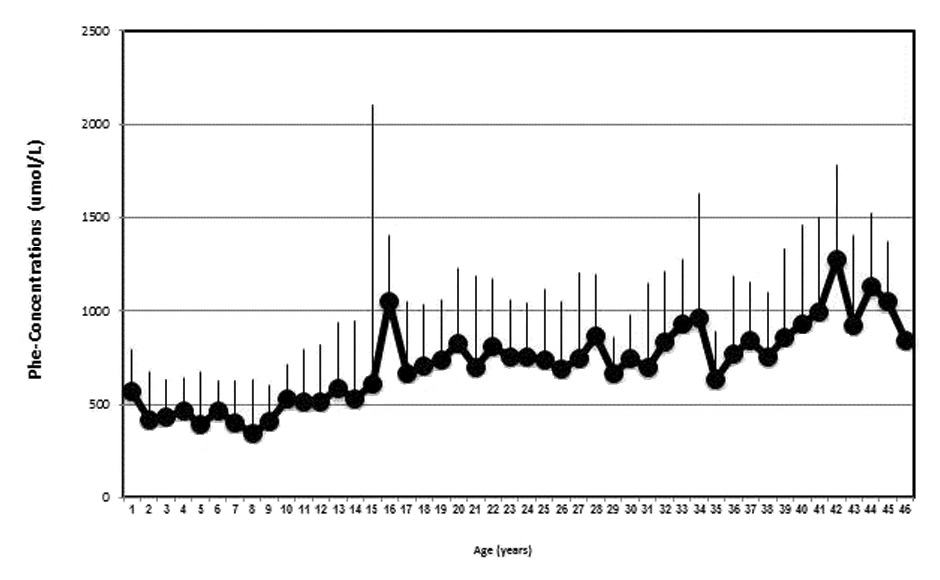
Figure 1
Age dependent Phenylalanine concentrations (mean ± SD). With advancing age, mean Phe-concentrations of the whole cohort increase.
DOI: https://doi.org/10.4414/smw.2014.14074
Phenylketonuria (PKU) is an autosomal-recessive inherited metabolic disease, due to partial or complete phenylalanine hydroxylase deficiency (PAH), the enzyme responsible for the conversion of phenylalanine to tyrosine [1]. Its incidence is 1:8000 births in Switzerland, PKU and hyperphenylalaninaemia included [2]. PAH deficiency leads to neurotoxic phenylalanine (Phe) accumulation, causing irreversible damage to the developing central nervous system (CNS) [3]. Nowadays, owing to newborn screening, the disease can be diagnosed within a few days after birth and therapy can be initiated.
At birth, the children are completely healthy. However, if nutritional therapy is not implemented as soon as possible, severe mental retardation may ensue [4]. In addition, eczema and the typical “musty and mousy” smell of skin, hair, sweat and urine can result [3]. Amongst these symptoms particularly the impaired CNS function and the associated difficulties of the school career have a high impact on the integration into the professional life of these patients.
Long-term outcome data – including childhood and adulthood – in patients with PKU in relation to metabolic control are scarce. They have mainly focused on neuropsychological parameters such as Intelligence quotient (IQ) or executive functions [5]. There is data indicating that adequate control of blood phenylalanine levels is effective in preventing most of the CNS deficits [6]. However, even in treated patients with PKU subtle disabilities remain including lower average IQ [5, 7] and impaired executive function of CNS [8]. Importantly, the degree of impairment appears to be correlated with life time exposure to Phe concentrations, in particular the exposure during early childhood [9]. Low IQ and impaired executive CNS function impact on school career and integration into professional life.
Accordingly, we aimed to investigate the long-term follow-up of patients with PKU in relation to Phe exposure during childhood and adulthood. We hypothesised that the time point of diagnosis and the Phe exposure during follow-up has a significant impact on the integration into the professional life.
In this retrospective analysis all adult patients with PKU currently treated at the adult Divison of Endocrinology, Diabetology and Clinical Nutrition of the Inselspital, Bern, Switzerland were included. During childhood, they were treated by the paediatric metabolic team, which collaborates with the adult metabolic team where the patients are transferred, usually at the age of 16–18 years. Importantly, only patients that needed a dietary intervention during the follow-up were included. The data recorded were the time point of the diagnosis (by neonatal screening vs. diagnosis in childhood), all phenylalanine-concentrations measured during the follow-up (expressed as mean phenylalanine level/year and patient), the professional career, the additional specialised schooling support and potential difficult psychosocial context.
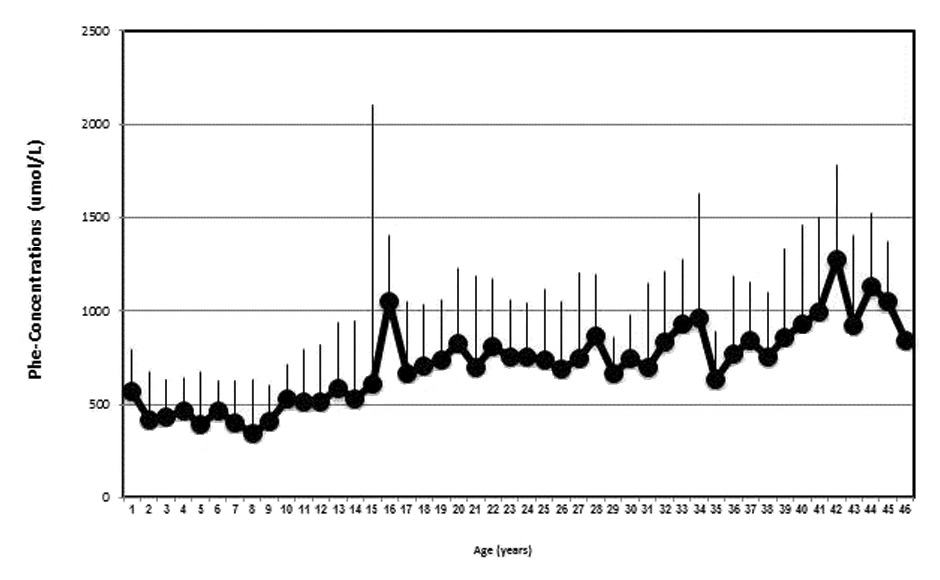
Figure 1
Age dependent Phenylalanine concentrations (mean ± SD). With advancing age, mean Phe-concentrations of the whole cohort increase.
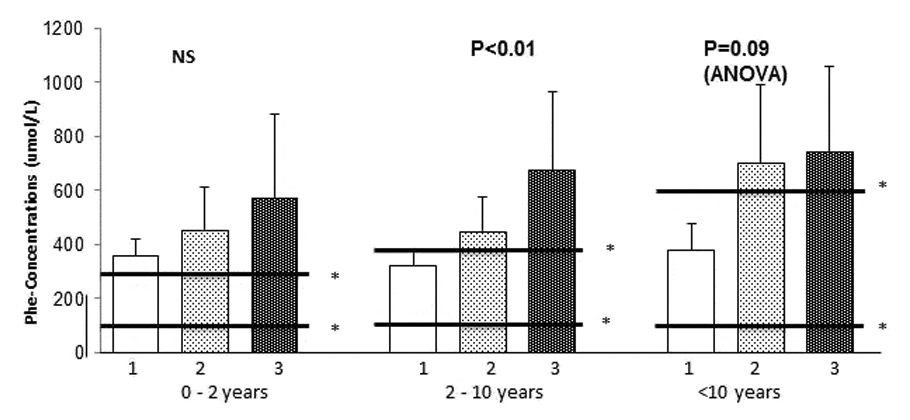
Figure 2
Professional integration in relation to Phenylalanine concentrations during the whole follow-up period.
In all three age groups, the patients of the non-professional study-group have the highest and the patients of the high school diploma-group the lowest mean Phenylalanine concentrations. The accomplished apprenticeship-group present with Phe concentrations in-between. Statistical significant differences were detected in the age-group of 2–10 years.
There was a tendency for higher values with advancing age, in particular in the apprenticeship group.
1 = high school diploma or university; 2 = accomplished apprenticeship at least 3 years; 3 = no professional studies/disability annuity.
* Target range in the respective age group according to the recommendation of the Swiss Metabolic Group [10]
The primary outcome was documented as patients with a high school or university diploma (high school diploma), patients who accomplished an apprenticeship (accomplished apprenticeship) and patients with an inability to complete professional studies and/or with disability annuity in adulthood (non-professional study). The secondary outcomes were (1.) specialised schooling support defined as speech therapy, ergotherapy, dyslexia training and special school classes and (2.) psychosocial difficulties defined as financial problems and/or psychological therapy and/or broken home. Both had to be documented in the files.
Symptoms of the central nervous system included documented mental retardation and/or speech disorders, and/or neurocognitive impairment and/or attention deficit syndrome.
The frequency of Phe-concentrations measurements were highest in neonates and young children (once monthly up to one measurement every three months) and much lower in adulthood (1–2 times/year). The frequency of Phe-assessment mainly depended on the quality of metabolic control and was, therefore, not standardised. We, therefore, estimated life time Phe exposure as follows: every measured Phe-concentration in all patients was recorded. A mean Phe-concentration/year/patient was calculated. All the Phe concentrations of the patients were depicted in relation to their age (fig. 1). In addition, the mean of all recorded Phe concentrations of the age group (0–2, 2–10, >10 years) per patient was calculated and depicted in relation to the primary outcome (integration into the professional life; i.e. non-professional study; accomplished apprenticeship, high school diploma) and age group (fig. 2). The different time period of observation was chosen according to the therapeutic guidelines of the Swiss Metabolic Group for the follow-up of patients with phenylketonuria (0–2 years, 2–10 years and >10 years, [10]).
The control group consisted of all the healthy siblings and parents of the patients.
The study protocol was submitted to the ethics committee and based on the authorisation for retrospective research (Klinikbewilligung 30 June 2003 between the Inselspital and the Bundesamt für Gesundheit) was approved by the director of research (KEKBE 07–02–2011).
All parameters are given as mean ± SD. Phe-concentrations between the outcome groups (non-professional study, accomplished apprenticeship and high school diploma) were compared using two-way ANOVA. The comparisons between the patients group and the control group was performed by Fisher’s exact test. All analysis were carried out using the statistic program Instat (La Jolla, CA, USA).
The main clinical characteristics are summarised in table 1. A total of 27 patients (13 females, 14 males) were included in the study. The mean (SD) age at the last visit was 27.4 (7.9) years. The range was between 18 and 45 years. The mean follow-up period was 25.1 (7.6) years (range 17–43 years).
A total of 23 patients were diagnosed by neonatal screening, and the 4 remaining patients were diagnosed later during early childhood.
The patients were controlled at least once a month during their childhood (until the age of 5–7 years) and once or twice a year during puberty and adulthood.
A total of 57 controls subjects were recruited. This group consisted of the healthy siblings and parents of the patients, including 26 (45.6%) female and 31 male subjects (54.4%).
Seven patients (26%) did not accomplish professional studies and six of them (22%) required disability annuity (non-professional study). A total of 16 patients (59%) accomplished an apprenticeship (accomplished apprenticeship) and 4 patients (15%) went to a high school or graduated at university (high school diploma). All patients in the accomplished apprenticeship and high school diploma group were diagnosed by neonatal screening meanwhile 4 patients (out of seven) from the non-professional study group were diagnosed during early childhood (18 months up to 3 years old). There were no significant differences with regard to patients with mild PKU versus classical PKU in the three outcome groups.
The control group consisted of 57 subjects (healthy parents and siblings). A total of 9% (5 persons) were in the non-professional study-group, significantly less than in the patient group (p <0.05), 82% (47 persons) were in the accomplished apprenticeship-group, significantly more than in the patient group (p <0.04), and 9% (5 persons) were in the high school diploma-group with no statistical difference compared to the patients.
By excluding the four patients that were not diagnosed by neonatal screening there were no significant differences with regard to the integration into professional life between the patients and the controls.
A total of 55% of all patients needed specialised schooling support during childhood. In the non-professional study group, all 7 patients (100%) had specialised schooling support whereas in the accomplished apprenticeship group only 7 of 16 (44%) benefitted from this support. In the high school diploma group only one patient of four (25%) required it (table 2).
The mean age-dependent phenylalanine-concentrations are depicted in figure 1. There was a tendency for increasing Phenylalanine concentrations with increasing age. This is mainly due to a less strict control of Phe concentrations in the accomplished apprenticeship group.
In figure 2 the mean Phenylalanine concentrations in relation to the primary professional outcome (non-professional study, accomplished apprenticeship, high school diploma) are depicted.
The mean (SD) Phe levels of the non-professional study-group were: 0–2 years: 578 (307) μmol/l; 2–10 years: 679 (287) μmol/l; >10 years: 747 (310) μmol/l. The mean levels in this group were all above the recommended Phe target of the corresponding age group.
The mean (SD) Phe levels of the accomplished apprenticeship-group were: 0–2 years: 456 (156) μmol/l; 2–10 years: 454 (125) μmol/l; >10 years: 712 (284) μmol/l. The mean levels in this group were at the upper limit of the corresponding age and increased with advancing age.
The mean (SD) Phe levels of the high school diploma-group were: 0–2 years: 360 (62) μmol/l; 2–10 years: 320 (62) μmol/l; >10 years: 379 (98) μmol/l. The mean values were in the target range throughout the follow-up.
In the age period 0–2 years there was no statistical significant difference between the three outcome groups. This was due to the lack of sufficient data in this age group, related to the late diagnosis of 4 patients in the non-professional study group. Significant differences in Phe levels between the accomplished apprenticeship and the non-professional study group and the high diploma and the non-professional study group can be documented between 2–10 years with highest levels in the non-professional study group, followed by the accomplished apprenticeship and the high school diploma group (ANOVA p <0.01). In the oldest age group (>10 years old), there was only a tendency for significant differences using the ANOVA model (p = 0.09). The increase in the Phe levels in the accomplished apprenticeship group accounted for this result.
Seven patients (27%) did not accomplish professional studies. Potential causes for this outcome are summarised in table 3. The main reasons were late diagnosis of PKU mainly associated with CNS dysfunction (4 out of seven patients). The remaining 3 patients experienced a difficult psychosocial context and/or did not adhere to the therapy.
| Table 1: Integration into professional life of the patients and the control group. | |||
| No professional studies | Accomplished apprenticeship | High school diploma | |
| Patients (all) | 7 (26%)c | 16 (59%)b | 4 (15%)NS |
| Patients (excluding patients with late diagnosis) | 3 (13%) NS | 16 (70%) NS | 4 (17%) NS |
| Gender | 3F/4M | 7F/9M | 2F/2M |
| Time point of diagnosis | Late diagnosis: 57% (4) | Screening: 100% (16) | Screening: 100% (4) |
| Specialised schooling supporta | 7 (100%) | 7 (44%) | 1 (25%) |
| Control group Parents: Siblings: | 5 (9%) 4 (10.5%) 1 (5.5%) | 47 (82%) 32 (84%) 15 (79%) | 5 (9%) 2 (5.5%) 3 (15.5%) |
| a Defined as logopaedia, ergotherapy, legasthenia training, special school classes; b = p <0.04; c = p <0.05. NS = no statistical difference. | |||
| Table 2:Clinical characteristics of patients with no professional studies/disability annuity. | ||||
| Patient no. | LD | DA | CNS-symptomsa | Difficult psychosocial contextb |
| 1 | – | + | – | + |
| 2 | + | + | + | – |
| 3 | + | – | + | – |
| 4 | – | + | – | + |
| 5 | + | + | + | + |
| 6 | + | + | + | – |
| 7 | – | + | + | + |
| LD = Late diagnosis; DA = disability annuity. a CNS-symptoms = central nervous system, defined as mental retardation, speech disorder, neurocognitive impairment, attention deficit syndrome. b Difficult psychosocial context: defined as financial problems and/or broken home and/or need for psychiatric therapy. | ||||
| Table 3:Clinical Characteristics of Patients with no Professional Studies/Disability Annuity. | |||||
| No of patient | Late diagnosis | DA# | Symptoms of the CNS§ | Malcompliance | Difficult psychosocial context |
| 1 | – | + | + | + | |
| 2 | + | + | + | + | |
| 3 | + | – | + | ||
| 4 | – | + | + | + | |
| 5 | + | + | + | + | |
| 6 | + | + | + | ||
| 7 | – | + | + | + | + |
| § Symptoms of the CNS = central nervous system, defined as mental retardation, speech’s disorder, neurocognitive impairment, attention deficit syndrome. # DA = disability annuity Difficult psychosocial context: defined as financial problems and/or broken home and/or need for psychiatric therapy. | |||||
To our knowledge this is the first study specifically investigating the professional outcome of patients with PKU from childhood until adulthood in a single Swiss tertiary referral centre in relation to the metabolic control during the follow-up. The main findings can be summarised as follows. (1.) The time of diagnosis and the psychosocial context are essential for patients’ professional careers. (2.) The professional outcome of patients with PKU that are diagnosed by neonatal screening is not significantly different compared with a control population (3.) The exposure to elevated Phe levels during childhood may interfere with the professional success of the patients. (4.) Additional specialised schooling support is necessary for a substantial number of patients.
The mean phenylalanine-concentrations of the whole cohort increased with increasing age of the patients (fig. 1) consistent with data from other cohorts [11] and reflects the less strict control from childhood to adulthood. This is consistent with the target Phe concentrations with increasing age [10].
Patients with PKU accomplished professional studies (apprenticeship) significantly less often and received disability annuity significantly more often compared to controls. However, a similar percentage of patients passed a high school diploma compared with the controls. Interestingly, throughout the whole follow-up Phe exposure was significantly higher than the recommended target concentrations in the group without professional studies whereas in the accomplished apprenticeship group Phe levels during childhood were at the upper acceptable limit and increased with increasing age (fig. 2). In contrast, patients with a high school diploma had Phe levels mainly within the target range throughout the whole follow-up (fig. 2). If we assume that IQ, CNS executive function and psychological behaviour affect the integration into professional life and are related to metabolic control, the present data are consistent with the available information in the literature [12, 13]. It also indicates that a lifetime Phe exposure within the recommended target is compatible with high school diploma and studies at the university.
Seven patients (26%) did not accomplish professional studies and six of them (22%) received disability annuity (table 3). In comparison, in 2012 only about 5% of the Swiss population received disability annuity [14]. Four patients in this group were not diagnosed by neonatal screening but during early childhood. The age of definite diagnosis ranged from 18 months until 3 years old. These patients had immigrated to Switzerland from a country where neonatal screening was not mandatory or not available. These patients presented with symptoms and signs of CNS dysfunction that influenced their respective school career. Excluding the four patients with late diagnosis, the patients with PKU had a similar integration into professional life compared with the control group further substantiating the importance of early diagnosis of PKU.
More than half of the patients needed specialised schooling support, decreasing in frequency from the non-professional study to the accomplished apprenticeship and the high school diploma group, in keeping with data from the Netherlands [15] and Germany [16]. It is conceivable that these data can be considered as an early hint in childhood for a later difficult task for the professional integration of these patients. It also supports the notion that the main difficulties of these patients are related to the school career and that sustained support is necessary in order to integrate these patients later into professional life.
This study has limitations: (1.) It is a retrospective analysis. We deliberately included a reliable primary endpoint such as the integration into professional life. We did not include measurements of quality of life that are influenced by a panoply of confounding factors that may change over time. (2.) We included all patients with increased Phe levels (>600 μmol/l) in early childhood or at neonatal screening that needed regular follow-up and nutritional therapy. We are aware that patients with mild PKU have a lower risk for neuropsychological dysfunction that may affect the integration into professional life. However, the percentage of patients with mild PKU versus classical PKU was similar in the three groups and there are data suggesting that patients with hyperphenylalaninaemia can also present with decreased CNS executive functioning [17]. (3.) Based on the small sample size of the subgroups we were not able to clearly distinguish between the negative effect of late diagnosis and Phe exposure during childhood.
In conclusion, these findings indicate that patients with PKU who are diagnosed at neonatal screening and are consequently cared for during childhood and adulthood can accomplish an apprenticeship or a high school diploma. In contrast, late diagnosis and a difficult psychosocial context remains a significant risk for a poor school career. Importantly, specialised schooling support is important in more than 50% of these patients.
Acknowledgement:The authors would like to thank Brigitte Schütz for her meticulous documentation of these patients during childhood.
1 Scriver CR. The PAH gene, phenylketonuria, and a paradigm shift. Hum Mutat. 2007;28:831–45.
2 http://www.neoscreening.ch/de/jahresberichte.htm . Neugeborenenscreening Schweiz.
3 Mitchell John J, Yannis J Trakady, R SC. Phenylalanine Hydroxylase Deficiency. Genet Med. 2011;13:697–707.
4 Smith I, Beasley MG, Ades AE. Intelligence and quality of dietary treatment in phenylketonuria. Arch Dis Child. 1990;65:472–8.
5 Waisbren SE, Noel K, Fahrbach K, Cella C, Frame D, Dorenbaum A, et al. Phenylalanine blood levels and clinical outcomes in phenylketonuria: a systematic literature review and meta-analysis. Mol Genet Metab. 2007;92:63–70.
6 Blau N, van Spronsen FJ, Levy HL. Phenylketonuria. Lancet. 2010;376:1417–27.
7 Moyle JJ, Fox AM, Arthur M, Bynevelt M, Burnett JR. Meta-analysis of neuropsychological symptoms of adolescents and adults with PKU. Neuropsychol Rev. 2007;17:91–101.
8 van Zutphen KH PW, Sporri L, Needham MC, Morgan C, Weisiger K, et al. Executive Functioning in children and adults with phenylketonuria. Clinical Genetics. 2007;72:13–19.
9 Leuzzi V, Pansini M, Sechi E, Chiarotti F, Carducci C, Levi G, et al. Executive function impairment in early-treated PKU subjects with normal mental development. J Inherit Metab Dis. 2004;27:115–25.
10 Ballhausen D, Baumgartner M, Bonafé L, Fiege B, Kern I, JM N. Swiss Metabolic Group: Empfehlungen für die Behandlung der Phenylketonurie und Hyperphenylalaninämie. Paediatrica. 2006;17
11 Abadie V, Berthelot J, Feillet F, Maurin N, Mercier A, de Baulny HO, et al. Neonatal screening and long-term follow-up of phenylketonuria: the French database. Early Hum Dev. 2001;65:149–58.
12 Enns GM, Koch R, Brumm V, Blakely E, Suter R, Jurecki E. Suboptimal outcomes in patients with PKU treated early with diet alone: revisiting the evidence. Mol Genet Metab. 2010;101:99–109.
13 Hujibregts SC, de Sonneville LM, Licht R, van Spronsen FJ, JA S. Short-term dietary interventions in children and adolescents with treated phenylketonuria: effects on neuropsychological outcome of a well-controlled population. J Inherit Metab Dis. 2002;25:419–30.
14 www.bfs.admin.ch. Statistiken zur sozialen Sicherheit. IV Statistik 2012. 2012
15 Bosch AM, Tybout W, van Spronsen FJ, de Valk HW, Wijburg FA, Grootenhuis MA. The course of life and quality of life of early and continuously treated Dutch patients with phenylketonuria. J Inherit Metab Dis. 2007;30:29–34.
16 Simon E, Schwarz M, Roos J, Dragano N, Geraedts M, Siegrist J, et al. Evaluation of quality of life and description of the sociodemographic state in adolescent and young adult patients with phenylketonuria (PKU). Health Qual Life Outcomes. 2008;6:25.
17 Gassio R, Fuste E, Lopez-Sala A, Artuch R, Vilaseca MA, Campistol J, et al. School performance in early and continuously treated phenylketonuria. Pediatr Neurol. 2005;33:267–71.
Funding / potential competing interests: This study was performed in the context of a medical master-thesis of the first author. The authors declare that they have no conflict of interest with regard to this manuscript.
OMIM Number: # 261600