DOI: https://doi.org/10.4414/smw.2014.14040
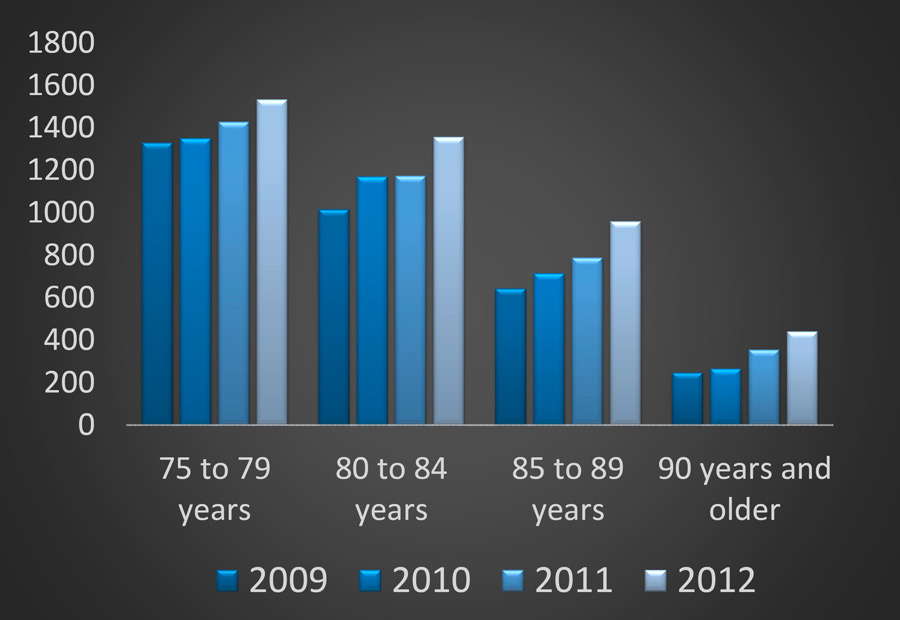
Why should we specifically address the age-centred care of older patients in emergency departments (EDs)? First, the use of EDs by old patients will continue to increase along with life expectancy, and older people are a growing demographic. Data from Bern University Hospital showed an increase in emergency consultations by patients aged 75 years and older from 2009 to 2012 (fig. 1). Secondly, older patients present to the ED with more complex problems [1]. Symptoms may be atypical and mislead the diagnostic process [2–4]. Older patients often have functional deficits and co-morbidities blending diagnosis [2–5]. Functional deficits and co-morbidities, including poly-pharmacy for co-morbidities, have to be taken into account when prescribing new medications and other treatments. Thirdly, outcomes are, in general, worse than in younger patients [1], and there is evidence that age-centred approaches improve outcomes [6]. Finally, many emergency physicians and nurses have not been specifically trained in emergency medicine for the elderly. Therefore, it is timely to review important aspects of specific care for older patients in EDs.
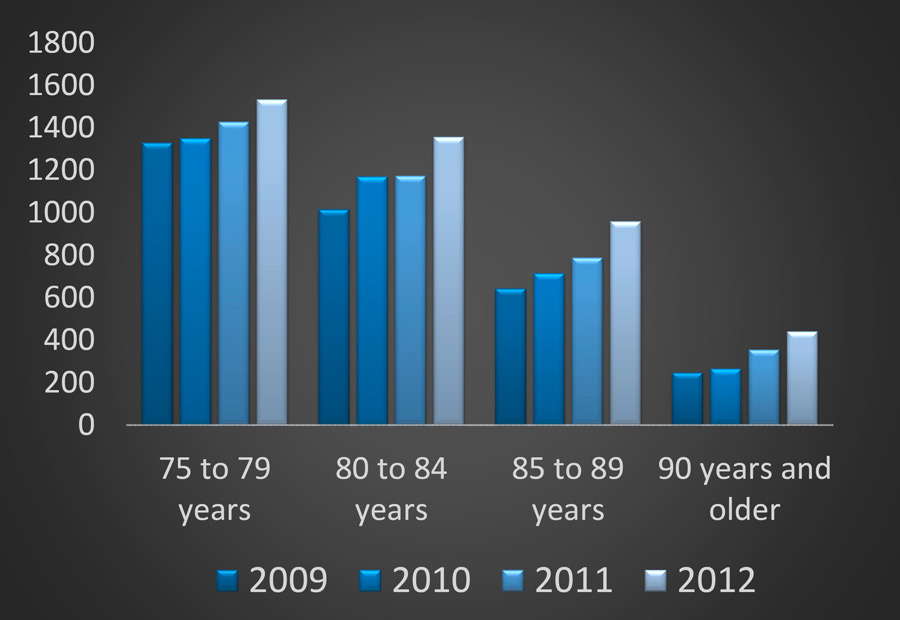
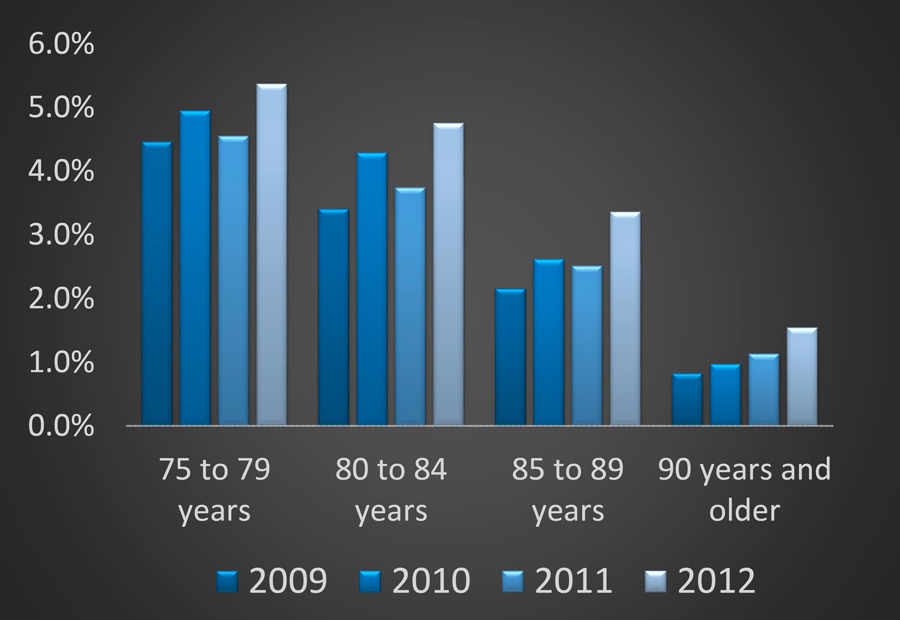
Figure 1
Emergency consultations of patients 75 years and older at Bern University Hospital from 2009 to 2012: absolute numbers (a) and percentage in relation to all ED consultations (b).
There are age-specific aspects in nearly every acute or chronic illness. This review intends to elucidate some specific conditions which deserve particular attention in older ED patients.
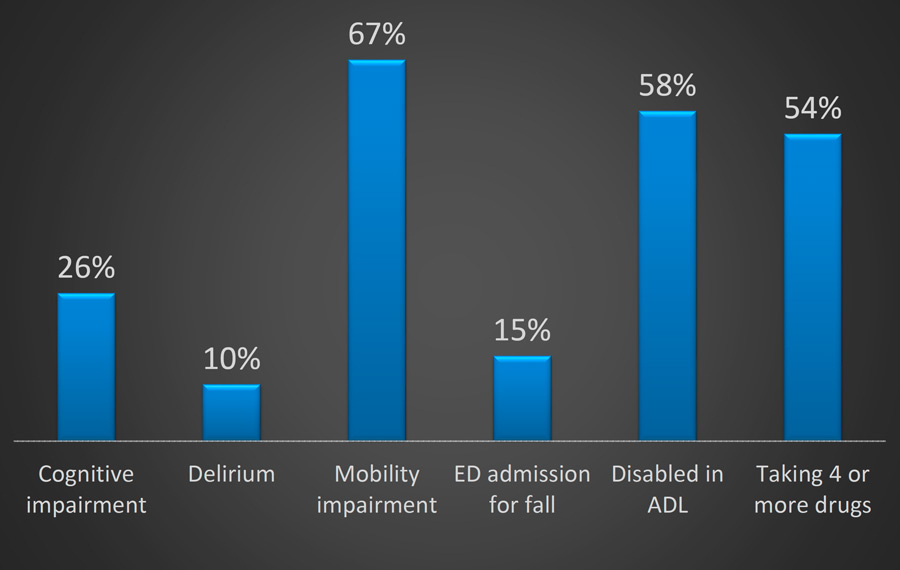
Figure 2
Prevalence of conditions needing attention in older ED patients. ADL = activities of daily living.
Cognition is a term standing for brain function. Cognitive screenings, adapted to the ED setting, should be part of routine examinations by emergency physicians for several reasons. Firstly, cognitive function is often impaired in older ED patients: cognitive impairment is found in approximately every fourth older ED patient (fig. 2) [7]. Secondly, cognitive impairment is recognised in fewer than half of patients, if not screened for routinely [7]. Thirdly, cognitive impairment has consequences. For example, information about the patient’s cognition is important to judge his/her ability to provide informed consent to the diagnostic and therapeutic interventions in the ED. Furthermore, cognitive impairment may lead to non-adherence, and this may have deleterious consequences in ED patients, particularly those discharged home after the ED stay. Fourth, cognitive impairment may indicate important underlying diseases with diagnostic and therapeutic consequences. The differential diagnosis of cognitive impairment embraces the three Ds: dementia, delirium, and depression.
Dementia is a chronic disorder of cognition and develops over a longer time period. It is not the primary focus of attention in EDs to make a new diagnosis of dementia. However, it is important to increase emergency physicians’ awareness of pre-existing dementia because dementia is the leading pre-disposing factor for delirium. Two-thirds of delirium cases occur in patients with pre-existing dementia [8]. Emergency physicians’ awareness of pre-existing dementia can be increased by cognition screening. In a recent study, routine cognitive screening nearly doubled the frequency of cognition-related diagnosis on ED discharge reports [5]. Delirium is an acute disorder of cognition and attention, and one of the main reasons for abnormal cognition in the ED. It is estimated that delirium is present in approximately 10% of older ED patients (fig. 2) [7]. Again, delirium is only recognised in about 16% of patients if screening is not performed routinely in each older ED patient [9]. Delirium worsens outcomes: older patients with delirium have a 3–fold increased risk of nursing home placement after the hospital stay and a nearly 2–fold increased risk of dying [10].
Mobility is another important condition which requires particular attention in older ED patients. Mobility is impaired in about 2 out of 3 older ED patients (fig. 2) [5]. Impaired mobility is a risk factor for falls. Falls are one of the leading causes of ED admission among older patients and account for approximately 15% of all ED admissions of patients 75 years or older [5]. Approximately 50% of older ED patients have had at least one fall within the 12 months prior to ED admission [5]. Impaired mobility is also a predictor of prolonged stay in hospital and worse outcomes, including nursing home admission and death [5, 11, 12]. As with cognition, mobility is often not routinely and systematically screened for in EDs. Mobility impairment therefore often remains undetected [5].
As a consequence of functional deficits, the conduct of usual daily activities may be compromised. Activities of daily living (ADL) embrace activities such as feeding, dressing, or bathing [13]. The older person may become dependent on another person’s help to perform ADL, and this is called disability. In today’s EDs, ADL and disability are seldom measured, even though approximately 3 out of 5 older ED patients are disabled in at least one ADL (fig. 2) [5]. Moreover, 3 out of 4 older ED patients affirm that a decrease in their ability to perform ADL was driving their decision to present to the ED [14]. Studies have also shown that a decline in the ability to perform ADL – either pre-existing or arising from acute illness – is an important predictor of further functional decline, in-hospital length of stay, repeat ED visits, nursing home admission or death [5, 15].
Along with the increasing number of co-morbidities, the number of medications increases with age. In an analysis of ED patients aged 65 years of age and older, 91% were taking one or more medications (prescribed or over the counter) and the mean number of medications was 4 (with a maximum range from 0 to 17) [16]. Approximately 54% of older ED patients take 4 or more medications (fig. 2) [16]. Due to the increasing number of medications with age and physiological changes with ageing, adverse drug-related events are more frequent in older than in younger patients. Data suggest that adverse drug-related events account for 11% of ED visits [16]. Using systematic medication checking, 11% of older ED patients were found to be taking potentially inappropriate medications [17].
Acute illness leading to ED admission often presents atypically in older patients [2, 3]. Atypical presentation in older ED patients is facilitated by several factors, in particular co-morbidities, medications and/or functional deficits that produce additional symptoms and/or mask the leading symptom. Atypical presentation has two important consequences. First, atypical presentation broadens the differential diagnosis. For example, acute myocardial infarction may present atypically as general weakness in older ED patients [4]. Second, atypical presentation may increase time delay to treatment due to undertriage. One recent study examined a widely-used triage instrument and found that the triage instrument identified fewer than half of older ED patients requiring an immediate life-saving intervention [18]. Undertriage contributes to the worse prognosis of older ED patients compared to younger patients [2, 3].
| Table 1: Selection of geriatric screening/assessment instruments suited for use in the ED. | |||||
| Domain | Instrument | Number of items | Rating method | Time needed to administer | References |
| Cognition | Short blessed test | 6 items | Performance-based | ~3–5 minutes | [19, 20] |
| Delirium | Confusion assessment method | 4 items | Observer-based | ~1–4 minutes | [21] |
| Mobility | Timed up and go test | 1 item | Performance-based | ~1–3 minutes | [23] |
| Autonomy | Activities of daily living | 5 items | Self-report | ~1–4 minutes | [13] |
| Multidimensional | Emergency geriatric screening | 15 items | Performance-based (for cognition and mobility) and self-report (for falls and ADL) | ~4–5 minutes | [5] |
| Risk screening tool | Identification of Seniors at Risk | 6 items | Self-report | ~1–2 minutes | [35] |
| ADL = activities of daily living | |||||
| Table 2: Emergency geriatric screening (EGS) tool, consisting of short validated instruments for screening four domains (cognition, falls, mobility, and activities of daily living) [13, 19, 23]. | ||
| Cognition | ||
| Instruction: Ask the patient the following questions. If the patient does not respond, the question is rated incorrect. | ||
| What day is today? | Incorrect* | Correct |
| What is the date today? (± 1 day is correct) | Incorrect* | Correct |
| What year is this? | Incorrect* | Correct |
| Spell “radio” backwards. | Incorrect | Correct |
| Evaluation consistent with impairment of cognition (if one single response was incorrect): | Yes | No |
| Falls | ||
| Instruction: Rate the following questions considering all available sources (patient, proxy, observation, reports). | ||
| Did the patient present to the ED because of a fall? | Yes* | No |
| Did the patient have one or more falls during the last 12 months? | Yes | No |
| Evaluation consistent with patient history of falls (if one single response was yes): | Yes | No |
| Mobility | ||
| Instruction: Rate the following question considering all available sources (patient, proxy, observation, reports). | ||
| Did the patient require walking aids (cane, wheeled walker, or helping person) in- or outdoors before presenting to the ED? | Yes | No |
| Instruction: Rate the following questions according to the current situation in the ED. | ||
| Is the patient currently confined to bed? | Yes* | No |
| Does the patient currently need help (walking aids or helping person) to get out of bed? | Yes* | No |
| Does the patient need ≥20 seconds for the Timed Up and Go Test? | Yes | No |
| Evaluation consistent with impairment of mobility (if one single response was yes): | Yes | No |
| ADL | ||
| Instruction: Rate the following question considering all available sources (patient, proxy, observation, reports). | ||
| Did the patient require assistance for personal hygiene (sponge bath, tub bath, or shower) before presenting to the ED? | Yes* | No |
| Instruction: Rate the following questions according to the current situation in the ED. | ||
| Is the patient currently confined to bed or does he need help (walking aid or helping person) to get out of bed? | Yes* | No |
| Does the patient require assistance (for direct help or instruction) for dressing (clothes or shoes)? | Yes* | No |
| Does the patient require assistance (for direct help or instruction) for toileting? | Yes* | No |
| Does the patient require assistance (for direct help or instruction) for feeding? | Yes | No |
| Evaluation consistent with impairment in ADL (if one single response was yes): | Yes | No |
| ADL = activities of daily living; ED = emergency department. * If one of the responses marked with an asterisk applies, the rater may directly proceed to evaluating the domain (hierarchical structure). | ||
Improving the care of older ED patients always includes screening and appropriate management. As described in the previous section, screening for functional deficits is of the utmost importance in detecting otherwise unrecognised conditions. Along with appropriate management, outcomes may be improved in older ED patients. As ED settings vary considerably between hospitals, screening and management steps have to be adapted to the local situation.
Concepts of care recommend cognition screening, including delirium [8]. We recommend performing a test for cognition first and, if the test is abnormal, to add a specific test to diagnose delirium and to differentiate it from dementia or depression. A widely used cognition test, that is feasible and validated in the ED setting, is the Short Blessed Test (SBT) (table 1) [19, 20]. The SBT consists of 6 short items testing orientation, short-term memory, and attention. If abnormal, the Confusion Assessment Method (CAM) may be added to diagnose or exclude delirium as a cause of the abnormal cognition (table 1) [21]. The CAM is a four-item tool, feasible within a few minutes, and detects delirium with high sensitivity and specificity. The four items are questions which are rated by the examining clinician. The rating of the CAM questions is particularly easy, fast and accurate, if the rating clinician has previously performed the SBT. Recently, a novel modified CAM was specifically developed for use in the ED [22].
In patients with cognitive impairment and/or delirium, several management steps have to be taken into consideration. The detected problem should be mentioned on reports. The ED physician should check whether potential causative factors have been sufficiently considered (e.g., laboratory measurements to rule out electrolyte imbalances, imaging of the brain to rule out brain affections). Drugs potentially causing the cognitive problem should be stopped, whenever possible. In acutely ill patients with pre-existing dementia, delirium prevention has to be administered, as this is an effective strategy to reduce delirium frequency and its complications (approximately 30–40% of delirium cases may be prevented) [8]. In ED patients with ongoing delirium, delirium treatment has to be initiated to improve outcomes. In cognitively impaired older ED patients discharged home, management includes measures guaranteeing adherence after ED discharge. For example, relatives, home nurses and/or general practitioners have to be informed and involved. Depending on the situation, dementia evaluation has to be recommended.
Screening for impaired mobility may be performed using validated tests, such as the Timed Up and Go Test (table 1) [23]. These tests may also be adapted for use in the ED setting. For example, introductory questions can quickly identify patients with impaired mobility who do not have to be mobilised for the test. This helps to reduce the mean time required for the test [8].
If mobility is impaired, the problem including its causative factors should be mentioned in the patient’s report. The ED physician should check whether all urgent consequences have been considered (e.g., stop of drugs facilitating the mobility problem) and whether further diagnostic and/or therapeutic steps have to be recommended. For example, mobility training may be useful in many patients discharged home. Depending on the situation, fall prevention measures should be implemented. In hospitalised patients, early geriatric management, which can be performed in any ward and has been evaluated successfully in geriatric wards, not only reduces in-hospital length of stay, but also improves the functional status of the patients and dramatically reduces discharge to a long-term care institution by 36% (relative risk reduction) [24]. If early mobility training is not available on the acute ward, the patient with impaired mobility should be considered a candidate for subsequent rehabilitation, in order to reduce his chance of being admitted to a nursing home [25].
In older ED patients admitted after a fall, it is important to search for the cause of the fall. The causes are different in older versus younger ED patients: whereas accidents (i.e., fall due to external force) or medical diseases (e.g., epilepsy) are frequent causes for falls in younger ED patients, the combination of intrinsic and extrinsic factors is the most frequent cause of a fall in older patients [26]. An intrinsic factor means an increased disposition of the body to fall (e.g., due to muscle weakness, disturbed equilibrium, or an eye problem). In combination with an extrinsic factor (e.g., carpet border, doorstep), a fall may result. In our experience, the intrinsic and extrinsic factors are frequently not checked in older fall patients, though these factors would provide important information about further treatment (e.g., rehabilitation after the acute phase, home assessment to reduce falls risk factors at home) [27, 28].
Screening for disability may be performed using the Katz index of ADL (table 1) [13]. This instrument is quick and easy to perform. In disabled patients discharged home after the ED visit, subsequent care has to be ensured to prevent ED re-admission. Disabled older ED patients should also be considered as candidates for early post-acute rehabilitation, in order to prevent nursing home admission [25].
It is important to have systematic approaches for older ED patients who take several medications, in order to reduce inappropriate medications and adverse drug-related events. In recent years, checklists have been developed to check for inappropriate medications in older patients [29, 30]. Furthermore, a variety of online tools are available to check for drug-drug interactions. Unfortunately, checklists and online tools are too time-consuming for most ED settings and most non-geriatricians are unfamiliar with these checklists. Ideally checklists for inappropriate medications and tools for checking drug-drug interactions are integrated in the electronic health record system and executed automatically when entering the medication of an older ED patient in the system. There is good evidence that such computerised support significantly reduces prescribing of inappropriate medications [31].
Older patients admitted to EDs are at risk of delayed evaluation due to undertriage [18]. The appropriate triage for older ED patients is still a matter of debate. A recent study showed that increased physicians’ awareness of the problem and better adherence to triage algorithms may reduce the risk of undertriage [32]. Some other authors recommend early geriatric assessment [33]. However, the term “triage” implicates that this initial evaluation has to be simple and fast. We conclude that the best triage approach for elderly patients is still unclear and more research in this area is needed.
Multidimensional geriatric assessment (MGA) (often called comprehensive geriatric assessment or CGA) is a diagnostic process, usually interdisciplinary, and is intended to determine an older person’s medical, psychosocial, functional and environmental resources, and problems, with the objective of developing an overall plan for treatment and long-term follow-up [34]. MGA incorporates functional tests for all relevant geriatric conditions needing attention in older ED patients (i.e., cognition, mobility, falls, and ADL). In older patients admitted to hospital, MGA reduces the risk of being institutionalised in a nursing home or dying by approximately 25% (relative risk reduction) and the number needed to treat is only 17 [6]. However, the commonly used functional tests for MGA require approximately 30 minutes, which is too time-consuming to apply in many ED settings.
To solve the problem of time with MGA, short and expeditious screening tools have been developed to identify older ED patients at increased risk, who should then receive MGA. A widely used screening tool is the Identification of Seniors at Risk (ISAR), which predicts a wide range of adverse health outcomes, including death, nursing home admission, or decline in physical or cognitive function (table 1) [35, 36]. The ISAR includes six simple questions which have to be answered by the patient with yes or no (e.g., whether the patient sees well, whether the patient has serious problems with his memory, or whether the patient takes more than three different medications every day). The problem with such screening tools is that they rely on patient self-report and not on objective performance tests for cognition or mobility. Therefore, it is conceivable that many patients with memory problems will not answer the corresponding question truthfully. In fact, the true prevalence of cognition problems in older ED patients is much higher than was found with the ISAR [37].
In response to the weaknesses of MGA and of short screening tools in the ED setting, a short multidimensional emergency geriatric screening (EGS) tool has recently been developed (table 1 and table 2) [5]. The EGS is based on short performance tests that have been validated in the ED [13, 19, 23]. It covers four domains relevant for older ED patients, namely cognition, mobility, falls, and ADL [5]. The EGS tool was feasible in the ED setting and took less than 5 minutes to perform in the majority of older ED patients. It revealed otherwise undetected conditions and predicted determinants of subsequent care. For example, older ED patients with limitations in three or four EGS domains had a 12–fold increase of being admitted to a nursing home after the hospital stay, as compared to older ED patients with fewer limitations [5]. The EGS tool may be suited for clinical routine in many ED settings.
The term “transitions of care” refers to the movements of a patient from one health care provider and/or setting of care (e.g., ED, hospital, primary care practice, nursing home) to another. Each transition constitutes a vulnerable phase, vulnerable to errors (e.g., medication prescription errors) and adverse events. Older patients, in particular those with functional deficits, are at greater risk of errors than younger patients. For example, a cognitively impaired patient discharged from the ED is prone to non-adherence and re-admission. There is good evidence that care transition programmes are a cost-effective way to reduce re-admissions, as well as mortality [38, 39]. Such programmes typically include interventions promoting communication between caregivers and continuity across settings of care.
In the coming decades, the proportion of older ED patients is expected to increase continuously. These patients are at greater risk of adverse outcomes than younger patients [1]. The currently used disease-oriented approaches do not sufficiently consider the complexity of older ED patients and their need for continuity. Though innovative instruments (e.g., ISAR) and novel care models (e.g., geriatric emergency room) have been introduced in clinical routine over the last two decades, further improvements are needed in the care of older ED patients. Such improvements are: 1) the implementation of brief screening tools for functional deficits along with appropriate management tailored to the specific needs of emergency physicians; 2) the systematic implementation of computerised systems reducing inappropriate medications and prescription errors; 3) the implementation of interventions improving continuity during transitions of care (e.g., integration of primary care physicians in the ED management of their patients); 4) education; and 5), last but not least, implementation of elder care boards and collaboration with interdisciplinary teams supported by geriatric specialists experienced in emergency care. The implementation and wide use of such age-centred approaches will help to further improve the quality of care for older ED patients.
Acknowledgment:The authors thank Professor Heinz Zimmermann for reading the manuscript and providing very constructive feedback.
1 Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med. 2002;39(3):238–47.
2 Coronado BE, Pope JH, Griffith JL, Beshansky JR, Selker HP. Clinical features, triage, and outcome of patients presenting to the ED with suspected acute coronary syndromes but without pain: a multicenter study. Am J Emerg Med. 2004;22(7):568–74.
3 Schoenenberger AW, Radovanovic D, Stauffer JC, Windecker S, Urban P, Eberli FR, et al.; Acute Myocardial Infarction in Switzerland Plus Investigators. Age-related differences in the use of guideline-recommended medical and interventional therapies for acute coronary syndromes: a cohort study. J Am Geriatr Soc. 2008;56(3):510–6.
4 Bingisser R, Nickel CH. The last century of symptom-oriented research in emergency presentations – have we made any progress? Swiss Med Wkly. 2013;143:w13829.
5 Schoenenberger AW, Bieri C, Ozgüler O, Moser A, Haberkern M, Zimmermann H, et al. A novel multidimensional geriatric screening tool in the ED: evaluation of feasibility and clinical relevance. Am J Emerg Med. 2014;32(6):623–8.
6 Ellis G, Whitehead MA, O’Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. 2011;(7):CD006211.
7 Hustey FM, Meldon SW. The prevalence and documentation of impaired mental status in elderly emergency department patients. Ann Emerg Med. 2002;39(3):248–53.
8 Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–22.
9 Lewis LM, Miller DK, Morley JE, Nork MJ, Lasater LC. Unrecognized delirium in ED geriatric patients. Am J Emerg Med. 1995;13(2):142–5.
10 Inouye SK, Rushing JT, Foreman MD, Palmer RM, Pompei P. Does delirium contribute to poor hospital outcomes? A three-site epidemiologic study. J Gen Intern Med. 1998;13(4):234–42.
11 Maguire PA, Taylor IC, Stout RW. Elderly patients in acute medical wards: factors predicting length of stay in hospital. Br Med J (Clin Res Ed). 1986;292(6530):1251–3.
12 Schoenenberger AW, Stortecky S, Neumann S, Moser A, Jüni P, Carrel T, et al. Predictors of functional decline in elderly patients undergoing transcatheter aortic valve implantation (TAVI). Eur Heart J. 2013;34(9):684–92.
13 Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9.
14 Wilber ST, Blanda M, Gerson LW. Does functional decline prompt emergency department visits and admission in older patients? Acad Emerg Med. 2006;13(6):680–2.
15 Caplan GA, Brown A, Croker WD, Doolan J. Risk of admission within 4 weeks of discharge of elderly patients from the emergency department – the DEED study. Discharge of elderly from emergency department. Age Ageing. 1998;27(6):697–702.
16 Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Ann Emerg Med. 2001;38(6):666–71.
17 Chin MH, Wang LC, Jin L, Mulliken R, Walter J, Hayley DC, et al. Appropriateness of medication selection for older persons in an urban academic emergency department. Acad Emerg Med. 1999;6(12):1232–42.
18 Platts-Mills TF, Travers D, Biese K, McCall B, Kizer S, LaMantia M, et al. Accuracy of the Emergency Severity Index triage instrument for identifying elder emergency department patients receiving an immediate life-saving intervention. Acad Emerg Med. 2010;17(3):238–43.
19 Carpenter CR, Bassett ER, Fischer GM, Shirshekan J, Galvin JE, Morris JC. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: brief Alzheimer’s Screen, Short Blessed Test, Ottawa 3DY, and the caregiver-completed AD8. Acad Emerg Med. 2011;18(4):374–84.
20 Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H. Validation of a short Orientation-Memory-Concentration Test of cognitive impairment. Am J Psychiatry. 1983;140(6):734–9.
21 Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990;113(12):941–8.
22 Grossmann FF, Hasemann W, Graber A, Bingisser R, Kressig RW, Nickel CH. Screening, detection and management of delirium in the emergency department – a pilot study on the feasibility of a new algorithm for use in older emergency department patients: the modified Confusion Assessment Method for the Emergency Department (mCAM-ED). Scand J Trauma Resusc Emerg Med. 2014;22:19.
23 Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
24 Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332(20):1338–44.
25 Bachmann S, Finger C, Huss A, Egger M, Stuck AE, Clough-Gorr KM. Inpatient rehabilitation specifically designed for geriatric patients: systematic review and meta-analysis of randomised controlled trials. BMJ. 2010;340:c1718.
26 Pfortmueller CA, Kunz M, Lindner G, Zisakis A, Puig S, Exadaktylos AK. Fall-related emergency department admission: fall environment and settings and related injury patterns in 6357 patients with special emphasis on the elderly. ScientificWorldJournal. 2014;2014:256519.
27 Pfortmueller CA, Lindner G, Exadaktylos AK. Reducing fall risk in the elderly: risk factors and fall prevention, a systematic review. Minerva Med. 2014 May 27. [Epub ahead of print]
28 Daniel H, Oesch P, Stuck AE, Born S, Bachmann S, Schoenenberger AW. Evaluation of a novel photography-based home assessment protocol for identification of environmental risk factors for falls in elderly persons. Swiss Med Wkly. 2013;143:w13884.
29 Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D. STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46(2):72–83.
30 Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24.
31 Terrell KM, Perkins AJ, Dexter PR, Hui SL, Callahan CM, Miller DK. Computerized decision support to reduce potentially inappropriate prescribing to older emergency department patients: a randomized, controlled trial. J Am Geriatr Soc. 2009;57(8):1388–94.
32 Grossmann FF, Zumbrunn T, Frauchiger A, Delport K, Bingisser R, Nickel CH. At risk of undertriage? Testing the performance and accuracy of the emergency severity index in older emergency department patients. Ann Emerg Med. 2012;60(3):317–25.
33 Rutschmann OT, Chevalley T, Zumwald C, Luthy C, Vermeulen B, Sarasin FP. Pitfalls in the emergency department triage of frail elderly patients without specific complaints. Swiss Med Wkly. 2005;135(9–10):145–50.
34 Rubenstein LZ, Stuck AE. Multidimensional geriatric assessment. In: Principles and Practice of Geriatric Medicine, Fifth Edition. Edited by Sinclair AJ, Morley JE and Vellas B. 2012 John Wiley & Sons.
35 McCusker J, Bellavance F, Cardin S, Trépanier S, Verdon J, Ardman O. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc. 1999;47(10):1229–37.
36 Graf CE, Giannelli SV, Herrmann FR, Sarasin FP, Michel JP, Zekry D, et al. Identification of older patients at risk of unplanned readmission after discharge from the emergency department – comparison of two screening tools. Swiss Med Wkly. 2012;141:w13327.
37 Goldberg SE, Whittamore KH, Harwood RH, Bradshaw LE, Gladman JR, Jones RG; Medical Crises in Older People Study Group. The prevalence of mental health problems among older adults admitted as an emergency to a general hospital. Age Ageing. 2012;41(1):80–6.
38 Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–8.
39 Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52(5):675–84.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.