Associations between alcohol use expectancies and drinking problems among French soldiers
DOI: https://doi.org/10.4414/smw.2015.14101
Vanessa
Marbac-Delon, Marie-Aude
Créach-Juzan, Jonathan
Gillard, Marc
Saintot, Aurélie
Mayet
Summary
AIMS: The aim of the study was to evaluate which alcohol use expectancies could predict harmful use in the French Army to explore some hypotheses concerning socialising or coping effects.
METHODS: A cross-sectional survey, using self-administered questionnaires, was conducted in two Army units in 2011 (n = 249). Hazardous alcohol use and dependence were screened using the Alcohol Use Disorders Identification Test (AUDIT). Alcohol expectancies were measured with the Alcohol Effects Questionnaire (AEFQ). A cluster analysis was performed to identify AEFQ dimensions in our sample. Relationships between AUDIT and AEFQ were explored using multinomial logistic regression.
RESULTS: According to AUDIT, 46.6% of soldiers used alcohol without hazard, 26.1% had hazardous use without dependence and 18.1% had use with dependence. The AEFQ had an adequate internal coherence with a 0.78 α coefficient. The scales identified by the cluster analysis in our sample fitted those retained in the originally validated AEFQ, with a correspondence ranging from 60% to 100%. In multivariate analysis, the scale “Social and physical pleasure” was associated with increasing hazardous use and subjects who scored higher on “Global positive” and “Social and physical pleasure” scales were more at risk of dependence.
CONCLUSION: The present study, in line with previous research in terms of importance of alcohol use disorders among military personnel, found that alcohol use expectancies are associated with alcohol misuse among soldiers. This could suggest underlying coping mechanisms towards stress that have to be further explored.
Introduction
A number of studies reported that excessive drinking and related harms are common among military personnel and that a higher percentage of active-duty military personnel misuse alcohol compared with civilian populations for the same age strata and genders [1–4]. Alcohol use disorders (AUD: hazardous use or dependence) are also observed in the Army, where personnel are particularly exposed to operational situations liable to induce stress and psychological disturbances that can lead to psychoactive substance use [4–6]. Indeed, acute hazardous use of alcohol, such as binge drinking or recurrent drunkenness, was observed among 59% of United States active-duty soldiers in 2005 and 56% of French active-duty soldiers in 2006 [7–8].
AUD and related harms could be considered as conflicting with the imperatives of the military profession, particularly in an operational setting. Thus, some studies have shown that AUD are associated with a high percentage of non-combat-related hospitalisations and deaths, usually the result of unintentional injuries, among military personnel, particularly if considering certain specific features of military professions (carrying weapons, piloting heavy vehicles or aircraft, etc.) [9–11]. Moreover, AUD involve a significant risk of impairment in operational activities and safety, as a result of lack of readiness [12].
However, a study of the main conflicts of the 20th century shows that alcohol has traditionally been used by the military to cope with the intense stress of battle, and also as a way of mediating the transition from the heightened experience of combat to routine safety [13]. Within the military, alcohol is also often claimed to have some positive effects: assisting in group bonding during training, raising the moral, providing confidence during battle and aiding unit cohesion, military personnel feeling welded into the same “family” [13–14].
However, agreement with a positive role of alcohol in the armed forces is based on the assumption that military personnel drink responsibly within safe limits, which is not in line with the high AUD prevalences observed in the armed forces of several countries [2–3]. Thus, in recent years, the short-term effects of alcohol on function have been addressed by tight restrictions in operational theatres [4]. The longer-term consequences of social and corporate drinking in the armed forces are more difficult to assess. The disparities existing between prohibitive alcohol policies in different military nations show the difficulty of striking an appropriate balance between responsible and harmful drinking, between public health and traditional military culture [4]. In this setting, we wanted to explore which motives for alcohol use were likely to induce AUD among soldiers, in order to identify targets for future health education programmes.
Thus, after estimating the prevalence of AUD in a sample of French soldiers, the main aim of the present study was to explore the relationships between alcohol use expectancies, screened with the Alcohol Effects Questionnaire (AEFQ), and AUD. The secondary aim was to evaluate the internal consistency of the AEFQ in this population.
Methods
Sample
A cross-sectional survey, based on self-administered questionnaires, was conducted in 2011 in two operational units of the Army stationed in continental France: one combat unit (infantry) and one logistical unit (supply). In each unit, we randomly selected a company (group that usually includes around 100–150 personnel under the command of a captain). The inclusion criteria were to be active-duty personnel, to be present in the unit on the day of survey and to agree to participate. The purpose of the survey was explained to the participants prior to questionnaire completion. Then the questionnaires, including socio-demographic characteristics and alcohol use variables, were completed by the listed personnel in a single session. Several methods were used to preserve participant anonymity: questionnaires were pre-identified with anonymous code numbers, the same questionnaire response time was allowed for all subjects (substance users and nonusers), envelopes containing the questionnaires were sealed in front of the participants immediately after completion, and participants had the possibility to refuse to participate or the option to leave it blank. This protocol was approved by the ethical committee of the French military health service. A total of 249 subjects participated.
Measures
AUD were identified using the French version of the Alcohol Use Disorders Identification Test (AUDIT) [15–16]. A score ranging between 7 and 11 for men (6–11 for women) defined hazardous use (sensitivity [Se] = 84% and specificity [Sp] = 80% among men; Se = 81% and Sp = 94% among women), and a score over 13 defined a risk for dependence for both genders (Se = 70% and Sp = 95% among men; Se = 95% and Sp = 98% among women). Alcohol expectancies were measured with the Alcohol Effects Questionnaire (AEFQ) [17], a revision and extension of the Alcohol Expectancy Questionnaire (AEQ) of Brown et al. [18], which was developed as a brief method of assessing both positive and negative effects people expect alcohol to have on themselves. This questionnaire includes 40 true/false rated items exploring six positive outcomes (Global Positive [POS], Social and Physical Pleasure [SPP], Sexual Enhancement [SEX], Power and Aggression [AGG], Social Expressiveness [SOC], Relaxation and Tension Reduction [REL]) and two negative outcomes (Cognitive and Physical Impairment [IMP] and Careless Unconcern [CU]). AEFQ items were translated into French, followed by a back translation. This was simplified by the correspondence between some AEFQ items with AEQ items that were already translated [19].
Statistical analyses
Analyses were performed using the Stata 11.1 software (Statacorp.). Internal consistency of the AEFQ and its eight scales was evaluated using the Cronbach α-coefficient. The AEFQ dimensions emerging in our sample were identified using a Ward cluster analysis performed on the 40 items. We explored the determinants of AUD using three stages of modelling. First, we performed a multinomial logistic regression (outcome: categorised AUDIT; reference: nonhazardous use) to study the impact of socio-demographic characteristics (gender, age, rank, military unit, lifetime deployment history and time elapsed since the last deployment). A multiple linear regression was then used to explore the relationships between alcohol consumption modalities and AUD. Finally, the relationships between AEFQ scores and AUD were studied using another multinomial logistic regression (outcome: categorised AUDIT; reference: nonhazardous use). These models had an exploratory purpose, and so they included all the variables studied at each stage without a selection procedure. A 5% significance level was chosen for all the analyses.
Results
Population
No-one refused to participate, but 23 subjects did not complete the AUDIT during the session (9.2%). These subjects did not differ from the responders in terms of gender (p = 0.5), age (p = 0.3), rank (p = 0.09) and unit (p = 0.1). Among the 249 subjects included, 92.3% were men. The combat unit accounted for 54.2% of the sample. The distribution according to rank (5.8% officers, 24.0% non-commissioned officers [NCOs] and 70.2% rank and file [i.e. lowest ranked soldiers who constitute the basis of the hierarchy]) was close to that observed in the French Army as a whole, even if the proportion of rank and file was higher in our sample. Men and younger people were also overrepresented by comparison with the Army as a whole. The mean age was 26.7 years (median = 26 years; interquartile range [IQR] = 23–30 years) and the mean length of service was 6.5 years (median = 4 years; IQR = 2–9 years). Lifetime deployment history concerned 72.3% of subjects and did not differ according to the unit (p = 0.2). The mean time since the last deployment was 1 year (median = 1 year; IQR = 0–7 years), and was shorter in the combat unit (p <0.001).
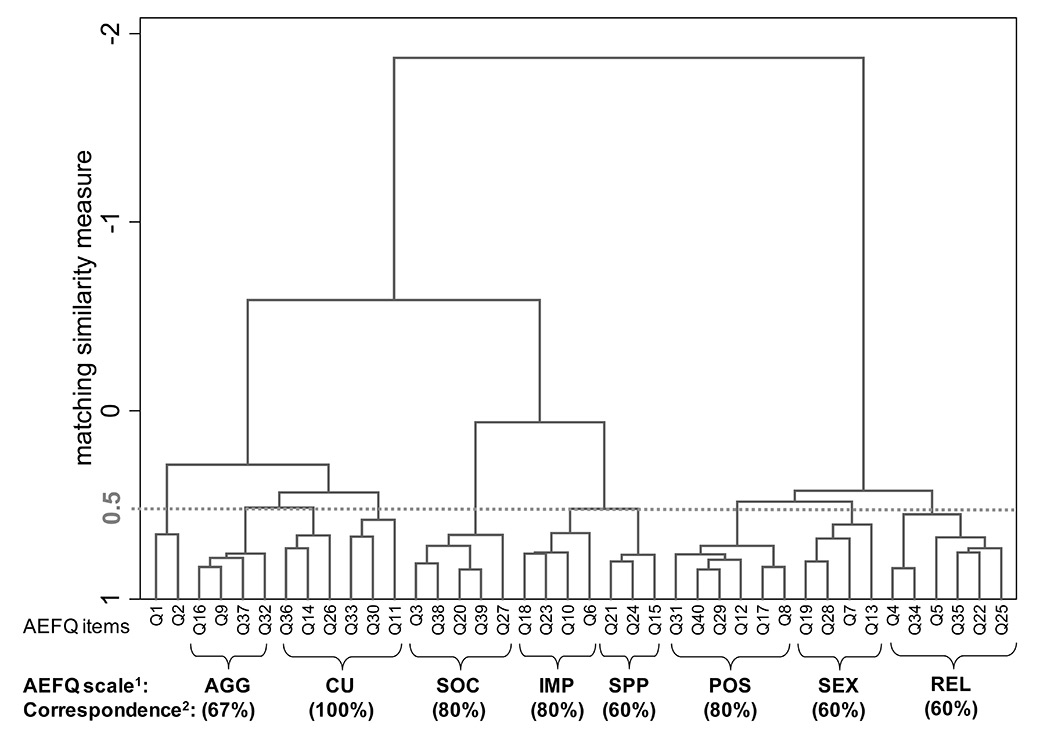
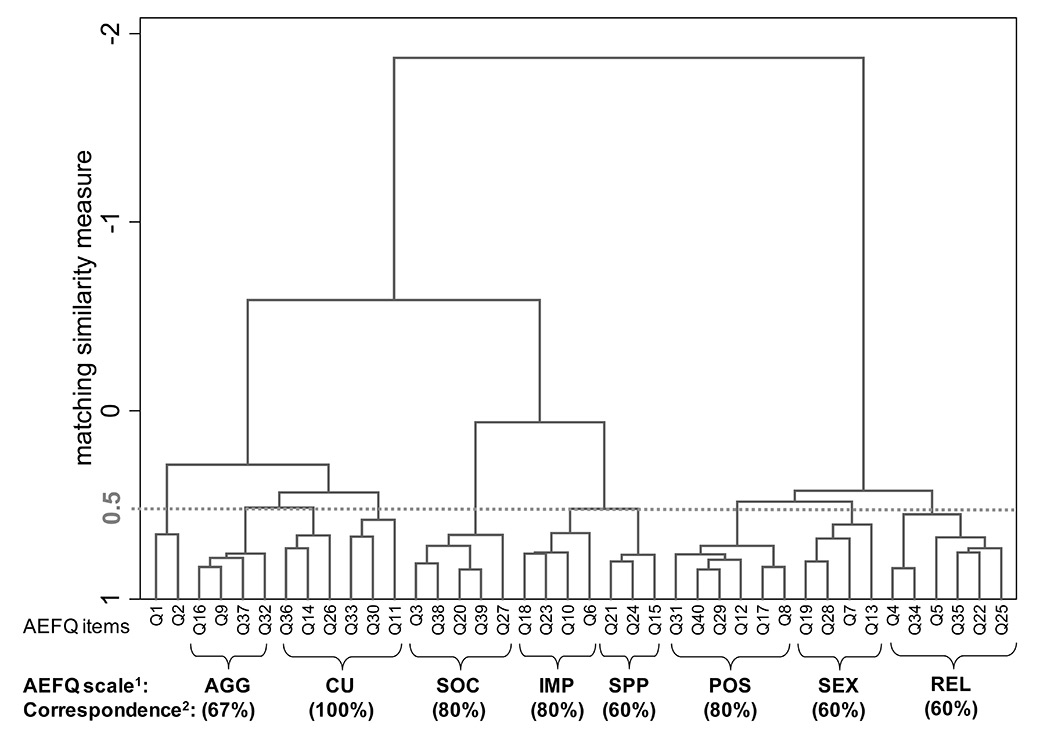
Figure 1
Cluster analysis dendrogram for the 40 items of the Alcohol Effects Questionnaire (AEFQ) – Ward’s linkage analysis.
1. AEFQ scales: Global Positive (POS), Social and Physical Pleasure (SPP), Sexual Enhancement (SEX), Power and Aggression (AGG), Social Expressiveness (SOC), Relaxation and Tension Reduction (REL), Cognitive and Physical Impairment (IMP), and Careless Unconcern (CU).
2. Correspondence, for each scale, between the variables clustered by our analysis and those originally retained in the validated AEFQ.
Note for the interpretation of this figure: the matching similarity measure (y axis) evaluates the degree of clustering of AEFQ items (x axis). For example, concerning the SOC score, we can see that the items Q3 and Q38 are strongly clustered with each other, like Q20 and Q39. Under a 0.5 threshold, we observe that Q3, Q38, Q20, Q39 and Q27 constitute a same cluster. Among these items, four belong to the SOC scale of the originally validated AEFQ that includes itself five items (correspondence of 4/5 or 80%).
Alcohol use patterns
The median age at onset of alcohol use was 15 years (IQR = 13–17 years) and the median age at first drunkenness was 16 years (IQR = 15–18). The mean AUDIT score among the 226 subjects who completed the test (90.8%) was 7.5 (median = 6; IQR = 3–11; range = 0–27): 116 (51.3%) had nonhazardous use, 65 (28.8%) had hazardous use without dependence and 45 (19.9%) could be classified as dependent (46.6%, 26.1% and 18.1%, respectively in the sample as a whole). The internal coherence of the AUDIT scale was adequate (α = 0.80). Bivariate analyses showed that the risk of dependence was greater among younger subjects (odds ratio [OR] = 3.3; 95% confidence interval [CI] 1.6–6.7 under 25 years compared with 25 years and older; p = 0.001), rank and file (OR = 15.6; CI 3.6‒7.7] compared with higher ranks; p <0.001), in the combat unit (OR = 2.3; p = 0.02) and among subject with a shorter time since the last deployment (OR = 0.4; CI 0.2–0.9, for a 1–year shorter time; p = 0.008). Only rank and file (OR = 10.0; 95% CI 1.1–89.2; p = 0.04) and more recent deployment (OR = 0.3 CI 0.1–0.9; p = 0.04) remained significant in multivariate analysis. No woman scored positive for dependence.
Variations of AUDIT score according to modalities of alcohol consumption are presented in table 1. Subjects who reported using alcohol in their family had a significantly lower AUDIT score(6.6 vs 8.3 for those having not reported this kind of use; p = 0.02). However, the AUDIT score was much higher among subjects who reported use at the unit (11.5 vs 6.9; p <0.001), with their colleagues (9.5 vs 6.4; p <0.001) or alone (14.8 vs 7.4 p <0.001). Uses at the unit or alone were still significantly associated with greater AUDIT values (p = 0.02 and p <0.001, respectively) after adjustment for unit, gender and rank.
Relationships between alcohol expectancies and drinking problems
The AEFQ had a satisfactory internal coherence with a global α coefficient equal to 0.78. As shown in table 2, the α values for the eight AEFQ scales ranged from 0.60 to 0.84, the better coherences being observed for the SOC scale (α = 0.84), the AGG scale (α = 0.75) and the SEX scale (α = 0.67).
The cluster analysis identified all AEFQ scales at a 0.5 matching similarity threshold, with the exception of the CU scale, which appeared clustered with the AGG scale (fig. 1). The correspondence between the variables clustered in our analysis and those originally retained in the validated AEFQ for each scale ranged from 60% to 100%. The analysis also retained a 9th cluster consisting of the questions 1 and 2 (“Drinking makes me feel flushed”) and 2 (“Alcohol decreases muscular tension in my body”).
As shown in table 3, in multivariate analysis subjects who had higher POS and SPP scales were more at risk of dependence (OR = 1.9; CI 1.2–3.1; p = 0.01 and OR = 2.5; CI 1.5–4.3; p = 0.001, respectively, for an increase of 1). However, the negative scale IMP appeared to be protective against dependence (OR = 0.7; CI 0.5–1.0; p = 0.05 for an increase of 1). Only the SPP scale was significantly associated with hazardous use without dependence in multivariate analysis (OR = 1.7; CI 1.2–2.3; p = 0.002). Finally, it is interesting to note that in bivariate analyses the SEX scale was significantly associated with both hazardous use (OR = 1.5; CI 1.2–1.9; p = 0.001) and dependence (OR = 1.7; CI 1.3–2.2; p <0.001), SOC and REL scales being also associated with dependence (OR = 1.7; CI 1.3–2.2; p <0.001 and OR; = 1.5; CI 1.2–1.8; p = 0.002, respectively). However, these relationships remained nonsignificant in multivariate analyses.
Finally, alcohol use expectancies did not significantly differed between the two units, except for the SPP scale that was greater in the combat unit (p = 0.02).
|
Table 1: Variations in scores of alcohol use disorders identification test (AUDIT) according to alcohol modalities of consumption – Multiple linear regression. |
|
Modalities of consumption
|
Yes
|
No
|
Bivariate model p1
|
Multivariate model 1 p2
|
Multivariate model 2 p3
|
|
n
|
Mean AUDIT (SD)
|
n
|
Mean AUDIT (SD)
|
| With family |
75 |
6.6 (5.1) |
140 |
8.3 (5.8) |
0.03
|
0.02
|
0.2 |
| At family house |
137 |
7.5 (5.4) |
79 |
8.1 (6.0) |
0.4 |
0.3 |
0.2 |
| With friends |
155 |
8.1 (5.5) |
59 |
6.9 (5.8) |
0.2 |
0.4 |
0.9 |
| At restaurant |
89 |
8.5 (5.8) |
127 |
7.2 (5.5) |
0.09 |
0.2 |
0.4 |
| With colleagues |
91 |
9.5 (5.6) |
123 |
6.4 (5.3) |
<0.001
|
0.08 |
0.2 |
| At military unit |
41 |
11.5 (5.8) |
175 |
6.9 (5.2) |
<0.001
|
0.001
|
0.02
|
| Alone |
10 |
14.8 (7.2) |
205 |
7.4 (5.3) |
<0.001
|
<0.001
|
<0.001
|
| n = number; SD = standard deviation
Bold p-values correspond to significant relationships at 5%.
1 A bivariate model was estimated for each modality of consumption (outcome: AUDIT value).
2 The multivariate model 1 included the modalities of consumption as a whole (outcome: AUDIT value).
3 The multivariate model 2 included the modalities of consumption as a whole, and was controlled for gender, age, rank and unit (outcome: AUDIT value). |
|
Table 2: Description of the 8 scales of the Alcohol Effects Questionnaire (AEFQ) and their internal coherence measured by the Cronbach α coefficient. |
|
Scale
|
Number of variables
|
Number of subjects
|
Mean
|
SD
|
α coefficient
|
| Global Positive (POS) |
5 |
231 |
0.9 |
1.2 |
0.60 |
| Social and Physical Pleasure (SPP) |
5 |
236 |
3.5 |
1.4 |
0.67 |
| Sexual Enhancement (SEX) |
5 |
234 |
1.2 |
1.4 |
0.68 |
| Power and Aggression (AGG) |
6 |
235 |
2.3 |
1.9 |
0.75 |
| Social Expressiveness (SOC) |
5 |
232 |
2.8 |
1.9 |
0.84 |
| Relaxation and Tension Reduction (REL) |
5 |
230 |
2.0 |
1.5 |
0.63 |
| Cognitive and Physical Impairment (IMP) |
5 |
235 |
3.3 |
1.4 |
0.61 |
| Careless Unconcern (CU) |
4 |
237 |
1.9 |
1.4 |
0.66 |
| SD = standard deviation. |
|
Table 3: Relationships between alcohol expectancies (measured by the Alcohol Effects Questionnaire (AEFQ)) and drinking problems (measured by the alcohol use disorders identification test (AUDIT)) among soldiers – multinomial logistic regressions (n = 201). |
|
Alcohol misuse level
|
AEFQ scale
|
Bivariate OR1
(95% CI)
|
p-value
|
Multivariate OR2
(95% CI)
|
p-value
|
| Hazardous use3
|
Global Positive (POS) |
1.0 (0.7–1.4) |
0.9 |
0.8 (0.5–1.3) |
0.4 |
| |
Social and Physical Pleasure (SPP) |
1.5 (1.2–1.9)
|
0.002
|
1.7 (1.2–2.3)
|
0.002
|
| |
Sexual Enhancement (SEX) |
1.5 (1.2–1.9)
|
0.001
|
1.3 (1.0–1.8) |
0.07 |
| |
Power and Aggression (AGG) |
0.9 (0.7–1.0) |
0.09 |
0.9 (0.7–1.1) |
0.4 |
| |
Social Expressiveness (SOC) |
1.0 (0.8–1.2) |
0.9 |
0.8 (0.6–1.1) |
0.2 |
| |
Relaxation and Tension Reduction (REL) |
1.2 (0.9–1.4) |
0.2 |
1.1 (0.8–1.5) |
0.4 |
|
|
Cognitive and Physical Impairment (IMP) |
0.8 (0.6–1.0)
|
0.05
|
0.8 (0.6–1.0) |
0.07 |
| |
Careless Unconcern (CU) |
0.9 (0.7–1.1) |
0.3 |
1.0 (0.7–1.5) |
0.8 |
| Dependence4
|
Global Positive (POS) |
2.1 (1.5–2.9)
|
<0.001
|
1.9 (1.2–3.1)
|
0.007
|
| |
Social and Physical Pleasure (SPP) |
2.6 (1.8–3.9)
|
<0.001
|
2.5 (1.5–4.3)
|
0.001
|
| |
Sexual Enhancement (SEX) |
1.7 (1.3–2.2)
|
<0.001
|
1.1 (0.8–1.6) |
0.5 |
| |
Power and Aggression (AGG) |
1.1 (0.9–1.3) |
0.4 |
0.9 (0.7–1.2) |
0.6 |
| |
Social Expressiveness (SOC) |
1.7 (1.3–2.2)
|
<0.001
|
1.2 (0.8–1.7) |
0.4 |
| |
Relaxation and Tension Reduction (REL) |
1.5 (1.2–1.8)
|
0.002
|
0.9 (0.6–1.3) |
0.5 |
| |
Cognitive and Physical Impairment (IMP) |
0.8 (0.6–1.0)
|
0.04
|
0.7 (0.5–1.0)
|
0.05
|
| |
Careless Unconcern (CU) |
1.0 (0.8–1.3) |
0.8 |
1.0 (0.6–1.5) |
0.9 |
| OR = Odds ratio for an increase of 1 for each score. Bold OR correspond to a significant p-value at 5%.
95% CI = 95% confidence interval.
1 A bivariate model was estimated for each AEFQ scale (outcomes: hazardous use and dependence according the AUDIT).
2 The multivariate model included the AEFQ scales as a whole (outcomes: hazardous use and dependence according the AUDIT).
3 AUDIT ranging between 7 and 12 for men and between 6 and 12 for women (reference: absence of misuse defined by an AUDIT <7 for men and an AUDIT <6 for women).
4 AUDIT ≥13 (reference: absence of misuse defined by an AUDIT <7 for men and an AUDIT<6 for women). |
Discussion
The first main finding of the present study is the importance of harmful alcohol use, which was observed for 46.6% of soldiers in our sample (51.3% of alcohol users) according to the AUDIT. This high prevalence is in the same range as the data from previous studies among soldiers of several nations (43% binge drinkers in the United Kingdom in 2002, 59% in United States in 2005, and 56% recurrent drunkenness in France in 2006) [5, 7–8], even if the measure of AUD in the present study cannot be considered as equivalent to binge drinking. This phenomenon can be much higher in certain military populations: a study conducted in 2009 among 1,559 Royal Navy personnel showed that 92% scored as hazardous drinkers [20]. However, prevalence of harmful alcohol use among soldiers is close than those observed in 2010 in the French general population for the same age strata (39% of hazardous users and 14% at risk for dependence according to the AUDIT at age 18–25 years, and 37% and 9%, respectively, for age 26–35 years) [21]. Our results, according to which alcohol use rates are higher among young males from the rank and file, are also is in line with previous research in armed forces from several countries [4, 22].
The French validation study of the AEQ found positive relationships between alcohol daily use and four scales: POS, SPP, SOC and REL [19, 23]. In the present study, we found associations between three AEFQ scales (POS, SPP and REL) and dependence, which appears in line with the results previously observed with AEQ. The internal coherence of the AEFQ scales also appeared adequate in our sample, close to those observed in the French validation of AEQ [19].
Multivariate analyses of the AEFQ scale showed that hazardous alcohol use and dependence were positively associated with social and physical pleasure. The search for social expressiveness was also associated with dependence, but only in bivariate analysis. Even if the cross-sectional design of our study does not allow this hypothesis to be tested, these results could reflect a military social alcohol use, which is also in line with the significant association found between increased AUDIT scores and alcohol use occasions at the unit and with colleagues. Indeed, another study based on focus groups conducted among enlisted personnel from the US Navy and Marine Corps showed that the climate in which servicepersons live and work seems to be conducive to drinking [24]. The focus group discussions revealed attitudes and norms regarding alcohol abuse shared across the participating military units. Issues of social isolation and boredom appeared to have a causative relationship with alcohol use. This climate, juxtaposed within the context of a military installation facilitating ready access to cheap available alcohol, allowed alcohol use to be viewed as “entertainment” by some and “comfort” by others, reflecting the spectrum of identified reasons for drinking from social to coping. Moreover, this took place within an institutional context that is not clear on its stand regarding excessive alcohol use. Participants reported that base leaders do not apply alcohol policies equally to all individuals at their installation, creating the perception that punishment is random, particularly in light of the high number of individuals engaging in drinking.
The search for global positive effects was positively associated with dependence in multivariate analysis, and not with hazardous alcohol use. Dependence was also positively associated with relaxation and tension reduction in bivariate analysis. These relationships could constitute a marker of an alcohol use to cope with stress at work. Although we were not able to verify this hypothesis owing to the design of the present study, we observed that shorter time since the last deployment was associated with a greater risk of dependence. It is known that military status implies permanent vigilance in many activities, some repetitive tasks and a quest of excellence that can induce a great deal of mental workload. In these contexts, alcohol use enables a coping strategy towards underlying depressive moods and an increase in group bonding [25]. Coping skills have been hypothesised to be a contributor to drinking behaviour, as reliance on drinking as a coping strategy may be associated with avoidant coping [26]. In students, avoidant coping was related to alcohol use through the mediation of positive expectancies [27]. Finally, particularly among military personnel, the potential role of post traumatic psychiatric disorders on subsequent alcohol dependence cannot be ignored. There is a consistent body of evidence for the association between post-deployment increased and/or heavy use of alcohol and combat exposure, leading to post-traumatic stress disorder (PTSD) and depression [28–29]. However, the relationships between PTSD and AUD appear to be complex. A study conducted among veteran women suggested that PTSD alone was not directly associated with an increase in AUDIT score; this relationship seeming to be mediated by both positive evaluations of the effects of alcohol and avoidant coping strategies [30].
It is also interesting to mention that the sexual enhancement scale was associated with both risky use and dependence, but only in bivariate analyses. This finding has to be placed in the perspective of the role of alcohol in hazardous sexual exposures, which constitute a public health problem among military personnel, particularly in operations [31]. Between 2007 and 2009, alcohol was suspected in 5% of condom misuse or nonuse cases in the French armed forces (French military centre for epidemiology and public health; unpublished data).
Finally, a negative expectancy, the fear of cognitive and physical impairment, remained as a protector against both hazardous use and dependence in bivariate analysis, the relationship with dependence persisting after adjustment on the other scales of the AEFQ. This finding probably reflects certain awareness of military personnel of the risk of impairment of their operational imperatives and their short-term safety. This is not surprising, considering that most of the military have activities requiring optimal vigilance, such as use of weapons, night work or vehicle driving [9–11]. This awareness should be more improved by reinforcing health education programmes on alcohol harms in this population.
According to the data from the French military social observatory, our sample includes more rank and file (70% vs 52% in the Army as a whole) and fewer female personnel (8% vs15%). Thus, if considering the known socio-demographic patterns of alcohol use, our results may overestimate the prevalence of AUD and have to be interpreted with caution. However, we could expect that this overestimation may be partially compensated by an underestimation induced by the 9.2% of subjects who did not complete the AUDIT (if we hypothesise that these subjects are more likely to conceal AUD). Thus, the results of another survey conducted in the French Army in 2006 show prevalences close to those observed here [8]. Another limitation is that the present study developed a measure that was tested on the same sample. Indeed, we explored the psychometrics of AEFQ in one sample using the AUDIT as a test of validity, but this measure has to be further tested on another sample.
Conclusions
The present study, in line with previous research in terms of importance of AUD among military personnel, also found that alcohol use expectancies are associated with alcohol misuse among soldiers. Some previous studies suggest that soldiers may not only use alcohol as an individual strategy to cope with underlying depressive disorders, but also as a collective strategy to increase group bonding in order to cope with the difficulties of a military profession. However, further investigation is needed in our population in order to verify these hypotheses, particularly measurement of depressive disorders and PTSD.
Key points
– The alcohol effect questionnaire appears to be accurate among military personnel.
– Alcohol use expectancies are significant predictors of alcohol use disorders among soldiers.
– These relationships may involve two mechanisms: individual coping strategy and group bonding collective strategy.
Acknowledgements: Authors would like to thank all the personnel of participating units and Dr. Karen Carvalho De Castro for their help.
References
1 Bray RM, Marsden ME, Guess LL, Herbold JR. Prevalence, trends, and correlates of alcohol use, nonmedical drug use, and tobacco use among U.S. military personnel. Mil Med. 1989;154(1):1–11.
2 Bray RM, Hourani LL. Substance use trends among active duty military personnel: findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction. 2007;102(7):1092–101.
3 Mayet A, Marimoutou C, Haus-Cheymol R, Verret C, Ollivier L, Berger F, et al. Etat des lieux des conduites addictives dans les armées françaises: une méta-analyse des enquêtes de prévalence conduites entre 2005 et 2009. Médecine et armées 2014. In press. French.
4 Verrall NG. A review of military research into alcohol consumption. In: NATO science and technology organization. Psychological Aspects of Deployment and Health Behaviours. 2011. Available at http://www.cso.nato.int/abstracts.aspx (accessed on February 12, 2014).
5 Hooper R, Rona RJ, Jones M, Fear NT, Hull L, Wessely S. Cigarette and alcohol use in the UK armed forces, and their association with combat exposures: A prospective study. Addict Behav. 2008;33:1067–71.
6 Foster EM. Deployment and the citizen soldier: need and resilience. Med Care. 2011;49:301–12.
7 Stahre MA, Brewer RD, Fonseca VP, Naimi TS. Binge drinking among U.S. active-duty military personnel. Am J Prev Med. 2009;36:209–17.
8 Marimoutou C, Queyriaux B, Michel R, Verret C, Haus-Cheymol R, Mayet A, et al. Survey of alcohol, tobacco and cannabis use in the French army. J Addict Dis. 2010;29:98–106.
9 Bell NS, Amoroso PJ, Yore MM, Smith GS, Jones BH. Self-reported risk-taking behaviors and hospitalization for motor-vehicle injury among active duty Army personnel. Am J Prev Med. 2000;18(3S):85–95.
10 Helmkamp J, Kennedy R. National mortality profile of active duty personnel in the U.S. Armed Forces: 1980–1993. Atlanta GA: CDC, 1996.
11 Stout RW, Parkinson MD, Wolfe WH. Alcohol-related mortality in the U.S. Air Force, 1990. Am J Prev Med. 1993;9:220–3
12 Zadoo V, Fengler S. The effects of alcohol and tobacco use on troop readiness. Mil Med. 1993;158:480–4.
13 Jones E, Fear NT. Alcohol use and misuse within the military: A review. Int Rev Psychiatry. 2011;23:166–72.
14 Prévot E. Alcool et sociabilité militaire: de la cohésion au contrôle, de l’intégration à l’exclusion. Travailler. 2007;2(18):159–81. French.
15 Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption? Addiction. 1993;88(6):791–804.
16 Gache P, Michaud P, Landry U, Accietto C, Arfaoui S, Wenger O, et al. The Alcohol Use Disorders Identification Test (AUDIT) as a screening tool for excessive drinking in primary care: reliability and validity of a French version. Alcohol Clin Exp Res. 2005;29(11):2001–7.
17 Rohsenow DJ. Drinking habits and expectancies about alcohol's effects for self versus others. J Consult Clin Psychol. 1983;51(5):752–6.
18 Brown SA, Christiansen BA, Goldman MS. The Alcohol Expectancy Questionnaire: an instrument for the assessment of adolescent and adult alcohol expectancies. J Stud Alcohol. 1987;48(5):483–91.
19 Carvalho de Castro K, Rascle N, Romo L, et al. Les attentes positives envers l’alcool. Adaptation française de la version adulte du “Alcohol Expectancy Questionnaire”. Journal de Thérapie Comportementale et cognitive 2007;17(1):33–7. French.
20 Henderson A, Langston V, Greenberg N. Alcohol misuse in the Royal Navy. Occupational Medicine 2009;59:25–31.
21 Beck F, Guignard R, Richard J-B, Tovar M-L, Spilka S. Les niveaux d’usage des drogues en France en 2010: exploitation des données du Baromètre santé 2010 relatives aux pratiques d’usages de substances psychoactives en population adulte. Tendances 2011;76. Available at http://www.ofdt.fr/ofdtdev/live/publi/tend/tend76.html (accessed on October 14, 2014). French.
22 Fear NT, Iversen A, Meltzer H, Workman L, Hull L, Greenberg N, et al. Patterns of drinking in the UK Armed Forces. Addiction. 2007;102:1749–59.
23 Carvalho de Castro K, Swendsen J, Husky MM. Les rôles des attentes par rapport aux effets de l’alcool et des antécédents familiaux d’alcoolisme sur la consommation quotidienne. Journal de Thérapie comportementale et cognitive 2010;20:118–24. French.
24 Poehlman JA, Schwerin MJ, Pemberton MR,Isenberg K, Lane ME , Aspinwall K. Socio-Cultural Factors That Foster Use and Abuse of Alcohol Among a Sample of Enlisted Personnel at Four Navy and Marine Corps Installations. Mil Med. 2011;176:397–401.
25 Zins M, Carle F, Bugel I, Leclerc A, Di Orio F, Goldberg M. Predictors of change in alcohol consumption among Frechmen of the Gazel study cohort. Addiction. 1999;94:385–95.
26 Moos RH, Brennan PL, Fondacaro MR, Moos BS. Approach and avoidance coping responses among older problem and nonproblem drinkers. Psychol Aging. 1990;5(1):31–40.
27 Hasking P, Lyvers M, Carlopio C. The relationship between coping strategies, alcohol expectancies, drinking motives and drinking behaviour. Add Behav. 2011;36(5):479–87.
28 Savarese VW, Suvak MK King LA, King DW. Relationship among alcohol use, hyperarousal, and marital abuse and violence in Vietnam veterans. J Traum Stress. 2001;14:717–32.
29 Shipherd JC, Stafford J Tanner LR. Predicting alcohol and drug abuse in Persian Gulf war veterans: what role do PTSD symptoms play? Add Behav. 2005;30:595–9.
30 Creech SK, Borsari B. Alcohol use, military sexual trauma, expectancies, and coping skills in women veterans presenting to primary care. Add Behav. 2014;39:379–85.
31 Anastario MP, Tavarez MI, Chun H. Sexual risk behavior among military personnel stationed at border-crossing zones in the Dominican Republic. Rev Panam Salud Publica. 2010;28(5):361–7.