopp-Kistler I, Donati F, Kressig RW, et al. Konsensusempfehlungen zur Beurteilung der medizinischen Mindestanforderungen für Fahreignung bei kognitiver Beeinträchtigung (Consensus recommendations for the assessment of fitness to drive in cognitively impaired patients). Praxis. 2012;101(7):451–64.
16 Collewijn H, van der Mark F, Jansen TC. Precise recording of human eye movements. Vision Res. 1975;15(3):447–50.
17 Robinson DA. A method of measuring eye movement using a scleral search coil in a magnetic field. IEEE Trans Biomed Eng. 1963;10:137–45.
18 Schmitt KU, Muser MH, Lanz C, Walz F, Schwarz U. Comparing eye movements recorded by search coil and infrared eye tracking. J Clin Monit Comput. 2007;21(1):49–53.
19 McDonald J. Handbook of Biological Statistics (3rd ed.). Sparky House Publishing, Baltimore, Maryland. 2014
20 Becker W. Metrics. In: Wurtz RH, Goldberg ME, editors. The neurobiology of saccadic eye movements Reviews of oculomotor research Vol 3. New York: Elsevier. 1989;13–67.
21 Schwarz U, Baumann K, Ilg U. Influence of global motion onset on goal-directed eye movements. NeuroReport. 2010;21(7):479–84
22 Crawford TJ, Higham S, Renvoize T, Patel J, Dale M, Suriya A, et al. Inhibitory control of saccadic eye movements and cognitive impairment in Alzheimer's disease. Biol Psychiatry. 2005;57(9):1052–60.
23 Corbetta M, Akbudak E, Conturo TE, Snyder AZ, Ollinger JM, et al. A common network of functional areas for attention and eye movements. Neuron. 1998;21:761–73.
24 Sakai H, Takahara M, Honjo NF, Doi S, Sadato N, Uchiyama Y. Regional frontal gray matter volume associated with executive function capacity as a risk factor for vehicle crashes in normal aging adults. PLoS One. 2012;7(9):