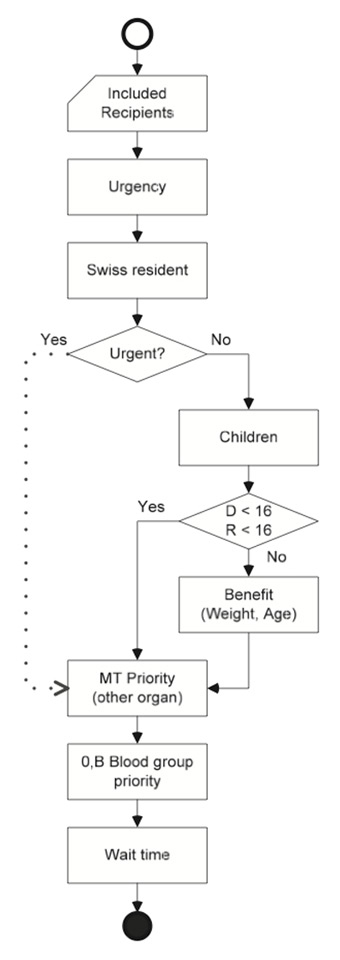
Figure 1
Heart allocation algorithm as implemented in the SOAS.
D = donor; MT = multi-organ transplantation; R = recipient
DOI: https://doi.org/10.4414/smw.2014.14057
During the last decade, the number of patients waiting for a cardiac transplant in Switzerland has almost tripled. In the meantime, the number of heart donors and transplantations performed has remained largely stable, at a low level [1]. With demand for donor organs exceeding the number of organs available for transplantation by far, unavoidably some of the eligible candidates will not receive a timely, often live-saving therapy. Thus, the mortality and morbidity on the Swiss heart transplant waiting list remain a major concern. Even though ventricular assist devices (VADs) are suitable for the stabilisation of patients and as a bridge to transplant, heart transplantation is currently the only established treatment for patients with end-stage heart failure, providing a significant survival benefit [2–5].
With the coming into force of the Swiss transplantation law on 1 July 2007, organ allocation policy changed from a centre-oriented to a patient-oriented national allocation. Along with this the Swiss Organ Allocation System (SOAS) was implemented which contains demographic and medical data of all transplant candidates and actual organ donors. Based on these data and an allocation algorithm, the SOAS computes the candidates’ positions on the waiting list, thereby guaranteeing organ allocation in accordance with the law. The aim of our retrospective analysis of SOAS data was to provide an overview on heart allocation and transplantation in Switzerland since the introduction of the SOAS.
We retrospectively analysed SOAS data related to heart allocation and transplantation between 1 July 2007 and 30 June 2013. This study includes all patients newly waitlisted for heart transplantation, all actual heart donors and all recipients of a cardiac transplant in Switzerland. In addition, the SOAS database was queried for all hearts offered for transplantation during the study period. No ethics committee approval was required for this study, as it contains exclusively non-patient identifiable registry data.
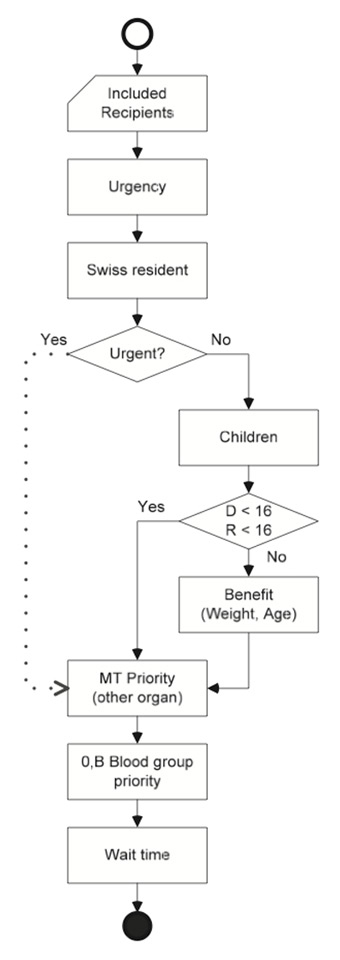
Figure 1
Heart allocation algorithm as implemented in the SOAS.
D = donor; MT = multi-organ transplantation; R = recipient
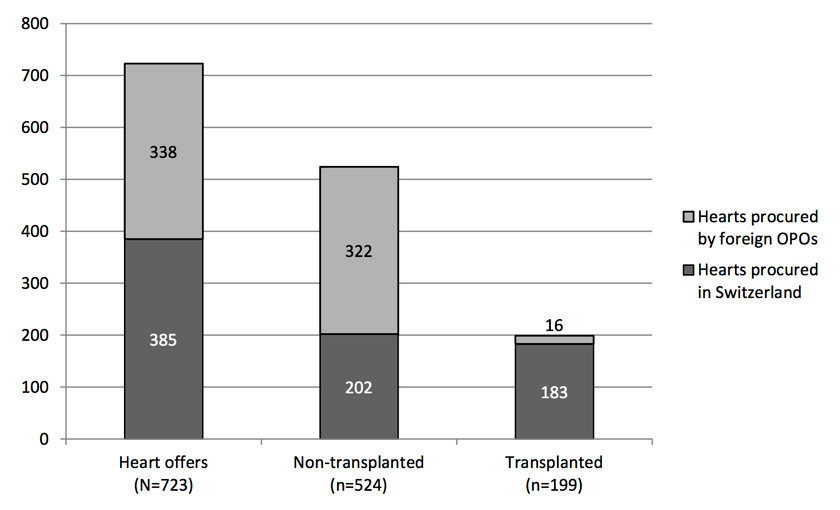
Figure 2
Heart offers: foreign vs Swiss procurement and non-transplanted vs transplanted.
The primary endpoint was the number of individuals newly waitlisted, the number of hearts offered for transplantation and the number of transplants performed. Secondary endpoints included patient characteristics and clinical data for donors and recipients, an assessment of the waiting list mortality as well as the quota of transplantations vs all heart offers.
The waiting list mortality was calculated as the number of patients who died while listed for a cardiac transplant expressed as a percentage of the comprehensive number of patients deceased while on the waiting list, transplanted and removed from the waiting list. The review of the heart offers included whether the donor organs were procured in Switzerland or offered by a foreign organ procurement organisation (OPO). These so-called “foreign offers” are organs for which no suitable recipient on the waiting list of the OPO of origin can be found. In order to minimise the loss of donor organs, such organs are being offered to OPOs of other countries for allocation to patients on their waiting list.
The SOAS is an Internet-based computer programme for the allocation of organs, run by the Federal Office of Public Health. It enables the national transplant coordinators at Swisstransplant, Switzerland’s OPO, to allocate the donor organs in compliance with the law. The SOAS database contains demographic and medical data of all waitlisted transplant candidates and actual organ donors in Switzerland. A patient’s position on the waiting list (SOAS rank) is determined in the SOAS, based on an organ-specific allocation algorithm that processes the donor data as well as demographic and medical data of all candidates (see fig. 1 for the heart allocation algorithm). The organ allocation ordinance defines four criteria for the allocation of organs which are (i.) medical urgency, (ii.) medical benefit, (iii.) equality of opportunity, and (iv.) time on waiting list [6].
A candidate for cardiac transplant may be listed in urgent status (highest medical urgency) if he or she fulfils at least one of the following criteria: (a.) the patient must be in an intensive care unit and require a high-dosed inotropic or equivalent vasoactive support; (b.) suffer from procedural complications after the implantation of a VAD; (c.) have experienced acute graft rejection; (d.) have a similarly poor prognosis without a transplant as patients who fulfil criteria a.–c. [6]. Patients listed in urgent status are given priority over candidates for elective transplantation, which is represented by the “Urgent? Yes/No” furcation in the allocation algorithm (fig. 1).
| Table 1: Patient characteristics of heart transplant candidates. | ||||||
| Total | ≥16 years | <16 years | ||||
| Patients on list on 30 June 2007 (n) | 27 | 27 | ||||
| Female (n, %) | 9 | (33.3%) | 9 | (33.3%) | ||
| Age (years; mean, ± 1 SD) | 46.4 | ±14 | 46.4 | ±14 | ||
| Weight (kg; mean, ± 1 SD) | 75.6 | ±18.8 | 75.6 | ±18.8 | ||
| Patients newly waitlisted during study period (n) | 300 | 271 | 29 | |||
| Female (n, %) | 85 | (28.3%) | 65 | (24.0%) | 20 | (69.0%) |
| Age (years; mean, ± 1 SD) | 45.7 | ±18.3 | 50.0 | ±13.2 | 5.2 | ±5.3 |
| Weight (kg; mean, ± 1 SD) | 70.0 | ±23.1 | 75.3 | ±16.5 | 21.3 | ±18.5 |
| Patients on list on 1 July 2013 (n) | 54 | 48 | 6 | |||
| Female (n, %) | 16 | (29.6%) | 12 | (25.0%) | 4 | (66.7%) |
| Age (years; mean, ± 1 SD) | 47.1 | ±19.4 | 52.4 | ±12.8 | 4.3 | ±5.8 |
| Weight (kg; mean, ± 1 SD) | 68.0 | ±25.1 | 74.4 | ±17.5 | 16.1 | ±13.9 |
During the 6 year study period, 300 patients were newly listed for a heart transplant in Switzerland, 199 patients received a transplant and 52 patients deceased while on the waiting list, whereof one was listed in urgent status. Of the 723 hearts offered by Swisstransplant to the three university hospitals with a heart transplant programme (Bern, Lausanne and Zurich), 524 (72.5%) were not transplanted. The main reasons for non-transplantation were poor organ quality due to age and pre-existing diseases, or transport time exceeding cold ischaemia time. Of the 199 patients on the waiting list who received a heart transplant, 26.1% (n = 52) were female and roughly half (n = 102) were between 41 and 60 years old.
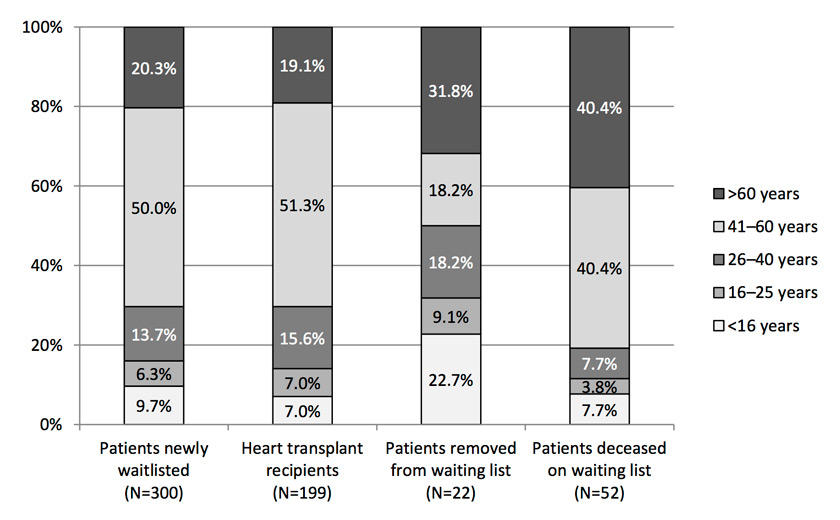
Figure 3
Age distribution of patients newly waitlisted, transplanted, removed from waiting list, and deceased on waiting list.
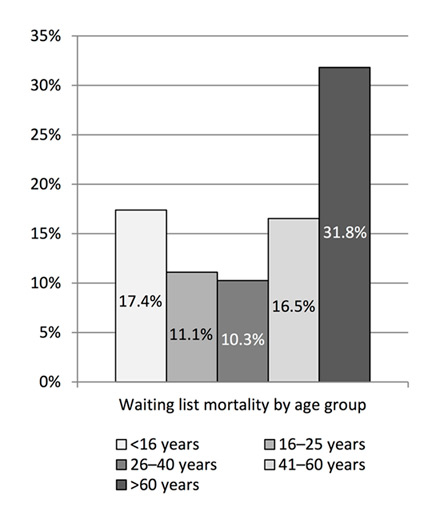
Figure 4
Waiting list mortality by age group.
Table 1 shows the patient characteristics of the individuals waiting for a heart transplant, including patients with a VAD as bridge to transplant. At the beginning of the analysed period, 27 candidates were on the waiting list. By the end of the study period the heart waiting list included 54 patients. During the 6 analysed years, 50 patients were newly listed for a heart transplantation, on average per year. Of these, 90.3% were 16 years or older (mean age 50 ± 13.2 years) and 9.7% younger than 16 (mean age 5.2 ± 5.3 years). While female patients accounted for roughly one fourth of candidates above 16 years in the newly listed group, they represented more than two thirds of paediatric candidates.
Figure 2 visualises the proportion of hearts offered to the transplant centres, those deemed unsuitable for transplantation by the specialists in the transplant centres, and the hearts transplanted. During the study period, 723 hearts were offered for transplantation and 199 (27.5%) were transplanted. Of all heart offers, 53.3% were offered from donors deceased in Switzerland and 46.7% by a foreign OPO. The 61.5% of foreign offers in the non-transplanted category reflects the fact that the approximate 4 hour cold ischaemia time for the heart is a major limiting factor in international organ exchange. Accordingly, only 4.7% of hearts offered by foreign OPOs were actually transplanted to candidates on the Swiss waiting list compared with the 47.5% transplant rate of hearts procured in Switzerland. Of the 199 hearts transplanted during the study period, 92.0% were procured in Switzerland and 8.0% were offered by a foreign OPO. Of the 385 hearts procured in Switzerland, 25 (6.5%) were transplanted to patients on the waiting lists of foreign OPOs.
Tables 2 and 3 show the patient characteristics of heart donors and recipients, respectively. The comparison reveals that in the donor group, the proportion of females was higher (34.2% vs 26.1%) and the mean age was lower (40.2 vs 46.4 years) than in the recipient group. Overall, 50.8% of donors had a history of nicotine dependence and 26.6% were resuscitated. The mean SOAS rank (designating the recipient’s position on the waiting list) was 2.2 ± 2.0 for the donor hearts, indicating that, in a majority of cases, the organs were not allocated to the patient in first position on the waiting list, but on average to the candidate on second position. Allocation to patients with SOAS rank >1 may take place in a variety of scenarios in which a transplantation of the donor heart to the candidate on first position would result in a lack of estimated medical benefit. Such scenarios include cases in which the patient on first position was listed in urgent status (resulting in SOAS rank 1 by default) but there is a donor-recipient mismatch (age and/or weight), when an extended criteria donor organ is allocated to a suitable recipient instead of the patient on first position, or in cases of elective transplantation with a positive crossmatch or an optimal compatibility of donor and recipient characteristics. The average waiting time for a heart transplantation was 233 ± 240 days, and 26.1% of recipients were transplanted with a heart while listed in urgent status. The mean cold ischaemia time of hearts transplanted during the study period was 161 ± 53 minutes.
Figure 3 shows that the age distribution of the 300 patients newly listed for a heart transplant was very similar to the age distribution of the 199 heart transplant recipients (first and second column). In both groups, half of the patients were between 41 and 60 years old. The third column shows the age distribution of the 22 patients who were removed from the waiting list due to improvement or deterioration of condition, patient reluctance or other reasons. Among these patients, those over 60 years old were the largest group. Of the 52 patients deceased on the heart waiting list (fourth column), the percentage of patients older than 60 years was approximately twice as big as the percentage in the same age group of patients newly listed or transplanted. The overall waiting list mortality during the study period was 19.0%. Figure 4 displays the mortality by age group, showing that it was highest among patients older than 60 years (31.8%) and lowest in patients aged between 26 and 40 years (10.3%).
| Table 2: Patient characteristics and clinical data of donors. | ||
| Heart donors from whom the heart was transplanted (n = 199) | ||
| Female (n, %) | 68 | (34.2%) |
| Age (years; mean, ± 1 SD) | 40.2 | ±15.9 |
| Weight (kg; mean, ± 1 SD) | 73.1 | ±17.5 |
| Height (cm; mean, ± 1 SD) | 171.5 | ±18.3 |
| Blood group | ||
| A | 86 | (43.2%) |
| 0 | 93 | (46.7%) |
| B | 16 | (8.0%) |
| AB | 4 | (2.0%) |
| Medical history | ||
| Hypertension (yes; n, %) | 22 | (11.1%) |
| Diabetes mellitus (yes; n, %) | 4 | (2.0%) |
| Nicotine dependence (yes; n, %) | 101 | (50.8%) |
| Resuscitation (yes; n, %) | 53 | (26.6%) |
| Duration of resuscitation (min; mean, ± 1 SD) | 20.3 | ±16.5 |
| Laboratory results | ||
| cTnI (µg/l; mean, ± 1 SD) | 1.6 | ±6.6 |
| Additional examinations | ||
| Heart echography (yes; n, %) | 195 | (98.0%) |
| LVEF (%; mean, ± 1 SD) | 61 | ±7 |
| Coronary angiogram (yes; n, %) | 103 | (51.8%) |
| LVEF (%; mean, ± 1 SD) | 64 | ±8 |
| Coronary artery disease (yes; n, %) | 18 | (9.0%) |
| SOAS rank (mean, ± 1 SD) | 2.2 | ±2.0 |
| cTnI = cardiac troponin I; LVEF = left ventricular ejection fraction; SOAS = Swiss Organ Allocation System | ||
| Table 3: Patient characteristics and clinical data of transplant recipients. | ||
| Heart transplant recipients (n = 199) | ||
| Female (n, %) | 52 | (26.1%) |
| Age (years; mean, ± 1 SD) | 46.4 | ±16.7 |
| Weight (kg; mean, ± 1 SD) | 71.3 | ±19.6 |
| Height (cm; mean, ± 1 SD) | 168.4 | ±19.1 |
| Blood group | ||
| A (n, %) | 89 | (44.7%) |
| 0 (n, %) | 76 | (38.2%) |
| B (n, %) | 22 | (11.1%) |
| AB (n, %) | 12 | (6.0%) |
| Time on waiting list (days; mean, ± 1 SD) | 233 | ±240 |
| Cold ischaemia time (min; mean, ± 1 SD) | 161 | ±53 |
| Transplanted while listed in urgent status (n, %) | 52 | (26.1%) |
This study is the first comprehensive overview of heart transplant activity in Switzerland since the coming into force of the national transplant law. On 1 July 2007, the starting point of our data analysis, 27 patients were on the waiting list for a cardiac transplant. During the 6 year study period, the average number per year of patients newly listed, transplanted and deceased while awaiting transplantation was 50.0, 33.2 and 8.7 respectively. As of the end of our study, the Swiss waiting list for heart transplantation included 54 patients.
We observed only minor variations in the patient characteristics of heart transplant candidates during the study period, except for an increase of 6 years in the mean age of candidates older than 16 years, and for the fact that initially, no paediatric patients were listed at all (table 1).
The overall ratio of hearts transplanted vs offered was 27.5% in our study (fig. 2). This relatively low percentage of actual allocations can be attributed to the large number of heart offers from foreign OPOs, of which only 4.7% were transplanted. Still, international organ exchange seems to be gaining importance for the Swiss transplant activity, as 8.0% of all hearts transplanted during the study period were offered by foreign OPOs, whereas a previous evaluation showed that between 2004 and 2008, foreign offers accounted for only 5.8% of all hearts transplanted to patients on the Swiss waiting list [7]. It is noteworthy, however, that in our study, more hearts procured in Switzerland were transplanted to patients on the waiting lists of foreign OPOs than vice versa. The quota of transplants with hearts procured in Switzerland exclusively (47.5%) was higher than it was in the years 1998–2008 (40.0%) [8]. The fact that Switzerland, with its pool of donors and recipients being limited by the population size (which increases the odds that no compatible candidate on the waiting list can be found), may in part explain why the percentage of hearts transplanted is lower than in larger OPOs, such as the 67.4% of heart offers transplanted in the Eurotransplant area in 2012 [9]. Also, some of the difference may be due to different allocation policies for extended criteria and marginal donors.
With regard to the patient characteristics of the heart donors (table 2), we found a 6.2 year decrease in the average age compared with a previous assessment of donor characteristics [8]. The 40.2-year mean donor age in our study matches the 40.4 years reported for Europe by the International Society for Heart and Lung Transplantation (ISHLT) for the 2006 to 2012 period [10]. Out of all the donors from whom the heart was transplanted during the six years we analysed, 26.6% underwent resuscitation and 50.8% had a history of nicotine dependence. The percentage of donors with a smoking history in our study was more than twice as big as in the ISHLT report.
The transplant recipients were 46.4 years old on average (table 3), which is younger than the 50.2 years mean age of recipients in Europe published by the ISHLT [10]. This report, however, includes only adult patients, while about 10% of our study population were paediatric patients. As shown in figure 3, the age distribution was almost identical in the groups of transplant recipients and candidates newly waitlisted. In contrast, patients older than 60 years were overrepresented in the group removed from the waiting list and, even more markedly, in the group deceased on the waiting list. This is also reflected by the fact that patients aged 60 and above were subject to the highest waiting list mortality by far (fig. 4). In view of the major technical advances achieved lately in mechanical circulatory support, the implantation of a VAD as destination therapy may be considered as an alternative to transplantation in selected older patients [11–14]. In severely symptomatic patients whose only alternative is medical management, a lifetime VAD implant seems to result in improved survival, functional status and quality of life [13, 14]. At present, however, it remains debatable to what extent VADs can provide equal results to transplantation in terms of functional status and quality of life [12].
The overall 19.0% waiting list mortality in our study was higher than the 5% reported by the Spanish Registry of Heart Transplantation for 2012 and the 12.1% calculated from 2011 data published by the Agence de la biomédecine, but lower than the 24.6% as calculated from the Eurotransplant data for the years 2008 to 2012 [9, 15, 16]. This wide range of mortality rates among OPOs is striking although it seems natural to assume that the waiting list mortality would be lower in countries with a high organ donation rate, such as Spain or France. The differences between the OPOs are even bigger if one looks at the ratios of urgent vs elective transplants. Our analysis showed that 26.1% of all candidates received a cardiac transplant while listed in urgent status, which is a remarkably low in international comparison. In Spain, the percentage of urgent transplantations ranged from 32 to 38% in the equivalent observation period, while recent studies from Germany and the USA revealed that 90% or more of their recipients were transplanted while listed in urgent status [15, 17, 18].
This study is a retrospective analysis of registry data and therefore has the shortcomings associated with this type of study design. However, due to the fact that the data were used in the SOAS for organ allocation, a high standard of data quality may be expected. Being the first comprehensive assessment of the heart transplant activity since the introduction of the SOAS, our study provides key figures and an important insight in the current practice of heart allocation in Switzerland.
Switzerland is faced with an increasing heart transplant waiting list, as since 2007, significantly more patients were newly waitlisted than transplanted. Compared with the international data, the acceptance rate of heart offers and the rate of urgent transplantations are relatively low, whereas the mortality rate on the waiting list is elevated. In view of the relatively low acceptance rate, a re-evaluation of the donor selection criteria may be appropriate, although this should, of course, not be done at the cost of compromising the outcome. A continued close collaboration between the experts of the STAH is warranted to keep the number of patients listed in urgent status low, thereby permitting a maximum amount of elective transplantations. The fact that candidates aged 60 and above suffered from the highest waiting list mortality suggests that the latest generation of VADs as a destination therapy should be considered as an alternative to transplantation in selected patients. The data presented in this study may serve as evidence in the decision making whether or not a patient ought to be listed for a cardiac transplantation.
Acknowledgements: The authors would like to thank Danick Gut for proofreading the manuscript. The members of the Swisstransplant Heart Working Group (STAH) are: Lars Englberger, MD, Department of Cardiovascular Surgery, Bern University Hospital; Prof Roger Hullin, MD, Department of Cardiology, Centre Hospitalier Universitaire Vaudois, Lausanne; Michele Martinelli, MD, Swiss Cardiovascular Centre, Bern University Hospital; Prof Frank Ruschitzka, MD, Division of Cardiology, Zurich University Hospital; Piergiorgio Tozzi, MD, Department of Cardiovascular Surgery, Centre Hospitalier Universitaire Vaudois, Lausanne; Markus Wilhelm, MD, Clinic for Cardiovascular Surgery, Zurich University Hospital.
1 Swisstransplant. Jahresbericht [annual report]. Bern: Schweizerische Nationale Stiftung für Organspende und Transplantation, 2012 [cited 2014, Jan 13]. Available from: www.swisstransplant.org
2 Deng MC, Ardehali A, Shemin R, Hickey A, MacLellan WR, Fonarow G. Relative roles of heart transplantation and long-term mechanical circulatory support in contemporary management of advanced heart failure – a critical appraisal 10 years after REMATCH. Eur J Cardiothorac Surg. 2011;40:781–2.
3 Mancini D, Lietz K. Selection of cardiac transplantation candidates in 2010. Circulation. 2010;122:173–83.
4 Lietz K, Miller LW. Improved survival of patients with end-stage heart failure listed for heart transplantation: analysis of organ procurement and transplantation network/U.S. United Network of Organ Sharing data, 1990 to 2005. J Am Coll Cardiol. 2007;50:1282–90.
5 Attisani M, Centofanti P, La Torre M, Boffini M, Ricci D, Ribezzo M, et al. Advanced heart failure in critical patients (INTERMACS 1 and 2 levels): ventricular assist devices or emergency transplantation? Interact Cardiovasc Thorac Surg. 2012;15:678–84.
6 SR 810.212.41. Verordnung des EDI über die Zuteilung von Organen zur Transplantation (Organzuteilungsverordnung EDI) vom 2. Mai 2007 (Stand am 1. Juli 2013) [organ allocation ordinance; cited 2014, Jan 13]. Available from: http://www.admin.ch/opc/de/classified-compilation/20062074/201307010000/810.212.41.pdf
7 Schneider S, Schreiner P, Weiss J, Immer FF. Assessing the potential of international organ exchange – the Swiss experience. Eur J Cardiothorac Surg. 2011;40:1368–73.
8 Weiss J, Hofmann SP, Immer FF. Patient Characteristics of Deceased Organ Donors in Switzerland 1998–2008. Swiss Med Wkly. 2011;141:w13265.
9 Eurotransplant. Annual report 2012. Leiden: Eurotransplant International Foundation, 2012 [cited 2014, Jan 13]. Available from: http://www.eurotransplant.org/cms/mediaobject.php?file=AR2012.pdf
10 Lund LH, Edwards LB, Kucheryavaya AY, Dipchand AI, Benden C, Christie JD, et al. The registry of the International Society for Heart and Lung Transplantation: thirtieth official adult heart transplant report – 2013; focus theme: age. J Heart Lung Transpl. 2013;32:951–64.
11 Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson L, Miller M, et al. Long-term mechanical circulatory support (destination therapy): on track to compete with heart transplantation? J Thorac Cardiovasc Surg. 2012;144:584–603.
12 Wilhelm MJ, Ruschitzka F, Falk V. Destination therapy – time for a paradigm change in heart failure therapy. Swiss Med Wkly. 2013;143:w13729.
13 Westaby S, Deng M. Continuous flow blood pumps: the new gold standard for advanced heart failure? Eur J Cardiothorac Surg. 2013;44:4–8.
14 Aggarwal S, Slaughter MS. Ventricular assist devices for destination therapy. In: Morgan JA, Naka Y (eds). Surgical treatment for advanced heart failure. New York: Springer, 2013:137–148.
15 Almenar L, Segovia J, Crespo-Leiro MG, Palomo J, Arizón JM, González-Vílchez F, et al. Spanish Registry on Heart Transplantation. 23rd official report of the Spanish Society of Cardiology Working Group on Heart Failure and Heart Transplantation (1984–2011). Rev Esp Cardiol. 2012;65:1030–8.
16 Agence de la biomédecine. Procurement and transplantation of organs and tissue; 2011 data [cited 2014, Jan 13]. Available from: http://www.agence-biomedecine.fr/Procurement-and-transplantation-of,530?lang=fr
17 Smits JM. Actual situation in Eurotransplant regarding high urgent heart transplantation. Eur J Cardiothorac Surg. 2012;42:609–11.
18 Stevenson L. The urgent priority for transplantation is to trim the waiting list. J Heart Lung Transpl. 2013;32:861–7.
Funding / potential competing interests: No financial support and no other potential conflict of interest relevant to this article was reported.