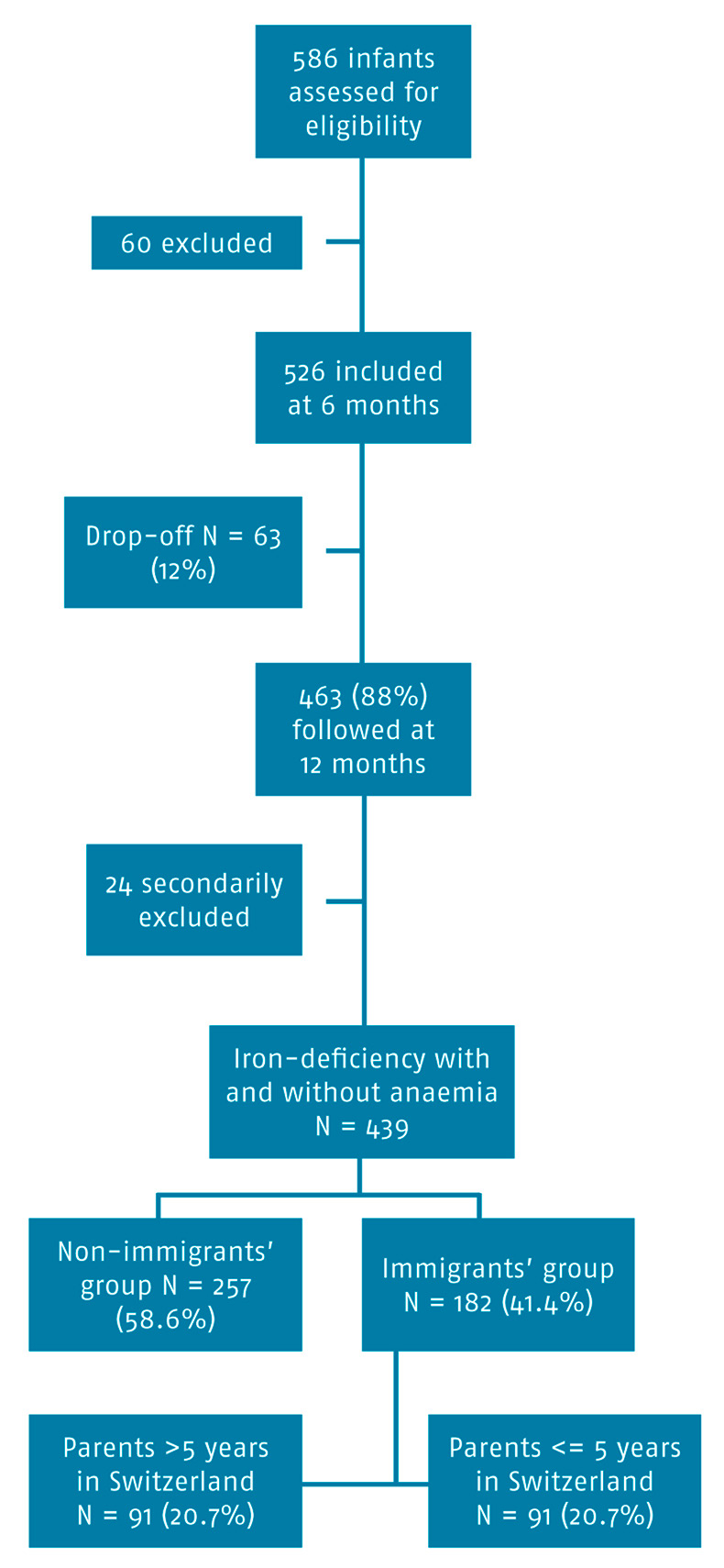
Figure 1
Inclusion of subjects.
DOI: https://doi.org/10.4414/smw.2014.14065
Iron deficiency with or without anaemia is the most common deficiency in the world, particularly in developing countries and in low socioeconomic populations [1–5]. The main cause of anaemia in infancy is low iron intake. Quick growth associated with inadequate intake puts children below 24 months of age at an increased risk of iron deficiency. In the long term, iron deficiency can cause neurocognitive problems, such as psychomotor development delay [6–12]. In the last few years, different risk factors have been reported in the literature: use of milk with poor iron content or excessive consumption of cow’s milk, exclusive breastfeeding over 6 months, prematurity, low birth weight, chronic diseases, and low socioeconomic income [13–18]. Unemployment and poor living conditions are also recognised risk factors for iron deficiency.
Several studies also highlighted the link between acculturation and unhealthy diet. Working antisocial hours or increased hours worked outside of the home, unavailability or high prices of familiar food products, changes in income status are factors for unhealthy diet which can cause iron deficiency [19–21].
The prevalence of iron deficiency and iron-deficient anaemia is not known in Switzerland. Studies conducted in similar countries show that the prevalence of iron-deficient anaemia is between 2% and 5%, and the prevalence of iron deficiency is between 2% and 20%, with a higher prevalence in precarious populations [22–25].
Iron stores are sufficient for the first four to six months after birth. For this reason, deficiency usually does not develop before nine months of age. The Swiss Society of Paediatrics advises that the haemoglobin in every child between six and nine months of age be measured, in order to detect anaemia and treat it. These recommendations take into consideration neither the risk factors nor the impact of such a screening in terms of public health. Moreover, the measurement of haemoglobin does not detect iron deficiency without anaemia.
The aims of our study were to determine the prevalence of iron deficiency with or without anaemia in a part of French-speaking Switzerland that is known for a high percentage of the immigrant population, and to evaluate whether the children of immigrants are at higher risks than the local children.
We conducted a prospective study in a population of infants aged 6 to 12 months and living in Lausanne and its suburbs. In this academic Swiss town with about 200,000 inhabitants and a multiethnic population, the Children’s Hospital of Lausanne is a facility dedicated to children. A high proportion of immigrants consult doctors there. At the Emergency Department, 60% of the consultations proceed from immigrants, with three quarters coming from European countries [26].
Three “family doctors” (paediatrician, general practitioner) and the Children’s Hospital of Lausanne participated in the enrolment of patients. Between 1 November 2005 and 31 October 2007, every parent had been notified of a routine check-up for their six month old infants who were allowed to participate in the study. Exclusion criteria were parental refusal, haematological disease (haemoglobinopathy, enzymatic deficits, or erythrocyte membrane pathology), diseases that could cause anaemia, previous iron supplementation, and participation in other studies.
Children were divided into two groups: immigrants’ and non-immigrants’ children, according to the length of stay of their parents in Switzerland. Families were considered immigrants if they had been in the country ≤10 years at the time of the study. The “immigrants’ group” was divided into two subgroups: those living in Switzerland for less than 5 years and those living there between 6 and 10 years. Unknown length of stay served as a criterion of exclusion from the analysis.
The duration of residence required for acquisition of citizenship varies enormously between European countries. Ranging from 3 (Belgium) to 12 years (Switzerland), the most common condition is 5 years of residence [27, 28]. The limit of 10 years to distinguish between immigrants and non-immigrants’ condition has been artificially defined, based on the median time of residence required to apply for citizenship in Switzerland and in its neighbouring countries. Article 6 of the 1997 European Convention on Nationality (ECN) recommends also a maximum of 10 years of residence to be required.
Paediatricians saw every child for a routine check-up at 12 (within 11 and 13) months of age. Weight, length, head circumference, duration of breastfeeding, time of introduction of formula, fruits and vegetables, cow’s milk, and meat were assessed with a standardised questionnaire. A capillary blood sample was taken to measure the haemoglobin and ferritin levels. MCV, MCH and MCHC were also measured to exclude other causes of anaemia. We also assessed socioeconomic markers such as the professional category of each parent, their comprehension of the French language, and the origin of the parents.
Socioeconomic markers have been rated in two steps: firstly, we categorised job of mother and father according to the professional classification of Largo [29]. A new item was added for unemployment. Then, we summed employments of both parents to determine the socioeconomic level of the family. Housewives were categorised similarly to their husbands.
“Iron deficiency” and “iron-deficient anaemia” were defined according to Looker and Dallman [1]; ferritin below 10 µg/l for iron deficiency and haemoglobin below 110 g/l for anaemia. Iron-deficient anaemia was defined as iron deficiency with anaemia. In the case of iron deficiency or iron-deficient anaemia, children were given an oral treatment of iron 3+ at a dose of 6 mg/kg/day for 3 months. A blood sample was taken at the end of the treatment.
The measurement of haemoglobin and ferritin was delayed if the child presented with 5 days of fever in the 10 days preceding study entry.
Data collected and blood results were entered in the Epidata database (Centers for Disease Control and Prevention, Atlanta, USA). Analyses were performed with Stata 12 (StataCorp LP, Texas, USA) and Epiinfo 3.4.3 (Centers for Disease Control and Prevention, Atlanta, USA). Unrecorded variables were coded as missing.
The aims of the statistical analyses were to determine the prevalence of iron deficiency stratified by groups and establish its risk factors. A p-value <0.05 was considered significant for any univariate analysis. Groups were compared based on their proportion of iron deficiency using non-parametric tests. Logistic regression models were fitted to calculate ORs for crude associations and associations adjusted for potential confounders.
This study was approved by the Ethics Committee of Lausanne. Parents received oral and written information and gave their informed consent.
A total of 586 infants were eligible and 463 were included in the study as they had assessment data at 12 months of age. Twenty-four children were secondarily excluded from the analysis: 13 for unknown length of stay, and 11 because of missing blood values (fig. 1).
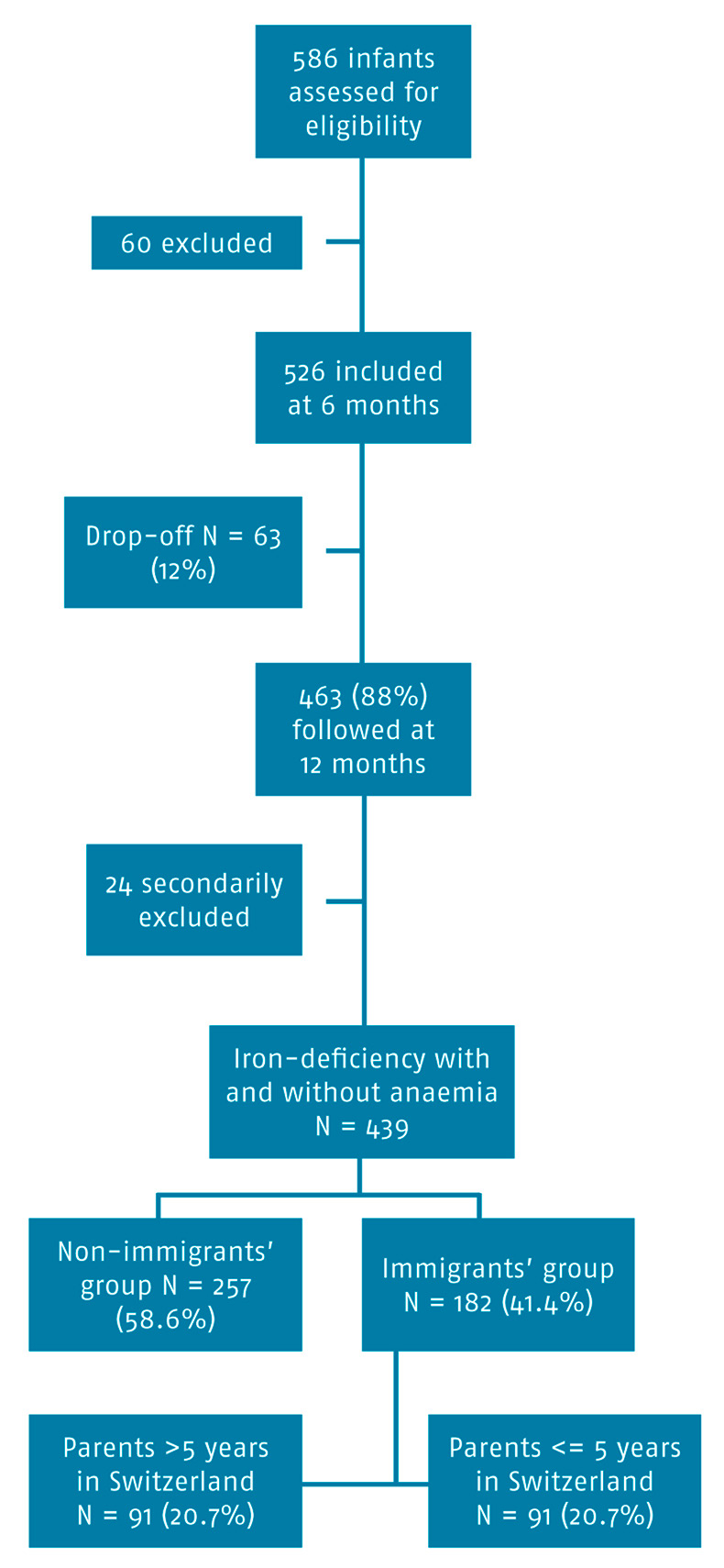
Figure 1
Inclusion of subjects.
The distribution among the two groups was 58.6% in the non-immigrants’ group and 41.4% in the immigrants’ group (20.7% in each subgroup). Our population is similar to our reference population with approximately 68% of permanent residents, 26% of annual permission to reside, and 6% of other permission to reside (table 1). The majority of immigrants came from European countries (West Europe: 70 (27.2 %) in the non-immigrants’ group and 56 (30.8%) in the immigrants’ group, East Europe: 20 (7.8 %) in the non-immigrants’ group and 40 (21.98%) the immigrants’ group). Switzerland represents 55.3% of the non-immigrants’ group with 142 residents.
Mean age at the time of consultation was 12.15 months. There were 230 (52.4%) boys and 209 (47.6%) girls.
More than countries of origin, it is the socio-professional categories that change among the immigrant population. According to the kind of permission to reside and the duration of stay in Switzerland, the categories of employment change. Globally, the proportion of low income or unemployment is higher among people in Switzerland who have been living there for less than 10 years (table 1).
Global prevalence of iron deficiency was 25 (5.7%) at 12 months. Median ferritin was 23.0 µg/l (4–166) at 12 months. Iron-deficient anaemia was diagnosed in two cases (0.5 %) at 12 months. Median haemoglobin was 124.0 g/l (91–174) at 12 months.
There was a statistically significant difference in the prevalence of iron deficiency at 12 months with a prevalence of 3.1% iron deficiency in the non-immigrants’ group versus 12.1% in the immigrants’ group ≤5 years in Switzerland and 6.6% in the immigrants’ group 6 to 10 years in Switzerland (p = 0.006). Iron-deficient anaemia has a low prevalence of 0.5%, with 2 cases. Mean haemoglobin did not differ significantly between groups (table 2).
With regard to food habits, the only statistically significant differences were the duration of breastfeeding and the time of introduction of fruits and vegetables. Breastfeeding lasted 4.02 months in the non-immigrants’ group versus 4.79 months in the immigrants’ group ≤5 years in Switzerland and 4.96 in the immigrants’ group 6 to10 years in Switzerland (p = 0.035); fruits and vegetables were introduced at 5.35 months in the non-immigrants’ group versus 5.07 months in immigrants’ group ≤5 years in Switzerland and 5.08 in the immigrants’ group 6–10 years in Switzerland (p = 0.001). Cow’s milk was introduced at 10.51 versus 10.09 and 10.27 months, baby cereals at 6.74 versus 6.73 and 6.60 months, and meat at 6.61 versus 6.55 and 6.47 months, respectively (NS) (table 1).
In the univariate analysis, the most significant predictors for iron-deficiency are the socio-professional background, especially if parents have a low income or are unemployed (p <0.005), duration of immigration, breastfeeding over 6 months and early cow’s milk feeding. Baby cereals before 9 months seem to serve as a protective factor (table 3).
The multivariable analysis confirmed those predictors of iron deficiency, except for breastfeeding over 6 months of age and early cow’s milk feeding. Immigration in the last 5 years and low income were the most significant predictors of iron deficiency, as the introduction of baby cereals before 9 months seems to serve as a protective factor (table 3).
| Table 1: Patient demographics. | |||||
| General | Non-immigrants n (%) | Immigrants | p-value | ||
| ≤5 years in CH | 6–10 years in CH | ||||
| No. total | 439 (100%) | 257 (58.6%) | 91 (20.7%) | 91 (20.7%) | |
| Permission to reside | |||||
| Swiss or naturalised citizen | 147 (33.5%) | 142 (55.3%) | 1 (1.1%) | 4 (4.4%) | N/A |
| Permanent permission to reside | 151 (34.4%) | 98 (38.1%) | 11 (12.1%) | 42 (46.1%) | |
| Annual permission to reside | 112 (25.5%) | 10 (3.9%) | 65 (71.4%) | 37 (40.7%) | |
| Other permission to reside | 17 (3.9%) | 10 (11.0%) | 7 (7.7%) | ||
| Unknown | 12 (2.7%) | 7 (2.7%) | 4 (4.4%) | 1 (1.1%) | |
| Gender | |||||
| Male | 230 (52.4) | 136 (52.9%) | 45 (49.5%) | 49 (53.8%) | 0.810 |
| Food habits | |||||
| Mean time of breastfeeding (sd) | 4.370 (3.132) | 4.019 (3.063) | 4.793 (3.249) | 4.959 (3.110) | 0.035 |
| Mean time of introduction of fruits/vegetables (sd) ** | 5.234 (0.830) | 5.347 (0.840) | 5.067 (0.802) | 5.083 (0.783) | 0.001 |
| Mean time of introduction of cow's milk (sd) | 10.352 (1.633) | 10.510 (1.324) | 10.094 (1.994) | 10.273 (1.825) | 0.712 |
| Mean time of introduction of baby cereals (sd) | 6.709 (0.977) | 6.739 (0.997) | 6.730 (1.075) | 6.603 (0.804) | 0.311 |
| Mean time of introduction of meat (sd) | 6.568 (0.883) | 6.608 (0.869) | 6.551 (0.957) | 6.471 (0.847) | 0.427 |
| Category of income | |||||
| High and middle-class income n (%) | 359 (81.8) | 230 (89.5) | 69 (75.8) | 60 (65.9) | N/A |
| Low income | 64 (14.6) | 21 (8.2) | 20 (22.0) | 23 (25.3) | |
| Unemployment | 14 (3.2) | 4 (1.5 ) | 2 (2.2) | 8 (8.8) | |
| Missing values | 2 (0.4 %) | 2 (0.8%) | N/A | ||
| **: statistically significant N/A: not applicable | |||||
| Table 2: Laboratory characteristics of subjects. | |||||
| General n = 439 | Non-immigrants n = 257 | Immigrants | p-value | ||
| ≤5 years in CH n = 91 | 6–10 years in CH n = 91 | ||||
| Median haemoglobin (range) | 124.0 (91.0–174.0) | 123 (91–174) | 122 (105–147) | 125 (98–146) | 0.549 |
| Median ferritin (range) ** | 23.0 (4.0–166.0) | 23 (4–122) | 19 (4–104) | 24 (4–166) | 0.036 |
| Iron-deficiency n (%) ** | 25 (5.7%) | 8 (3.1%) | 11 (12.1%) | 6 (6.6%) | 0.006 |
| Iron-deficient anaemia n (%) | 2 (0.5%) | 0 (0%) | 1 (1.1%) | 1 (1.1%) | 0.242 |
| **: Statistically significant N/A: not applicable | |||||
| Table 3: Predictors of iron-deficiency with or without anaemia at 12 months (crude associations). | |||||
| Parameters | Patients without iron-deficiency n = 414 (%) | Patients with iron-deficiency n = 25 (%) | Odds ratio | 95% CI | p-value |
| Male | 217 (94.3%) | 13 (5.7%) | 1.02 | 0.45–2.28 | 0.968 |
| Small for date | 23 (88.5%) | 3 (11.5%) | 2.27 | 0.63–8.15 | 0.208 |
| Prematurity | 17 (100%) | 0 (0%) | Undefined | Undefined | N/A |
| Anaemia (Hb <110 g/l) | 18 (90 %) | 2 (10 %) | 1.91 | 0.42–8.75 | 0.403 |
| Median haemoglobin (range)** | 124 (91–174) | 119 (105–130) | 0.922 | 0.88–0.97 | 0.001 |
| Immigrants | |||||
| Non-immigrants | 249 (96.9%) | 8 (3.1%) | 1 | ||
| 0–5 years in Switzerland** | 80 (87.9%) | 11 (12.1%) | 4.280 | 1.66–11.01 | 0.003 |
| 6–10 years in Switzerland | 85 (93.4%) | 6 (6.6%) | 2.20 | 0.74–6.51 | 0.156 |
| Nutrition | |||||
| Breastfeeding over 6 months** | 11 (44 %) | 14 (56 %) | 1.70 | 0.76–3.84 | 0.199 |
| Early cow's milk feeding (<9 months)** | 34 (87.2%) | 5 (12.8%) | 2.79 | 0.99–7.91 | 0.053 |
| Fruits before 6 months | 281 (94.3%) | 17 (5.7%) | 1.01 | 0.42–2.39 | 0.99 |
| Baby cereals after 9 months** | 26 (81.3%) | 6 (18.8%) | 4.71 | 1.73–12.81 | 0.002 |
| Meat before 6 months | 26 (89.7%) | 3 (10.3%) | 2.04 | 0.57–7.25 | 0.273 |
| Socioeconomic background | |||||
| Family <3 children | 355 (93.9%) | 23 (6.1%) | 1.91 | 0.44–8.32 | 0.388 |
| Single-parent family | 16 (88.9%) | 2 (11.1%) | 2.14 | 0.46–9.85 | 0.331 |
| Poor French comprehension of the mother | 40 (90.9%) | 4 (9.1%) | 1.77 | 0.58–5.42 | 0.316 |
| Socio-professional background | |||||
| High and middle-class income | 1 | ||||
| Low income** | 5.35 | 2.2–13.0 | 0.000 | ||
| Unemployment** | 7.89 | 1.94–32.0 | 0.004 | ||
| ** Statistically significant N/A: not applicable | |||||
This study aimed at evaluating the prevalence of iron deficiency and iron-deficient anaemia in a part of French-speaking Switzerland known for a high percentage of the immigrant population, and also at assessing whether the children of immigrants were at higher risks than the local children.
The prevalence of iron deficiency in similar countries is between 2% and 20%. In our study, prevalence was generally in the mean for iron deficiency and low for iron-deficient anaemia.
At 12 months, we found a significant difference in the prevalence of iron deficiency between immigrants and non-immigrants. Among risk factors, we underline the prevalent role of immigration and employment as well as the protective effect of baby cereals, but not food diversification in itself.
As far as it is known, food is the main source of iron and, thus, the best way to avoid iron deficiency. It should be noted that in Switzerland, all baby cereals contain iron supplementation, which explains its protective role. Several studies mention iron supplementation in some kind of food, such as rice or cereals, as a means to treat and avoid iron deficiencies in low-income and poor families [12, 30–32].
One of the risk factors for iron deficiency is the immigrants’ status. There are a number of definitions of a migrant, all focusing on one point or another. According to the UN convention on the rights of migrants, “The term migrant can be understood as “any person who lives temporarily or permanently in a country where he or she was not born, and has acquired some significant social ties to this country.” However, this may be a too narrow definition when considering that, according to some states’ policies, a person can be considered as a migrant even when s/he is born in the country” [33].
In our study, the first five years in a country seem to be crucial, after which the odds decline significantly (table 3). Migration and food have been largely studied, and the lack of some special kind of food as well as the contact with local people lead to changes in the diets. After a few years, people become accustomed to the host country, and new ingredients are included in the diet [21, 34, 35].
Breastfeeding interacts with every other variables in the multivariable analysis. Though the duration of breastfeeding varies between immigration’s groups, our study cannot highlight any influence on iron deficiency.
Some studies report early cow’s milk feeding as a factor of iron deficiency. We did not find any significant association, but the multivariable analysis shows that early cow’s milk feeding interacts with the category of income as well as with the duration of immigration. The explanation could be of cultural habits or because of income difficulties, as infant formula is more expensive. Several studies also observe racial/ethnic disparities. We cannot exclude such an influence on our results, although we did not find any differences based on the origin of the parents. We did not investigate the link between ethnicity and socio-professional categories.
The strong correlation between the category of employment and iron deficiency enhances the link between socioeconomic conditions and iron deficiency, irrespective of the immigration status. Unemployment and low income multiply by six the risk of iron depletion and serve as our strongest predictor (table 3). Unfortunately, we only assessed the time of introduction of each type of food. It would have been interesting to also assess its quantity, as socioeconomic conditions determine the quality and quantity of food ingested [36]. In contrast to what we expected, we did not find other known risk factors such as gender, prematurity, low birth weight, and prolonged breastfeeding. Good health, nutritional and socioeconomic conditions of our country can explain those differences. However, recruiting our population through three paediatricians and a paediatric hospital may have induced a selection bias; all patients included, as most people in Switzerland, had an optimal access to health care and a regular medical follow-up.
Serum ferritin is the most common and inexpensive tool for the detection of iron deficiency. It is, however, influenced by inflammation or infection [37]. Though we delayed the blood tests in every child presenting fever, we could not exclude some falsely elevated ferritin in our sample. Usually, iron-deficient anaemia is discovered at two or three years of age. Our study permitted the detection and treatment of many iron deficiencies at 12 months.
We conclude that in our studied population, the prevalence of iron deficiency was lower than that reported in the literature for a similar population. Good socioeconomic conditions in Switzerland, the quality of food for pregnant women and young infants can explain this phenomenon. Immigrants are more at risk than non-immigrants, especially after six months of age. Low income and unemployment in both groups seem to be the best predictors of iron deficiency. A study up to five years of age is needed before drawing general conclusions on infancy.
| Table 4: Predictors of iron-deficiency with or without anaemia at 12 months (multivariable analysis). | |||
| Risk factors | Adjusted odds ratio | 95% CI | p-value |
| Immigration | |||
| Non-immigrants | 1 | ||
| Immigration at 0–5 years in CH** | 2.91 | 1.05–8.04 | 0.0399 |
| Immigration at 6–10 years in CH | 1.12 | 0.32–3.93 | 0.8556 |
| Nutrition | |||
| Early cow's milk feeding | 3.0481 | 0.96–9.68 | 0.0587 |
| Baby cereals after 9 months** | 6.8872 | 2.18–21.77 | 0.0010 |
| Breastfeeding over 6 months | 1.9606 | 0.80–4.82 | 0.1427 |
| Socio-professional background | |||
| High and middle-class income | 1 | ||
| Low income** | 5.9308 | 2.18–16.11 | 0.0005 |
| Unemployment** | 6.0861 | 1.18–31.30 | 0.0307 |
| **Statistically significant | |||
Prevalence of iron deficiency is lower than that reported in the literature for a similar population.
Low income and immigration seem to be the best predictors of iron deficiency.
Starting baby cereals before nine months is a protective factor.
Acknowledgments: The authors gratefully acknowledge the contribution and support of Doctor JD. Krähenbühl, Doctor M. Monney, Doctor F. Basha and Doctor H. Vienny, as well as Mrs J. Bersier and her team of the laboratory for the precious contribution to the study. They also thank the participating children, their parents, and the study team, including field workers. This work has been orally presented at the annual congress of the Swiss Society of Paediatrics in Montreux on 1 September 2011.
1 Looker AC, Dallman PR, Carroll MD, et al. Prevalence of iron deficiency in the United States. JAMA: the journal of the American Medical Association. 1997;277(12):973–6.
2 Centers for Disease C, Prevention. Iron deficiency – United States, 1999–2000. MMWR Morbidity and mortality weekly report. 2002;51(40):897–9.
3 Who/Cdc. Assessing the iron status of populations: report of a Joint World Health Organization / Centres for Disease Control and Prevention Technical Consultation on the assessment of iron status at the population level. Geneva, Switzerland 2005.
4 Oski FA. Iron deficiency in infancy and childhood. N Engl J Med. 1993;329(3):190–3.
5 Zlotkin S. Clinical nutrition: 8. The role of nutrition in the prevention of iron deficiency anemia in infants, children and adolescents. CMAJ: Canadian Medical Association journal = journal de l’Association medicale canadienne. 2003;168(1):59–63.
6 Boutry M, Needlman R. Use of diet history in the screening of iron deficiency. Pediatrics. 1996;98(6 Pt 1):1138–42.
7 Idjradinata P, Pollitt E. Reversal of developmental delays in iron-deficient anaemic infants treated with iron. Lancet. 1993;341(8836):1–4.
8 Lozoff B, Jimenez E, Wolf AW. Long-term developmental outcome of infants with iron deficiency. N Engl J Med. 1991;325(10):687–94.
9 Lukowski AF, Koss M, Burden MJ, et al. Iron deficiency in infancy and neurocognitive functioning at 19 years: evidence of long-term deficits in executive function and recognition memory. Nutr Neurosci. 2010;13(2):54–70.
10 Pisacane A, De Vizia B, Valiante A, et al. Iron status in breast-fed infants. J Pediatr. 1995;127(3):429–31.
11 Carter RC, Jacobson JL, Burden MJ, et al. Iron deficiency anemia and cognitive function in infancy. Pediatrics. 2010;126(2):e427–34.
12 Falkingham M, Abdelhamid A, Curtis P, et al. The effects of oral iron supplementation on cognition in older children and adults: a systematic review and meta-analysis. Nutrition journal. 2010;9:4.
13 Aggett PJ, Agostoni C, Axelsson I, et al. Iron metabolism and requirements in early childhood: do we know enough?: a commentary by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2002;34(4):337–45.
14 Bamberg R. Occurrence and detection of iron-deficiency anemia in infants and toddlers. Clinical laboratory science: journal of the American Society for Medical Technology. 2008;21(4):225–31.
15 Beard J. Recent evidence from human and animal studies regarding iron status and infant development. J Nutr. 2007;137(2):524S–30S.
16 Grant CC, Wall CR, Wilson C, et al. Risk factors for iron deficiency in a hospitalized urban New Zealand population. J Paediatr Child Health. 2003;39(2):100–6.
17 Kahigwa E, Schellenberg D, Sanz S, et al. Risk factors for presentation to hospital with severe anaemia in Tanzanian children: a case-control study. Tropical medicine & international health: TM & IH. 2002;7(10):823–30.
18 Yang Z, Lonnerdal B, Adu-Afarwuah S, et al. Prevalence and predictors of iron deficiency in fully breastfed infants at 6 mo of age: comparison of data from 6 studies. Am J Clin Nutr. 2009;89(5):1433–40.
19 Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. J Am Diet Assoc. 2008;108(8):1330–44.
20 Popovic-Lipovac A, Strasser B. A Review on Changes in Food Habits Among Immigrant Women and Implications for Health. Journal of immigrant and minority health / Center for Minority Public Health. 2013 Jul 28.
21 Mata Codesal D. Eating abroad, remembering (at) home. Anthropology of food [online]. 2010;7 | December 2010.
22 Cusick SE, Mei Z, Freedman DS, et al. Unexplained decline in the prevalence of anemia among US children and women between 1988–1994 and 1999–2002. Am J Clin Nutr. 2008;88(6):1611–7.
23 Male C, Persson LA, Freeman V, et al. Prevalence of iron deficiency in 12–mo-old infants from 11 European areas and influence of dietary factors on iron status (Euro-Growth study). Acta Paediatr. 2001;90(5):492–8.
24 Brotanek JM, Gosz J, Weitzman M, et al. Iron deficiency in early childhood in the United States: risk factors and racial/ethnic disparities. Pediatrics. 2007;120(3):568–75.
25 Brotanek JM, Halterman JS, Auinger P, et al. Iron deficiency, prolonged bottle-feeding, and racial/ethnic disparities in young children. Arch Pediatr Adolesc Med. 2005;159(11):1038–42.
26 Gehri M, Hunziker B, Geraud F, et al. Migrant populations at the Hopital de l’Enfance of Lausanne (HEL): evaluation inquiry, taking care and contribution of cultural mediators-translators. Sozial- und Praventivmedizin. 1999;44(6):264–71.
27 Niessen J, Huddleston T. Setting up a system of benchmarking to measure the success of integration policies in Europe. Brussels, European Parliament: The European Parliament’s committee on Civil Liberties Justice and Home Affairs; 2007. Report No.: IP/C/LIBE/ST/2005–93.
28 Goodmann SW. Naturalisation Policies in Europe: Exploring Patterns of Inclusion and Exclusion. San Domenico di Fiesole (FI), Italy: EUDO Citizenship Observatory, Robert Schuman Centre for Advanced Studies; 2010. Report No.: Comparative Report, RS CAS/EUDO-CIT-Comp.2010/7.
29 Largo RH, Pfister D, Molinari L, et al. Significance of prenatal, perinatal and postnatal factors in the development of AGA preterm infants at five to seven years. Dev Med Child Neurol. 1989;31(4):440–56.
30 Brotanek JM, Gosz J, Weitzman M, et al. Secular trends in the prevalence of iron deficiency among US toddlers, 1976–2002. Arch Pediatr Adolesc Med. 2008;162(4):374–81.
31 (Scris). Population étrangère selon la nationalité et le type de permis de résidence, Commune de Lausanne, 2000 2000 [Accessed; Available from: http://www.scris-lausanne.vd.ch/Default.aspix?DomID=1597
32 Hercberg S, Preziosi P, Galan P. Iron deficiency in Europe. Public health nutrition. 2001;4(2B):537–45.
33 Unesco. Accessed 10 October 2012; Available from: http://www.unesco.org/new/en/social-and-human-sciences/themes/international-migration/glossary/migrant/
34 Rivera JA, Shamah T, Villalpando S, et al. Effectiveness of a large-scale iron-fortified milk distribution program on anemia and iron deficiency in low-income young children in Mexico. Am J Clin Nutr. 2010;91(2):431–9.
35 Roville-Sausse F, Prado Martinez C. Alimentation et santé des femmes migrantes chinoises et de leurs enfants en Europe occidentale: l’exemple de la France et de l’Espagne (Food and Health of the Chinese migrant women and their children in West Europe: the example of France and Spain). Anthrop. 2009(19):47–56.
36 Dedaire M, Tozanli S. Les paradoxes des distances dans la construction des identités alimentaires par acculturation (Paradoxes of acculturation process that arise during the identity (re)constructionin the field of food consumption and eating habits). Anthropology of food [online]. 2007;S3 | December 2007.
37 Goddard AF, James MW, Mcintyre AS, et al. Guidelines for the management of iron deficiency anaemia. Gut. 2011;60(10):1309–16.
Funding / potential competing interests: The study was supported by the Wyeth Foundation.