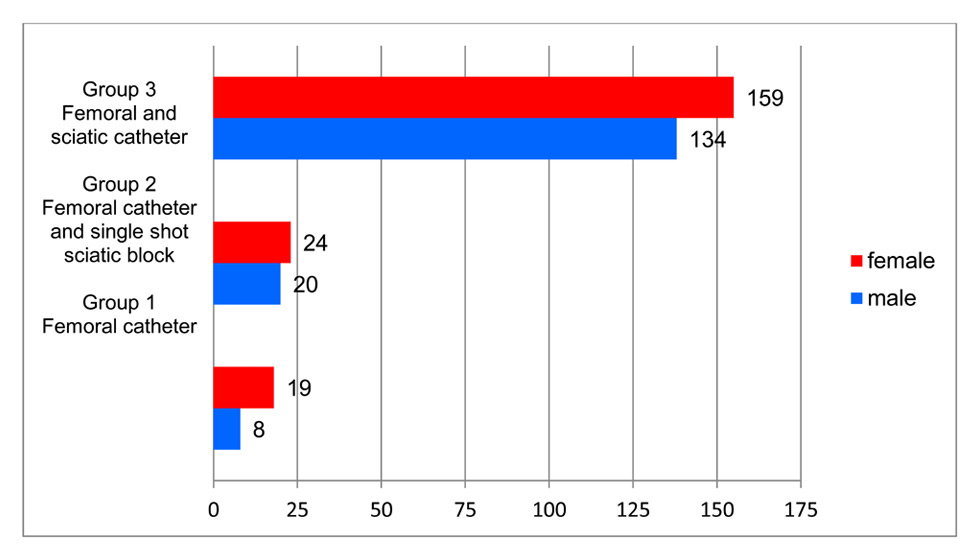
Figure 1
Group distribution.
DOI: https://doi.org/10.4414/smw.2015.14119
Total or hemi-knee arthoplasty (TKA) is an operation that is increasing in number. There are several reasons for this. One is an ageing community with high expectations of mobility and activity. Postoperative pain is a serious problem with TKA, which is one of the procedures with the highest levels of postoperative pain [1]. Sufficient postoperative analgesia with early mobilisation of the patient is important for the postoperative outcome [2, 3], so cooperation of the surgeon and anaesthesiologist is paramount. The aim of this study was to investigate the efficiency of combined continuous sciatic nerve analgesia with femoral nerve analgesia, as this has been be discussed in the recent literature.
Pain is almost always documented on an individual patient basis as there are few other ways to achieve a clear picture of postoperative pain. Postoperative documentation of medication consumption has proven to be unreliable as this is dependent on other factors (metabolic) as well. A visual analogue scale (VAS) defining pain from 1 (none) to 10 (unbearable) is a reliable method for measuring the scale of pain and, therefore, most often used in studies reported in the literature. Its limitations (intraindividual variability) are well known but it remains the preferred method for pain documentation.
Regional anaesthesia after knee surgery may be applied in different forms [4]: since the relevant nerves all come from the lumbar and sacral plexus, analgesia of the femoral nerve as it branches off from the lumbar plexus has developed into a standard procedure for postoperative analgesia in knee surgery.
Peripheral nerve stimulation and/or ultrasound-aided techniques are possible with the patient resting in a lateral or supine position. Single-shot or catheter techniques may be applied. The supine position has the advantage of easier access for postoperative care of the catheter and continuous or single-shot application of the relevant medication. A reliable anaesthesia of the sciatic nerve distal to the catheter is usually accomplished. Another advantage of the supine position is block of the cutaneus femoris posterior nerve, which may reduce postoperative pain after application of a tourniquet [4]. Ultrasound-guided application of the local anaesthetic seems to give better results for intra- and postoperative pain therapy [5].
A total of 362 patients with a hemi- or total knee replacement from July 2005 to December 2012 were included in this retrospective study. All operations were performed by the same surgeon using the same technique. The nerve blocks were applied with ultrasound guidance. Anonymised documentation in a standard form was evaluated. In addition, all patient documentation on the relevant charts was investigated and analysed. Our standard protocol included the indication for pain therapy, the side of the catheter, the number of the pain pump, the form and position of catheter, and the name, amount and duration of any medication given. The VAS score was documented after 8 and 24 hours. Usually, the patient was mobilised for the first time after 24 hours
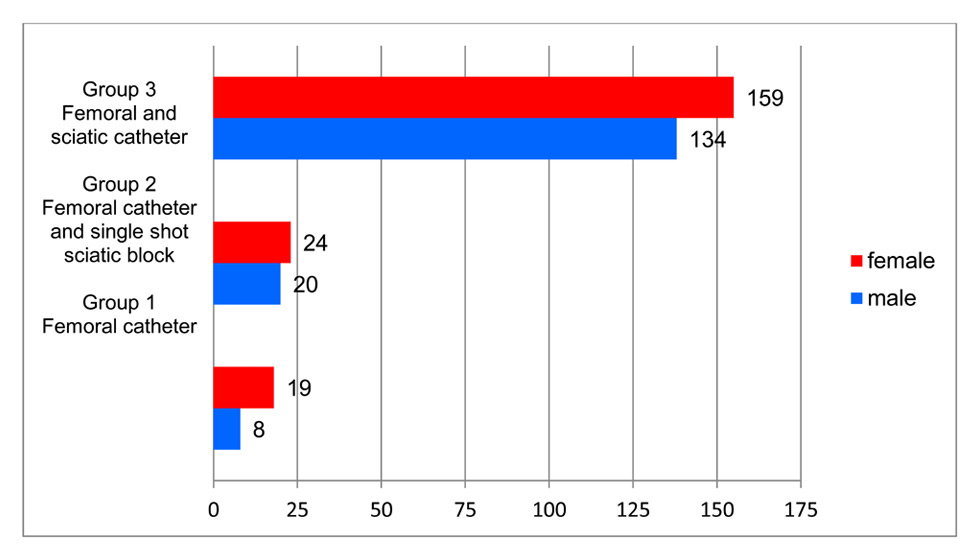
Figure 1
Group distribution.
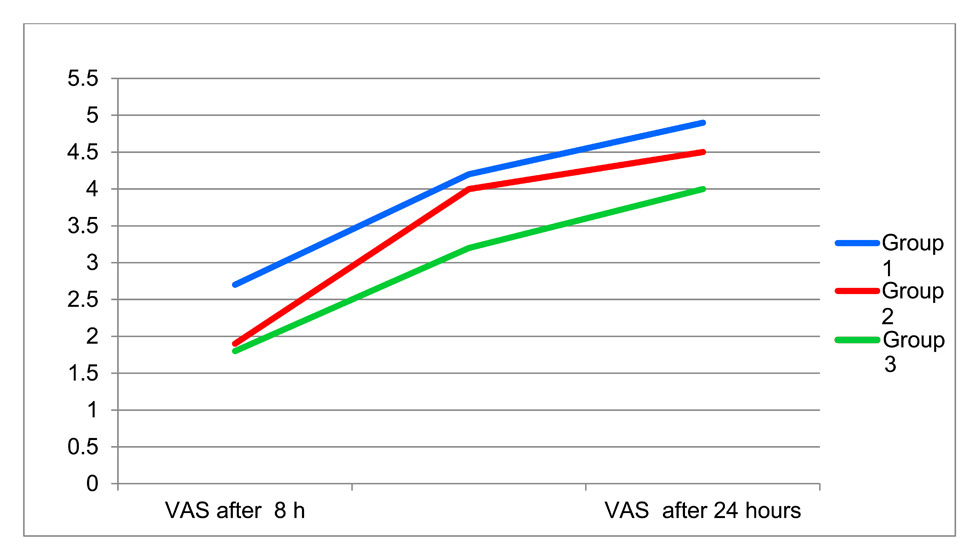
Figure 2
Development of VAS score over time with different catheter techniques.
Age, sex, location of catheter, VAS, opioids, nonsteroidal antirheumatics (NSARs) and possible side effects were documented. The knee operations were performed by a single surgeon using the same implant; the post-operative pain evaluation was performed by the hospital’s pain team, which is part of our department of anaesthesiology. VAS scores were measured using a standard VAS scale. The following groups were defined:
Group 1: July to December 2005; block of the femoral nerve only.
Group 2: January to June 2006; anterior placement of a sciatic nerve catheter. Patients operated on at a later date where placement of a continuous pain catheter was impossible were also included into this group.
Group 3: July 2006 to December 2012; placement of femoral nerve and anterior sciatic nerve catheter with continuous analgesia for 24 hours.
The primary blocks of the femoral and sciatic nerves were performed under sterile conditions with a weight-adapted dose of mepivacaine, while monitoring the application with a nerve stimulation technique (Stimuplex HNS, B Braun, Germany). Catheters were supplied by Pajunk Company (Uniplex, Plexolong).
For all groups, 2 hours after primary analgesia a CADD-Legacy pump (Smiths medical Company) was connected to the catheter. A continuous infusion with ropivacaine 0.3% was applied; after emptying of the reservoir, a ropivacaine 0.2% infusion was applied. The pump worked at a continuous rate of 5–12 ml/h with a locking interval of 20 min. A bolus of 4–6 ml ropivacaine was defined. The first bolus of 20 ml ropivacaine 0.2% and 75 µg clonidine was applied after termination of the operation in the postoperative care unit. According to the development of postoperative pain, the bolus was repeated after a minimum of 4 hours and a maximum of 8 hours.
Postoperative medication was as follows. Paracetamol and mefenamic acid (NSAR) were routinely administered, and in patients above 65 a proton pump inhibitor was applied to prevent gastrointestinal side effects. If this medication was ineffective, opioids were applied: pethidine was our opioid of first choice, followed by morphine or fentanyl. The total amount of opioids administered during the first 24 hours was monitored and documented. Typical side effects as nausea, vomiting, itching and urinary retention were documented. The total opioid equivalent was converted to pethidine and not morphine because pethidine was our opioid of choice.
The mean and standard deviation of the VAS values in the study groups were determined and compared between the different methods of pain catheter. A possible significant difference between the groups was determined by applying the t-test.
Age, sex and the mean opioid consumption were determined in each patient group. The number of patients with side effects of the opioids was assessed.
From January 2005 to December 2012, a total of 464 patients underwent total knee arthroplasty (TKA); 364 patient files could be assessed. The operations performed were either total or unicondylar knee replacements. There were a total of 202 (56%) female patients, and a total of 162 (44%) male patients. Mean age was 67.7 years, with male patients being slightly younger than females. The results analysed pertain to patients, not knee operations.
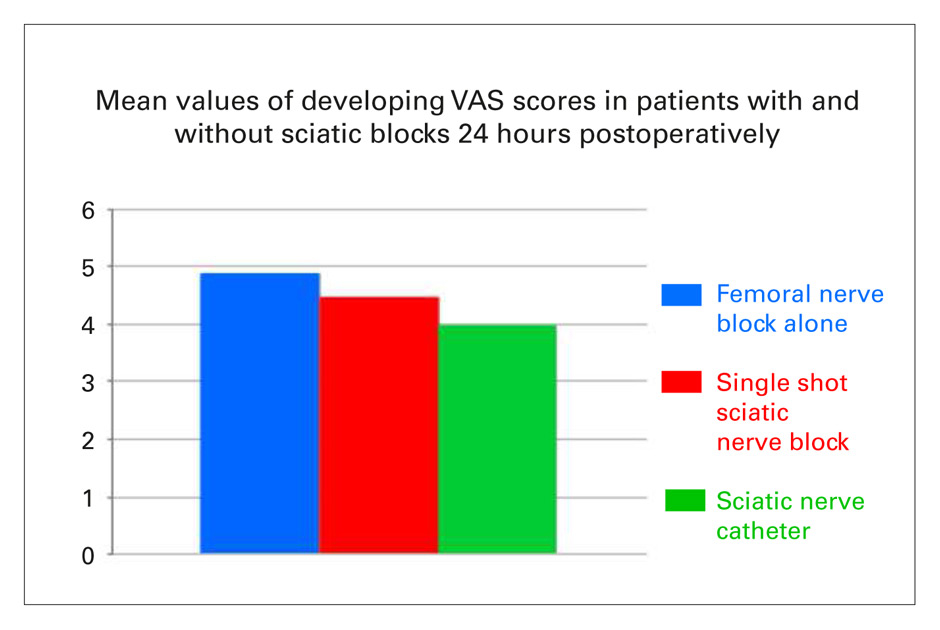
Figure 3
Mean values of developing VAS scores in patients with and without a sciatic blocks at 8 hours (a, above) and 24 hours (b, below) postoperatively.
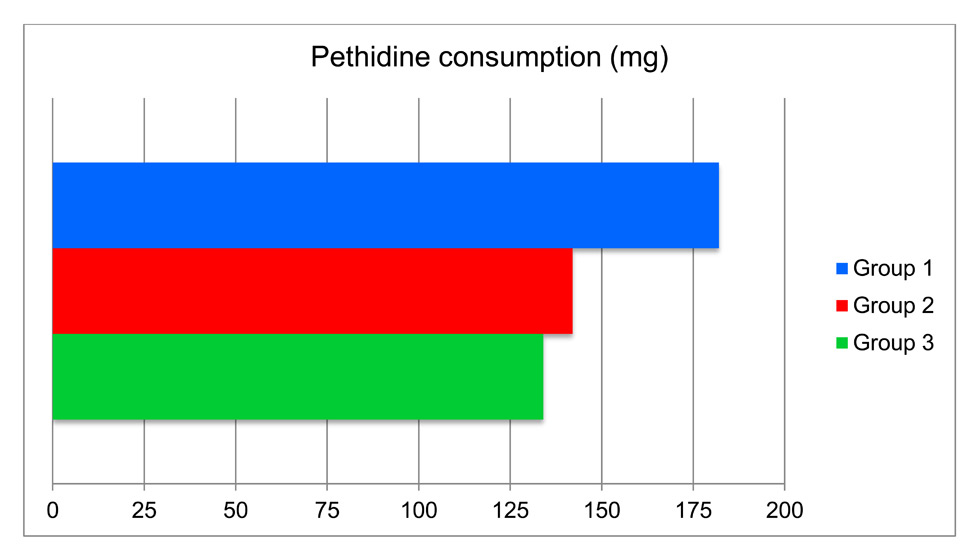
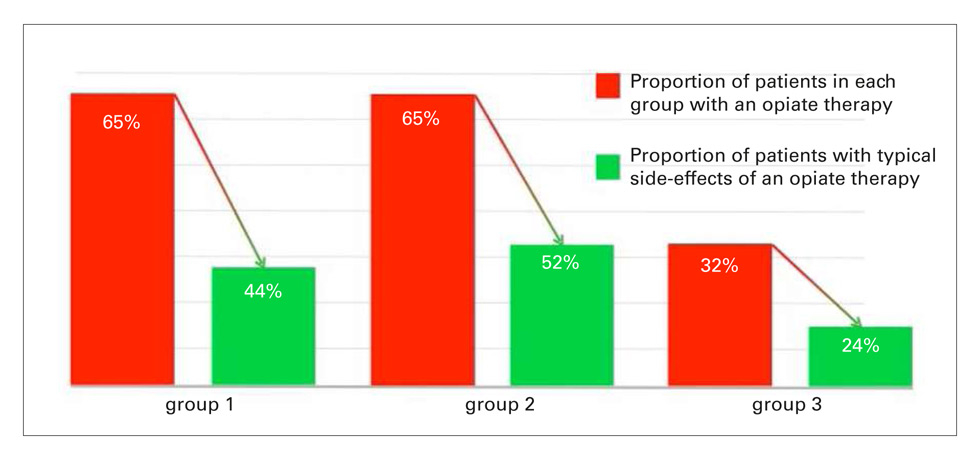
Figure 4
Group differences in pethidine consumption (a) and drop in side effects of opioids per group (b).
Group 1 (femoral catheter only) consisted of a total of 27 patients (19 females, 8 males).
Group 2 (femoral catheter and single shot in the sciatic nerve) comprised of 44 patients (24 females, 20 males).
Group 3 (femoral and sciatic nerve catheters) was the largest group (293 patients, 159 females and 134 males).
The VAS score was analysed after 8 and 24 hours for each group at a single timepoint.
Comparing the three groups, the average VAS scores 8 hours and 24 hours after the operation were lowest in group 3 (mean values 1.8 and 4.0, respectively). The VAS scores after continuous blocking of the femoral nerve and single-shot sciatic nerve analgesia were also lower (mean values 1.9 and 4.5) than those after block of the femoral nerve alone (mean values 2.7 and 4.9).
The VAS scores after 8 and 24 hours (mean values 1.8 and 4.0) were lower after continuous block of the sciatic nerve as compared with single-shot anaesthesia (mean values 1.9 and 4.5).
The postoperative opioid consumption in mg was calculated from prescriptions to the individual patients after 24 hours. It was lowest (mean value 134 mg) in group 3, with mean values of 142 mg in group 2 and 182 mg in group1. Only 94 of the patients (32%) in group 3 needed opioids as compared with 27 patients (65%) in group 1 and 44 patients (65%) in group 2.
These typical side effects of opioids were recorded 24 hours after the operation and the medication with pethidine: pruritus, nausea, vomiting and urinary obstruction. Seven of the 17 patients (44%) in group 1, 15/28 (52%) patients in group 2 and 23/94 (24%) patients in group 3 had typical side effects (fig. 4b).
Paracetamol and nonsteroidal antirheumatics (NSARs) were applied routinely in combination with opioids. We could not observe any significant group differences in the consumption of these medications.
| Table 1:Opioid consumption and side effects from opioid. | |||
| Group | Mean pethidine consumption | Patients with opioid therapy | Patients with typical side effects |
| Group 1 (n = 26) | 182 mg | 65% | 44% |
| Group 2 (n = 43) | 142 mg | 65% | 52% |
| Group 3 (n = 293) | 134 mg | 32% | 24% |
It should be clearly stated that in our study the group sizes are different, therefore comparison of the results between these groups is difficult and does not give statistically significant results. Since the group sizes are different, it was impossible to make a group matching or variable adjustment. The groups included hemi- and total knee prostheses, which may also present factors impacting postoperative pain occurrence. This was also a retrospective study with all its possible biases, and our results were based on the VAS, which in its nature is a subjective assessment. However, many studies were designed similarly to ours. We think our results nevertheless seem to point towards an advantage of a continuous sciatic nerve block combined with a continuous femoral nerve block. This is still discussed controversially in the literature as will be seen below. Patient questionnaires are standard procedures in evaluating the effects of regional anaesthesia. As there are few ways to determine the subjective perception of pain, the visual analogue scale (VAS) is well established. This study used a standard postoperative questionnaire [6].
TKA is one of the more frequent operations in orthopaedic surgery, often requiring adequate postoperative analgesia. Our retrospective study shows that continuous block of the femoral nerve alone is not sufficient to alleviate postoperative pain. Blocking the femoral nerve alone yielded the highest VAS scores in our study. Insufficient postoperative pain control may result in worse results after TKA [1].
The positive role of anaesthesia of the sciatic nerve in addition to femoral nerve block alone was described by Pham Dang et al. [7]. Morin et al. [8] reached similar conclusions and recommended the sciatic nerve block in addition to a psoas compartment block and femoral nerve anaesthesia. Both Pham Dang and Morin stressed the value of a continuous sciatic nerve block. Morin et al. [8] gave additional value to the psoas compartment block. Our study results compare well with these positive findings. In addition, we may conclude that a single-shot sciatic nerve block is not as effective as a continuous sciatic nerve block.
The Australia-New Zealand College of Anesthesiology guidelines [9] for treatment of acute postoperative pain, however, do not include the application of a double catheter procedure. They recommend continuous femoral nerve block and psoas compartment block. The femoral block is seen to be superior to intravenous opioid therapy alone. Capdevilla et al. [10, 11] described lower pain scores after a femoral block as compared with intravenous pain therapy. Naturally, the side effects of opioids were also fewer in patients with a femoral block. Singelyn et al. [12] described significantly better analgesia in patients with a femoral block than in patients having a patient-controlled analgesia (PCA) pump supplied with opioids.
The role of the femoral nerve block in postoperative analgesia is mostly undisputed, although there is some dispute over the role of the femoral nerve block, especially in the era of early mobilisation [4]. However, there is no consensus in the literature concerning additional single-shot or continuous sciatic nerve blocks. Our study analysed the femoral block in comparison with the two-catheter technique either as a single shot or continuous sciatic nerve block.
Retrospectively, we found that patients having femoral nerve blocks alone needed a higher dose of opioids than patients in whom a double catheter technique was applied (fig. 4a). Consequently, these patients with a higher opioid consumption also suffer from higher rates of typical side effects such as nausea, vomiting and constipation (fig. 4b). Keita et al. [13] found a lower consumption of opioids in patients with a continuous sciatic nerve block as compared with patients with a single-shot block. Our results confirm these findings (fig. 4a). Wegener et al. [14] found no differences in groups with single-shot or continuous sciatic nerve blocks. Their study found that a single-injection sciatic nerve block reduced the pain on the day of surgery, whereas the continuous sciatic nerve blocks reduced postoperative pain after mobilisation. Our study leads to different conclusions: the single-shot sciatic nerve block does not contribute much to postoperative pain control. These results are supported by the postoperative VAS measurements and opioid consumption. Ben-David et al. [15] found that continuous femoral analgesia alone is inferior to an added continuous sciatic nerve block, which compares well with our results. Cappelleri et al. [16] concluded in their study that continuous sciatic nerve blockade reduces opioid consumption and improves early rehabilitation as compared with single-shot blocks. Frassanito et al. [17], however, found that either continuous or single-shot block of the sciatic nerve yield the same postoperative opioid consumption and pain scores. A similar view was shared by Paul et al. [18]. Their meta-analysis did not find significant differences between a femoral nerve block and additional sciatic nerve anaesthesia, either intermittent or continuous. Hunt et al. [21] found good results after single-shot sciatic and femoral nerve blocks. Abdallah et al. [19] in their review found that continuous sciatic nerve blocking is not advantageous after 24 hours. Hunt et al. [20] described a significantly lower level of pain after single-shot sciatic and femoral nerve blocks following general anaesthesia.
Despite a controversial discussion in the literature, femoral nerve block alone seems to be insufficient for postoperative pain control after TKR. Our results, which pertain to late mobilisation only, demonstrate that continuous sciatic nerve blockade in addition to a femoral nerve block reduce opioid consumption postoperatively and significantly reduce the VAS. We changed our postoperative regimen according to these results. We strongly advocate cooperation between the surgeon and the anaesthesiologist for postoperative pain management.
1 Albert, TJ, Cohn JC, Rothman JS, Springstead J, Rothman RH, Booth RL Jr. Patient-controlled analgesia in a postoperative total joint arthroplasty population. J Arthroplasty. 1991;6(Suppl):23–28.
2 Enneking FK, Chan V, Greger J, Hadzic A, Lang SA, Horlocker TT. Lower-extremity peripheral nerve blockade: essentials of our current understanding. Reg Anesth Pain Med. 2005;30:4–35.
3 Paysant J, Jardin C, Biau D, Coudeyre E, revel M, Rannou F. What is in the interest of early knee mobilization after total knee arthroplasty? Ann Readapt Med Phys. 2008;51(2):138–43.
4 Gligorijevic S. Lower extremity blocks for day surgery. Techniques. Reg Anesth Pain Med. 2000;4:30–7.
5 Shantanna H, Huilgol M, Manivackam VK, Maniar A. Comparative study of ultrasound-guided continuous femoral nerve blockade with continuous epidural analgesia for pain relief following total knee replacement. Indian J Anaesth. 2012;56(3):270–5.
6 Ironfield CM, Barrington MJ, Kluger R, M Biostat, Sites B. Are Patients Satisfied After Peripheral Nerve Blockade? Results from an International Registry of Regional Anesthesia. Reg Anesth Pain Med. 2014;39:48–55.
7 Pham-Dang C, Gautheron E, Guilley J, et al. The value of adding sciatic nerve block to continuous femoral block for analgesia after total knee replacement. Reg Anesth Pain Med. 2005;30:128–33.
8 Morin AM, Kratz CD, Eberhart LH, Dinges G, Heider E, Schwarz N, Eisenhardt G, Geldner G, Wulf H. Postoperative analgesia and functional recovery after total-knee replacement: comparison of a continuous posterior lumbar plexus (psoas compartment) block, a continuous femoral nerve block, and the combination of a continuous femoral and sciatic nerve block. Reg Anesth Pain Med. 2005;30:434–45.
9 Macintyre PE, Schug SA, Scott DA, Visser EJ, Walker SM; APM:SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Acute Pain Management: Scientific Evidence.3rd edition. Melbourne: ANZCA & FPM; 2010. http://www.anzca.edu.au/resources/college-publications/pdfs/Acute%20Pain%20Management
10 Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d’Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999;1:8–15.
11 Capdevila X, Biboulet P, Morau D, Bernard N, Deschodt J, Lopez S, d’Athis F. Continuous psoas compartment block for postoperative analgesia after total hip arthroplasty: new landmarks, technical guidelines and clinical evaluation. Anesth Analg. 2002;94:1606–13.
12 Singelyn FJ, Gouverneur JM. Postoperative analgesia after total hip arthroplasty: i.v. PCA with morphine, patient-controlled epidural analgesia, or continuous “3–in-1” block?: a prospective evaluation by our acute pain service in more than 1,300 patients. J Clin Anesth. 1999;7:550–55.
13 Keita S, Takehiko A, Naoto S, Noriko N. Continuous versus Single-Injection Sciatic Nerve Block Added To Continuous Femoral Nerve Block for Analgesia After Total Knee Arthroplasty. Reg Anesth Pain Med. 2014;39,3:225–9.
14 Wegener JT, van Ooij B, van Dijk CN, Hollmann MW, Preckel B, Stevens MF. Value of single-injection or continuous sciatic nerve block in addition to continuous femoral nerve block in patient undergoing total knee arthroplasty. Reg Anesth Pain Med. 2011;36:481–8.
15 Ben-David B, Schmalenberger K, Chelly JE. Analgesia after total knee arthroplasty. Is continuous sciatic blockade needed in addition to continuous femoral blockade? Anesth Analg. 2004;98:747–9.
16 Cappelleri G, Ghisi D, Fanelli A, Albertin A, Somalvico F, Aldegheri G. Does Continuous Sciatic Nerve Block Improve Postoperative Analgesia and Early Rehabilitation After Total Knee Arthroplasty? Reg Anesth Pain Med. 2011;36:489–92.
17 Frassanito L, Vergari A, Messina A, Piotini S, Puglisi C, Chierichini A. Anaesthesia for Total Knee Arthroplasty: Efficacy Of Single-Injection or Continuous Lumbar Plexus Associated with Sciatic Nerve Blocks- A randomized Controlled Study. Eur Rev Med Pharmacol Sci. 2009;13(5):375–82.
18 Paul JE, Arya A, Hurlburt L, Cheng J, Thabane L, Tidy A, Murthy Y. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a meta-analysis of randomized controlled trials. Anesthesiology. 2010;113:1144–62.
19 Abdallah FW, Brull R. Is sciatic nerve block advantageous when combined with femoral nerve block for postoperative analgesia following total knee arthroplasty? Reg Anesth Pain Med. 2011;36:493–98.
20 Hunt KJ, Bourne MH, Mariani EM. Single-injection femoral and sciatic nerve blocks for pain control after total knee arthroplasty. J Arthroplasty. 2009;24:533–53.
Disclosures: No financial support and no other potential conflict of interest relevant to this article was reported.